osteoporosis.pptx
- Количество слайдов: 26
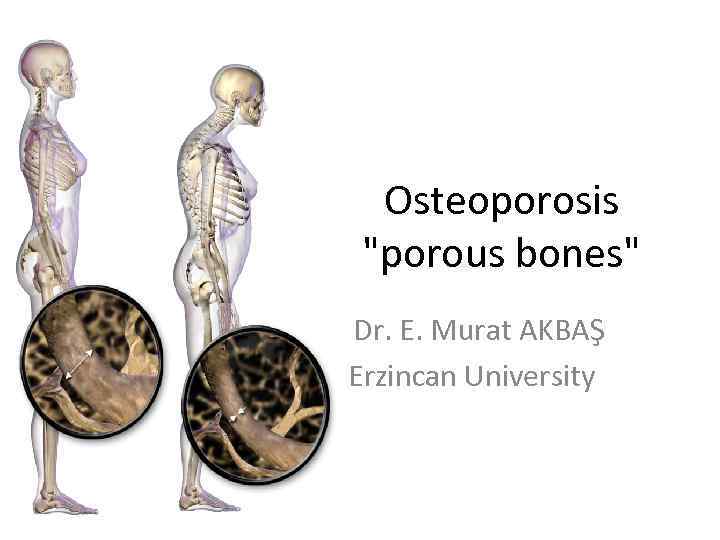
Osteoporosis "porous bones" Dr. E. Murat AKBAŞ Erzincan University
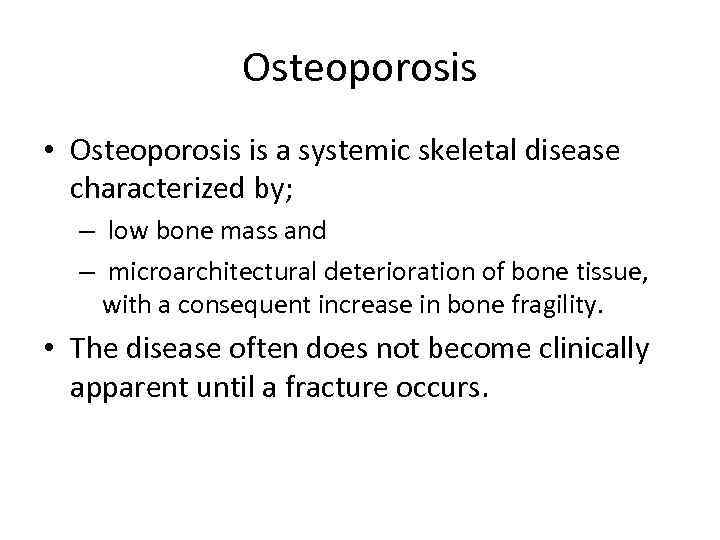
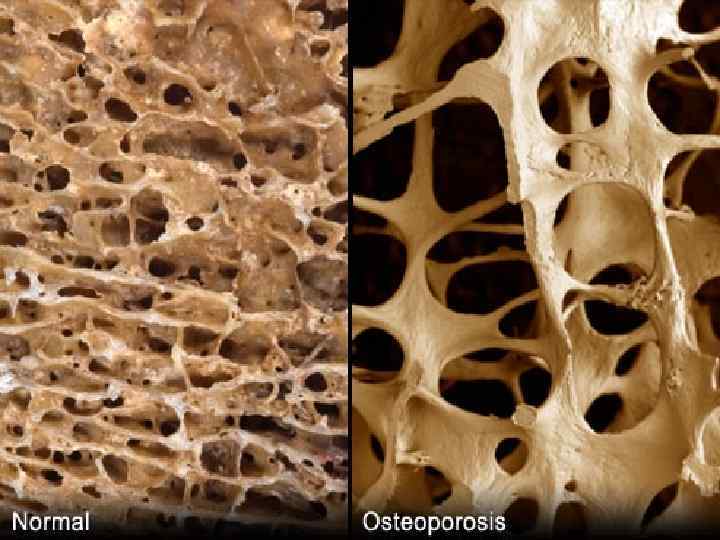
Osteoporosis • Osteoporosis is a systemic skeletal disease characterized by; – low bone mass and – microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility. • The disease often does not become clinically apparent until a fracture occurs.
