5e0e6bb48731e9d7cbe6612a92574002.ppt
- Количество слайдов: 22
 Overview of Changes to the NAEP Asthma Guidelines Breathe California’s Clinical Asthma Collaborative Susan M. Pollart, MD, MS University of Virginia Family Medicine June 24, 2009
Overview of Changes to the NAEP Asthma Guidelines Breathe California’s Clinical Asthma Collaborative Susan M. Pollart, MD, MS University of Virginia Family Medicine June 24, 2009
 Overview § Asthma classification by Severity and Control § Level of Severity and of Control relate to current impairment and future risk. § ICS Mainstay of treatment § Low dose ICS plus LABA equal to Medium dose LABA in adults and children >5 § Written action plans important.
Overview § Asthma classification by Severity and Control § Level of Severity and of Control relate to current impairment and future risk. § ICS Mainstay of treatment § Low dose ICS plus LABA equal to Medium dose LABA in adults and children >5 § Written action plans important.
 New Classification § “Classification” is based on SEVERITY at time of DIAGNOSIS. § Patient is not taking long-term controller medication § Based on two parameters – impairment and risk § Can also be determined once asthma control is achieved.
New Classification § “Classification” is based on SEVERITY at time of DIAGNOSIS. § Patient is not taking long-term controller medication § Based on two parameters – impairment and risk § Can also be determined once asthma control is achieved.
 Assess Control to Adjust Therapy § Once therapy is initiated, the emphasis is on control. § Control determined by two parameters – impairment and risk. § Level of control guides decisions about adjusting therapy. § Step-up and Step-down still apply
Assess Control to Adjust Therapy § Once therapy is initiated, the emphasis is on control. § Control determined by two parameters – impairment and risk. § Level of control guides decisions about adjusting therapy. § Step-up and Step-down still apply
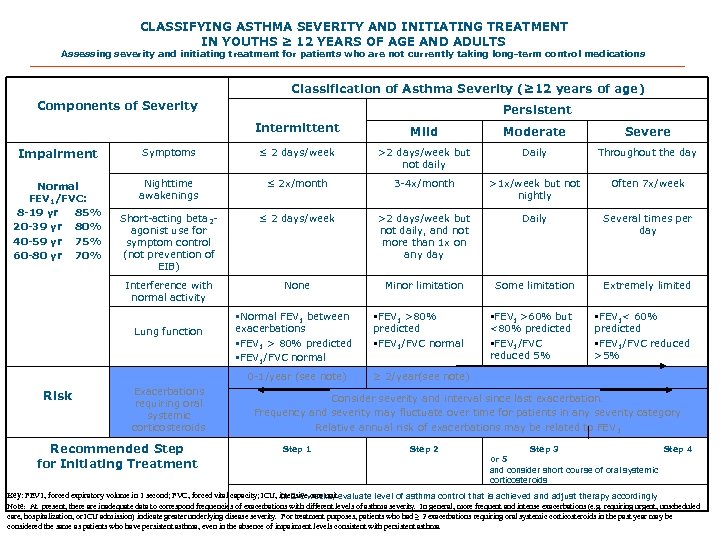 CLASSIFYING ASTHMA SEVERITY AND INITIATING TREATMENT IN YOUTHS ≥ 12 YEARS OF AGE AND ADULTS Assessing severity and initiating treatment for patients who are not currently taking long-term control medications Classification of Asthma Severity (≥ 12 years of age) Components of Severity Persistent Intermittent Mild Moderate Severe Impairment Symptoms ≤ 2 days/week >2 days/week but not daily Daily Throughout the day Normal FEV 1/FVC: 8 -19 yr 85% 20 -39 yr 80% 40 -59 yr 75% 60 -80 yr 70% Nighttime awakenings ≤ 2 x/month 3 -4 x/month >1 x/week but not nightly Often 7 x/week Short-acting beta 2 agonist use for symptom control (not prevention of EIB) ≤ 2 days/week >2 days/week but not daily, and not more than 1 x on any day Daily Several times per day Interference with normal activity None Minor limitation Some limitation Extremely limited §FEV 1 >80% predicted §FEV 1/FVC normal §FEV 1 >60% but <80% predicted §FEV 1/FVC reduced 5% §FEV 1< 60% predicted §FEV 1/FVC reduced >5% Lung function §Normal FEV 1 between exacerbations §FEV 1 > 80% predicted §FEV 1/FVC normal 0 -1/year (see note) Risk Exacerbations requiring oral systemic corticosteroids Recommended Step for Initiating Treatment ≥ 2/year(see note) Consider severity and interval since last exacerbation. Frequency and severity may fluctuate over time for patients in any severity category Relative annual risk of exacerbations may be related to FEV 1 Step 2 Step 3 Step 4 or 5 and consider short course of oral systemic corticosteroids