e36384036d80f7d9628ee98aee4595c4.ppt
- Количество слайдов: 16

Orbital Pseudotumor with Wegener's Granulomatosis Developing Antiphospholipid Syndrome Authors: Tatiana Rosca, MD, Ph. D, * Cristina Tanaseanu, MD, Ph. D, ** Codruţ Sarafoleanu, MD, Ph. D, *** Ana Tatiana Şerban, MD **** *Emergency Clinical Hospital St. Pantelimon , Neurosurgery Departmnet, Bucharest, Romania ** Emergency Clinical Hospital St. Pantelimon, Internal Medicine Department, Bucharest, Romania *** Clinical Hospital Sf. Maria, ENT Department, Bucharest, Romania ****Endocrinology Institute I. C. Parhon, Bucharest, Romania
Aim: We report a rare case of Wegener granulomatosis eventually ending in catastrophic antiphospholipid syndrome. Method: A 42 year- old female patient, diagnosed and treated for Wegener granulomatosis since 14 y. o. , suddenly manifests a left orbital pseudotumor. The clinical exam revealed: left orbital panniculitis, visual acuity loss, papillary oedema in the left eye and limited motility of the left globe. Results: The investigations demonstrated the presence of the infectious Lysteria monocitogenes causing orbital pseudotumor. The treatment targeted both the infectious cause and the Wegener granulomatosis. The outcome was the anatomic recovery of the left globe, but the function was lost. Discussion: Besides the granulomatosis vasculitis, the presence of the microorganisms also induces increased antiphospholipid antibodies (APLA). APLA induce cell humoral immunity disorders, as a consequence of the infectious process. Conclusion: The infection represents the mutual trigger both for the increase of c. ANCA and for the exacerbation of the thrombosis mechanism due to APLA, leading finally to a catastrophic antiphospholipid syndrome. The evolution pattern of the antiphospholipid antibodies leads to the catastrophic systemic inflammatory syndrome, due to the second infection impossible to controle two years after.
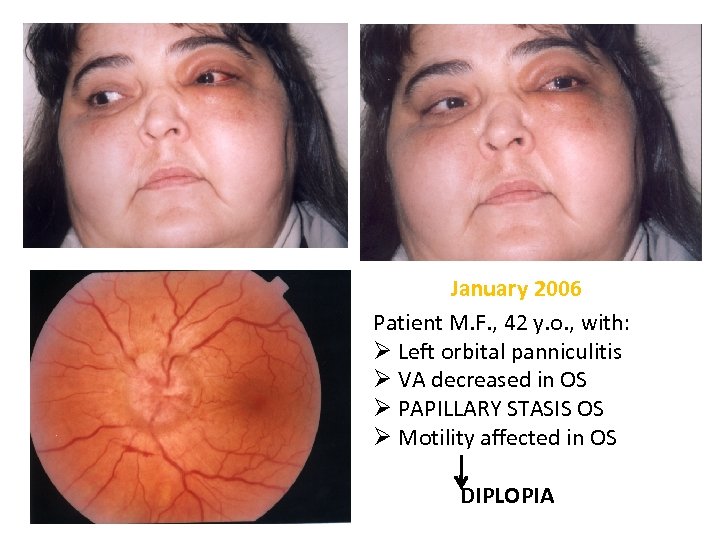
