cc89b2cb72a7eef1e479313f9b1ab4ed.ppt
- Количество слайдов: 34
Outcome-based research in Obstetric simulation Dr Jo Crofts Academic Clinical Lecturer in Obstetrics University of Bristol, UK
Outline • Why simulation training is required • 9 years of progress • Simulation and clinical outcomes • Characteristics of effective training • Outcome based research is required • Future of obstetric simulation
Childbirth is dangerous 1000 women die every day due to pregnancy and childbirth complications that ‘could have been prevented’
The Safety Problem • 1 : 12 labours associated with adverse outcomes Nielsen P at al, Obstet Gynecol 2007 • 50% adverse outcomes preventable with better care CESDI – 4 th Annual Report. 1997 CEMD – Why Mothers Die. 1998 CEMACH – Saving Mothers Lives 2007
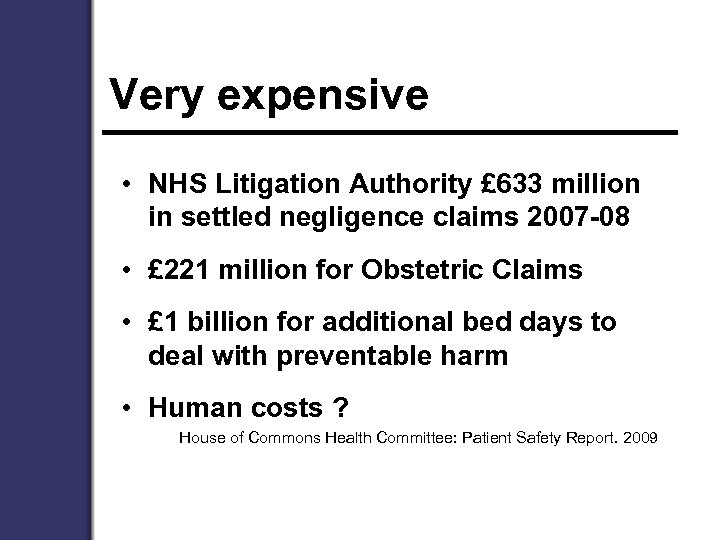
Very expensive • NHS Litigation Authority £ 633 million in settled negligence claims 2007 -08 • £ 221 million for Obstetric Claims • £ 1 billion for additional bed days to deal with preventable harm • Human costs ? House of Commons Health Committee: Patient Safety Report. 2009
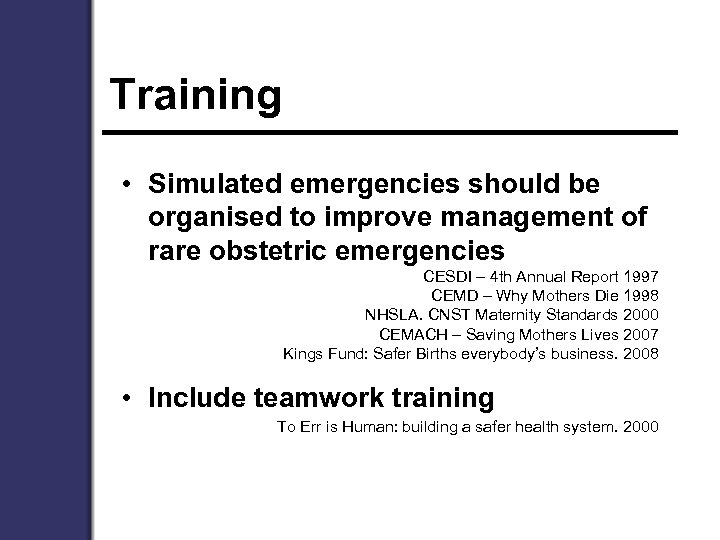
Training • Simulated emergencies should be organised to improve management of rare obstetric emergencies CESDI – 4 th Annual Report 1997 CEMD – Why Mothers Die 1998 NHSLA. CNST Maternity Standards 2000 CEMACH – Saving Mothers Lives 2007 Kings Fund: Safer Births everybody’s business. 2008 • Include teamwork training To Err is Human: building a safer health system. 2000