Key: FEV 1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICU, intensiveweeks, evaluate level of asthma control that is achieved and adjust therapy accordingly In 2 -6 care unit Note: At present, there are inadequate data to correspond frequencies of exacerbations with different levels of asthma severity. In general, more frequent and intense exacerbations (e. g. requiring urgent, unscheduled care, hospitalization, or ICU admission) indicate greater underlying disease severity. For treatment purposes, patients who had ≥ 2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
CLASSIFYING ASTHMA SEVERITY AND INITIATING TREATMENT IN YOUTHS ≥ 12 YEARS OF AGE AND ADULTS Assessing severity and initiating treatment for patients who are not currently taking long-term control medications Classification of Asthma Severity (≥ 12 years of age) Components of Severity Persistent Intermittent Mild Moderate Severe Impairment Symptoms ≤ 2 days/week >2 days/week but not daily Daily Throughout the day Normal FEV 1/FVC: 8 -19 yr 85% 20 -39 yr 80% 40 -59 yr 75% 60 -80 yr 70% Nighttime awakenings ≤ 2 x/month 3 -4 x/month >1 x/week but not nightly Often 7 x/week Short-acting beta 2 agonist use for symptom control (not prevention of EIB) ≤ 2 days/week >2 days/week but not daily, and not more than 1 x on any day Daily Several times per day Interference with normal activity None Minor limitation Some limitation Extremely limited §FEV 1 >80% predicted §FEV 1/FVC normal §FEV 1 >60% but <80% predicted §FEV 1/FVC reduced 5% §FEV 1< 60% predicted §FEV 1/FVC reduced >5% Lung function §Normal FEV 1 between exacerbations §FEV 1 > 80% predicted §FEV 1/FVC normal 0 -1/year (see note) Risk Exacerbations requiring oral systemic corticosteroids Recommended Step for Initiating Treatment ≥ 2/year(see note) Consider severity and interval since last exacerbation. Frequency and severity may fluctuate over time for patients in any severity category Relative annual risk of exacerbations may be related to FEV 1 Step 2 Step 3 Step 4 or 5 and consider short course of oral systemic corticosteroids Key: FEV 1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICU, intensiveweeks, evaluate level of asthma control that is achieved and adjust therapy accordingly In 2 -6 care unit Note: At present, there are inadequate data to correspond frequencies of exacerbations with different levels of asthma severity. In general, more frequent and intense exacerbations (e. g. requiring urgent, unscheduled care, hospitalization, or ICU admission) indicate greater underlying disease severity. For treatment purposes, patients who had ≥ 2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
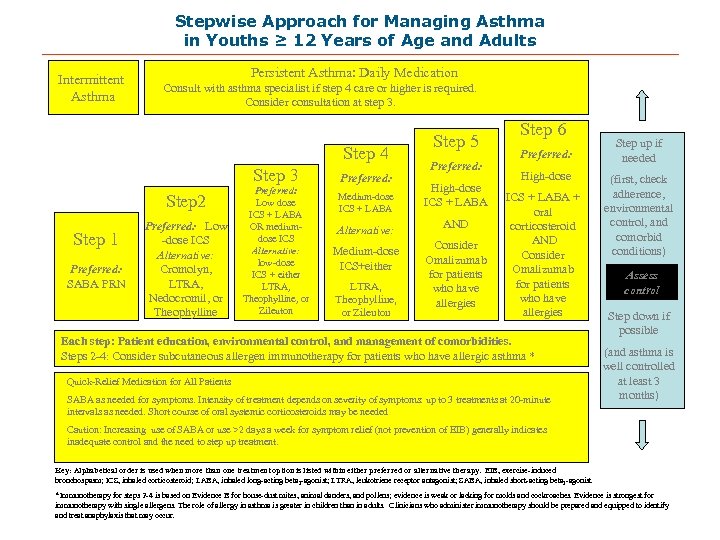 Stepwise Approach for Managing Asthma in Youths ≥ 12 Years of Age and Adults Intermittent Asthma Persistent Asthma: Daily Medication Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3. Step 4 Step 3 Step 2 Step 1 Preferred: SABA PRN Preferred: Low -dose ICS Alternative: Cromolyn, LTRA, Nedocromil, or Theophylline Preferred: Low dose ICS + LABA OR mediumdose ICS Alternative: low-dose ICS + either LTRA, Theophylline, or Zileuton Preferred: Medium-dose ICS + LABA Step 5 Preferred: High-dose ICS + LABA Alternative: AND Medium-dose ICS+either Consider Omalizumab for patients who have allergies LTRA, Theophylline, or Zileuton Step 6 Preferred: High-dose ICS + LABA + oral corticosteroid AND Consider Omalizumab for patients who have allergies Each step: Patient education, environmental