69b3629f1f8c698a0ed008fa07ab29a0.ppt
- Количество слайдов: 149
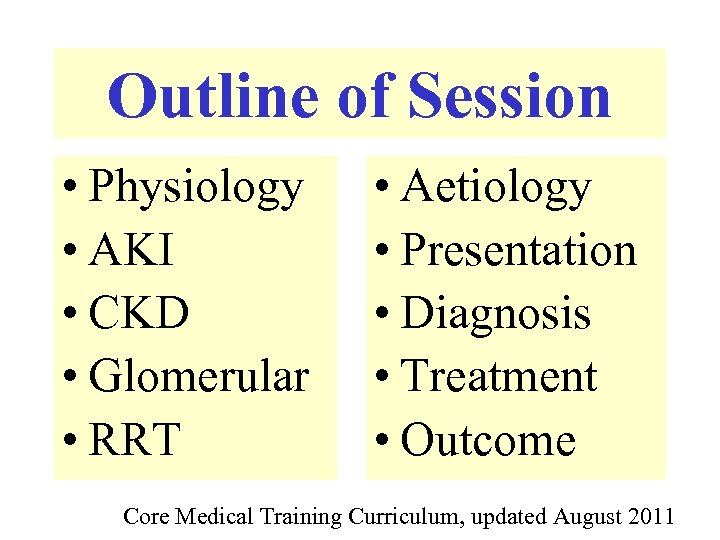 Outline of Session • Physiology • AKI • CKD • Glomerular • RRT • Aetiology • Presentation • Diagnosis • Treatment • Outcome Core Medical Training Curriculum, updated August 2011
Outline of Session • Physiology • AKI • CKD • Glomerular • RRT • Aetiology • Presentation • Diagnosis • Treatment • Outcome Core Medical Training Curriculum, updated August 2011
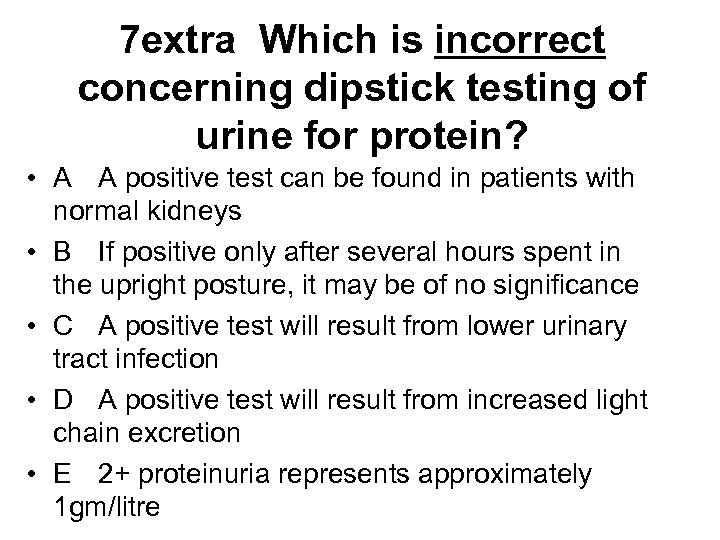 7 extra Which is incorrect concerning dipstick testing of urine for protein? • A A positive test can be found in patients with normal kidneys • B If positive only after several hours spent in the upright posture, it may be of no significance • C A positive test will result from lower urinary tract infection • D A positive test will result from increased light chain excretion • E 2+ proteinuria represents approximately 1 gm/litre
7 extra Which is incorrect concerning dipstick testing of urine for protein? • A A positive test can be found in patients with normal kidneys • B If positive only after several hours spent in the upright posture, it may be of no significance • C A positive test will result from lower urinary tract infection • D A positive test will result from increased light chain excretion • E 2+ proteinuria represents approximately 1 gm/litre
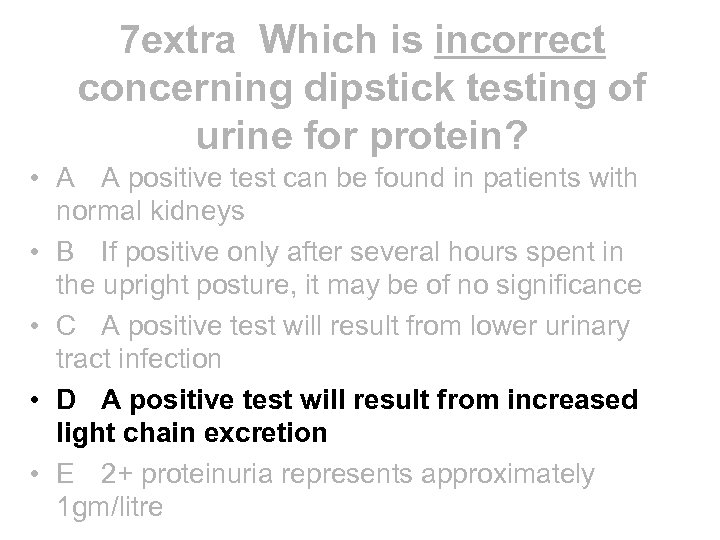 7 extra Which is incorrect concerning dipstick testing of urine for protein? • A A positive test can be found in patients with normal kidneys • B If positive only after several hours spent in the upright posture, it may be of no significance • C A positive test will result from lower urinary tract infection • D A positive test will result from increased light chain excretion • E 2+ proteinuria represents approximately 1 gm/litre
7 extra Which is incorrect concerning dipstick testing of urine for protein? • A A positive test can be found in patients with normal kidneys • B If positive only after several hours spent in the upright posture, it may be of no significance • C A positive test will result from lower urinary tract infection • D A positive test will result from increased light chain excretion • E 2+ proteinuria represents approximately 1 gm/litre
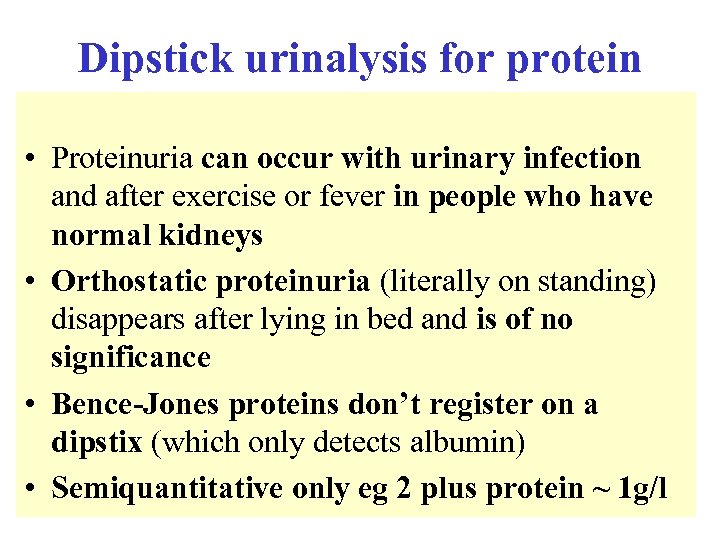 Dipstick urinalysis for protein • Proteinuria can occur with urinary infection and after exercise or fever in people who have normal kidneys • Orthostatic proteinuria (literally on standing) disappears after lying in bed and is of no significance • Bence-Jones proteins don’t register on a dipstix (which only detects albumin) • Semiquantitative only eg 2 plus protein ~ 1 g/l
Dipstick urinalysis for protein • Proteinuria can occur with urinary infection and after exercise or fever in people who have normal kidneys • Orthostatic proteinuria (literally on standing) disappears after lying in bed and is of no significance • Bence-Jones proteins don’t register on a dipstix (which only detects albumin) • Semiquantitative only eg 2 plus protein ~ 1 g/l
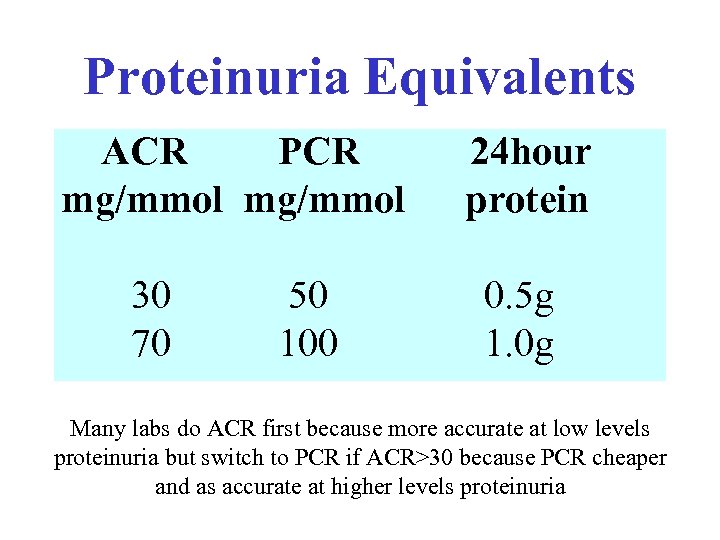 Proteinuria Equivalents ACR PCR mg/mmol 30 70 50 100 24 hour protein 0. 5 g 1. 0 g Many labs do ACR first because more accurate at low levels proteinuria but switch to PCR if ACR>30 because PCR cheaper and as accurate at higher levels proteinuria
Proteinuria Equivalents ACR PCR mg/mmol 30 70 50 100 24 hour protein 0. 5 g 1. 0 g Many labs do ACR first because more accurate at low levels proteinuria but switch to PCR if ACR>30 because PCR cheaper and as accurate at higher levels proteinuria
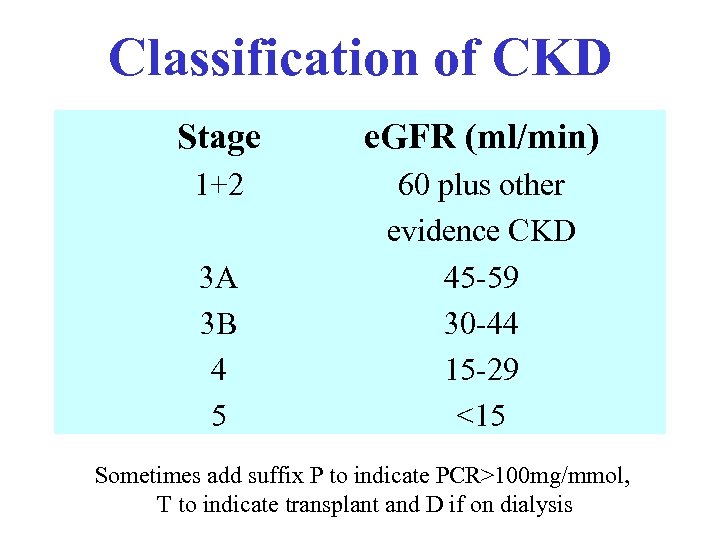 Classification of CKD Stage e. GFR (ml/min) 1+2 60 plus other evidence CKD 45 -59 30 -44 15 -29 <15 3 A 3 B 4 5 Sometimes add suffix P to indicate PCR>100 mg/mmol, T to indicate transplant and D if on dialysis
Classification of CKD Stage e. GFR (ml/min) 1+2 60 plus other evidence CKD 45 -59 30 -44 15 -29 <15 3 A 3 B 4 5 Sometimes add suffix P to indicate PCR>100 mg/mmol, T to indicate transplant and D if on dialysis
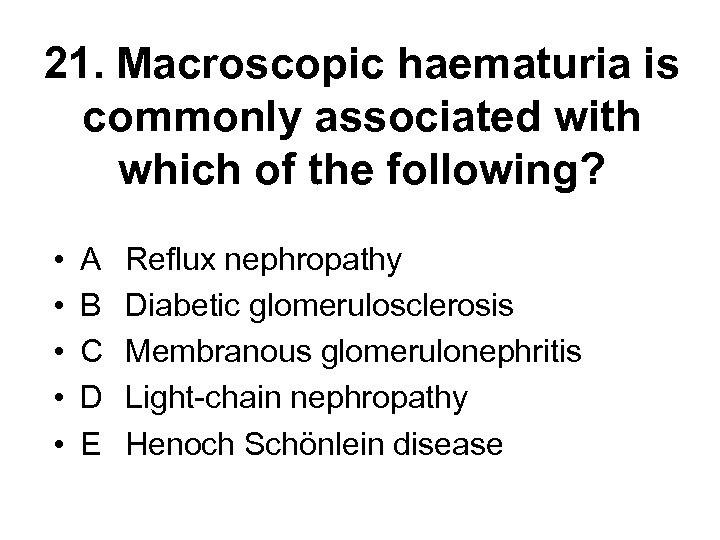 21. Macroscopic haematuria is commonly associated with which of the following? • • • A B C D E Reflux nephropathy Diabetic glomerulosclerosis Membranous glomerulonephritis Light-chain nephropathy Henoch Schönlein disease
21. Macroscopic haematuria is commonly associated with which of the following? • • • A B C D E Reflux nephropathy Diabetic glomerulosclerosis Membranous glomerulonephritis Light-chain nephropathy Henoch Schönlein disease
 21. Macroscopic haematuria is commonly associated with which of the following? • • • A B C D E Reflux nephropathy Diabetic glomerulosclerosis Membranous glomerulonephritis Light-chain nephropathy Henoch Schönlein disease
21. Macroscopic haematuria is commonly associated with which of the following? • • • A B C D E Reflux nephropathy Diabetic glomerulosclerosis Membranous glomerulonephritis Light-chain nephropathy Henoch Schönlein disease
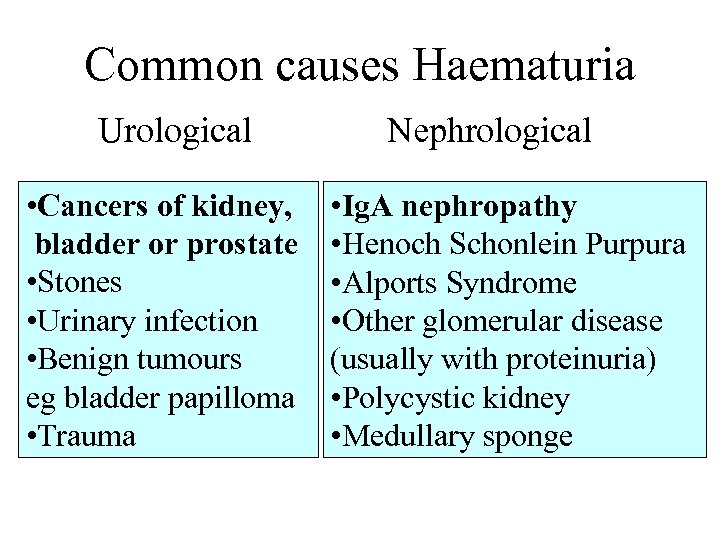 Common causes Haematuria Urological • Cancers of kidney, bladder or prostate • Stones • Urinary infection • Benign tumours eg bladder papilloma • Trauma Nephrological • Ig. A nephropathy • Henoch Schonlein Purpura • Alports Syndrome • Other glomerular disease (usually with proteinuria) • Polycystic kidney • Medullary sponge
Common causes Haematuria Urological • Cancers of kidney, bladder or prostate • Stones • Urinary infection • Benign tumours eg bladder papilloma • Trauma Nephrological • Ig. A nephropathy • Henoch Schonlein Purpura • Alports Syndrome • Other glomerular disease (usually with proteinuria) • Polycystic kidney • Medullary sponge
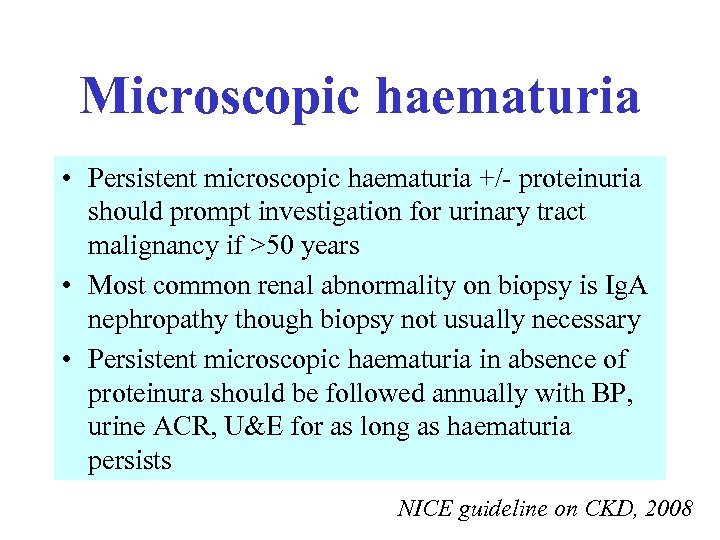 Microscopic haematuria • Persistent microscopic haematuria +/- proteinuria should prompt investigation for urinary tract malignancy if >50 years • Most common renal abnormality on biopsy is Ig. A nephropathy though biopsy not usually necessary • Persistent microscopic haematuria in absence of proteinura should be followed annually with BP, urine ACR, U&E for as long as haematuria persists NICE guideline on CKD, 2008
Microscopic haematuria • Persistent microscopic haematuria +/- proteinuria should prompt investigation for urinary tract malignancy if >50 years • Most common renal abnormality on biopsy is Ig. A nephropathy though biopsy not usually necessary • Persistent microscopic haematuria in absence of proteinura should be followed annually with BP, urine ACR, U&E for as long as haematuria persists NICE guideline on CKD, 2008
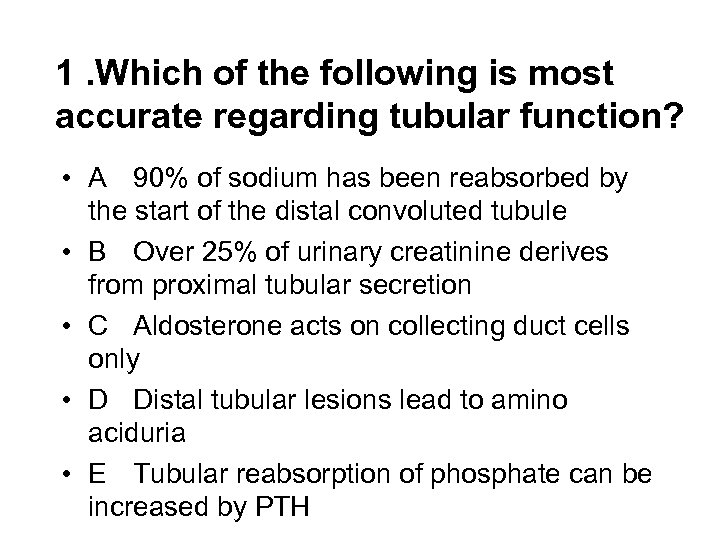 1. Which of the following is most accurate regarding tubular function? • A 90% of sodium has been reabsorbed by the start of the distal convoluted tubule • B Over 25% of urinary creatinine derives from proximal tubular secretion • C Aldosterone acts on collecting duct cells only • D Distal tubular lesions lead to amino aciduria • E Tubular reabsorption of phosphate can be increased by PTH
1. Which of the following is most accurate regarding tubular function? • A 90% of sodium has been reabsorbed by the start of the distal convoluted tubule • B Over 25% of urinary creatinine derives from proximal tubular secretion • C Aldosterone acts on collecting duct cells only • D Distal tubular lesions lead to amino aciduria • E Tubular reabsorption of phosphate can be increased by PTH
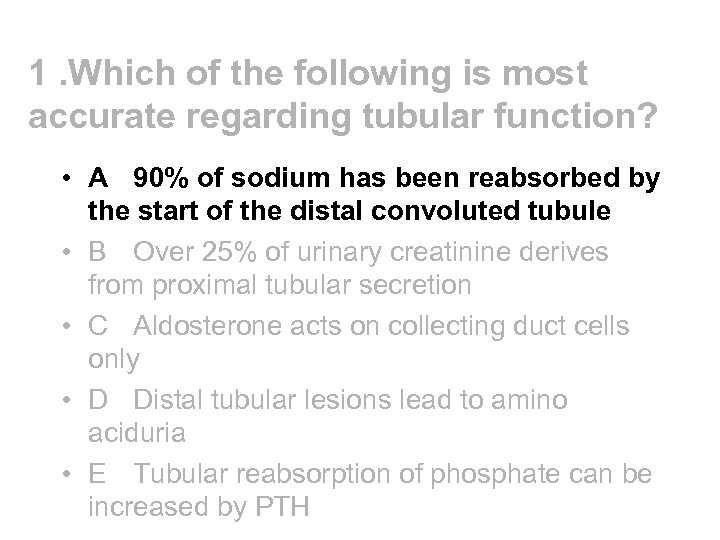 1. Which of the following is most accurate regarding tubular function? • A 90% of sodium has been reabsorbed by the start of the distal convoluted tubule • B Over 25% of urinary creatinine derives from proximal tubular secretion • C Aldosterone acts on collecting duct cells only • D Distal tubular lesions lead to amino aciduria • E Tubular reabsorption of phosphate can be increased by PTH
1. Which of the following is most accurate regarding tubular function? • A 90% of sodium has been reabsorbed by the start of the distal convoluted tubule • B Over 25% of urinary creatinine derives from proximal tubular secretion • C Aldosterone acts on collecting duct cells only • D Distal tubular lesions lead to amino aciduria • E Tubular reabsorption of phosphate can be increased by PTH
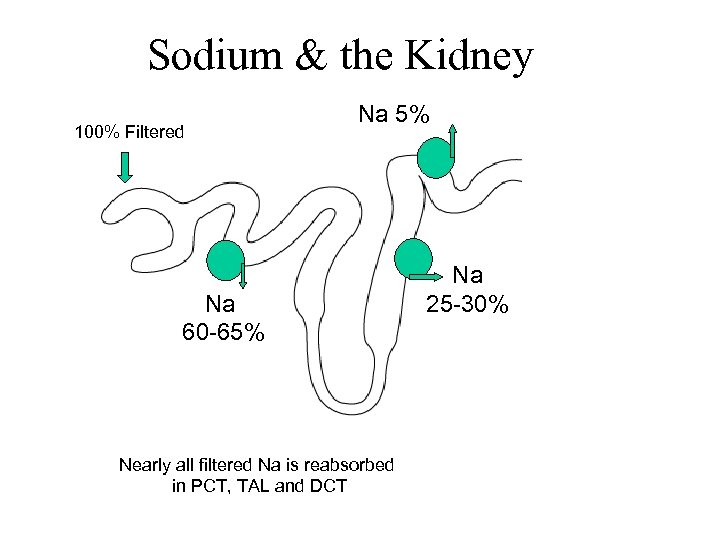 Sodium & the Kidney 100% Filtered Na 5% Na 60 -65% Nearly all filtered Na is reabsorbed in PCT, TAL and DCT Na 25 -30% Na 4% Day to day control of Na excretion takes place in CCD by aldo and ADH
Sodium & the Kidney 100% Filtered Na 5% Na 60 -65% Nearly all filtered Na is reabsorbed in PCT, TAL and DCT Na 25 -30% Na 4% Day to day control of Na excretion takes place in CCD by aldo and ADH
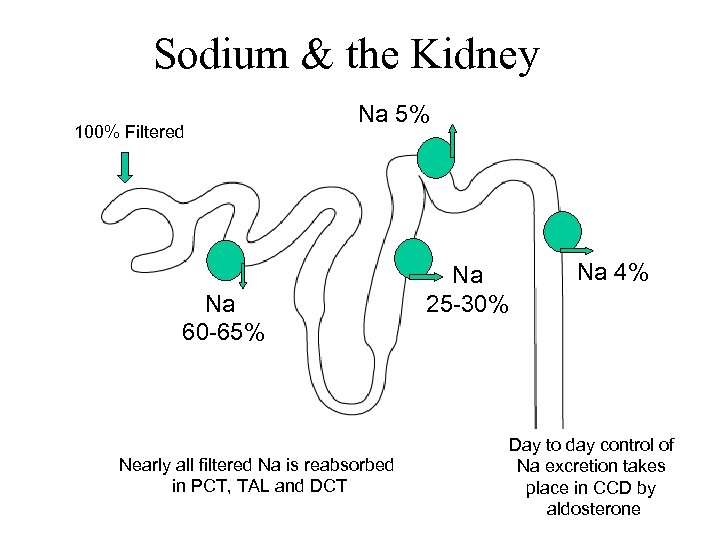 Sodium & the Kidney 100% Filtered Na 5% Na 60 -65% Nearly all filtered Na is reabsorbed in PCT, TAL and DCT Na 25 -30% Na 4% Day to day control of Na excretion takes place in CCD by aldosterone
Sodium & the Kidney 100% Filtered Na 5% Na 60 -65% Nearly all filtered Na is reabsorbed in PCT, TAL and DCT Na 25 -30% Na 4% Day to day control of Na excretion takes place in CCD by aldosterone
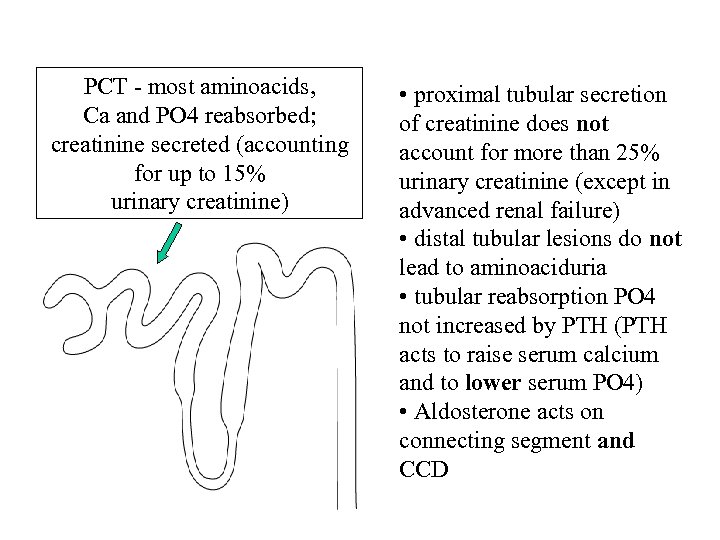 PCT - most aminoacids, Ca and PO 4 reabsorbed; creatinine secreted (accounting for up to 15% urinary creatinine) • proximal tubular secretion of creatinine does not account for more than 25% urinary creatinine (except in advanced renal failure) • distal tubular lesions do not lead to aminoaciduria • tubular reabsorption PO 4 not increased by PTH (PTH acts to raise serum calcium and to lower serum PO 4) • Aldosterone acts on connecting segment and CCD
PCT - most aminoacids, Ca and PO 4 reabsorbed; creatinine secreted (accounting for up to 15% urinary creatinine) • proximal tubular secretion of creatinine does not account for more than 25% urinary creatinine (except in advanced renal failure) • distal tubular lesions do not lead to aminoaciduria • tubular reabsorption PO 4 not increased by PTH (PTH acts to raise serum calcium and to lower serum PO 4) • Aldosterone acts on connecting segment and CCD
 3. With metabolic acidosis, a normal anion gap would be most suggestive of: • A Alcohol excess • B Lactic acidosis • C Diarrhoea • D Salicylate poisoning • E Diabetic ketosis
3. With metabolic acidosis, a normal anion gap would be most suggestive of: • A Alcohol excess • B Lactic acidosis • C Diarrhoea • D Salicylate poisoning • E Diabetic ketosis
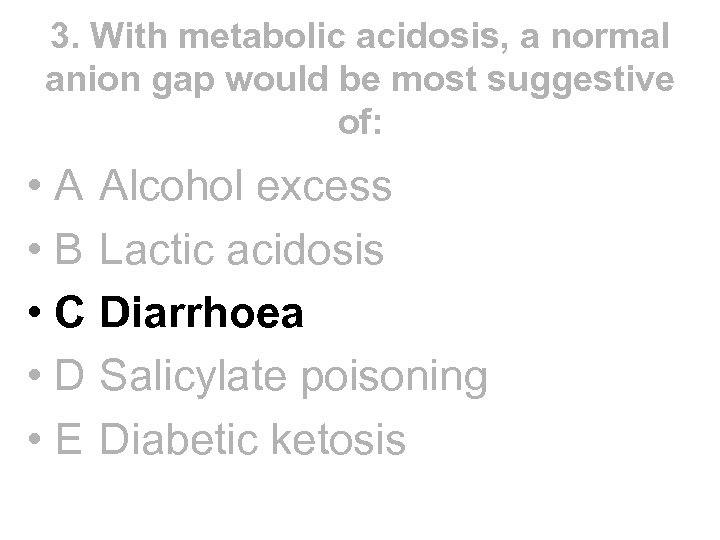 3. With metabolic acidosis, a normal anion gap would be most suggestive of: • A Alcohol excess • B Lactic acidosis • C Diarrhoea • D Salicylate poisoning • E Diabetic ketosis
3. With metabolic acidosis, a normal anion gap would be most suggestive of: • A Alcohol excess • B Lactic acidosis • C Diarrhoea • D Salicylate poisoning • E Diabetic ketosis
 How do you know if acidosis is due to diarrhoea or to some other cause?
How do you know if acidosis is due to diarrhoea or to some other cause?
