d2aed051a4c28a19a15227bb72eb2033.ppt
- Количество слайдов: 88
OSCE Feb 2012 Dr. Wong Kim Chiu Associate Consultant North District Hospital
Case 1 ¡ 2/3/2011 ¡ M/67 ¡ Chronic smoker ¡ GERD
Case 1 ¡ c/o: found collapsed at home at 10: 15 a. m. ¡ Last seen well at 10 a. m ¡ Arrived A&E at 10: 51 a. m. ¡ ? Preceded by headache and neck pain
Case 1 ¡ On arrival : ¡ P/E: GCS E 3, V 2, M 6 ¡ PERL, 3 mm ¡ Left hemiparesis ¡ (Rt. side power 4/5, Lt. side power 2/5)
Case 1 ¡ ECG : SR, no acute ischemic changes
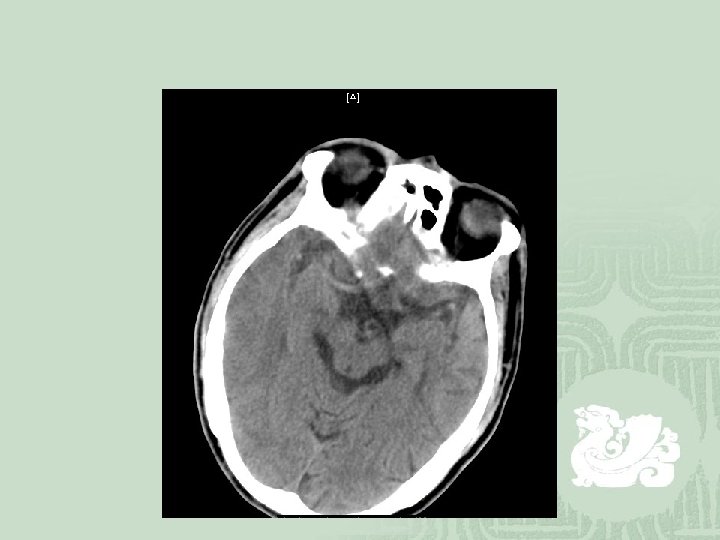
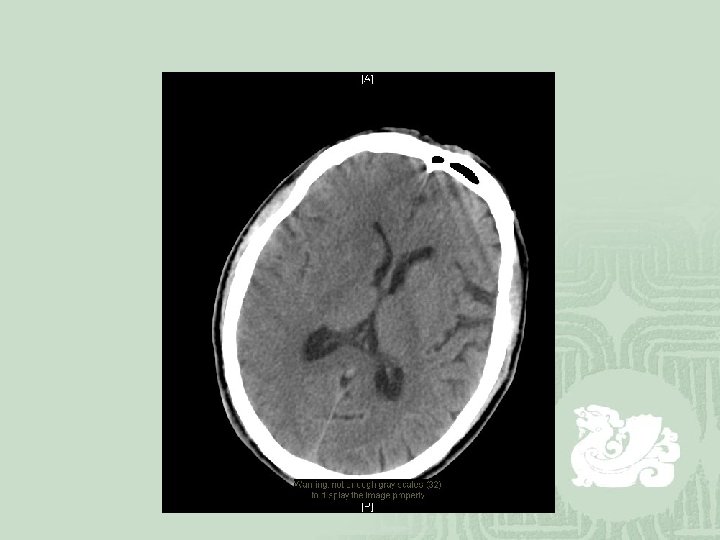
Case 1 ¡ CT brain : Evidence of right MCA infarct with dense MCA sign and effacement of sulci.
Case 1 ¡ rt PA was given at 11: 55 a. m. ¡ Transferred to ICU for close monitoring
Case 1 ¡ Developed hypotension at 3: 30 p. m. ¡ PR no tarry stool ¡ H’cue 11. 2 ¡ No evidence of acute hemorrhage
Case 1 ¡ ECG : new onset ST depression over inferior leads ¡ Bedside Echo: no free fluid in abdomen no pericardial effusion / pleural effusion RWMA +ve RV no dilated ¡ Dx: NSTEMI
Case 1 ¡ Neurologist consulted: Not for aspirin in view of recent adminstration of rt PA
Case 1 ¡ Rapid deterioration with shock and bradycardia ¡ Intubation ¡ Adrenaline and noradrenaline were given ¡ BP on low side despite inotropes support
Case 1 ¡ Succumbed at 6: 44 p. m. on the same day.
Case 2 ¡ M/59 ¡ Good past health ¡ c/o: constricting chest pain after running on the day of attention ¡ P/E: unremarkable ¡ 1 st ECG showed SR with V. E. x 1

Case 2 ¡ Proceed chest pain protocol in O Ward. ¡ Smart M. O. dug out history of right calf pain for 20 days. ¡ ? Right calf swelling ¡ Feeling SOB just after jogging ¡ Still pending 1 st Tn. I
Case 2 ¡ USG doppler was booked. ¡ It showed right superficial femoral vein and popliteal vein thrombosis. ¡ 1 st Tn. I came back 0. 26 ¡ ECG repeated : sinus tachy 139/min. , No RAD or RBBB No S 1 Q 3 T 3
Case 2 ¡ CT thorax showed: Extensive intra-arterial tubular filling defects suggestive of bilateral pulmonary thromboembolism involving the main pulmonary trunk and all of its branches, the right pulmonary lobar arteries and their branches. Both lungs are clear, no pleural effusion Dx: acute massive pulmonary thromboembolism


Diagnosis of PE ¡ The decision to do medical imaging is usually based on clinical grounds, i. e. the medical history, symptoms and findings on physical examination, followed by an assessment of clinical probability.