control, and management of comorbidities. Steps 2 -4: Consider subcutaneous allergen immunotherapy for patients who have allergic asthma * Quick-Relief Medication for All Patients SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20 -minute intervals as needed. Short course of oral systemic corticosteroids may be needed Step up if needed (first, check adherence, environmental control, and comorbid conditions) Assess control Step down if possible (and asthma is well controlled at least 3 months) Caution: Increasing use of SABA or use >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate control and the need to step up treatment. Key: Alphabetical order is used when more than one treatment option is listed within either preferred or alternative therapy. EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, inhaled long-acting beta 2 -agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled short-acting beta 2 -agonist *Immunotherapy for steps 2 -4 is based on Evidence B for house-dust mites, animal danders, and pollens; evidence is weak or lacking for molds and cockroaches. Evidence is strongest for immunotherapy with single allergens. The role of allergy in asthma is greater in children than in adults. Clinicians who administer immunotherapy should be prepared and equipped to identify and treat anaphylaxis that may occur.
Stepwise Approach for Managing Asthma in Youths ≥ 12 Years of Age and Adults Intermittent Asthma Persistent Asthma: Daily Medication Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3. Step 4 Step 3 Step 2 Step 1 Preferred: SABA PRN Preferred: Low -dose ICS Alternative: Cromolyn, LTRA, Nedocromil, or Theophylline Preferred: Low dose ICS + LABA OR mediumdose ICS Alternative: low-dose ICS + either LTRA, Theophylline, or Zileuton Preferred: Medium-dose ICS + LABA Step 5 Preferred: High-dose ICS + LABA Alternative: AND Medium-dose ICS+either Consider Omalizumab for patients who have allergies LTRA, Theophylline, or Zileuton Step 6 Preferred: High-dose ICS + LABA + oral corticosteroid AND Consider Omalizumab for patients who have allergies Each step: Patient education, environmental control, and management of comorbidities. Steps 2 -4: Consider subcutaneous allergen immunotherapy for patients who have allergic asthma * Quick-Relief Medication for All Patients SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20 -minute intervals as needed. Short course of oral systemic corticosteroids may be needed Step up if needed (first, check adherence, environmental control, and comorbid conditions) Assess control Step down if possible (and asthma is well controlled at least 3 months) Caution: Increasing use of SABA or use >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate control and the need to step up treatment. Key: Alphabetical order is used when more than one treatment option is listed within either preferred or alternative therapy. EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, inhaled long-acting beta 2 -agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled short-acting beta 2 -agonist *Immunotherapy for steps 2 -4 is based on Evidence B for house-dust mites, animal danders, and pollens; evidence is weak or lacking for molds and cockroaches. Evidence is strongest for immunotherapy with single allergens. The role of allergy in asthma is greater in children than in adults. Clinicians who administer immunotherapy should be prepared and equipped to identify and treat anaphylaxis that may occur.
