47f8d6bf6aab761c23c86e457e44eaaa.ppt
- Количество слайдов: 25
 Organ Donor Detection, Identification and Clinical Evaluation Essentials in Organ Donation
Organ Donor Detection, Identification and Clinical Evaluation Essentials in Organ Donation
 Types of Donors (Solid organs and tissues) • Living • Cadaveric – Cardiac arrest – Asystolic donors • Tissue Only Donors • Non-Heart-Beating Donors (Donors after Cardiac Death) – Encephalic death (Heart-beating donors) 2
Types of Donors (Solid organs and tissues) • Living • Cadaveric – Cardiac arrest – Asystolic donors • Tissue Only Donors • Non-Heart-Beating Donors (Donors after Cardiac Death) – Encephalic death (Heart-beating donors) 2
 Who becomes a potential Donor No age limitations ! • BDD (cerebral vascular diseases, cranio-cerebral trauma, hypoxic encephalopathy, etc. ) • CAD (Maastricht) in hospital / out of hospital (Failure of CPR, unexpected cardiac arrest of brain-dead patients, withdrawal of life support)
Who becomes a potential Donor No age limitations ! • BDD (cerebral vascular diseases, cranio-cerebral trauma, hypoxic encephalopathy, etc. ) • CAD (Maastricht) in hospital / out of hospital (Failure of CPR, unexpected cardiac arrest of brain-dead patients, withdrawal of life support)
 Non-heart-beating donors NHBD • Witnessed Cardiopulmonary Arrest • Complex proceedings in very short time • Cooling and preservation started in less than 30 min • Kidney, Liver, Lung, Tissues • Types (Maastrich 1995) 1. CPA outside hospital 2. Failure of CPR in Witnessed CPA 3. CPA after withdrawing therapy in ICU 4. In ICU, patients being assessed as brain dead donors who suffer an irreversible unexpected CPA 4
Non-heart-beating donors NHBD • Witnessed Cardiopulmonary Arrest • Complex proceedings in very short time • Cooling and preservation started in less than 30 min • Kidney, Liver, Lung, Tissues • Types (Maastrich 1995) 1. CPA outside hospital 2. Failure of CPR in Witnessed CPA 3. CPA after withdrawing therapy in ICU 4. In ICU, patients being assessed as brain dead donors who suffer an irreversible unexpected CPA 4
 Encephalic Death Donors • Declared dead based on neurological criteria • Heart-beating donors • Must die in hospital • Main source of organs 5
Encephalic Death Donors • Declared dead based on neurological criteria • Heart-beating donors • Must die in hospital • Main source of organs 5
 Tissue Donors. Peculiarities • Death could occur outside the hospital • Big potential pool of tissue donors • Tissues can be obtained several hours after cardiopulmonary arrest • Cornea, Bone, Skin, Tendons, Cardiac Valves, Vessels … • Afterwards, tissues are preserved and banked 6
Tissue Donors. Peculiarities • Death could occur outside the hospital • Big potential pool of tissue donors • Tissues can be obtained several hours after cardiopulmonary arrest • Cornea, Bone, Skin, Tendons, Cardiac Valves, Vessels … • Afterwards, tissues are preserved and banked 6
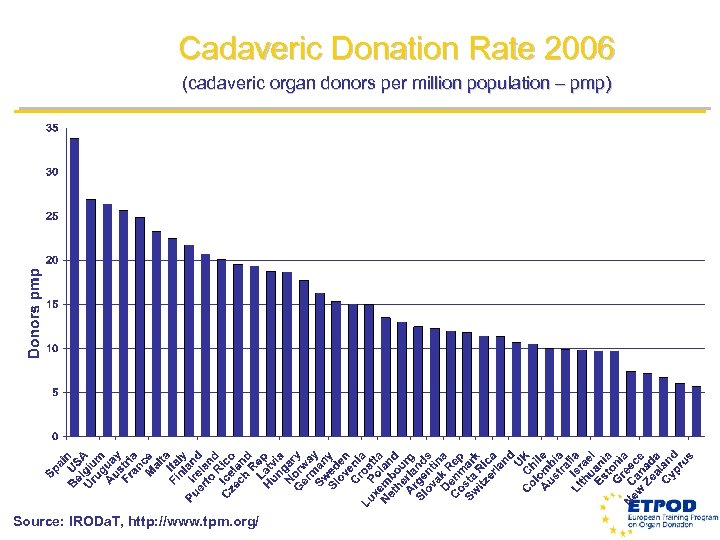 Cadaveric Donation Rate 2006 (cadaveric organ donors per million population – pmp) Source: IRODa. T, http: //www. tpm. org/
Cadaveric Donation Rate 2006 (cadaveric organ donors per million population – pmp) Source: IRODa. T, http: //www. tpm. org/