Diagnosis of PE ¡ The most commonly used method to predict clinical probability, the Wells score, is a clinical prediction rule.
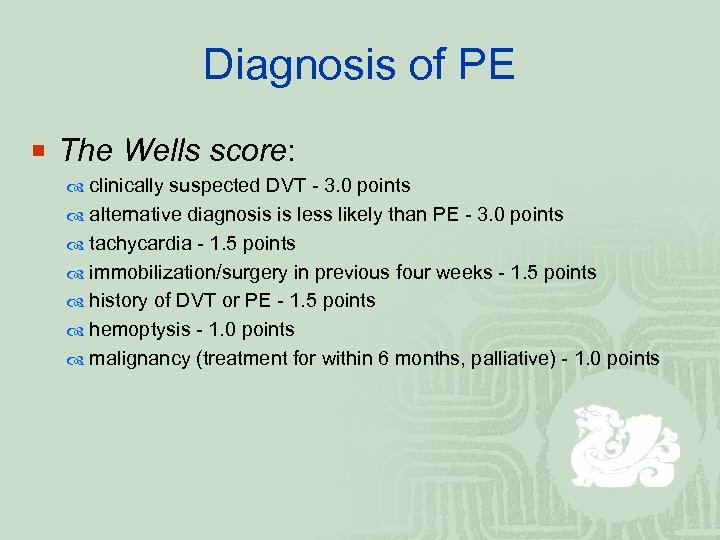
Diagnosis of PE ¡ The Wells score: clinically suspected DVT - 3. 0 points alternative diagnosis is less likely than PE - 3. 0 points tachycardia - 1. 5 points immobilization/surgery in previous four weeks - 1. 5 points history of DVT or PE - 1. 5 points hemoptysis - 1. 0 points malignancy (treatment for within 6 months, palliative) - 1. 0 points
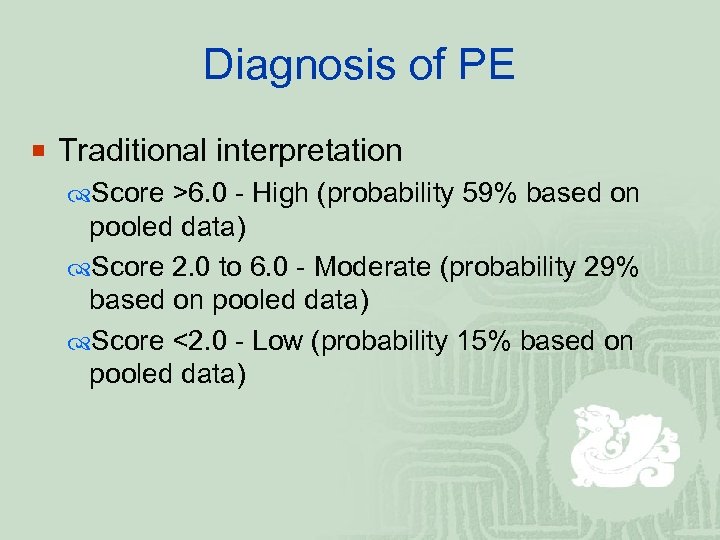
Diagnosis of PE ¡ Traditional interpretation Score >6. 0 - High (probability 59% based on pooled data) Score 2. 0 to 6. 0 - Moderate (probability 29% based on pooled data) Score <2. 0 - Low (probability 15% based on pooled data)
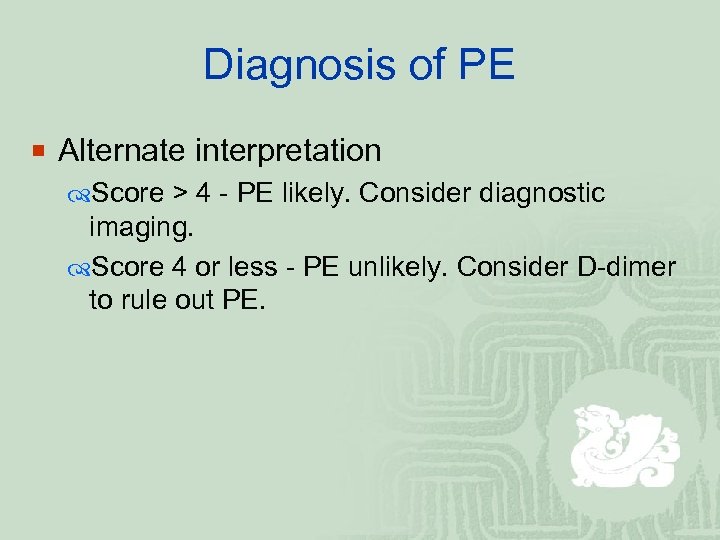
Diagnosis of PE ¡ Alternate interpretation Score > 4 - PE likely. Consider diagnostic imaging. Score 4 or less - PE unlikely. Consider D-dimer to rule out PE.