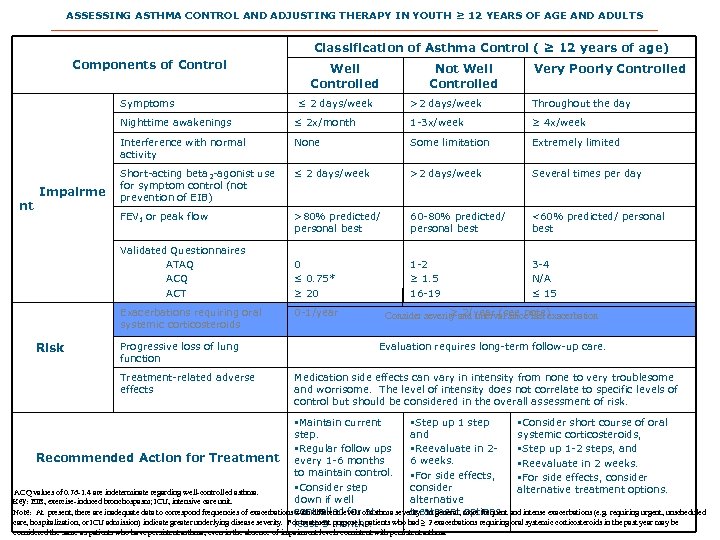 ASSESSING ASTHMA CONTROL AND ADJUSTING THERAPY IN YOUTH ≥ 12 YEARS OF AGE AND ADULTS Classification of Asthma Control ( ≥ 12 years of age) Components of Control Symptoms Well Controlled ≤ 2 days/week Not Well Controlled Very Poorly Controlled >2 days/week Throughout the day Nighttime awakenings nt 1 -3 x/week ≥ 4 x/week Interference with normal activity None Some limitation Extremely limited Short-acting beta 2 -agonist use for symptom control (not prevention of EIB) ≤ 2 days/week >2 days/week Several times per day FEV 1 or peak flow Impairme ≤ 2 x/month >80% predicted/ personal best 60 -80% predicted/ personal best <60% predicted/ personal best 0 ≤ 0. 75* ≥ 20 1 -2 ≥ 1. 5 16 -19 3 -4 N/A ≤ 15 Validated Questionnaires ATAQ ACT Exacerbations requiring oral systemic corticosteroids Risk Progressive loss of lung function Treatment-related adverse effects 0 -1/year ≥ 2/year (see note) Consider severity and interval since last exacerbation Evaluation requires long-term follow-up care. Medication side effects can vary in intensity from none to very troublesome and worrisome. The level of intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk. §Maintain current §Step up 1 step §Consider short course of oral step. and systemic corticosteroids, §Regular follow ups §Reevaluate in 2§Step up 1 -2 steps, and Recommended Action for Treatment every 1 -6 months 6 weeks. §Reevaluate in 2 weeks. to maintain control. §For side effects, consider §Consider step consider alternative treatment options. *ACQ values of 0. 76 -1. 4 are indeterminate regarding well-controlled asthma. down if well alternative Key: EIB, exercise-induced bronchospasm; ICU, intensive care unit. treatment options. Note: At present, there are inadequate data to correspond frequencies of exacerbations controlled for of asthma severity. In general, more frequent and intense exacerbations (e. g. requiring urgent, unscheduled with different levels at care, hospitalization, or ICU admission) indicate greater underlying disease severity. For treatment months. least 3 purposes, patients who had ≥ 2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