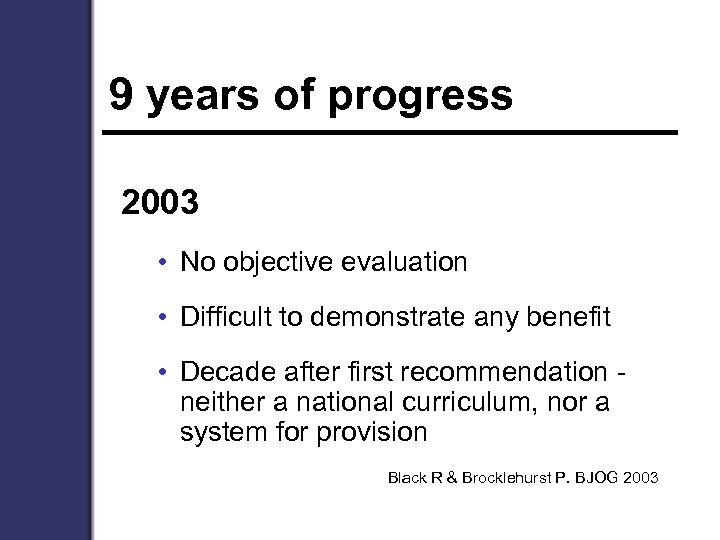
9 years of progress 2003 • No objective evaluation • Difficult to demonstrate any benefit • Decade after first recommendation neither a national curriculum, nor a system for provision Black R & Brocklehurst P. BJOG 2003
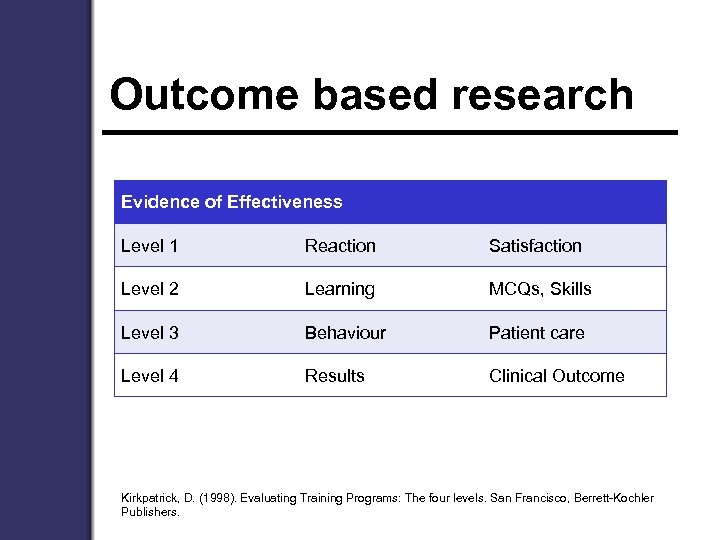
Outcome based research Evidence of Effectiveness Level 1 Reaction Satisfaction Level 2 Learning MCQs, Skills Level 3 Behaviour Patient care Level 4 Results Clinical Outcome Kirkpatrick, D. (1998). Evaluating Training Programs: The four levels. San Francisco, Berrett-Kochler Publishers.
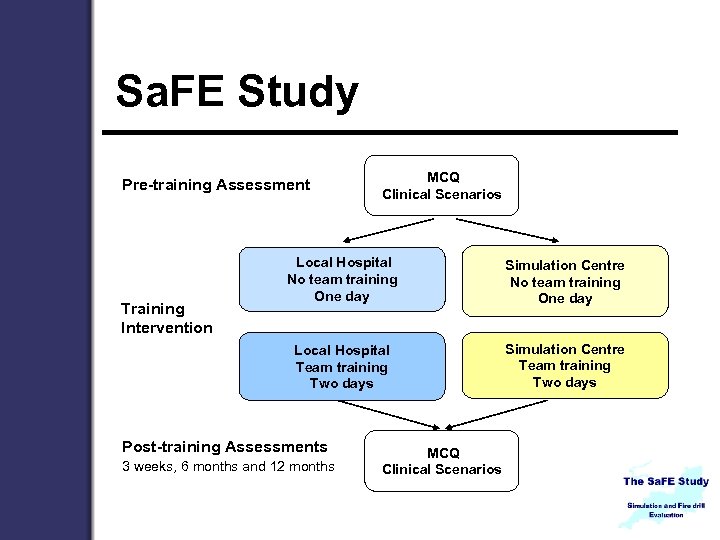
Sa. FE Study Pre-training Assessment MCQ Clinical Scenarios Simulation Centre No team training One day Local Hospital Team training Two days Training Intervention Local Hospital No team training One day Simulation Centre Team training Two days Post-training Assessments 3 weeks, 6 months and 12 months MCQ Clinical Scenarios
Knowledge Summary • Significant increase in knowledge following training • 93% increased MCQ score • Knowledge at 6 & 12 months was significantly higher than pre-training • None of the training interventions appeared to be superior Crofts, J. , D. Ellis, et al. (2007). "Change in knowledge of midwives and obstetricians following obstetric emergency training: a randomised controlled trial of local hospital, simulation centre and teamwork training. " BJOG: An International Journal of Obstetrics and Gynaecology 114(12): 1534 -1541.