Diagnosis of PE ¡ The gold standard for diagnosing pulmonary embolism (PE) is pulmonary angiography. Pulmonary angiography is used less often due to wider acceptance of CT scans, which are non-invasive.
Treatment of PE ¡ Anticoagulation In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required.
Treatment of PE ¡ Thrombolysis Massive PE causing hemodynamic instability (shock and/or hypotension, defined as a systolic blood pressure <90 mm. Hg or a pressure drop of 40 mm. Hg for>15 min if not caused by newonset arrhythmia, hypovolemia or sepsis) is an indication for thrombolysis.
Treatment of PE ¡ Surgery Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes.
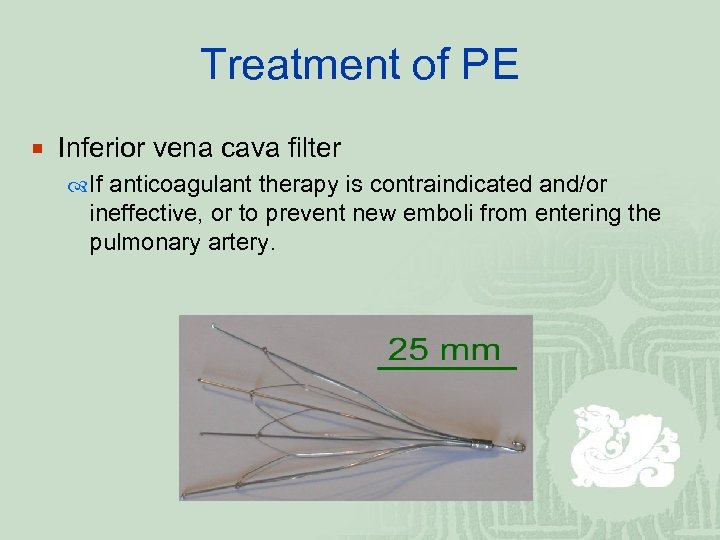
Treatment of PE ¡ Inferior vena cava filter If anticoagulant therapy is contraindicated and/or ineffective, or to prevent new emboli from entering the pulmonary artery.
Case 3 ¡ M/33 ¡ Chronic smoker ¡ Good past health ¡ c/o: sudden onset of chest pain after repeated vomiting because of drunk
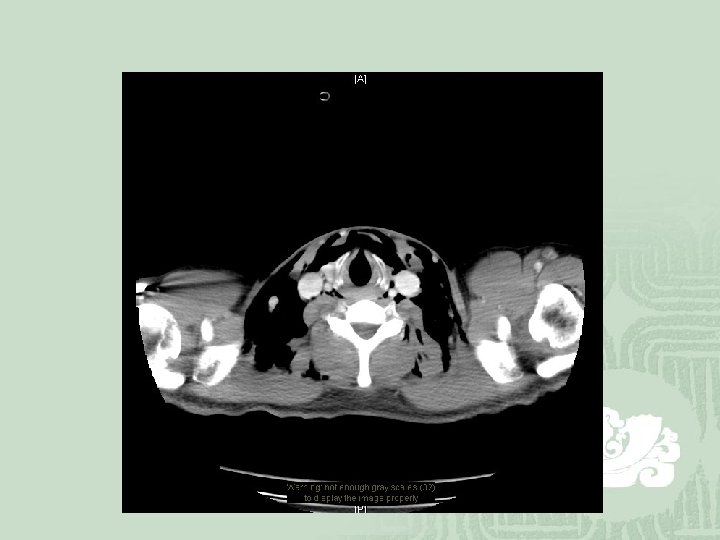
Case 3 ¡ GCS 15/15 ¡ BP 167/67, P 67/min ¡ Temp 36. 9 C ¡ Sa. O 2 100% ¡ Surgical emphysema +ve
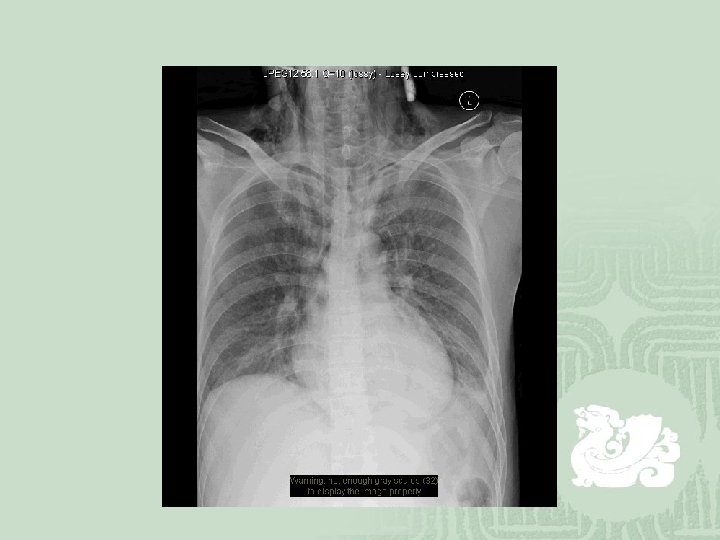
Case 3 ¡ CXR showed pneumomediastinum & diffuse subcutaneous emphysema
Case 3 ¡ ECG showed normal sinus rhythm
Case 3 ¡ CT thorax: Pneumomediastinum & surgical emphysema. Diffuse increase in mediastinal fat density and patch of oral contrast of irregular outline over the lower thoracic region (at level of T 10), suspicious of acute mediastinitis due to leaking from the lower oesophagus.