ASSESSING ASTHMA CONTROL AND ADJUSTING THERAPY IN YOUTH ≥ 12 YEARS OF AGE AND ADULTS Classification of Asthma Control ( ≥ 12 years of age) Components of Control Symptoms Well Controlled ≤ 2 days/week Not Well Controlled Very Poorly Controlled >2 days/week Throughout the day Nighttime awakenings nt 1 -3 x/week ≥ 4 x/week Interference with normal activity None Some limitation Extremely limited Short-acting beta 2 -agonist use for symptom control (not prevention of EIB) ≤ 2 days/week >2 days/week Several times per day FEV 1 or peak flow Impairme ≤ 2 x/month >80% predicted/ personal best 60 -80% predicted/ personal best <60% predicted/ personal best 0 ≤ 0. 75* ≥ 20 1 -2 ≥ 1. 5 16 -19 3 -4 N/A ≤ 15 Validated Questionnaires ATAQ ACT Exacerbations requiring oral systemic corticosteroids Risk Progressive loss of lung function Treatment-related adverse effects 0 -1/year ≥ 2/year (see note) Consider severity and interval since last exacerbation Evaluation requires long-term follow-up care. Medication side effects can vary in intensity from none to very troublesome and worrisome. The level of intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk. §Maintain current §Step up 1 step §Consider short course of oral step. and systemic corticosteroids, §Regular follow ups §Reevaluate in 2§Step up 1 -2 steps, and Recommended Action for Treatment every 1 -6 months 6 weeks. §Reevaluate in 2 weeks. to maintain control. §For side effects, consider §Consider step consider alternative treatment options. *ACQ values of 0. 76 -1. 4 are indeterminate regarding well-controlled asthma. down if well alternative Key: EIB, exercise-induced bronchospasm; ICU, intensive care unit. treatment options. Note: At present, there are inadequate data to correspond frequencies of exacerbations controlled for of asthma severity. In general, more frequent and intense exacerbations (e. g. requiring urgent, unscheduled with different levels at care, hospitalization, or ICU admission) indicate greater underlying disease severity. For treatment months. least 3 purposes, patients who had ≥ 2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
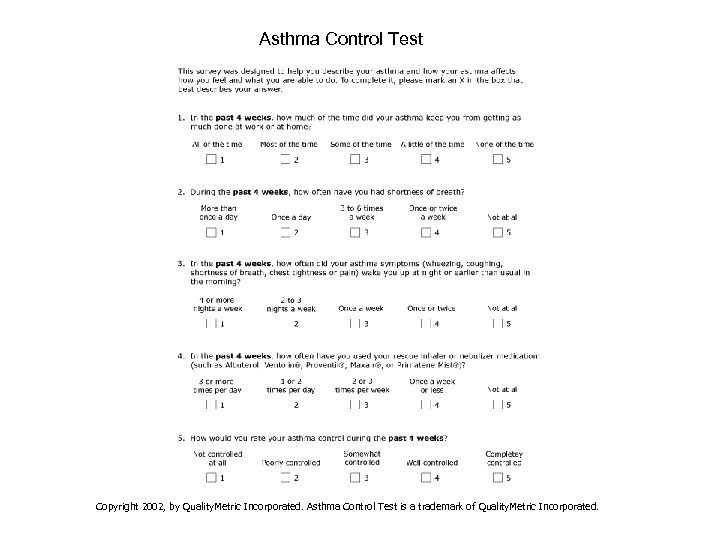 Asthma Control Test Copyright 2002, by Quality. Metric Incorporated. Asthma Control Test is a trademark of Quality. Metric Incorporated.
Asthma Control Test Copyright 2002, by Quality. Metric Incorporated. Asthma Control Test is a trademark of Quality. Metric Incorporated.