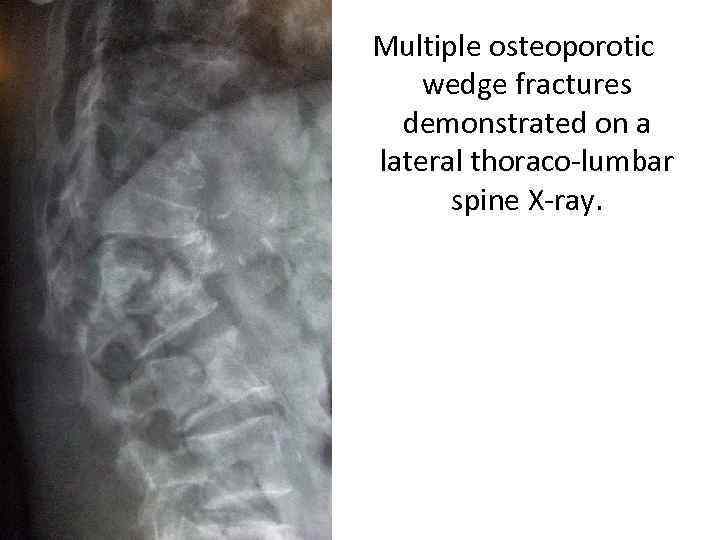
Multiple osteoporotic wedge fractures demonstrated on a lateral thoraco-lumbar spine X-ray.
Osteoporosis • Osteoporosis, a chronic, progressive disease of multifactorial etiology. • It is the most common metabolic bone disease all around the world. • It has been most frequently recognized in elderly white women, although it does occur in both sexes, all races, and all age groups. • Screening at-risk populations is essential.
Osteoporosis • Osteoporosis represents an increasingly serious health and economic problem in the United States and around the world. • Many individuals, male and female, experience ; – pain, – disability, – and diminished quality of life as a result of having this condition. • However, it is so often clinically silent before manifesting in the form of fracture.
Signs and symptoms • Osteoporosis generally does not become clinically apparent until a fracture occurs. • Two thirds of vertebral fractures are painless. • Typical findings in patients with painful fractures may include the following: – The episode of acute pain may follow a fall or minor trauma. – Pain is often accompanied by paravertebral muscle spasms exacerbated by activity and decreased by lying supine. – Marked pain with ambulation. – Subsequent loss of lumbar lordosis. – A decrease in height of 2 -3 cm after each vertebral compression fracture and progressive kyphosis. – Tenderness to palpation, percussion, or both. – Loss of function specific to fracture site.
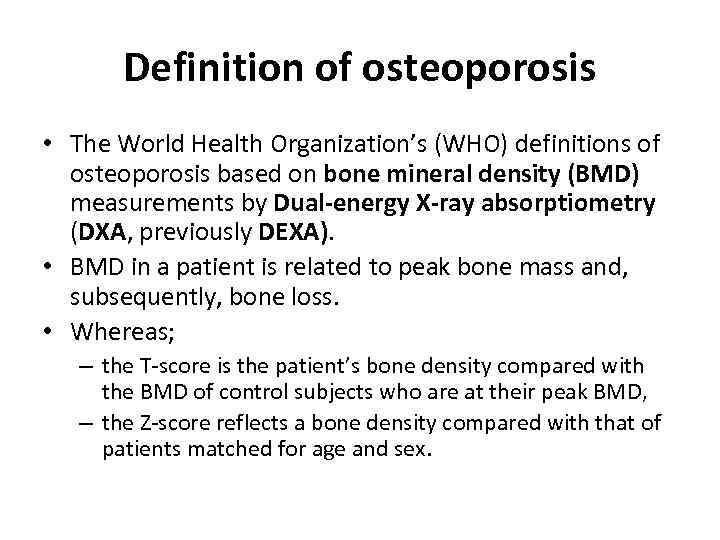
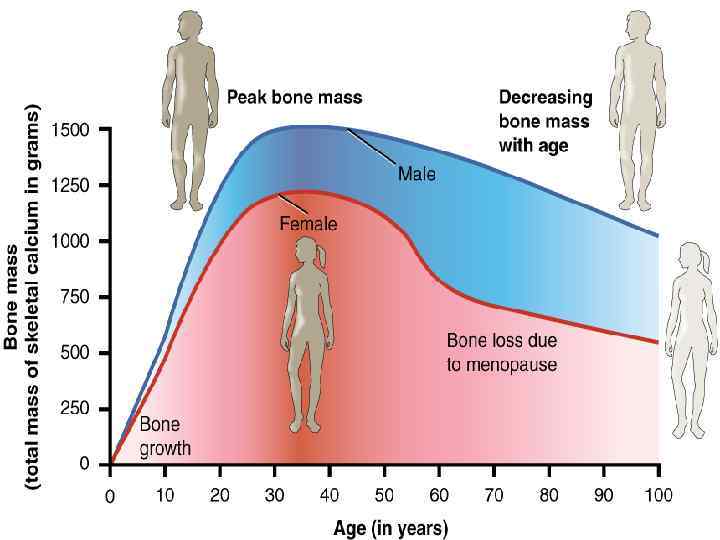
Definition of osteoporosis • The World Health Organization’s (WHO) definitions of osteoporosis based on bone mineral density (BMD) measurements by Dual-energy X-ray absorptiometry (DXA, previously DEXA). • BMD in a patient is related to peak bone mass and, subsequently, bone loss. • Whereas; – the T-score is the patient’s bone density compared with the BMD of control subjects who are at their peak BMD, – the Z-score reflects a bone density compared with that of patients matched for age and sex.
