dffc7af7b2c77dcdf497b7248bf3d262.ppt
- Количество слайдов: 43
 Pain Management and Addiction Medicine Russell K. Portenoy, MD Chairman, Department of Pain Medicine and Palliative Care Gerald J. Friedman Chair in Pain Medicine and Palliative Care Beth Israel Medical Center Professor of Neurology and Anesthesiology Albert Einstein College of Medicine New York, New York
Pain Management and Addiction Medicine Russell K. Portenoy, MD Chairman, Department of Pain Medicine and Palliative Care Gerald J. Friedman Chair in Pain Medicine and Palliative Care Beth Israel Medical Center Professor of Neurology and Anesthesiology Albert Einstein College of Medicine New York, New York
 Pain Management and Addiction Medicine ¨ Role of opioid therapy in pain management ¨ Risk management during opioid therapy for pain ¨ Other issues – New formulations
Pain Management and Addiction Medicine ¨ Role of opioid therapy in pain management ¨ Risk management during opioid therapy for pain ¨ Other issues – New formulations
 Opioid Therapy: 2011 ¨ Acute pain – International consensus that opioid therapy is first line for moderate to severe acute pain ¨ Chronic pain related to active cancer or other advanced illness – International consensus that opioid therapy is first line for moderate to severe pain 3
Opioid Therapy: 2011 ¨ Acute pain – International consensus that opioid therapy is first line for moderate to severe acute pain ¨ Chronic pain related to active cancer or other advanced illness – International consensus that opioid therapy is first line for moderate to severe pain 3
 Opioid Therapy: 2011 ¨ Long-term opioid therapy for so-called chronic non-cancer pain – Pain specialists agree that long-term opioid therapy is safe and effective for some patients – Risks are significant and must be understood and managed – No consensus about the positioning of this therapy, patient selection, or treatment guidelines 4
Opioid Therapy: 2011 ¨ Long-term opioid therapy for so-called chronic non-cancer pain – Pain specialists agree that long-term opioid therapy is safe and effective for some patients – Risks are significant and must be understood and managed – No consensus about the positioning of this therapy, patient selection, or treatment guidelines 4
 Chronic Pain: Immense Public Health Problem ¨ Persistent pain in primary care: WHO Study – 5438 primary care patients from 15 sites in 14 countries assessed by interview and questionnaires – 22% had persistent pain (>6 months + care or disability) • More likely to have anxiety or depressive disorder (OR=4. 14) – Pain-distress relationships were more consistent across cultures than pain-disability Gureje et al, JAMA, 1998: 280: 147
Chronic Pain: Immense Public Health Problem ¨ Persistent pain in primary care: WHO Study – 5438 primary care patients from 15 sites in 14 countries assessed by interview and questionnaires – 22% had persistent pain (>6 months + care or disability) • More likely to have anxiety or depressive disorder (OR=4. 14) – Pain-distress relationships were more consistent across cultures than pain-disability Gureje et al, JAMA, 1998: 280: 147
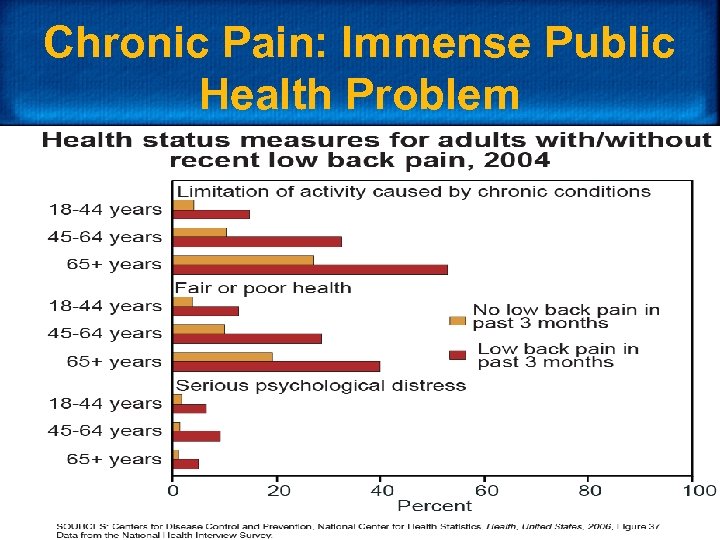 Chronic Pain: Immense Public Health Problem
Chronic Pain: Immense Public Health Problem
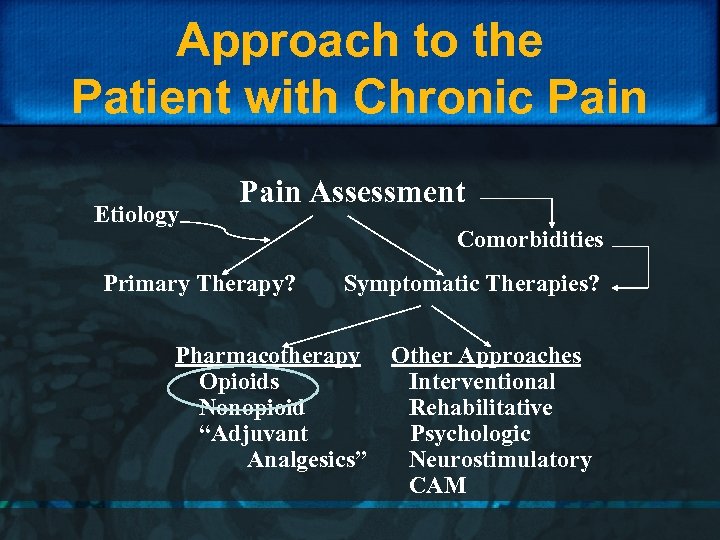 Approach to the Patient with Chronic Pain Etiology Pain Assessment Primary Therapy? Comorbidities Symptomatic Therapies? Pharmacotherapy Opioids Nonopioid “Adjuvant Analgesics” Other Approaches Interventional Rehabilitative Psychologic Neurostimulatory CAM
Approach to the Patient with Chronic Pain Etiology Pain Assessment Primary Therapy? Comorbidities Symptomatic Therapies? Pharmacotherapy Opioids Nonopioid “Adjuvant Analgesics” Other Approaches Interventional Rehabilitative Psychologic Neurostimulatory CAM
 Key Issue in Positioning Opioid Therapy: Effectiveness ¨ Many RCTs and systematic reviews yield mixed findings and provide little help in developing evidence-based therapy
Key Issue in Positioning Opioid Therapy: Effectiveness ¨ Many RCTs and systematic reviews yield mixed findings and provide little help in developing evidence-based therapy
 Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for chronic noncancer pain ¨ Meta-analysis of RCTs through May, 2005 ¨ 41 RCTs (N=6019) of any oral opioid therapy for any type of pain, with study duration averaging 5 weeks (range 1 -16) ¨ Opioids outperformed placebo for pain and functional outcomes in nociceptive and neuropathic pain, and fibromyalgia ¨ “Strong” opioids were superior to naproxen and nortriptyline only for pain relief Furlan AD et al. , CMAJ. 2006 May 23; 174(11): 1589 -94
Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for chronic noncancer pain ¨ Meta-analysis of RCTs through May, 2005 ¨ 41 RCTs (N=6019) of any oral opioid therapy for any type of pain, with study duration averaging 5 weeks (range 1 -16) ¨ Opioids outperformed placebo for pain and functional outcomes in nociceptive and neuropathic pain, and fibromyalgia ¨ “Strong” opioids were superior to naproxen and nortriptyline only for pain relief Furlan AD et al. , CMAJ. 2006 May 23; 174(11): 1589 -94
 Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for chronic noncancer pain ¨ Conclusion: There is short-term efficacy for pain and function in all types of pain; opioids are better than other drugs for pain, but not functional outcomes. There are insufficient data to judge long-term outcomes. Furlan AD et al. , CMAJ. 2006 May 23; 174(11): 1589 -94
Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for chronic noncancer pain ¨ Conclusion: There is short-term efficacy for pain and function in all types of pain; opioids are better than other drugs for pain, but not functional outcomes. There are insufficient data to judge long-term outcomes. Furlan AD et al. , CMAJ. 2006 May 23; 174(11): 1589 -94
 Key Issue in Positioning Opioid Therapy: Effectiveness Opioid treatment for chronic back pain ¨ Systematic review and meta-analysis through 2005 ¨ Studies of oral, topical, or transdermal opioids for chronic back pain, with study duration less than 16 weeks ¨ Meta-analysis of 4 studies of opioids vs. placebo or nonopioid did not show efficacy (p=0. 136) ¨ Meta-analysis of 5 studies of different opioids did not show reduced baseline pain (p=0. 055) ¨ Abuse behaviors ranged from 5% to 24% Martell BA et al. Ann Intern Med. 2007; 146: 116 -27
Key Issue in Positioning Opioid Therapy: Effectiveness Opioid treatment for chronic back pain ¨ Systematic review and meta-analysis through 2005 ¨ Studies of oral, topical, or transdermal opioids for chronic back pain, with study duration less than 16 weeks ¨ Meta-analysis of 4 studies of opioids vs. placebo or nonopioid did not show efficacy (p=0. 136) ¨ Meta-analysis of 5 studies of different opioids did not show reduced baseline pain (p=0. 055) ¨ Abuse behaviors ranged from 5% to 24% Martell BA et al. Ann Intern Med. 2007; 146: 116 -27
 Key Issue in Positioning Opioid Therapy: Effectiveness Opioid treatment for chronic back pain ¨ CONCLUSIONS: Opioids have limited, if any, short-term value in chronic low back pain. Evidence about substance abuse is too limited to draw any conclusions. There are insufficient data to judge longterm outcomes. Martell BA et al. Ann Intern Med. 2007; 146: 116 -27
Key Issue in Positioning Opioid Therapy: Effectiveness Opioid treatment for chronic back pain ¨ CONCLUSIONS: Opioids have limited, if any, short-term value in chronic low back pain. Evidence about substance abuse is too limited to draw any conclusions. There are insufficient data to judge longterm outcomes. Martell BA et al. Ann Intern Med. 2007; 146: 116 -27
 Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for noncancer pain: surveys ¨ Systematic review of open-label prospective studies through April, 2007 ¨ 17 studies (N=3079) of oral, transdermal or neuraxial opioid, with study duration at least 6 months ¨ Many patients stopped treatment due to AEs or poor response (oral 32. 5%, transdermal 17. 5%, neuraxial 6. 3%) ¨ Signs of addiction in 0. 05%; abuse in 0. 43% ¨ Small but significant pain reduction for oral therapy (mean 1. 99 points) and neuraxial therapy (mean 1. 33 points); too few data to judge transdermal Noble M et al. , JPSM. 2008; 35: 214 -228
Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for noncancer pain: surveys ¨ Systematic review of open-label prospective studies through April, 2007 ¨ 17 studies (N=3079) of oral, transdermal or neuraxial opioid, with study duration at least 6 months ¨ Many patients stopped treatment due to AEs or poor response (oral 32. 5%, transdermal 17. 5%, neuraxial 6. 3%) ¨ Signs of addiction in 0. 05%; abuse in 0. 43% ¨ Small but significant pain reduction for oral therapy (mean 1. 99 points) and neuraxial therapy (mean 1. 33 points); too few data to judge transdermal Noble M et al. , JPSM. 2008; 35: 214 -228
 Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for noncancer pain: surveys ¨ Conclusion: Many patients stop therapy but there is weak evidence that those who continue have pain relief over time. There are insufficient data to judge other longterm outcomes, including function and drug abuse. Noble M et al. , JPSM. 2008; 35: 214 -228
Key Issue in Positioning Opioid Therapy: Effectiveness Opioids for noncancer pain: surveys ¨ Conclusion: Many patients stop therapy but there is weak evidence that those who continue have pain relief over time. There are insufficient data to judge other longterm outcomes, including function and drug abuse. Noble M et al. , JPSM. 2008; 35: 214 -228
 Key Issue in Positioning Opioid Therapy: Effectiveness ¨ Conclusions – RCTs suggest efficacy but have very limited relevance to long-term therapy – Observational studies provide weak evidence that many patients stop therapy due to side effects or poor response, but those who continue may benefit – Other outcomes, including those related to risk, are poorly characterized
Key Issue in Positioning Opioid Therapy: Effectiveness ¨ Conclusions – RCTs suggest efficacy but have very limited relevance to long-term therapy – Observational studies provide weak evidence that many patients stop therapy due to side effects or poor response, but those who continue may benefit – Other outcomes, including those related to risk, are poorly characterized
 Positioning Opioid Therapy ¨ Despite limited evidence, APS-AAPM evidence-based guidelines: – Support consideration of an opioid trial for all patients with severe pain, but case-by-case decision based on an analysis: • • What is conventional practice? Are there reasonable alternatives? Is there relatively high risk of adverse effects? Is the patient likely to be a responsible drug-taker? Chou R et al. J Pain 2009; 10: 113 -130
Positioning Opioid Therapy ¨ Despite limited evidence, APS-AAPM evidence-based guidelines: – Support consideration of an opioid trial for all patients with severe pain, but case-by-case decision based on an analysis: • • What is conventional practice? Are there reasonable alternatives? Is there relatively high risk of adverse effects? Is the patient likely to be a responsible drug-taker? Chou R et al. J Pain 2009; 10: 113 -130
 Positioning Opioid Therapy ¨ Trends over two decades – Rapid increase in opioid use by pain specialists and primary care physicians – Rapid increase in adverse outcomes • Abuse, addiction and diversion • Unintentional overdose – Evolving responses by the • Clinical community • Regulatory and law enforcement communities
Positioning Opioid Therapy ¨ Trends over two decades – Rapid increase in opioid use by pain specialists and primary care physicians – Rapid increase in adverse outcomes • Abuse, addiction and diversion • Unintentional overdose – Evolving responses by the • Clinical community • Regulatory and law enforcement communities
 Trends in Long-Term Opioid Use ¨ Study of health care claims data – From 1997 to 2005, age-gender groups had an increased • incidence of long-term opioid use by 16% to 87% • prevalence of long-term opioid use by 61% to 135% – Women used more opioids than men and older women had the highest prevalence (8%-9%) – Sedative-hypnotics commonly used with opioids Campbell CI et al. Am J Public Health 2010; 100: 2541 -7
Trends in Long-Term Opioid Use ¨ Study of health care claims data – From 1997 to 2005, age-gender groups had an increased • incidence of long-term opioid use by 16% to 87% • prevalence of long-term opioid use by 61% to 135% – Women used more opioids than men and older women had the highest prevalence (8%-9%) – Sedative-hypnotics commonly used with opioids Campbell CI et al. Am J Public Health 2010; 100: 2541 -7
 Trends in Opioid Use: Patients with SUD ¨ Study of health care claims data – From 1997 to 2005, prevalence of long-term opioid use • Increased from 7. 6% to 18. 6% in patients with SUD • Increased from 2. 7% to 4. 2% in those w/o SUD • Dx of opioid disorder among those treated increased from 15. 7% to 52. 4% • Those with prior SUD received higher doses, more Schedule II and long-acting opioids, and more sedative-hypnotics Weisner, et al. Pain 2009; 145: 287 -93.
Trends in Opioid Use: Patients with SUD ¨ Study of health care claims data – From 1997 to 2005, prevalence of long-term opioid use • Increased from 7. 6% to 18. 6% in patients with SUD • Increased from 2. 7% to 4. 2% in those w/o SUD • Dx of opioid disorder among those treated increased from 15. 7% to 52. 4% • Those with prior SUD received higher doses, more Schedule II and long-acting opioids, and more sedative-hypnotics Weisner, et al. Pain 2009; 145: 287 -93.