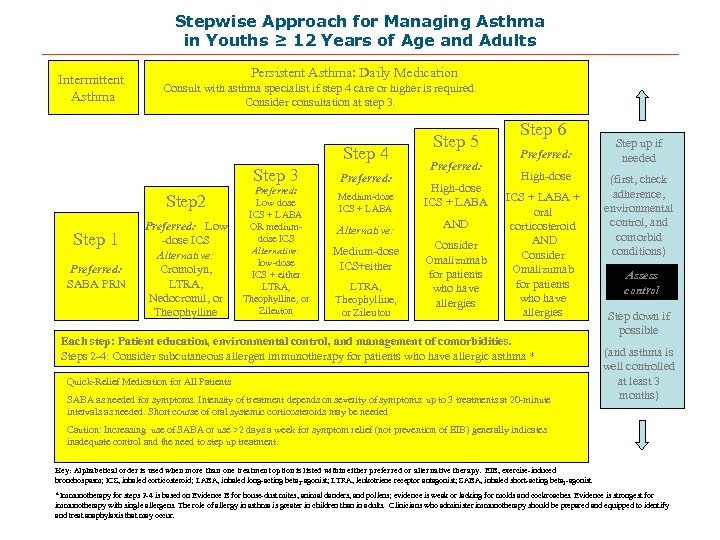 Stepwise Approach for Managing Asthma in Youths ≥ 12 Years of Age and Adults Intermittent Asthma Persistent Asthma: Daily Medication Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3. Step 4 Step 3 Step 2 Step 1 Preferred: SABA PRN Preferred: Low -dose ICS Alternative: Cromolyn, LTRA, Nedocromil, or Theophylline Preferred: Low dose ICS + LABA OR mediumdose ICS Alternative: low-dose ICS + either LTRA, Theophylline, or Zileuton Preferred: Medium-dose ICS + LABA Step 5 Preferred: High-dose ICS + LABA Alternative: AND Medium-dose ICS+either Consider Omalizumab for patients who have allergies LTRA, Theophylline, or Zileuton Step 6 Preferred: High-dose ICS + LABA + oral corticosteroid AND Consider Omalizumab for patients who have allergies Each step: Patient education, environmental control, and management of comorbidities. Steps 2 -4: Consider subcutaneous allergen immunotherapy for patients who have allergic asthma * Quick-Relief Medication for All Patients SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20 -minute intervals as needed. Short course of oral systemic corticosteroids may be needed Step up if needed (first, check adherence, environmental control, and comorbid conditions) Assess control Step down if possible (and asthma is well controlled at least 3 months) Caution: Increasing use of SABA or use >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate control and the need to step up treatment. Key: Alphabetical order is used when more than one treatment option is listed within either preferred or alternative therapy. EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, inhaled long-acting beta 2 -agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled short-acting beta 2 -agonist *Immunotherapy for steps 2 -4 is based on Evidence B for house-dust mites, animal danders, and pollens; evidence is weak or lacking for molds and cockroaches. Evidence is strongest for immunotherapy with single allergens. The role of allergy in asthma is greater in children than in adults. Clinicians who administer immunotherapy should be prepared and equipped to identify and treat anaphylaxis that may occur.
