daa73acda39de7e369b7705f514c08cf.ppt
- Количество слайдов: 78
Orbital Tumors Yaser Badr MD Neurosurgery OCT 08
What is the Orbit?
Introduction Does a mass lesion cause the symptom? What is the nature of this lesion? Is it surgical? What is the surgical approach of choice?
CLINICAL PRESENTATION
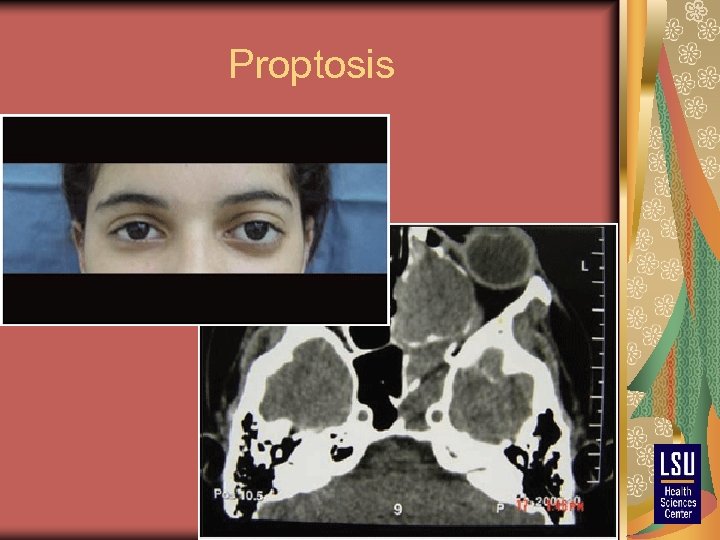
Proptosis
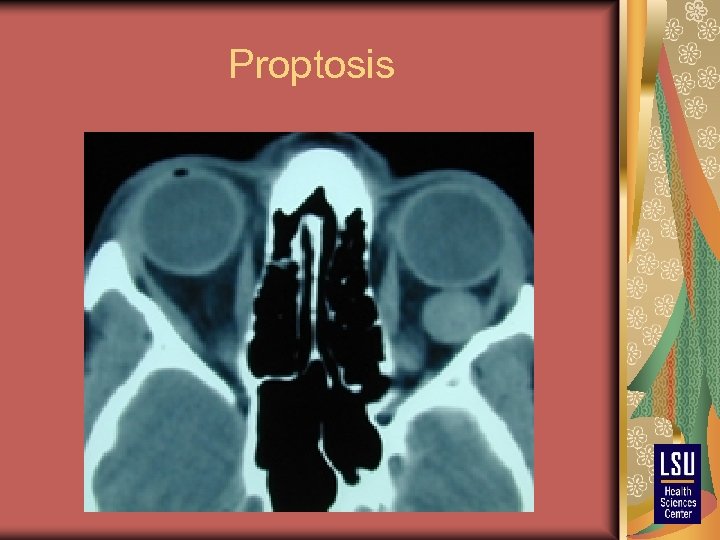
Proptosis
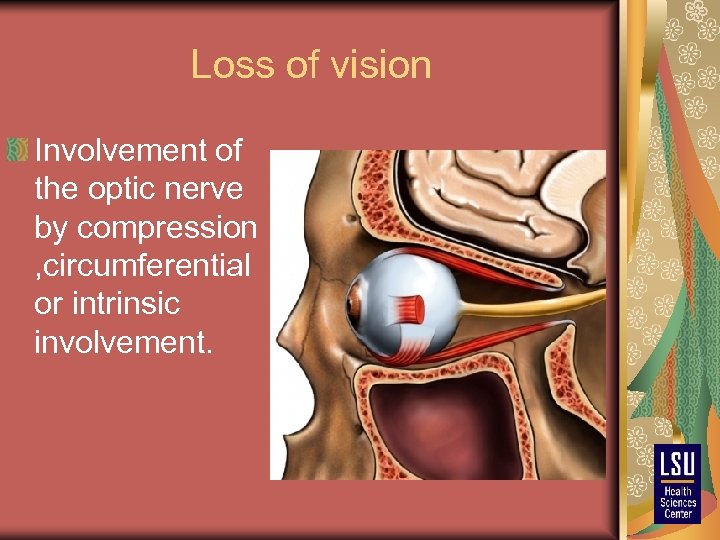
Loss of vision Involvement of the optic nerve by compression , circumferential or intrinsic involvement.
Diplopia is caused by ophthalmoplegia, which may result from neural dysfunction or local orbital disease restricting the motion of the globe and the extraocular muscles.
RADIOLOGIC STUDIES Computed tomography (CT) Magnetic resonance imaging (MRI) Ultrasonography Angiography
CT Delineate the bony involvement Contrast between the lesion and the orbital fat precisely Coronal reconstruction images can precisely reveal involvement of the optic canal in disease involving the bony structure. i. e. , fibrous dysplasia and sphenoid meningiomas

MRI Fat-suppression sequences to allow precise visualization of the lesion. MRI also identifies more clearly the relationship between a posterior orbital mass and the optic nerve if axial and coronal views are obtained with contrast and fat suppression.
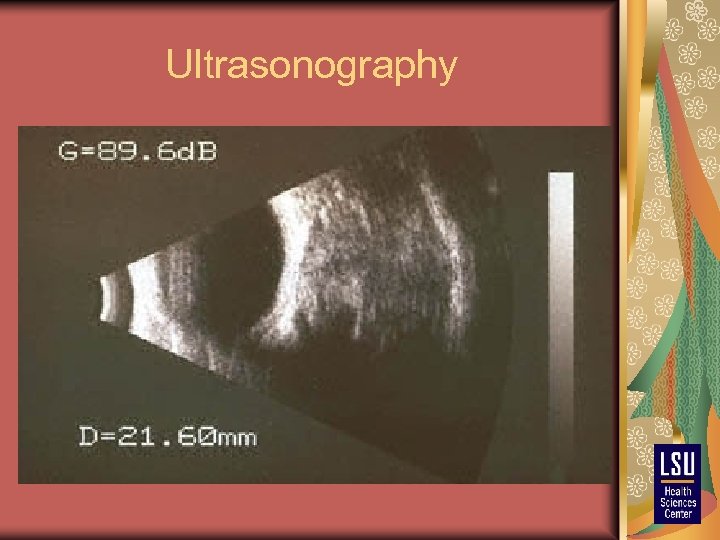
Ultrasonography
Angiography Replaced by MR angiography Mostly used for vascular lesions of the orbit, mainly arteriovenous malformations and arteriovenous fistulas MR venography can delineate orbital varices and confirm venous occlusive disease such as cavernous sinus thrombosis
MANAGEMENT ALGORITHM Treatment is chosen according to the specific pathologic entity If the lesion is surgical, the pathologic diagnosis can be definitively established with surgery If radiotherapy is contemplated or if the imaging features are equivocal, fine-needle aspiration biopsy is warranted in anterior, infiltrative lesions to verify the accurate pathologic diagnosis
MANAGEMENT ALGORITHM Nonsurgical cases, observation is warranted with serial imaging and neuro-ophthalmic examinations. .
