d9a540947c982444bcb7977b79425d16.ppt
- Количество слайдов: 32
 Otitis Media Epidemiology and Drug-Resistant Streptococcus pneumoniae G. Scott Giebink, M. D. Professor of Pediatrics and Otolaryngology Director, Otitis Media Research Center University of Minnesota School of Medicine
Otitis Media Epidemiology and Drug-Resistant Streptococcus pneumoniae G. Scott Giebink, M. D. Professor of Pediatrics and Otolaryngology Director, Otitis Media Research Center University of Minnesota School of Medicine
 Acute Otitis Media in the US > 24 million acute otitis media office visits per year (1) § ~ 80% of children in the US have at least 1 episode of otitis media by age 3 (2) § ~ 50% have > 3 episodes by age 3 (2) § ~ 7– 12 million cases are caused by S. pneumoniae (1) Giebink – FDA – 01/2001 (1) MMWR. 1997; 46: 1 -24 (2) Teele DW et al. J Infect Dis. 1989; 160: 83 -94
Acute Otitis Media in the US > 24 million acute otitis media office visits per year (1) § ~ 80% of children in the US have at least 1 episode of otitis media by age 3 (2) § ~ 50% have > 3 episodes by age 3 (2) § ~ 7– 12 million cases are caused by S. pneumoniae (1) Giebink – FDA – 01/2001 (1) MMWR. 1997; 46: 1 -24 (2) Teele DW et al. J Infect Dis. 1989; 160: 83 -94
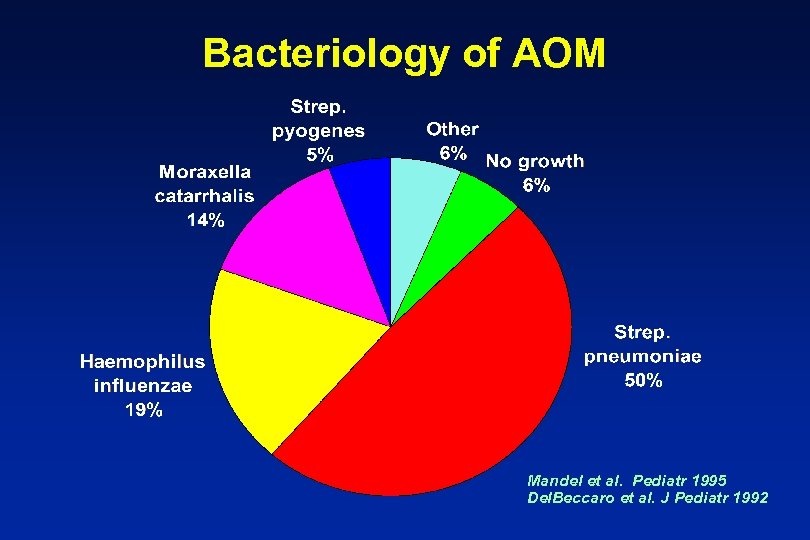 Bacteriology of AOM Mandel et al. Pediatr 1995 Del. Beccaro et al. J Pediatr 1992
Bacteriology of AOM Mandel et al. Pediatr 1995 Del. Beccaro et al. J Pediatr 1992
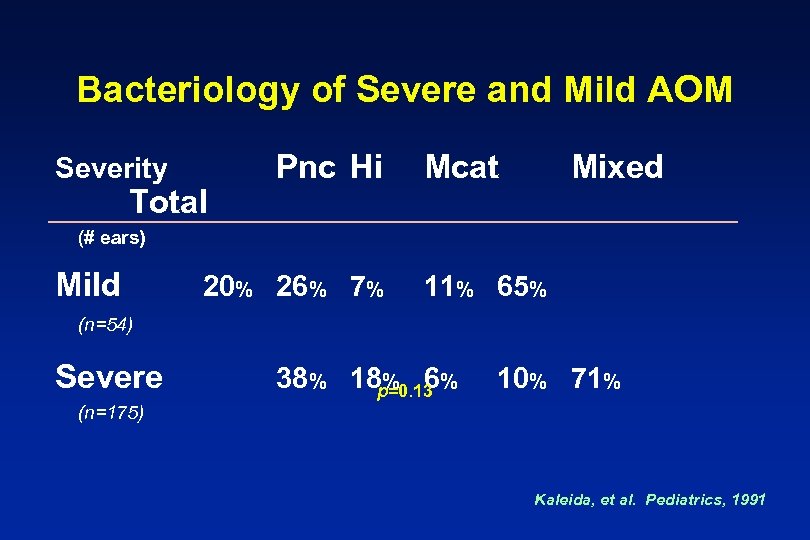 Bacteriology of Severe and Mild AOM Severity Total Pnc Hi Mcat Mixed (# ears) Mild 20% 26% 7% 11% 65% (n=54) Severe 38% 18 p=0. 13 % % 6 10% 71% (n=175) Kaleida, et al. Pediatrics, 1991
Bacteriology of Severe and Mild AOM Severity Total Pnc Hi Mcat Mixed (# ears) Mild 20% 26% 7% 11% 65% (n=54) Severe 38% 18 p=0. 13 % % 6 10% 71% (n=175) Kaleida, et al. Pediatrics, 1991
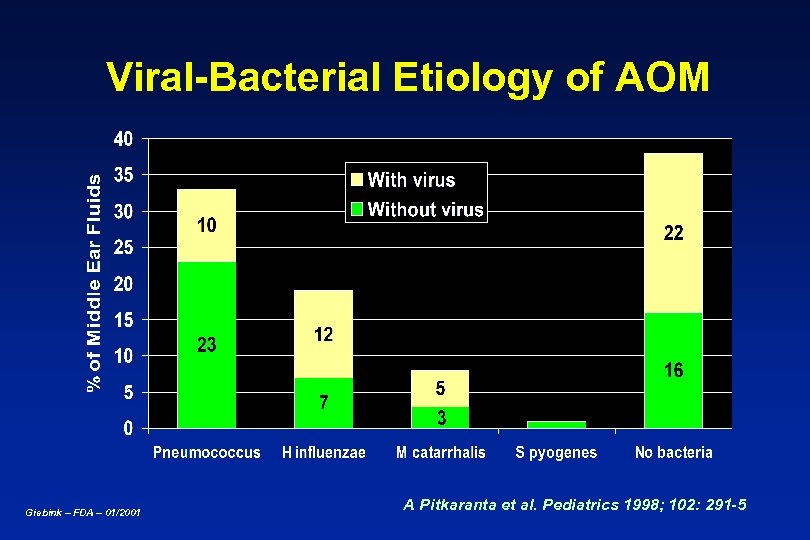 Viral-Bacterial Etiology of AOM Giebink – FDA – 01/2001 A Pitkaranta et al. Pediatrics 1998; 102: 291 -5
Viral-Bacterial Etiology of AOM Giebink – FDA – 01/2001 A Pitkaranta et al. Pediatrics 1998; 102: 291 -5
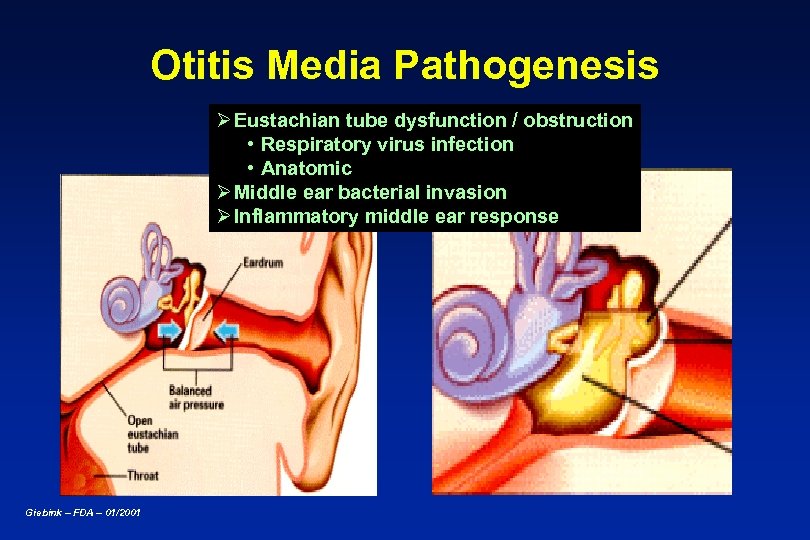 Otitis Media Pathogenesis Ø Eustachian tube dysfunction / obstruction • Respiratory virus infection • Anatomic Ø Middle ear bacterial invasion Ø Inflammatory middle ear response Giebink – FDA – 01/2001