 Trends in Opioid Use: Commercial vs M’Caid ¨ Study of health care claims data in a MCO and a Medicaid population – In 2000, chronic opioid therapy • MCO population: 8% in those with mental health disorder (MHD) or SUD vs 3% w/o MHD or SUD • Medicaid: 20% with MHD or SUD vs 13% w/o MHD or SUD – From 2000 to 2005, chronic opioid therapy • MCO population: increased 34. 9% in those with MHD or SUD vs. 27. 8% w/o MHD or SUD • Medicaid: increased 55. 4% in those with MHD or SUD vs. 39. 8% w/o MHD or SUD Edlund MJ, et al. Clin J Pain. 2010; 26(1): 1 -8
Trends in Opioid Use: Commercial vs M’Caid ¨ Study of health care claims data in a MCO and a Medicaid population – In 2000, chronic opioid therapy • MCO population: 8% in those with mental health disorder (MHD) or SUD vs 3% w/o MHD or SUD • Medicaid: 20% with MHD or SUD vs 13% w/o MHD or SUD – From 2000 to 2005, chronic opioid therapy • MCO population: increased 34. 9% in those with MHD or SUD vs. 27. 8% w/o MHD or SUD • Medicaid: increased 55. 4% in those with MHD or SUD vs. 39. 8% w/o MHD or SUD Edlund MJ, et al. Clin J Pain. 2010; 26(1): 1 -8
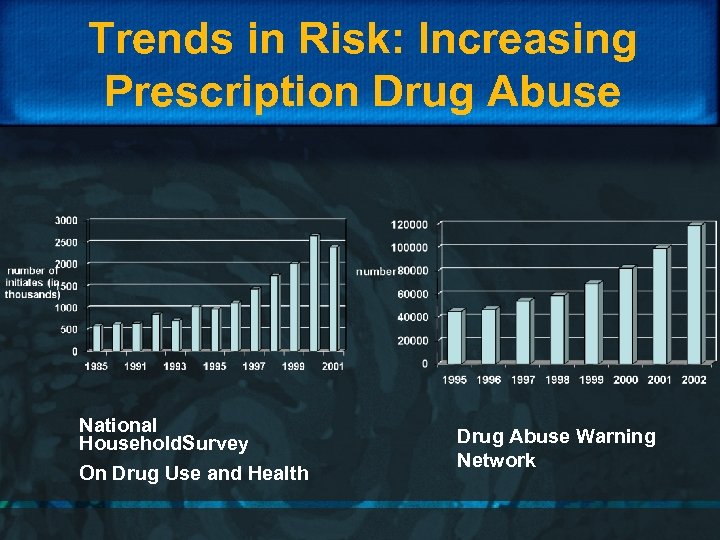 Trends in Risk: Increasing Prescription Drug Abuse National Household. Survey On Drug Use and Health Drug Abuse Warning Network
Trends in Risk: Increasing Prescription Drug Abuse National Household. Survey On Drug Use and Health Drug Abuse Warning Network
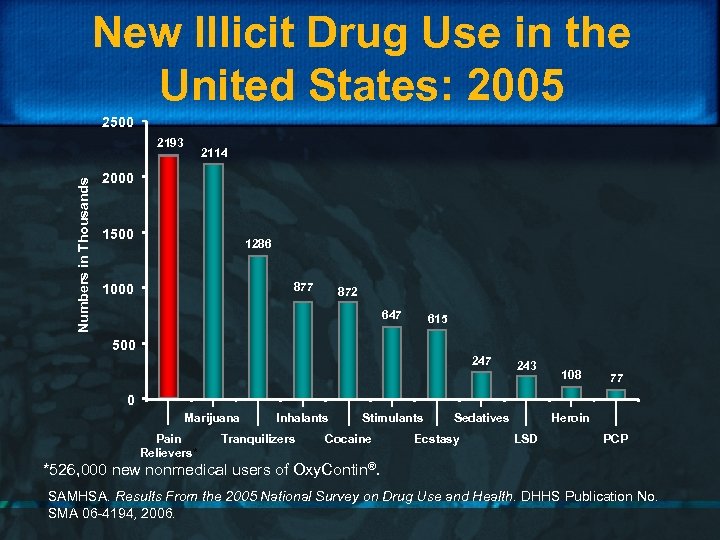 New Illicit Drug Use in the United States: 2005 2500 Numbers in Thousands 2193 2114 2000 1500 1286 877 1000 872 647 615 500 247 243 108 77 0 Marijuana Pain Relievers* Inhalants Tranquilizers Stimulants Cocaine Sedatives Ecstasy Heroin LSD PCP *526, 000 new nonmedical users of Oxy. Contin®. SAMHSA. Results From the 2005 National Survey on Drug Use and Health. DHHS Publication No. SMA 06 -4194, 2006.
New Illicit Drug Use in the United States: 2005 2500 Numbers in Thousands 2193 2114 2000 1500 1286 877 1000 872 647 615 500 247 243 108 77 0 Marijuana Pain Relievers* Inhalants Tranquilizers Stimulants Cocaine Sedatives Ecstasy Heroin LSD PCP *526, 000 new nonmedical users of Oxy. Contin®. SAMHSA. Results From the 2005 National Survey on Drug Use and Health. DHHS Publication No. SMA 06 -4194, 2006.
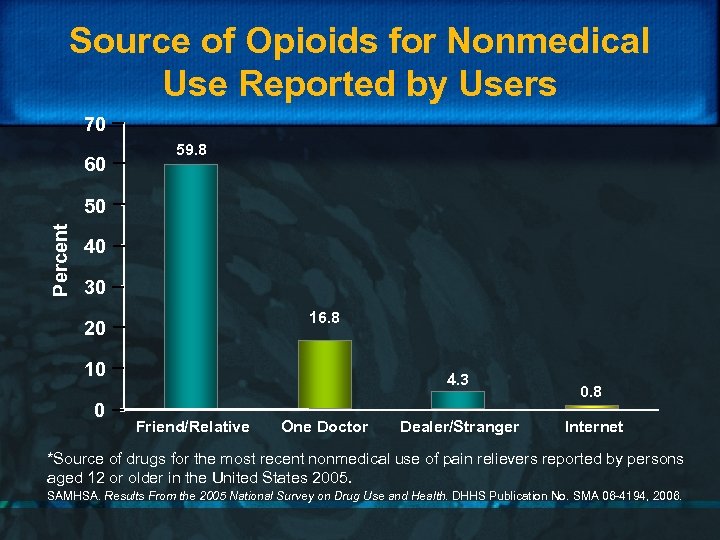 Source of Opioids for Nonmedical Use Reported by Users 70 60 59. 8 Percent 50 40 30 16. 8 20 10 0 4. 3 Friend/Relative One Doctor Dealer/Stranger 0. 8 Internet *Source of drugs for the most recent nonmedical use of pain relievers reported by persons aged 12 or older in the United States 2005. SAMHSA. Results From the 2005 National Survey on Drug Use and Health. DHHS Publication No. SMA 06 -4194, 2006.
Source of Opioids for Nonmedical Use Reported by Users 70 60 59. 8 Percent 50 40 30 16. 8 20 10 0 4. 3 Friend/Relative One Doctor Dealer/Stranger 0. 8 Internet *Source of drugs for the most recent nonmedical use of pain relievers reported by persons aged 12 or older in the United States 2005. SAMHSA. Results From the 2005 National Survey on Drug Use and Health. DHHS Publication No. SMA 06 -4194, 2006.