TYPES OF SURGICAL APPROACHES There are two types of surgical approaches: the transorbital approaches, which are undertaken by the ophthalmologist alone. extraorbital approaches, which are best performed in collaboration with a neurosurgeon or an ENT surgeon.
Transorbital Approaches 1)Anterior orbitotomy 2)Lateral orbitotomy 3)Medial orbitotomy 4)Combination of the lateral and medial orbitotomies.
Extraorbital Approaches There are two primary extraorbital approaches: 1) The frontotemporal approach 2) The inferior orbital approach.
Which one to do?
Lesions with intracranial extension, lesions involving the optic canal, or lesions medial to the optic nerve in the apex are approached through the transcranial frontoorbital temporal approach. Lesions lateral to the optic nerve and apex are treated through a lateral microsurgical approach. Tumor located anteriorly in the orbit may be approached anteriorly through an eyelid incision or conjunctival incision.
Lesions medial to the optic nerve are best approached through a medial orbitotomy. If the lesions are large or posterior, the medial orbitotomy can be combined with a lateral orbitotomy for improved exposure. Sphenoid wing meningiomas with orbital extension are removed through a pterional approach
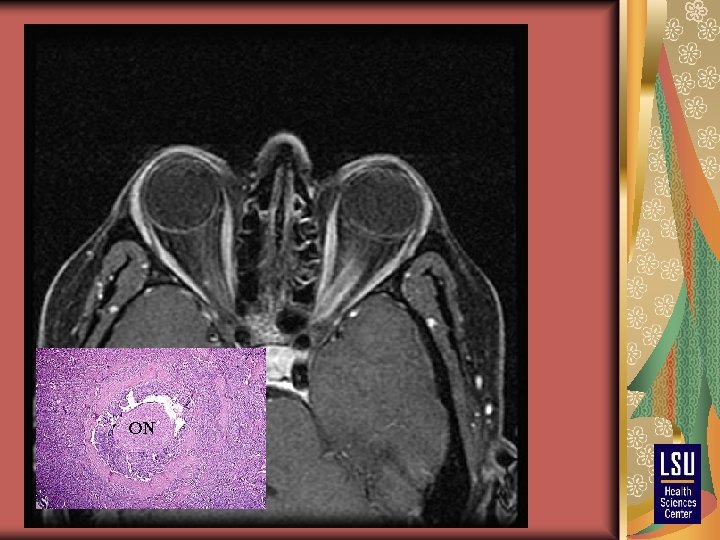
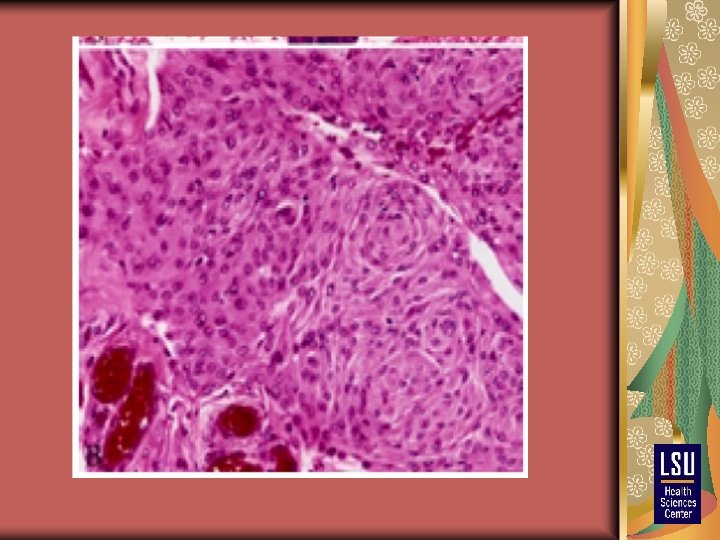
Orbital Meningiomas 5% and 20% of orbital tumors They can be purely intraorbital or within the sphenoid wing or periorbita with secondary orbital involvement Typically manifest in women in their fourth or fifth decade Younger age group, they may be associated with neurofibromatosis (NF).
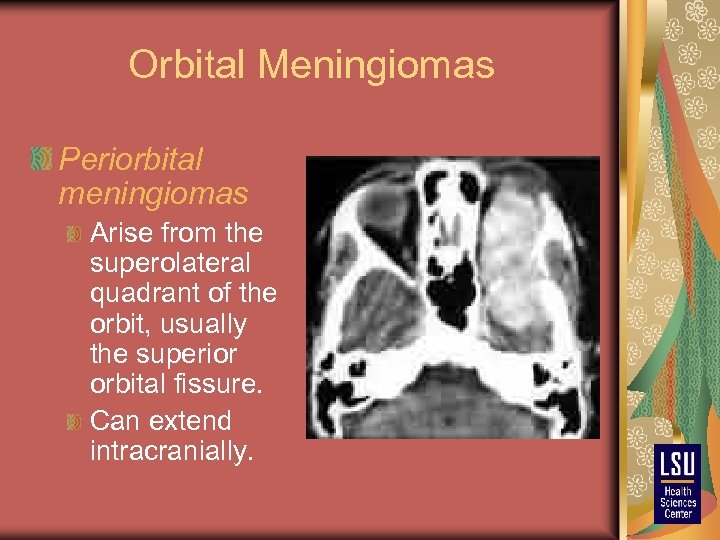
Orbital Meningiomas Periorbital meningiomas Arise from the superolateral quadrant of the orbit, usually the superior orbital fissure. Can extend intracranially.