Otitis Media Pathogenesis Ø Eustachian tube dysfunction / obstruction • Respiratory virus infection • Anatomic Ø Middle ear bacterial invasion Ø Inflammatory middle ear response Giebink – FDA – 01/2001
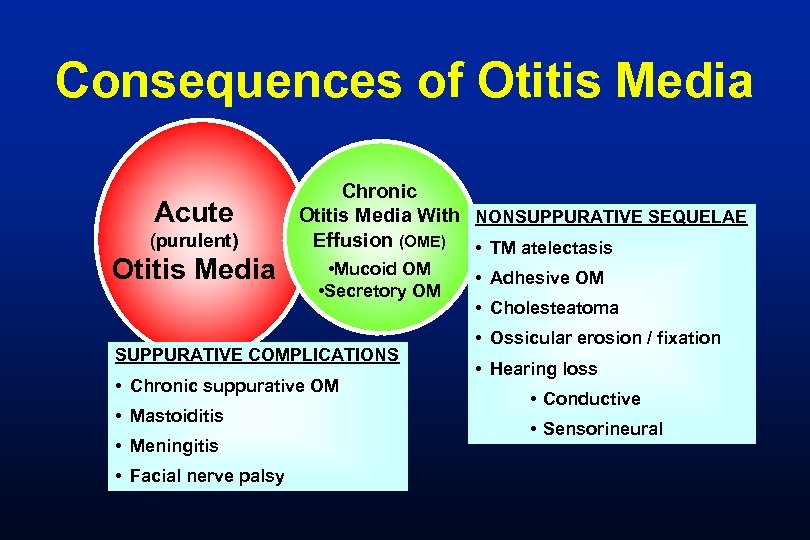 Consequences of Otitis Media Acute (purulent) Otitis Media Chronic Otitis Media With NONSUPPURATIVE SEQUELAE Effusion (OME) • TM atelectasis • Mucoid OM • Secretory OM SUPPURATIVE COMPLICATIONS • Chronic suppurative OM • Mastoiditis • Meningitis • Facial nerve palsy • Adhesive OM • Cholesteatoma • Ossicular erosion / fixation • Hearing loss • Conductive • Sensorineural
Consequences of Otitis Media Acute (purulent) Otitis Media Chronic Otitis Media With NONSUPPURATIVE SEQUELAE Effusion (OME) • TM atelectasis • Mucoid OM • Secretory OM SUPPURATIVE COMPLICATIONS • Chronic suppurative OM • Mastoiditis • Meningitis • Facial nerve palsy • Adhesive OM • Cholesteatoma • Ossicular erosion / fixation • Hearing loss • Conductive • Sensorineural
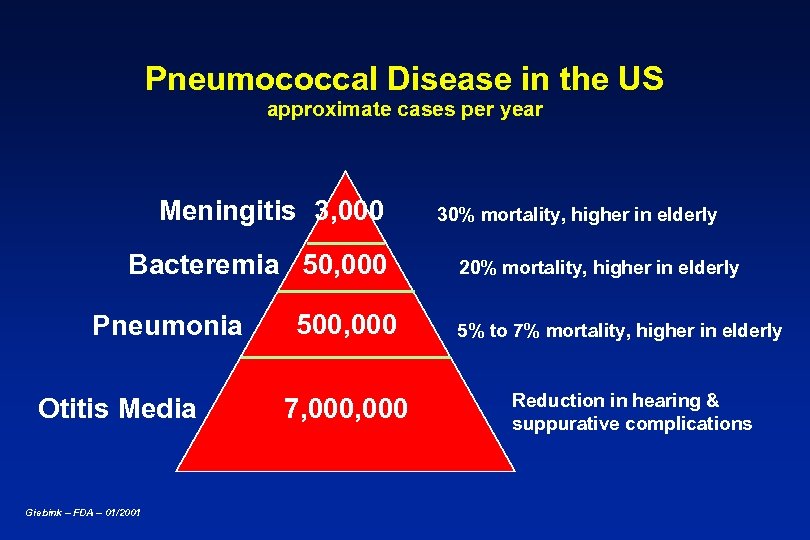 Pneumococcal Disease in the US approximate cases per year Meningitis 3, 000 Bacteremia 50, 000 Pneumonia Otitis Media Giebink – FDA – 01/2001 500, 000 7, 000 30% mortality, higher in elderly 20% mortality, higher in elderly 5% to 7% mortality, higher in elderly Reduction in hearing & suppurative complications
Pneumococcal Disease in the US approximate cases per year Meningitis 3, 000 Bacteremia 50, 000 Pneumonia Otitis Media Giebink – FDA – 01/2001 500, 000 7, 000 30% mortality, higher in elderly 20% mortality, higher in elderly 5% to 7% mortality, higher in elderly Reduction in hearing & suppurative complications
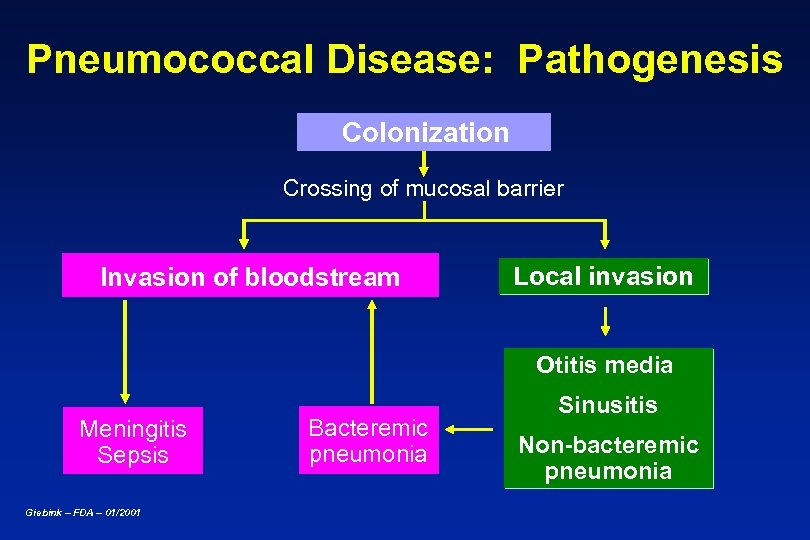 Pneumococcal Disease: Pathogenesis Colonization Crossing of mucosal barrier Invasion of bloodstream Local invasion Otitis media Meningitis Sepsis Giebink – FDA – 01/2001 Bacteremic pneumonia Sinusitis Non-bacteremic pneumonia
Pneumococcal Disease: Pathogenesis Colonization Crossing of mucosal barrier Invasion of bloodstream Local invasion Otitis media Meningitis Sepsis Giebink – FDA – 01/2001 Bacteremic pneumonia Sinusitis Non-bacteremic pneumonia
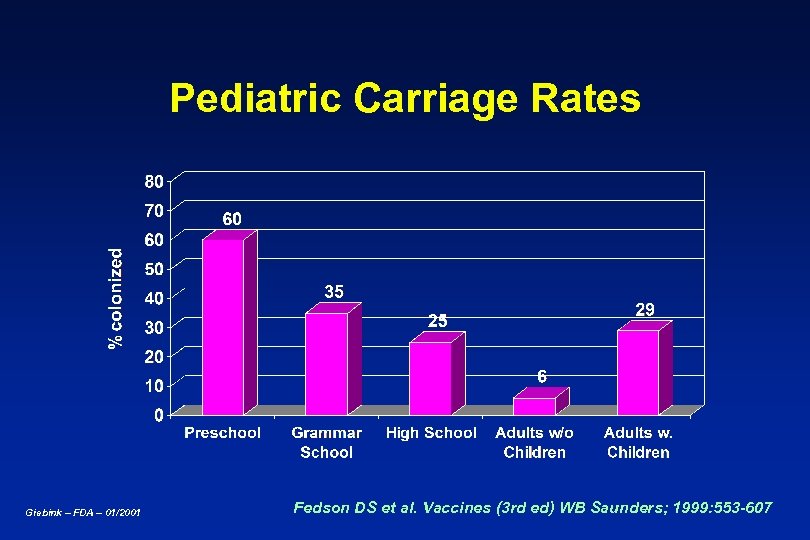 Pediatric Carriage Rates Giebink – FDA – 01/2001 Fedson DS et al. Vaccines (3 rd ed) WB Saunders; 1999: 553 -607
Pediatric Carriage Rates Giebink – FDA – 01/2001 Fedson DS et al. Vaccines (3 rd ed) WB Saunders; 1999: 553 -607