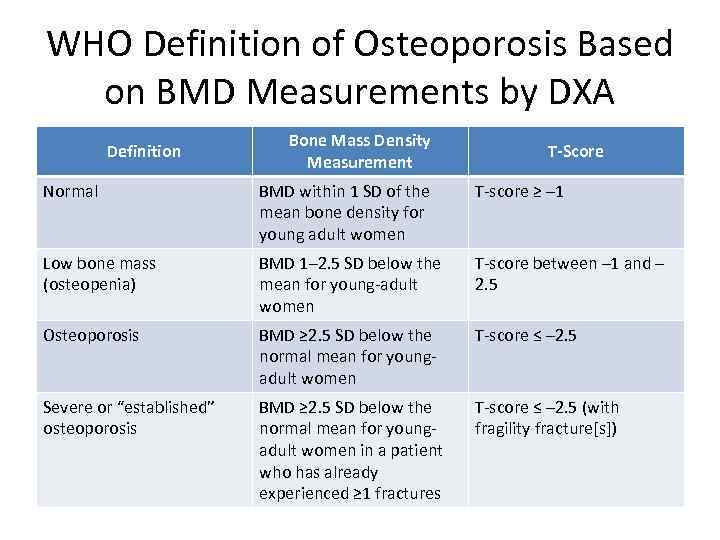
WHO Definition of Osteoporosis Based on BMD Measurements by DXA Definition Bone Mass Density Measurement T-Score Normal BMD within 1 SD of the mean bone density for young adult women T-score ≥ – 1 Low bone mass (osteopenia) BMD 1– 2. 5 SD below the mean for young-adult women T-score between – 1 and – 2. 5 Osteoporosis BMD ≥ 2. 5 SD below the normal mean for youngadult women T-score ≤ – 2. 5 Severe or “established” osteoporosis BMD ≥ 2. 5 SD below the normal mean for youngadult women in a patient who has already experienced ≥ 1 fractures T-score ≤ – 2. 5 (with fragility fracture[s])

Definition of osteoporosis • Z-scores should be used in premenopausal women, men younger than 50 years, and children. • Z-scores adjusted for ethnicity or race should be used, with Z-scores of – 2. 0 or lower defined as "below the expected range for age" and with Zscores above – 2. 0 being defined as "within the expected range for age. " The diagnosis of osteoporosis in these groups should not be based on densitometric criteria alone.