January 2006 Patient M. F. , 42 y. o. , with: Ø Left orbital panniculitis Ø VA decreased in OS Ø PAPILLARY STASIS OS Ø Motility affected in OS DIPLOPIA
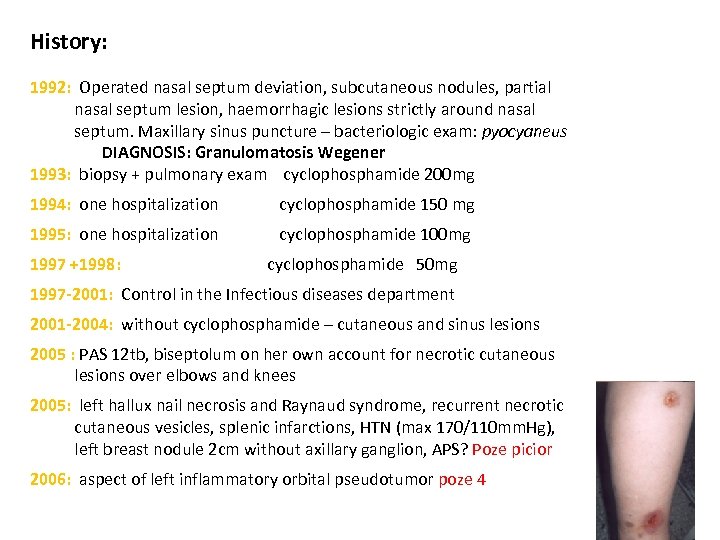
History: 1992: Operated nasal septum deviation, subcutaneous nodules, partial nasal septum lesion, haemorrhagic lesions strictly around nasal septum. Maxillary sinus puncture – bacteriologic exam: pyocyaneus DIAGNOSIS: Granulomatosis Wegener 1993: biopsy + pulmonary exam cyclophosphamide 200 mg 1994: one hospitalization cyclophosphamide 150 mg 1995: one hospitalization cyclophosphamide 100 mg 1997 +1998: cyclophosphamide 50 mg 1997 -2001: Control in the Infectious diseases department 2001 -2004: without cyclophosphamide – cutaneous and sinus lesions 2005 : PAS 12 tb, biseptolum on her own account for necrotic cutaneous lesions over elbows and knees 2005: left hallux nail necrosis and Raynaud syndrome, recurrent necrotic cutaneous vesicles, splenic infarctions, HTN (max 170/110 mm. Hg), left breast nodule 2 cm without axillary ganglion, APS? Poze picior 2006: aspect of left inflammatory orbital pseudotumor poze 4
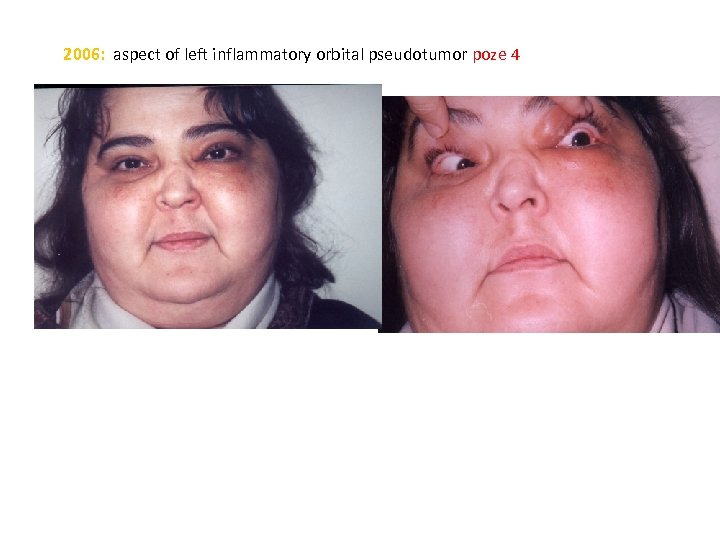
2006: aspect of left inflammatory orbital pseudotumor poze 4
Invastigation: ESR = 40 mm/1 hour, fibrinogen = 519, thrombocytes = 450, 000 Hb = 11, 9%; The tuberculin skin test (IDR) = + 15, c-ANCA = normal, C-reactive protein = normal Ø Lungs: pulmonary x-ray – enlarged right hilar Ø Kidneys : AP max = 170 mm. Hg, creatinine = normal Ø Left breast nodule 2 cm without axillary ganglion, normal left breast mammography, Ø Recurrent necrotic cutaneous vesicles LA = positive, aß 2 GPI = 36 UE, Protein C = 85% (N > 75%) Protein S = 62% (N > 65%), AT III = 118% (N > 80%) Ø ELISA for listeria Ig. M = 1, 305 (N =0, 500) Ø PARACLINICAL : MRI
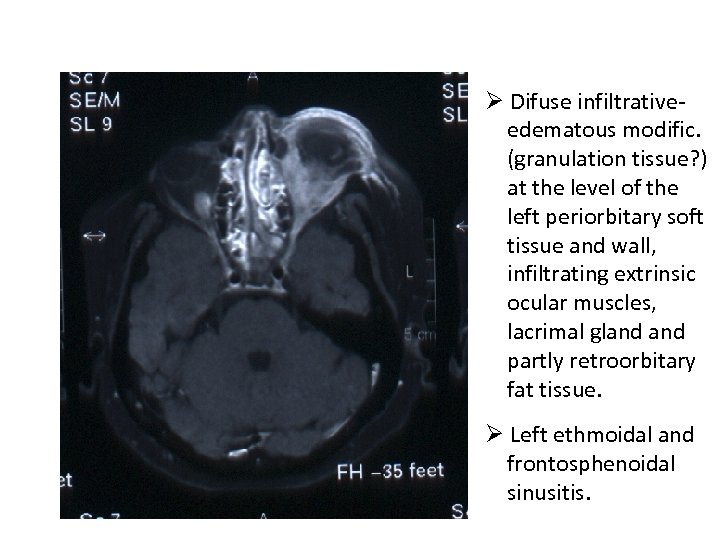
Ø Difuse infiltrative- edematous modific. (granulation tissue? ) at the level of the left periorbitary soft tissue and wall, infiltrating extrinsic ocular muscles, lacrimal gland partly retroorbitary fat tissue. Ø Left ethmoidal and frontosphenoidal sinusitis.
