dda8bf1bb6661b7f2d6287164128d323.ppt
- Количество слайдов: 35
Orthopaedic Management of Bladder Exstrophy Jessica J. M. Telleria, MD Resident PYG-1 Department of Orthopaedics and Sports Medicine University of Washington, Seattle, WA, USA Pediatric Surgery Weekly Conference 07/07/2011
Disclosures No disclosures
Outline • Anatomic anomalies in bladder exstrophy • Indications & goals for surgery • Operative approaches • Complications • Conclusions
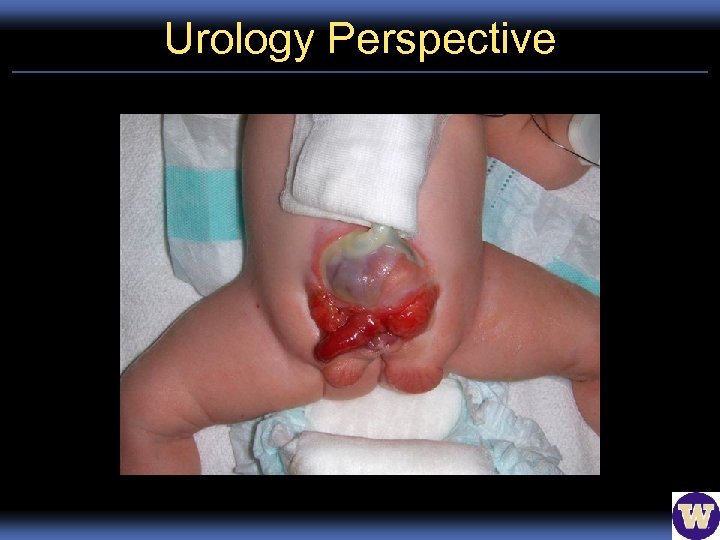
Urology Perspective
Ortho Perspective
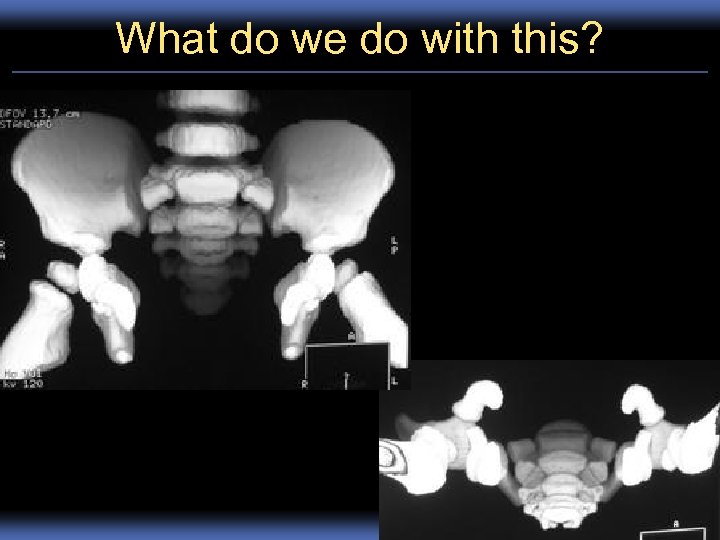
What do we do with this?