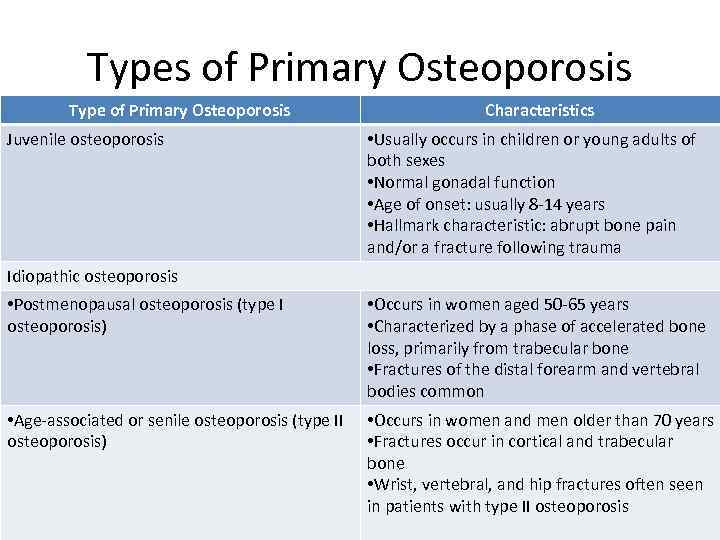
Types of Primary Osteoporosis Type of Primary Osteoporosis Juvenile osteoporosis Characteristics • Usually occurs in children or young adults of both sexes • Normal gonadal function • Age of onset: usually 8 -14 years • Hallmark characteristic: abrupt bone pain and/or a fracture following trauma Idiopathic osteoporosis • Postmenopausal osteoporosis (type I osteoporosis) • Occurs in women aged 50 -65 years • Characterized by a phase of accelerated bone loss, primarily from trabecular bone • Fractures of the distal forearm and vertebral bodies common • Age-associated or senile osteoporosis (type II osteoporosis) • Occurs in women and men older than 70 years • Fractures occur in cortical and trabecular bone • Wrist, vertebral, and hip fractures often seen in patients with type II osteoporosis
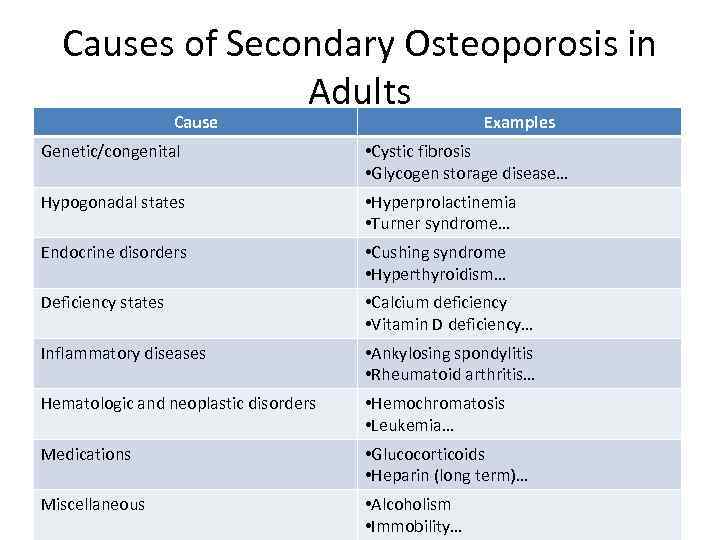
Causes of Secondary Osteoporosis in Adults Cause Examples Genetic/congenital • Cystic fibrosis • Glycogen storage disease… Hypogonadal states • Hyperprolactinemia • Turner syndrome… Endocrine disorders • Cushing syndrome • Hyperthyroidism… Deficiency states • Calcium deficiency • Vitamin D deficiency… Inflammatory diseases • Ankylosing spondylitis • Rheumatoid arthritis… Hematologic and neoplastic disorders • Hemochromatosis • Leukemia… Medications • Glucocorticoids • Heparin (long term)… Miscellaneous • Alcoholism • Immobility…
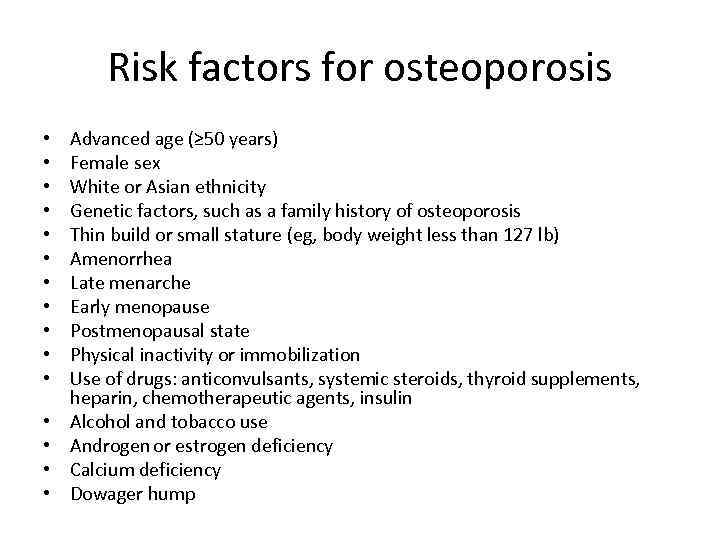