![Measure anion gap = [Na+ + K+] - [Cl- + HCO 3 -] Normal Measure anion gap = [Na+ + K+] - [Cl- + HCO 3 -] Normal](https://present5.com/presentation/69b3629f1f8c698a0ed008fa07ab29a0/image-19.jpg) Measure anion gap = [Na+ + K+] - [Cl- + HCO 3 -] Normal 12 -18 Diarrhoea RTA Urinary diversion Normal because when bicarb is lost kidneys retain chloride to maintain electroneutrality Raised >18 DKA Renal Failure Salicylate Methanol, ethylene glycol Raised due to presence of unmeasured anions
Measure anion gap = [Na+ + K+] - [Cl- + HCO 3 -] Normal 12 -18 Diarrhoea RTA Urinary diversion Normal because when bicarb is lost kidneys retain chloride to maintain electroneutrality Raised >18 DKA Renal Failure Salicylate Methanol, ethylene glycol Raised due to presence of unmeasured anions
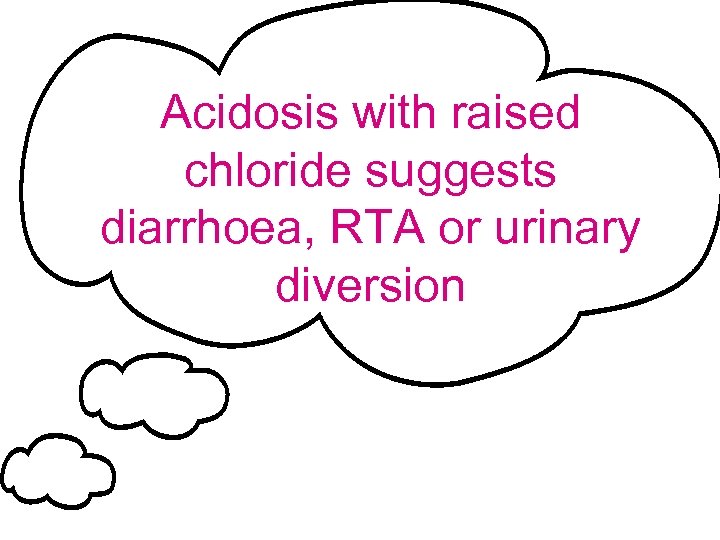 Acidosis with raised chloride suggests diarrhoea, RTA or urinary diversion
Acidosis with raised chloride suggests diarrhoea, RTA or urinary diversion
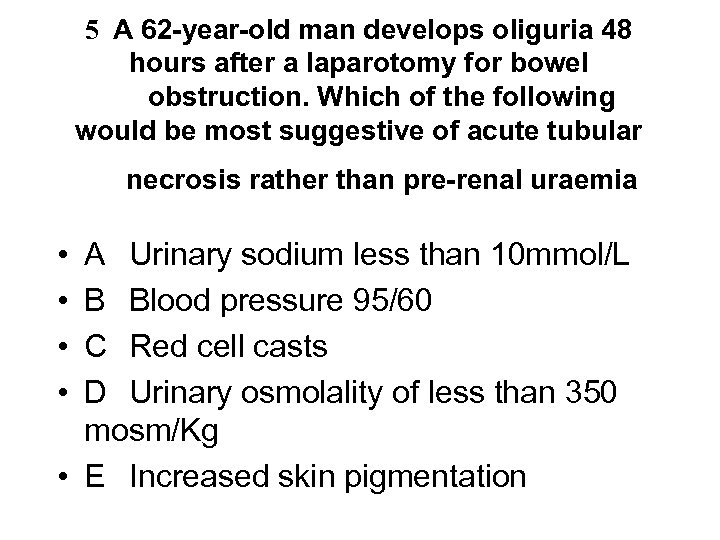 5 A 62 -year-old man develops oliguria 48 hours after a laparotomy for bowel obstruction. Which of the following would be most suggestive of acute tubular necrosis rather than pre-renal uraemia • • A Urinary sodium less than 10 mmol/L B Blood pressure 95/60 C Red cell casts D Urinary osmolality of less than 350 mosm/Kg • E Increased skin pigmentation
5 A 62 -year-old man develops oliguria 48 hours after a laparotomy for bowel obstruction. Which of the following would be most suggestive of acute tubular necrosis rather than pre-renal uraemia • • A Urinary sodium less than 10 mmol/L B Blood pressure 95/60 C Red cell casts D Urinary osmolality of less than 350 mosm/Kg • E Increased skin pigmentation
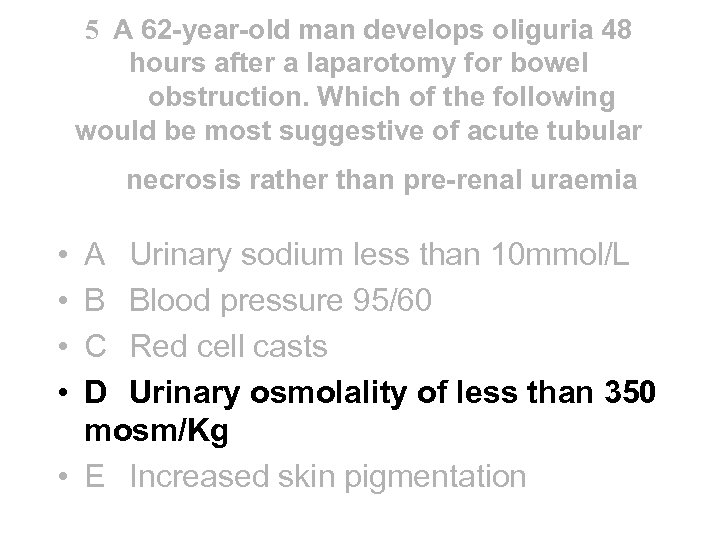 5 A 62 -year-old man develops oliguria 48 hours after a laparotomy for bowel obstruction. Which of the following would be most suggestive of acute tubular necrosis rather than pre-renal uraemia • • A Urinary sodium less than 10 mmol/L B Blood pressure 95/60 C Red cell casts D Urinary osmolality of less than 350 mosm/Kg • E Increased skin pigmentation
5 A 62 -year-old man develops oliguria 48 hours after a laparotomy for bowel obstruction. Which of the following would be most suggestive of acute tubular necrosis rather than pre-renal uraemia • • A Urinary sodium less than 10 mmol/L B Blood pressure 95/60 C Red cell casts D Urinary osmolality of less than 350 mosm/Kg • E Increased skin pigmentation
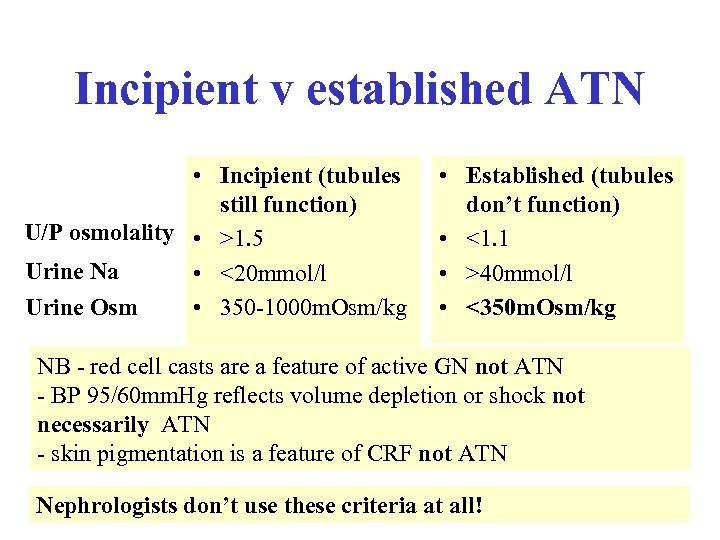 Incipient v established ATN • Incipient (tubules still function) U/P osmolality • >1. 5 Urine Na • <20 mmol/l Urine Osm • 350 -1000 m. Osm/kg • Established (tubules don’t function) • <1. 1 • >40 mmol/l • <350 m. Osm/kg NB - red cell casts are a feature of active GN not ATN - BP 95/60 mm. Hg reflects volume depletion or shock not necessarily ATN - skin pigmentation is a feature of CRF not ATN Nephrologists don’t use these criteria at all!
Incipient v established ATN • Incipient (tubules still function) U/P osmolality • >1. 5 Urine Na • <20 mmol/l Urine Osm • 350 -1000 m. Osm/kg • Established (tubules don’t function) • <1. 1 • >40 mmol/l • <350 m. Osm/kg NB - red cell casts are a feature of active GN not ATN - BP 95/60 mm. Hg reflects volume depletion or shock not necessarily ATN - skin pigmentation is a feature of CRF not ATN Nephrologists don’t use these criteria at all!
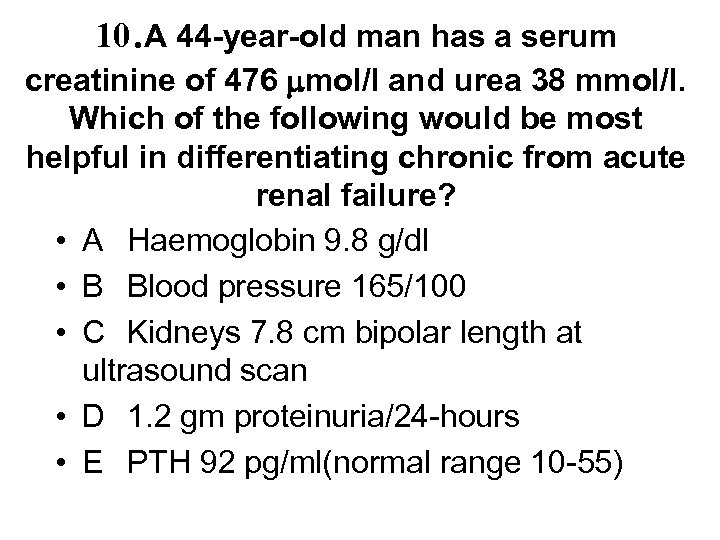 10. A 44 -year-old man has a serum creatinine of 476 mol/l and urea 38 mmol/l. Which of the following would be most helpful in differentiating chronic from acute renal failure? • A Haemoglobin 9. 8 g/dl • B Blood pressure 165/100 • C Kidneys 7. 8 cm bipolar length at ultrasound scan • D 1. 2 gm proteinuria/24 -hours • E PTH 92 pg/ml(normal range 10 -55)
10. A 44 -year-old man has a serum creatinine of 476 mol/l and urea 38 mmol/l. Which of the following would be most helpful in differentiating chronic from acute renal failure? • A Haemoglobin 9. 8 g/dl • B Blood pressure 165/100 • C Kidneys 7. 8 cm bipolar length at ultrasound scan • D 1. 2 gm proteinuria/24 -hours • E PTH 92 pg/ml(normal range 10 -55)
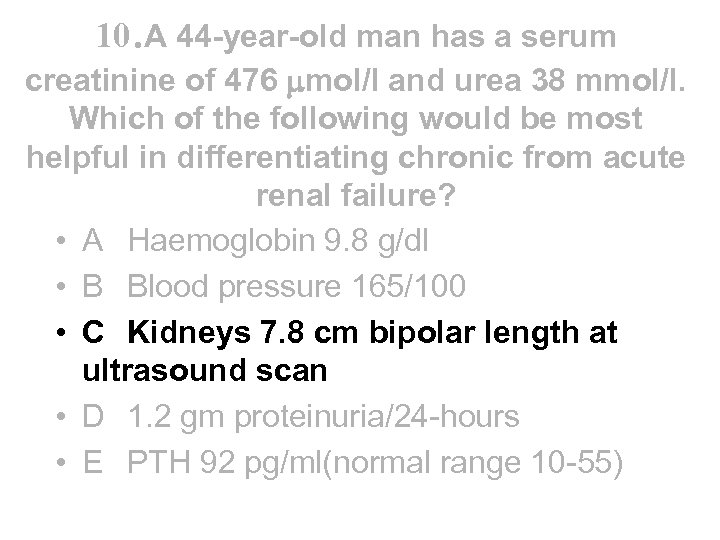 10. A 44 -year-old man has a serum creatinine of 476 mol/l and urea 38 mmol/l. Which of the following would be most helpful in differentiating chronic from acute renal failure? • A Haemoglobin 9. 8 g/dl • B Blood pressure 165/100 • C Kidneys 7. 8 cm bipolar length at ultrasound scan • D 1. 2 gm proteinuria/24 -hours • E PTH 92 pg/ml(normal range 10 -55)
10. A 44 -year-old man has a serum creatinine of 476 mol/l and urea 38 mmol/l. Which of the following would be most helpful in differentiating chronic from acute renal failure? • A Haemoglobin 9. 8 g/dl • B Blood pressure 165/100 • C Kidneys 7. 8 cm bipolar length at ultrasound scan • D 1. 2 gm proteinuria/24 -hours • E PTH 92 pg/ml(normal range 10 -55)
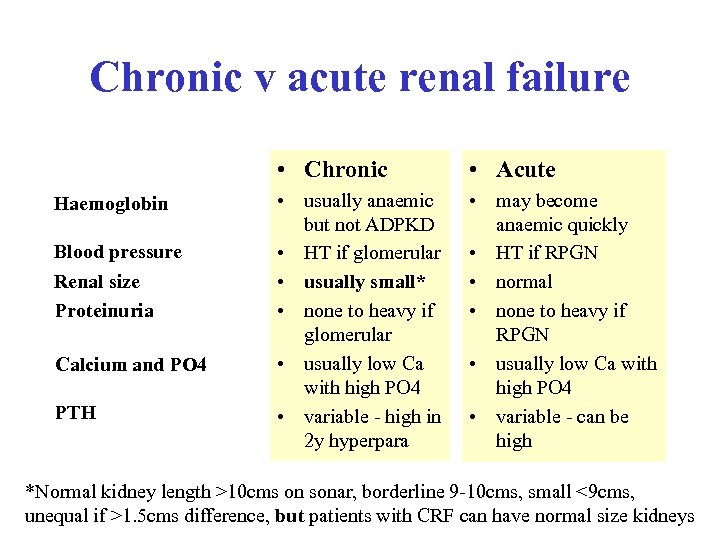 Chronic v acute renal failure • Chronic Haemoglobin Blood pressure Renal size Proteinuria Calcium and PO 4 PTH • Acute • usually anaemic but not ADPKD • HT if glomerular • usually small* • none to heavy if glomerular • usually low Ca with high PO 4 • variable - high in 2 y hyperpara • may become anaemic quickly • HT if RPGN • normal • none to heavy if RPGN • usually low Ca with high PO 4 • variable - can be high *Normal kidney length >10 cms on sonar, borderline 9 -10 cms, small <9 cms, unequal if >1. 5 cms difference, but patients with CRF can have normal size kidneys
Chronic v acute renal failure • Chronic Haemoglobin Blood pressure Renal size Proteinuria Calcium and PO 4 PTH • Acute • usually anaemic but not ADPKD • HT if glomerular • usually small* • none to heavy if glomerular • usually low Ca with high PO 4 • variable - high in 2 y hyperpara • may become anaemic quickly • HT if RPGN • normal • none to heavy if RPGN • usually low Ca with high PO 4 • variable - can be high *Normal kidney length >10 cms on sonar, borderline 9 -10 cms, small <9 cms, unequal if >1. 5 cms difference, but patients with CRF can have normal size kidneys
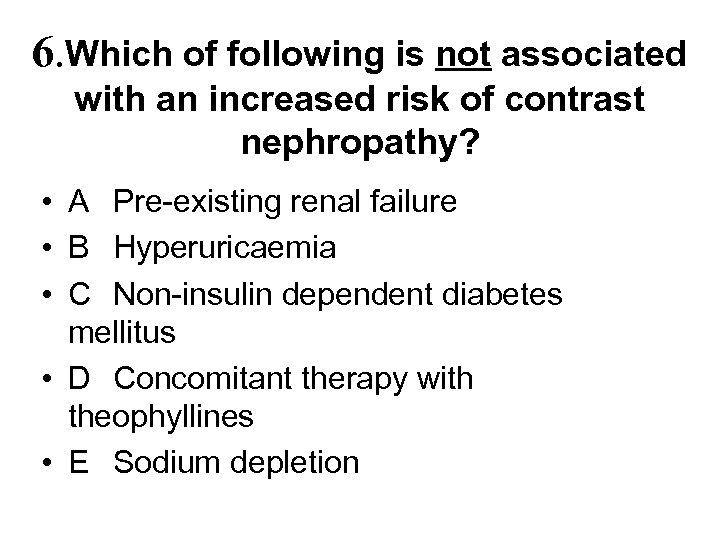 6. Which of following is not associated with an increased risk of contrast nephropathy? • A Pre-existing renal failure • B Hyperuricaemia • C Non-insulin dependent diabetes mellitus • D Concomitant therapy with theophyllines • E Sodium depletion
6. Which of following is not associated with an increased risk of contrast nephropathy? • A Pre-existing renal failure • B Hyperuricaemia • C Non-insulin dependent diabetes mellitus • D Concomitant therapy with theophyllines • E Sodium depletion
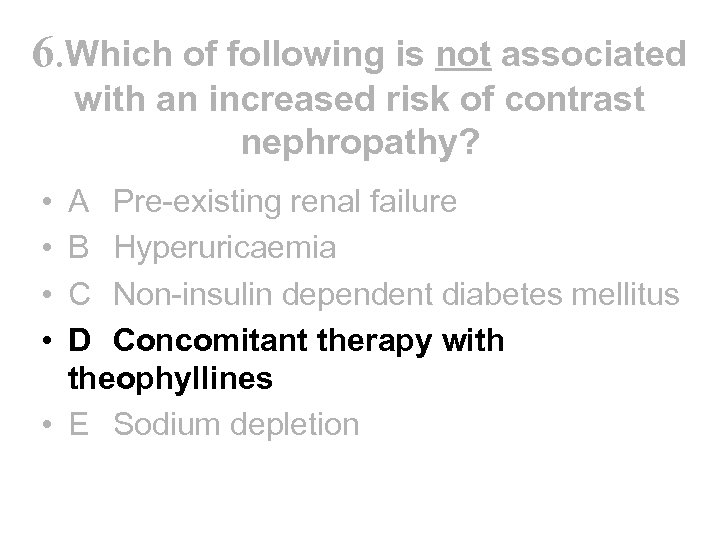 6. Which of following is not associated with an increased risk of contrast nephropathy? • • A Pre-existing renal failure B Hyperuricaemia C Non-insulin dependent diabetes mellitus D Concomitant therapy with theophyllines • E Sodium depletion
6. Which of following is not associated with an increased risk of contrast nephropathy? • • A Pre-existing renal failure B Hyperuricaemia C Non-insulin dependent diabetes mellitus D Concomitant therapy with theophyllines • E Sodium depletion
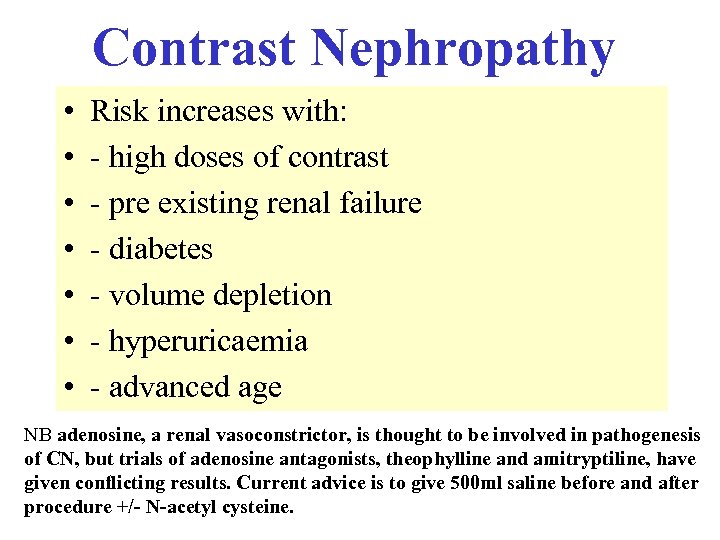 Contrast Nephropathy • • Risk increases with: - high doses of contrast - pre existing renal failure - diabetes - volume depletion - hyperuricaemia - advanced age NB adenosine, a renal vasoconstrictor, is thought to be involved in pathogenesis of CN, but trials of adenosine antagonists, theophylline and amitryptiline, have given conflicting results. Current advice is to give 500 ml saline before and after procedure +/- N-acetyl cysteine.
Contrast Nephropathy • • Risk increases with: - high doses of contrast - pre existing renal failure - diabetes - volume depletion - hyperuricaemia - advanced age NB adenosine, a renal vasoconstrictor, is thought to be involved in pathogenesis of CN, but trials of adenosine antagonists, theophylline and amitryptiline, have given conflicting results. Current advice is to give 500 ml saline before and after procedure +/- N-acetyl cysteine.
 7. Which of the following statements concerning HUS is correct ? • A Infective diarrhoea is invariably associated • B Platelet counts are usually higher than in thrombotic thrombocytopaenic purpura • C It is usually fatal in children • D Steroids are of proven benefit • E Surviving patients are likely to require long term dialysis
7. Which of the following statements concerning HUS is correct ? • A Infective diarrhoea is invariably associated • B Platelet counts are usually higher than in thrombotic thrombocytopaenic purpura • C It is usually fatal in children • D Steroids are of proven benefit • E Surviving patients are likely to require long term dialysis
 7. Which of the following statements concerning HUS is correct ? • A Infective diarrhoea is invariably associated • B Platelet counts are usually higher than in thrombotic thrombocytopenic purpura • C It is usually fatal in children • D Steroids are of proven benefit • E Surviving patients are likely to require long term dialysis
7. Which of the following statements concerning HUS is correct ? • A Infective diarrhoea is invariably associated • B Platelet counts are usually higher than in thrombotic thrombocytopenic purpura • C It is usually fatal in children • D Steroids are of proven benefit • E Surviving patients are likely to require long term dialysis
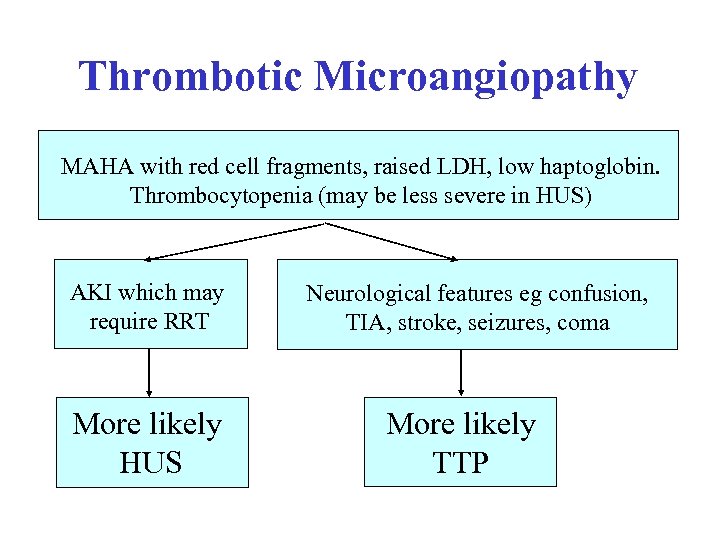 Thrombotic Microangiopathy MAHA with red cell fragments, raised LDH, low haptoglobin. Thrombocytopenia (may be less severe in HUS) AKI which may require RRT More likely HUS Neurological features eg confusion, TIA, stroke, seizures, coma More likely TTP
Thrombotic Microangiopathy MAHA with red cell fragments, raised LDH, low haptoglobin. Thrombocytopenia (may be less severe in HUS) AKI which may require RRT More likely HUS Neurological features eg confusion, TIA, stroke, seizures, coma More likely TTP
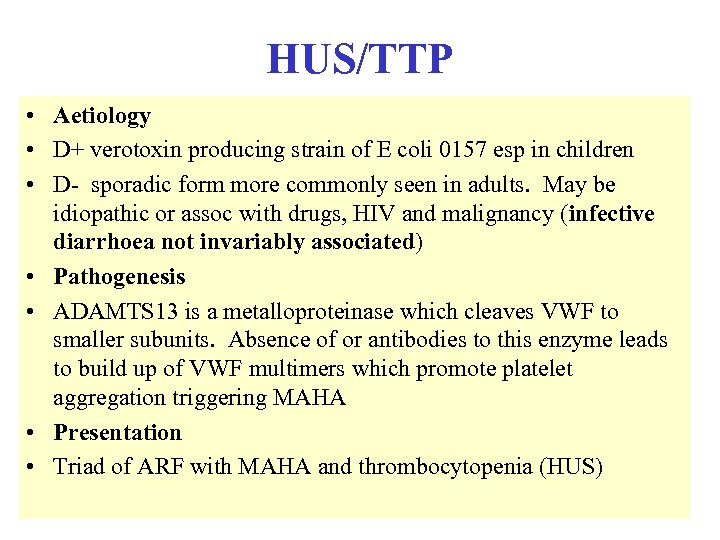 HUS/TTP • Aetiology • D+ verotoxin producing strain of E coli 0157 esp in children • D- sporadic form more commonly seen in adults. May be idiopathic or assoc with drugs, HIV and malignancy (infective diarrhoea not invariably associated) • Pathogenesis • ADAMTS 13 is a metalloproteinase which cleaves VWF to smaller subunits. Absence of or antibodies to this enzyme leads to build up of VWF multimers which promote platelet aggregation triggering MAHA • Presentation • Triad of ARF with MAHA and thrombocytopenia (HUS)
HUS/TTP • Aetiology • D+ verotoxin producing strain of E coli 0157 esp in children • D- sporadic form more commonly seen in adults. May be idiopathic or assoc with drugs, HIV and malignancy (infective diarrhoea not invariably associated) • Pathogenesis • ADAMTS 13 is a metalloproteinase which cleaves VWF to smaller subunits. Absence of or antibodies to this enzyme leads to build up of VWF multimers which promote platelet aggregation triggering MAHA • Presentation • Triad of ARF with MAHA and thrombocytopenia (HUS)
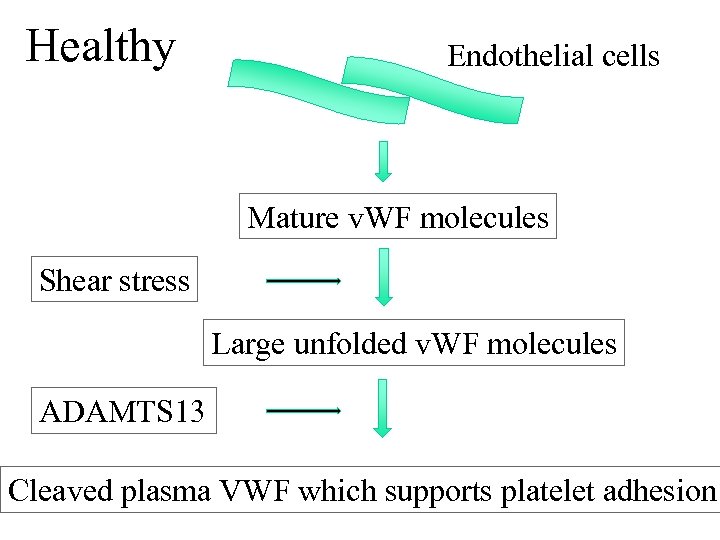 Healthy Endothelial cells Mature v. WF molecules Shear stress Large unfolded v. WF molecules ADAMTS 13 Cleaved plasma VWF which supports platelet adhesion
Healthy Endothelial cells Mature v. WF molecules Shear stress Large unfolded v. WF molecules ADAMTS 13 Cleaved plasma VWF which supports platelet adhesion
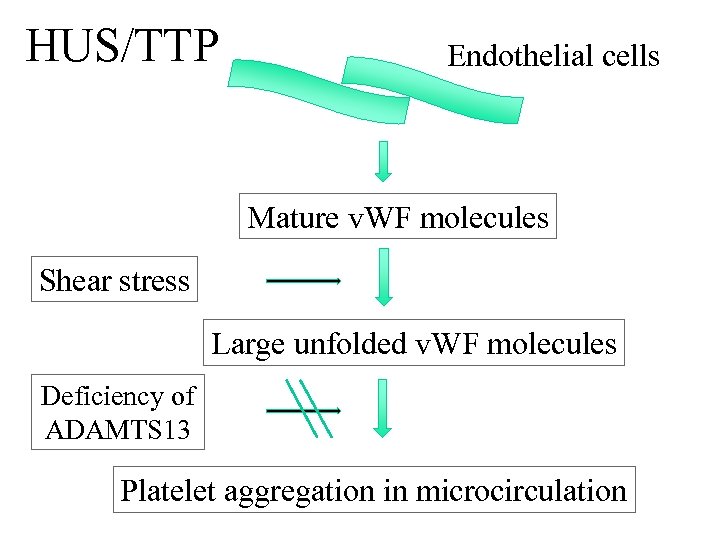 HUS/TTP Endothelial cells Mature v. WF molecules Shear stress Large unfolded v. WF molecules Deficiency of ADAMTS 13 Platelet aggregation in microcirculation
HUS/TTP Endothelial cells Mature v. WF molecules Shear stress Large unfolded v. WF molecules Deficiency of ADAMTS 13 Platelet aggregation in microcirculation
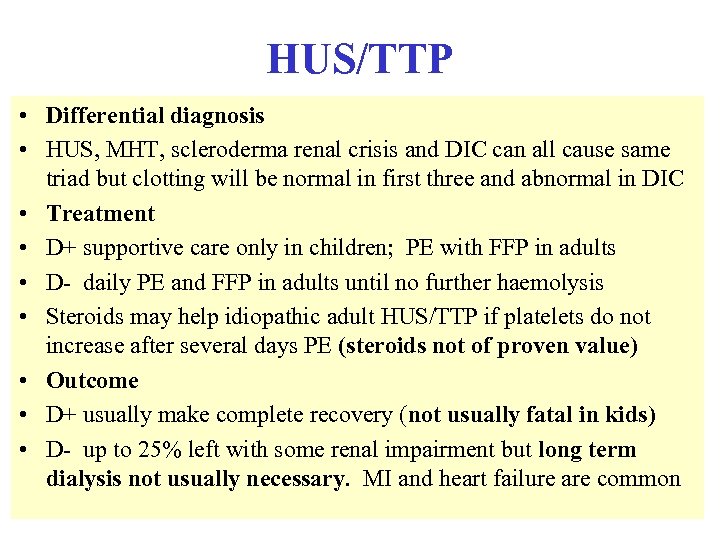 HUS/TTP • Differential diagnosis • HUS, MHT, scleroderma renal crisis and DIC can all cause same triad but clotting will be normal in first three and abnormal in DIC • Treatment • D+ supportive care only in children; PE with FFP in adults • D- daily PE and FFP in adults until no further haemolysis • Steroids may help idiopathic adult HUS/TTP if platelets do not increase after several days PE (steroids not of proven value) • Outcome • D+ usually make complete recovery (not usually fatal in kids) • D- up to 25% left with some renal impairment but long term dialysis not usually necessary. MI and heart failure are common
HUS/TTP • Differential diagnosis • HUS, MHT, scleroderma renal crisis and DIC can all cause same triad but clotting will be normal in first three and abnormal in DIC • Treatment • D+ supportive care only in children; PE with FFP in adults • D- daily PE and FFP in adults until no further haemolysis • Steroids may help idiopathic adult HUS/TTP if platelets do not increase after several days PE (steroids not of proven value) • Outcome • D+ usually make complete recovery (not usually fatal in kids) • D- up to 25% left with some renal impairment but long term dialysis not usually necessary. MI and heart failure are common

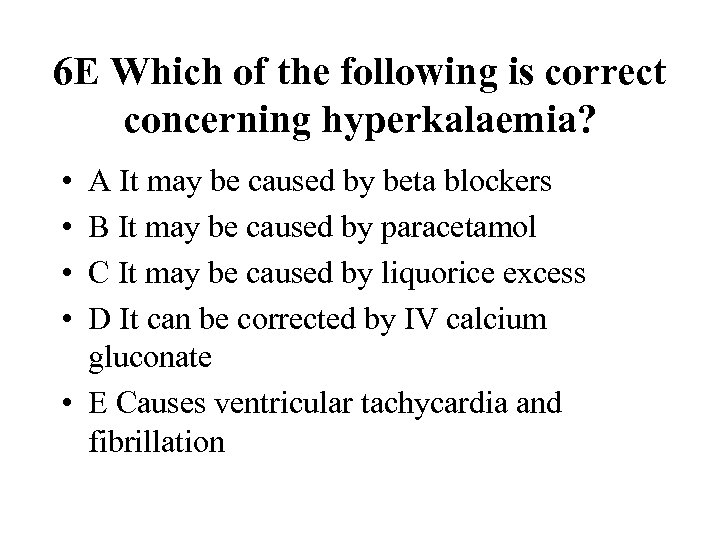 6 E Which of the following is correct concerning hyperkalaemia? • • A It may be caused by beta blockers B It may be caused by paracetamol C It may be caused by liquorice excess D It can be corrected by IV calcium gluconate • E Causes ventricular tachycardia and fibrillation
6 E Which of the following is correct concerning hyperkalaemia? • • A It may be caused by beta blockers B It may be caused by paracetamol C It may be caused by liquorice excess D It can be corrected by IV calcium gluconate • E Causes ventricular tachycardia and fibrillation
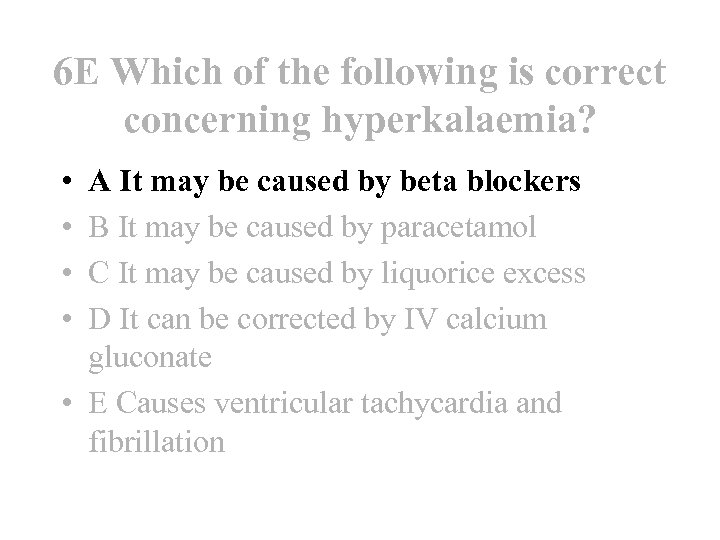 6 E Which of the following is correct concerning hyperkalaemia? • • A It may be caused by beta blockers B It may be caused by paracetamol C It may be caused by liquorice excess D It can be corrected by IV calcium gluconate • E Causes ventricular tachycardia and fibrillation
6 E Which of the following is correct concerning hyperkalaemia? • • A It may be caused by beta blockers B It may be caused by paracetamol C It may be caused by liquorice excess D It can be corrected by IV calcium gluconate • E Causes ventricular tachycardia and fibrillation
 Hyperkalaemia • Aetiology • Main causes begin with A - ARF, Addisons, Acidosis, Artefact, ACEI, ARBs, Aldosterone antagonists, anti-inflammatories eg NSAIDs, also beta blockers but not paracetamol (no effect) or liquorice (hypokalaemic alkalosis) • Presentation • Peaked T waves followed by loss of P wave, broadening of QRS complex (may mimic LBBB) then bradycardia leading to asystole or VF (but not VT) • Management • Depends on level of K, likelihood it will rise further (always more dangerous in ARF than CRF) and ECG changes