What is Normal in Exstrophy • Sacral width • Iliac segment (posterior Pelvis) length • Microscopic histology normal – Boney and cartilaginous differentiation & development – Endochondral ossification (cartilage model)
Defects in Boney Anatomy • Pubic diastasis incomplete pelvic ring – Mean ~4 cm (birth) 8 cm (10 yrs) – Normal 0. 6 cm (all ages) • Ischiopubic segment (anterior pelvis) is 30% shorter – Reduced symphyseal tension/mechanical stress • Anterior segment externally rotated extra 18º • Posterior segment externally rotated extra 12º
Defects in Boney Anatomy • Wider hips – 31% greater distance between triradiate cartilage • Acetabular retroversion – 13° retroversion, normal = 0°
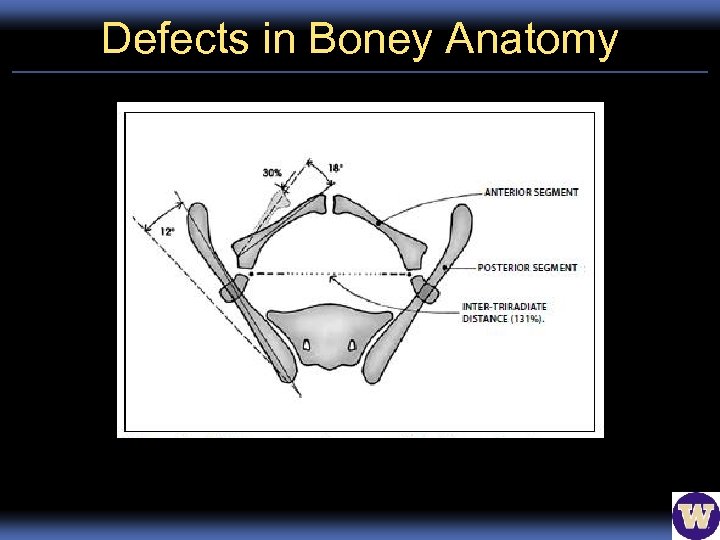
Defects in Boney Anatomy
Defects in Muscular Anatomy • Obturator internus externally rotated extra 15º • Obturator externus externally rotated extra 17º – “Frame” for pelvic diaphragm • Levator ani – 15° greater anterosuperior rotation – 68% of puborectus sling is posterior to rectum (normal = 52%) • Further from bladder neck less support incontinence – Hiatus is 2 x wider & 1. 3 x longer • Wider/flatter Greater pelvic organ prolapse
