08adc53229afab3805756dfe87f91e13.ppt
- Количество слайдов: 59
Orange County Public Health and Bioterrorism Hildy Meyers, M. D. , M. P. H. Medical Director Epidemiology & Assessment Public Health Services Orange County Health Care Agency December 10, 2001
Bioterrorism (BT) - Definition Biological terrorism is the use of microorganisms (bacteria, viruses, and fungi) or toxins from living organisms to produce death or disease in humans, animals, and plants.
Ideal BT Agent n n Can be delivered as an aerosol High disease/infection ratio Maintains viability/infectivity in environment Vaccine or prophylaxis to protect in manufacture and delivery
Environmental Constraints n n Sunlight - UV light kills many bacteria Wind - spreads biological agents Temperature - heat inactivates many biological agents; most are resistant to freezing Desiccation - may inactivate or inhibit growth
Agents of BT—Top Suspects Anthrax (Bacillus anthracis) n Smallpox (Variola major) n Plague (Yersinia pestis) n Tularemia (Francisella tularensis) n Botulism (Botulinum toxin) n Viral hemorrhagic fevers (Filoviruses and Arenaviruses ) n
Health Care Agency Planning Improve communications u Requesting fax number and/or e-mail address from all O. C. physicians u Web postings u Grand rounds u Public Health Bulletin n Improve surveillance n Improve staff training n