Hyperkalaemia • Aetiology • Main causes begin with A - ARF, Addisons, Acidosis, Artefact, ACEI, ARBs, Aldosterone antagonists, anti-inflammatories eg NSAIDs, also beta blockers but not paracetamol (no effect) or liquorice (hypokalaemic alkalosis) • Presentation • Peaked T waves followed by loss of P wave, broadening of QRS complex (may mimic LBBB) then bradycardia leading to asystole or VF (but not VT) • Management • Depends on level of K, likelihood it will rise further (always more dangerous in ARF than CRF) and ECG changes
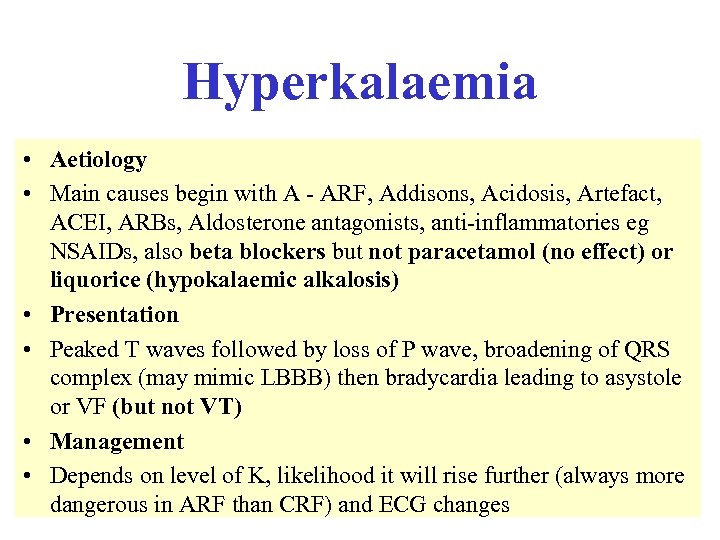
 Treatment of hyperkalaemia in acute renal failure Reduce risk of asystole Calcium Chloride/ Gluconate Drive K+ into cells Insulin/dextrose Beta agonists Sodium bicarbonate Remove K+ from body Dialysis Resonium
Treatment of hyperkalaemia in acute renal failure Reduce risk of asystole Calcium Chloride/ Gluconate Drive K+ into cells Insulin/dextrose Beta agonists Sodium bicarbonate Remove K+ from body Dialysis Resonium

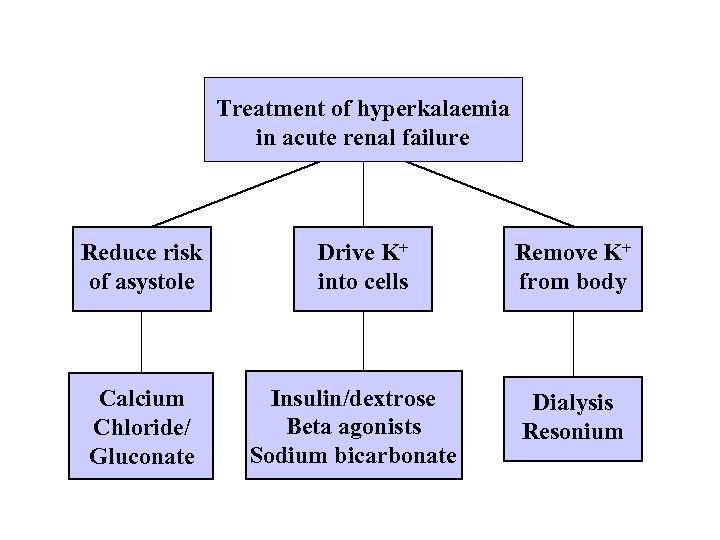
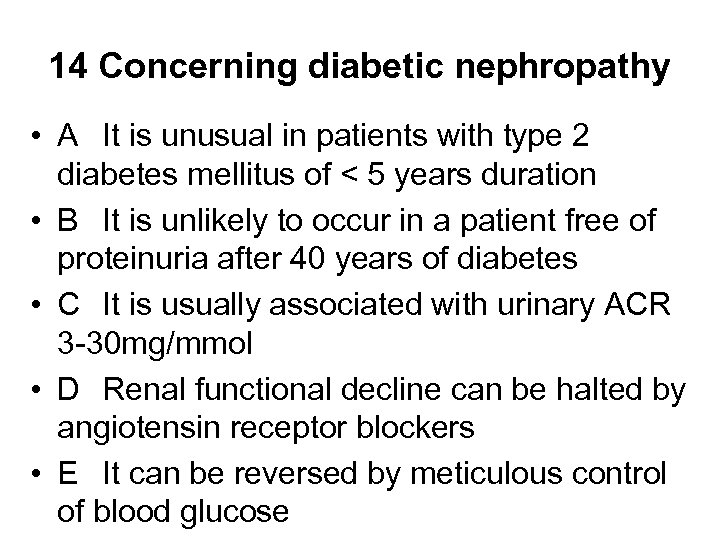 14 Concerning diabetic nephropathy • A It is unusual in patients with type 2 diabetes mellitus of < 5 years duration • B It is unlikely to occur in a patient free of proteinuria after 40 years of diabetes • C It is usually associated with urinary ACR 3 -30 mg/mmol • D Renal functional decline can be halted by angiotensin receptor blockers • E It can be reversed by meticulous control of blood glucose
14 Concerning diabetic nephropathy • A It is unusual in patients with type 2 diabetes mellitus of < 5 years duration • B It is unlikely to occur in a patient free of proteinuria after 40 years of diabetes • C It is usually associated with urinary ACR 3 -30 mg/mmol • D Renal functional decline can be halted by angiotensin receptor blockers • E It can be reversed by meticulous control of blood glucose
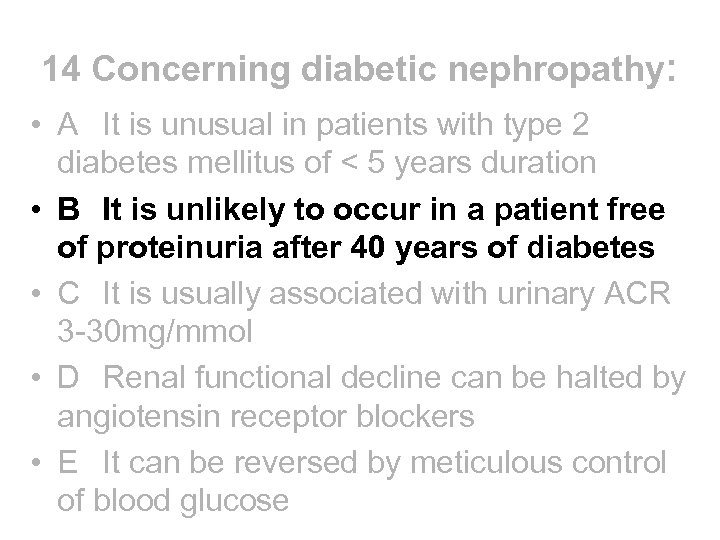 14 Concerning diabetic nephropathy: • A It is unusual in patients with type 2 diabetes mellitus of < 5 years duration • B It is unlikely to occur in a patient free of proteinuria after 40 years of diabetes • C It is usually associated with urinary ACR 3 -30 mg/mmol • D Renal functional decline can be halted by angiotensin receptor blockers • E It can be reversed by meticulous control of blood glucose
14 Concerning diabetic nephropathy: • A It is unusual in patients with type 2 diabetes mellitus of < 5 years duration • B It is unlikely to occur in a patient free of proteinuria after 40 years of diabetes • C It is usually associated with urinary ACR 3 -30 mg/mmol • D Renal functional decline can be halted by angiotensin receptor blockers • E It can be reversed by meticulous control of blood glucose
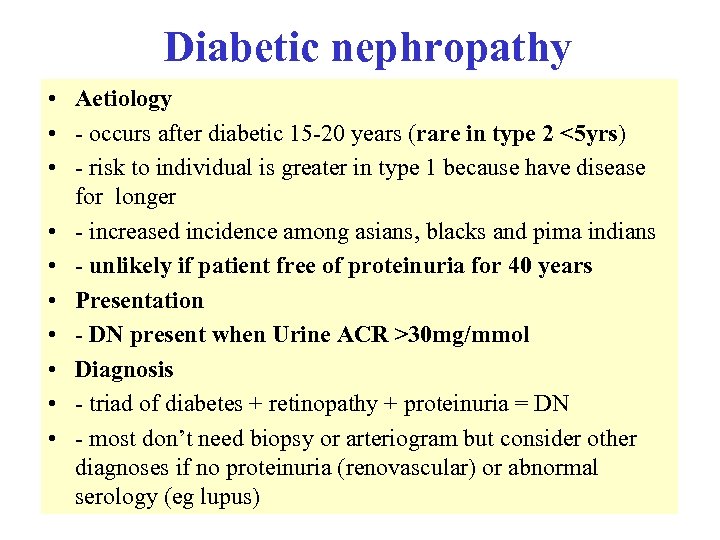 Diabetic nephropathy • Aetiology • - occurs after diabetic 15 -20 years (rare in type 2 <5 yrs) • - risk to individual is greater in type 1 because have disease for longer • - increased incidence among asians, blacks and pima indians • - unlikely if patient free of proteinuria for 40 years • Presentation • - DN present when Urine ACR >30 mg/mmol • Diagnosis • - triad of diabetes + retinopathy + proteinuria = DN • - most don’t need biopsy or arteriogram but consider other diagnoses if no proteinuria (renovascular) or abnormal serology (eg lupus)
Diabetic nephropathy • Aetiology • - occurs after diabetic 15 -20 years (rare in type 2 <5 yrs) • - risk to individual is greater in type 1 because have disease for longer • - increased incidence among asians, blacks and pima indians • - unlikely if patient free of proteinuria for 40 years • Presentation • - DN present when Urine ACR >30 mg/mmol • Diagnosis • - triad of diabetes + retinopathy + proteinuria = DN • - most don’t need biopsy or arteriogram but consider other diagnoses if no proteinuria (renovascular) or abnormal serology (eg lupus)
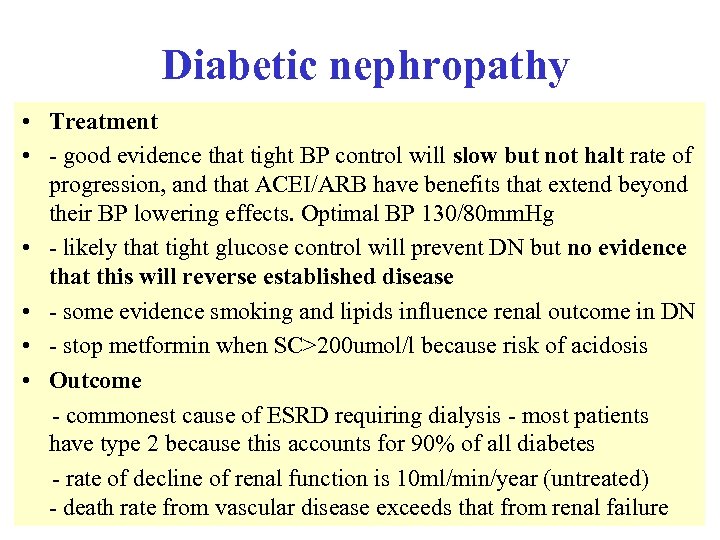 Diabetic nephropathy • Treatment • - good evidence that tight BP control will slow but not halt rate of progression, and that ACEI/ARB have benefits that extend beyond their BP lowering effects. Optimal BP 130/80 mm. Hg • - likely that tight glucose control will prevent DN but no evidence that this will reverse established disease • - some evidence smoking and lipids influence renal outcome in DN • - stop metformin when SC>200 umol/l because risk of acidosis • Outcome - commonest cause of ESRD requiring dialysis - most patients have type 2 because this accounts for 90% of all diabetes - rate of decline of renal function is 10 ml/min/year (untreated) - death rate from vascular disease exceeds that from renal failure
Diabetic nephropathy • Treatment • - good evidence that tight BP control will slow but not halt rate of progression, and that ACEI/ARB have benefits that extend beyond their BP lowering effects. Optimal BP 130/80 mm. Hg • - likely that tight glucose control will prevent DN but no evidence that this will reverse established disease • - some evidence smoking and lipids influence renal outcome in DN • - stop metformin when SC>200 umol/l because risk of acidosis • Outcome - commonest cause of ESRD requiring dialysis - most patients have type 2 because this accounts for 90% of all diabetes - rate of decline of renal function is 10 ml/min/year (untreated) - death rate from vascular disease exceeds that from renal failure
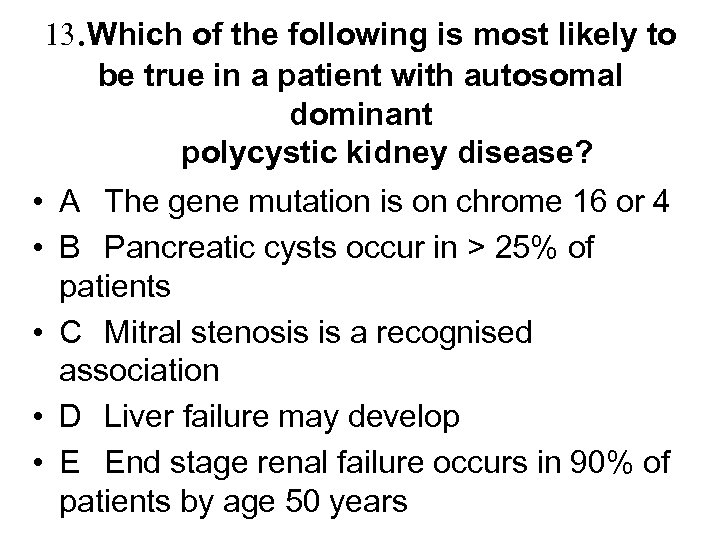 13. Which of the following is most likely to be true in a patient with autosomal dominant polycystic kidney disease? • A The gene mutation is on chrome 16 or 4 • B Pancreatic cysts occur in > 25% of patients • C Mitral stenosis is a recognised association • D Liver failure may develop • E End stage renal failure occurs in 90% of patients by age 50 years
13. Which of the following is most likely to be true in a patient with autosomal dominant polycystic kidney disease? • A The gene mutation is on chrome 16 or 4 • B Pancreatic cysts occur in > 25% of patients • C Mitral stenosis is a recognised association • D Liver failure may develop • E End stage renal failure occurs in 90% of patients by age 50 years
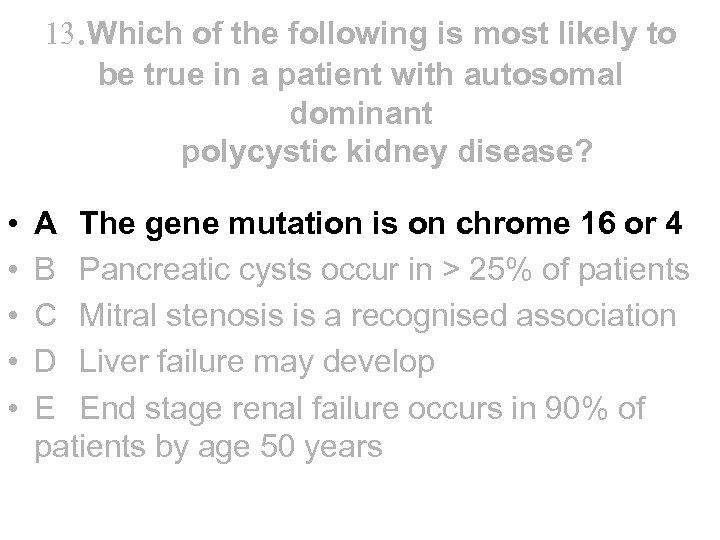 13. Which of the following is most likely to be true in a patient with autosomal dominant polycystic kidney disease? • • • A The gene mutation is on chrome 16 or 4 B Pancreatic cysts occur in > 25% of patients C Mitral stenosis is a recognised association D Liver failure may develop E End stage renal failure occurs in 90% of patients by age 50 years
13. Which of the following is most likely to be true in a patient with autosomal dominant polycystic kidney disease? • • • A The gene mutation is on chrome 16 or 4 B Pancreatic cysts occur in > 25% of patients C Mitral stenosis is a recognised association D Liver failure may develop E End stage renal failure occurs in 90% of patients by age 50 years
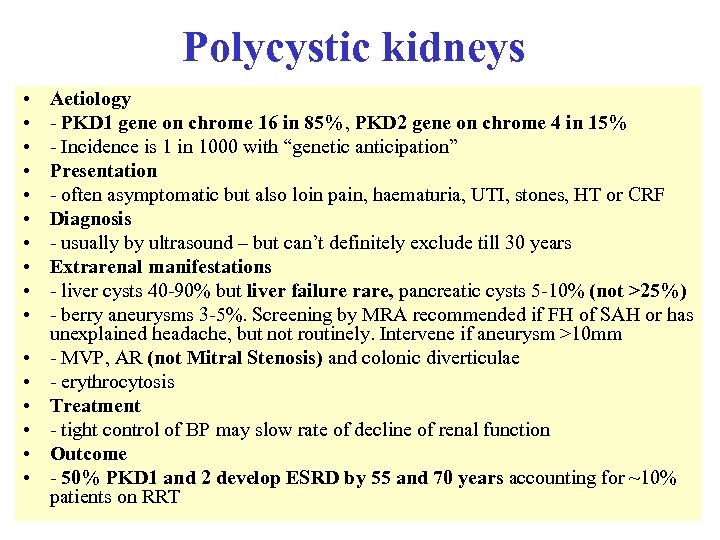 Polycystic kidneys • • • • Aetiology - PKD 1 gene on chrome 16 in 85%, PKD 2 gene on chrome 4 in 15% - Incidence is 1 in 1000 with “genetic anticipation” Presentation - often asymptomatic but also loin pain, haematuria, UTI, stones, HT or CRF Diagnosis - usually by ultrasound – but can’t definitely exclude till 30 years Extrarenal manifestations - liver cysts 40 -90% but liver failure rare, pancreatic cysts 5 -10% (not >25%) - berry aneurysms 3 -5%. Screening by MRA recommended if FH of SAH or has unexplained headache, but not routinely. Intervene if aneurysm >10 mm - MVP, AR (not Mitral Stenosis) and colonic diverticulae - erythrocytosis Treatment - tight control of BP may slow rate of decline of renal function Outcome - 50% PKD 1 and 2 develop ESRD by 55 and 70 years accounting for ~10% patients on RRT
Polycystic kidneys • • • • Aetiology - PKD 1 gene on chrome 16 in 85%, PKD 2 gene on chrome 4 in 15% - Incidence is 1 in 1000 with “genetic anticipation” Presentation - often asymptomatic but also loin pain, haematuria, UTI, stones, HT or CRF Diagnosis - usually by ultrasound – but can’t definitely exclude till 30 years Extrarenal manifestations - liver cysts 40 -90% but liver failure rare, pancreatic cysts 5 -10% (not >25%) - berry aneurysms 3 -5%. Screening by MRA recommended if FH of SAH or has unexplained headache, but not routinely. Intervene if aneurysm >10 mm - MVP, AR (not Mitral Stenosis) and colonic diverticulae - erythrocytosis Treatment - tight control of BP may slow rate of decline of renal function Outcome - 50% PKD 1 and 2 develop ESRD by 55 and 70 years accounting for ~10% patients on RRT
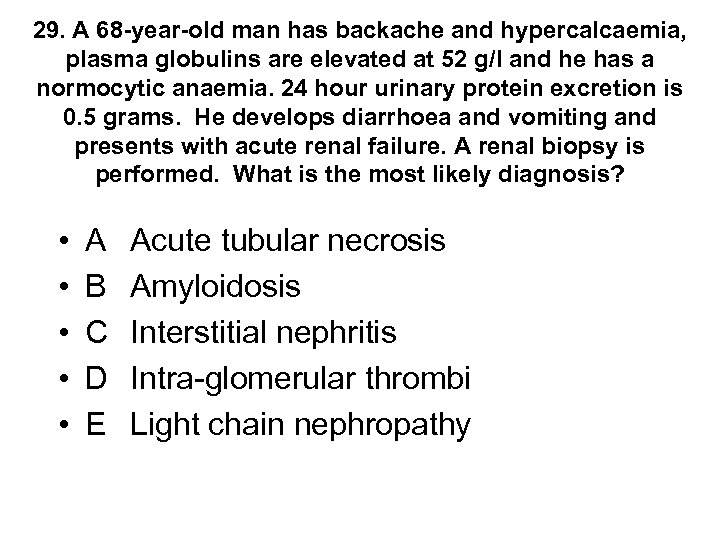 29. A 68 -year-old man has backache and hypercalcaemia, plasma globulins are elevated at 52 g/l and he has a normocytic anaemia. 24 hour urinary protein excretion is 0. 5 grams. He develops diarrhoea and vomiting and presents with acute renal failure. A renal biopsy is performed. What is the most likely diagnosis? • • • A B C D E Acute tubular necrosis Amyloidosis Interstitial nephritis Intra-glomerular thrombi Light chain nephropathy
29. A 68 -year-old man has backache and hypercalcaemia, plasma globulins are elevated at 52 g/l and he has a normocytic anaemia. 24 hour urinary protein excretion is 0. 5 grams. He develops diarrhoea and vomiting and presents with acute renal failure. A renal biopsy is performed. What is the most likely diagnosis? • • • A B C D E Acute tubular necrosis Amyloidosis Interstitial nephritis Intra-glomerular thrombi Light chain nephropathy
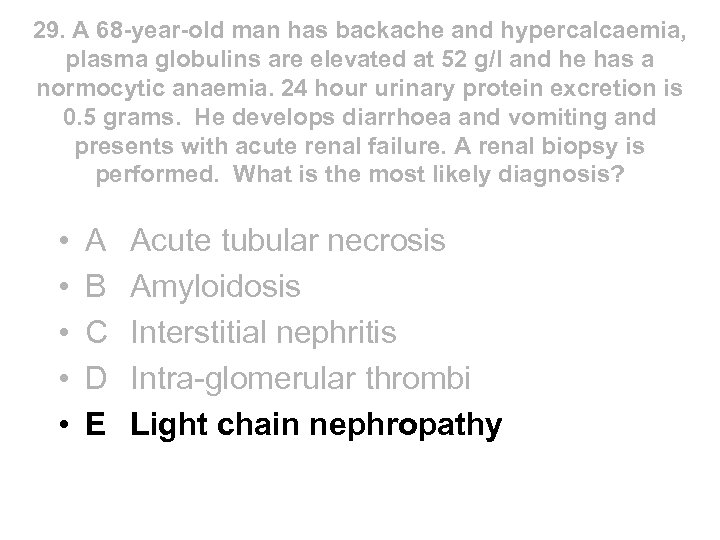 29. A 68 -year-old man has backache and hypercalcaemia, plasma globulins are elevated at 52 g/l and he has a normocytic anaemia. 24 hour urinary protein excretion is 0. 5 grams. He develops diarrhoea and vomiting and presents with acute renal failure. A renal biopsy is performed. What is the most likely diagnosis? • • • A B C D E Acute tubular necrosis Amyloidosis Interstitial nephritis Intra-glomerular thrombi Light chain nephropathy
29. A 68 -year-old man has backache and hypercalcaemia, plasma globulins are elevated at 52 g/l and he has a normocytic anaemia. 24 hour urinary protein excretion is 0. 5 grams. He develops diarrhoea and vomiting and presents with acute renal failure. A renal biopsy is performed. What is the most likely diagnosis? • • • A B C D E Acute tubular necrosis Amyloidosis Interstitial nephritis Intra-glomerular thrombi Light chain nephropathy
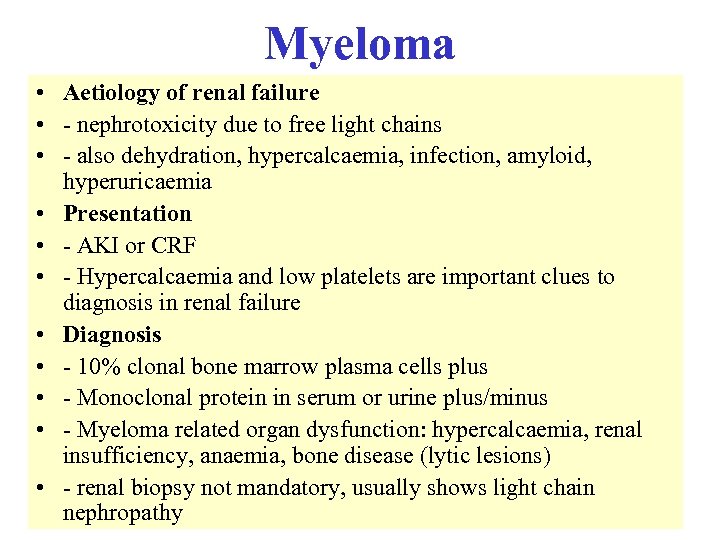 Myeloma • Aetiology of renal failure • - nephrotoxicity due to free light chains • - also dehydration, hypercalcaemia, infection, amyloid, hyperuricaemia • Presentation • - AKI or CRF • - Hypercalcaemia and low platelets are important clues to diagnosis in renal failure • Diagnosis • - 10% clonal bone marrow plasma cells plus • - Monoclonal protein in serum or urine plus/minus • - Myeloma related organ dysfunction: hypercalcaemia, renal insufficiency, anaemia, bone disease (lytic lesions) • - renal biopsy not mandatory, usually shows light chain nephropathy
Myeloma • Aetiology of renal failure • - nephrotoxicity due to free light chains • - also dehydration, hypercalcaemia, infection, amyloid, hyperuricaemia • Presentation • - AKI or CRF • - Hypercalcaemia and low platelets are important clues to diagnosis in renal failure • Diagnosis • - 10% clonal bone marrow plasma cells plus • - Monoclonal protein in serum or urine plus/minus • - Myeloma related organ dysfunction: hypercalcaemia, renal insufficiency, anaemia, bone disease (lytic lesions) • - renal biopsy not mandatory, usually shows light chain nephropathy
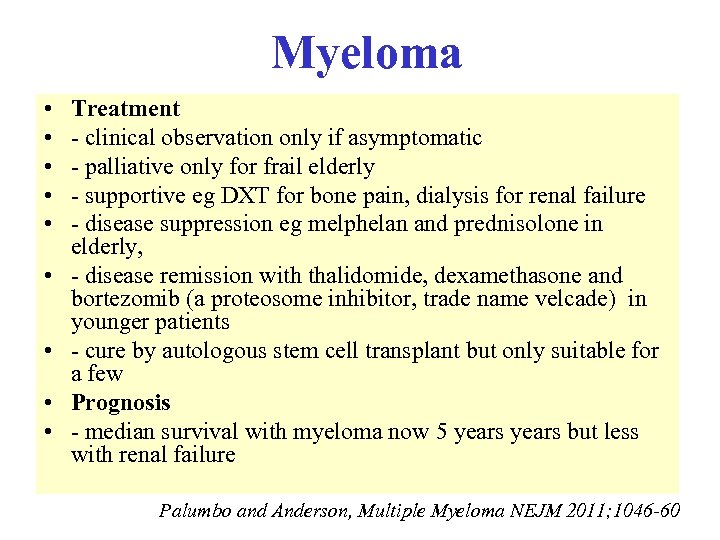 Myeloma • • • Treatment - clinical observation only if asymptomatic - palliative only for frail elderly - supportive eg DXT for bone pain, dialysis for renal failure - disease suppression eg melphelan and prednisolone in elderly, - disease remission with thalidomide, dexamethasone and bortezomib (a proteosome inhibitor, trade name velcade) in younger patients - cure by autologous stem cell transplant but only suitable for a few Prognosis - median survival with myeloma now 5 years but less with renal failure Palumbo and Anderson, Multiple Myeloma NEJM 2011; 1046 -60
Myeloma • • • Treatment - clinical observation only if asymptomatic - palliative only for frail elderly - supportive eg DXT for bone pain, dialysis for renal failure - disease suppression eg melphelan and prednisolone in elderly, - disease remission with thalidomide, dexamethasone and bortezomib (a proteosome inhibitor, trade name velcade) in younger patients - cure by autologous stem cell transplant but only suitable for a few Prognosis - median survival with myeloma now 5 years but less with renal failure Palumbo and Anderson, Multiple Myeloma NEJM 2011; 1046 -60

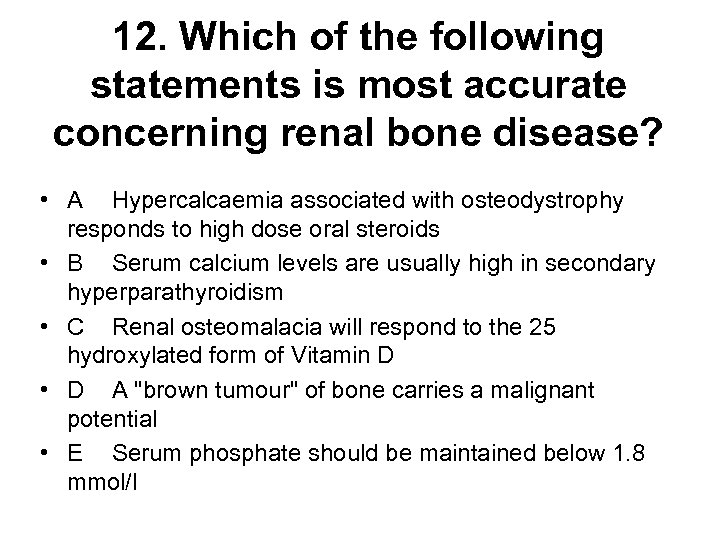 12. Which of the following statements is most accurate concerning renal bone disease? • A Hypercalcaemia associated with osteodystrophy responds to high dose oral steroids • B Serum calcium levels are usually high in secondary hyperparathyroidism • C Renal osteomalacia will respond to the 25 hydroxylated form of Vitamin D • D A "brown tumour" of bone carries a malignant potential • E Serum phosphate should be maintained below 1. 8 mmol/l
12. Which of the following statements is most accurate concerning renal bone disease? • A Hypercalcaemia associated with osteodystrophy responds to high dose oral steroids • B Serum calcium levels are usually high in secondary hyperparathyroidism • C Renal osteomalacia will respond to the 25 hydroxylated form of Vitamin D • D A "brown tumour" of bone carries a malignant potential • E Serum phosphate should be maintained below 1. 8 mmol/l
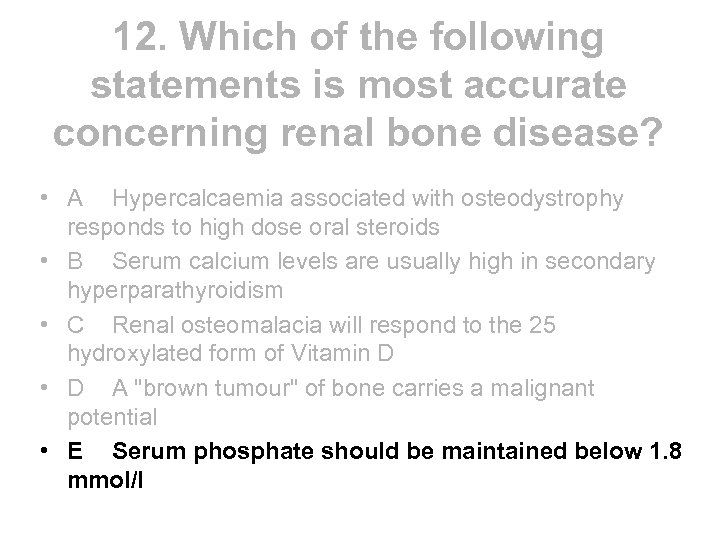 12. Which of the following statements is most accurate concerning renal bone disease? • A Hypercalcaemia associated with osteodystrophy responds to high dose oral steroids • B Serum calcium levels are usually high in secondary hyperparathyroidism • C Renal osteomalacia will respond to the 25 hydroxylated form of Vitamin D • D A "brown tumour" of bone carries a malignant potential • E Serum phosphate should be maintained below 1. 8 mmol/l
