34a2a23e39c6bcd9a5639810d90a472e.ppt
- Количество слайдов: 63
Oxygenation of the Neonate
Abbreviations O 2 - oxygen n Fi. O 2 - inspired O 2 concentration n PO 2 - partial pressure of O 2 n Pa. O 2 - arterial O 2 tension n Sa. O 2 - arterial oxygen saturation n
What is oxygen?
Most widely occurring element on Earth n Considered by some to be a air pollutant n Catalyst for free radical formation n – contains one or more unpaired electrons – superoxide theory of oxygen toxicity (oxidative stress) is due to excess formation of superoxide radical (reduction product of O 2) n effects are countered by superoxide dismutase (antioxidant enzymes) n
n Oxidative Stress – occurs when generation of reactive oxygen species exceed the ability of the cell to remove them produces physiologic, inflammatory and histologic changes n produces injury in proteins (amino acids, DNA), membrane lipids, carbohydrates n
n Protective Forces – Compartmentalize processes which create free radicals – Superoxide dismutase and other enzymes – Vitamin E- most abundant antioxidant – Vitamin C – Bilirubin and other antioxidants
Why is oxygen important?
Mitochondria (power house of the cell) is oxygen dependent n Oxygen is necessary for aerobic metabolism (breakdown of glucose) n – ATP – limited storage capacity
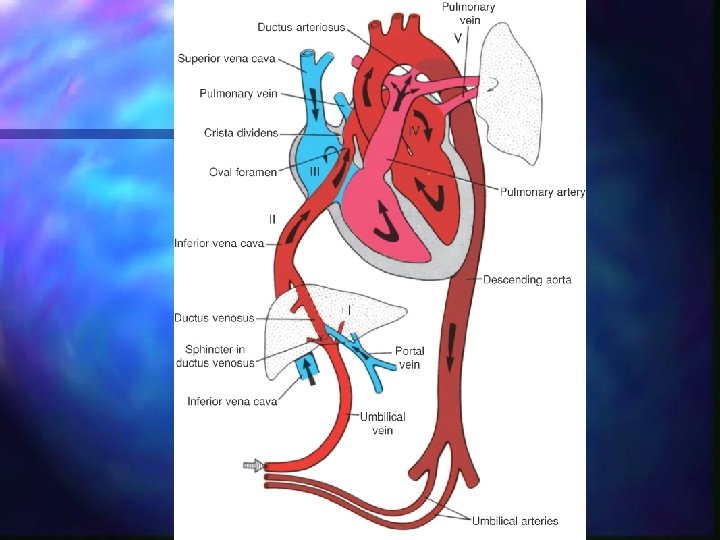
Fetal Oxygenation Umbilical venous blood from placenta to fetus has a Pa. O 2 20 -30 mm Hg. n Fetus able to survive secondary to low metabolic demands (placenta/mother provide support) n In fetus low Pa. O 2 causes pulmonary vasoconstriction and ductus arteriosus vasodilation n
Introduction of oxygen to body Regulated by the oxygen pressure gradient n Convection of air into the lungs n Diffusion of oxygen into the blood n Convection flow of blood to the tissue n Diffusion of oxygen into the cells n Diffusion of oxygen into the mitochondria n
n Oxygen transport is dependent on – availability of oxygen – oxygen carrying capacity of blood – rate of blood flow
n Factors affecting oxygen carrying capacity and delivery to tissue – respiratory status – hemoglobin level and configuration – cardiac output blood pressure n heart rate n – tissue ischemia/edema – disease state
n Oxygen in the blood is found – dissolved in plasma small quantity n linear relationship to PO 2 n ~ 10% Fi. O 2 equals 1% of blood’s O 2 content n – bound to hemoglobin larger quantity n fully saturated- one gram hemoglobin will bind 1. 34 ml of oxygen n nonlinear relationship to PO 2 n – oxygen dissociation curve
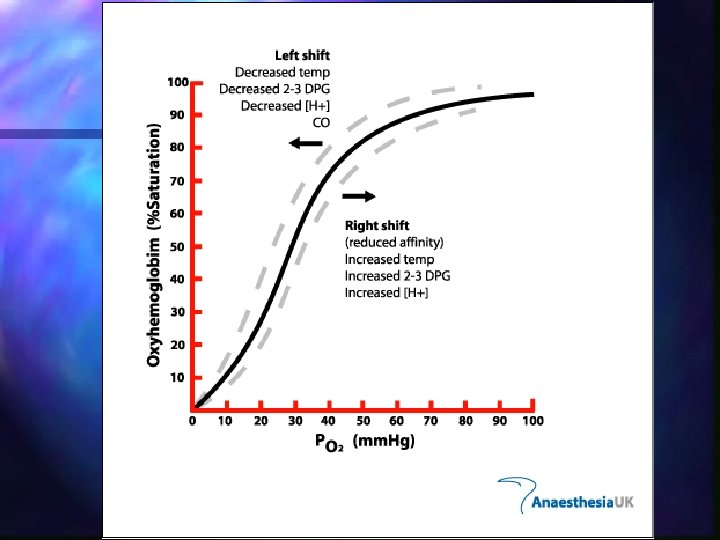