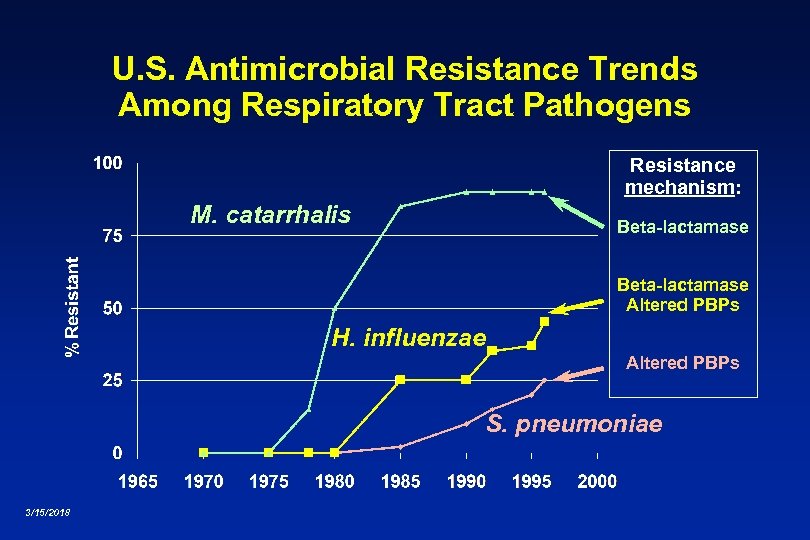 U. S. Antimicrobial Resistance Trends Among Respiratory Tract Pathogens Resistance mechanism: M. catarrhalis Beta-lactamase Altered PBPs H. influenzae Altered PBPs S. pneumoniae 3/15/2018
U. S. Antimicrobial Resistance Trends Among Respiratory Tract Pathogens Resistance mechanism: M. catarrhalis Beta-lactamase Altered PBPs H. influenzae Altered PBPs S. pneumoniae 3/15/2018
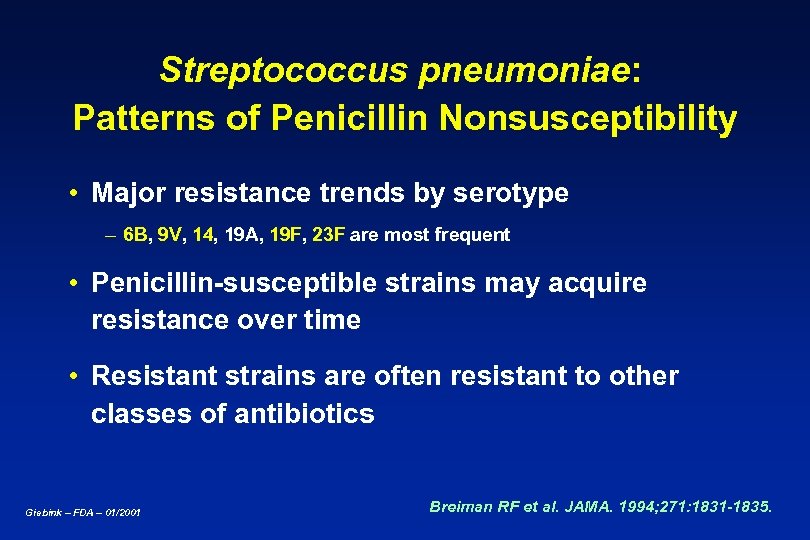 Streptococcus pneumoniae: Patterns of Penicillin Nonsusceptibility • Major resistance trends by serotype – 6 B, 9 V, 14, 19 A, 19 F, 23 F are most frequent • Penicillin-susceptible strains may acquire resistance over time • Resistant strains are often resistant to other classes of antibiotics Giebink – FDA – 01/2001 Breiman RF et al. JAMA. 1994; 271: 1831 -1835.
Streptococcus pneumoniae: Patterns of Penicillin Nonsusceptibility • Major resistance trends by serotype – 6 B, 9 V, 14, 19 A, 19 F, 23 F are most frequent • Penicillin-susceptible strains may acquire resistance over time • Resistant strains are often resistant to other classes of antibiotics Giebink – FDA – 01/2001 Breiman RF et al. JAMA. 1994; 271: 1831 -1835.
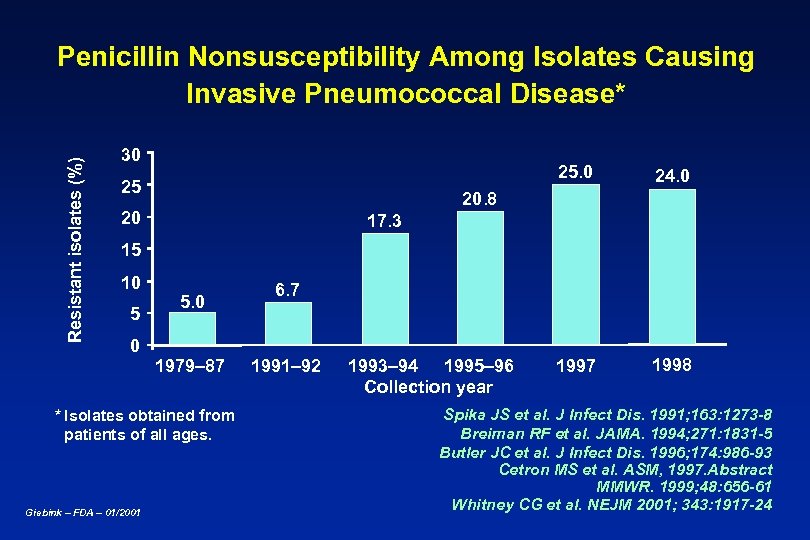 Resistant isolates (%) Penicillin Nonsusceptibility Among Isolates Causing Invasive Pneumococcal Disease* 30 25 24. 0 1997 1998 20 17. 3 15 10 5 0 5. 0 1979– 87 * Isolates obtained from patients of all ages. Giebink – FDA – 01/2001 6. 7 1991– 92 1993– 94 1995– 96 Collection year Spika JS et al. J Infect Dis. 1991; 163: 1273 -8 Breiman RF et al. JAMA. 1994; 271: 1831 -5 Butler JC et al. J Infect Dis. 1996; 174: 986 -93 Cetron MS et al. ASM, 1997. Abstract MMWR. 1999; 48: 656 -61 Whitney CG et al. NEJM 2001; 343: 1917 -24
Resistant isolates (%) Penicillin Nonsusceptibility Among Isolates Causing Invasive Pneumococcal Disease* 30 25 24. 0 1997 1998 20 17. 3 15 10 5 0 5. 0 1979– 87 * Isolates obtained from patients of all ages. Giebink – FDA – 01/2001 6. 7 1991– 92 1993– 94 1995– 96 Collection year Spika JS et al. J Infect Dis. 1991; 163: 1273 -8 Breiman RF et al. JAMA. 1994; 271: 1831 -5 Butler JC et al. J Infect Dis. 1996; 174: 986 -93 Cetron MS et al. ASM, 1997. Abstract MMWR. 1999; 48: 656 -61 Whitney CG et al. NEJM 2001; 343: 1917 -24
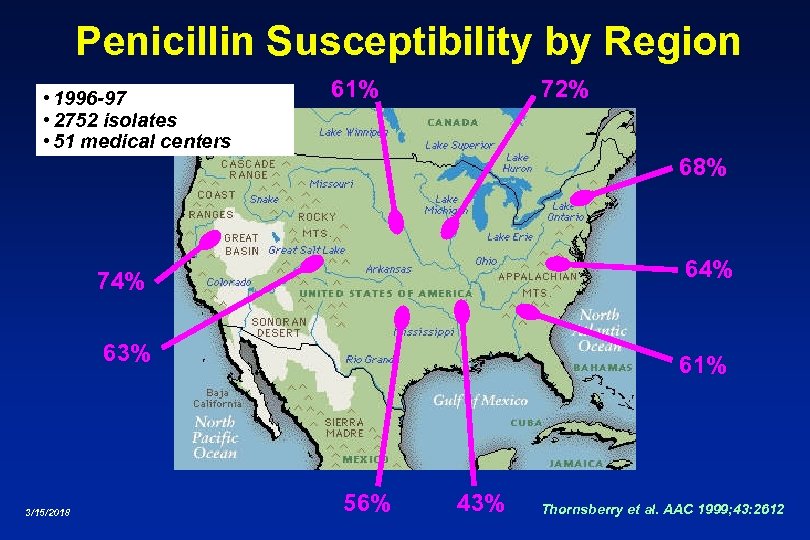 Penicillin Susceptibility by Region • 1996 -97 • 2752 isolates • 51 medical centers 61% 72% 68% 64% 74% 63% 3/15/2018 61% 56% 43% Thornsberry et al. AAC 1999; 43: 2612