12. Which of the following statements is most accurate concerning renal bone disease? • A Hypercalcaemia associated with osteodystrophy responds to high dose oral steroids • B Serum calcium levels are usually high in secondary hyperparathyroidism • C Renal osteomalacia will respond to the 25 hydroxylated form of Vitamin D • D A "brown tumour" of bone carries a malignant potential • E Serum phosphate should be maintained below 1. 8 mmol/l
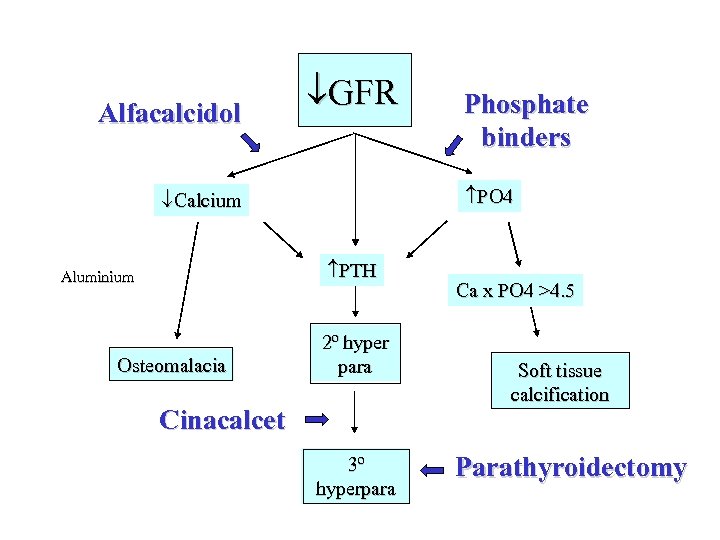
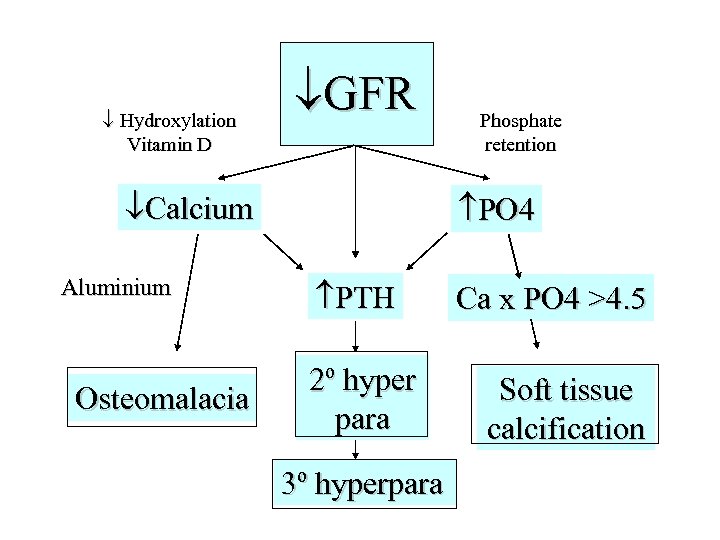 Hydroxylation Vitamin D GFR Calcium Aluminium Osteomalacia Phosphate retention PO 4 PTH 2º hyper para 3º hyperpara Ca x PO 4 >4. 5 Soft tissue calcification
Hydroxylation Vitamin D GFR Calcium Aluminium Osteomalacia Phosphate retention PO 4 PTH 2º hyper para 3º hyperpara Ca x PO 4 >4. 5 Soft tissue calcification
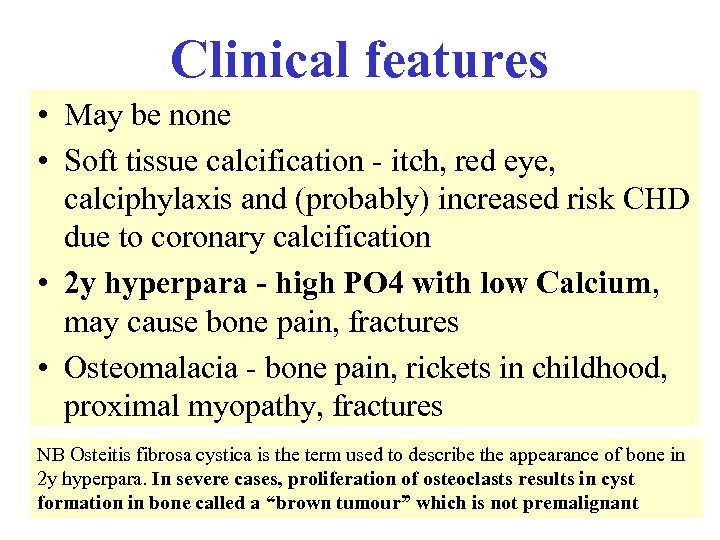 Clinical features • May be none • Soft tissue calcification - itch, red eye, calciphylaxis and (probably) increased risk CHD due to coronary calcification • 2 y hyperpara - high PO 4 with low Calcium, may cause bone pain, fractures • Osteomalacia - bone pain, rickets in childhood, proximal myopathy, fractures NB Osteitis fibrosa cystica is the term used to describe the appearance of bone in 2 y hyperpara. In severe cases, proliferation of osteoclasts results in cyst formation in bone called a “brown tumour” which is not premalignant
Clinical features • May be none • Soft tissue calcification - itch, red eye, calciphylaxis and (probably) increased risk CHD due to coronary calcification • 2 y hyperpara - high PO 4 with low Calcium, may cause bone pain, fractures • Osteomalacia - bone pain, rickets in childhood, proximal myopathy, fractures NB Osteitis fibrosa cystica is the term used to describe the appearance of bone in 2 y hyperpara. In severe cases, proliferation of osteoclasts results in cyst formation in bone called a “brown tumour” which is not premalignant
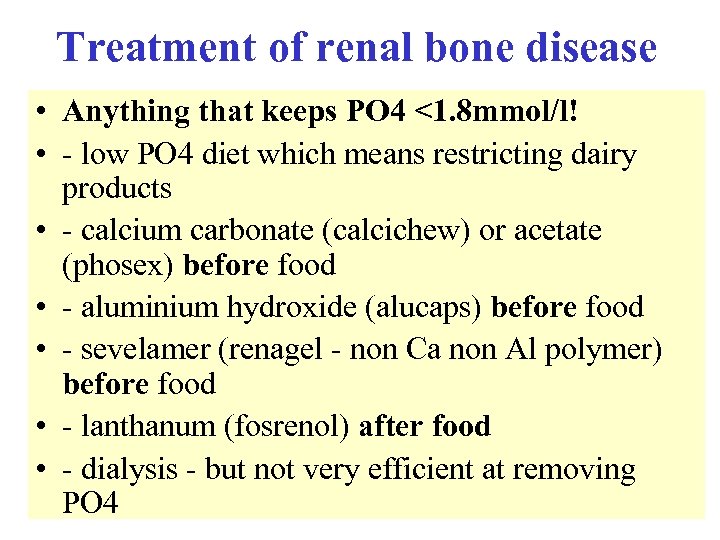 Treatment of renal bone disease • Anything that keeps PO 4 <1. 8 mmol/l! • - low PO 4 diet which means restricting dairy products • - calcium carbonate (calcichew) or acetate (phosex) before food • - aluminium hydroxide (alucaps) before food • - sevelamer (renagel - non Ca non Al polymer) before food • - lanthanum (fosrenol) after food • - dialysis - but not very efficient at removing PO 4
Treatment of renal bone disease • Anything that keeps PO 4 <1. 8 mmol/l! • - low PO 4 diet which means restricting dairy products • - calcium carbonate (calcichew) or acetate (phosex) before food • - aluminium hydroxide (alucaps) before food • - sevelamer (renagel - non Ca non Al polymer) before food • - lanthanum (fosrenol) after food • - dialysis - but not very efficient at removing PO 4
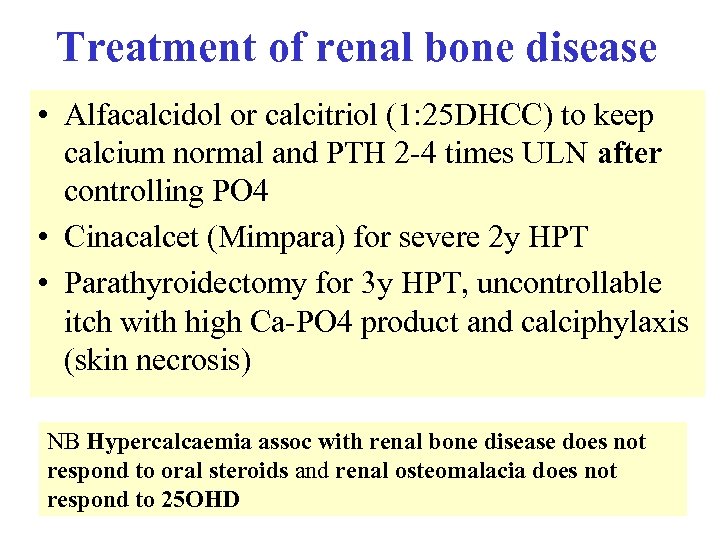 Treatment of renal bone disease • Alfacalcidol or calcitriol (1: 25 DHCC) to keep calcium normal and PTH 2 -4 times ULN after controlling PO 4 • Cinacalcet (Mimpara) for severe 2 y HPT • Parathyroidectomy for 3 y HPT, uncontrollable itch with high Ca-PO 4 product and calciphylaxis (skin necrosis) NB Hypercalcaemia assoc with renal bone disease does not respond to oral steroids and renal osteomalacia does not respond to 25 OHD
Treatment of renal bone disease • Alfacalcidol or calcitriol (1: 25 DHCC) to keep calcium normal and PTH 2 -4 times ULN after controlling PO 4 • Cinacalcet (Mimpara) for severe 2 y HPT • Parathyroidectomy for 3 y HPT, uncontrollable itch with high Ca-PO 4 product and calciphylaxis (skin necrosis) NB Hypercalcaemia assoc with renal bone disease does not respond to oral steroids and renal osteomalacia does not respond to 25 OHD
 Alfacalcidol GFR PO 4 Calcium PTH Aluminium Osteomalacia Phosphate binders 2º hyper para Cinacalcet 3º hyperpara Ca x PO 4 >4. 5 Soft tissue calcification Parathyroidectomy
Alfacalcidol GFR PO 4 Calcium PTH Aluminium Osteomalacia Phosphate binders 2º hyper para Cinacalcet 3º hyperpara Ca x PO 4 >4. 5 Soft tissue calcification Parathyroidectomy
 15 A 45 -year-old woman has a 10 week history of oedema. Serum albumin is 22 g/l, creatinine 98 µmol/l and 24 -hour urinary protein output 7. 3 gm. Which of the following is most applicable? • A A trial of steroids is justified before proceeding to renal biopsy • B A history of rheumatoid arthritis would be helpful for diagnosis • C Renal vein thrombosis is likely if the patient has diuretic-resistant oedema • D There is a low risk of progressive renal failure
15 A 45 -year-old woman has a 10 week history of oedema. Serum albumin is 22 g/l, creatinine 98 µmol/l and 24 -hour urinary protein output 7. 3 gm. Which of the following is most applicable? • A A trial of steroids is justified before proceeding to renal biopsy • B A history of rheumatoid arthritis would be helpful for diagnosis • C Renal vein thrombosis is likely if the patient has diuretic-resistant oedema • D There is a low risk of progressive renal failure
 15 A 45 -year-old woman has a 10 week history of oedema. Serum albumin is 22 g/l, creatinine 98 µmol/l and 24 -hour urinary protein output 7. 3 gm. Which of the following is most applicable? • A A trial of steroids is justified before proceeding to renal biopsy • B A history of rheumatoid arthritis would be helpful for diagnosis • C Renal vein thrombosis is likely if the patient has diuretic-resistant oedema • D There is a low risk of progressive renal failure
15 A 45 -year-old woman has a 10 week history of oedema. Serum albumin is 22 g/l, creatinine 98 µmol/l and 24 -hour urinary protein output 7. 3 gm. Which of the following is most applicable? • A A trial of steroids is justified before proceeding to renal biopsy • B A history of rheumatoid arthritis would be helpful for diagnosis • C Renal vein thrombosis is likely if the patient has diuretic-resistant oedema • D There is a low risk of progressive renal failure
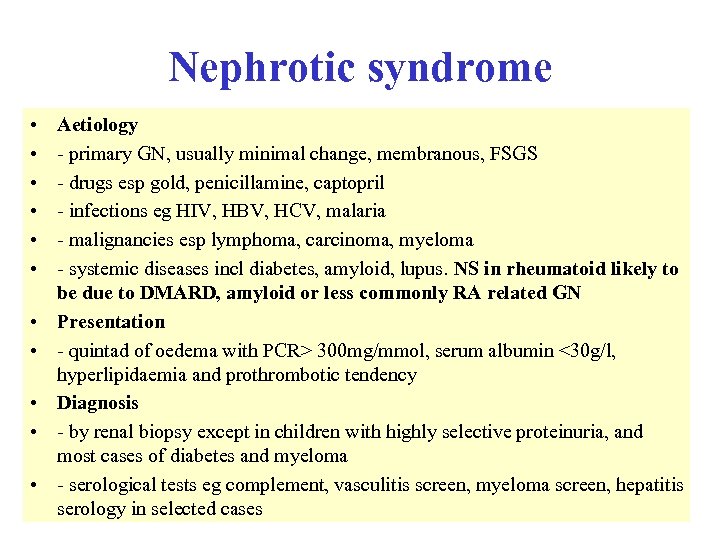 Nephrotic syndrome • • • Aetiology - primary GN, usually minimal change, membranous, FSGS - drugs esp gold, penicillamine, captopril - infections eg HIV, HBV, HCV, malaria - malignancies esp lymphoma, carcinoma, myeloma - systemic diseases incl diabetes, amyloid, lupus. NS in rheumatoid likely to be due to DMARD, amyloid or less commonly RA related GN Presentation - quintad of oedema with PCR> 300 mg/mmol, serum albumin <30 g/l, hyperlipidaemia and prothrombotic tendency Diagnosis - by renal biopsy except in children with highly selective proteinuria, and most cases of diabetes and myeloma - serological tests eg complement, vasculitis screen, myeloma screen, hepatitis serology in selected cases
Nephrotic syndrome • • • Aetiology - primary GN, usually minimal change, membranous, FSGS - drugs esp gold, penicillamine, captopril - infections eg HIV, HBV, HCV, malaria - malignancies esp lymphoma, carcinoma, myeloma - systemic diseases incl diabetes, amyloid, lupus. NS in rheumatoid likely to be due to DMARD, amyloid or less commonly RA related GN Presentation - quintad of oedema with PCR> 300 mg/mmol, serum albumin <30 g/l, hyperlipidaemia and prothrombotic tendency Diagnosis - by renal biopsy except in children with highly selective proteinuria, and most cases of diabetes and myeloma - serological tests eg complement, vasculitis screen, myeloma screen, hepatitis serology in selected cases
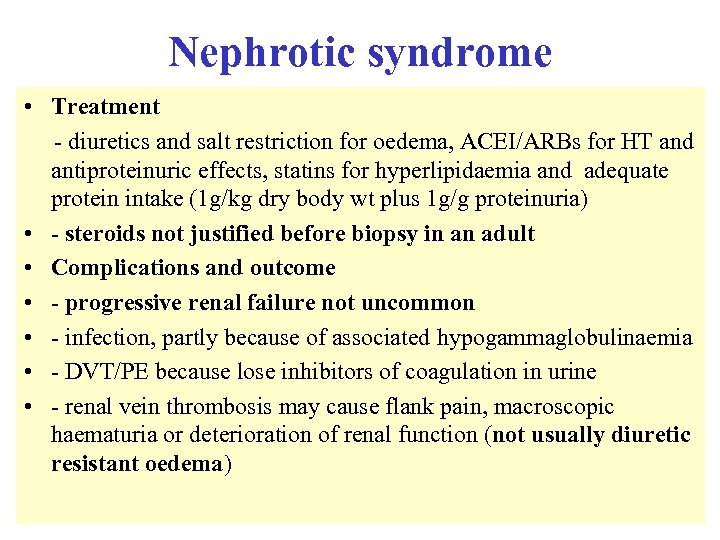 Nephrotic syndrome • Treatment - diuretics and salt restriction for oedema, ACEI/ARBs for HT and antiproteinuric effects, statins for hyperlipidaemia and adequate protein intake (1 g/kg dry body wt plus 1 g/g proteinuria) • - steroids not justified before biopsy in an adult • Complications and outcome • - progressive renal failure not uncommon • - infection, partly because of associated hypogammaglobulinaemia • - DVT/PE because lose inhibitors of coagulation in urine • - renal vein thrombosis may cause flank pain, macroscopic haematuria or deterioration of renal function (not usually diuretic resistant oedema)
Nephrotic syndrome • Treatment - diuretics and salt restriction for oedema, ACEI/ARBs for HT and antiproteinuric effects, statins for hyperlipidaemia and adequate protein intake (1 g/kg dry body wt plus 1 g/g proteinuria) • - steroids not justified before biopsy in an adult • Complications and outcome • - progressive renal failure not uncommon • - infection, partly because of associated hypogammaglobulinaemia • - DVT/PE because lose inhibitors of coagulation in urine • - renal vein thrombosis may cause flank pain, macroscopic haematuria or deterioration of renal function (not usually diuretic resistant oedema)
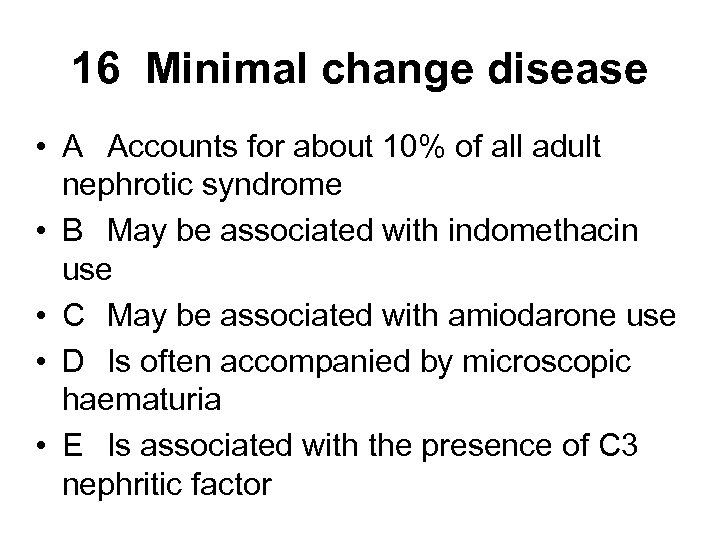 16 Minimal change disease • A Accounts for about 10% of all adult nephrotic syndrome • B May be associated with indomethacin use • C May be associated with amiodarone use • D Is often accompanied by microscopic haematuria • E Is associated with the presence of C 3 nephritic factor
16 Minimal change disease • A Accounts for about 10% of all adult nephrotic syndrome • B May be associated with indomethacin use • C May be associated with amiodarone use • D Is often accompanied by microscopic haematuria • E Is associated with the presence of C 3 nephritic factor
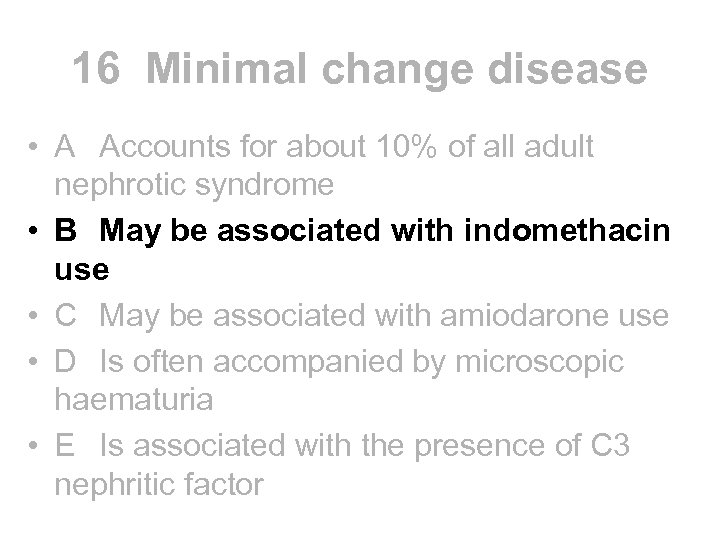 16 Minimal change disease • A Accounts for about 10% of all adult nephrotic syndrome • B May be associated with indomethacin use • C May be associated with amiodarone use • D Is often accompanied by microscopic haematuria • E Is associated with the presence of C 3 nephritic factor
16 Minimal change disease • A Accounts for about 10% of all adult nephrotic syndrome • B May be associated with indomethacin use • C May be associated with amiodarone use • D Is often accompanied by microscopic haematuria • E Is associated with the presence of C 3 nephritic factor
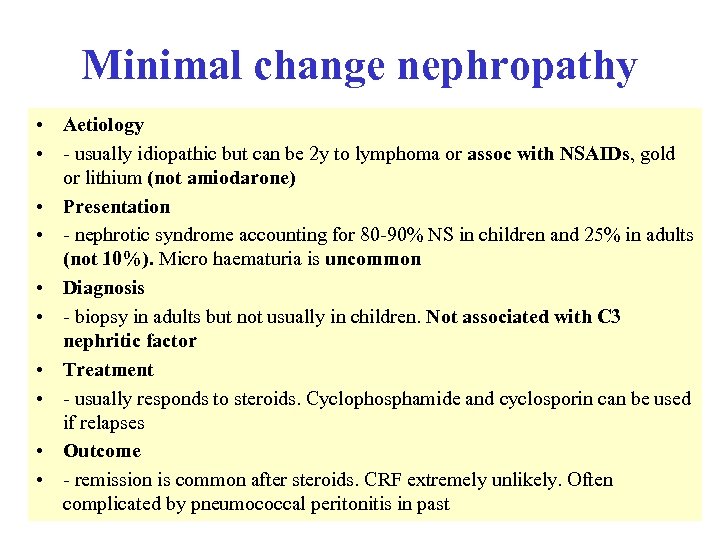 Minimal change nephropathy • Aetiology • - usually idiopathic but can be 2 y to lymphoma or assoc with NSAIDs, gold or lithium (not amiodarone) • Presentation • - nephrotic syndrome accounting for 80 -90% NS in children and 25% in adults (not 10%). Micro haematuria is uncommon • Diagnosis • - biopsy in adults but not usually in children. Not associated with C 3 nephritic factor • Treatment • - usually responds to steroids. Cyclophosphamide and cyclosporin can be used if relapses • Outcome • - remission is common after steroids. CRF extremely unlikely. Often complicated by pneumococcal peritonitis in past
Minimal change nephropathy • Aetiology • - usually idiopathic but can be 2 y to lymphoma or assoc with NSAIDs, gold or lithium (not amiodarone) • Presentation • - nephrotic syndrome accounting for 80 -90% NS in children and 25% in adults (not 10%). Micro haematuria is uncommon • Diagnosis • - biopsy in adults but not usually in children. Not associated with C 3 nephritic factor • Treatment • - usually responds to steroids. Cyclophosphamide and cyclosporin can be used if relapses • Outcome • - remission is common after steroids. CRF extremely unlikely. Often complicated by pneumococcal peritonitis in past
 17 Ig. A nephropathy • A Is the commonest primary GN leading to renal failure • B Leads to end stage renal failure in 50% of patients over 20 years • C Occurs more commonly among Europeans than Japanese • D Commonly presents with nephrotic syndrome • E May be histologically indistinguishable from Haemolytic Uraemic syndrome
17 Ig. A nephropathy • A Is the commonest primary GN leading to renal failure • B Leads to end stage renal failure in 50% of patients over 20 years • C Occurs more commonly among Europeans than Japanese • D Commonly presents with nephrotic syndrome • E May be histologically indistinguishable from Haemolytic Uraemic syndrome
 17 Ig. A nephropathy • A Is the commonest primary GN leading to renal failure • B Leads to end stage renal failure in 50% of patients over 20 years • C Occurs more commonly among Europeans than Japanese • D Commonly presents with nephrotic syndrome • E May be histologically indistinguishable from Haemolytic Uraemic syndrome
17 Ig. A nephropathy • A Is the commonest primary GN leading to renal failure • B Leads to end stage renal failure in 50% of patients over 20 years • C Occurs more commonly among Europeans than Japanese • D Commonly presents with nephrotic syndrome • E May be histologically indistinguishable from Haemolytic Uraemic syndrome
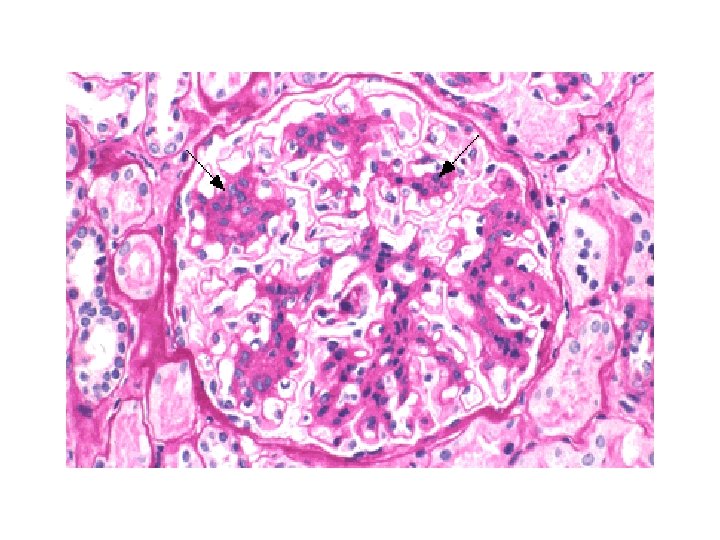
 Ig. A nephropathy • Aetiology • - commonest GN on renal biopsy, more common among japanese than europeans and can also run in families though mode of inheritance unclear • Presentation • - usually with micro or macro haematuria esp following URTI, but also with asymptomatic proteinuria, nephrotic syndrome (3%), CRF and occas as RPGN with crescentic nephritis • Diagnosis • - biopsy shows mesangial proliferation with deposition of Ig. A. identical to HSP (not HUS which shows intraglomerular thrombi) • Treatment • - control of HT, otherwise no specific therapy has been shown to alter progression to ESRD. No evidence that tonsillectomy helps • Outcome • - 10 -30% progress to ESRD over 20 years (the commonest primary GN leading to renal failure)
Ig. A nephropathy • Aetiology • - commonest GN on renal biopsy, more common among japanese than europeans and can also run in families though mode of inheritance unclear • Presentation • - usually with micro or macro haematuria esp following URTI, but also with asymptomatic proteinuria, nephrotic syndrome (3%), CRF and occas as RPGN with crescentic nephritis • Diagnosis • - biopsy shows mesangial proliferation with deposition of Ig. A. identical to HSP (not HUS which shows intraglomerular thrombi) • Treatment • - control of HT, otherwise no specific therapy has been shown to alter progression to ESRD. No evidence that tonsillectomy helps • Outcome • - 10 -30% progress to ESRD over 20 years (the commonest primary GN leading to renal failure)
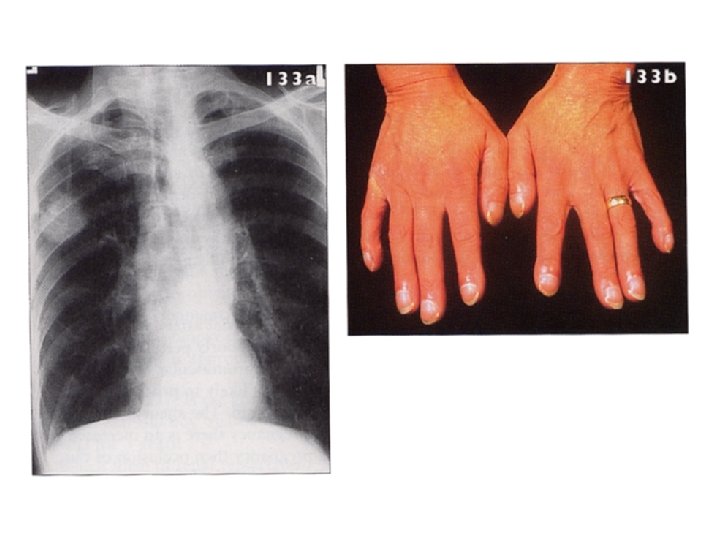
 4 extra Membranous nephropathy • A Is caused by deposition of an autoantibody to glomerular basement membrane • B Is associated with Familial lipodystrophy • C Should be treated with plasma exchange • D Leads to progressive renal failure in the majority of cases • E May be the first manifestation of lung cancer
4 extra Membranous nephropathy • A Is caused by deposition of an autoantibody to glomerular basement membrane • B Is associated with Familial lipodystrophy • C Should be treated with plasma exchange • D Leads to progressive renal failure in the majority of cases • E May be the first manifestation of lung cancer