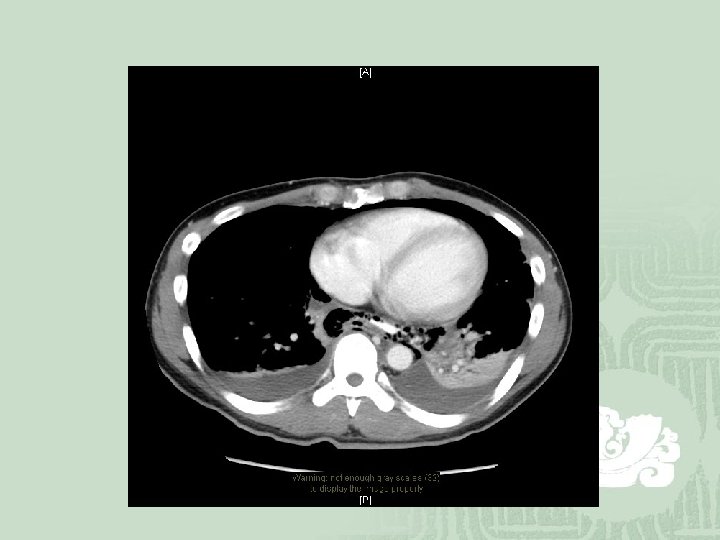
Case 3 ¡ EOT was done: 1. 5 cm x 0. 5 cm perforation at left side of lower oesophagus at T 10 level Loculation of ~ 6 ml pus surrounding the perforation

Case 3 ¡ Esophageal rupture (also known as Boerhaave's syndrome) is rupture of the esophageal wall due to vomiting.
Case 3 ¡ 56% of esophageal perforations are iatrogenic, usually due to medical instrumentation such as an endoscopy. ¡ Boerhaave's syndrome is reserved for the 10% of esophageal perforations which occur due to vomiting.
Case 3 ¡ Boerhaave's syndrome is the result of a sudden rise in internal esophageal pressure produced during vomiting, as a result of neuromuscular incoordination causing failure of the cricopharyngeus muscle to relax.
Case 3 ¡ In most cases of Boerhaave's syndrome, the tear occurs at the left postero-lateral aspect of the distal esophagus and extends for several centimeters. ¡ It is associated with high morbidity and mortality. ¡ The mortality of untreated Boerhaave syndrome is nearly 100%.