Risk factors for osteoporosis • • • • Advanced age (≥ 50 years) Female sex White or Asian ethnicity Genetic factors, such as a family history of osteoporosis Thin build or small stature (eg, body weight less than 127 lb) Amenorrhea Late menarche Early menopause Postmenopausal state Physical inactivity or immobilization Use of drugs: anticonvulsants, systemic steroids, thyroid supplements, heparin, chemotherapeutic agents, insulin Alcohol and tobacco use Androgen or estrogen deficiency Calcium deficiency Dowager hump
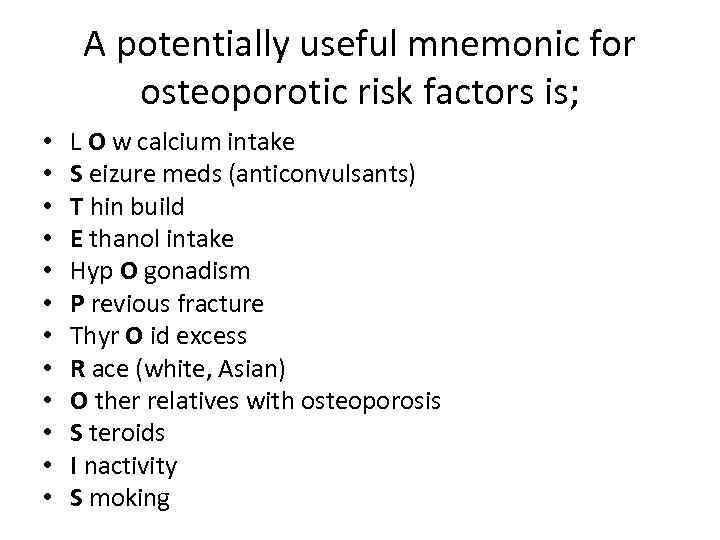
A potentially useful mnemonic for osteoporotic risk factors is; • • • L O w calcium intake S eizure meds (anticonvulsants) T hin build E thanol intake Hyp O gonadism P revious fracture Thyr O id excess R ace (white, Asian) O ther relatives with osteoporosis S teroids I nactivity S moking
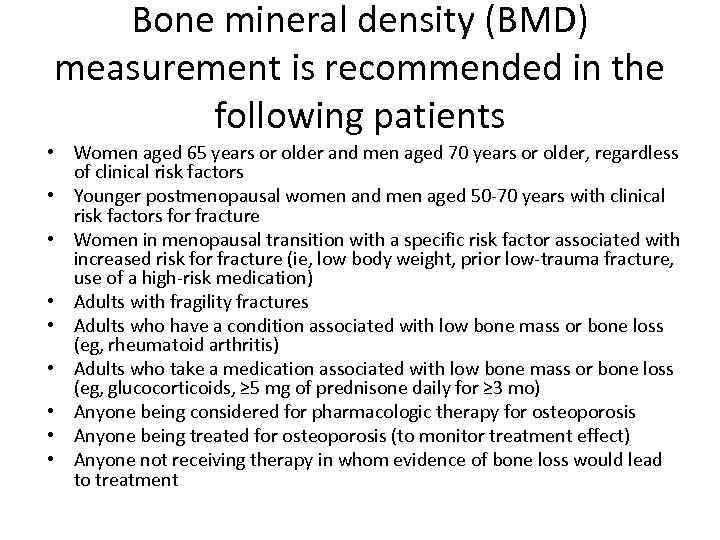
Bone mineral density (BMD) measurement is recommended in the following patients • Women aged 65 years or older and men aged 70 years or older, regardless of clinical risk factors • Younger postmenopausal women and men aged 50 -70 years with clinical risk factors for fracture • Women in menopausal transition with a specific risk factor associated with increased risk for fracture (ie, low body weight, prior low-trauma fracture, use of a high-risk medication) • Adults with fragility fractures • Adults who have a condition associated with low bone mass or bone loss (eg, rheumatoid arthritis) • Adults who