Penicillin Susceptibility by Region • 1996 -97 • 2752 isolates • 51 medical centers 61% 72% 68% 64% 74% 63% 3/15/2018 61% 56% 43% Thornsberry et al. AAC 1999; 43: 2612
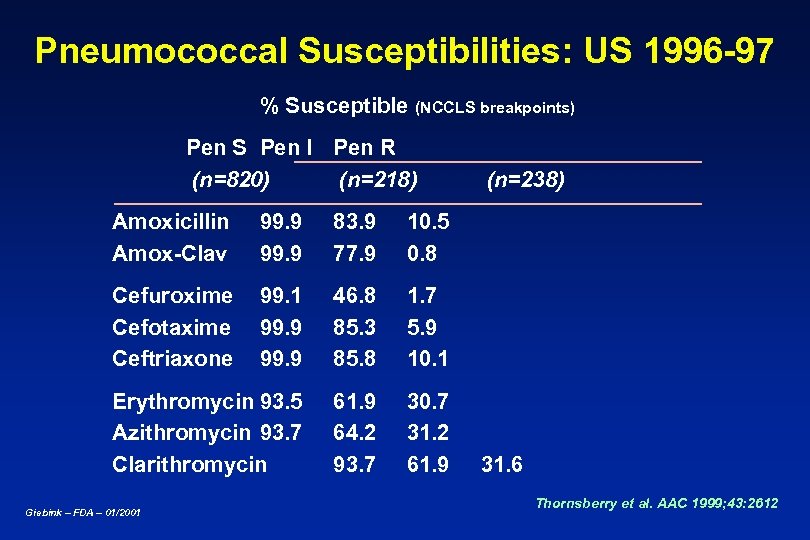 Pneumococcal Susceptibilities: US 1996 -97 % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=820) (n=218) Amoxicillin Amox-Clav 99. 9 83. 9 77. 9 10. 5 0. 8 Cefuroxime Cefotaxime Ceftriaxone 99. 1 99. 9 46. 8 85. 3 85. 8 1. 7 5. 9 10. 1 Erythromycin 93. 5 Azithromycin 93. 7 Clarithromycin 61. 9 64. 2 93. 7 30. 7 31. 2 61. 9 (n=238) Giebink – FDA – 01/2001 31. 6 Thornsberry et al. AAC 1999; 43: 2612
Pneumococcal Susceptibilities: US 1996 -97 % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=820) (n=218) Amoxicillin Amox-Clav 99. 9 83. 9 77. 9 10. 5 0. 8 Cefuroxime Cefotaxime Ceftriaxone 99. 1 99. 9 46. 8 85. 3 85. 8 1. 7 5. 9 10. 1 Erythromycin 93. 5 Azithromycin 93. 7 Clarithromycin 61. 9 64. 2 93. 7 30. 7 31. 2 61. 9 (n=238) Giebink – FDA – 01/2001 31. 6 Thornsberry et al. AAC 1999; 43: 2612
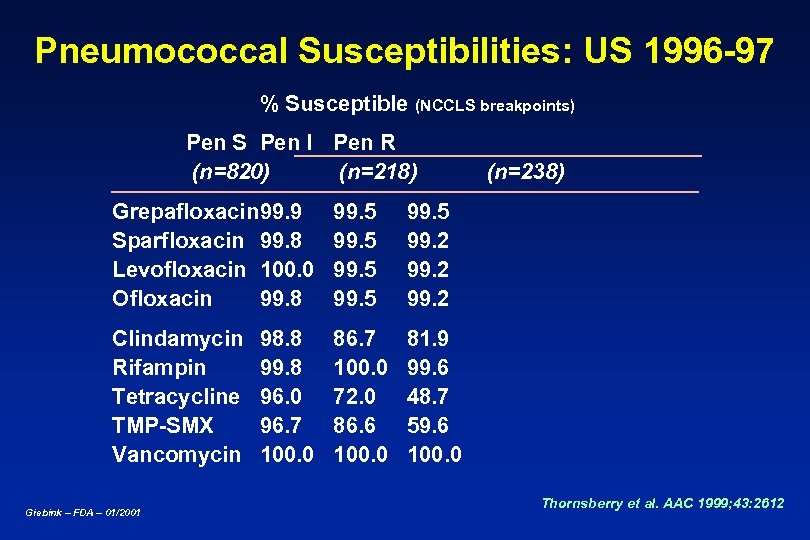 Pneumococcal Susceptibilities: US 1996 -97 % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=820) (n=218) Grepafloxacin 99. 9 Sparfloxacin 99. 8 Levofloxacin 100. 0 Ofloxacin 99. 8 99. 5 99. 2 Clindamycin Rifampin Tetracycline TMP-SMX Vancomycin 86. 7 100. 0 72. 0 86. 6 100. 0 (n=238) 81. 9 99. 6 48. 7 59. 6 100. 0 Giebink – FDA – 01/2001 98. 8 99. 8 96. 0 96. 7 100. 0 Thornsberry et al. AAC 1999; 43: 2612
Pneumococcal Susceptibilities: US 1996 -97 % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=820) (n=218) Grepafloxacin 99. 9 Sparfloxacin 99. 8 Levofloxacin 100. 0 Ofloxacin 99. 8 99. 5 99. 2 Clindamycin Rifampin Tetracycline TMP-SMX Vancomycin 86. 7 100. 0 72. 0 86. 6 100. 0 (n=238) 81. 9 99. 6 48. 7 59. 6 100. 0 Giebink – FDA – 01/2001 98. 8 99. 8 96. 0 96. 7 100. 0 Thornsberry et al. AAC 1999; 43: 2612
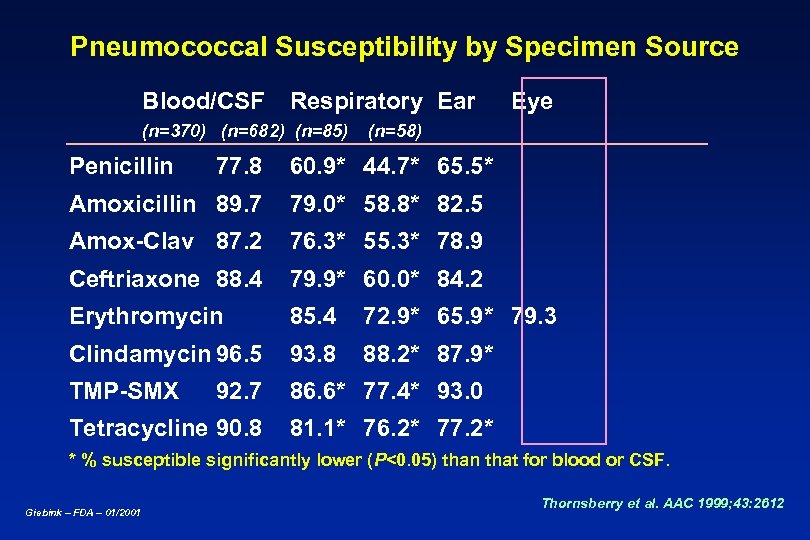 Pneumococcal Susceptibility by Specimen Source Blood/CSF Respiratory Ear (n=370) (n=682) (n=85) Penicillin 77. 8 Eye (n=58) 60. 9* 44. 7* 65. 5* Amoxicillin 89. 7 79. 0* 58. 8* 82. 5 Amox-Clav 87. 2 76. 3* 55. 3* 78. 9 Ceftriaxone 88. 4 79. 9* 60. 0* 84. 2 Erythromycin 85. 4 72. 9* 65. 9* 79. 3 Clindamycin 96. 5 93. 8 88. 2* 87. 9* TMP-SMX 86. 6* 77. 4* 93. 0 92. 7 Tetracycline 90. 8 81. 1* 76. 2* 77. 2* * % susceptible significantly lower (P<0. 05) than that for blood or CSF. Giebink – FDA – 01/2001 Thornsberry et al. AAC 1999; 43: 2612