Case 3 ¡ The diagnosis of Boerhaave's syndrome is suggested on the plain chest radiography and confirmed by chest CT scan.
Case 3 ¡ Its treatment includes immediate antibiotics therapy to prevent mediatinits and sepsis, surgical repair of the perforation.
Case 4 ¡ M/79 ¡ PMHx: DM, HT, Gout
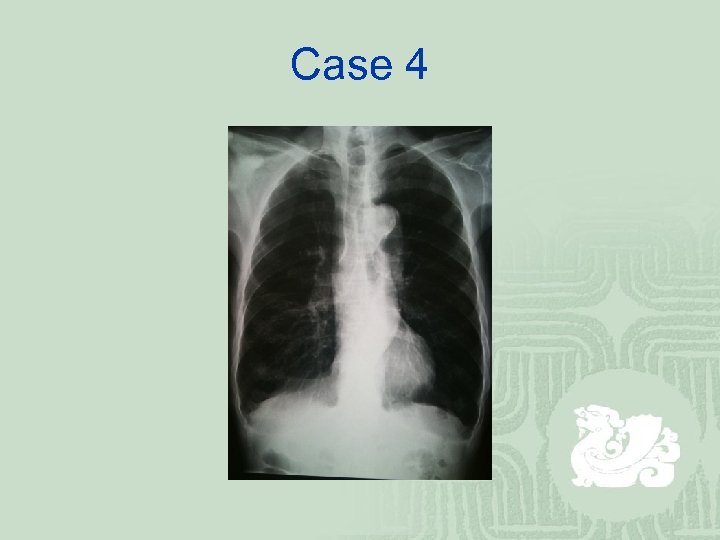
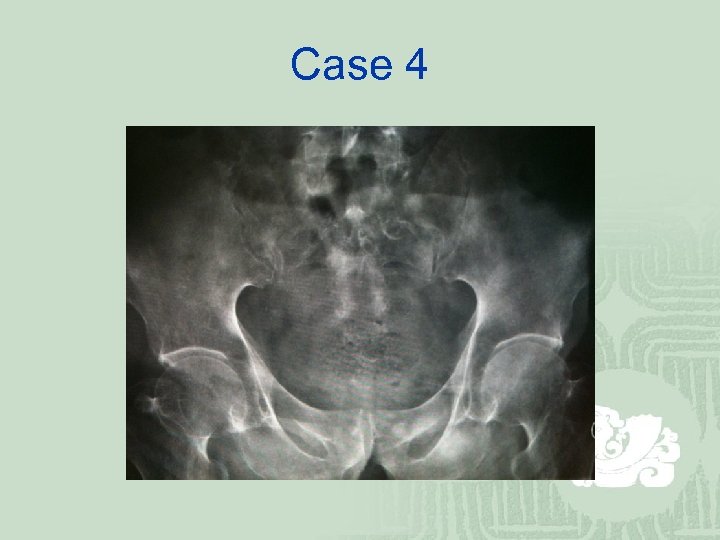
Case 4 ¡ c/o: persistent right shoulder pain after sprain while putting on clothes 1 month ago. ¡ Progressively increase in pain ¡ No systemic symptoms ¡ Treated by bone settor
Case 4 ¡ P/E: ¡ No swelling or bruises ¡ non-specific tenderness over the right shoulder. ¡ ROM: Flexion 30 Ext 0 Abd 30
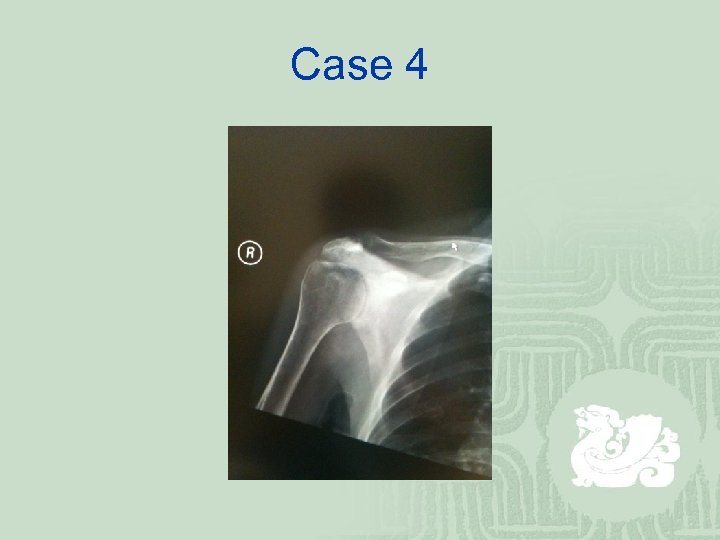
Case 4
Case 4
Case 4
Case 4 ¡ PSA 329 ¡ CT right shoulder: Bony sclerosis with irregularity at the bony outline is seen at the right scapula, involving its body, glenoid process, acromion and coracoid process.

Case 4
Case 4 ¡ TRUS Bx: Adenocarcinoma Gleason score 9 (4+5) Extensive involvement