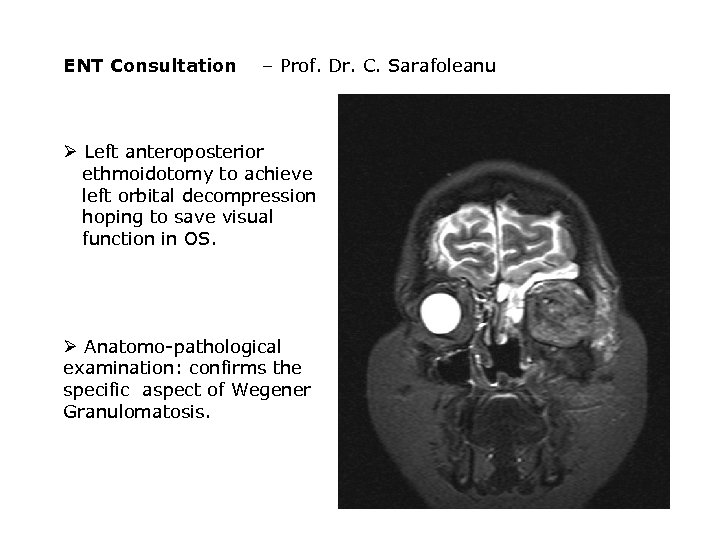
ENT Consultation – Prof. Dr. C. Sarafoleanu Ø Left anteroposterior ethmoidotomy to achieve left orbital decompression hoping to save visual function in OS. Ø Anatomo-pathological examination: confirms the specific aspect of Wegener Granulomatosis.

The 4 th day after The 8 th day after decompression surgery Stage diagnosis: Ø CLINICAL Left inflammatory orbital pseudotumor afecting all orbitary elements: - optic nerve, - oculomotory muscles, - cellulitis, - pannicullitis - vessels → hyperviscosy syndrome by rheological mechanism and affectation of vascular endothelium Ø PARACLINICAL Ø-biological - MRI - anatomopathological exam
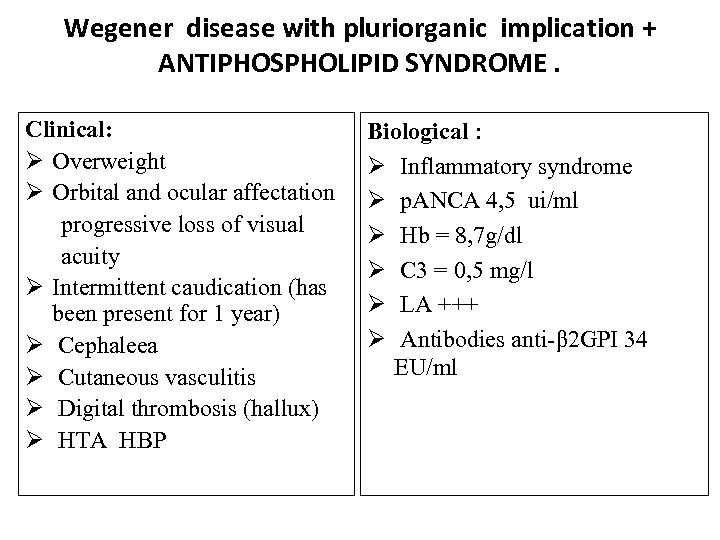
Wegener disease with pluriorganic implication + ANTIPHOSPHOLIPID SYNDROME. Clinical: Ø Overweight Ø Orbital and ocular affectation progressive loss of visual acuity Ø Intermittent caudication (has been present for 1 year) Ø Cephaleea Ø Cutaneous vasculitis Ø Digital thrombosis (hallux) Ø HTA HBP Biological : Ø Inflammatory syndrome Ø p. ANCA 4, 5 ui/ml Ø Hb = 8, 7 g/dl Ø C 3 = 0, 5 mg/l Ø LA +++ Ø Antibodies anti-β 2 GPI 34 EU/ml
• Solumedrol (1, 5 g/3 days) in recurrent pulses with evolution to remission of cutaneous vasculitis and orbitary inflammatory process. • Cyclophosphamide • Prednisone • Vessel Due F • Acenocumarol (Sintrom) • Statine • Coversion enzymes inhibitor • Calcium channel blockers Clinical progress under the treatment, but vision loss in OS. September 2006
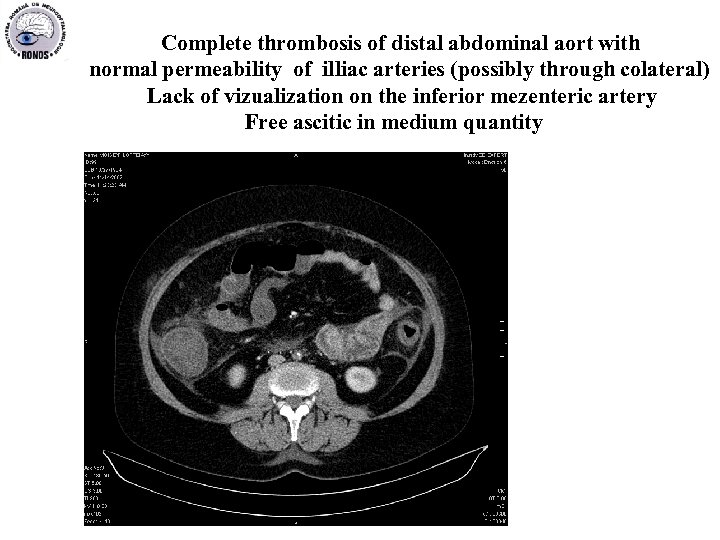
Complete thrombosis of distal abdominal aort with normal permeability of illiac arteries (possibly through colateral) Lack of vizualization on the inferior mezenteric artery Free ascitic in medium quantity