Pneumococcal Susceptibility by Specimen Source Blood/CSF Respiratory Ear (n=370) (n=682) (n=85) Penicillin 77. 8 Eye (n=58) 60. 9* 44. 7* 65. 5* Amoxicillin 89. 7 79. 0* 58. 8* 82. 5 Amox-Clav 87. 2 76. 3* 55. 3* 78. 9 Ceftriaxone 88. 4 79. 9* 60. 0* 84. 2 Erythromycin 85. 4 72. 9* 65. 9* 79. 3 Clindamycin 96. 5 93. 8 88. 2* 87. 9* TMP-SMX 86. 6* 77. 4* 93. 0 92. 7 Tetracycline 90. 8 81. 1* 76. 2* 77. 2* * % susceptible significantly lower (P<0. 05) than that for blood or CSF. Giebink – FDA – 01/2001 Thornsberry et al. AAC 1999; 43: 2612
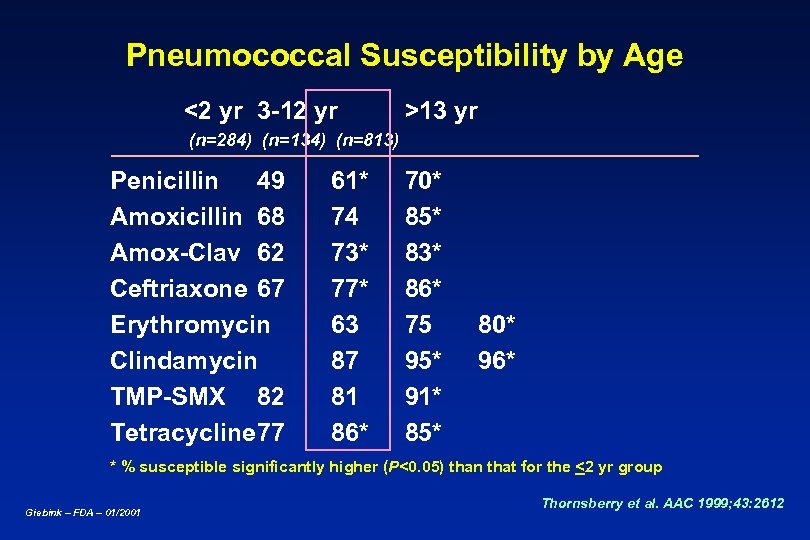 Pneumococcal Susceptibility by Age <2 yr 3 -12 yr >13 yr (n=284) (n=134) (n=813) Penicillin 49 Amoxicillin 68 Amox-Clav 62 Ceftriaxone 67 Erythromycin Clindamycin TMP-SMX 82 Tetracycline 77 61* 74 73* 77* 63 87 81 86* 70* 85* 83* 86* 75 95* 91* 85* 80* 96* * % susceptible significantly higher (P<0. 05) than that for the <2 yr group Giebink – FDA – 01/2001 Thornsberry et al. AAC 1999; 43: 2612
Pneumococcal Susceptibility by Age <2 yr 3 -12 yr >13 yr (n=284) (n=134) (n=813) Penicillin 49 Amoxicillin 68 Amox-Clav 62 Ceftriaxone 67 Erythromycin Clindamycin TMP-SMX 82 Tetracycline 77 61* 74 73* 77* 63 87 81 86* 70* 85* 83* 86* 75 95* 91* 85* 80* 96* * % susceptible significantly higher (P<0. 05) than that for the <2 yr group Giebink – FDA – 01/2001 Thornsberry et al. AAC 1999; 43: 2612
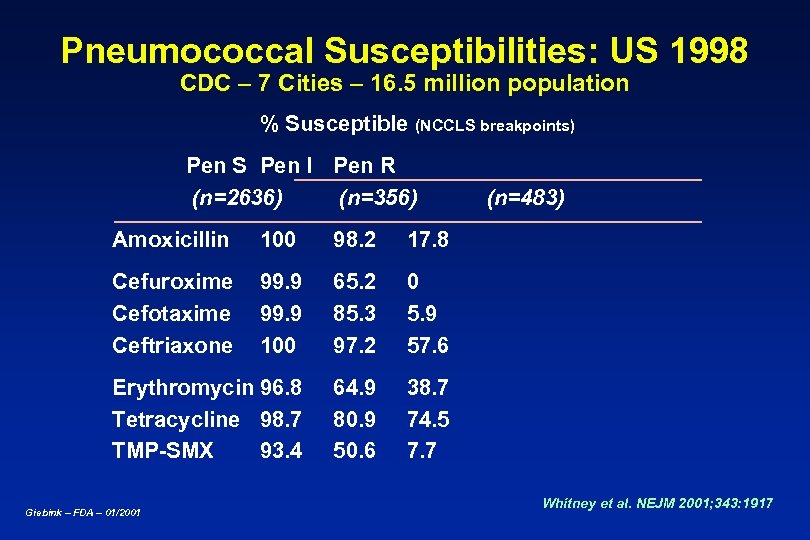 Pneumococcal Susceptibilities: US 1998 CDC – 7 Cities – 16. 5 million population % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=2636) (n=356) Amoxicillin 100 98. 2 17. 8 Cefuroxime Cefotaxime Ceftriaxone 99. 9 100 65. 2 85. 3 97. 2 0 5. 9 57. 6 Erythromycin 96. 8 Tetracycline 98. 7 TMP-SMX 93. 4 64. 9 80. 9 50. 6 (n=483) 38. 7 74. 5 7. 7 Giebink – FDA – 01/2001 Whitney et al. NEJM 2001; 343: 1917
Pneumococcal Susceptibilities: US 1998 CDC – 7 Cities – 16. 5 million population % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=2636) (n=356) Amoxicillin 100 98. 2 17. 8 Cefuroxime Cefotaxime Ceftriaxone 99. 9 100 65. 2 85. 3 97. 2 0 5. 9 57. 6 Erythromycin 96. 8 Tetracycline 98. 7 TMP-SMX 93. 4 64. 9 80. 9 50. 6 (n=483) 38. 7 74. 5 7. 7 Giebink – FDA – 01/2001 Whitney et al. NEJM 2001; 343: 1917