Case 4 ¡ Dx: Ca prostate with extensive bone mets ¡ Rx: Pt. refused orchidectomy For palliative RT and hormonal therapy
Sclerotic lesions of bone ¡ Mnemonic = VINDICATE
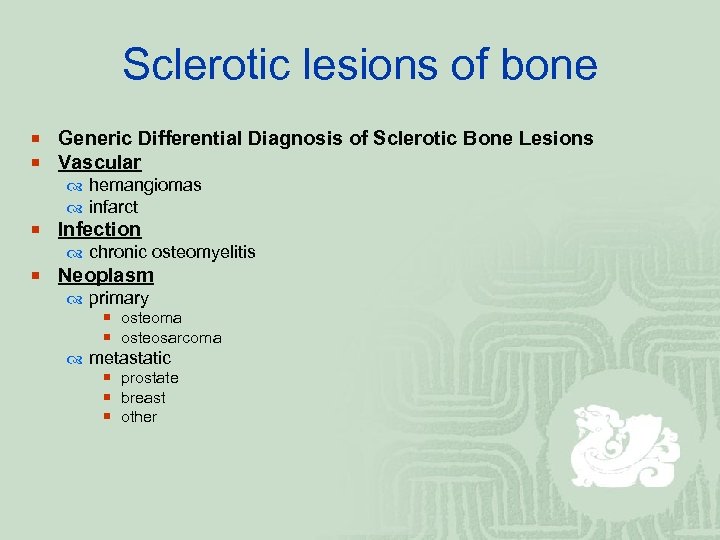
Sclerotic lesions of bone ¡ Generic Differential Diagnosis of Sclerotic Bone Lesions ¡ Vascular hemangiomas infarct ¡ Infection chronic osteomyelitis ¡ Neoplasm primary ¡ osteoma ¡ osteosarcoma metastatic ¡ prostate ¡ breast ¡ other
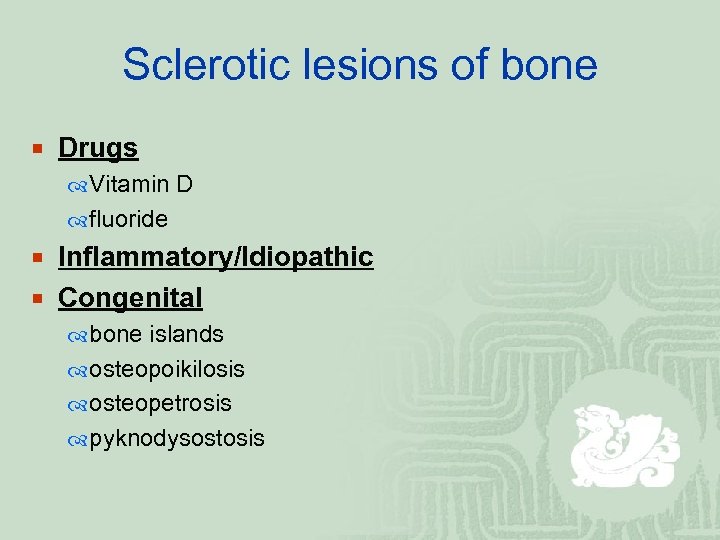
Sclerotic lesions of bone ¡ Drugs Vitamin D fluoride ¡ Inflammatory/Idiopathic ¡ Congenital bone islands osteopoikilosis osteopetrosis pyknodysostosis
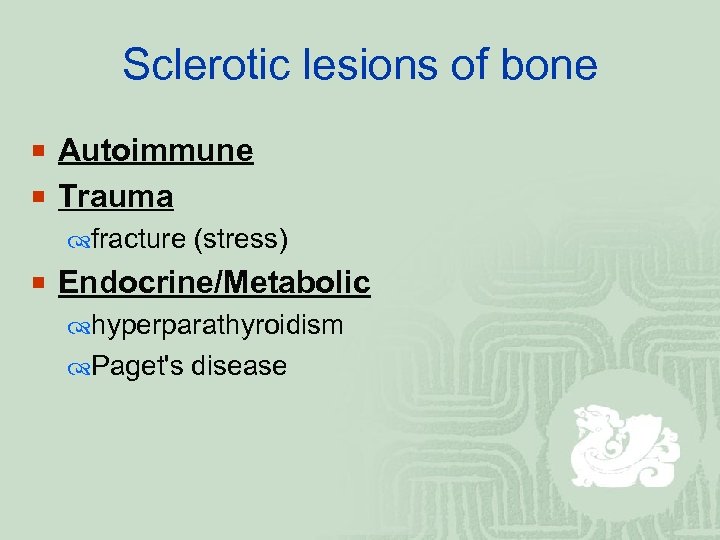
Sclerotic lesions of bone ¡ Autoimmune ¡ Trauma fracture (stress) ¡ Endocrine/Metabolic hyperparathyroidism Paget's disease
Case 5 ¡ M/22 ¡ Good past health ¡ Renovation worker ¡ Chronic smoker, chronic drinker
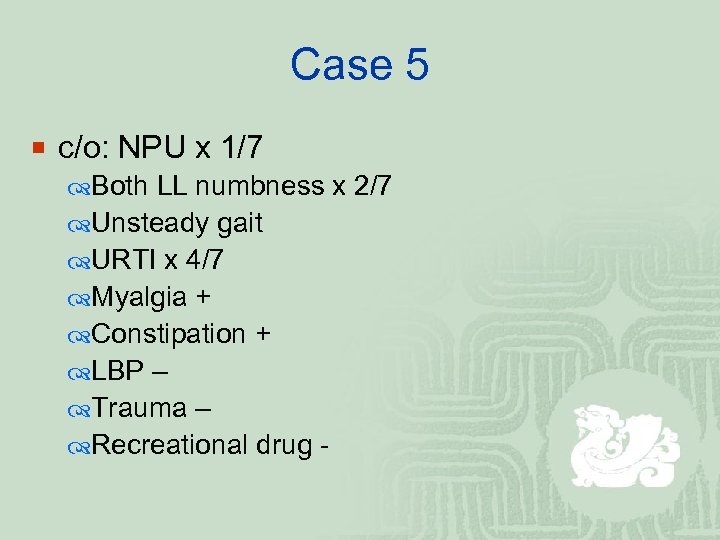
Case 5 ¡ c/o: NPU x 1/7 Both LL numbness x 2/7 Unsteady gait URTI x 4/7 Myalgia + Constipation + LBP – Trauma – Recreational drug -