 Management of Risk Is a “Package Deal” ¨ Best practice requires – Skills to optimize pharmacological outcomes – Skills to minimize risk ¨ Risk is defined – Side effects – Abuse, addiction and diversion – Unintentional overdose
Management of Risk Is a “Package Deal” ¨ Best practice requires – Skills to optimize pharmacological outcomes – Skills to minimize risk ¨ Risk is defined – Side effects – Abuse, addiction and diversion – Unintentional overdose
 Management of Risk Is a “Package Deal” ¨ Understanding laws and regulations ¨ Screening & risk stratification: “Universal Precautions’ ¨ Compliance monitoring commensurate with risk stratum ¨ Dealing with problems over time ¨ Education about drug storage & sharing
Management of Risk Is a “Package Deal” ¨ Understanding laws and regulations ¨ Screening & risk stratification: “Universal Precautions’ ¨ Compliance monitoring commensurate with risk stratum ¨ Dealing with problems over time ¨ Education about drug storage & sharing
 Risk: Laws and Regulation ¨ Federal: Controlled Substances Act – Prescribing is legal if it is consistent with • Usual professional practice • Legitimate medical purpose – Must stop prescribing if diversion occurs ¨ State criminal statutes concerned with diversion: role for prescription monitoring programs ¨ State civil laws/regulations concerned with physician practice
Risk: Laws and Regulation ¨ Federal: Controlled Substances Act – Prescribing is legal if it is consistent with • Usual professional practice • Legitimate medical purpose – Must stop prescribing if diversion occurs ¨ State criminal statutes concerned with diversion: role for prescription monitoring programs ¨ State civil laws/regulations concerned with physician practice
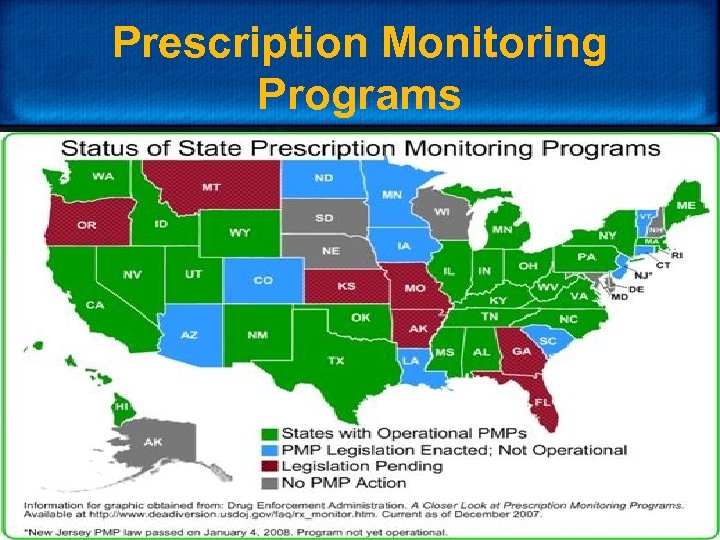 Prescription Monitoring Programs
Prescription Monitoring Programs
 Practical Considerations in Risk Management ¨ Patient selection based on assessment ¨ Distinguishing a trial from long-term therapy ¨ Stratifying risk ¨ Structuring therapy commensurate with risk ¨ Educating ¨ Assessing appropriate outcomes ¨ Adjusting over time ¨ Document and communicate
Practical Considerations in Risk Management ¨ Patient selection based on assessment ¨ Distinguishing a trial from long-term therapy ¨ Stratifying risk ¨ Structuring therapy commensurate with risk ¨ Educating ¨ Assessing appropriate outcomes ¨ Adjusting over time ¨ Document and communicate
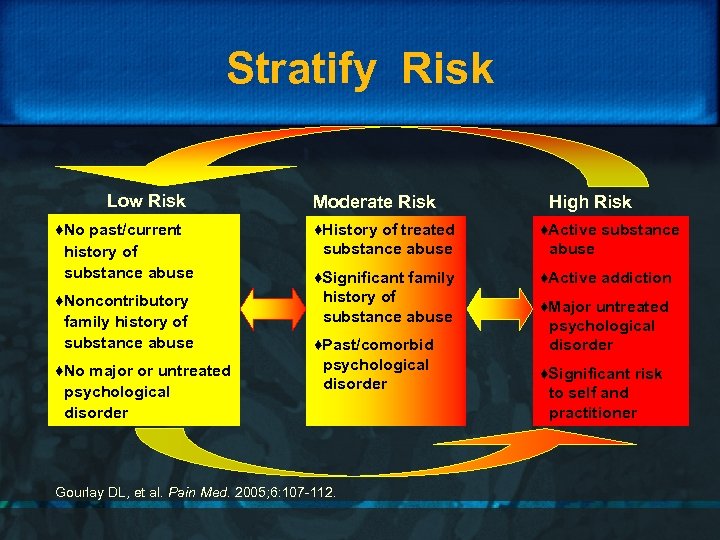 Stratify Risk Low Risk ♦No past/current history of substance abuse ♦Noncontributory family history of substance abuse ♦No major or untreated psychological disorder Moderate Risk High Risk ♦History of treated substance abuse ♦Active substance abuse ♦Significant family history of substance abuse ♦Active addiction ♦Past/comorbid psychological disorder Gourlay DL, et al. Pain Med. 2005; 6: 107 -112. ♦Major untreated psychological disorder ♦Significant risk to self and practitioner