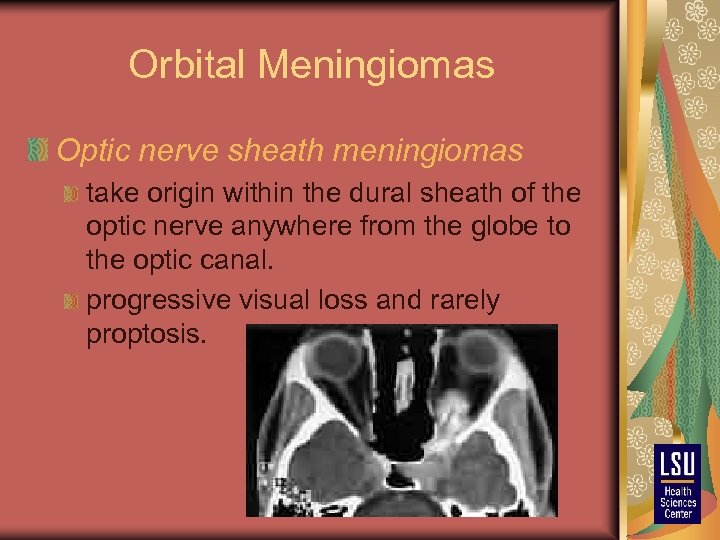
Orbital Meningiomas Optic nerve sheath meningiomas take origin within the dural sheath of the optic nerve anywhere from the globe to the optic canal. progressive visual loss and rarely proptosis.
Management of orbital meningioma Sphenoid wing meningiomas surgical resection by the pterional approach. If there is optic canal involvement, optic canal decompression should be performed. Excision of the involved bone and dura is important. Postoperative irradiation for incompletely resected tumors will retard regrowth of the tumor.
Management of orbital meningioma Optic nerve sheath meningioma Patients with stable vision and anteriorly located or apical meningioma are followed closely with imaging and visual studies. With progressive visual loss, external beam radiation therapy (50 Gy) is recommended. There is evidence that radiation can arrest the growth of optic nerve sheath meningiomas and preserve vision. Aggressive resection in sighted patients results in postoperative visual loss!. If the vision is lost completely, the tumor is resected transcranially, especially if growth is demonstrated on neuroimaging.
Optic Nerve Gliomas Optic nerve gliomas account for 2% to 5% of orbital tumors. Typically occur in the first decade of life Can be solitary or associated with neurofibromatosis type 1 (NF 1). When bilateral, they are pathognomonic of NF 1.
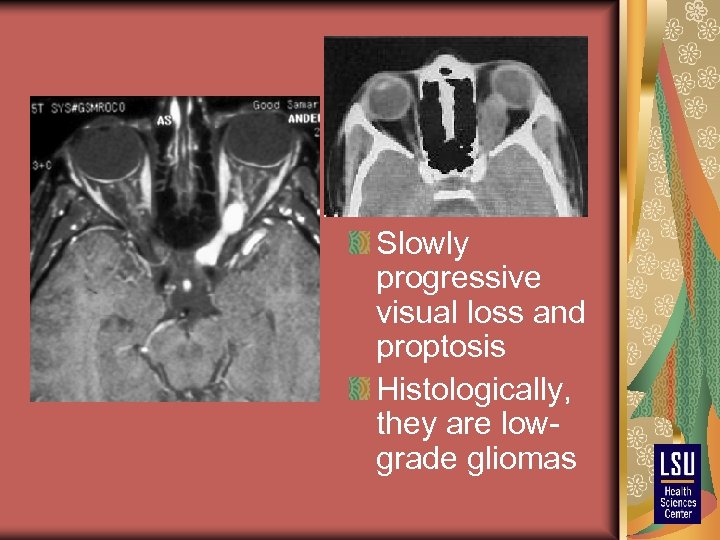
Slowly progressive visual loss and proptosis Histologically, they are lowgrade gliomas
Management of Optic Nerve Glioma Without evidence of radiologic growth or clinical deterioration, observation is the best management. Surgery is recommended when there is significant loss of vision or radiologic progression. Surgery is resection of the optic nerve Chiasmatic involement requires radiation therapy. Malginant variant treated also by radiation therapy with lethal outcome within a year.
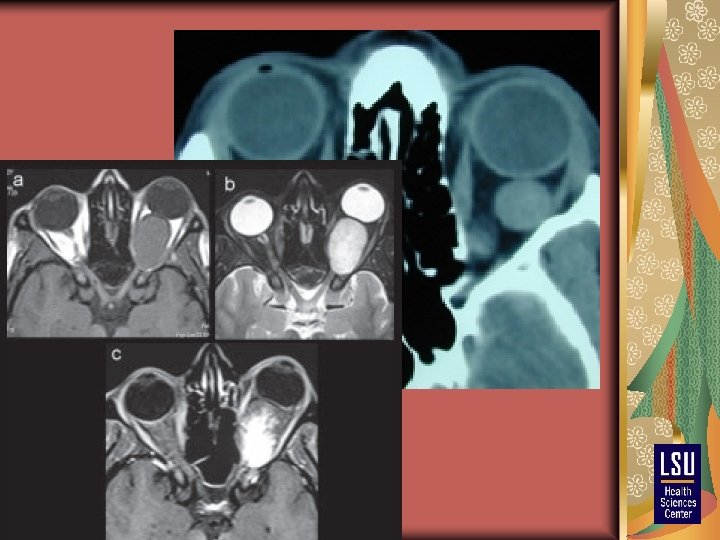
Cavernous Hemangioma Occur most commonly in adults in the second to fourth decades of life. They comprise 10% to 30% of tumors causing proptosis in this age group. The most common primary benign orbital tumor in adults.

Encapsulated with a good cleavage plane from the adjacent structures
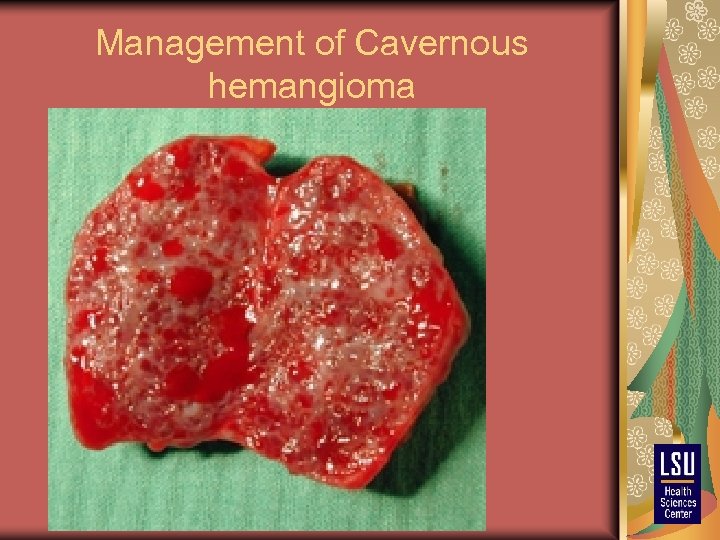
Management of Cavernous hemangioma
Peripheral Nerve Tumors of the Orbit Peripheral nerve tumors constitute 5% to 15% of orbital tumors Solitary neurofibromas. Diffuse neurofibromas. Plexiform neurofibromas. Schwannomas. Malignant peripheral nerve tumors.