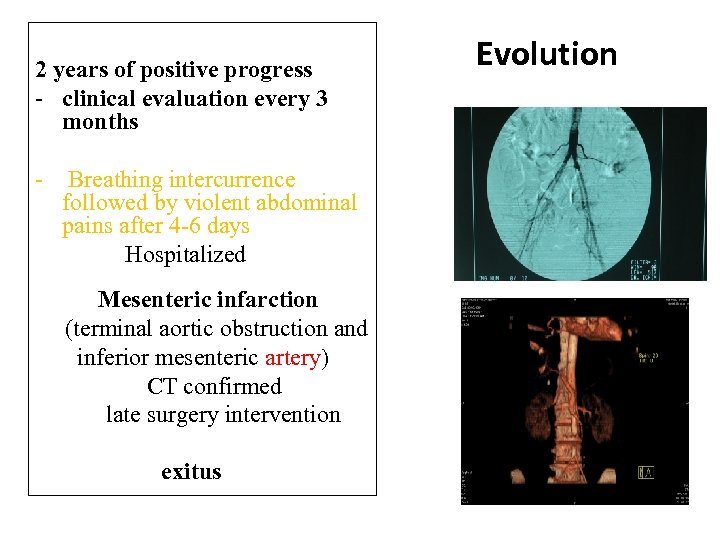
2 years of positive progress - clinical evaluation every 3 months - Breathing intercurrence followed by violent abdominal pains after 4 -6 days Hospitalized Mesenteric infarction (terminal aortic obstruction and inferior mesenteric artery) CT confirmed late surgery intervention exitus Evolution
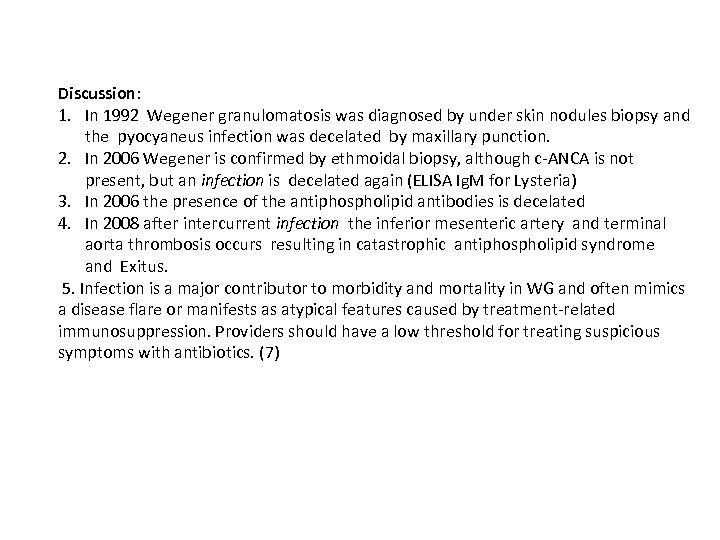
Discussion: 1. In 1992 Wegener granulomatosis was diagnosed by under skin nodules biopsy and the pyocyaneus infection was decelated by maxillary punction. 2. In 2006 Wegener is confirmed by ethmoidal biopsy, although c-ANCA is not present, but an infection is decelated again (ELISA Ig. M for Lysteria) 3. In 2006 the presence of the antiphospholipid antibodies is decelated 4. In 2008 after intercurrent infection the inferior mesenteric artery and terminal aorta thrombosis occurs resulting in catastrophic antiphospholipid syndrome and Exitus. 5. Infection is a major contributor to morbidity and mortality in WG and often mimics a disease flare or manifests as atypical features caused by treatment-related immunosuppression. Providers should have a low threshold for treating suspicious symptoms with antibiotics. (7)
Conclusion: The infection represents the mutual trigger both for the increase of c. ANCA and for the exacerbation of the thrombosis mechanism due to APLA, leading finally to a catastrophic antiphospholipid syndrome. The evolution pattern of the antiphospholipid antibodies leads to the catastrophic systemic inflammatory syndrome, due to the second infection impossible to controle