take a medication associated with low bone mass or bone loss (eg, glucocorticoids, ≥ 5 mg of prednisone daily for ≥ 3 mo) • Anyone being considered for pharmacologic therapy for osteoporosis • Anyone being treated for osteoporosis (to monitor treatment effect) • Anyone not receiving therapy in whom evidence of bone loss would lead to treatment
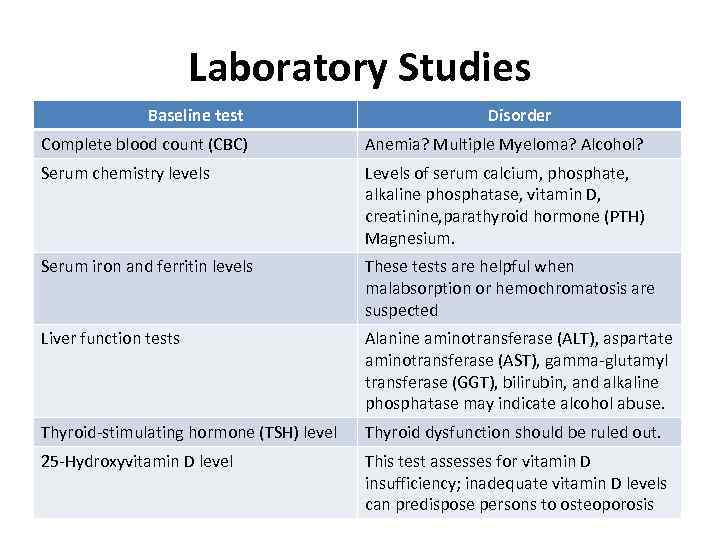
Laboratory Studies Baseline test Disorder Complete blood count (CBC) Anemia? Multiple Myeloma? Alcohol? Serum chemistry levels Levels of serum calcium, phosphate, alkaline phosphatase, vitamin D, creatinine, parathyroid hormone (PTH) Magnesium. Serum iron and ferritin levels These tests are helpful when malabsorption or hemochromatosis are suspected Liver function tests Alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), bilirubin, and alkaline phosphatase may indicate alcohol abuse. Thyroid-stimulating hormone (TSH) level Thyroid dysfunction should be ruled out. 25 -Hydroxyvitamin D level This test assesses for vitamin D insufficiency; inadequate vitamin D levels can predispose persons to osteoporosis
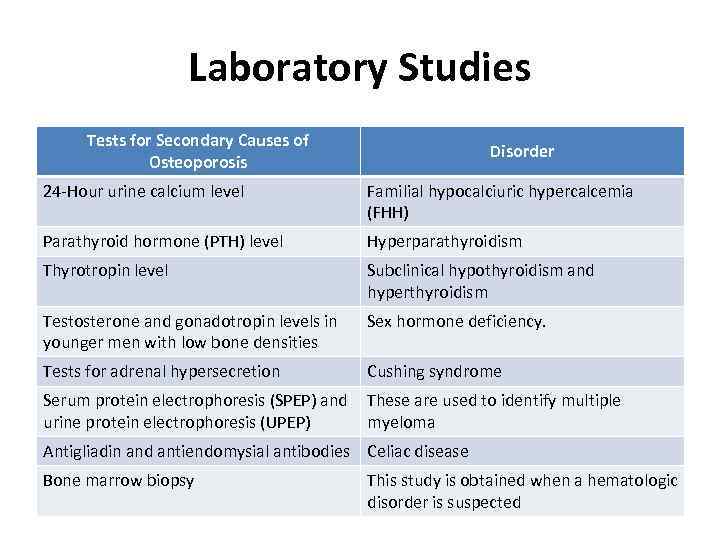
Laboratory Studies Tests for Secondary Causes of Osteoporosis Disorder 24 -Hour urine calcium level Familial hypocalciuric hypercalcemia (FHH) Parathyroid hormone (PTH) level Hyperparathyroidism Thyrotropin level Subclinical hypothyroidism and hyperthyroidism Testosterone and gonadotropin levels in younger men with low bone densities