 4 extra Membranous nephropathy • A Is caused by deposition of an autoantibody to glomerular basement membrane • B Is associated with Familial lipodystrophy • C Should be treated with plasma exchange • D Leads to progressive renal failure in the majority of cases • E May be the first manifestation of lung cancer
4 extra Membranous nephropathy • A Is caused by deposition of an autoantibody to glomerular basement membrane • B Is associated with Familial lipodystrophy • C Should be treated with plasma exchange • D Leads to progressive renal failure in the majority of cases • E May be the first manifestation of lung cancer
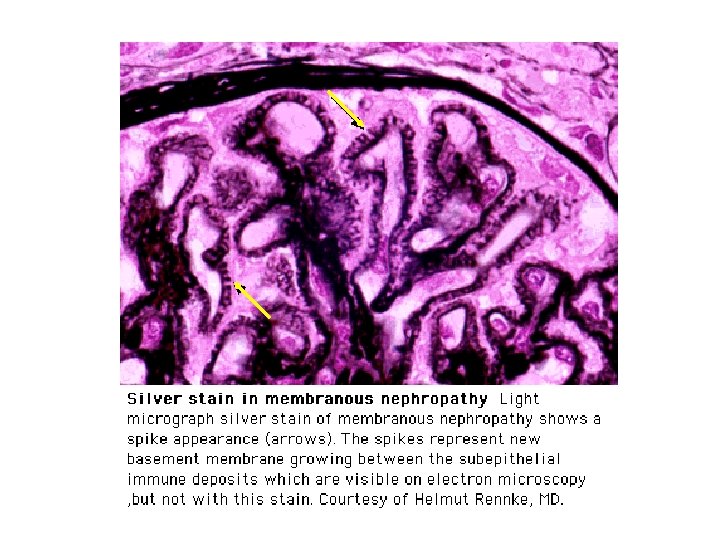
 Membranous nephropathy • Aetiology • - usually idiopathic but can be 2 y to drugs, SLE and malignancy in up to 20% cases. Should consider lung, colon and breast cancer in elderly patients • Presentation • - asymptomatic proteinuria or nephrotic syndrome. (MCGN type 2 not membranous is associated with partial lipodystrophy) • Diagnosis • - LM shows uniform thickening of GBM, EM subepithelial humps and IF granular deposition of Ig. G along GBM. Humps are Ag/Ab complexes in the GBM. Their origin is not known. The Ab is not directed at the GBM itself • Treatment • - supportive only unless progressive decline in function (MRC trial) • - no evidence for plasma exchange • Outcome • - 33% stay the same, 33% get better and only 33% develop progressive renal failure
Membranous nephropathy • Aetiology • - usually idiopathic but can be 2 y to drugs, SLE and malignancy in up to 20% cases. Should consider lung, colon and breast cancer in elderly patients • Presentation • - asymptomatic proteinuria or nephrotic syndrome. (MCGN type 2 not membranous is associated with partial lipodystrophy) • Diagnosis • - LM shows uniform thickening of GBM, EM subepithelial humps and IF granular deposition of Ig. G along GBM. Humps are Ag/Ab complexes in the GBM. Their origin is not known. The Ab is not directed at the GBM itself • Treatment • - supportive only unless progressive decline in function (MRC trial) • - no evidence for plasma exchange • Outcome • - 33% stay the same, 33% get better and only 33% develop progressive renal failure
 23. Which of the following parameters indicates the poorest prognosis in a patient with acute Wegener’s granulomatosis? • A 100% active crescents on renal biopsy • B c. ANCA positivity • C Extrarenal vasculitis • D Female sex • E Acute renal failure requiring dialysis
23. Which of the following parameters indicates the poorest prognosis in a patient with acute Wegener’s granulomatosis? • A 100% active crescents on renal biopsy • B c. ANCA positivity • C Extrarenal vasculitis • D Female sex • E Acute renal failure requiring dialysis
 23. Which of the following parameters indicates the poorest prognosis in a patient with acute Wegener’s granulomatosis? • A 100% active crescents on renal biopsy • B c. ANCA positivity • C Extrarenal vasculitis • D Female sex • E Acute renal failure requiring dialysis
23. Which of the following parameters indicates the poorest prognosis in a patient with acute Wegener’s granulomatosis? • A 100% active crescents on renal biopsy • B c. ANCA positivity • C Extrarenal vasculitis • D Female sex • E Acute renal failure requiring dialysis
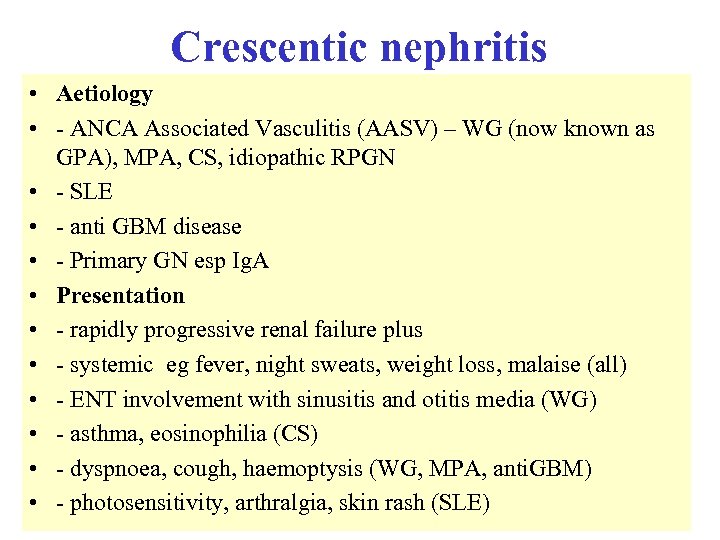 Crescentic nephritis • Aetiology • - ANCA Associated Vasculitis (AASV) – WG (now known as GPA), MPA, CS, idiopathic RPGN • - SLE • - anti GBM disease • - Primary GN esp Ig. A • Presentation • - rapidly progressive renal failure plus • - systemic eg fever, night sweats, weight loss, malaise (all) • - ENT involvement with sinusitis and otitis media (WG) • - asthma, eosinophilia (CS) • - dyspnoea, cough, haemoptysis (WG, MPA, anti. GBM) • - photosensitivity, arthralgia, skin rash (SLE)
Crescentic nephritis • Aetiology • - ANCA Associated Vasculitis (AASV) – WG (now known as GPA), MPA, CS, idiopathic RPGN • - SLE • - anti GBM disease • - Primary GN esp Ig. A • Presentation • - rapidly progressive renal failure plus • - systemic eg fever, night sweats, weight loss, malaise (all) • - ENT involvement with sinusitis and otitis media (WG) • - asthma, eosinophilia (CS) • - dyspnoea, cough, haemoptysis (WG, MPA, anti. GBM) • - photosensitivity, arthralgia, skin rash (SLE)
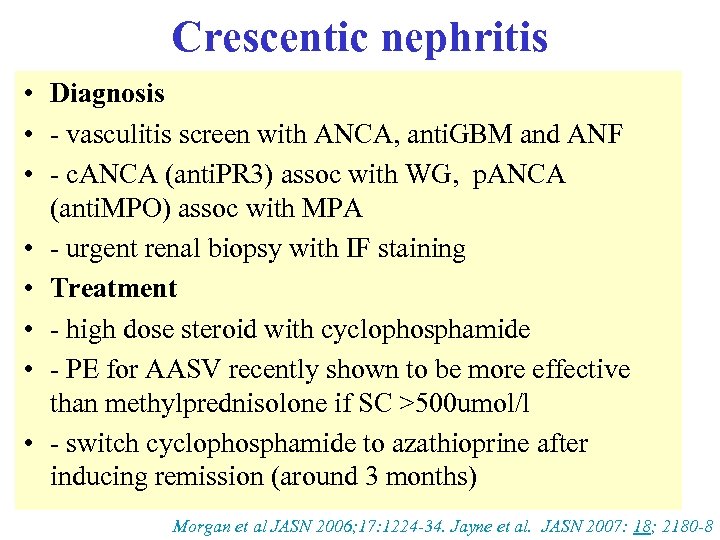 Crescentic nephritis • Diagnosis • - vasculitis screen with ANCA, anti. GBM and ANF • - c. ANCA (anti. PR 3) assoc with WG, p. ANCA (anti. MPO) assoc with MPA • - urgent renal biopsy with IF staining • Treatment • - high dose steroid with cyclophosphamide • - PE for AASV recently shown to be more effective than methylprednisolone if SC >500 umol/l • - switch cyclophosphamide to azathioprine after inducing remission (around 3 months) Morgan et al JASN 2006; 17: 1224 -34. Jayne et al. JASN 2007: 18; 2180 -8
Crescentic nephritis • Diagnosis • - vasculitis screen with ANCA, anti. GBM and ANF • - c. ANCA (anti. PR 3) assoc with WG, p. ANCA (anti. MPO) assoc with MPA • - urgent renal biopsy with IF staining • Treatment • - high dose steroid with cyclophosphamide • - PE for AASV recently shown to be more effective than methylprednisolone if SC >500 umol/l • - switch cyclophosphamide to azathioprine after inducing remission (around 3 months) Morgan et al JASN 2006; 17: 1224 -34. Jayne et al. JASN 2007: 18; 2180 -8
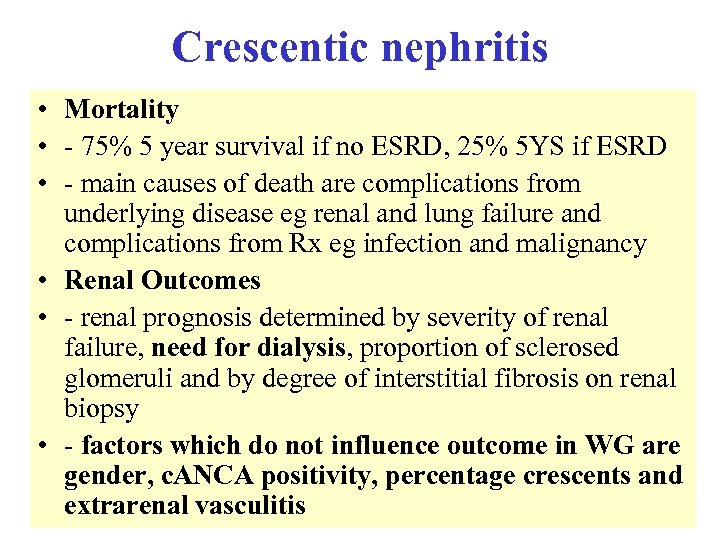 Crescentic nephritis • Mortality • - 75% 5 year survival if no ESRD, 25% 5 YS if ESRD • - main causes of death are complications from underlying disease eg renal and lung failure and complications from Rx eg infection and malignancy • Renal Outcomes • - renal prognosis determined by severity of renal failure, need for dialysis, proportion of sclerosed glomeruli and by degree of interstitial fibrosis on renal biopsy • - factors which do not influence outcome in WG are gender, c. ANCA positivity, percentage crescents and extrarenal vasculitis
Crescentic nephritis • Mortality • - 75% 5 year survival if no ESRD, 25% 5 YS if ESRD • - main causes of death are complications from underlying disease eg renal and lung failure and complications from Rx eg infection and malignancy • Renal Outcomes • - renal prognosis determined by severity of renal failure, need for dialysis, proportion of sclerosed glomeruli and by degree of interstitial fibrosis on renal biopsy • - factors which do not influence outcome in WG are gender, c. ANCA positivity, percentage crescents and extrarenal vasculitis
 22. A 32 -year-old woman complaining of painful hands is found to have hypertension, proteinuria and dipstick haematuria. Plasma creatinine is 147 µmol/l. Renal biopsy shows proliferative glomerulonephritis with occasional cellular crescents. Immuno-fluorescence shows diffuse granular staining for Ig. A, Ig. G, Ig. M, C 3 and C 4. What is the diagnosis? • • • A B C D E Ig. A nephropathy lupus Membranous Minimal change Systemic vasculitis
22. A 32 -year-old woman complaining of painful hands is found to have hypertension, proteinuria and dipstick haematuria. Plasma creatinine is 147 µmol/l. Renal biopsy shows proliferative glomerulonephritis with occasional cellular crescents. Immuno-fluorescence shows diffuse granular staining for Ig. A, Ig. G, Ig. M, C 3 and C 4. What is the diagnosis? • • • A B C D E Ig. A nephropathy lupus Membranous Minimal change Systemic vasculitis
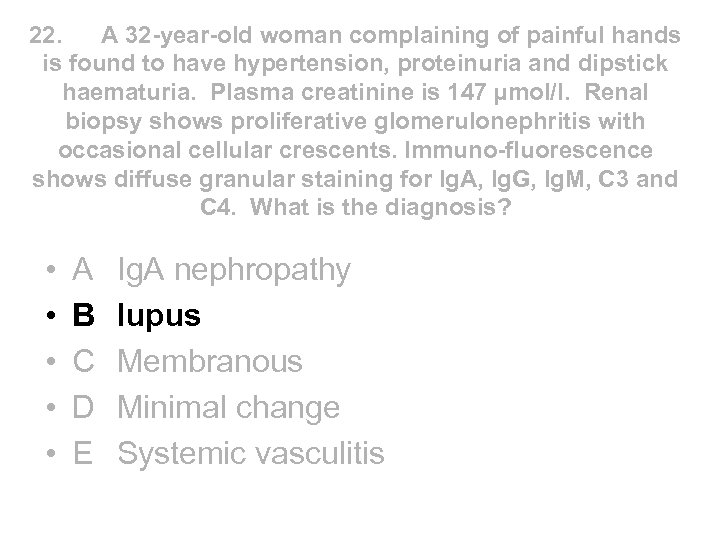 22. A 32 -year-old woman complaining of painful hands is found to have hypertension, proteinuria and dipstick haematuria. Plasma creatinine is 147 µmol/l. Renal biopsy shows proliferative glomerulonephritis with occasional cellular crescents. Immuno-fluorescence shows diffuse granular staining for Ig. A, Ig. G, Ig. M, C 3 and C 4. What is the diagnosis? • • • A B C D E Ig. A nephropathy lupus Membranous Minimal change Systemic vasculitis
22. A 32 -year-old woman complaining of painful hands is found to have hypertension, proteinuria and dipstick haematuria. Plasma creatinine is 147 µmol/l. Renal biopsy shows proliferative glomerulonephritis with occasional cellular crescents. Immuno-fluorescence shows diffuse granular staining for Ig. A, Ig. G, Ig. M, C 3 and C 4. What is the diagnosis? • • • A B C D E Ig. A nephropathy lupus Membranous Minimal change Systemic vasculitis
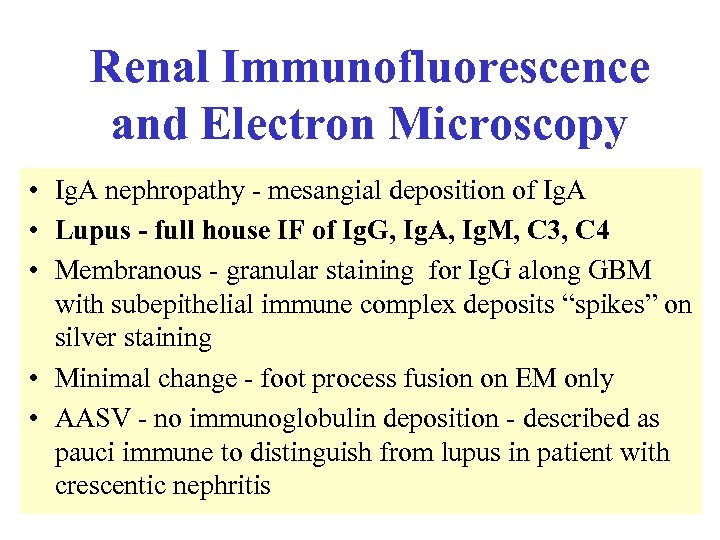 Renal Immunofluorescence and Electron Microscopy • Ig. A nephropathy - mesangial deposition of Ig. A • Lupus - full house IF of Ig. G, Ig. A, Ig. M, C 3, C 4 • Membranous - granular staining for Ig. G along GBM with subepithelial immune complex deposits “spikes” on silver staining • Minimal change - foot process fusion on EM only • AASV - no immunoglobulin deposition - described as pauci immune to distinguish from lupus in patient with crescentic nephritis
Renal Immunofluorescence and Electron Microscopy • Ig. A nephropathy - mesangial deposition of Ig. A • Lupus - full house IF of Ig. G, Ig. A, Ig. M, C 3, C 4 • Membranous - granular staining for Ig. G along GBM with subepithelial immune complex deposits “spikes” on silver staining • Minimal change - foot process fusion on EM only • AASV - no immunoglobulin deposition - described as pauci immune to distinguish from lupus in patient with crescentic nephritis
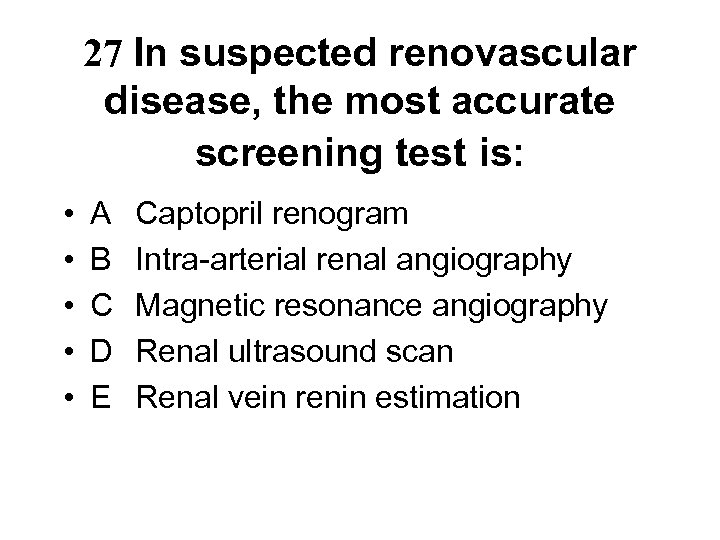 27 In suspected renovascular disease, the most accurate screening test is: • • • A B C D E Captopril renogram Intra-arterial renal angiography Magnetic resonance angiography Renal ultrasound scan Renal vein renin estimation
27 In suspected renovascular disease, the most accurate screening test is: • • • A B C D E Captopril renogram Intra-arterial renal angiography Magnetic resonance angiography Renal ultrasound scan Renal vein renin estimation
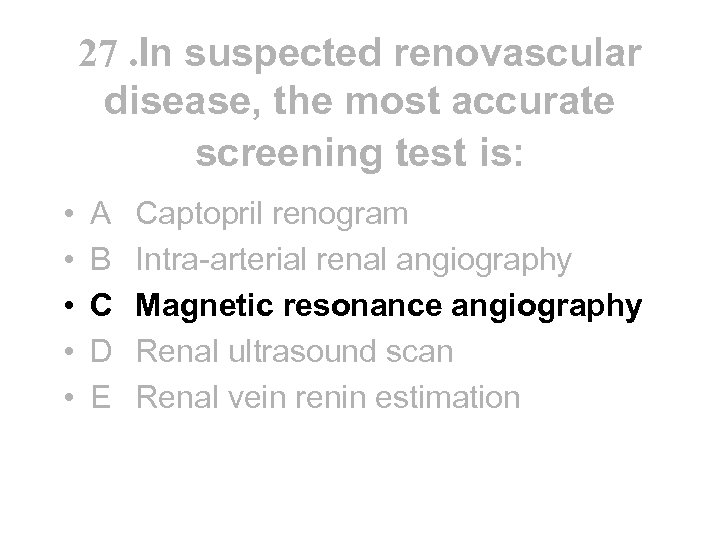 27. In suspected renovascular disease, the most accurate screening test is: • • • A B C D E Captopril renogram Intra-arterial renal angiography Magnetic resonance angiography Renal ultrasound scan Renal vein renin estimation
27. In suspected renovascular disease, the most accurate screening test is: • • • A B C D E Captopril renogram Intra-arterial renal angiography Magnetic resonance angiography Renal ultrasound scan Renal vein renin estimation
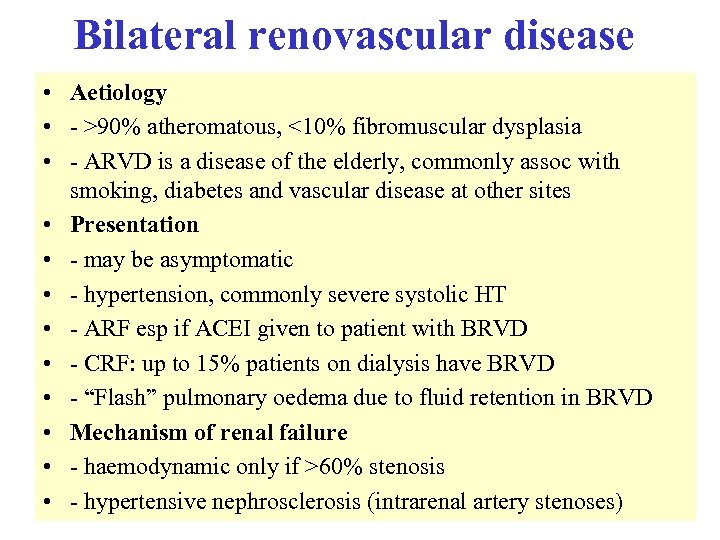 Bilateral renovascular disease • Aetiology • - >90% atheromatous, <10% fibromuscular dysplasia • - ARVD is a disease of the elderly, commonly assoc with smoking, diabetes and vascular disease at other sites • Presentation • - may be asymptomatic • - hypertension, commonly severe systolic HT • - ARF esp if ACEI given to patient with BRVD • - CRF: up to 15% patients on dialysis have BRVD • - “Flash” pulmonary oedema due to fluid retention in BRVD • Mechanism of renal failure • - haemodynamic only if >60% stenosis • - hypertensive nephrosclerosis (intrarenal artery stenoses)
Bilateral renovascular disease • Aetiology • - >90% atheromatous, <10% fibromuscular dysplasia • - ARVD is a disease of the elderly, commonly assoc with smoking, diabetes and vascular disease at other sites • Presentation • - may be asymptomatic • - hypertension, commonly severe systolic HT • - ARF esp if ACEI given to patient with BRVD • - CRF: up to 15% patients on dialysis have BRVD • - “Flash” pulmonary oedema due to fluid retention in BRVD • Mechanism of renal failure • - haemodynamic only if >60% stenosis • - hypertensive nephrosclerosis (intrarenal artery stenoses)
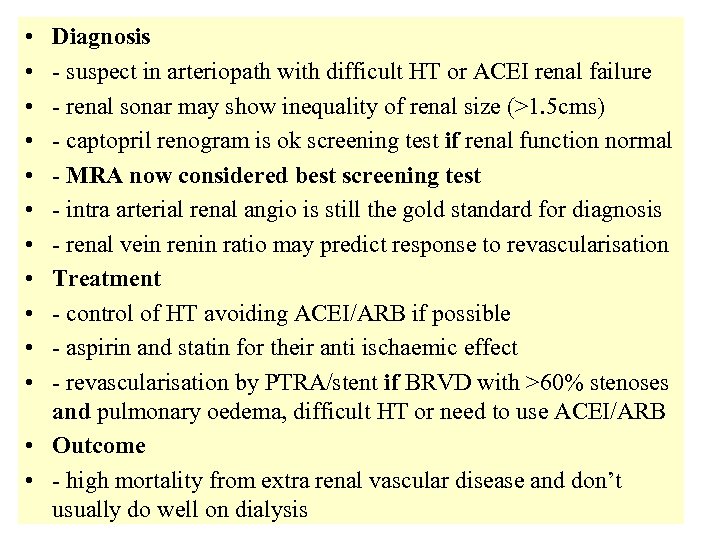 • • • Diagnosis - suspect in arteriopath with difficult HT or ACEI renal failure - renal sonar may show inequality of renal size (>1. 5 cms) - captopril renogram is ok screening test if renal function normal - MRA now considered best screening test - intra arterial renal angio is still the gold standard for diagnosis - renal vein renin ratio may predict response to revascularisation Treatment - control of HT avoiding ACEI/ARB if possible - aspirin and statin for their anti ischaemic effect - revascularisation by PTRA/stent if BRVD with >60% stenoses and pulmonary oedema, difficult HT or need to use ACEI/ARB • Outcome • - high mortality from extra renal vascular disease and don’t usually do well on dialysis
• • • Diagnosis - suspect in arteriopath with difficult HT or ACEI renal failure - renal sonar may show inequality of renal size (>1. 5 cms) - captopril renogram is ok screening test if renal function normal - MRA now considered best screening test - intra arterial renal angio is still the gold standard for diagnosis - renal vein renin ratio may predict response to revascularisation Treatment - control of HT avoiding ACEI/ARB if possible - aspirin and statin for their anti ischaemic effect - revascularisation by PTRA/stent if BRVD with >60% stenoses and pulmonary oedema, difficult HT or need to use ACEI/ARB • Outcome • - high mortality from extra renal vascular disease and don’t usually do well on dialysis
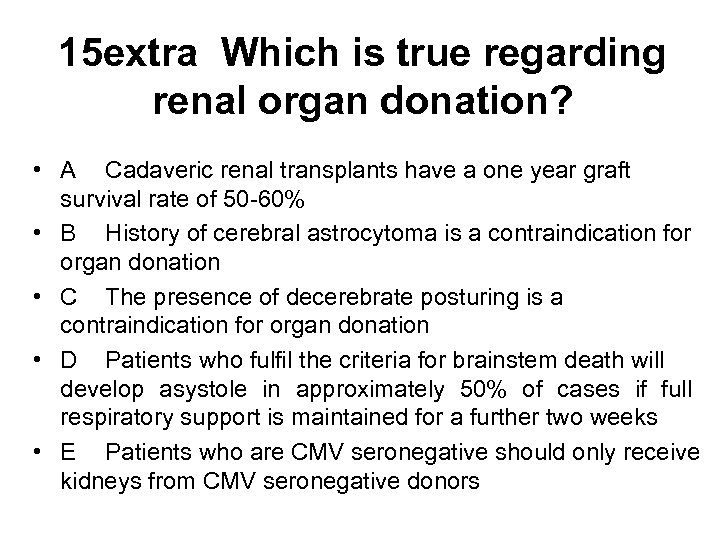 15 extra Which is true regarding renal organ donation? • A Cadaveric renal transplants have a one year graft survival rate of 50 -60% • B History of cerebral astrocytoma is a contraindication for organ donation • C The presence of decerebrate posturing is a contraindication for organ donation • D Patients who fulfil the criteria for brainstem death will develop asystole in approximately 50% of cases if full respiratory support is maintained for a further two weeks • E Patients who are CMV seronegative should only receive kidneys from CMV seronegative donors
15 extra Which is true regarding renal organ donation? • A Cadaveric renal transplants have a one year graft survival rate of 50 -60% • B History of cerebral astrocytoma is a contraindication for organ donation • C The presence of decerebrate posturing is a contraindication for organ donation • D Patients who fulfil the criteria for brainstem death will develop asystole in approximately 50% of cases if full respiratory support is maintained for a further two weeks • E Patients who are CMV seronegative should only receive kidneys from CMV seronegative donors
 15 extra Which is true regarding renal organ donation? • A Cadaveric renal transplants have a one year graft survival rate of 50 -60% • B History of cerebral astrocytoma is a contraindication for organ donation • C The presence of decerebrate posturing is a contraindication for organ donation • D Patients who fulfil the criteria for brainstem death will develop asystole in approximately 50% of cases if full respiratory support is maintained for a further two weeks • E Patients who are CMV seronegative should only receive kidneys from CMV seronegative donors