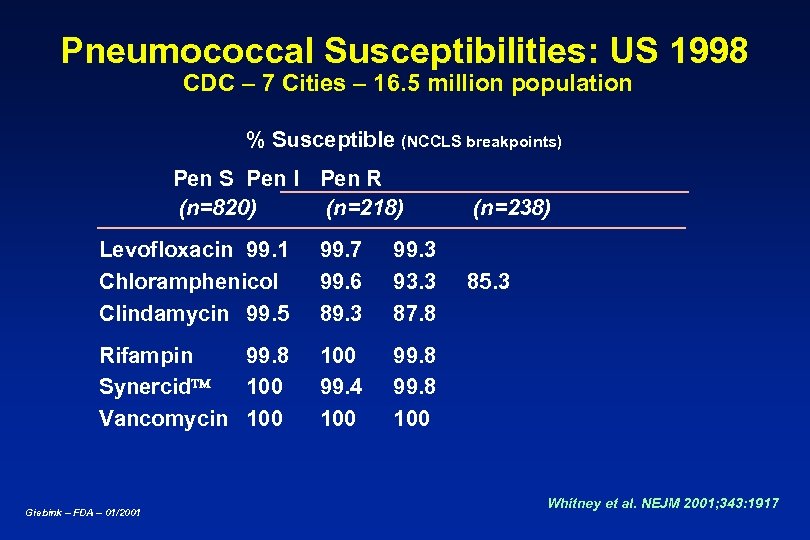 Pneumococcal Susceptibilities: US 1998 CDC – 7 Cities – 16. 5 million population % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=820) (n=218) Levofloxacin 99. 1 Chloramphenicol Clindamycin 99. 5 99. 7 99. 6 89. 3 93. 3 87. 8 Rifampin 99. 8 Synercid 100 Vancomycin 100 99. 4 100 (n=238) 99. 8 100 Giebink – FDA – 01/2001 85. 3 Whitney et al. NEJM 2001; 343: 1917
Pneumococcal Susceptibilities: US 1998 CDC – 7 Cities – 16. 5 million population % Susceptible (NCCLS breakpoints) Pen S Pen I Pen R (n=820) (n=218) Levofloxacin 99. 1 Chloramphenicol Clindamycin 99. 5 99. 7 99. 6 89. 3 93. 3 87. 8 Rifampin 99. 8 Synercid 100 Vancomycin 100 99. 4 100 (n=238) 99. 8 100 Giebink – FDA – 01/2001 85. 3 Whitney et al. NEJM 2001; 343: 1917
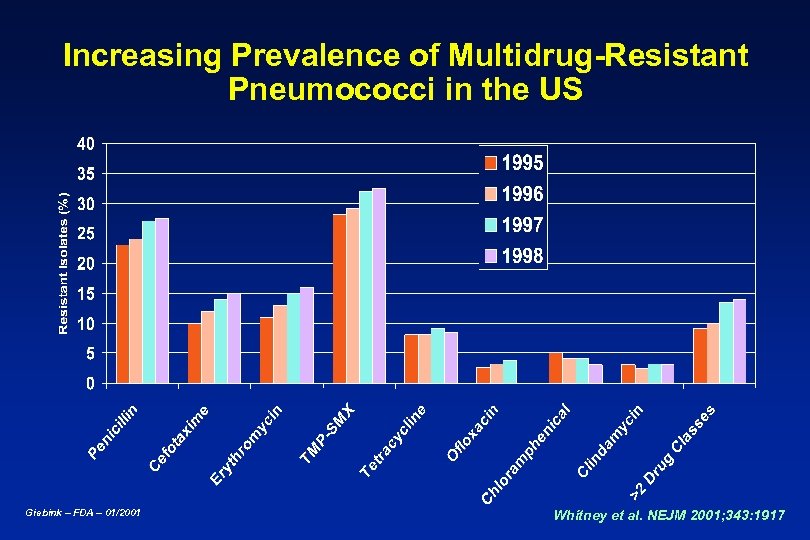 Increasing Prevalence of Multidrug-Resistant Pneumococci in the US Giebink – FDA – 01/2001 Whitney et al. NEJM 2001; 343: 1917
Increasing Prevalence of Multidrug-Resistant Pneumococci in the US Giebink – FDA – 01/2001 Whitney et al. NEJM 2001; 343: 1917
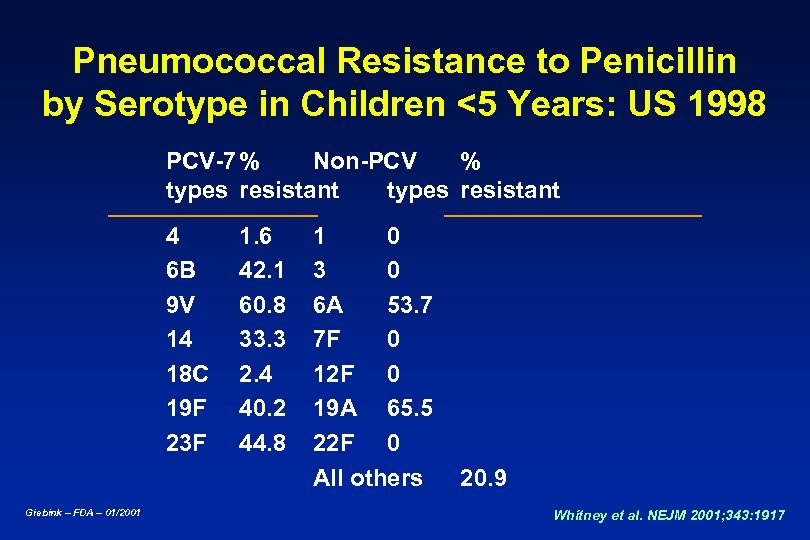 Pneumococcal Resistance to Penicillin by Serotype in Children <5 Years: US 1998 PCV-7 % Non-PCV % types resistant 4 6 B 9 V 14 18 C 19 F 23 F Giebink – FDA – 01/2001 1. 6 42. 1 60. 8 33. 3 2. 4 40. 2 44. 8 1 0 3 0 6 A 53. 7 7 F 0 12 F 0 19 A 65. 5 22 F 0 All others 20. 9 Whitney et al. NEJM 2001; 343: 1917
Pneumococcal Resistance to Penicillin by Serotype in Children <5 Years: US 1998 PCV-7 % Non-PCV % types resistant 4 6 B 9 V 14 18 C 19 F 23 F Giebink – FDA – 01/2001 1. 6 42. 1 60. 8 33. 3 2. 4 40. 2 44. 8 1 0 3 0 6 A 53. 7 7 F 0 12 F 0 19 A 65. 5 22 F 0 All others 20. 9 Whitney et al. NEJM 2001; 343: 1917
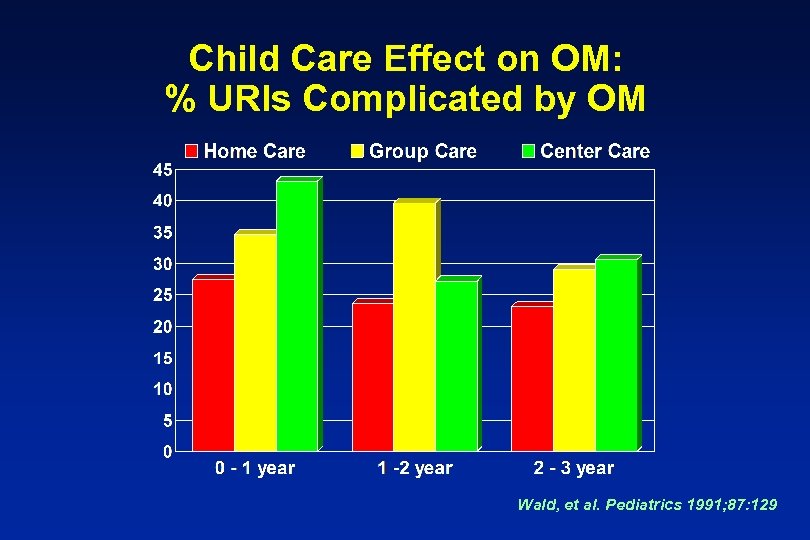 Child Care Effect on OM: % URIs Complicated by OM Wald, et al. Pediatrics 1991; 87: 129
Child Care Effect on OM: % URIs Complicated by OM Wald, et al. Pediatrics 1991; 87: 129
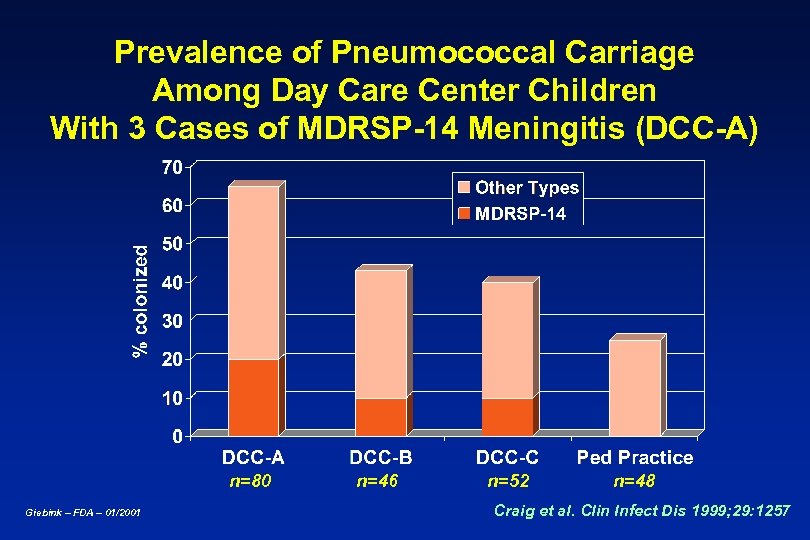 Prevalence of Pneumococcal Carriage Among Day Care Center Children With 3 Cases of MDRSP-14 Meningitis (DCC-A) n=80 Giebink – FDA – 01/2001 n=46 n=52 n=48 Craig et al. Clin Infect Dis 1999; 29: 1257
Prevalence of Pneumococcal Carriage Among Day Care Center Children With 3 Cases of MDRSP-14 Meningitis (DCC-A) n=80 Giebink – FDA – 01/2001 n=46 n=52 n=48 Craig et al. Clin Infect Dis 1999; 29: 1257