Oxygen Dissociation Curve At low PO 2 levels, O 2 binds quickly to hemoglobin n Between 40 -80 mm Hg, binding slows n Above 100 mm Hg, binding is relatively static (hemoglobin is saturated) n Levels above 50 -80 mm Hg have the potential to cause harm n
Shifting of Curve n To the left (increased affinity of hemoglobin to O 2) – hemoglobin saturation can be achieved at lower PO 2 levels n n greater percentage of fetal hemoglobin decrease in 2, 3 -diphosphoglycerate content – occurs in premature infants with RDS n n n alkalemia hypocapnia hypothermia
n To the right (decreased affinity of hemoglobin to O 2) – hemoglobin saturation is achieved at higher PO 2 levels reduction in fetal hemoglobin n increased 2, 3 -DPG n acidemia n hypercapnia n hyperthermia n
Hemoglobin is ~ 1/3 of hematocrit n Hemoglobin levels are important n – Hgb 15 X 1. 34 ml = 20. 1 ml O 2 (if 100% saturated) – Hgb 10 x 1. 34 ml = 13. 4 ml O 2 (if 100% saturated) – Hgb 7 x 1. 34 ml = 9. 38 ml O 2 (if 100% saturated)
Adequate Oxygenation n PO 2 necessary to deliver an amount of oxygen to the tissues for effective metabolism without creating a toxic effect – Variable among individuals – Continuous fluctuations
What is 21% Fi. O 2? Total pressure in the atmosphere at sea level is 760 mm Hg n Water vapor 47 mm Hg n 21% of remaining pressure (760 - 47) is exerted by oxygen- 150 mm Hg (which means Pa. O 2 of room air is 150 mm Hg) n Nitrogen makes up the majority of the remaining air n Carbon dioxide is miniscule (0. 001 %)
First breaths n n Arterial-alveolar oxygen tension ratio Normal term infant – – – Initial PCO 2 60 -80 mm Hg Inhales room air (150 mm Hg) Mixing causes dilution of oxygen diffusing into blood – At ~ 20 minutes of age PCO 2 30 -40 mm Hg – Ultimately PO 2 diffusing into blood is ~80 -100 mm Hg
Lung Development Individual variations n Stages overlap n
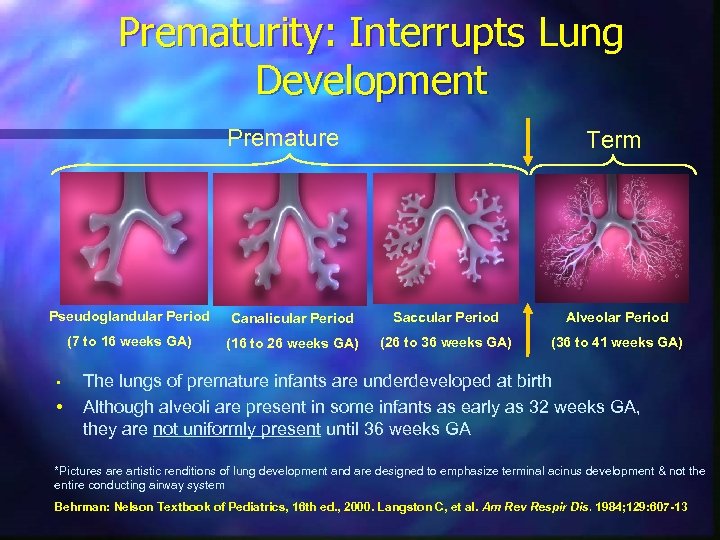
Prematurity: Interrupts Lung Development Premature Term Pseudoglandular Period Canalicular Period Saccular Period Alveolar Period (7 to 16 weeks GA) (16 to 26 weeks GA) (26 to 36 weeks GA) (36 to 41 weeks GA) • • The lungs of premature infants are underdeveloped at birth Although alveoli are present in some infants as early as 32 weeks GA, they are not uniformly present until 36 weeks GA *Pictures are artistic renditions of lung development and are designed to emphasize terminal acinus development & not the entire conducting airway system Behrman: Nelson Textbook of Pediatrics, 16 th ed. , 2000. Langston C, et al. Am Rev Respir Dis. 1984; 129: 607 -13