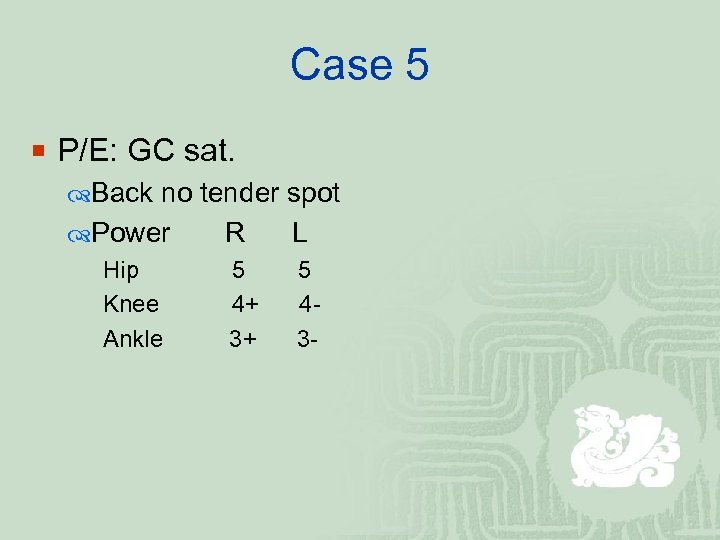
Case 5 ¡ P/E: GC sat. Back no tender spot Power R L Hip Knee Ankle 5 4+ 3+ 5 43 -
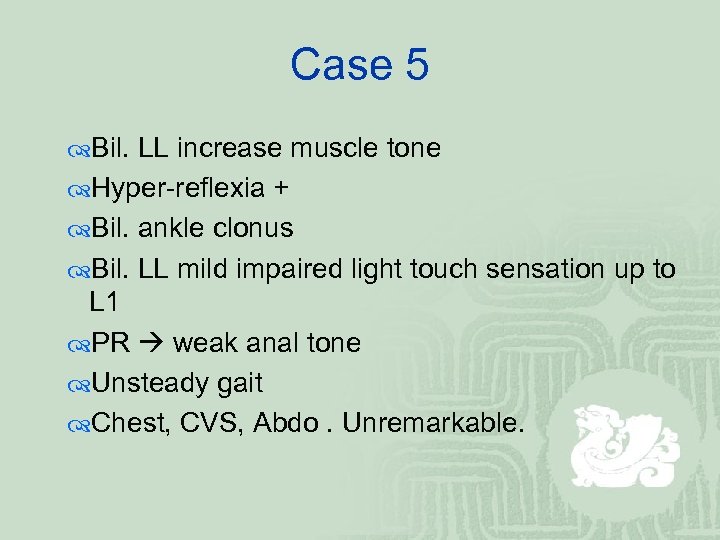
Case 5 Bil. LL increase muscle tone Hyper-reflexia + Bil. ankle clonus Bil. LL mild impaired light touch sensation up to L 1 PR weak anal tone Unsteady gait Chest, CVS, Abdo. Unremarkable.
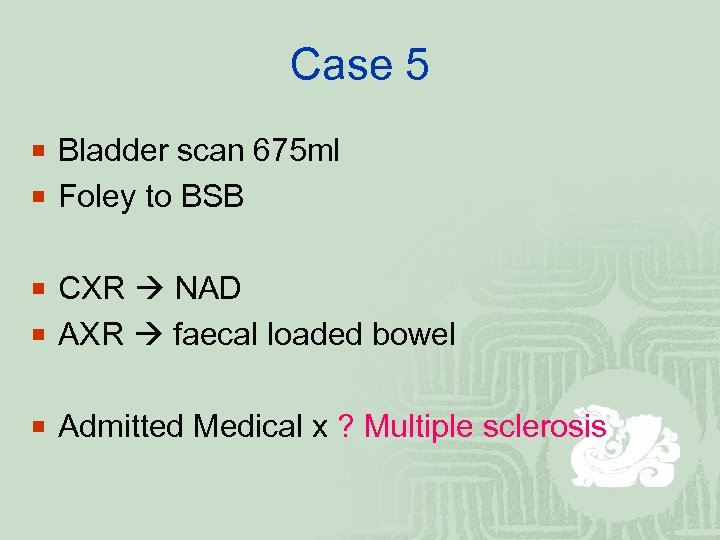
Case 5 ¡ Bladder scan 675 ml ¡ Foley to BSB ¡ CXR NAD ¡ AXR faecal loaded bowel ¡ Admitted Medical x ? Multiple sclerosis
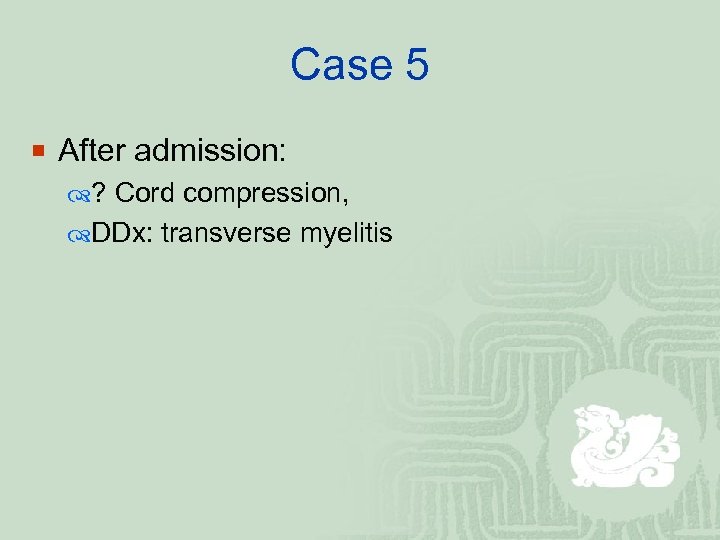
Case 5 ¡ After admission: ? Cord compression, DDx: transverse myelitis
Case 5 ¡ LP: Normal cell count Mild raised TP 0. 53 Glucose 3. 4
Case 5 ¡ Orthopaedics consulted: MRI spine with contrast : ¡ T 11 enhancing intramedullary nodule ~ 0. 4 cm associated with extensive cord oedema and evidence of previous hemorrhage. Overall features favour an intramedullary tumour such as ependymoma.