Why Correct Boney Deformity? • Prior to boney correction well executed softtissue repairs subject to complications: – Dehiscence/Poor wound healing – Fistula formation – Wound infection – Incontinence – Recurrence of exstrophic defect • Many related to excess soft tissue tension on bladder/urethra/abdominal wall – Pubic diastasis & innominate external rotation
Goals of Surgery • Restore stability to pelvic ring – Close anterior ring • Reconstitute “scaffold” for pelvic diaphragm • Provide tension-free closure for bladder/soft tissues wound healing
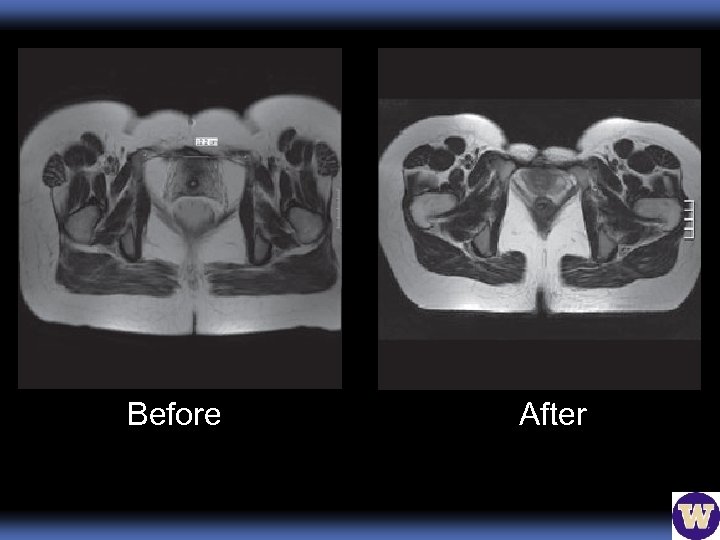
Before After
Approaches • Posterior iliac osteotomy • Anterior osteotomy of superior pubic rami • Anterior diagonal iliac osteotomy • Anterior transverse iliac osteotomy • Combine posterior vertical and anterior transverse iliac osteotomy
Combined Vertical/Transverse • Corrects both anterior & posterior defects • Transverse osteotomy: ~10 mm proximal to AIIS most proximal (superior) sciatic notch • Posterior vertical osteotomy: 2 -3 cm lateral to SI joint sacral notch. – Symphysis secured with wire through obturator foramen – External table left intact – Vertical closing wedge (hinged greenstick)