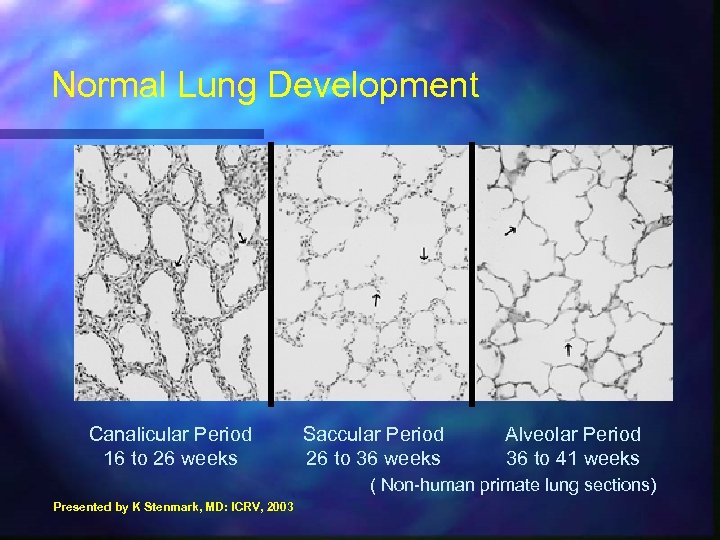
Normal Lung Development Canalicular Period 16 to 26 weeks Saccular Period 26 to 36 weeks Alveolar Period 36 to 41 weeks ( Non-human primate lung sections) Presented by K Stenmark, MD: ICRV, 2003
n Embryonic (0 -7 weeks) – lung buds form, blood vessels connect to heart n Pseudoglandular (6 -17 weeks) – pre-acinar airways and blood vessels develop
n Canalicular (16 -27 weeks) – respiratory regions develop – peripheral epithelium and mesenchyme thin – type I and II pneumonocytes develop
n Alveolar (27 weeks to term) – saccules develop and produce alveoli n Post natal – alveoli and small blood vessels multiple
Complications of hyperoxia
Individual variations n Must keep in mind that all disease states are multifactorial n Controlling oxygen exposure is critical but other complicating factors must also be addressed n
Retinopathy of Prematurity Proliferative vascular disease
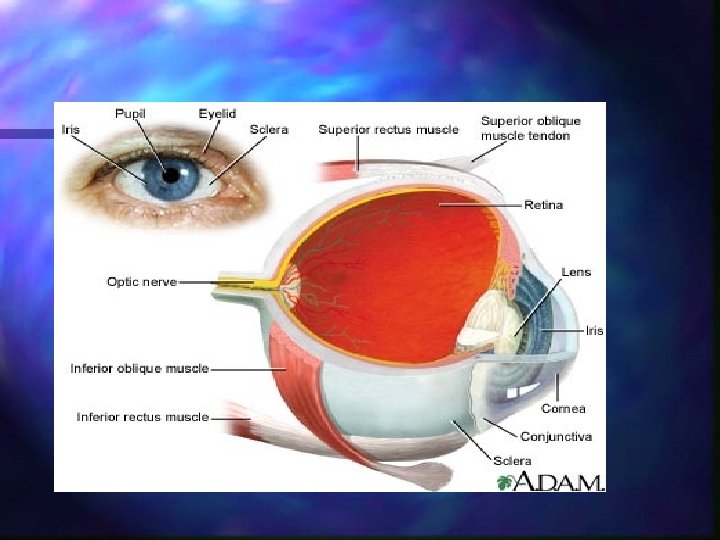
n n Vitreous gel – clear gel that fills the inside of the eye Optic nerve – bundle of more than 1, 000 nerve fibers that carry visual messages from the retina to the brain Macula – small sensitive area of the retina that gives central vision Fovea – center of macula, gives sharpest vision
n n n Retina – light sensitive tissue lining the back of the eye, converts light into electrical impulses that are sent to the brain via the optic nerve Iris – colored part of eye, regulates amount of light entering the eye Cornea – clear outer part of eye’s focusing system
n n n Pupil – opening at center of the iris, adjusts the size of the pupil to control amount of light entering the eye Lens – clear part of eye behind iris that helps focus light on retina Iris – colored part of eye, regulates the amount of light entering the eye
Normal Eye Development n n n Eye starts development at ~ 16 weeks – blood vessels of retina begin to form at the optic nerve – grow towards the edge of the retina, supplying oxygen and nutrients Last trimester – eye develops rapidly Term – eye growth is almost complete (vessels have reached the edge of the retina)
Risk factors for ROP Prematurity n Low birth weight n Complicated hospital course n Co-morbidities n Oxygen exposure (toxicity) n
Preterm Eye Development n Preterm eye – blood vessels have not reached edges of the retina – vessel growth may be arrested – vessel growth is resumed and continues to periphery unless abnormalities occur