Case 5 ¡ Dexamethasone was started ¡ Neurosurgery was consulted and took over ¡ Gradual improvement in symptoms and signs. ¡ Started walking exercise 2 days after dexa. ¡ Dexa was tailed down on day 5. ¡ Planned MRI and MRA/V study for T-L spine 6 weeks later. ¡ On 26 -10 -2011
Causes of Spinal Cord Compression ¡ 1. Vertebral ¡ 2. Outside the dura ¡ 3. Within the dura but extramedullary ¡ 4. Intramedullary
Causes of Spinal Cord Compression ¡ 1. Vertebral Spondylosis Trauma Prolapse of a disc Tumour Infection
Causes of Spinal Cord Compression ¡ 2. Outside the dura Lymphoma, metastases Infection – e. g. abscess
Causes of Spinal Cord Compression ¡ 3. Within the dura but extramedullary Tumour – e. g. meningioma, neurofibroma
Causes of Spinal Cord Compression ¡ 4. Intramedullary Tumour – e. g. glioma, ependymoma Syringomyelia Haematomyelia
Transverse myelitis ¡ a neurological disorder caused by an inflammatory process of the spinal cord, and can cause axonal demyelination.
Transverse myelitis ¡ arises idiopathically following infections or vaccination, or due to multiple sclerosis. One major theory posits that immunemediated inflammation is present as the result of exposure to a viral antigen.
Transverse myelitis ¡ involve the spinal cord typically on both sides ¡ onset is sudden and progresses rapidly in hours and days ¡ can be present anywhere in the spinal cord, though it is usually restricted to only a small portion.
Transverse myelitis ¡ DDx: compression of the spinal cord in the spinal canal dissection of the Aorta, extending into one or more of the spinal arteries ¡ An urgent MRI is thus indicated.
Transverse myelitis ¡ Symptoms & signs weakness and numbness of the limbs as well as motor, sensory, and sphincter deficits Severe back pain may occur in some patients at the onset of the disease depend upon the level of the spinal cord involved and the extent of the involvement of the various long tracts
Transverse myelitis ¡ Prognosis: Recovery from transverse myelitis usually begins between weeks 2 and 12 following onset may continue for up to 2 years in some patients Some patients may never show signs of recovery significant recovery from acute transverse myelitis is poor in approximately 80% of the cases
Transverse myelitis ¡ Treatment: symptomatic only corticosteroids being used with limited success
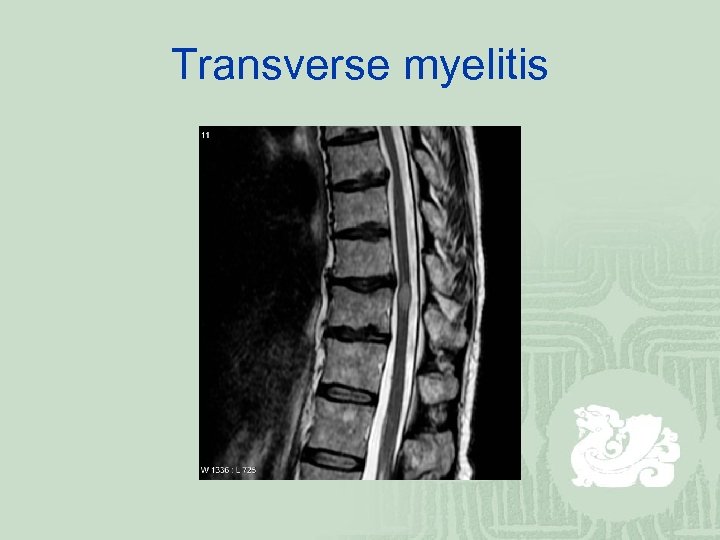
Transverse myelitis
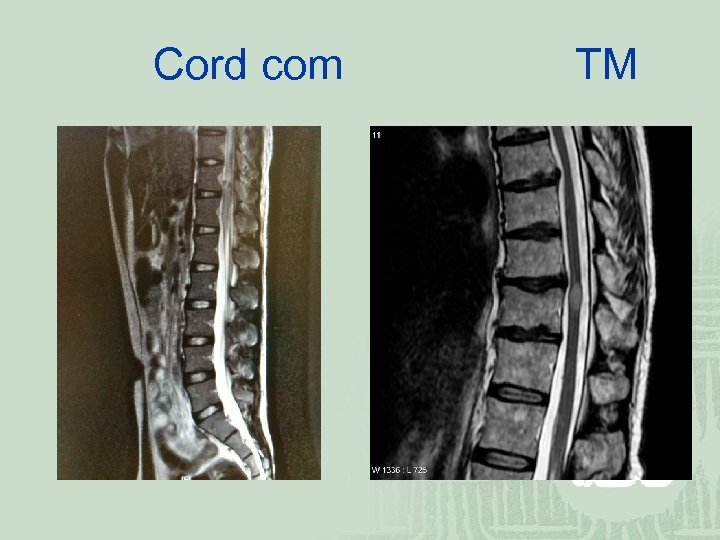
Cord com TM
Thank you
d2aed051a4c28a19a15227bb72eb2033.ppt