Stratify Risk Low Risk ♦No past/current history of substance abuse ♦Noncontributory family history of substance abuse ♦No major or untreated psychological disorder Moderate Risk High Risk ♦History of treated substance abuse ♦Active substance abuse ♦Significant family history of substance abuse ♦Active addiction ♦Past/comorbid psychological disorder Gourlay DL, et al. Pain Med. 2005; 6: 107 -112. ♦Major untreated psychological disorder ♦Significant risk to self and practitioner
 Measures for Screening ¨ CAGE AID ¨ Opioid Risk Tool ¨ SOAPP ¨ Many others
Measures for Screening ¨ CAGE AID ¨ Opioid Risk Tool ¨ SOAPP ¨ Many others
 Structuring Therapy Based on Risk ¨ May include – – – – Written agreement Frequent visits Prescribing small quantities Long-acting drugs with no rescue doses One pharmacy Pill counts, no replacements or early scripts Urine toxicology screening Coordination with addiction medicine specialist, psychotherapist, others
Structuring Therapy Based on Risk ¨ May include – – – – Written agreement Frequent visits Prescribing small quantities Long-acting drugs with no rescue doses One pharmacy Pill counts, no replacements or early scripts Urine toxicology screening Coordination with addiction medicine specialist, psychotherapist, others
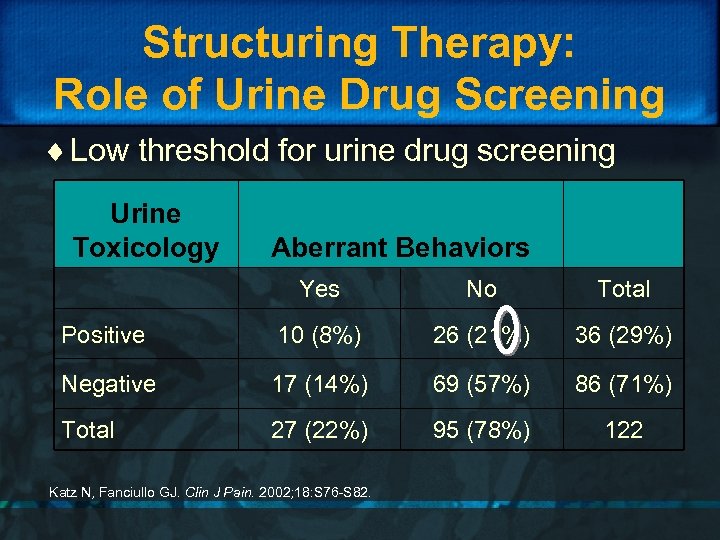 Structuring Therapy: Role of Urine Drug Screening ¨ Low threshold for urine drug screening Urine Toxicology Aberrant Behaviors Yes No Total Positive 10 (8%) 26 (21%) 36 (29%) Negative 17 (14%) 69 (57%) 86 (71%) Total 27 (22%) 95 (78%) 122 Katz N, Fanciullo GJ. Clin J Pain. 2002; 18: S 76 -S 82.
Structuring Therapy: Role of Urine Drug Screening ¨ Low threshold for urine drug screening Urine Toxicology Aberrant Behaviors Yes No Total Positive 10 (8%) 26 (21%) 36 (29%) Negative 17 (14%) 69 (57%) 86 (71%) Total 27 (22%) 95 (78%) 122 Katz N, Fanciullo GJ. Clin J Pain. 2002; 18: S 76 -S 82.
 Opioid Therapy: Monitoring Outcomes ¨ Critical outcomes: The 4 A’s – Analgesia – Adverse effects – Activities – Aberrant drug-related behaviors
Opioid Therapy: Monitoring Outcomes ¨ Critical outcomes: The 4 A’s – Analgesia – Adverse effects – Activities – Aberrant drug-related behaviors
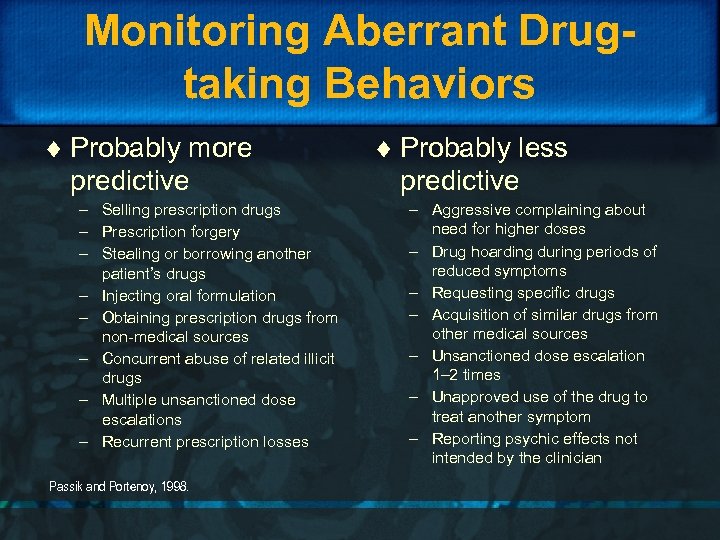 Monitoring Aberrant Drugtaking Behaviors ¨ Probably more predictive – Selling prescription drugs – Prescription forgery – Stealing or borrowing another patient’s drugs – Injecting oral formulation – Obtaining prescription drugs from non-medical sources – Concurrent abuse of related illicit drugs – Multiple unsanctioned dose escalations – Recurrent prescription losses Passik and Portenoy, 1998. ¨ Probably less predictive – Aggressive complaining about need for higher doses – Drug hoarding during periods of reduced symptoms – Requesting specific drugs – Acquisition of similar drugs from other medical sources – Unsanctioned dose escalation 1– 2 times – Unapproved use of the drug to treat another symptom – Reporting psychic effects not intended by the clinician