Stepwise Approach for Managing Asthma in Youths ≥ 12 Years of Age and Adults Intermittent Asthma Persistent Asthma: Daily Medication Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3. Step 4 Step 3 Step 2 Step 1 Preferred: SABA PRN Preferred: Low -dose ICS Alternative: Cromolyn, LTRA, Nedocromil, or Theophylline Preferred: Low dose ICS + LABA OR mediumdose ICS Alternative: low-dose ICS + either LTRA, Theophylline, or Zileuton Preferred: Medium-dose ICS + LABA Step 5 Preferred: High-dose ICS + LABA Alternative: AND Medium-dose ICS+either Consider Omalizumab for patients who have allergies LTRA, Theophylline, or Zileuton Step 6 Preferred: High-dose ICS + LABA + oral corticosteroid AND Consider Omalizumab for patients who have allergies Each step: Patient education, environmental control, and management of comorbidities. Steps 2 -4: Consider subcutaneous allergen immunotherapy for patients who have allergic asthma * Quick-Relief Medication for All Patients SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20 -minute intervals as needed. Short course of oral systemic corticosteroids may be needed Step up if needed (first, check adherence, environmental control, and comorbid conditions) Assess control Step down if possible (and asthma is well controlled at least 3 months) Caution: Increasing use of SABA or use >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate control and the need to step up treatment. Key: Alphabetical order is used when more than one treatment option is listed within either preferred or alternative therapy. EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, inhaled long-acting beta 2 -agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled short-acting beta 2 -agonist *Immunotherapy for steps 2 -4 is based on Evidence B for house-dust mites, animal danders, and pollens; evidence is weak or lacking for molds and cockroaches. Evidence is strongest for immunotherapy with single allergens. The role of allergy in asthma is greater in children than in adults. Clinicians who administer immunotherapy should be prepared and equipped to identify and treat anaphylaxis that may occur.
 Preferred Medications § § § STEP 1 – SABA STEP 2 – ICS STEP 3 – ICS plus LABA or med dose ICS STEP 4 – med dose ICS plus LABA STEP 5 – high dose ICS and LABA STEP 6 – high dose ICA and LABA and oral corticosteroids.
Preferred Medications § § § STEP 1 – SABA STEP 2 – ICS STEP 3 – ICS plus LABA or med dose ICS STEP 4 – med dose ICS plus LABA STEP 5 – high dose ICS and LABA STEP 6 – high dose ICA and LABA and oral corticosteroids.
 Alternative Medications § § § Mast cell inhibitors Leukotriene receptor antagonists Leukotriene modifier Theophylline Omalizumab
Alternative Medications § § § Mast cell inhibitors Leukotriene receptor antagonists Leukotriene modifier Theophylline Omalizumab
 Inhaled medication § Short-acting beta-agonists – albuterol mentioned as “preferred” in pregnancy § Long-acting beta-agonists – used w/ low dose ICS (vs medium dose ICS) as step up in all but 0 -4 age group. Alternative at step 4 and above in all.
Inhaled medication § Short-acting beta-agonists – albuterol mentioned as “preferred” in pregnancy § Long-acting beta-agonists – used w/ low dose ICS (vs medium dose ICS) as step up in all but 0 -4 age group. Alternative at step 4 and above in all.
 Inhaled medication § Inhaled corticosteroids (ICS) the preferred long term controller in all age groups. § Low dose ICS alone in step 2 for all. § Low dose plus add-on OR medium dose ICS for step 3 except ages 0 -4.
Inhaled medication § Inhaled corticosteroids (ICS) the preferred long term controller in all age groups. § Low dose ICS alone in step 2 for all. § Low dose plus add-on OR medium dose ICS for step 3 except ages 0 -4.
 Leukotriene modifiers § Montelukast safe for all patients, of all ages, as alternative to low dose ICS or add on to low, medium or high dose ICS. § Zafirlukast same role in all but 0 -4 age group. § Zileuton in age > 12 as add on to low dose ICS + LABA, or to medium dose ICS
Leukotriene modifiers § Montelukast safe for all patients, of all ages, as alternative to low dose ICS or add on to low, medium or high dose ICS. § Zafirlukast same role in all but 0 -4 age group. § Zileuton in age > 12 as add on to low dose ICS + LABA, or to medium dose ICS
 Cromolyn and Nedocromil § Stabilize mast cells and interfere with chloride channels § Can be used as an alternative but not preferred medication in step 2 in all. § Preventive therapy for exercise/exposure
Cromolyn and Nedocromil § Stabilize mast cells and interfere with chloride channels § Can be used as an alternative but not preferred medication in step 2 in all. § Preventive therapy for exercise/exposure
 Theophylline § Mild to moderate bronchodilator § May have mild anti-inflammatory effect. § Alternative or adjunctive therapy with ICS in all patients > 5 § Monitoring levels essential.