Solitary neurofibromas Older age group between the third and fifth decades. Slowly progressive, painless proptosis and with minimal or no visual dysfunction. Typically located in the superolateral orbital quadrant and produce upward gaze limitation. CT/MRI, they are homogenous, wellcircumscribed, enhancing lesions. Treatment is surgical, using the anterior medial, lateral, or transcranial route.
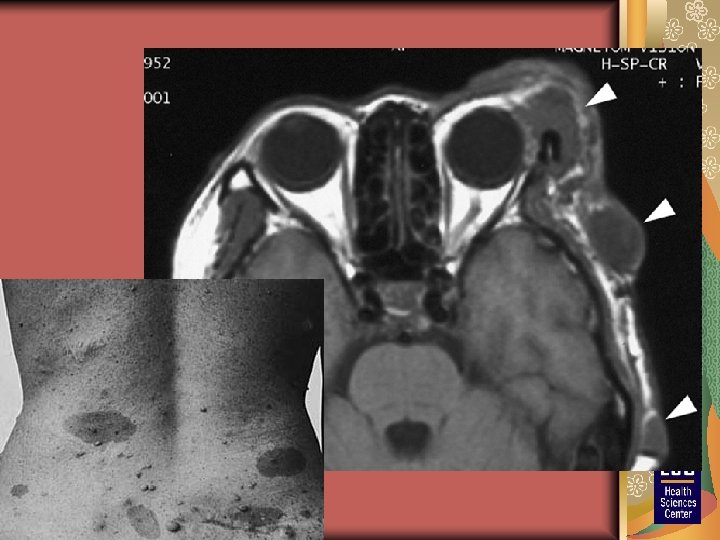
Plexiform neurofibromas Younger age group, mostly infants and children. associated with NF Palpable mass in the eyelid (usually lateral third) with subsequent ptosis and lid hypertrophy CT and MRI, these lesions are infiltrative with irregular borders and enhance with contrast. Do not have a good dissection plane, making total excision almost impossible and recurrence frequent. The goal of surgery is to debulk the tumor.
Schwannomas Benign tumors that arise form peripheral nervous system Schwann cells Second to fifth decades of life, and there is a slight female predilection Proptosis and dysmotility, these tumors may manifest with trigeminal distribution of pain and numbness.
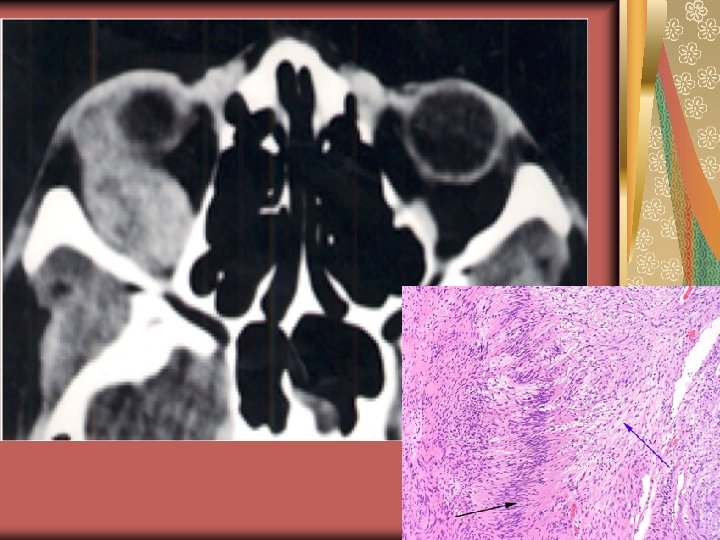
Malignant peripheral nerve tumors Rare, with less than 15 reported cases. They are aggressive and commonly have intracranial extension into the middle fossa. Treatment consists of excision with subsequent radiotherapy or chemotherapy.
Dermoid and Epidermoid Cysts Dermoid cysts usually occur in children and make up 4% to 6% of orbital tumors. Painless mass, free from the skin, with variable ocular displacement The intensity of dermoid and epidermoid cysts is similar to that of fat on MRI and CT.
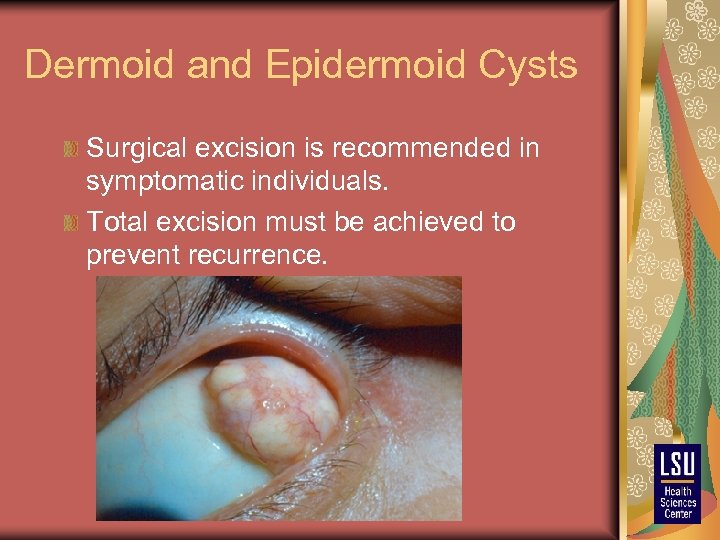
Dermoid and Epidermoid Cysts Surgical excision is recommended in symptomatic individuals. Total excision must be achieved to prevent recurrence.
Osteomas Form 1% of orbital tumors. They are usually extraperiosteal pedunculated masses displacing the eyeball. They may be isolated or associated with Gardner's syndrome. The diagnosis can be made on the basis of plain x-ray films or CT with bone windows.