two years after. Could the infection be the trigger of the catastrophic evolution of the Wegener granulomatosis? ! Is there any possibility that the human body should produce antiphospholipid antibodies to protect vessels endothelium against any agressive infection ? ! In conclusion Granulomatosis ……… pyocyaneus Orbital inflammatory pseudotumor …………. Lysteria ……. . APS Granulomatosis………. . SEPSIS………. . CAPS…………. DEATH
References: 1. Erkan D, Cervera R, Asherson RA. Catastrophic antiphospholipid syndrome: where do we stand? Arthritis Rheum 2003; 48: 3320 -7 2. Piette JC, Cervera R, Levy RA, Nasonov EL, Triplett DA, Shoenfeld Y. The catastrophic antiphospholipid syndrome-Asherson's syndrome. Ann Med Interne Paris 2003; 154: 195 -6. Medline] 3. Asherson RA, Shoenfeld Y. The role of infection in the pathogenesis of catastrophic antiphospholipid syndrome. Molecular mimicry? J Rheumatol 2000; 27: 12 -4. Medline] 4. Shoenfeld Y, Blank M, Cervera R, Font J, Raschi E, Meroni PL. Infectious origin of the antiphospholipid syndrome. Ann Rheum Dis 2006; 65: 2 -6. Medline] 5. Cervera R, Asherson RA, Acevedo ML, et al. Antiphospholipid syndrome associated with infections: clinical and microbiological characteristics of 100 patients. Ann Rheum Dis 2004; 63: 1312 -7. Medline] 6. Asherson RA, Espinosa G, Cervera R, et al. Disseminated intravascular coagulation in catastrophic antiphospholipid syndrome: clinical and haematological characteristics of 23 patients. Ann Rheum Dis 2005; 64: 943 -6. Medline] 7. Seo P. Wegener's granulomatosis: managing more than inflammation. Curr Opin Rheum. January 2008; 20: 10 -16. [Medline]
e36384036d80f7d9628ee98aee4595c4.ppt