15 extra Which is true regarding renal organ donation? • A Cadaveric renal transplants have a one year graft survival rate of 50 -60% • B History of cerebral astrocytoma is a contraindication for organ donation • C The presence of decerebrate posturing is a contraindication for organ donation • D Patients who fulfil the criteria for brainstem death will develop asystole in approximately 50% of cases if full respiratory support is maintained for a further two weeks • E Patients who are CMV seronegative should only receive kidneys from CMV seronegative donors
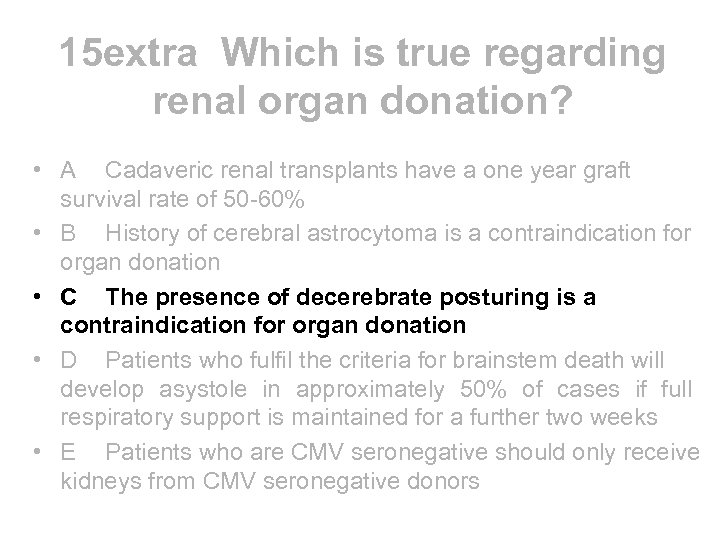
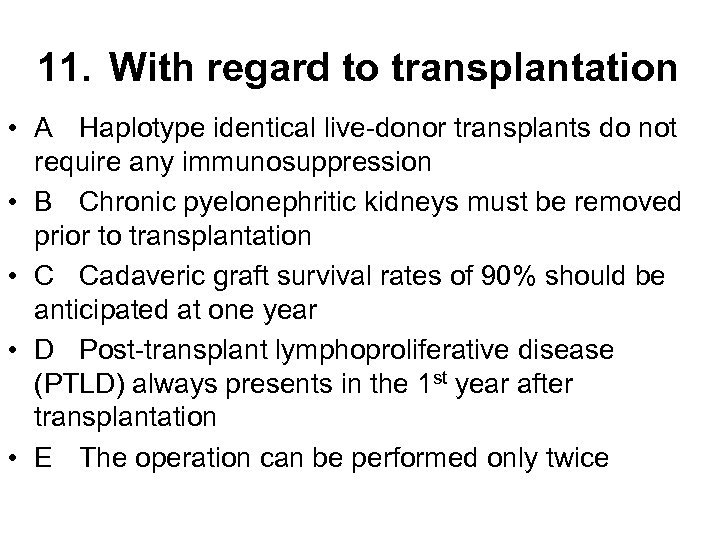 11. With regard to transplantation • A Haplotype identical live-donor transplants do not require any immunosuppression • B Chronic pyelonephritic kidneys must be removed prior to transplantation • C Cadaveric graft survival rates of 90% should be anticipated at one year • D Post-transplant lymphoproliferative disease (PTLD) always presents in the 1 st year after transplantation • E The operation can be performed only twice
11. With regard to transplantation • A Haplotype identical live-donor transplants do not require any immunosuppression • B Chronic pyelonephritic kidneys must be removed prior to transplantation • C Cadaveric graft survival rates of 90% should be anticipated at one year • D Post-transplant lymphoproliferative disease (PTLD) always presents in the 1 st year after transplantation • E The operation can be performed only twice
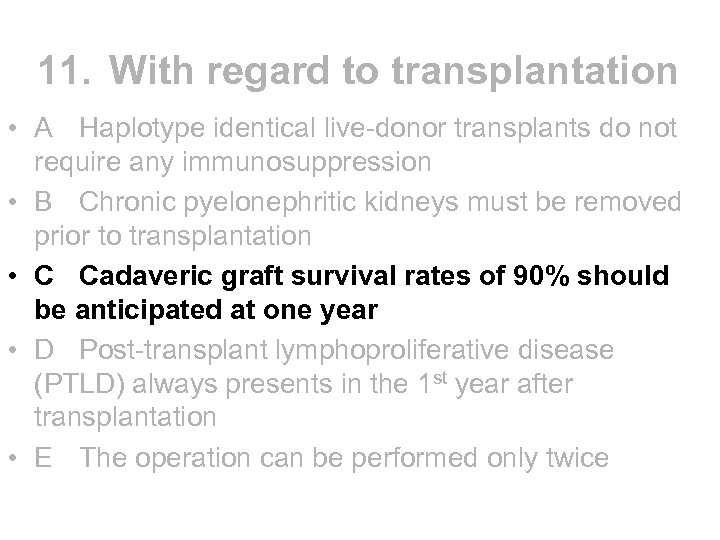 11. With regard to transplantation • A Haplotype identical live-donor transplants do not require any immunosuppression • B Chronic pyelonephritic kidneys must be removed prior to transplantation • C Cadaveric graft survival rates of 90% should be anticipated at one year • D Post-transplant lymphoproliferative disease (PTLD) always presents in the 1 st year after transplantation • E The operation can be performed only twice
11. With regard to transplantation • A Haplotype identical live-donor transplants do not require any immunosuppression • B Chronic pyelonephritic kidneys must be removed prior to transplantation • C Cadaveric graft survival rates of 90% should be anticipated at one year • D Post-transplant lymphoproliferative disease (PTLD) always presents in the 1 st year after transplantation • E The operation can be performed only twice
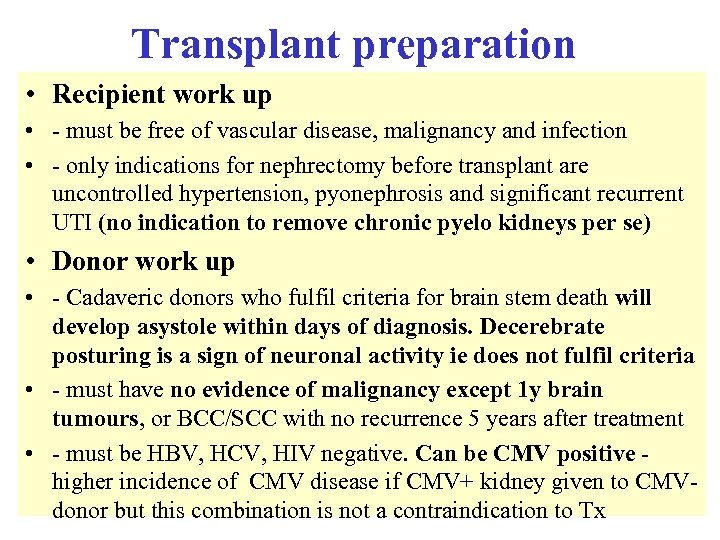 Transplant preparation • Recipient work up • - must be free of vascular disease, malignancy and infection • - only indications for nephrectomy before transplant are uncontrolled hypertension, pyonephrosis and significant recurrent UTI (no indication to remove chronic pyelo kidneys per se) • Donor work up • - Cadaveric donors who fulfil criteria for brain stem death will develop asystole within days of diagnosis. Decerebrate posturing is a sign of neuronal activity ie does not fulfil criteria • - must have no evidence of malignancy except 1 y brain tumours, or BCC/SCC with no recurrence 5 years after treatment • - must be HBV, HCV, HIV negative. Can be CMV positive higher incidence of CMV disease if CMV+ kidney given to CMVdonor but this combination is not a contraindication to Tx
Transplant preparation • Recipient work up • - must be free of vascular disease, malignancy and infection • - only indications for nephrectomy before transplant are uncontrolled hypertension, pyonephrosis and significant recurrent UTI (no indication to remove chronic pyelo kidneys per se) • Donor work up • - Cadaveric donors who fulfil criteria for brain stem death will develop asystole within days of diagnosis. Decerebrate posturing is a sign of neuronal activity ie does not fulfil criteria • - must have no evidence of malignancy except 1 y brain tumours, or BCC/SCC with no recurrence 5 years after treatment • - must be HBV, HCV, HIV negative. Can be CMV positive higher incidence of CMV disease if CMV+ kidney given to CMVdonor but this combination is not a contraindication to Tx
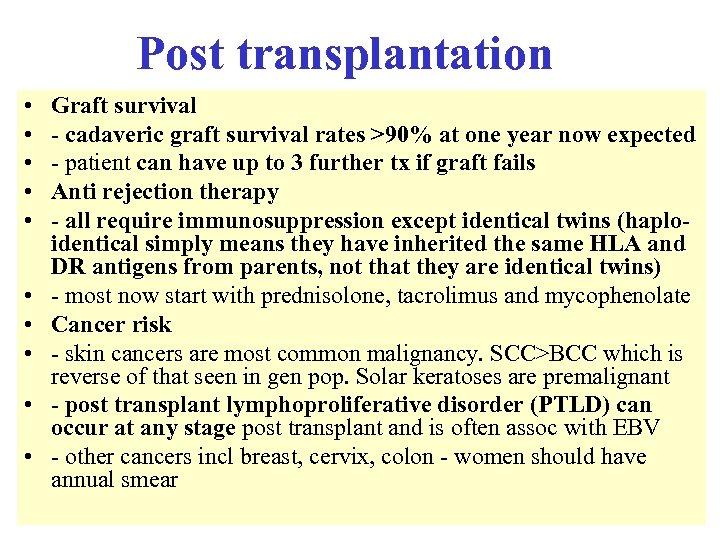 Post transplantation • • • Graft survival - cadaveric graft survival rates >90% at one year now expected - patient can have up to 3 further tx if graft fails Anti rejection therapy - all require immunosuppression except identical twins (haploidentical simply means they have inherited the same HLA and DR antigens from parents, not that they are identical twins) - most now start with prednisolone, tacrolimus and mycophenolate Cancer risk - skin cancers are most common malignancy. SCC>BCC which is reverse of that seen in gen pop. Solar keratoses are premalignant - post transplant lymphoproliferative disorder (PTLD) can occur at any stage post transplant and is often assoc with EBV - other cancers incl breast, cervix, colon - women should have annual smear
Post transplantation • • • Graft survival - cadaveric graft survival rates >90% at one year now expected - patient can have up to 3 further tx if graft fails Anti rejection therapy - all require immunosuppression except identical twins (haploidentical simply means they have inherited the same HLA and DR antigens from parents, not that they are identical twins) - most now start with prednisolone, tacrolimus and mycophenolate Cancer risk - skin cancers are most common malignancy. SCC>BCC which is reverse of that seen in gen pop. Solar keratoses are premalignant - post transplant lymphoproliferative disorder (PTLD) can occur at any stage post transplant and is often assoc with EBV - other cancers incl breast, cervix, colon - women should have annual smear
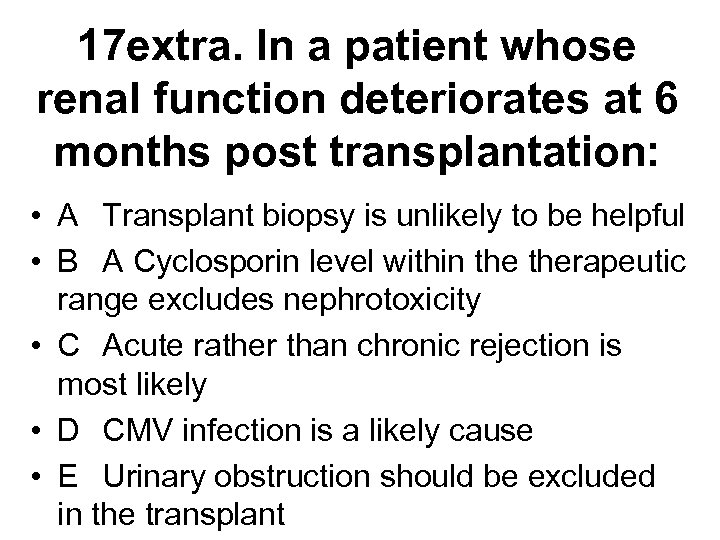 17 extra. In a patient whose renal function deteriorates at 6 months post transplantation: • A Transplant biopsy is unlikely to be helpful • B A Cyclosporin level within therapeutic range excludes nephrotoxicity • C Acute rather than chronic rejection is most likely • D CMV infection is a likely cause • E Urinary obstruction should be excluded in the transplant
17 extra. In a patient whose renal function deteriorates at 6 months post transplantation: • A Transplant biopsy is unlikely to be helpful • B A Cyclosporin level within therapeutic range excludes nephrotoxicity • C Acute rather than chronic rejection is most likely • D CMV infection is a likely cause • E Urinary obstruction should be excluded in the transplant
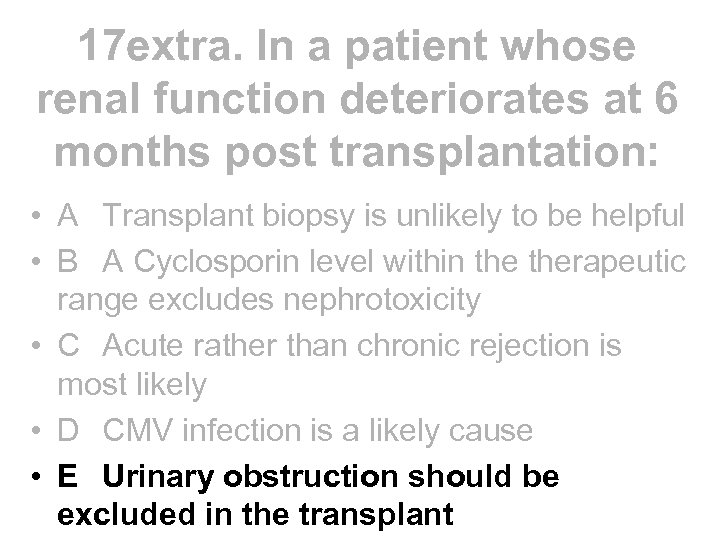 17 extra. In a patient whose renal function deteriorates at 6 months post transplantation: • A Transplant biopsy is unlikely to be helpful • B A Cyclosporin level within therapeutic range excludes nephrotoxicity • C Acute rather than chronic rejection is most likely • D CMV infection is a likely cause • E Urinary obstruction should be excluded in the transplant
17 extra. In a patient whose renal function deteriorates at 6 months post transplantation: • A Transplant biopsy is unlikely to be helpful • B A Cyclosporin level within therapeutic range excludes nephrotoxicity • C Acute rather than chronic rejection is most likely • D CMV infection is a likely cause • E Urinary obstruction should be excluded in the transplant
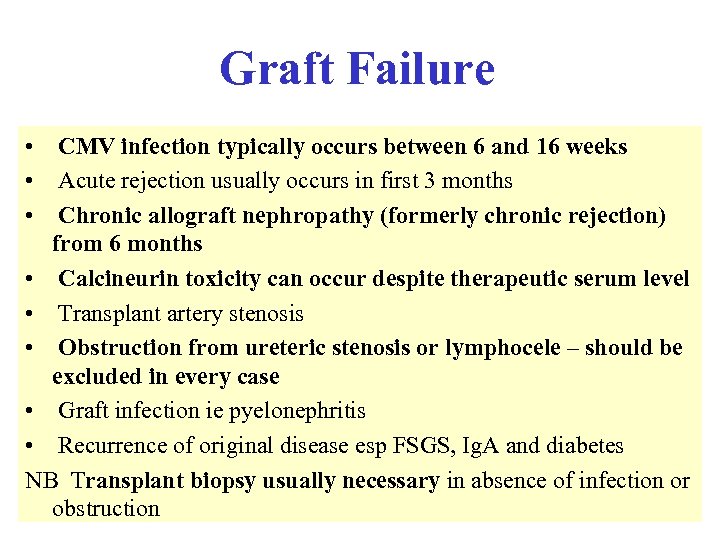 Graft Failure • CMV infection typically occurs between 6 and 16 weeks • Acute rejection usually occurs in first 3 months • Chronic allograft nephropathy (formerly chronic rejection) from 6 months • Calcineurin toxicity can occur despite therapeutic serum level • Transplant artery stenosis • Obstruction from ureteric stenosis or lymphocele – should be excluded in every case • Graft infection ie pyelonephritis • Recurrence of original disease esp FSGS, Ig. A and diabetes NB Transplant biopsy usually necessary in absence of infection or obstruction
Graft Failure • CMV infection typically occurs between 6 and 16 weeks • Acute rejection usually occurs in first 3 months • Chronic allograft nephropathy (formerly chronic rejection) from 6 months • Calcineurin toxicity can occur despite therapeutic serum level • Transplant artery stenosis • Obstruction from ureteric stenosis or lymphocele – should be excluded in every case • Graft infection ie pyelonephritis • Recurrence of original disease esp FSGS, Ig. A and diabetes NB Transplant biopsy usually necessary in absence of infection or obstruction
 Carpe Diem! and good luck
Carpe Diem! and good luck

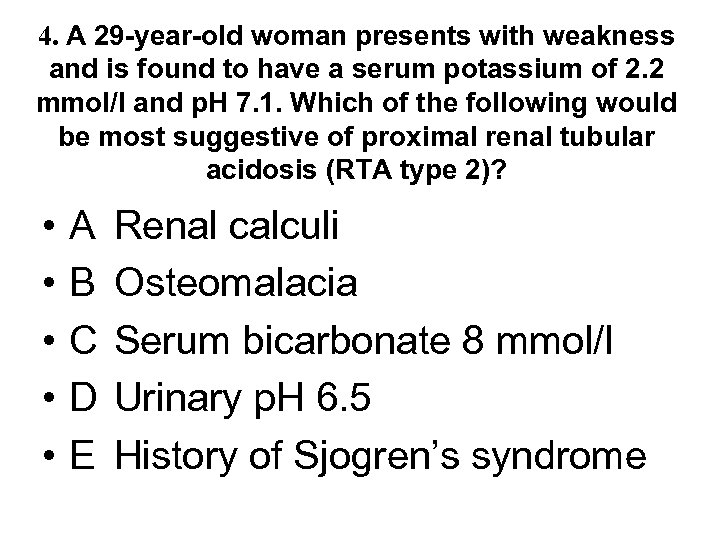 4. A 29 -year-old woman presents with weakness and is found to have a serum potassium of 2. 2 mmol/l and p. H 7. 1. Which of the following would be most suggestive of proximal renal tubular acidosis (RTA type 2)? • • • A B C D E Renal calculi Osteomalacia Serum bicarbonate 8 mmol/l Urinary p. H 6. 5 History of Sjogren’s syndrome
4. A 29 -year-old woman presents with weakness and is found to have a serum potassium of 2. 2 mmol/l and p. H 7. 1. Which of the following would be most suggestive of proximal renal tubular acidosis (RTA type 2)? • • • A B C D E Renal calculi Osteomalacia Serum bicarbonate 8 mmol/l Urinary p. H 6. 5 History of Sjogren’s syndrome
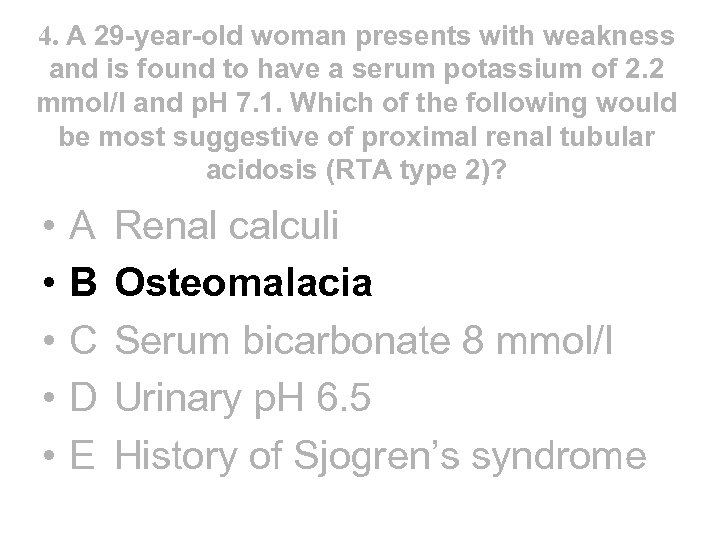 4. A 29 -year-old woman presents with weakness and is found to have a serum potassium of 2. 2 mmol/l and p. H 7. 1. Which of the following would be most suggestive of proximal renal tubular acidosis (RTA type 2)? • • • A B C D E Renal calculi Osteomalacia Serum bicarbonate 8 mmol/l Urinary p. H 6. 5 History of Sjogren’s syndrome
4. A 29 -year-old woman presents with weakness and is found to have a serum potassium of 2. 2 mmol/l and p. H 7. 1. Which of the following would be most suggestive of proximal renal tubular acidosis (RTA type 2)? • • • A B C D E Renal calculi Osteomalacia Serum bicarbonate 8 mmol/l Urinary p. H 6. 5 History of Sjogren’s syndrome
 How do kidneys regulate acid base balance?
How do kidneys regulate acid base balance?
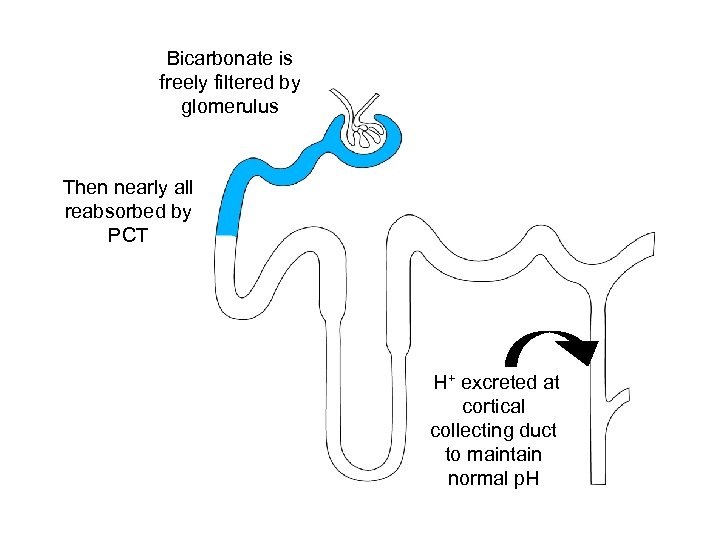 Bicarbonate is freely filtered by glomerulus Then nearly all reabsorbed by PCT H+ excreted at cortical collecting duct to maintain normal p. H
Bicarbonate is freely filtered by glomerulus Then nearly all reabsorbed by PCT H+ excreted at cortical collecting duct to maintain normal p. H
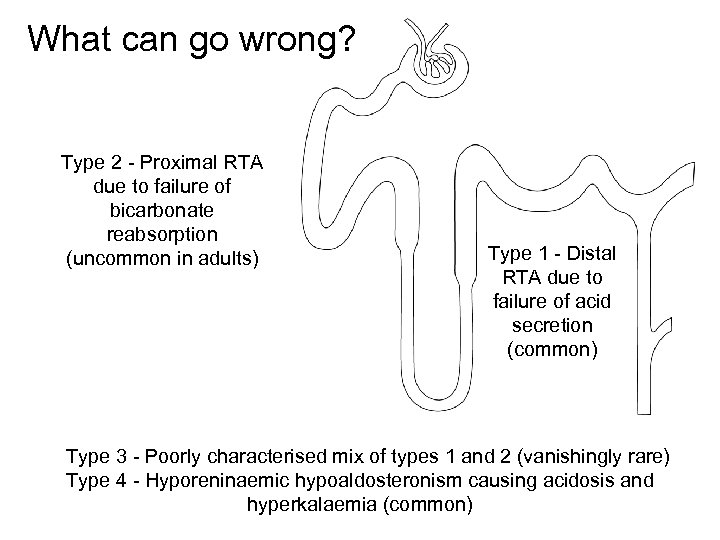 What can go wrong? Type 2 - Proximal RTA due to failure of bicarbonate reabsorption (uncommon in adults) Type 1 - Distal RTA due to failure of acid secretion (common) Type 3 - Poorly characterised mix of types 1 and 2 (vanishingly rare) Type 4 - Hyporeninaemic hypoaldosteronism causing acidosis and hyperkalaemia (common)
What can go wrong? Type 2 - Proximal RTA due to failure of bicarbonate reabsorption (uncommon in adults) Type 1 - Distal RTA due to failure of acid secretion (common) Type 3 - Poorly characterised mix of types 1 and 2 (vanishingly rare) Type 4 - Hyporeninaemic hypoaldosteronism causing acidosis and hyperkalaemia (common)
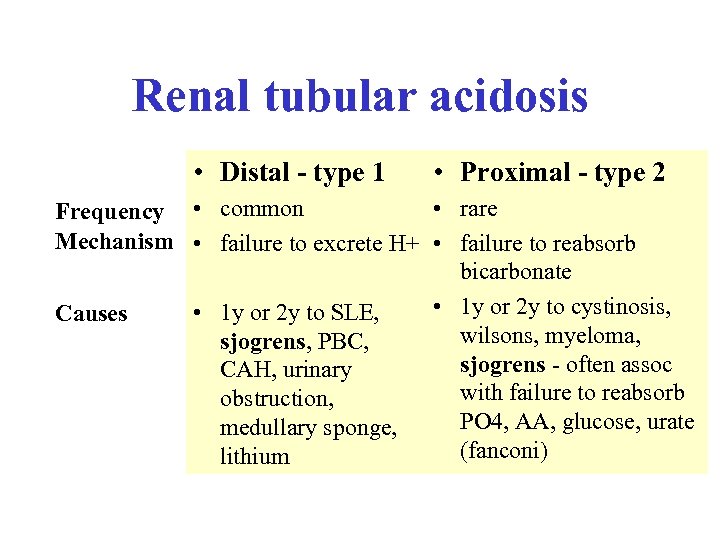 Renal tubular acidosis • Distal - type 1 • Proximal - type 2 • rare Frequency • common Mechanism • failure to excrete H+ • failure to reabsorb bicarbonate • 1 y or 2 y to cystinosis, • 1 y or 2 y to SLE, Causes wilsons, myeloma, sjogrens, PBC, sjogrens - often assoc CAH, urinary with failure to reabsorb obstruction, PO 4, AA, glucose, urate medullary sponge, (fanconi) lithium
Renal tubular acidosis • Distal - type 1 • Proximal - type 2 • rare Frequency • common Mechanism • failure to excrete H+ • failure to reabsorb bicarbonate • 1 y or 2 y to cystinosis, • 1 y or 2 y to SLE, Causes wilsons, myeloma, sjogrens, PBC, sjogrens - often assoc CAH, urinary with failure to reabsorb obstruction, PO 4, AA, glucose, urate medullary sponge, (fanconi) lithium
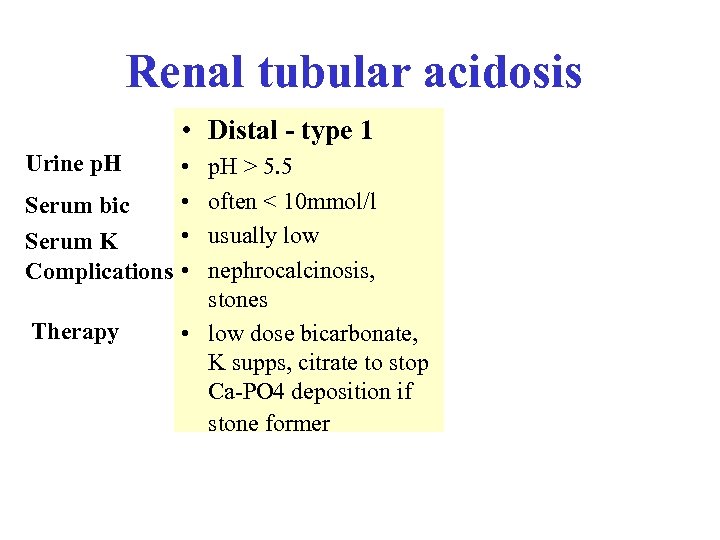 Renal tubular acidosis • Distal - type 1 Urine p. H • • Serum bic • Serum K Complications • Therapy p. H > 5. 5 often < 10 mmol/l usually low nephrocalcinosis, stones • low dose bicarbonate, K supps, citrate to stop Ca-PO 4 deposition if stone former
Renal tubular acidosis • Distal - type 1 Urine p. H • • Serum bic • Serum K Complications • Therapy p. H > 5. 5 often < 10 mmol/l usually low nephrocalcinosis, stones • low dose bicarbonate, K supps, citrate to stop Ca-PO 4 deposition if stone former
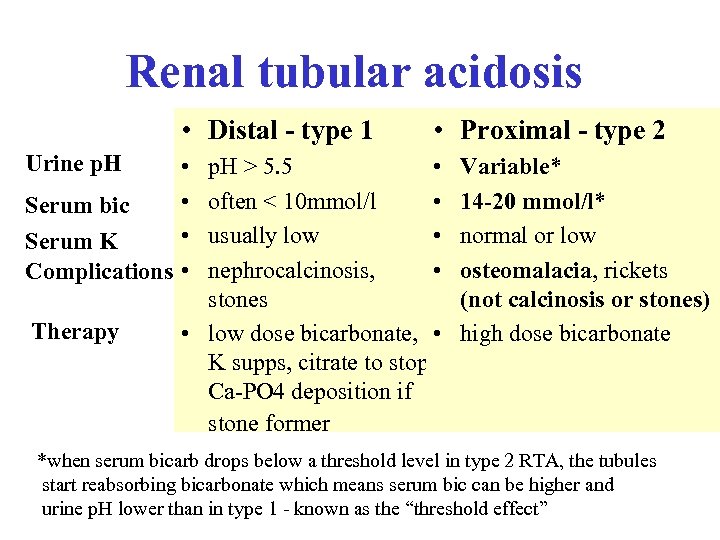 Renal tubular acidosis • Distal - type 1 Urine p. H • • Serum bic • Serum K Complications • Therapy • Proximal - type 2 p. H > 5. 5 • often < 10 mmol/l • usually low • nephrocalcinosis, • stones • low dose bicarbonate, • K supps, citrate to stop Ca-PO 4 deposition if stone former Variable* 14 -20 mmol/l* normal or low osteomalacia, rickets (not calcinosis or stones) high dose bicarbonate *when serum bicarb drops below a threshold level in type 2 RTA, the tubules start reabsorbing bicarbonate which means serum bic can be higher and urine p. H lower than in type 1 - known as the “threshold effect”
Renal tubular acidosis • Distal - type 1 Urine p. H • • Serum bic • Serum K Complications • Therapy • Proximal - type 2 p. H > 5. 5 • often < 10 mmol/l • usually low • nephrocalcinosis, • stones • low dose bicarbonate, • K supps, citrate to stop Ca-PO 4 deposition if stone former Variable* 14 -20 mmol/l* normal or low osteomalacia, rickets (not calcinosis or stones) high dose bicarbonate *when serum bicarb drops below a threshold level in type 2 RTA, the tubules start reabsorbing bicarbonate which means serum bic can be higher and urine p. H lower than in type 1 - known as the “threshold effect”
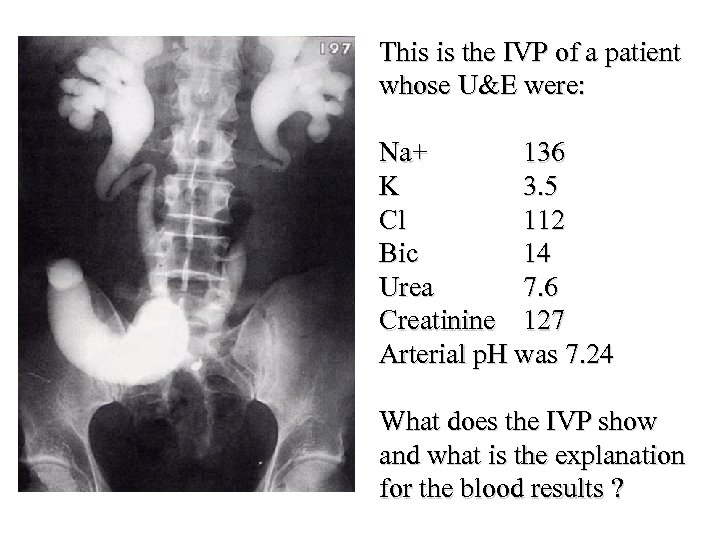 This is the IVP of a patient whose U&E were: Na+ 136 K 3. 5 Cl 112 Bic 14 Urea 7. 6 Creatinine 127 Arterial p. H was 7. 24 What does the IVP show and what is the explanation for the blood results ?
This is the IVP of a patient whose U&E were: Na+ 136 K 3. 5 Cl 112 Bic 14 Urea 7. 6 Creatinine 127 Arterial p. H was 7. 24 What does the IVP show and what is the explanation for the blood results ?
 1. The IVP shows an ileal conduit. 2. The blood results show evidence of a normal anion gap acidosis. This is due to direct loss of bicarbonate through the gut (eg diarrhoea, urinary diversion) or through the kidney (eg RTA). When bicarbonate is lost, more chloride is retained by the renal tubules to maintain electroneutrality.
1. The IVP shows an ileal conduit. 2. The blood results show evidence of a normal anion gap acidosis. This is due to direct loss of bicarbonate through the gut (eg diarrhoea, urinary diversion) or through the kidney (eg RTA). When bicarbonate is lost, more chloride is retained by the renal tubules to maintain electroneutrality.