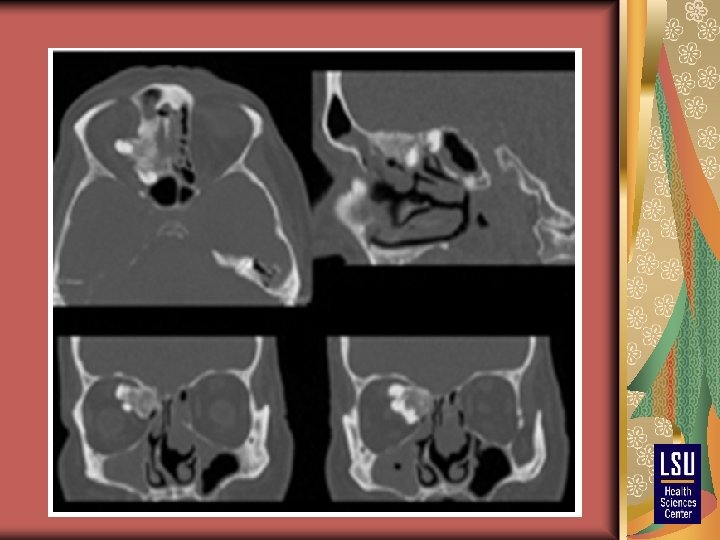
Treatment is indicated for symptomatic lesions and is usually surgical. The approach depends on the location of lesion.
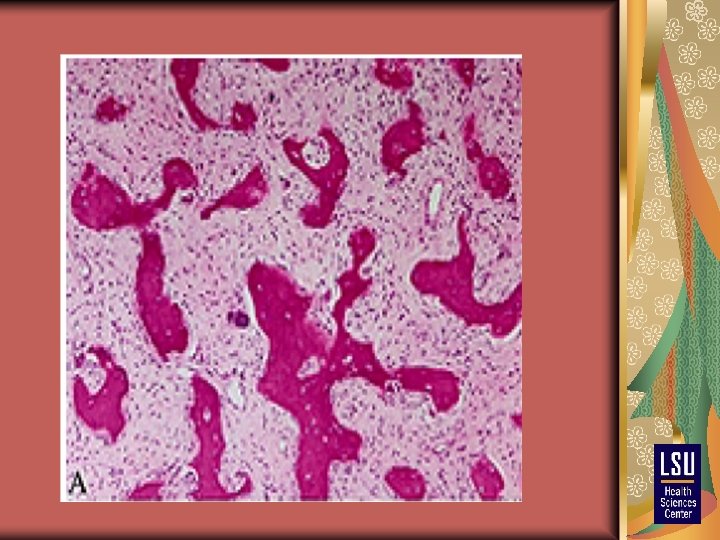
Fibrous Dysplasia Bone disease occurring most commonly in children and young adults It can be mono-ostotic or polyostotic It occurs in the first 2 decades of life. The clinical presentation depends on the bone involved
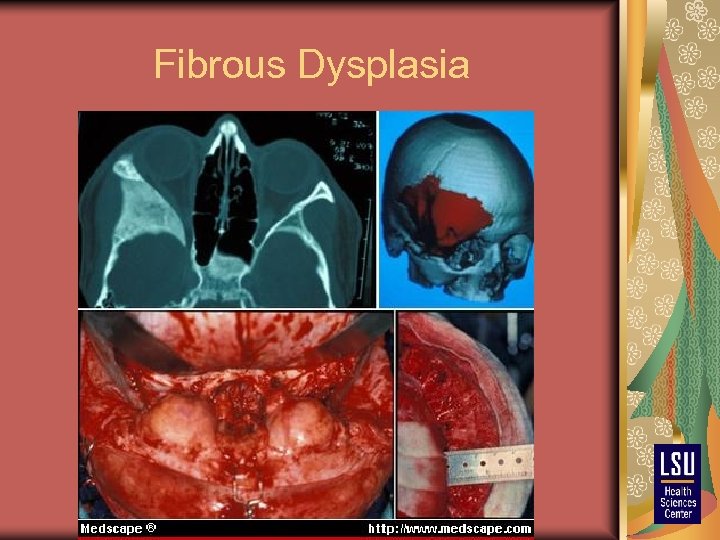
Fibrous Dysplasia
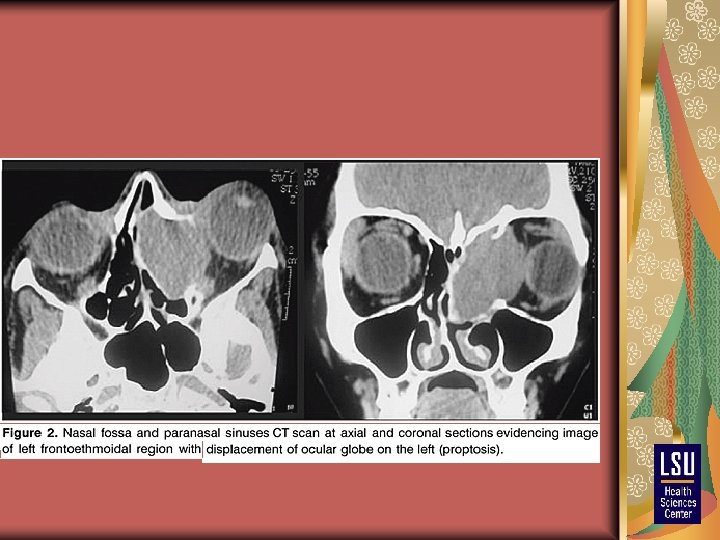
Mucocele Cystic lesions, with a wall formed by the mucous lining of the sinuses. Arise from the paranasal sinuses when there is an obstruction to the normal draining pathways. Long-standing obstruction leads to outward expansion of the sinus. The bony walls expand may completely disappear, but the periosteal lining persists.
Orbital Rhabdomyosarcoma Most common primary orbital malignant tumor in children. Usually seen before age 16, with an average of 7 years at presentation. Usually unilateral. These tumors present with a rapidly progressive proptosis.