ROP n Pathogenesis – any factor causing vasoconstriction of immature retinal vessels – interruption of migration of blood vessels from the optic nerve to the ora serrata retina sends out signals to induce renewal of growth n abnormal vessels may develop (fragile, weak) n leads to scarring which can lead to pulling on retina n
n Stage I – mild abnormal blood vessel growth (demarcation line) n Stage II – moderately abnormal blood vessels growth (ridge)
n Stage III – severely abnormal blood vessel growth (extraretinal fibrovascular proliferation) – blood vessel growth is towards the center of the eye instead of along surface of retina n Plus Disease – blood vessels of the retina are enlarging and twisting “tortuosity”
n Stage IV – partially detached retina – caused by traction from scarring and abnormal vessel growth n Stage V – complete retina detachment – end stage of disease
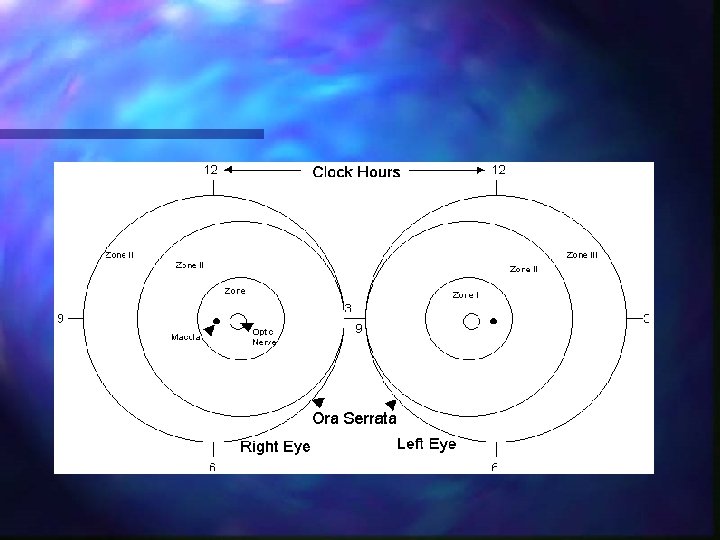
n Zone I – most posterior, near optic nerve n Zone II – extends to ora serrata n Zone III – extends to periphery
n Oxygen’s implication – retinal vessels form in an environment of low Pa. O 2 (20 -30 mm Hg) – at birth, dramatic increase in Pa. O 2 (even RA creates significant increase) – retinal vessels constrict in response to increased Pa. O 2, diminishing flow and nutrients – down regulation of vascular endothelial growth factor (secondary to hyperoxia)
– as metabolic demands of growing eye increase, nonvascularized areas of the eye become hypoxic – eye sends signals for help – neovascularization and increased levels of VEGF occurs – cycles of hyperoxia and hypoxia
n Treatment – prevention – surgical intervention laser or cryotherapy- burns away periphery of retina where abnormal vessels abound (loss peripheral vision) (stage III with plus dz) n scleral buckle- banding the eye to prevent vitreous gel from pulling on scar tissue, releases pressure from retina (stage IV, V) n vitrectomy- replacing vitreous gel with saline in order to remove scar tissue (stage V) n
Oxygen toxicity in the Lung
Incomplete development and inadequate responsiveness of pulmonary antioxidant enzyme system n Cessation of transplacental substrates n Lungs are susceptible due to large surface area of type I and II cells coming into direct contact with Fi. O 2 n
Increased production of cytotoxic oxygen free radicals n Overwhelms the antioxidant defenses in the capillary endothelial and alveolar cells n Radicals react with intracellular constituents producing chain reaction n
Pulmonary Changes Atelectasis n Edema n Alveolar hemorrhage n Inflammation n Fibrin deposition n Thickening and hyalinization of alveolar membranes n