Sex hormone deficiency. Tests for adrenal hypersecretion Cushing syndrome Serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) These are used to identify multiple myeloma Antigliadin and antiendomysial antibodies Celiac disease Bone marrow biopsy This study is obtained when a hematologic disorder is suspected
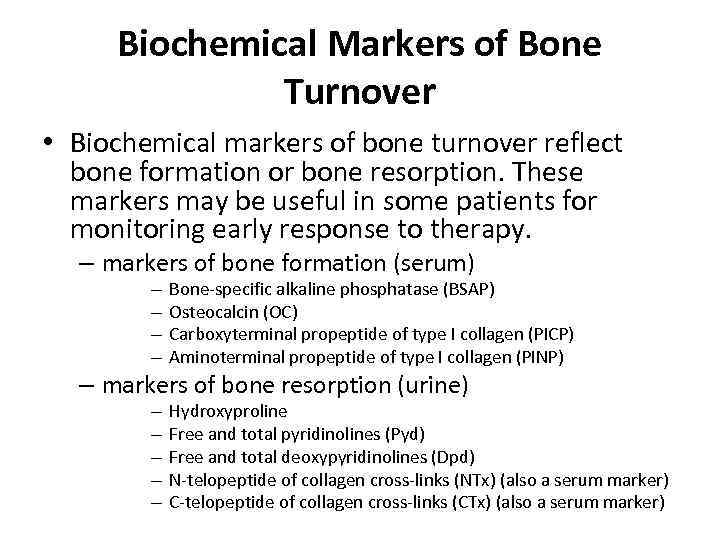
Biochemical Markers of Bone Turnover • Biochemical markers of bone turnover reflect bone formation or bone resorption. These markers may be useful in some patients for monitoring early response to therapy. – markers of bone formation (serum) – – Bone-specific alkaline phosphatase (BSAP) Osteocalcin (OC) Carboxyterminal propeptide of type I collagen (PICP) Aminoterminal propeptide of type I collagen (PINP) – markers of bone resorption (urine) – – – Hydroxyproline Free and total pyridinolines (Pyd) Free and total deoxypyridinolines (Dpd) N-telopeptide of collagen cross-links (NTx) (also a serum marker) C-telopeptide of collagen cross-links (CTx) (also a serum marker)
Screening and Diagnosis
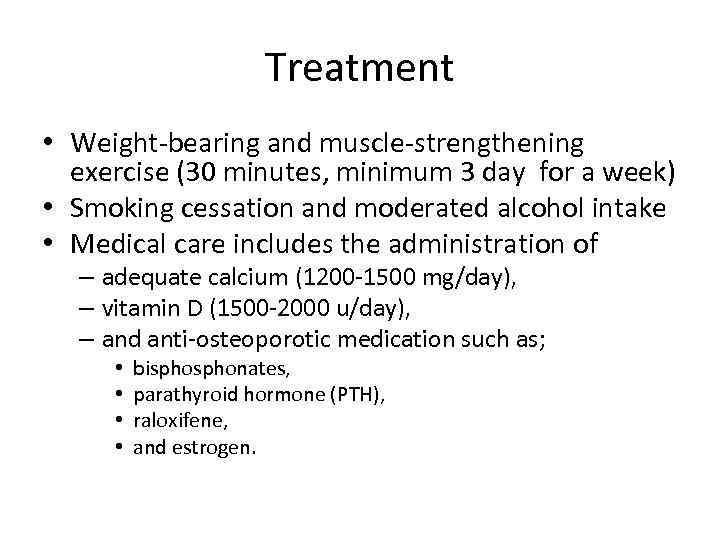
Treatment • Weight-bearing and muscle-strengthening exercise (30 minutes, minimum 3 day for a week) • Smoking cessation and moderated alcohol intake • Medical care includes the administration of – adequate calcium (1200 -1500 mg/day), – vitamin D (1500 -2000 u/day), – and anti-osteoporotic medication such as; • • bisphonates, parathyroid hormone (PTH), raloxifene, and estrogen.