Eclampsia • 140 staff randomised to training on patient-actor or whole body simulator • Following training • completion of basic tasks (87% to 100%) • administration of Mg. SO 4 (61% to 92%) • medication given 2 minutes earlier • No differences in training style except improved communication with actress Ellis et al. (2008). "Hospital, Simulation Center, and Teamwork Training for Eclampsia Management: A Randomized Controlled Trial. " Obstet Gynecol 111(3): 723 -731.
Shoulder Dystocia
Simulation of SD
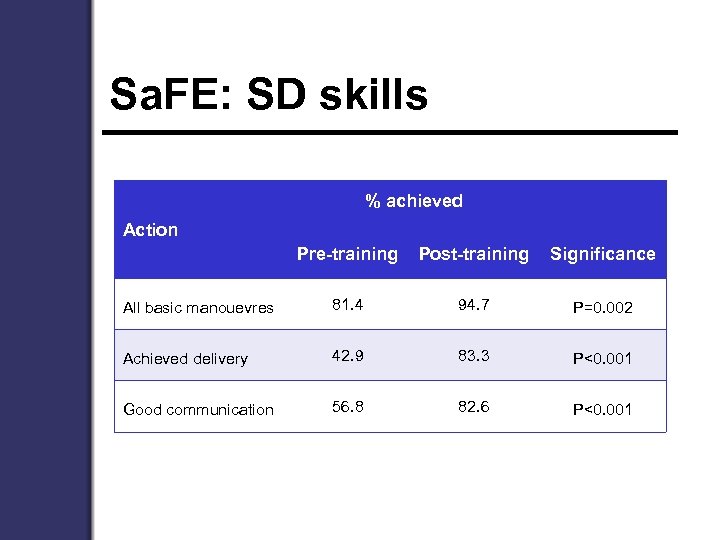
Sa. FE: SD skills % achieved Action Pre-training Post-training Significance All basic manouevres 81. 4 94. 7 P=0. 002 Achieved delivery 42. 9 83. 3 P<0. 001 Good communication 56. 8 82. 6 P<0. 001
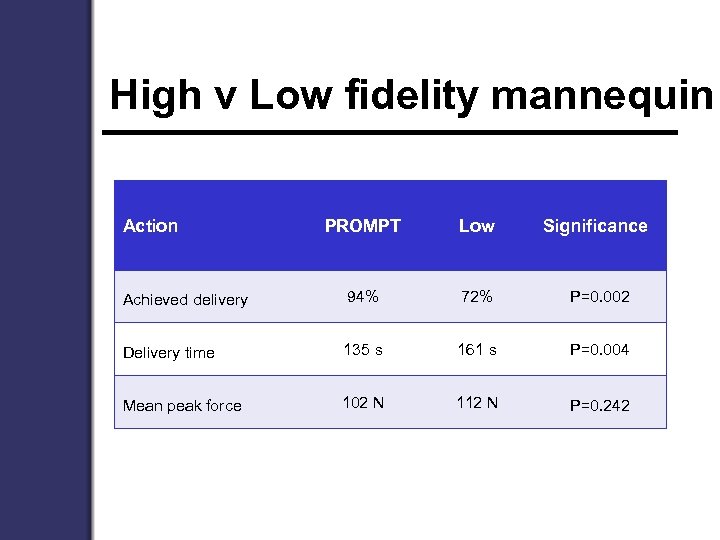
High v Low fidelity mannequin Action PROMPT Low Significance Achieved delivery 94% 72% P=0. 002 Delivery time 135 s 161 s P=0. 004 Mean peak force 102 N 112 N P=0. 242
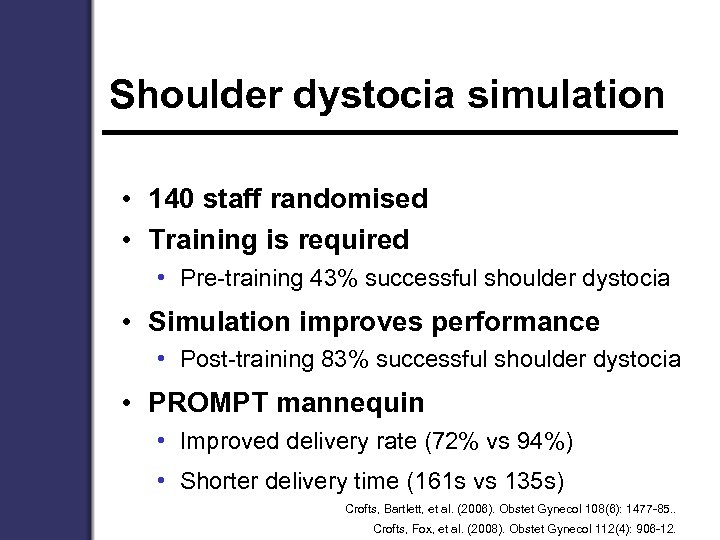
Shoulder dystocia simulation • 140 staff randomised • Training is required • Pre-training 43% successful shoulder dystocia • Simulation improves performance • Post-training 83% successful shoulder dystocia • PROMPT mannequin • Improved delivery rate (72% vs 94%) • Shorter delivery time (161 s vs 135 s) Crofts, Bartlett, et al. (2006). Obstet Gynecol 108(6): 1477 -85. . Crofts, Fox, et al. (2008). Obstet Gynecol 112(4): 906 -12.