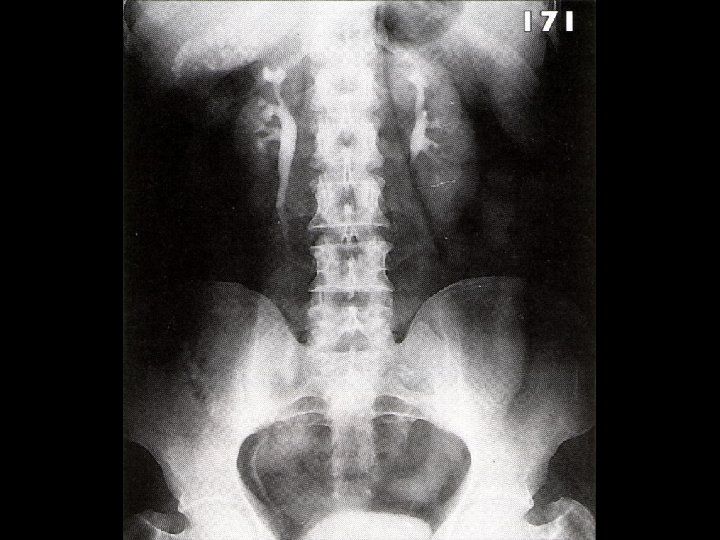
 25. In a patient with reflux nephropathy which of the following is most accurate? • A If reflux persists into adolescence ureteric reimplantation will become likely • B Renal scarring rarely occurs beyond 8 years of age • C The patient has a > 50% chance of requiring dialysis during his lifetime • D There is a 5% chance of the patient’s offspring suffering vesico-ureteric reflux • E There is usually evidence of urinary infection
25. In a patient with reflux nephropathy which of the following is most accurate? • A If reflux persists into adolescence ureteric reimplantation will become likely • B Renal scarring rarely occurs beyond 8 years of age • C The patient has a > 50% chance of requiring dialysis during his lifetime • D There is a 5% chance of the patient’s offspring suffering vesico-ureteric reflux • E There is usually evidence of urinary infection
 25. In a patient with reflux nephropathy which of the following is most accurate? • A If reflux persists into adolescence ureteric reimplantation will become likely • B Renal scarring rarely occurs beyond 8 years of age • C The patient has a > 50% chance of requiring dialysis during his lifetime • D There is a 5% chance of the patient’s offspring suffering vesico-ureteric reflux • E There is usually evidence of urinary infection
25. In a patient with reflux nephropathy which of the following is most accurate? • A If reflux persists into adolescence ureteric reimplantation will become likely • B Renal scarring rarely occurs beyond 8 years of age • C The patient has a > 50% chance of requiring dialysis during his lifetime • D There is a 5% chance of the patient’s offspring suffering vesico-ureteric reflux • E There is usually evidence of urinary infection
 2 extra Concerning chronic pyelonephritis: • A It is the most common cause of renal failure in the UK • B It is usually caused by recurrent acute pyelonephritis • C It may give rise to a salt losing nephropathy • D Bilateral native nephrectomy is necessary prior to renal transplantation • E The IVU shows cortical scarring and a normal calyceal pattern
2 extra Concerning chronic pyelonephritis: • A It is the most common cause of renal failure in the UK • B It is usually caused by recurrent acute pyelonephritis • C It may give rise to a salt losing nephropathy • D Bilateral native nephrectomy is necessary prior to renal transplantation • E The IVU shows cortical scarring and a normal calyceal pattern
 2 extra Concerning chronic pyelonephritis: • A It is the most common cause of renal failure in the UK • B It is usually caused by recurrent acute pyelonephritis • C It may give rise to a salt losing nephropathy • D Bilateral native nephrectomy is necessary prior to renal transplantation • E The IVU shows cortical scarring and a normal calyceal pattern
2 extra Concerning chronic pyelonephritis: • A It is the most common cause of renal failure in the UK • B It is usually caused by recurrent acute pyelonephritis • C It may give rise to a salt losing nephropathy • D Bilateral native nephrectomy is necessary prior to renal transplantation • E The IVU shows cortical scarring and a normal calyceal pattern
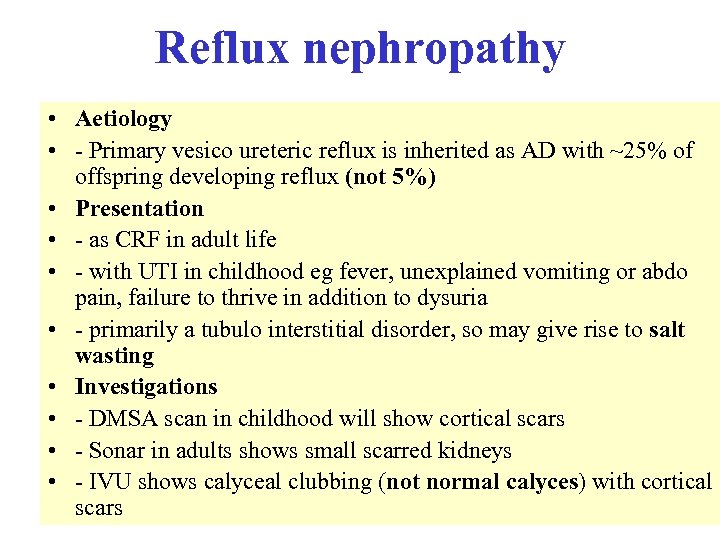 Reflux nephropathy • Aetiology • - Primary vesico ureteric reflux is inherited as AD with ~25% of offspring developing reflux (not 5%) • Presentation • - as CRF in adult life • - with UTI in childhood eg fever, unexplained vomiting or abdo pain, failure to thrive in addition to dysuria • - primarily a tubulo interstitial disorder, so may give rise to salt wasting • Investigations • - DMSA scan in childhood will show cortical scars • - Sonar in adults shows small scarred kidneys • - IVU shows calyceal clubbing (not normal calyces) with cortical scars
Reflux nephropathy • Aetiology • - Primary vesico ureteric reflux is inherited as AD with ~25% of offspring developing reflux (not 5%) • Presentation • - as CRF in adult life • - with UTI in childhood eg fever, unexplained vomiting or abdo pain, failure to thrive in addition to dysuria • - primarily a tubulo interstitial disorder, so may give rise to salt wasting • Investigations • - DMSA scan in childhood will show cortical scars • - Sonar in adults shows small scarred kidneys • - IVU shows calyceal clubbing (not normal calyces) with cortical scars
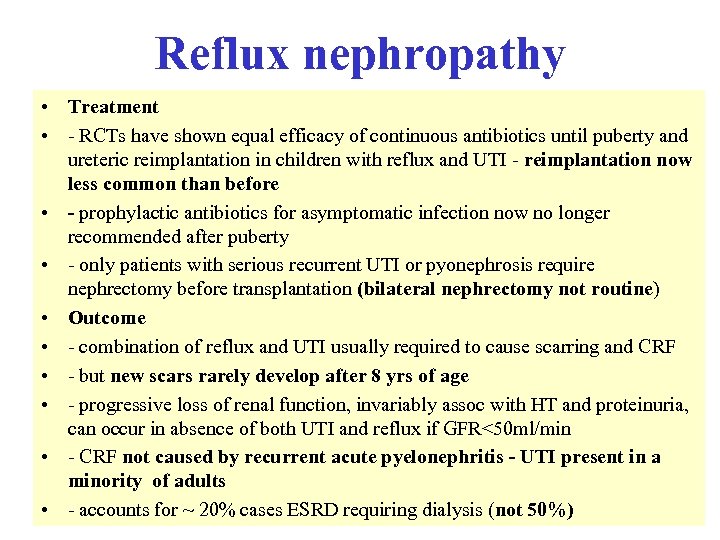 Reflux nephropathy • Treatment • - RCTs have shown equal efficacy of continuous antibiotics until puberty and ureteric reimplantation in children with reflux and UTI - reimplantation now less common than before • - prophylactic antibiotics for asymptomatic infection now no longer recommended after puberty • - only patients with serious recurrent UTI or pyonephrosis require nephrectomy before transplantation (bilateral nephrectomy not routine) • Outcome • - combination of reflux and UTI usually required to cause scarring and CRF • - but new scars rarely develop after 8 yrs of age • - progressive loss of renal function, invariably assoc with HT and proteinuria, can occur in absence of both UTI and reflux if GFR<50 ml/min • - CRF not caused by recurrent acute pyelonephritis - UTI present in a minority of adults • - accounts for ~ 20% cases ESRD requiring dialysis (not 50%)
Reflux nephropathy • Treatment • - RCTs have shown equal efficacy of continuous antibiotics until puberty and ureteric reimplantation in children with reflux and UTI - reimplantation now less common than before • - prophylactic antibiotics for asymptomatic infection now no longer recommended after puberty • - only patients with serious recurrent UTI or pyonephrosis require nephrectomy before transplantation (bilateral nephrectomy not routine) • Outcome • - combination of reflux and UTI usually required to cause scarring and CRF • - but new scars rarely develop after 8 yrs of age • - progressive loss of renal function, invariably assoc with HT and proteinuria, can occur in absence of both UTI and reflux if GFR<50 ml/min • - CRF not caused by recurrent acute pyelonephritis - UTI present in a minority of adults • - accounts for ~ 20% cases ESRD requiring dialysis (not 50%)
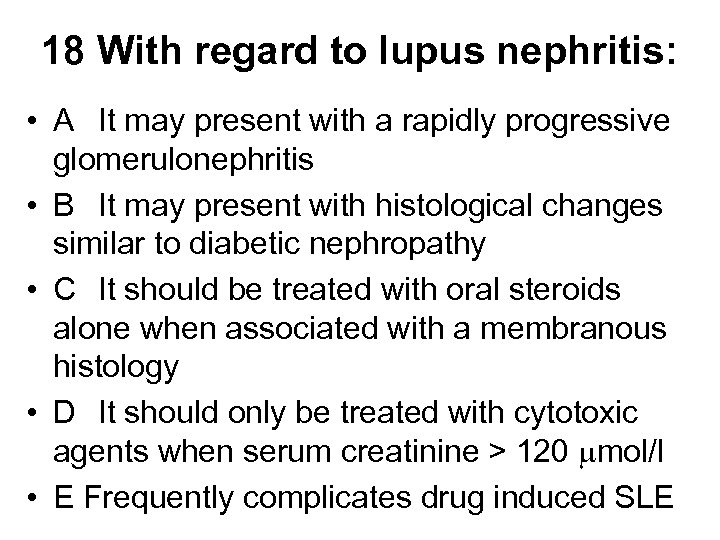 18 With regard to lupus nephritis: • A It may present with a rapidly progressive glomerulonephritis • B It may present with histological changes similar to diabetic nephropathy • C It should be treated with oral steroids alone when associated with a membranous histology • D It should only be treated with cytotoxic agents when serum creatinine > 120 mol/l • E Frequently complicates drug induced SLE
18 With regard to lupus nephritis: • A It may present with a rapidly progressive glomerulonephritis • B It may present with histological changes similar to diabetic nephropathy • C It should be treated with oral steroids alone when associated with a membranous histology • D It should only be treated with cytotoxic agents when serum creatinine > 120 mol/l • E Frequently complicates drug induced SLE
 18 With regard to lupus nephritis: • A It may present with a rapidly progressive glomerulonephritis • B It may present with histological changes similar to diabetic nephropathy • C It should be treated with oral steroids alone when associated with a membranous histology • D It should only be treated with cytotoxic agents when serum creatinine > 120 mol/l • E Frequently complicates drug induced SLE
18 With regard to lupus nephritis: • A It may present with a rapidly progressive glomerulonephritis • B It may present with histological changes similar to diabetic nephropathy • C It should be treated with oral steroids alone when associated with a membranous histology • D It should only be treated with cytotoxic agents when serum creatinine > 120 mol/l • E Frequently complicates drug induced SLE
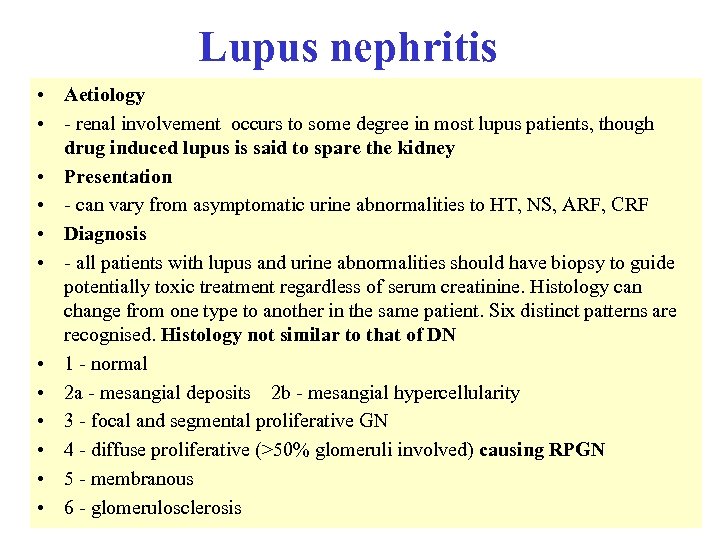 Lupus nephritis • Aetiology • - renal involvement occurs to some degree in most lupus patients, though drug induced lupus is said to spare the kidney • Presentation • - can vary from asymptomatic urine abnormalities to HT, NS, ARF, CRF • Diagnosis • - all patients with lupus and urine abnormalities should have biopsy to guide potentially toxic treatment regardless of serum creatinine. Histology can change from one type to another in the same patient. Six distinct patterns are recognised. Histology not similar to that of DN • 1 - normal • 2 a - mesangial deposits 2 b - mesangial hypercellularity • 3 - focal and segmental proliferative GN • 4 - diffuse proliferative (>50% glomeruli involved) causing RPGN • 5 - membranous • 6 - glomerulosclerosis
Lupus nephritis • Aetiology • - renal involvement occurs to some degree in most lupus patients, though drug induced lupus is said to spare the kidney • Presentation • - can vary from asymptomatic urine abnormalities to HT, NS, ARF, CRF • Diagnosis • - all patients with lupus and urine abnormalities should have biopsy to guide potentially toxic treatment regardless of serum creatinine. Histology can change from one type to another in the same patient. Six distinct patterns are recognised. Histology not similar to that of DN • 1 - normal • 2 a - mesangial deposits 2 b - mesangial hypercellularity • 3 - focal and segmental proliferative GN • 4 - diffuse proliferative (>50% glomeruli involved) causing RPGN • 5 - membranous • 6 - glomerulosclerosis
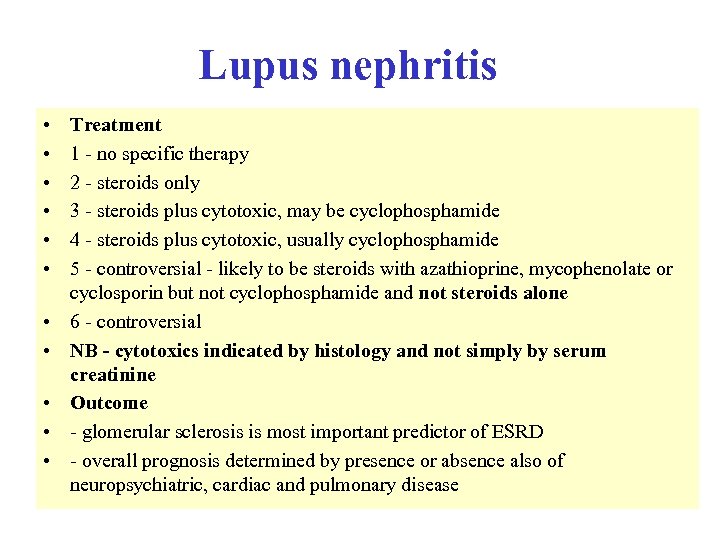 Lupus nephritis • • • Treatment 1 - no specific therapy 2 - steroids only 3 - steroids plus cytotoxic, may be cyclophosphamide 4 - steroids plus cytotoxic, usually cyclophosphamide 5 - controversial - likely to be steroids with azathioprine, mycophenolate or cyclosporin but not cyclophosphamide and not steroids alone 6 - controversial NB - cytotoxics indicated by histology and not simply by serum creatinine Outcome - glomerular sclerosis is most important predictor of ESRD - overall prognosis determined by presence or absence also of neuropsychiatric, cardiac and pulmonary disease
Lupus nephritis • • • Treatment 1 - no specific therapy 2 - steroids only 3 - steroids plus cytotoxic, may be cyclophosphamide 4 - steroids plus cytotoxic, usually cyclophosphamide 5 - controversial - likely to be steroids with azathioprine, mycophenolate or cyclosporin but not cyclophosphamide and not steroids alone 6 - controversial NB - cytotoxics indicated by histology and not simply by serum creatinine Outcome - glomerular sclerosis is most important predictor of ESRD - overall prognosis determined by presence or absence also of neuropsychiatric, cardiac and pulmonary disease
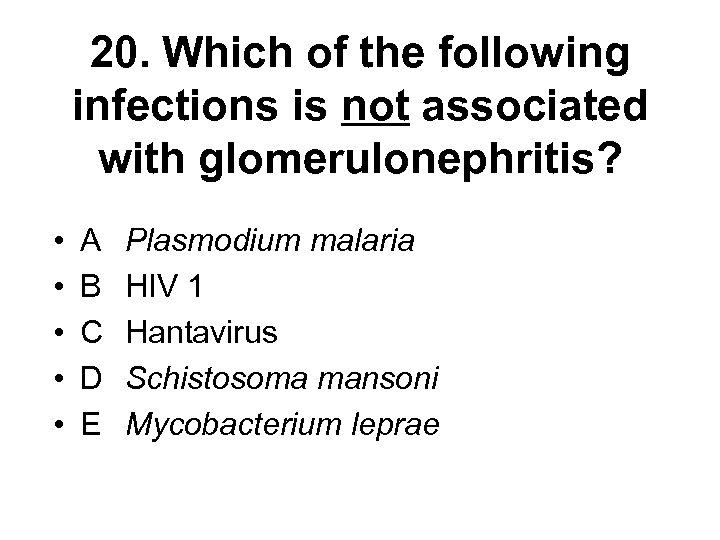 20. Which of the following infections is not associated with glomerulonephritis? • • • A B C D E Plasmodium malaria HIV 1 Hantavirus Schistosoma mansoni Mycobacterium leprae
20. Which of the following infections is not associated with glomerulonephritis? • • • A B C D E Plasmodium malaria HIV 1 Hantavirus Schistosoma mansoni Mycobacterium leprae
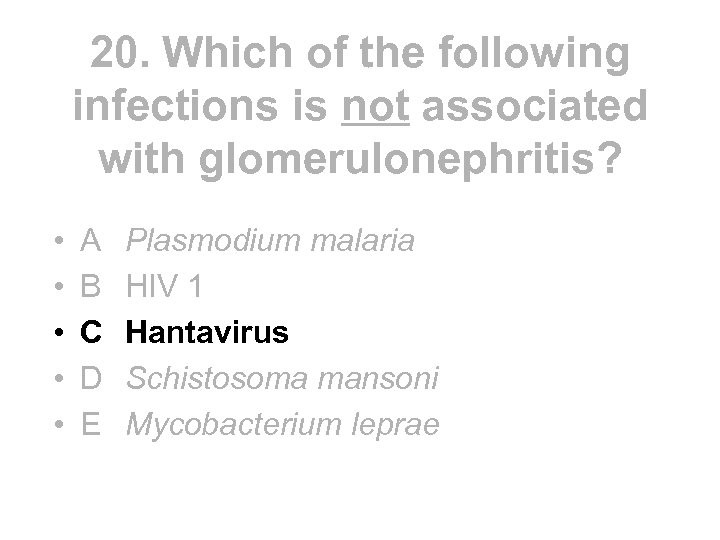 20. Which of the following infections is not associated with glomerulonephritis? • • • A B C D E Plasmodium malaria HIV 1 Hantavirus Schistosoma mansoni Mycobacterium leprae
20. Which of the following infections is not associated with glomerulonephritis? • • • A B C D E Plasmodium malaria HIV 1 Hantavirus Schistosoma mansoni Mycobacterium leprae
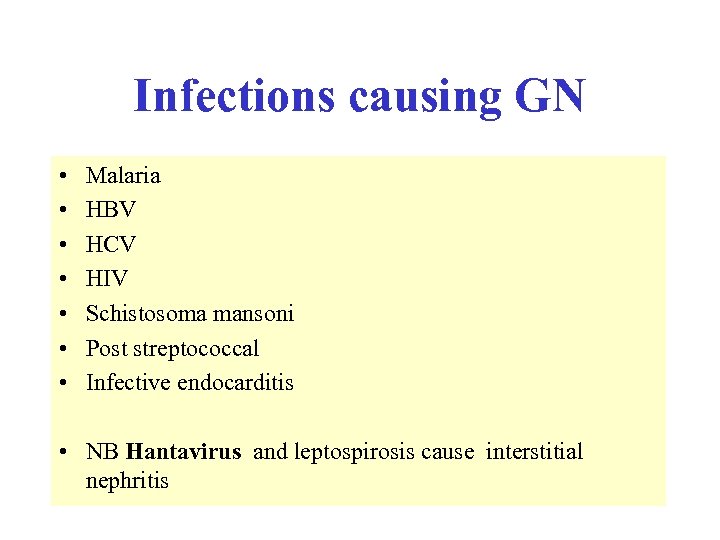 Infections causing GN • • Malaria HBV HCV HIV Schistosoma mansoni Post streptococcal Infective endocarditis • NB Hantavirus and leptospirosis cause interstitial nephritis
Infections causing GN • • Malaria HBV HCV HIV Schistosoma mansoni Post streptococcal Infective endocarditis • NB Hantavirus and leptospirosis cause interstitial nephritis
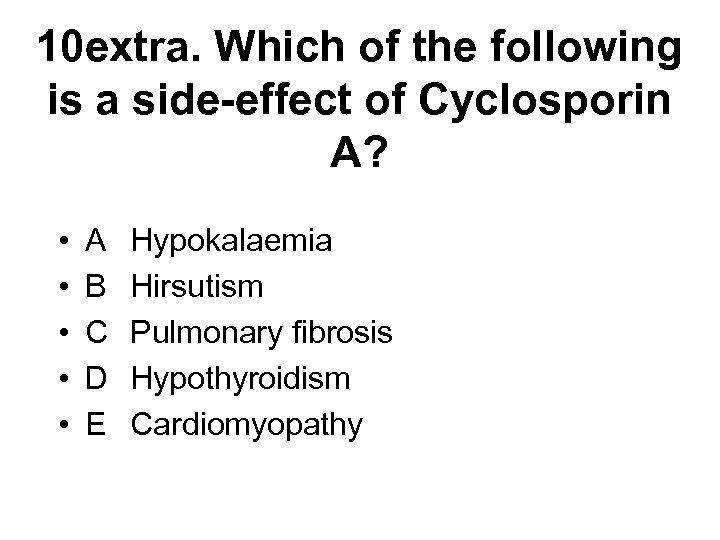 10 extra. Which of the following is a side-effect of Cyclosporin A? • • • A B C D E Hypokalaemia Hirsutism Pulmonary fibrosis Hypothyroidism Cardiomyopathy
10 extra. Which of the following is a side-effect of Cyclosporin A? • • • A B C D E Hypokalaemia Hirsutism Pulmonary fibrosis Hypothyroidism Cardiomyopathy
 10 extra. Which of the following is a side-effect of Cyclosporin A? • • • A B C D E Hypokalaemia Hirsutism Pulmonary fibrosis Hypothyroidism Cardiomyopathy
10 extra. Which of the following is a side-effect of Cyclosporin A? • • • A B C D E Hypokalaemia Hirsutism Pulmonary fibrosis Hypothyroidism Cardiomyopathy
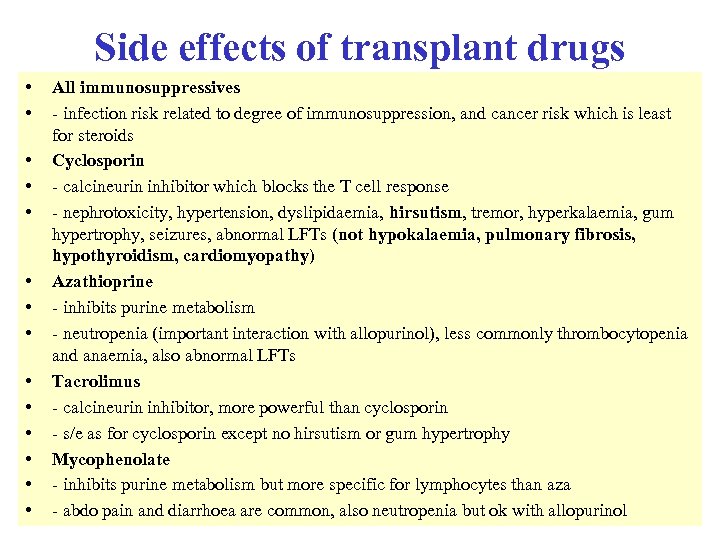 Side effects of transplant drugs • • • • All immunosuppressives - infection risk related to degree of immunosuppression, and cancer risk which is least for steroids Cyclosporin - calcineurin inhibitor which blocks the T cell response - nephrotoxicity, hypertension, dyslipidaemia, hirsutism, tremor, hyperkalaemia, gum hypertrophy, seizures, abnormal LFTs (not hypokalaemia, pulmonary fibrosis, hypothyroidism, cardiomyopathy) Azathioprine - inhibits purine metabolism - neutropenia (important interaction with allopurinol), less commonly thrombocytopenia and anaemia, also abnormal LFTs Tacrolimus - calcineurin inhibitor, more powerful than cyclosporin - s/e as for cyclosporin except no hirsutism or gum hypertrophy Mycophenolate - inhibits purine metabolism but more specific for lymphocytes than aza - abdo pain and diarrhoea are common, also neutropenia but ok with allopurinol
Side effects of transplant drugs • • • • All immunosuppressives - infection risk related to degree of immunosuppression, and cancer risk which is least for steroids Cyclosporin - calcineurin inhibitor which blocks the T cell response - nephrotoxicity, hypertension, dyslipidaemia, hirsutism, tremor, hyperkalaemia, gum hypertrophy, seizures, abnormal LFTs (not hypokalaemia, pulmonary fibrosis, hypothyroidism, cardiomyopathy) Azathioprine - inhibits purine metabolism - neutropenia (important interaction with allopurinol), less commonly thrombocytopenia and anaemia, also abnormal LFTs Tacrolimus - calcineurin inhibitor, more powerful than cyclosporin - s/e as for cyclosporin except no hirsutism or gum hypertrophy Mycophenolate - inhibits purine metabolism but more specific for lymphocytes than aza - abdo pain and diarrhoea are common, also neutropenia but ok with allopurinol
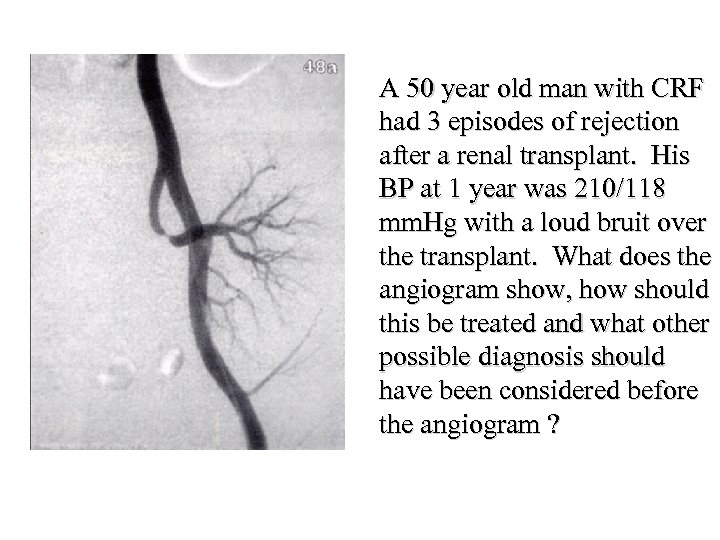 A 50 year old man with CRF had 3 episodes of rejection after a renal transplant. His BP at 1 year was 210/118 mm. Hg with a loud bruit over the transplant. What does the angiogram show, how should this be treated and what other possible diagnosis should have been considered before the angiogram ?
A 50 year old man with CRF had 3 episodes of rejection after a renal transplant. His BP at 1 year was 210/118 mm. Hg with a loud bruit over the transplant. What does the angiogram show, how should this be treated and what other possible diagnosis should have been considered before the angiogram ?
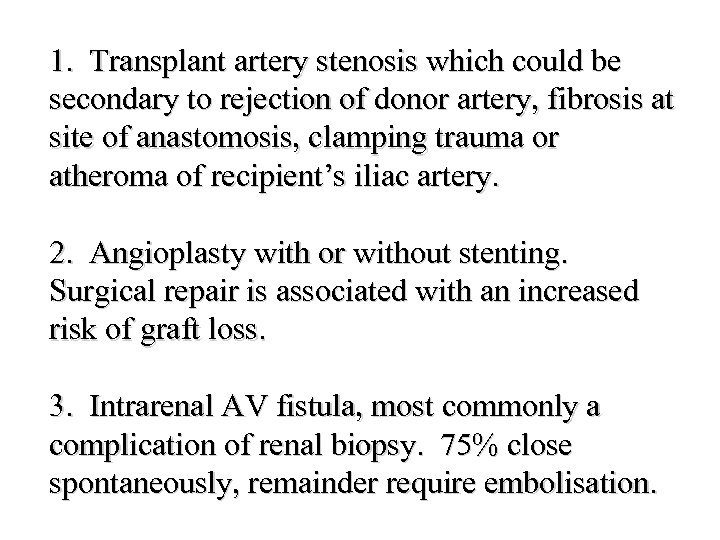 1. Transplant artery stenosis which could be secondary to rejection of donor artery, fibrosis at site of anastomosis, clamping trauma or atheroma of recipient’s iliac artery. 2. Angioplasty with or without stenting. Surgical repair is associated with an increased risk of graft loss. 3. Intrarenal AV fistula, most commonly a complication of renal biopsy. 75% close spontaneously, remainder require embolisation.
1. Transplant artery stenosis which could be secondary to rejection of donor artery, fibrosis at site of anastomosis, clamping trauma or atheroma of recipient’s iliac artery. 2. Angioplasty with or without stenting. Surgical repair is associated with an increased risk of graft loss. 3. Intrarenal AV fistula, most commonly a complication of renal biopsy. 75% close spontaneously, remainder require embolisation.