Plasma leakage through endothelium n Inactivation of surfactant n Damage to mucocilary function n Lung growth arrest and decreased branching morphogenesis n n AKA- Bronchopulmonary Dysplasia
Hypoxic effect n Inadequate oxygenation forces a change from aerobic to anaerobic metabolism – decreases cellular energy aerobic metabolism- net production of 36 ATP n anaerobic metabolism- net production of 2 ATP n – toxic by-products (lactic acid) – leading to cellular damage and death

Middle Ground
Goals Minimize hypoxic/hyperoxic swings n Reduce titration of Fi. O 2 n Avoid high saturations n
Obtaining Blood Gases n May alter results by aspirating room air into blood gas syringe/tube – Remember room air PO 2 is ~ 150 mm Hg, PCO 2 is <2 mm Hg – If aspirated into sample may give false values increase the Pa. O 2 reading n decrease the Pa. CO 2 reading n
Pulse Oximetry n Pulse oximetry- determines the amount of saturated hemoglobin by the absorption of light – setting the limits – interference n n movement, poor perfusion, loose probe Pulse ox becomes unreliable predictor of Pa. O 2 as Hgb becomes > 90% saturated
Oxygen Management n Know your target audience – older infants have different biological needs – some disease states require increased Pa. O 2 for appropriate management n Don’t start at 100% – select situations may call for increasing to 100% – don’t use 100% O 2 breaths
n Watchful waiting – especially if normal heart rate Don’t increase Fi. O 2 by more than 5% at a time n Wean Fi. O 2 as soon as recovery process stabilized (don’t wait for high saturations) n Keep ambu bag Fi. O 2 at appropriate level n
Monitoring n Attend to cause of desaturations – – – – – Is it real? know where the ETT is (especially on x-ray) bronchospasm activity gastroesphogeal reflux hypotension apnea blocked airway vagal stimulation
n Take responsibility for the role we play in the long term outcome of these infants
References n n n Chow, L. , Wright, K. , & Sola, A. (2003) Can Changes in Clinical Practice Decrease the Incidence of Severe Retinopathy of Prematurity in Very Low Birth Weight Infants? Fanaroff, A. & Martin, R. (2002) Neonatal. Perinatal Medicine, Diseases of the Fetus and Infant, 7 th ed. Goldsmith, J. & Karotkin, E. (2003) Assisted Ventilation of the Neonate, 4 th ed.
Greenough, A. & Milner, A. (2003) Neonatal Respiratory Disorders, 2 nd ed. n Halliwell, B. & Cross, C. (1994) Oxygenderived Species: Their Relation to Human Disease and Environmental Stress. n http: //www. nei. nih. gov/health/rop n
34a2a23e39c6bcd9a5639810d90a472e.ppt