Bioterrorism Response Most important for physicians: n n Preparation u Familiarity with agents of BT u Personal/office disaster preparedness u Hospital preparedness Recognition—“the astute physician” Reporting to Orange County Public Health— this will activate the response system Also notify hospital infection control, laboratory, and administration
How to report During regular business hours u Call Epidemiology t (714) 834 -8180 n After hours, weekends and holidays For physicians and health care facilities ONLY u County Communications t (714) 628 -7008 t Ask for Public Health Official on call n
Orange County Health Care Agency Response Case investigation and case finding n Establish diagnosis n Activate Orange County emergency plans n Notify: u California Dept of Health Services u Centers for Disease Control & Prevention u FBI and local law enforcement n
Orange County Health Care Agency Response, cont. n Recommend treatment and infection control measures n Establish exposure date(s) and location(s) n Identify exposed persons n Follow-up cases and contacts n Provide mass prophylaxis (if indicated)
Identifying Suspicious Letters or Packages n n n n Excessive postage Handwritten or poorly typed addresses Incorrect titles; title, but no name Misspellings of common words Oily stains, discolorations or odor No return address or postmark does not match return address Excessive weight Lopsided or uneven envelope
Response to Suspicious Powder or Package n n n Call law enforcement Law enforcement performs threat assessment and contacts FBI as needed u If no credible threat exists, incident is closed without further testing If credible threat exists u FBI arranges for laboratory testing of specimen (and environment, if indicated) u Public Health is notified