Theophylline § Mild to moderate bronchodilator § May have mild anti-inflammatory effect. § Alternative or adjunctive therapy with ICS in all patients > 5 § Monitoring levels essential.
 Written Action Plan § Written action plans detailing medications and environmental control strategies tailored for each patient are recommended for all patients with asthma § Environmental Control § Awareness and control
Written Action Plan § Written action plans detailing medications and environmental control strategies tailored for each patient are recommended for all patients with asthma § Environmental Control § Awareness and control
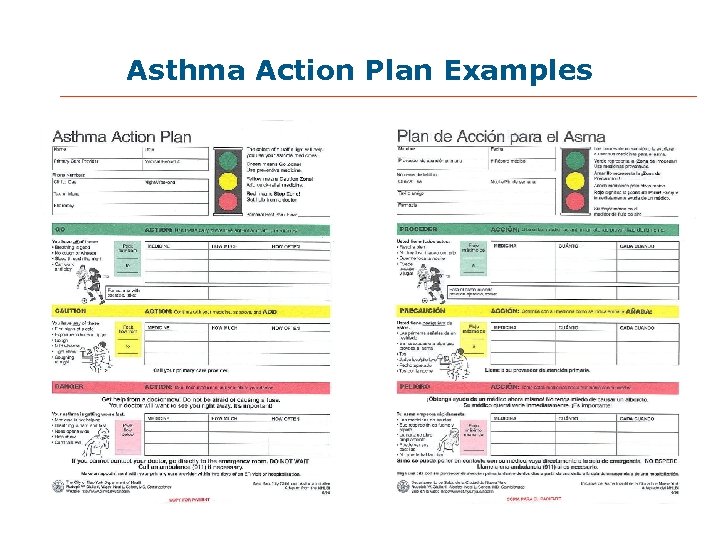 Asthma Action Plan Examples
Asthma Action Plan Examples
 Written Action Plan Components § Note when and how to treat signs of an exacerbation § Adjust meds by increasing SABA, add oral CS. § To be effective, patient must have prescription for oral CS available § Doubling dose of ICS not part of plan – not effective during exacerbation.
Written Action Plan Components § Note when and how to treat signs of an exacerbation § Adjust meds by increasing SABA, add oral CS. § To be effective, patient must have prescription for oral CS available § Doubling dose of ICS not part of plan – not effective during exacerbation.
 Peak Expiratory Flow § PEF based plan particularly useful for those who have difficulty perceiving airflow obstruction or have history of severe exacerbations § “Gold standard” is patient’s personal best. § Green/yellow/red zones objective data.
Peak Expiratory Flow § PEF based plan particularly useful for those who have difficulty perceiving airflow obstruction or have history of severe exacerbations § “Gold standard” is patient’s personal best. § Green/yellow/red zones objective data.
 Environmental Control § House dust mite – mattress covers, pillow covers, washing in hot water, acaricides § Cat Allergen – air filters, washing the cat, keep cat out of the bedroom. § Cockroach – extermination and thorough cleaning No evidence that any of these change patient oriented outcomes.
Environmental Control § House dust mite – mattress covers, pillow covers, washing in hot water, acaricides § Cat Allergen – air filters, washing the cat, keep cat out of the bedroom. § Cockroach – extermination and thorough cleaning No evidence that any of these change patient oriented outcomes.
 Summary § Asthma classification by Severity and Control § Level of Severity and of Control relate to current impairment and future risk. § ICS Mainstay of treatment § Low dose ICS plus LABA equal to Medium dose LABA in adults and children >5 § Written action plans important.
Summary § Asthma classification by Severity and Control § Level of Severity and of Control relate to current impairment and future risk. § ICS Mainstay of treatment § Low dose ICS plus LABA equal to Medium dose LABA in adults and children >5 § Written action plans important.