Monitoring Aberrant Drugtaking Behaviors ¨ Probably more predictive – Selling prescription drugs – Prescription forgery – Stealing or borrowing another patient’s drugs – Injecting oral formulation – Obtaining prescription drugs from non-medical sources – Concurrent abuse of related illicit drugs – Multiple unsanctioned dose escalations – Recurrent prescription losses Passik and Portenoy, 1998. ¨ Probably less predictive – Aggressive complaining about need for higher doses – Drug hoarding during periods of reduced symptoms – Requesting specific drugs – Acquisition of similar drugs from other medical sources – Unsanctioned dose escalation 1– 2 times – Unapproved use of the drug to treat another symptom – Reporting psychic effects not intended by the clinician
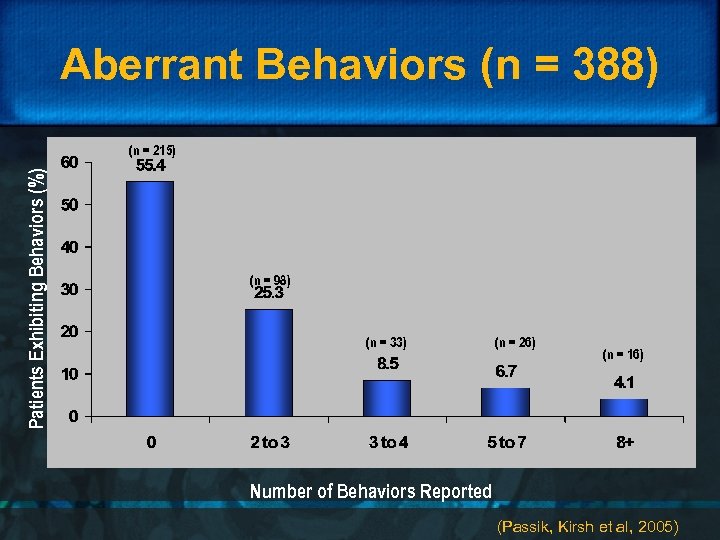 Aberrant Behaviors (n = 388) Patients Exhibiting Behaviors (%) (n = 215) (n = 98) (n = 33) (n = 26) (n = 16) Number of Behaviors Reported (Passik, Kirsh et al, 2005)
Aberrant Behaviors (n = 388) Patients Exhibiting Behaviors (%) (n = 215) (n = 98) (n = 33) (n = 26) (n = 16) Number of Behaviors Reported (Passik, Kirsh et al, 2005)
 Unintentional Overdose ¨ Factors poorly understood ¨ Methadone for pain significantly contributes ¨ Probably multifactorial – Prescribing to patients at risk • Axis I and Axis II: impulsivity and suicidality • Predisposed to opioid-induced sleep-disordered breathing • Predisposed to methadone-induced QTc prolongation – Lacking knowledge of drug-specific risks
Unintentional Overdose ¨ Factors poorly understood ¨ Methadone for pain significantly contributes ¨ Probably multifactorial – Prescribing to patients at risk • Axis I and Axis II: impulsivity and suicidality • Predisposed to opioid-induced sleep-disordered breathing • Predisposed to methadone-induced QTc prolongation – Lacking knowledge of drug-specific risks
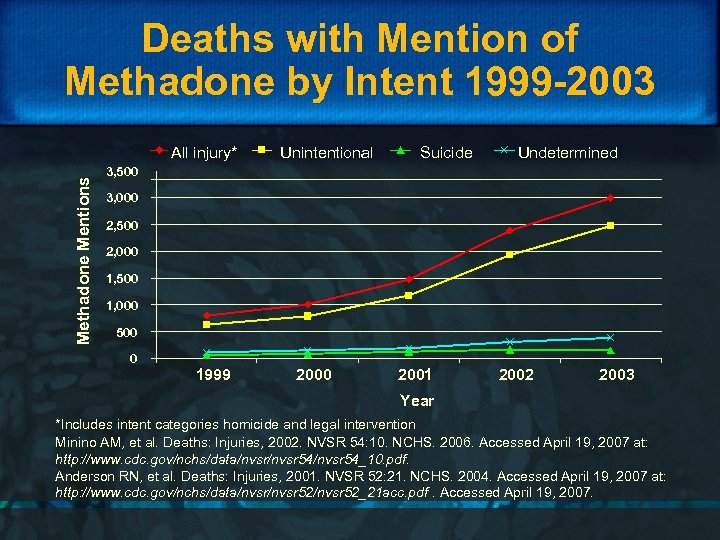 Deaths with Mention of Methadone by Intent 1999 -2003 Methadone Mentions All injury* Unintentional Suicide Undetermined 3, 500 3, 000 2, 500 2, 000 1, 500 1, 000 500 0 1999 2000 2001 2002 2003 Year *Includes intent categories homicide and legal intervention Minino AM, et al. Deaths: Injuries, 2002. NVSR 54: 10. NCHS. 2006. Accessed April 19, 2007 at: http: //www. cdc. gov/nchs/data/nvsr 54/nvsr 54_10. pdf. Anderson RN, et al. Deaths: Injuries, 2001. NVSR 52: 21. NCHS. 2004. Accessed April 19, 2007 at: http: //www. cdc. gov/nchs/data/nvsr 52/nvsr 52_21 acc. pdf. Accessed April 19, 2007.
Deaths with Mention of Methadone by Intent 1999 -2003 Methadone Mentions All injury* Unintentional Suicide Undetermined 3, 500 3, 000 2, 500 2, 000 1, 500 1, 000 500 0 1999 2000 2001 2002 2003 Year *Includes intent categories homicide and legal intervention Minino AM, et al. Deaths: Injuries, 2002. NVSR 54: 10. NCHS. 2006. Accessed April 19, 2007 at: http: //www. cdc. gov/nchs/data/nvsr 54/nvsr 54_10. pdf. Anderson RN, et al. Deaths: Injuries, 2001. NVSR 52: 21. NCHS. 2004. Accessed April 19, 2007 at: http: //www. cdc. gov/nchs/data/nvsr 52/nvsr 52_21 acc. pdf. Accessed April 19, 2007.