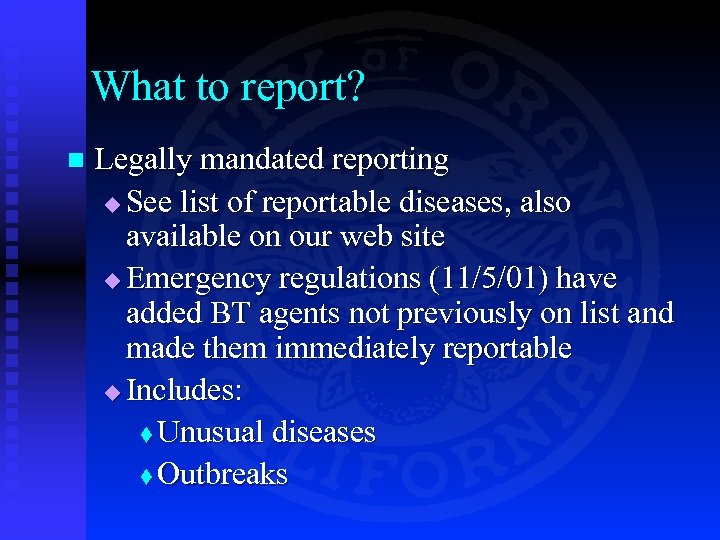
What to report? n Legally mandated reporting u See list of reportable diseases, also available on our web site u Emergency regulations (11/5/01) have added BT agents not previously on list and made them immediately reportable u Includes: t Unusual diseases t Outbreaks
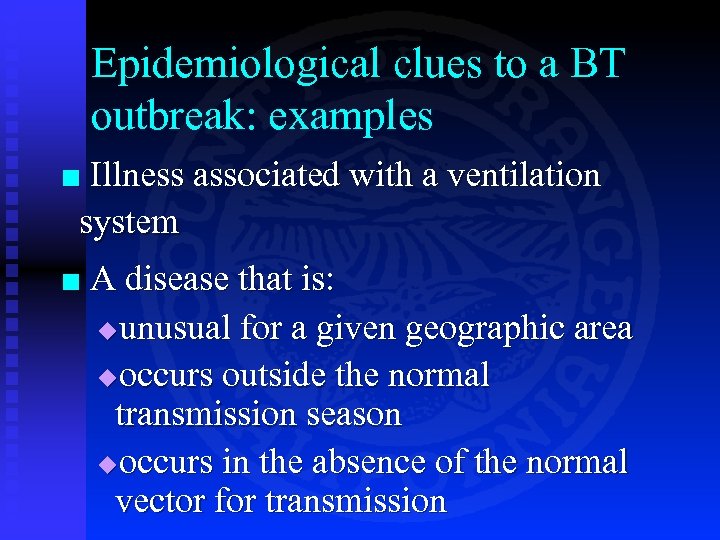
Epidemiological clues to a BT outbreak: examples Illness associated with a ventilation system ¢ ¢ A disease that is: uunusual for a given geographic area uoccurs outside the normal transmission season uoccurs in the absence of the normal vector for transmission
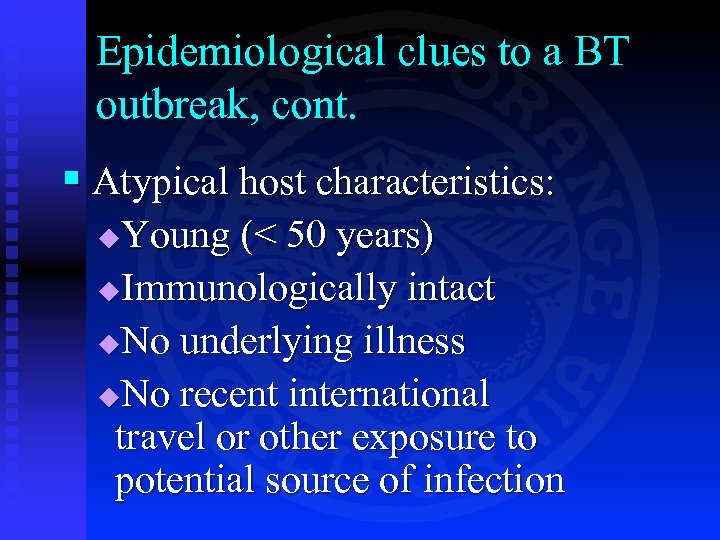
Epidemiological clues to a BT outbreak, cont. § Atypical host characteristics: Young (< 50 years) u. Immunologically intact u. No underlying illness u. No recent international travel or other exposure to potential source of infection u
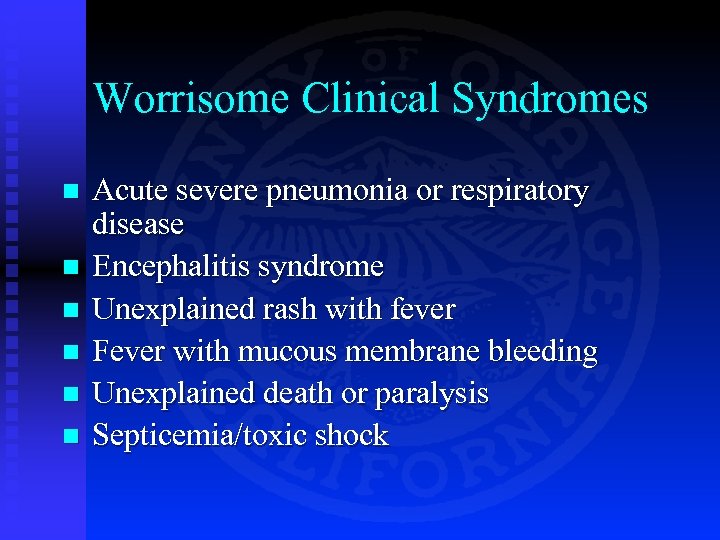
Worrisome Clinical Syndromes n n n Acute severe pneumonia or respiratory disease Encephalitis syndrome Unexplained rash with fever Fever with mucous membrane bleeding Unexplained death or paralysis Septicemia/toxic shock
Anthrax
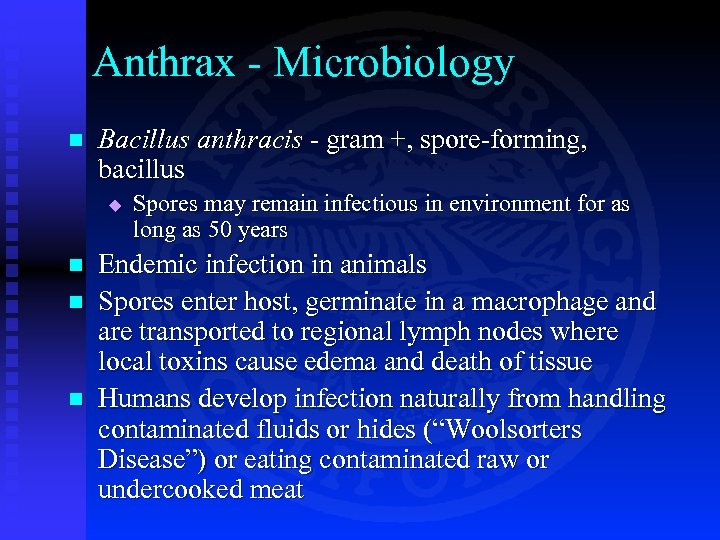