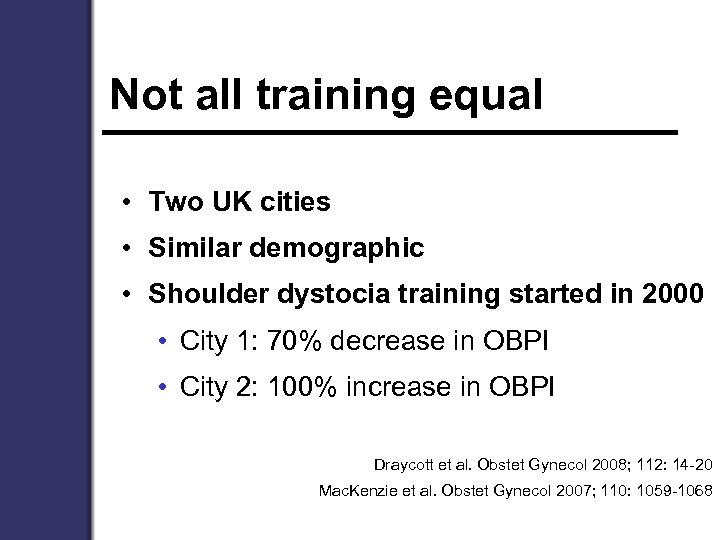
Not all training equal • Two UK cities • Similar demographic • Shoulder dystocia training started in 2000 • City 1: 70% decrease in OBPI • City 2: 100% increase in OBPI Draycott et al. Obstet Gynecol 2008; 112: 14 -20 Mac. Kenzie et al. Obstet Gynecol 2007; 110: 1059 -1068
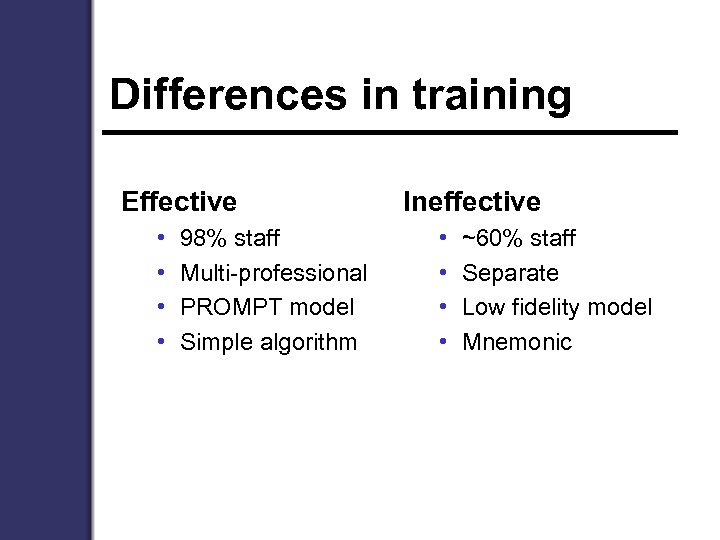
Differences in training Effective • • 98% staff Multi-professional PROMPT model Simple algorithm Ineffective • • ~60% staff Separate Low fidelity model Mnemonic

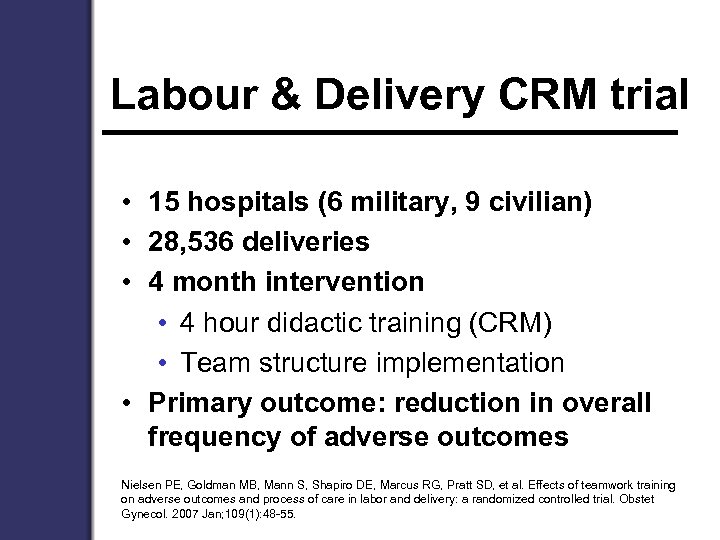
Labour & Delivery CRM trial • 15 hospitals (6 military, 9 civilian) • 28, 536 deliveries • 4 month intervention • 4 hour didactic training (CRM) • Team structure implementation • Primary outcome: reduction in overall frequency of adverse outcomes Nielsen PE, Goldman MB, Mann S, Shapiro DE, Marcus RG, Pratt SD, et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial. Obstet Gynecol. 2007 Jan; 109(1): 48 -55.
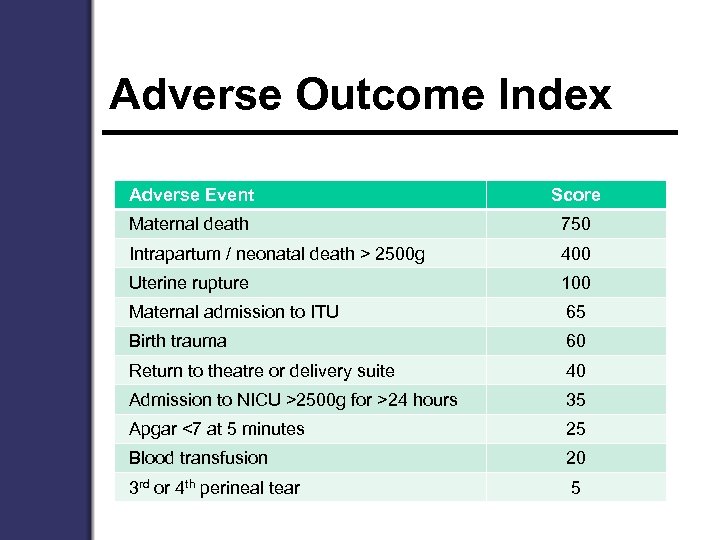
Adverse Outcome Index Adverse Event Score Maternal death 750 Intrapartum / neonatal death > 2500 g 400 Uterine rupture 100 Maternal admission to ITU 65 Birth trauma 60 Return to theatre or delivery suite 40 Admission to NICU >2500 g for >24 hours 35 Apgar <7 at 5 minutes 25 Blood transfusion 20 3 rd or 4 th perineal tear 5
Labour & Delivery CRM trial • No difference in adverse outcomes (both groups improved) • Problems • CRM does not work / as implemented ? • Short implementation period • Wrong measures ? • Hawthorne effect ? • Underpowered ?
Nine years of progress • What works • Where • Why • What next……?
Common Effective Themes • Simulation of emergencies • High fidelity training tools • Situated ‘Local’ training • Nearly 100% staff • Multi-professional • Insurance based financial incentives Siassakos, Crofts, et al. (2009). "The active components of effective training in obstetric emergencies. " Bjog 116(8): 1028 -32.
Does Simulation work ? Yes (Some, but not all) Increasing retrospective data suggesting improvements in neonatal outcome after the introduction of simulation training
Can we do better ? Yes Increasing retrospective data suggesting improvements in neonatal outcome after the introduction of simulation training
Nine year vision • Effective evidenced based training to reduce preventable harm • All staff • All mothers & babies • Improved training materials • Commit to more, and better research for the future • Prospective • Hard clinical outcomes

The Future • Whole body mannequins • Sepsis • Maternal collapse • Virtual reality • Instrumental delivery
The Future • Accessible training • Simple training aids
Simulation training is required • 1000 women die every day due to pregnancy and childbirth complications that ‘could have been prevented’ • Almost all of them (99%) live and die in developing countries World Health Organisation
Thank you • jo. crofts@bristol. ac. uk
cc89b2cb72a7eef1e479313f9b1ab4ed.ppt