Combined Vertical/Transverse • Ex-fix to close pubic symphysis, x 4 wks – Applied under direct visualization – Adjustable if incomplete reduction • Better symphyseal approximation and lower recurrence ( p < 0. 05 compared to posterior alone)
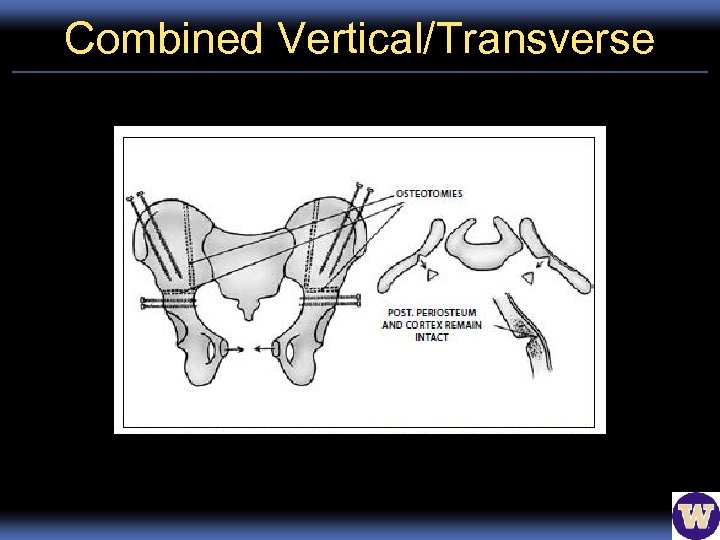
Combined Vertical/Transverse

Anterior Transverse Osteotomy Preoperative
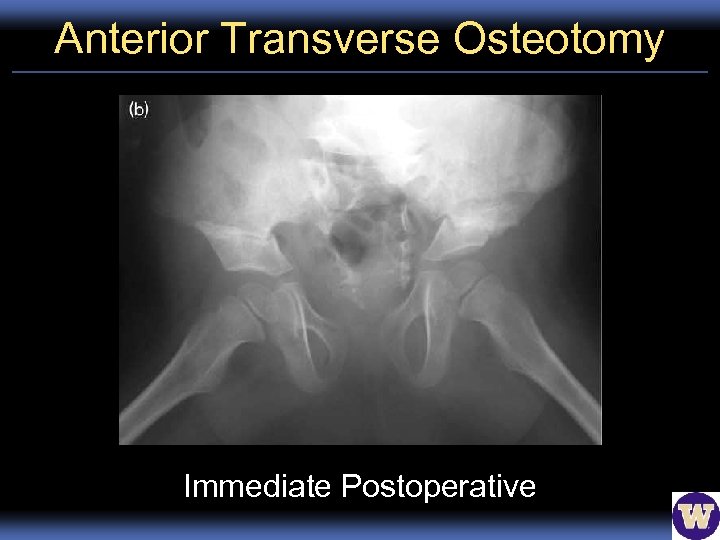
Anterior Transverse Osteotomy Immediate Postoperative
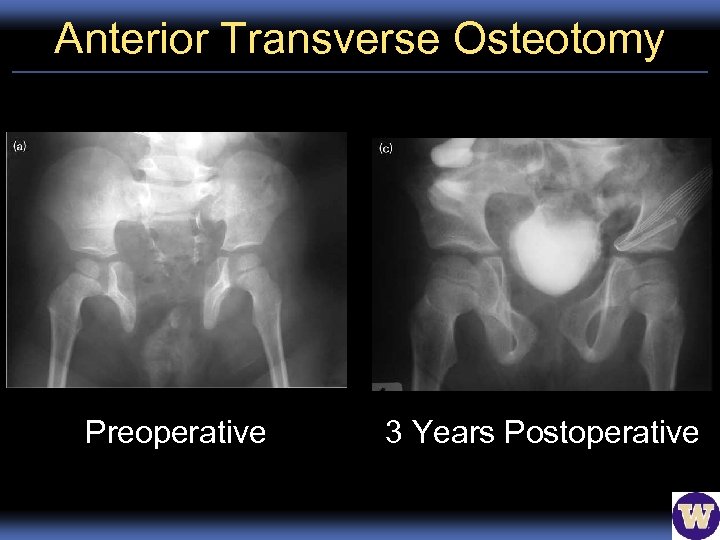
Anterior Transverse Osteotomy Preoperative 3 Years Postoperative
Posterior Iliac Osteotomy • Landmark procedure (1958) • 1 st stage: Vertical osteotomy 2 -3 cm lateral to iliosacral joints. Iliac crest sacral notch. • 2 nd stage: Pubic rami closed/secured with wire through obturator foramina – Sturdy anterior ring prevents prolapse, infection, dehiscence of bladder – Soft tissue reconstruction proceeds • Improved urinary continence 5% 43 -69%