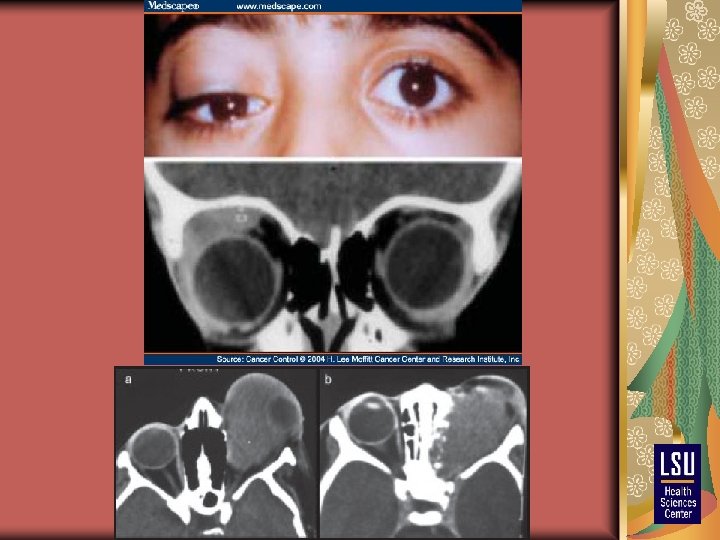
Orbital Rhabdomyosarcoma Diagnosis is based on the clinical progression and the radiologic features but must be confirmed by tissue analysis Fine-needle aspiration of the orbital component is sometimes diagnostic
Orbital Rhabdomyosarcoma Prompt treatment is indicated to improve the outcome and avoid blindness. Excision of the maximal amount of tumor with the least morbidity is followed by radiation therapy and chemotherapy. Survival depends on the amount of residual tumor. The 5 -year survival varies from 90% for minimal or no residual disease to 35% for significant residual tumor.
Fibrous Histiocytoma
Metastatic Lesions Six percent of orbital tumors are metastases.