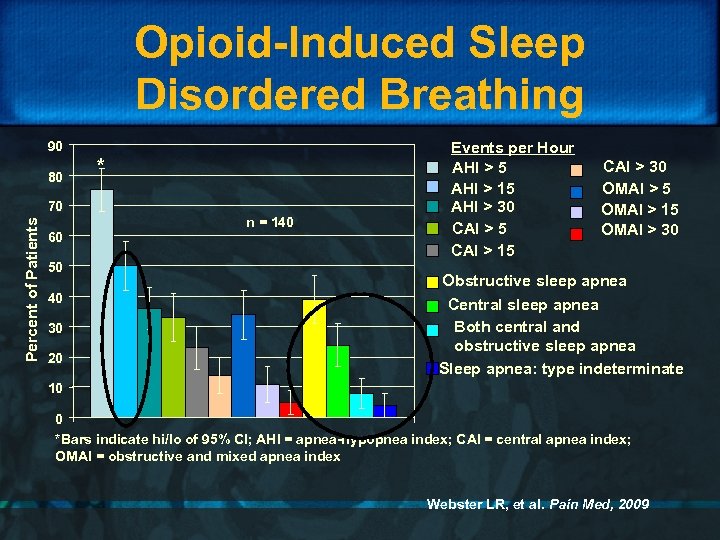 Opioid-Induced Sleep Disordered Breathing 90 80 * Percent of Patients 70 60 50 40 30 20 n = 140 Events per Hour AHI > 5 AHI > 15 AHI > 30 CAI > 5 CAI > 15 CAI > 30 OMAI > 5 OMAI > 15 OMAI > 30 Obstructive sleep apnea Central sleep apnea Both central and obstructive sleep apnea Sleep apnea: type indeterminate 10 0 *Bars indicate hi/lo of 95% CI; AHI = apnea-hypopnea index; CAI = central apnea index; OMAI = obstructive and mixed apnea index Webster LR, et al. Pain Med, 2009
Opioid-Induced Sleep Disordered Breathing 90 80 * Percent of Patients 70 60 50 40 30 20 n = 140 Events per Hour AHI > 5 AHI > 15 AHI > 30 CAI > 5 CAI > 15 CAI > 30 OMAI > 5 OMAI > 15 OMAI > 30 Obstructive sleep apnea Central sleep apnea Both central and obstructive sleep apnea Sleep apnea: type indeterminate 10 0 *Bars indicate hi/lo of 95% CI; AHI = apnea-hypopnea index; CAI = central apnea index; OMAI = obstructive and mixed apnea index Webster LR, et al. Pain Med, 2009
 Formulations and Risk ¨ Risk of abuse may vary with drug and formulation – Higher concern: Short-acting drugs, including the rapid onset fentanyl drugs for breakthrough pain – Higher concern: Higher street value drugs, e. g. oxycodone, hydromorphone – Lower concern: Transdermal fentanyl and methadone
Formulations and Risk ¨ Risk of abuse may vary with drug and formulation – Higher concern: Short-acting drugs, including the rapid onset fentanyl drugs for breakthrough pain – Higher concern: Higher street value drugs, e. g. oxycodone, hydromorphone – Lower concern: Transdermal fentanyl and methadone
 Formulations and Risk ¨ Emergence of abuse deterrent formulations – May reduce unintentional overdose during recreational or impulsive use – May reduce diversion if less attractive to those with addiction – Benefits not yet demonstrated and will be difficult to track
Formulations and Risk ¨ Emergence of abuse deterrent formulations – May reduce unintentional overdose during recreational or impulsive use – May reduce diversion if less attractive to those with addiction – Benefits not yet demonstrated and will be difficult to track
 Formulations and Risk ¨ Mechanical abuse deterrent formulations – Oxycontin ™ and Remoxy™ • Deters dose dumping: as gelatin capsule dissolves, SR oxycodone released via GI tract • Difficult to crush, break, dissolve • Cannot inject or snort
Formulations and Risk ¨ Mechanical abuse deterrent formulations – Oxycontin ™ and Remoxy™ • Deters dose dumping: as gelatin capsule dissolves, SR oxycodone released via GI tract • Difficult to crush, break, dissolve • Cannot inject or snort
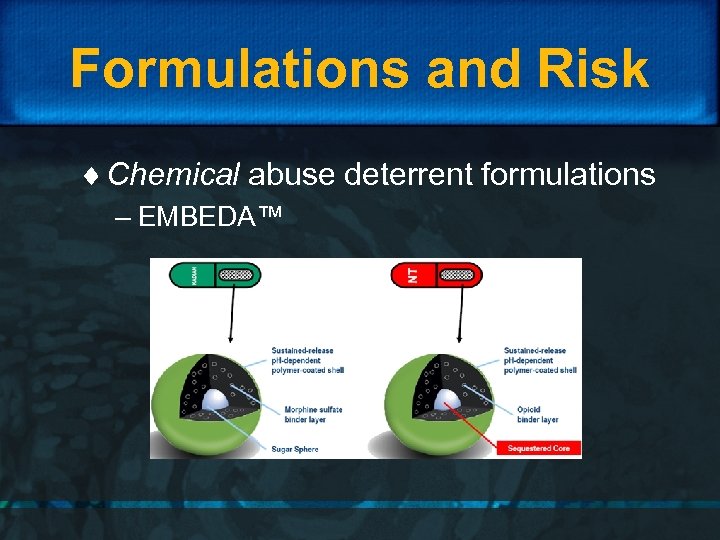 Formulations and Risk ¨ Chemical abuse deterrent formulations – EMBEDA™
Formulations and Risk ¨ Chemical abuse deterrent formulations – EMBEDA™
 Conclusion ¨ Despite lack of consensus, there is growing use of opioid therapy for chronic pain – Some is good – Some does harm ¨ Reducing harm requires education and balanced policies based on best practice approaches
Conclusion ¨ Despite lack of consensus, there is growing use of opioid therapy for chronic pain – Some is good – Some does harm ¨ Reducing harm requires education and balanced policies based on best practice approaches