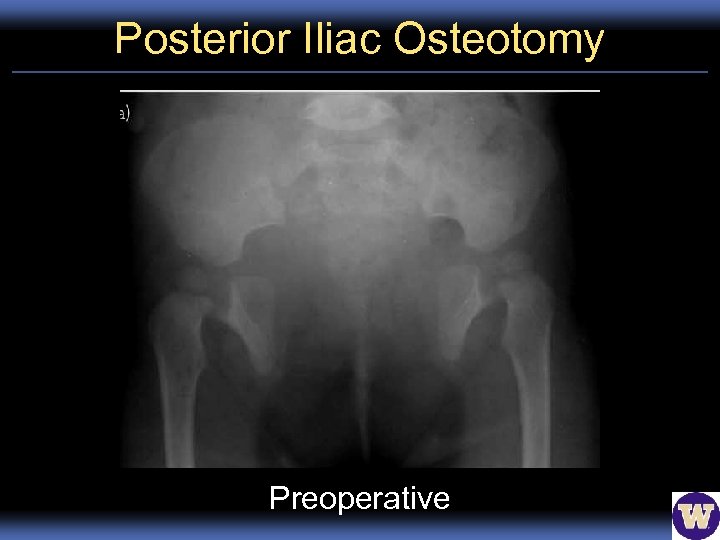
Posterior Iliac Osteotomy Preoperative
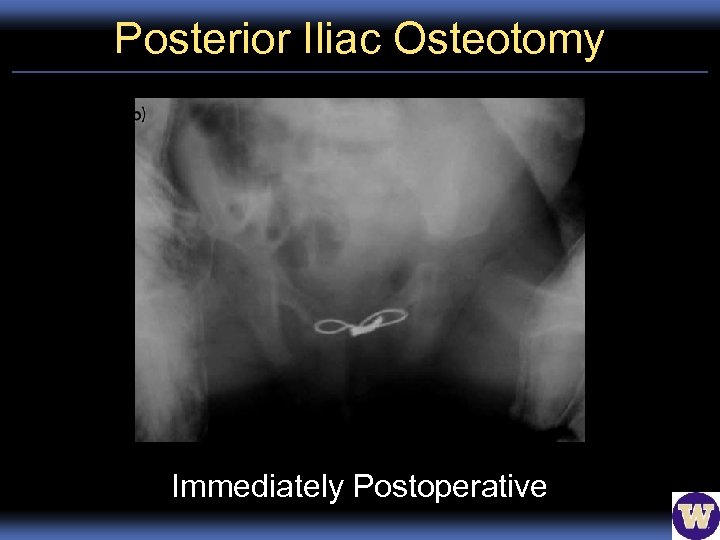
Posterior Iliac Osteotomy Immediately Postoperative
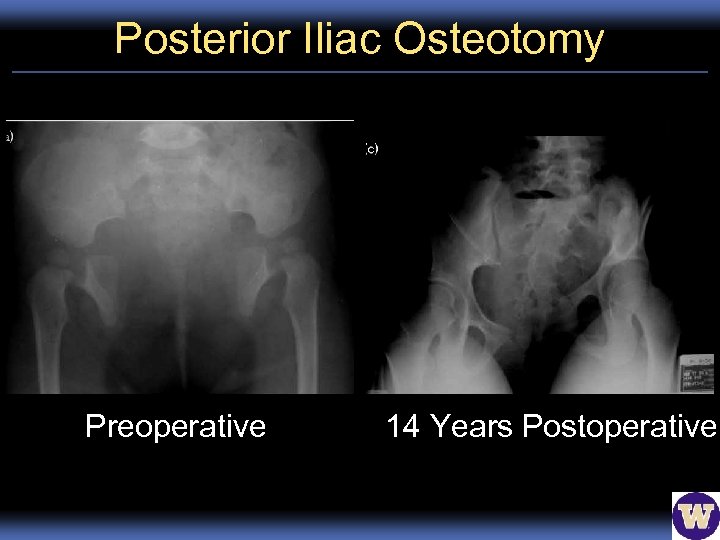
Posterior Iliac Osteotomy Preoperative 14 Years Postoperative
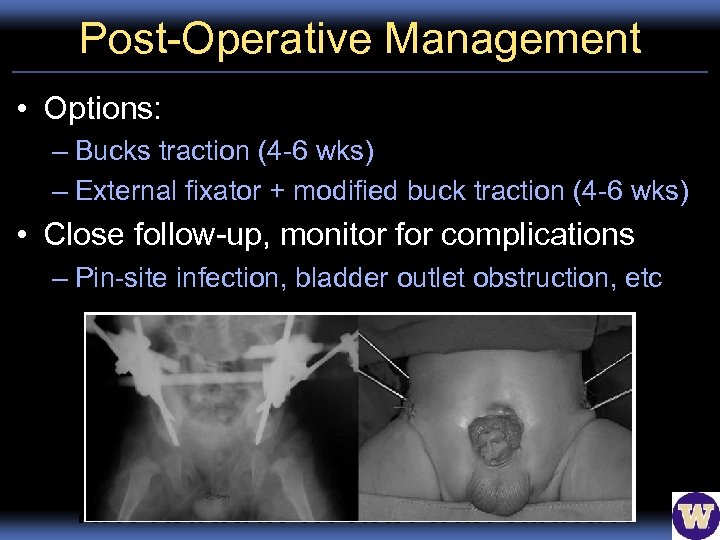
Post-Operative Management • Options: – Bucks traction (4 -6 wks) – External fixator + modified buck traction (4 -6 wks) • Close follow-up, monitor for complications – Pin-site infection, bladder outlet obstruction, etc
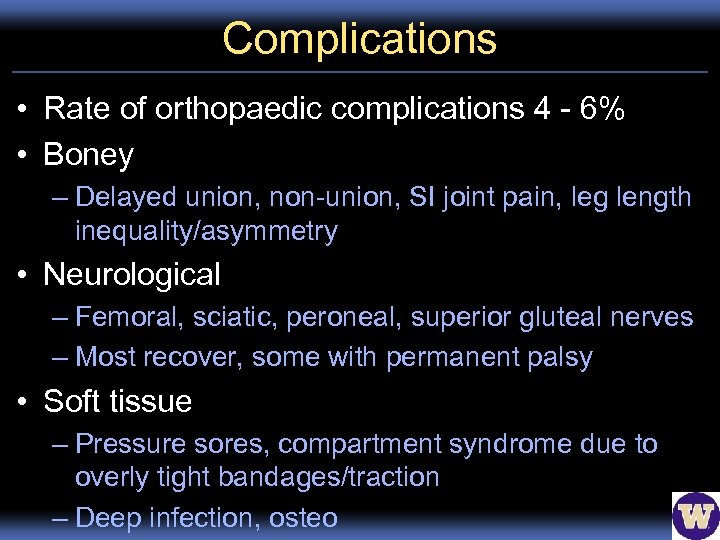
Complications • Rate of orthopaedic complications 4 - 6% • Boney – Delayed union, non-union, SI joint pain, leg length inequality/asymmetry • Neurological – Femoral, sciatic, peroneal, superior gluteal nerves – Most recover, some with permanent palsy • Soft tissue – Pressure sores, compartment syndrome due to overly tight bandages/traction – Deep infection, osteo
Complications • Overall complication rates higher (up to 25%) • Include urologic complications: bladder prolapse, dehiscence, bladder outlet obstruction, ischemic injury to penis, etc.