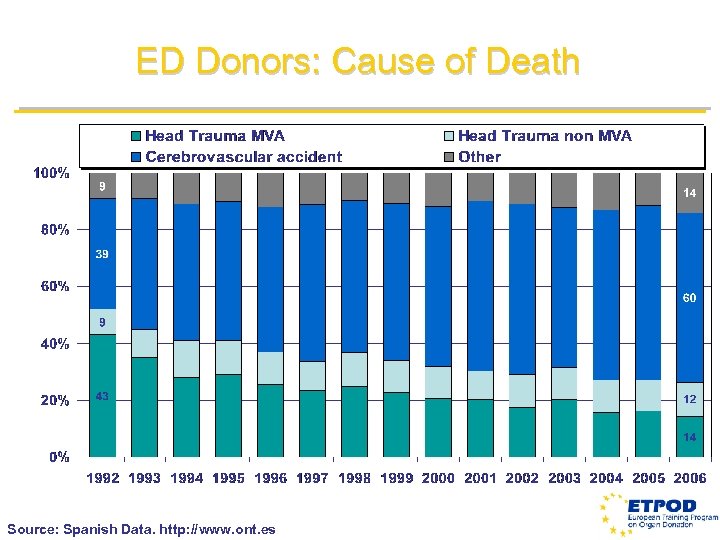 ED Donors: Cause of Death Source: Spanish Data. http: //www. ont. es
ED Donors: Cause of Death Source: Spanish Data. http: //www. ont. es
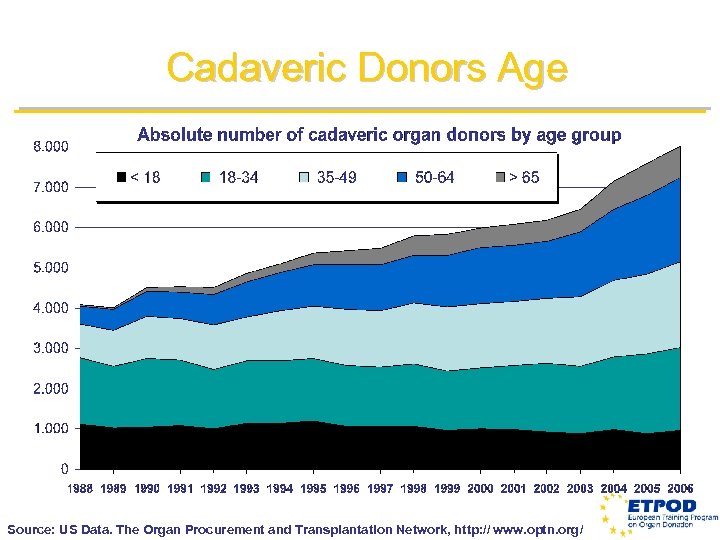 Cadaveric Donors Age Source: US Data. The Organ Procurement and Transplantation Network, http: // www. optn. org/
Cadaveric Donors Age Source: US Data. The Organ Procurement and Transplantation Network, http: // www. optn. org/
 Organ donor potentiality • 50 donors pmp / year (in Spain) • 1, 5 donors* / 100 hospital deaths • 2, 5 donors* / 100 hospital beds / year • 10 donors* / 100 ICU deaths • 50 donors* / 100 ICU beds / year * In hospitals with a neurosurgery dept. (half of that in case of no neurosurgery)
Organ donor potentiality • 50 donors pmp / year (in Spain) • 1, 5 donors* / 100 hospital deaths • 2, 5 donors* / 100 hospital beds / year • 10 donors* / 100 ICU deaths • 50 donors* / 100 ICU beds / year * In hospitals with a neurosurgery dept. (half of that in case of no neurosurgery)
 How to detect • Administrative way (reviewing all the patients admitted in 24 hours) • Active way (daily visits to ICU, reviewing CT scans etc. ) • Passive way ( waiting for other health staff or medical centers to notify)
How to detect • Administrative way (reviewing all the patients admitted in 24 hours) • Active way (daily visits to ICU, reviewing CT scans etc. ) • Passive way ( waiting for other health staff or medical centers to notify)
 Tools for detection • Staff (available team, health workers knowing how to contact them) • Protocols (local, area, national, european) • Communications network (ICU and in/out emergency systems/dept. )
Tools for detection • Staff (available team, health workers knowing how to contact them) • Protocols (local, area, national, european) • Communications network (ICU and in/out emergency systems/dept. )
 Organ Donor Clinical Evaluation
Organ Donor Clinical Evaluation
 General Donor Evaluation • Evaluate the risk of disease transmission through organ transplantation – Infections – Tumors • Ensure that transplanted organs will function 14
General Donor Evaluation • Evaluate the risk of disease transmission through organ transplantation – Infections – Tumors • Ensure that transplanted organs will function 14
 Donor Evaluation Main points • Family interview • History • Clinical evaluation
Donor Evaluation Main points • Family interview • History • Clinical evaluation
 Donor Evaluation History • Medical family antecedents • Risk factors (sexual habits, drug abuse, smoking, traveling. . ) • Medical antecedents (previous diseases and treatments)
Donor Evaluation History • Medical family antecedents • Risk factors (sexual habits, drug abuse, smoking, traveling. . ) • Medical antecedents (previous diseases and treatments)
 Donor Evaluation Clinical evaluation • • • Identification of brain death‘s cause Physical examination Current medical history Current clinical state Laboratory Imagery data
Donor Evaluation Clinical evaluation • • • Identification of brain death‘s cause Physical examination Current medical history Current clinical state Laboratory Imagery data