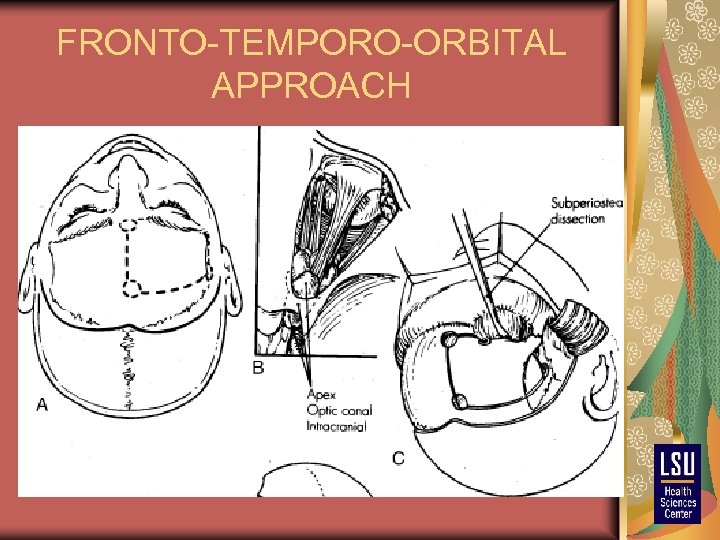
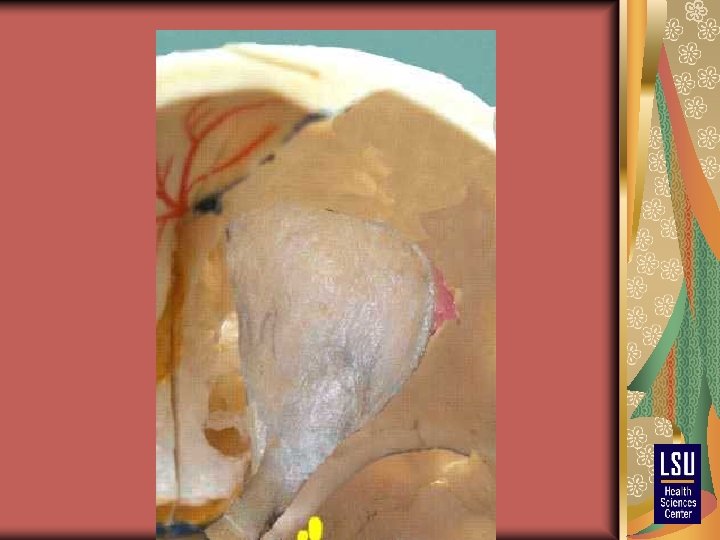
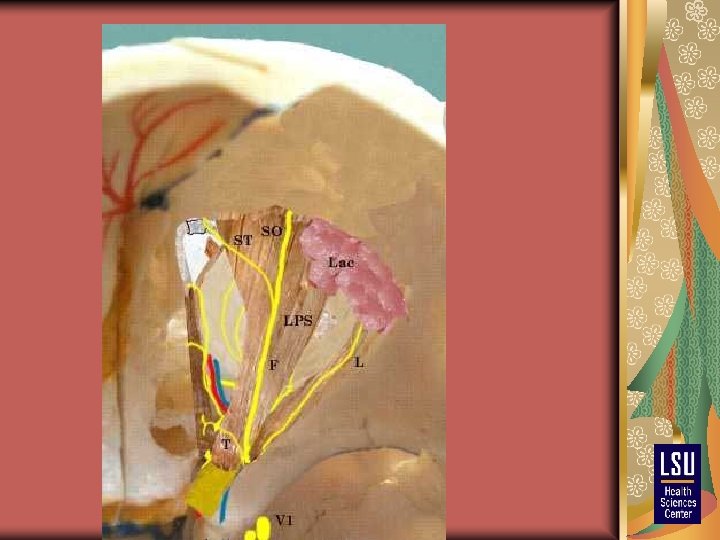
FRONTO-TEMPORO-ORBITAL APPROACH
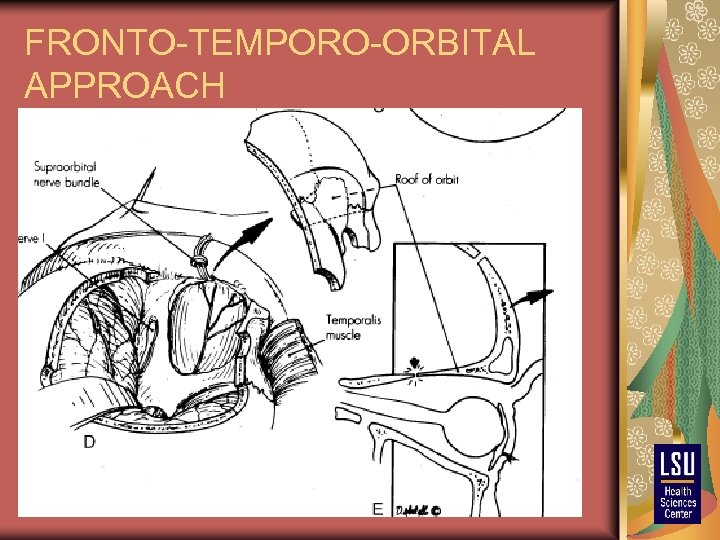
FRONTO-TEMPORO-ORBITAL APPROACH
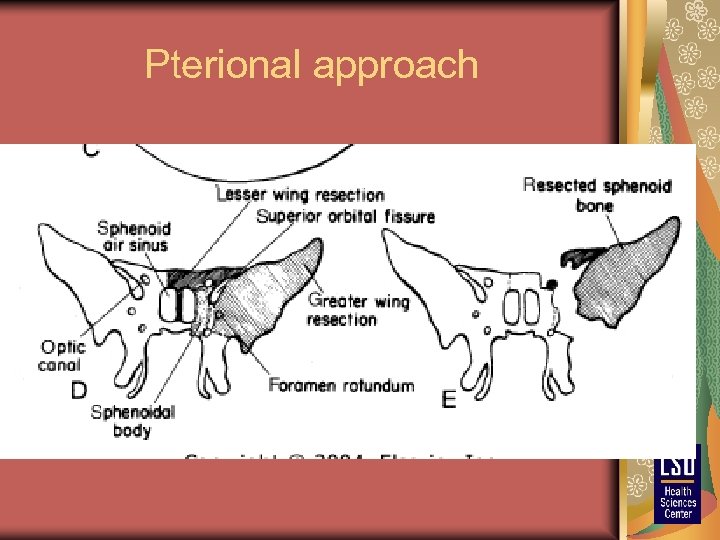
Pterional approach
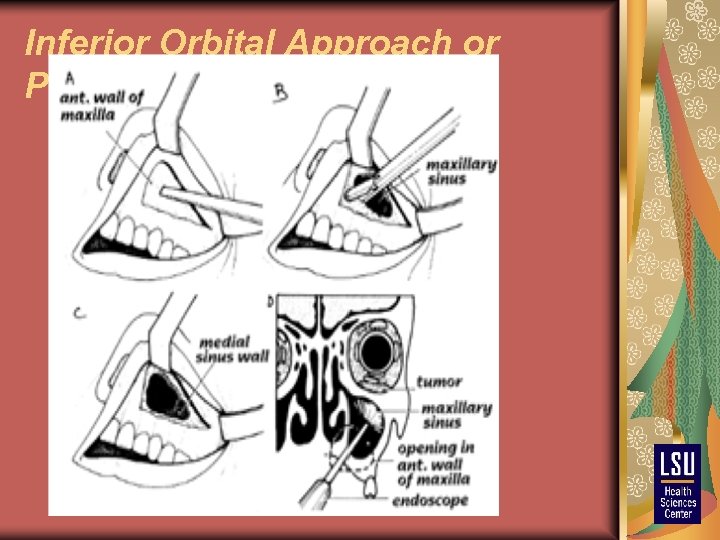
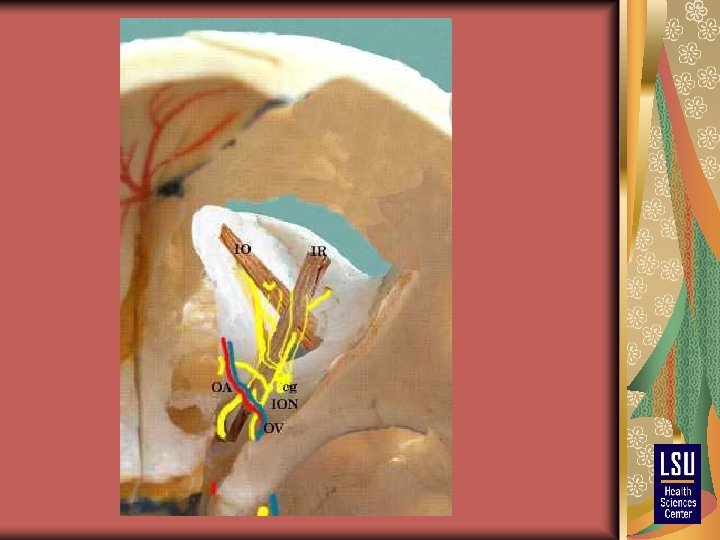
Inferior Orbital Approach or Posteroinferior Orbitotomy
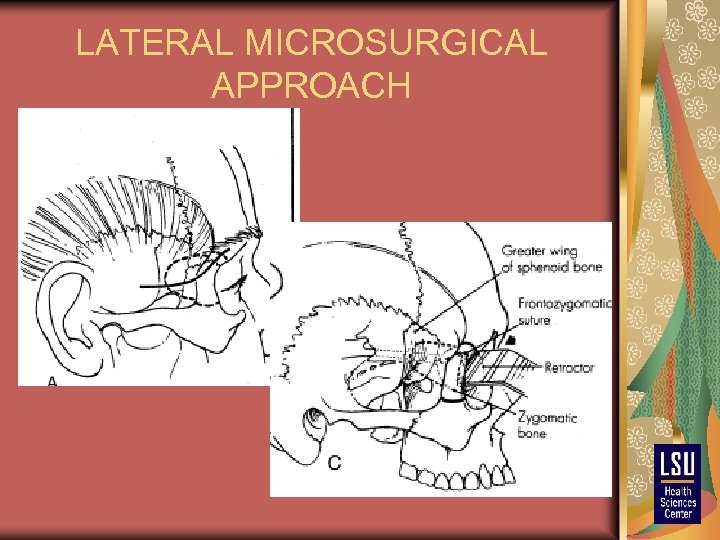
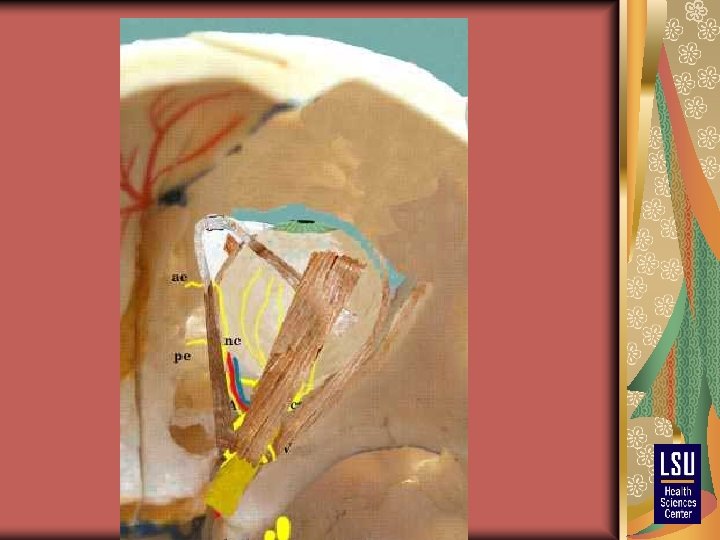
LATERAL MICROSURGICAL APPROACH
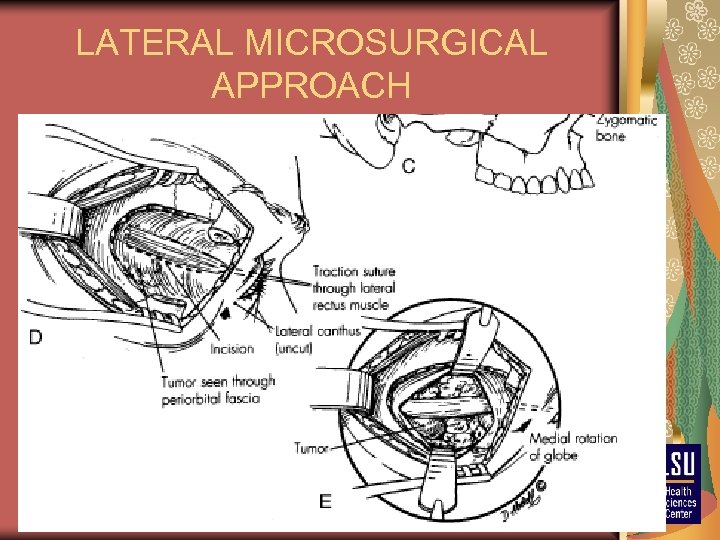
LATERAL MICROSURGICAL APPROACH
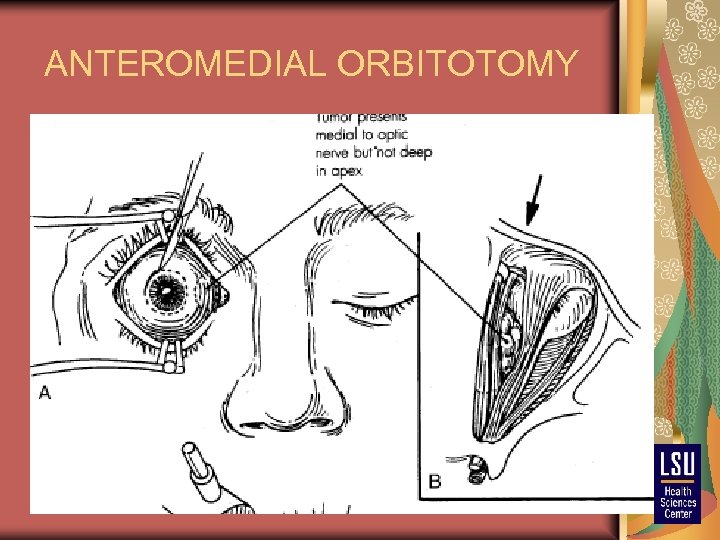
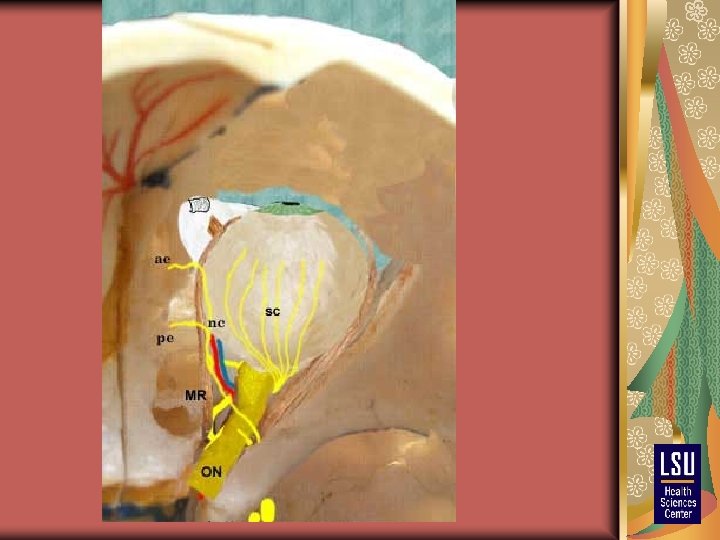