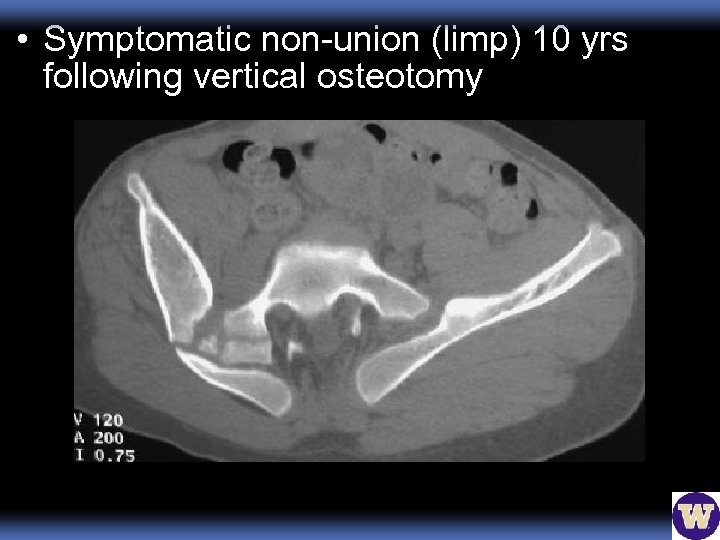
• Symptomatic non-union (limp) 10 yrs following vertical osteotomy
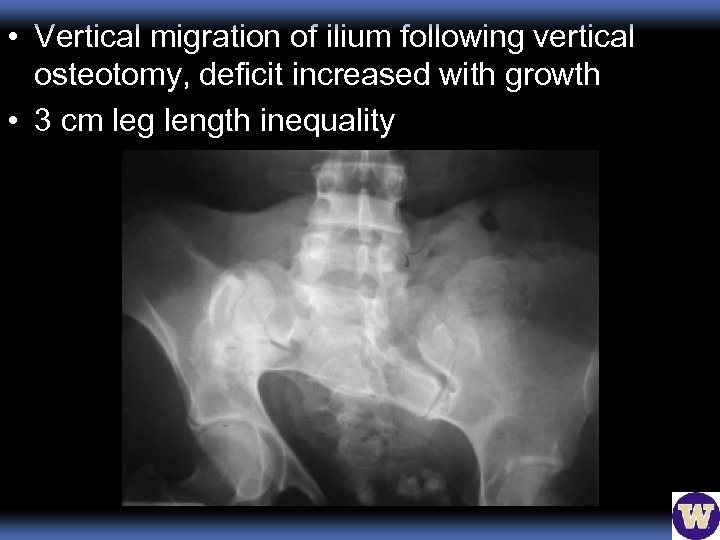
• Vertical migration of ilium following vertical osteotomy, deficit increased with growth • 3 cm leg length inequality
Take Home Points • Care of these patients requires a multidisciplinary approach • Benefits of osteotomy outweigh risks • Major technical surgery, requires: – Careful planning – Creativity – Experienced hands – Know your limits • Success dependent on tension free construct • Evolution of management, continued research and reporting
References 1. Sponseller PD, Bisson LJ, Gearhart JP, et al. The anatomy of the pelvis in the exstrophy complex. J Bone Joint Surg Am 1995; 77 -A: 177 -89. 2. Stec AA, Wakim A, Barbet P, et al. Fetal bony pelvis in the bladder exstrophy complex: Normal potential for growth. J Pediatr Urol 2003; 62: 337 -41. 3. Delaere O, Dhem A. Prenatal development of the human pelvis and acetabulum. Acta Orthop Belg 1999; 65: 255 -60. 4. Stec AA, Pannu HK, Tadros YE, et al. Pelvic floor anatomy in classic bladder exstrophy using 3 -dimensional computerized tomography: Initial insights. J Urol 2001; 166: 1444 -9.
Thanks!
Ant. Osteotomy Sup. Pubic Ramus • Goal: simplify process for completion by pediatric urologist, not ortho (1980 s) – Concurent boney & soft tissue repair – Faster, no repositioning, fewer incisions – Tension free closure of abdominal wall • Bilateral superior pubic ramus osteotomies between pectineus & adductor insertions • Medial segments tilted toward midline, suture secured through cartilagenous symphysis • Problem: almost always have complete recurrence of diastasis
Anterior Diagonal Iliac Osteotomy • Originated from computer modeling (1990 s) • Diagonal osteotomy, greater sciatic notch 12 cm posterior to ASIS – Optional bone graft in defect • Pelvis compressed rami approximated symphysis secured with suture • Best of both worlds: – Tension free closure, faster, no repositioning – Lowest wound infection and dehiscence rates – Failure rate similar to posterior iliac osteotomy
dda8bf1bb6661b7f2d6287164128d323.ppt