 General Donor Evaluation • Physical examination – Traumatism – Tattoos and piercing – Genital Areas – Thyroid, breasts, testicles, lymph nodes – Rectal exam – Non-medical injections of drugs – Skin Cancers – Scars of previous surgery 18
General Donor Evaluation • Physical examination – Traumatism – Tattoos and piercing – Genital Areas – Thyroid, breasts, testicles, lymph nodes – Rectal exam – Non-medical injections of drugs – Skin Cancers – Scars of previous surgery 18
 Donor Evaluation Current Clinical State – Current treatment and status in ICU • Volume replacement • Temperature maintenance • Correction of diabetes insipidus • Suspected or Documented infection ? • Antibiotics
Donor Evaluation Current Clinical State – Current treatment and status in ICU • Volume replacement • Temperature maintenance • Correction of diabetes insipidus • Suspected or Documented infection ? • Antibiotics
 Donor Evaluation Current Clinical Situation – Hemodynamic Status • AP, CVP, HR, UO • Cathecolamines, dose, timing • Cardiac arrest • Episodes of hypotension • Hemodilution – Respiratory • Hipoxemia, acidosis – Metabolic • Electrolytes, glucemia
Donor Evaluation Current Clinical Situation – Hemodynamic Status • AP, CVP, HR, UO • Cathecolamines, dose, timing • Cardiac arrest • Episodes of hypotension • Hemodilution – Respiratory • Hipoxemia, acidosis – Metabolic • Electrolytes, glucemia
 Donor Evaluation • Serological determinations – HIV – Hepatitis B – Hepatitis C – Other • CMV, toxoplasma, EBV, HTLV, syphilis, malaria, tuberculosis 21
Donor Evaluation • Serological determinations – HIV – Hepatitis B – Hepatitis C – Other • CMV, toxoplasma, EBV, HTLV, syphilis, malaria, tuberculosis 21
 Donor Evaluation Other tests • • ECG Chest X – ray Abdominal Ultrasound Echocardiography Coronary Angiography Retinal vessels Bronchoscopy
Donor Evaluation Other tests • • ECG Chest X – ray Abdominal Ultrasound Echocardiography Coronary Angiography Retinal vessels Bronchoscopy
 Absolute Contraindications: Infections • HIV (or Risk Factors) • Generalized infection – Sepsis with systemic involvement – Systemic acute viral infection – Active tuberculosis • Other – Viral encephalitis – Prion diseases – Tropical diseases
Absolute Contraindications: Infections • HIV (or Risk Factors) • Generalized infection – Sepsis with systemic involvement – Systemic acute viral infection – Active tuberculosis • Other – Viral encephalitis – Prion diseases – Tropical diseases
 Absolute Contraindications: Tumors • Any malignancy within the last 5 years – Exceptions • Some low-grade primary CNS tumors • Carcinoma basocellular of the skin • Carcinoma in situ of the uterine cervix – Rule out incidental cancer • Abdominal and thoracic inspection during organ extraction • Donor autopsy in selected cases
Absolute Contraindications: Tumors • Any malignancy within the last 5 years – Exceptions • Some low-grade primary CNS tumors • Carcinoma basocellular of the skin • Carcinoma in situ of the uterine cervix – Rule out incidental cancer • Abdominal and thoracic inspection during organ extraction • Donor autopsy in selected cases
 Conclusion Balance Risk and Benefit
Conclusion Balance Risk and Benefit