ANTEROMEDIAL ORBITOTOMY
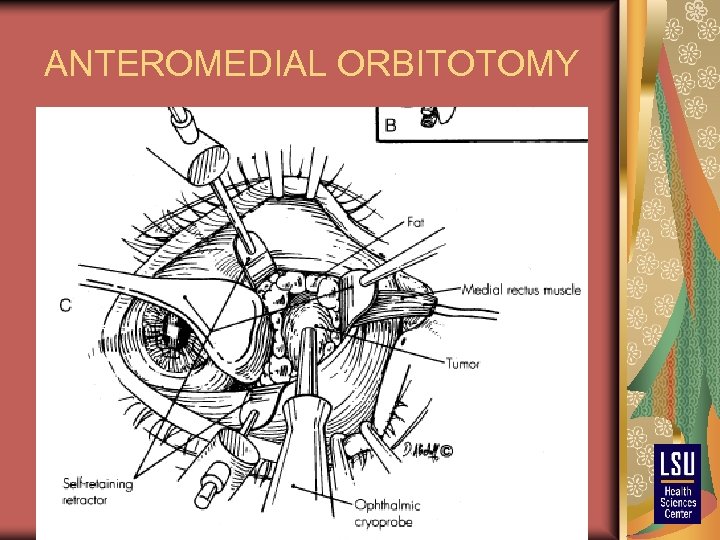
ANTEROMEDIAL ORBITOTOMY
CONCLUSION Orbital tumors encompass a wide clinical spectrum and can present diagnostic and therapeutic dilemmas. Diagnosis is greatly facilitated by modern neuroimaging techniques and by fine-needle aspiration biopsy for infiltrating lesions. External beam radiation therapy plays an important role in the management of gliomas, meningiomas, lymphomas, and orbital inflammation. The surgical management of orbital tumors has benefited from the cooperation between neurosurgeons and ophthalmologists with special expertise in orbital disease and skull base surgery.
daa73acda39de7e369b7705f514c08cf.ppt