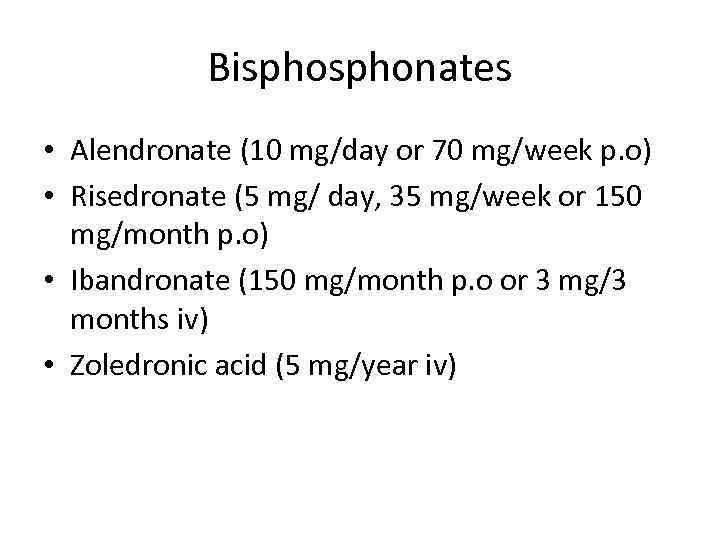
Bisphonates • Alendronate (10 mg/day or 70 mg/week p. o) • Risedronate (5 mg/ day, 35 mg/week or 150 mg/month p. o) • Ibandronate (150 mg/month p. o or 3 mg/3 months iv) • Zoledronic acid (5 mg/year iv)
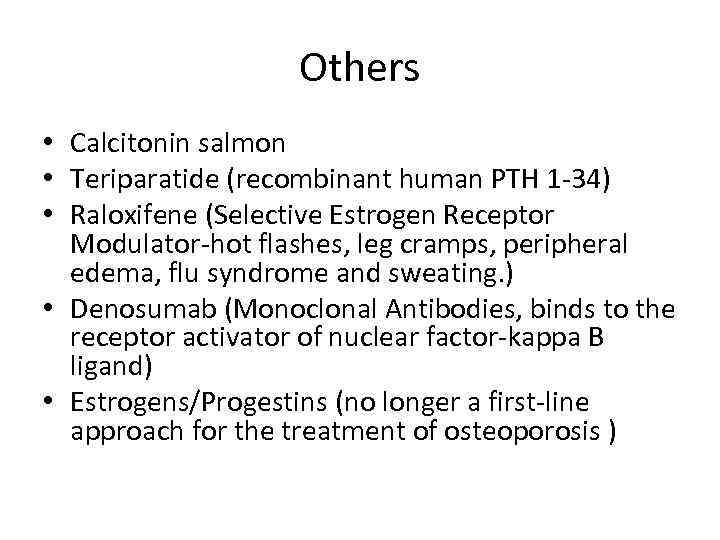
Others • Calcitonin salmon • Teriparatide (recombinant human PTH 1 -34) • Raloxifene (Selective Estrogen Receptor Modulator-hot flashes, leg cramps, peripheral edema, flu syndrome and sweating. ) • Denosumab (Monoclonal Antibodies, binds to the receptor activator of nuclear factor-kappa B ligand) • Estrogens/Progestins (no longer a first-line approach for the treatment of osteoporosis )
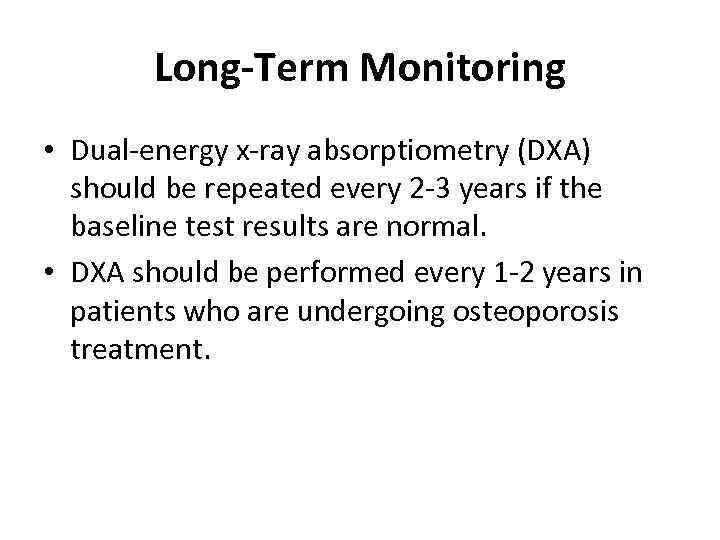
Long-Term Monitoring • Dual-energy x-ray absorptiometry (DXA) should be repeated every 2 -3 years if the baseline test results are normal. • DXA should be performed every 1 -2 years in patients who are undergoing osteoporosis treatment.
Keep in mind; • Osteoporosis occurs in many people who have no factors, or just a few risk factors, for this condition. • This disease is a "silent thief" that generally does not become clinically apparent until a fracture occurs. • Screening at-risk populations is, therefore, essential; unfortunately, many women are not receiving proper screening or treatment for osteoporosis.

Thank you for your patience. . .
osteoporosis.pptx