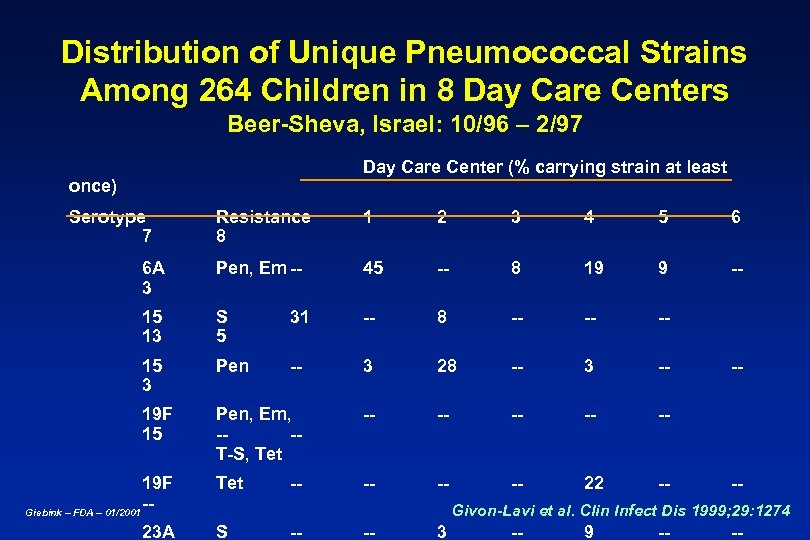 Distribution of Unique Pneumococcal Strains Among 264 Children in 8 Day Care Centers Beer-Sheva, Israel: 10/96 – 2/97 Day Care Center (% carrying strain at least once) Serotype 7 Resistance 8 1 2 3 4 5 6 6 A 3 Pen, Em -- 45 -- 8 19 9 -- 15 13 S 5 31 -- 8 -- -- -- 15 3 Pen -- 3 28 -- 3 -- 19 F 15 Pen, Em, --T-S, Tet -- -- -- 22 -- 19 F -Giebink – FDA – 01/2001 23 A -- -- -- Givon-Lavi et al. Clin Infect Dis 1999; 29: 1274 S -- -- 3 -- 9 -- --
Distribution of Unique Pneumococcal Strains Among 264 Children in 8 Day Care Centers Beer-Sheva, Israel: 10/96 – 2/97 Day Care Center (% carrying strain at least once) Serotype 7 Resistance 8 1 2 3 4 5 6 6 A 3 Pen, Em -- 45 -- 8 19 9 -- 15 13 S 5 31 -- 8 -- -- -- 15 3 Pen -- 3 28 -- 3 -- 19 F 15 Pen, Em, --T-S, Tet -- -- -- 22 -- 19 F -Giebink – FDA – 01/2001 23 A -- -- -- Givon-Lavi et al. Clin Infect Dis 1999; 29: 1274 S -- -- 3 -- 9 -- --
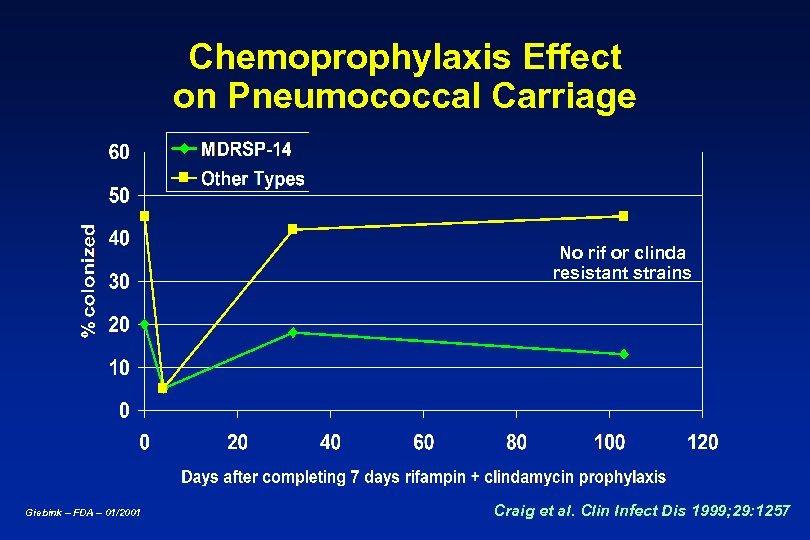 Chemoprophylaxis Effect on Pneumococcal Carriage No rif or clinda resistant strains Giebink – FDA – 01/2001 Craig et al. Clin Infect Dis 1999; 29: 1257
Chemoprophylaxis Effect on Pneumococcal Carriage No rif or clinda resistant strains Giebink – FDA – 01/2001 Craig et al. Clin Infect Dis 1999; 29: 1257
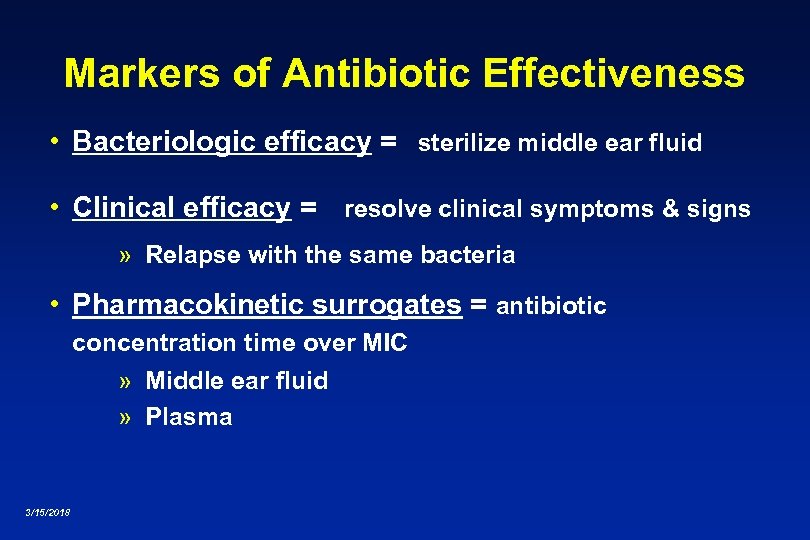 Markers of Antibiotic Effectiveness • Bacteriologic efficacy = sterilize middle ear fluid • Clinical efficacy = resolve clinical symptoms & signs » Relapse with the same bacteria • Pharmacokinetic surrogates = antibiotic concentration time over MIC » Middle ear fluid » Plasma 3/15/2018
Markers of Antibiotic Effectiveness • Bacteriologic efficacy = sterilize middle ear fluid • Clinical efficacy = resolve clinical symptoms & signs » Relapse with the same bacteria • Pharmacokinetic surrogates = antibiotic concentration time over MIC » Middle ear fluid » Plasma 3/15/2018
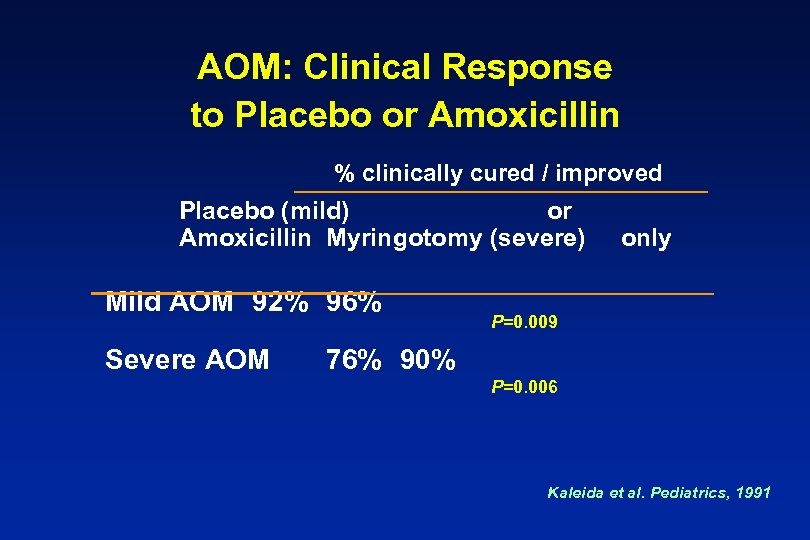 AOM: Clinical Response to Placebo or Amoxicillin % clinically cured / improved Placebo (mild) or Amoxicillin Myringotomy (severe) Mild AOM 92% 96% Severe AOM only P=0. 009 76% 90% P=0. 006 Kaleida et al. Pediatrics, 1991
AOM: Clinical Response to Placebo or Amoxicillin % clinically cured / improved Placebo (mild) or Amoxicillin Myringotomy (severe) Mild AOM 92% 96% Severe AOM only P=0. 009 76% 90% P=0. 006 Kaleida et al. Pediatrics, 1991
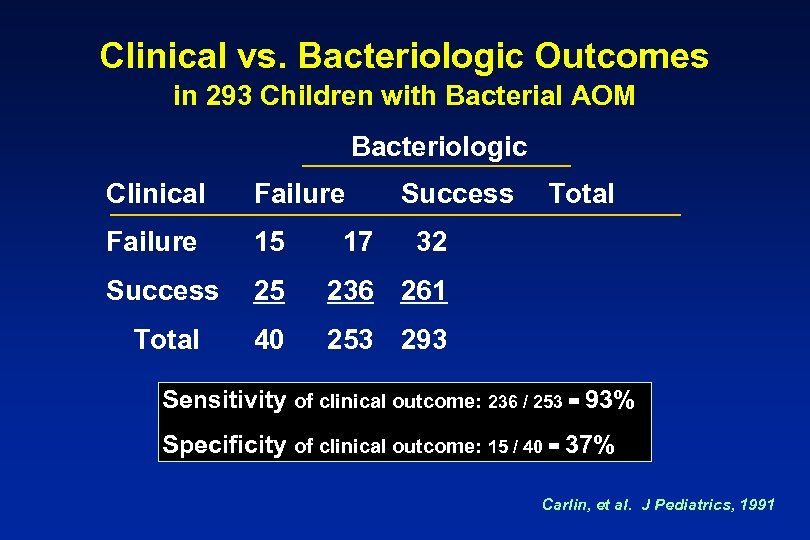 Clinical vs. Bacteriologic Outcomes in 293 Children with Bacterial AOM Bacteriologic Clinical Failure 15 Success 25 236 261 Total 40 253 293 17 Success Total 32 Sensitivity of clinical outcome: 236 / 253 = 93% Specificity of clinical outcome: 15 / 40 = 37% Carlin, et al. J Pediatrics, 1991