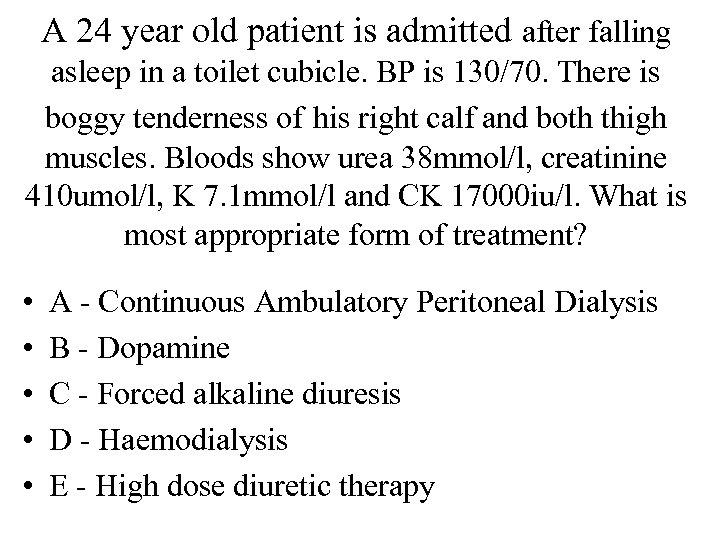 A 24 year old patient is admitted after falling asleep in a toilet cubicle. BP is 130/70. There is boggy tenderness of his right calf and both thigh muscles. Bloods show urea 38 mmol/l, creatinine 410 umol/l, K 7. 1 mmol/l and CK 17000 iu/l. What is most appropriate form of treatment? • • • A - Continuous Ambulatory Peritoneal Dialysis B - Dopamine C - Forced alkaline diuresis D - Haemodialysis E - High dose diuretic therapy
A 24 year old patient is admitted after falling asleep in a toilet cubicle. BP is 130/70. There is boggy tenderness of his right calf and both thigh muscles. Bloods show urea 38 mmol/l, creatinine 410 umol/l, K 7. 1 mmol/l and CK 17000 iu/l. What is most appropriate form of treatment? • • • A - Continuous Ambulatory Peritoneal Dialysis B - Dopamine C - Forced alkaline diuresis D - Haemodialysis E - High dose diuretic therapy
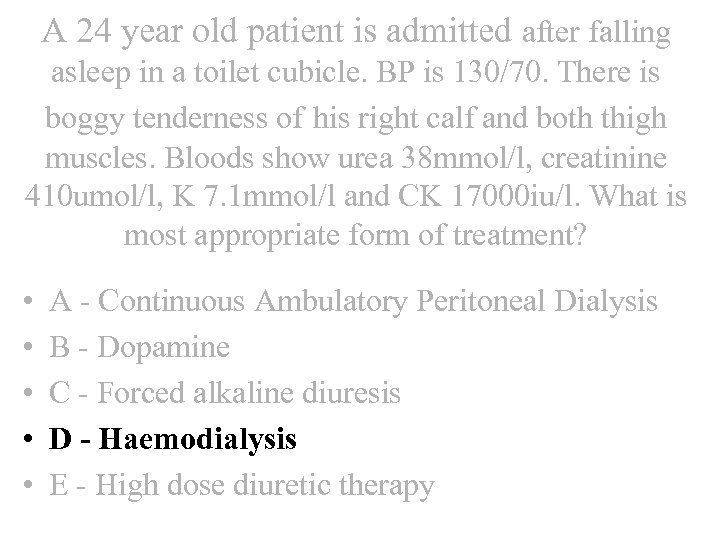 A 24 year old patient is admitted after falling asleep in a toilet cubicle. BP is 130/70. There is boggy tenderness of his right calf and both thigh muscles. Bloods show urea 38 mmol/l, creatinine 410 umol/l, K 7. 1 mmol/l and CK 17000 iu/l. What is most appropriate form of treatment? • • • A - Continuous Ambulatory Peritoneal Dialysis B - Dopamine C - Forced alkaline diuresis D - Haemodialysis E - High dose diuretic therapy
A 24 year old patient is admitted after falling asleep in a toilet cubicle. BP is 130/70. There is boggy tenderness of his right calf and both thigh muscles. Bloods show urea 38 mmol/l, creatinine 410 umol/l, K 7. 1 mmol/l and CK 17000 iu/l. What is most appropriate form of treatment? • • • A - Continuous Ambulatory Peritoneal Dialysis B - Dopamine C - Forced alkaline diuresis D - Haemodialysis E - High dose diuretic therapy
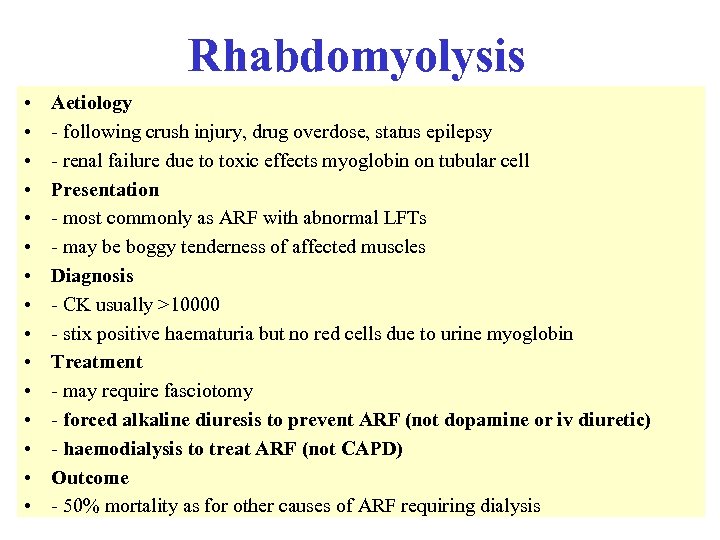 Rhabdomyolysis • • • • Aetiology - following crush injury, drug overdose, status epilepsy - renal failure due to toxic effects myoglobin on tubular cell Presentation - most commonly as ARF with abnormal LFTs - may be boggy tenderness of affected muscles Diagnosis - CK usually >10000 - stix positive haematuria but no red cells due to urine myoglobin Treatment - may require fasciotomy - forced alkaline diuresis to prevent ARF (not dopamine or iv diuretic) - haemodialysis to treat ARF (not CAPD) Outcome - 50% mortality as for other causes of ARF requiring dialysis
Rhabdomyolysis • • • • Aetiology - following crush injury, drug overdose, status epilepsy - renal failure due to toxic effects myoglobin on tubular cell Presentation - most commonly as ARF with abnormal LFTs - may be boggy tenderness of affected muscles Diagnosis - CK usually >10000 - stix positive haematuria but no red cells due to urine myoglobin Treatment - may require fasciotomy - forced alkaline diuresis to prevent ARF (not dopamine or iv diuretic) - haemodialysis to treat ARF (not CAPD) Outcome - 50% mortality as for other causes of ARF requiring dialysis
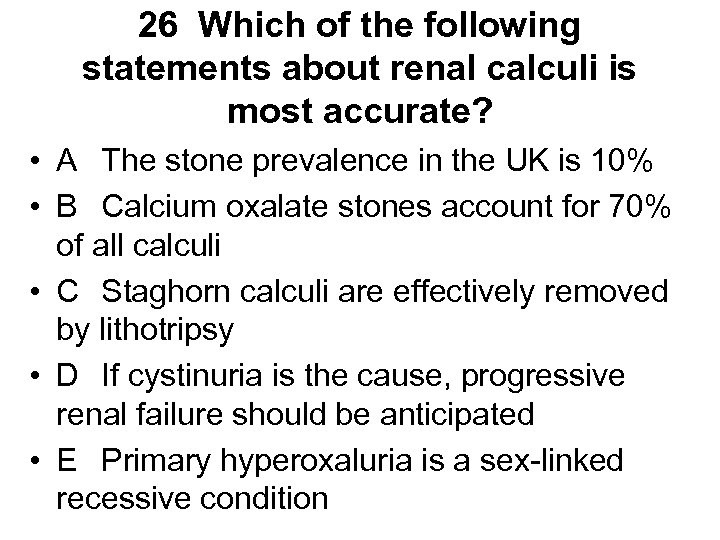 26 Which of the following statements about renal calculi is most accurate? • A The stone prevalence in the UK is 10% • B Calcium oxalate stones account for 70% of all calculi • C Staghorn calculi are effectively removed by lithotripsy • D If cystinuria is the cause, progressive renal failure should be anticipated • E Primary hyperoxaluria is a sex-linked recessive condition
26 Which of the following statements about renal calculi is most accurate? • A The stone prevalence in the UK is 10% • B Calcium oxalate stones account for 70% of all calculi • C Staghorn calculi are effectively removed by lithotripsy • D If cystinuria is the cause, progressive renal failure should be anticipated • E Primary hyperoxaluria is a sex-linked recessive condition
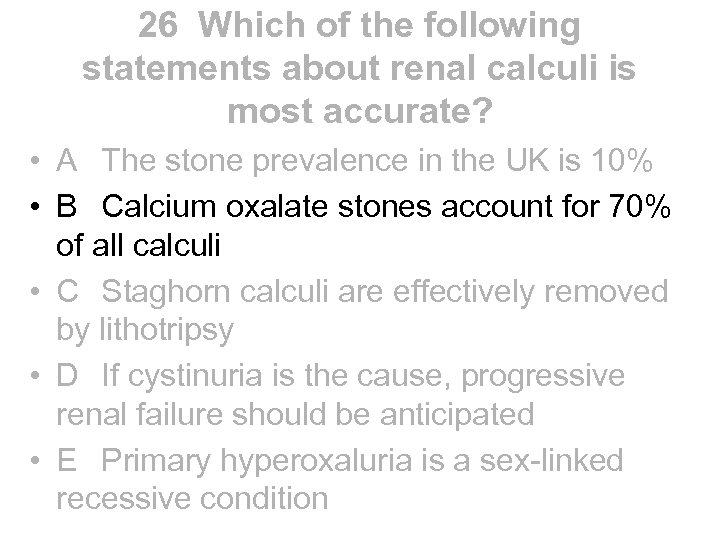 26 Which of the following statements about renal calculi is most accurate? • A The stone prevalence in the UK is 10% • B Calcium oxalate stones account for 70% of all calculi • C Staghorn calculi are effectively removed by lithotripsy • D If cystinuria is the cause, progressive renal failure should be anticipated • E Primary hyperoxaluria is a sex-linked recessive condition
26 Which of the following statements about renal calculi is most accurate? • A The stone prevalence in the UK is 10% • B Calcium oxalate stones account for 70% of all calculi • C Staghorn calculi are effectively removed by lithotripsy • D If cystinuria is the cause, progressive renal failure should be anticipated • E Primary hyperoxaluria is a sex-linked recessive condition
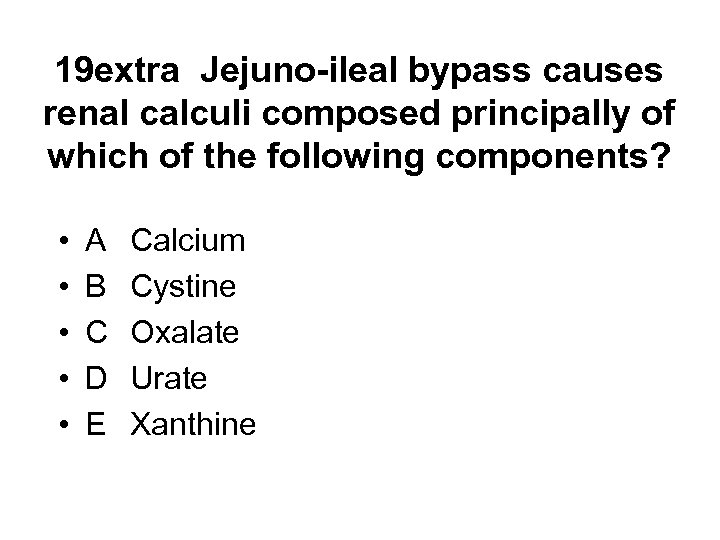 19 extra Jejuno-ileal bypass causes renal calculi composed principally of which of the following components? • • • A B C D E Calcium Cystine Oxalate Urate Xanthine
19 extra Jejuno-ileal bypass causes renal calculi composed principally of which of the following components? • • • A B C D E Calcium Cystine Oxalate Urate Xanthine
 19 extra Jejuno-ileal bypass causes renal calculi composed principally of which of the following components? • • • A B C D E Calcium Cystine Oxalate Urate Xanthine
19 extra Jejuno-ileal bypass causes renal calculi composed principally of which of the following components? • • • A B C D E Calcium Cystine Oxalate Urate Xanthine
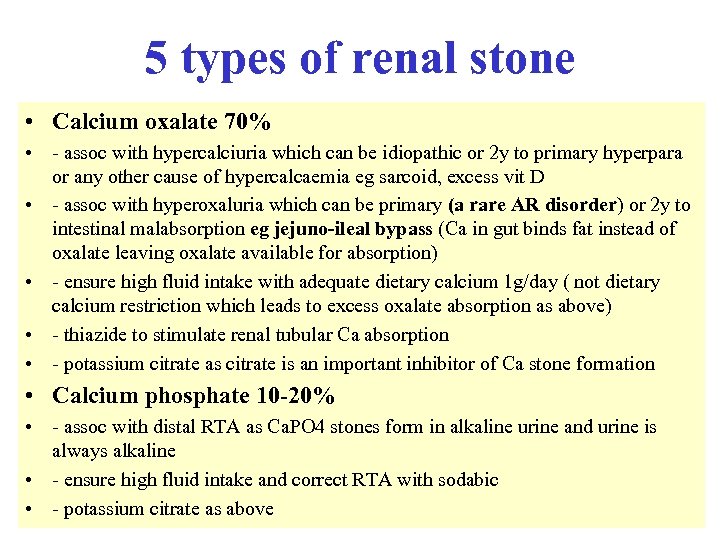 5 types of renal stone • Calcium oxalate 70% • - assoc with hypercalciuria which can be idiopathic or 2 y to primary hyperpara or any other cause of hypercalcaemia eg sarcoid, excess vit D • - assoc with hyperoxaluria which can be primary (a rare AR disorder) or 2 y to intestinal malabsorption eg jejuno-ileal bypass (Ca in gut binds fat instead of oxalate leaving oxalate available for absorption) • - ensure high fluid intake with adequate dietary calcium 1 g/day ( not dietary calcium restriction which leads to excess oxalate absorption as above) • - thiazide to stimulate renal tubular Ca absorption • - potassium citrate as citrate is an important inhibitor of Ca stone formation • Calcium phosphate 10 -20% • - assoc with distal RTA as Ca. PO 4 stones form in alkaline urine and urine is always alkaline • - ensure high fluid intake and correct RTA with sodabic • - potassium citrate as above
5 types of renal stone • Calcium oxalate 70% • - assoc with hypercalciuria which can be idiopathic or 2 y to primary hyperpara or any other cause of hypercalcaemia eg sarcoid, excess vit D • - assoc with hyperoxaluria which can be primary (a rare AR disorder) or 2 y to intestinal malabsorption eg jejuno-ileal bypass (Ca in gut binds fat instead of oxalate leaving oxalate available for absorption) • - ensure high fluid intake with adequate dietary calcium 1 g/day ( not dietary calcium restriction which leads to excess oxalate absorption as above) • - thiazide to stimulate renal tubular Ca absorption • - potassium citrate as citrate is an important inhibitor of Ca stone formation • Calcium phosphate 10 -20% • - assoc with distal RTA as Ca. PO 4 stones form in alkaline urine and urine is always alkaline • - ensure high fluid intake and correct RTA with sodabic • - potassium citrate as above
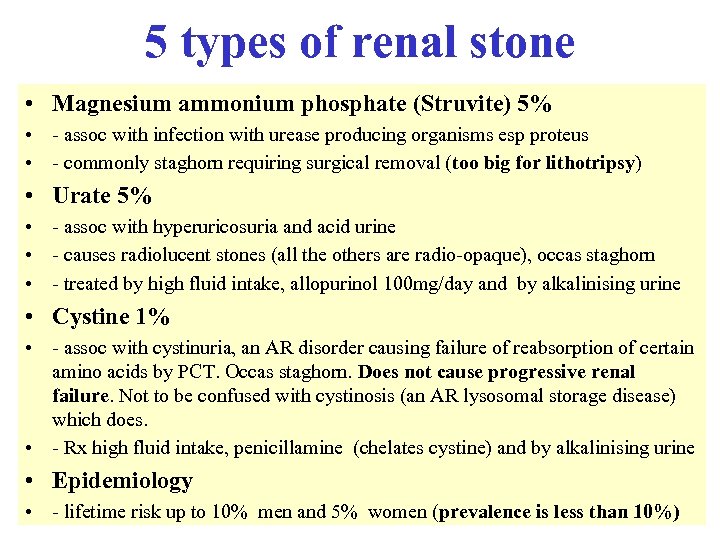 5 types of renal stone • Magnesium ammonium phosphate (Struvite) 5% • - assoc with infection with urease producing organisms esp proteus • - commonly staghorn requiring surgical removal (too big for lithotripsy) • Urate 5% • - assoc with hyperuricosuria and acid urine • - causes radiolucent stones (all the others are radio-opaque), occas staghorn • - treated by high fluid intake, allopurinol 100 mg/day and by alkalinising urine • Cystine 1% • - assoc with cystinuria, an AR disorder causing failure of reabsorption of certain amino acids by PCT. Occas staghorn. Does not cause progressive renal failure. Not to be confused with cystinosis (an AR lysosomal storage disease) which does. • - Rx high fluid intake, penicillamine (chelates cystine) and by alkalinising urine • Epidemiology • - lifetime risk up to 10% men and 5% women (prevalence is less than 10%)
5 types of renal stone • Magnesium ammonium phosphate (Struvite) 5% • - assoc with infection with urease producing organisms esp proteus • - commonly staghorn requiring surgical removal (too big for lithotripsy) • Urate 5% • - assoc with hyperuricosuria and acid urine • - causes radiolucent stones (all the others are radio-opaque), occas staghorn • - treated by high fluid intake, allopurinol 100 mg/day and by alkalinising urine • Cystine 1% • - assoc with cystinuria, an AR disorder causing failure of reabsorption of certain amino acids by PCT. Occas staghorn. Does not cause progressive renal failure. Not to be confused with cystinosis (an AR lysosomal storage disease) which does. • - Rx high fluid intake, penicillamine (chelates cystine) and by alkalinising urine • Epidemiology • - lifetime risk up to 10% men and 5% women (prevalence is less than 10%)
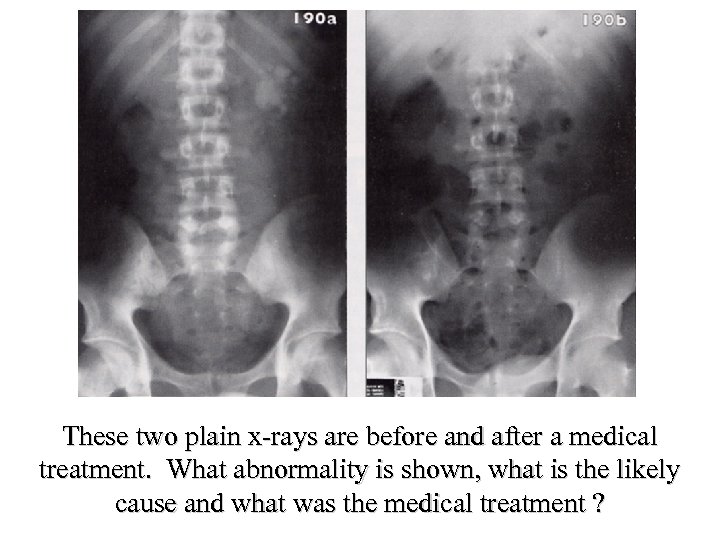 These two plain x-rays are before and after a medical treatment. What abnormality is shown, what is the likely cause and what was the medical treatment ?
These two plain x-rays are before and after a medical treatment. What abnormality is shown, what is the likely cause and what was the medical treatment ?
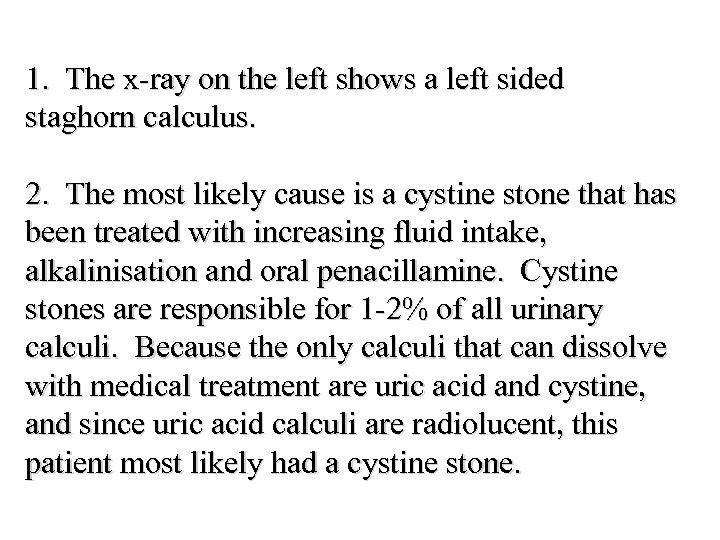 1. The x-ray on the left shows a left sided staghorn calculus. 2. The most likely cause is a cystine stone that has been treated with increasing fluid intake, alkalinisation and oral penacillamine. Cystine stones are responsible for 1 -2% of all urinary calculi. Because the only calculi that can dissolve with medical treatment are uric acid and cystine, and since uric acid calculi are radiolucent, this patient most likely had a cystine stone.
1. The x-ray on the left shows a left sided staghorn calculus. 2. The most likely cause is a cystine stone that has been treated with increasing fluid intake, alkalinisation and oral penacillamine. Cystine stones are responsible for 1 -2% of all urinary calculi. Because the only calculi that can dissolve with medical treatment are uric acid and cystine, and since uric acid calculi are radiolucent, this patient most likely had a cystine stone.
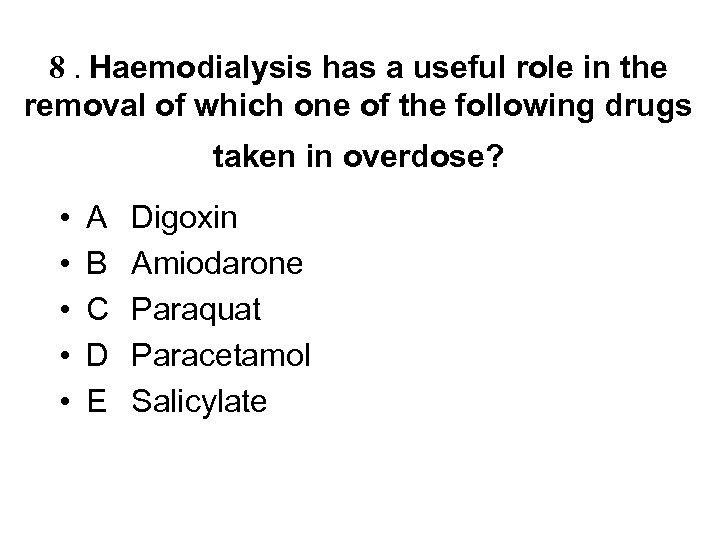 8. Haemodialysis has a useful role in the removal of which one of the following drugs taken in overdose? • • • A B C D E Digoxin Amiodarone Paraquat Paracetamol Salicylate
8. Haemodialysis has a useful role in the removal of which one of the following drugs taken in overdose? • • • A B C D E Digoxin Amiodarone Paraquat Paracetamol Salicylate
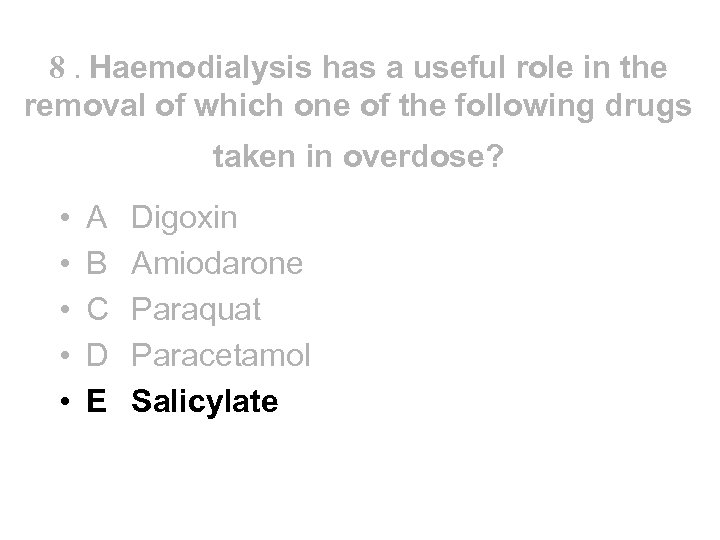 8. Haemodialysis has a useful role in the removal of which one of the following drugs taken in overdose? • • • A B C D E Digoxin Amiodarone Paraquat Paracetamol Salicylate
8. Haemodialysis has a useful role in the removal of which one of the following drugs taken in overdose? • • • A B C D E Digoxin Amiodarone Paraquat Paracetamol Salicylate
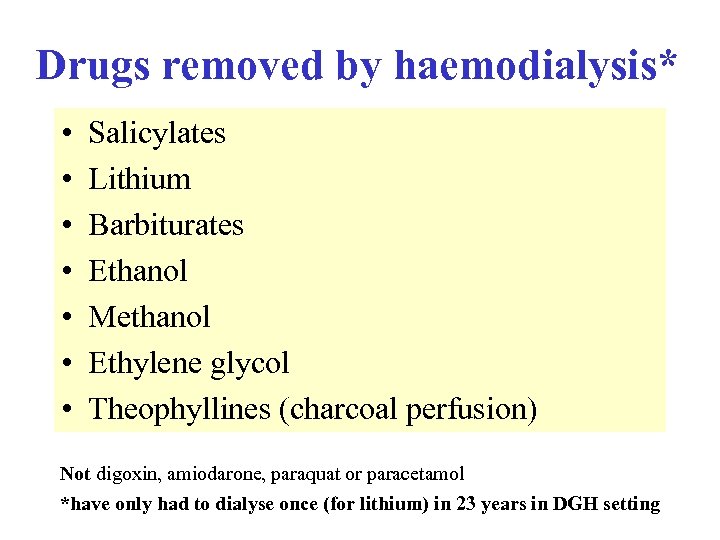 Drugs removed by haemodialysis* • • Salicylates Lithium Barbiturates Ethanol Methanol Ethylene glycol Theophyllines (charcoal perfusion) Not digoxin, amiodarone, paraquat or paracetamol *have only had to dialyse once (for lithium) in 23 years in DGH setting
Drugs removed by haemodialysis* • • Salicylates Lithium Barbiturates Ethanol Methanol Ethylene glycol Theophyllines (charcoal perfusion) Not digoxin, amiodarone, paraquat or paracetamol *have only had to dialyse once (for lithium) in 23 years in DGH setting
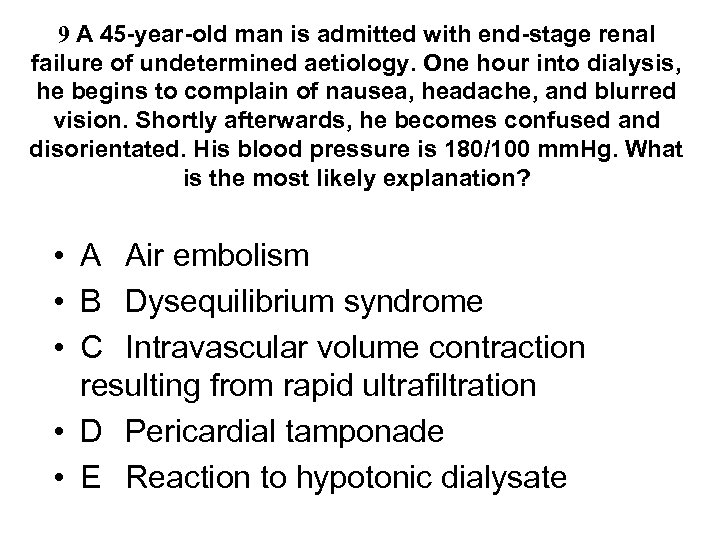 9 A 45 -year-old man is admitted with end-stage renal failure of undetermined aetiology. One hour into dialysis, he begins to complain of nausea, headache, and blurred vision. Shortly afterwards, he becomes confused and disorientated. His blood pressure is 180/100 mm. Hg. What is the most likely explanation? • A Air embolism • B Dysequilibrium syndrome • C Intravascular volume contraction resulting from rapid ultrafiltration • D Pericardial tamponade • E Reaction to hypotonic dialysate
9 A 45 -year-old man is admitted with end-stage renal failure of undetermined aetiology. One hour into dialysis, he begins to complain of nausea, headache, and blurred vision. Shortly afterwards, he becomes confused and disorientated. His blood pressure is 180/100 mm. Hg. What is the most likely explanation? • A Air embolism • B Dysequilibrium syndrome • C Intravascular volume contraction resulting from rapid ultrafiltration • D Pericardial tamponade • E Reaction to hypotonic dialysate
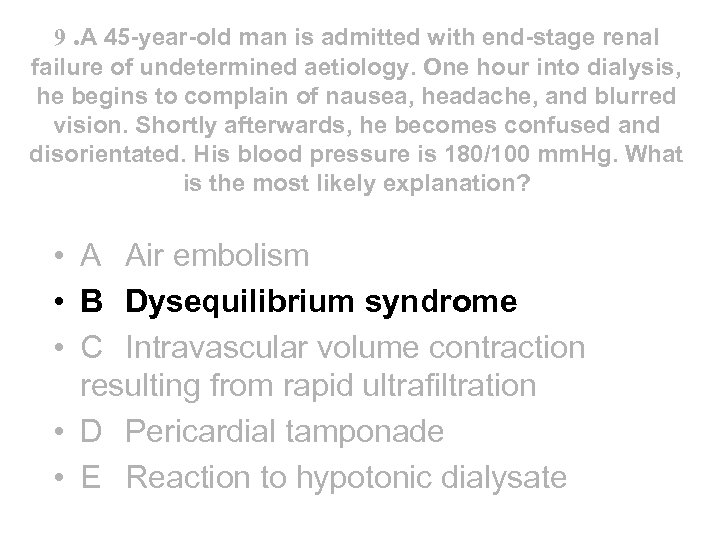 9. A 45 -year-old man is admitted with end-stage renal failure of undetermined aetiology. One hour into dialysis, he begins to complain of nausea, headache, and blurred vision. Shortly afterwards, he becomes confused and disorientated. His blood pressure is 180/100 mm. Hg. What is the most likely explanation? • A Air embolism • B Dysequilibrium syndrome • C Intravascular volume contraction resulting from rapid ultrafiltration • D Pericardial tamponade • E Reaction to hypotonic dialysate
9. A 45 -year-old man is admitted with end-stage renal failure of undetermined aetiology. One hour into dialysis, he begins to complain of nausea, headache, and blurred vision. Shortly afterwards, he becomes confused and disorientated. His blood pressure is 180/100 mm. Hg. What is the most likely explanation? • A Air embolism • B Dysequilibrium syndrome • C Intravascular volume contraction resulting from rapid ultrafiltration • D Pericardial tamponade • E Reaction to hypotonic dialysate
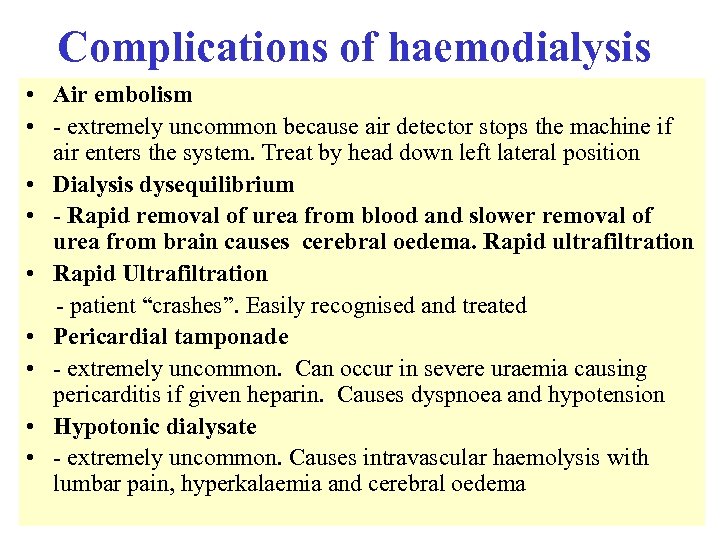 Complications of haemodialysis • Air embolism • - extremely uncommon because air detector stops the machine if air enters the system. Treat by head down left lateral position • Dialysis dysequilibrium • - Rapid removal of urea from blood and slower removal of urea from brain causes cerebral oedema. Rapid ultrafiltration • Rapid Ultrafiltration - patient “crashes”. Easily recognised and treated • Pericardial tamponade • - extremely uncommon. Can occur in severe uraemia causing pericarditis if given heparin. Causes dyspnoea and hypotension • Hypotonic dialysate • - extremely uncommon. Causes intravascular haemolysis with lumbar pain, hyperkalaemia and cerebral oedema
Complications of haemodialysis • Air embolism • - extremely uncommon because air detector stops the machine if air enters the system. Treat by head down left lateral position • Dialysis dysequilibrium • - Rapid removal of urea from blood and slower removal of urea from brain causes cerebral oedema. Rapid ultrafiltration • Rapid Ultrafiltration - patient “crashes”. Easily recognised and treated • Pericardial tamponade • - extremely uncommon. Can occur in severe uraemia causing pericarditis if given heparin. Causes dyspnoea and hypotension • Hypotonic dialysate • - extremely uncommon. Causes intravascular haemolysis with lumbar pain, hyperkalaemia and cerebral oedema
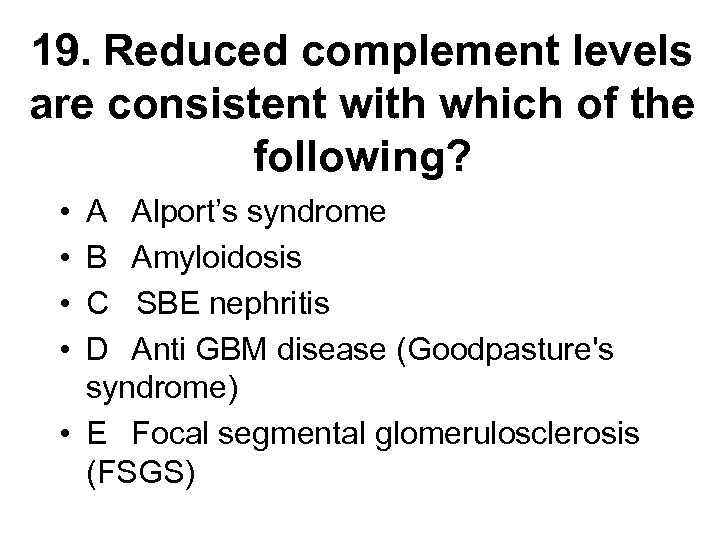 19. Reduced complement levels are consistent with which of the following? • • A Alport’s syndrome B Amyloidosis C SBE nephritis D Anti GBM disease (Goodpasture's syndrome) • E Focal segmental glomerulosclerosis (FSGS)
19. Reduced complement levels are consistent with which of the following? • • A Alport’s syndrome B Amyloidosis C SBE nephritis D Anti GBM disease (Goodpasture's syndrome) • E Focal segmental glomerulosclerosis (FSGS)
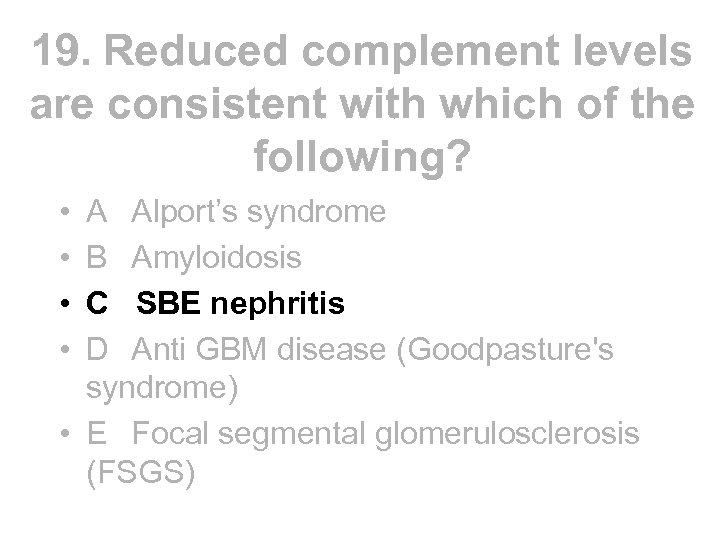 19. Reduced complement levels are consistent with which of the following? • • A Alport’s syndrome B Amyloidosis C SBE nephritis D Anti GBM disease (Goodpasture's syndrome) • E Focal segmental glomerulosclerosis (FSGS)
19. Reduced complement levels are consistent with which of the following? • • A Alport’s syndrome B Amyloidosis C SBE nephritis D Anti GBM disease (Goodpasture's syndrome) • E Focal segmental glomerulosclerosis (FSGS)
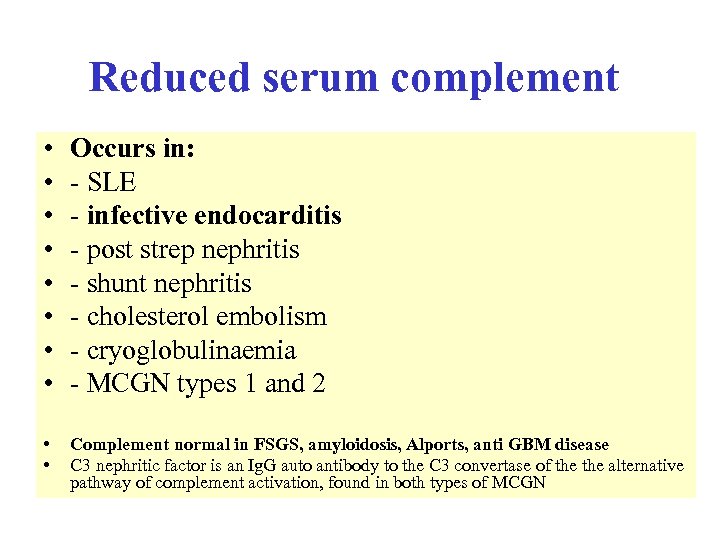 Reduced serum complement • • Occurs in: - SLE - infective endocarditis - post strep nephritis - shunt nephritis - cholesterol embolism - cryoglobulinaemia - MCGN types 1 and 2 • • Complement normal in FSGS, amyloidosis, Alports, anti GBM disease C 3 nephritic factor is an Ig. G auto antibody to the C 3 convertase of the alternative pathway of complement activation, found in both types of MCGN
Reduced serum complement • • Occurs in: - SLE - infective endocarditis - post strep nephritis - shunt nephritis - cholesterol embolism - cryoglobulinaemia - MCGN types 1 and 2 • • Complement normal in FSGS, amyloidosis, Alports, anti GBM disease C 3 nephritic factor is an Ig. G auto antibody to the C 3 convertase of the alternative pathway of complement activation, found in both types of MCGN