Clinical vs. Bacteriologic Outcomes in 293 Children with Bacterial AOM Bacteriologic Clinical Failure 15 Success 25 236 261 Total 40 253 293 17 Success Total 32 Sensitivity of clinical outcome: 236 / 253 = 93% Specificity of clinical outcome: 15 / 40 = 37% Carlin, et al. J Pediatrics, 1991
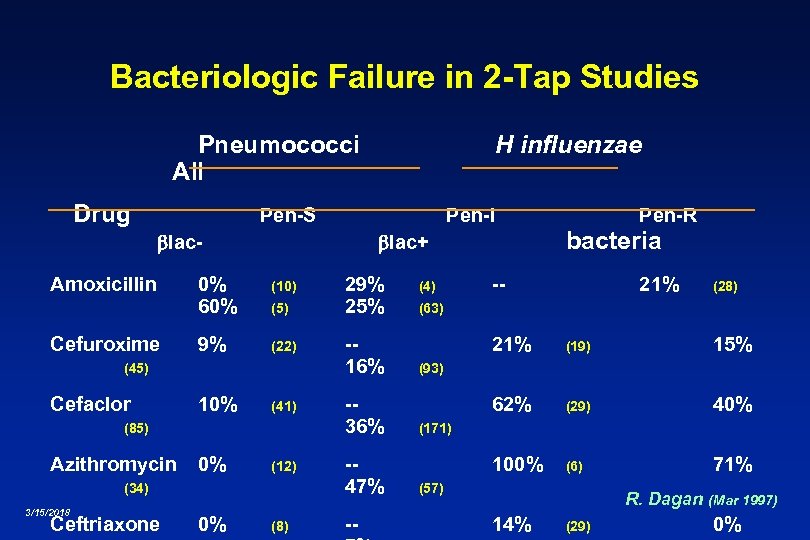 Bacteriologic Failure in 2 -Tap Studies Pneumococci All Drug Pen-S Pen-I lac. Amoxicillin Cefuroxime 0% 60% (10) 9% (22) (5) Cefaclor 10% (41) (85) Azithromycin 0% (12) (34) Ceftriaxone 0% (8) 29% 25% -16% -36% -47% -- (4) Pen-R bacteria lac+ (45) 3/15/2018 H influenzae -- 21% (28) (63) 21% (19) 15% 62% (29) 40% 100% (6) 71% (93) (171) (57) R. Dagan (Mar 1997) 14% (29) 0%
Bacteriologic Failure in 2 -Tap Studies Pneumococci All Drug Pen-S Pen-I lac. Amoxicillin Cefuroxime 0% 60% (10) 9% (22) (5) Cefaclor 10% (41) (85) Azithromycin 0% (12) (34) Ceftriaxone 0% (8) 29% 25% -16% -36% -47% -- (4) Pen-R bacteria lac+ (45) 3/15/2018 H influenzae -- 21% (28) (63) 21% (19) 15% 62% (29) 40% 100% (6) 71% (93) (171) (57) R. Dagan (Mar 1997) 14% (29) 0%
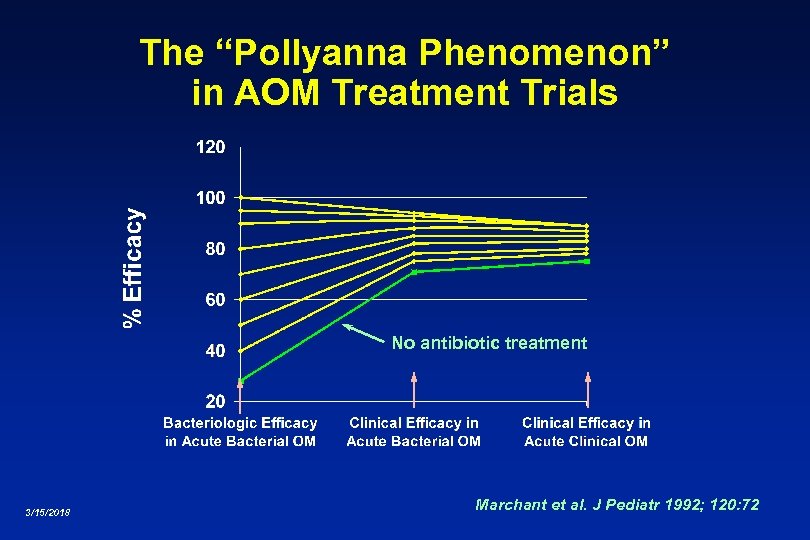 The “Pollyanna Phenomenon” in AOM Treatment Trials No antibiotic treatment 3/15/2018 Marchant et al. J Pediatr 1992; 120: 72
The “Pollyanna Phenomenon” in AOM Treatment Trials No antibiotic treatment 3/15/2018 Marchant et al. J Pediatr 1992; 120: 72
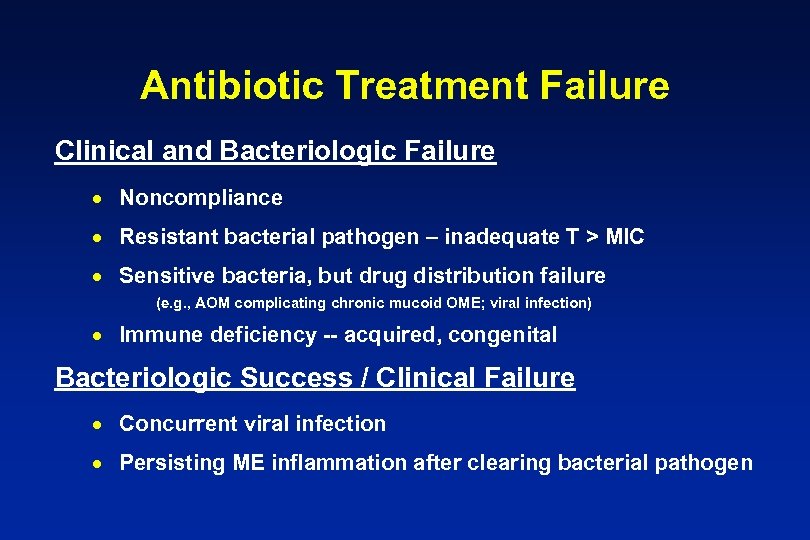 Antibiotic Treatment Failure Clinical and Bacteriologic Failure · Noncompliance · Resistant bacterial pathogen – inadequate T > MIC · Sensitive bacteria, but drug distribution failure (e. g. , AOM complicating chronic mucoid OME; viral infection) · Immune deficiency -- acquired, congenital Bacteriologic Success / Clinical Failure · Concurrent viral infection · Persisting ME inflammation after clearing bacterial pathogen
Antibiotic Treatment Failure Clinical and Bacteriologic Failure · Noncompliance · Resistant bacterial pathogen – inadequate T > MIC · Sensitive bacteria, but drug distribution failure (e. g. , AOM complicating chronic mucoid OME; viral infection) · Immune deficiency -- acquired, congenital Bacteriologic Success / Clinical Failure · Concurrent viral infection · Persisting ME inflammation after clearing bacterial pathogen