Anthrax - Microbiology n Bacillus anthracis - gram +, spore-forming, bacillus u n n n Spores may remain infectious in environment for as long as 50 years Endemic infection in animals Spores enter host, germinate in a macrophage and are transported to regional lymph nodes where local toxins cause edema and death of tissue Humans develop infection naturally from handling contaminated fluids or hides (“Woolsorters Disease”) or eating contaminated raw or undercooked meat
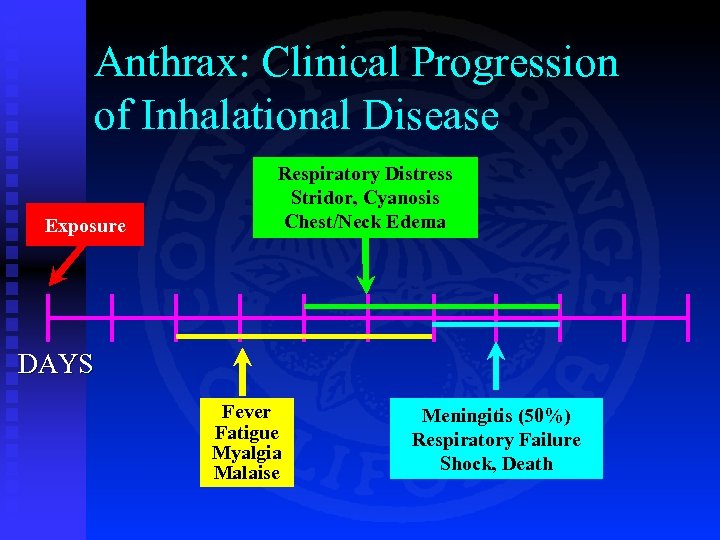
Anthrax: Clinical Progression of Inhalational Disease Exposure Respiratory Distress Stridor, Cyanosis Chest/Neck Edema DAYS Fever Fatigue Myalgia Malaise Meningitis (50%) Respiratory Failure Shock, Death
Anthrax: Inhalational, N=10 Incubation (known for 6 cases) u Range: 4 -6 days u Median: 4 days n Age u Range: 43 -73 u Median: 56 years n 7 of 10: male n
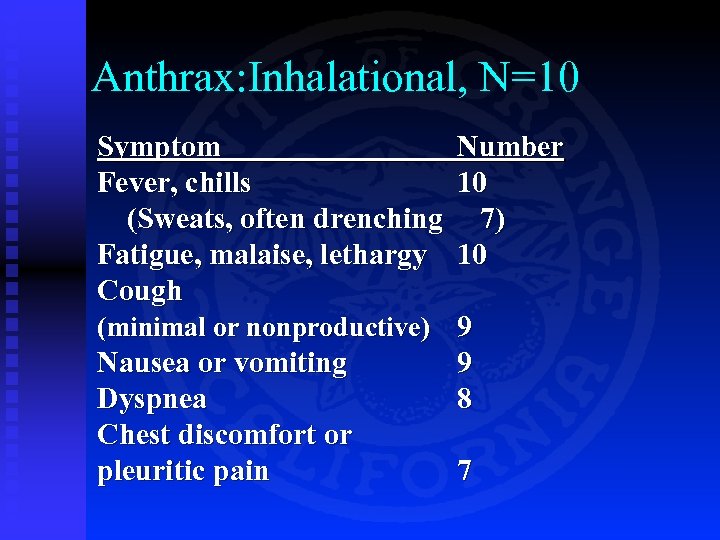
Anthrax: Inhalational, N=10 Symptom Number Fever, chills 10 (Sweats, often drenching 7) Fatigue, malaise, lethargy 10 Cough (minimal or nonproductive) 9 Nausea or vomiting 9 Dyspnea 8 Chest discomfort or pleuritic pain 7
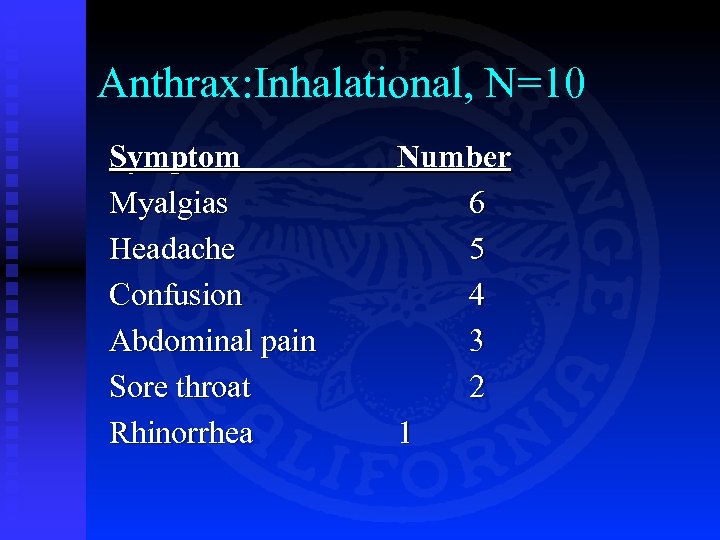
Anthrax: Inhalational, N=10 Symptom Myalgias Headache Confusion Abdominal pain Sore throat Rhinorrhea Number 6 5 4 3 2 1
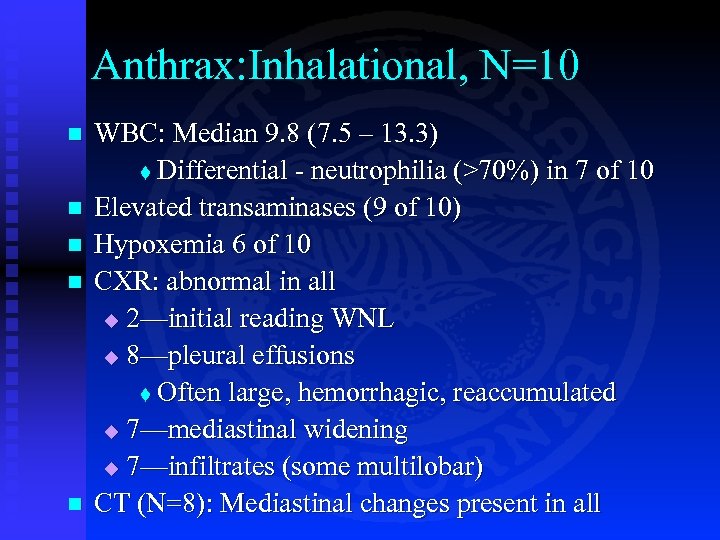
Anthrax: Inhalational, N=10 n n n WBC: Median 9. 8 (7. 5 – 13. 3) t Differential - neutrophilia (>70%) in 7 of 10 Elevated transaminases (9 of 10) Hypoxemia 6 of 10 CXR: abnormal in all u 2—initial reading WNL u 8—pleural effusions t Often large, hemorrhagic, reaccumulated u 7—mediastinal widening u 7—infiltrates (some multilobar) CT (N=8): Mediastinal changes present in all
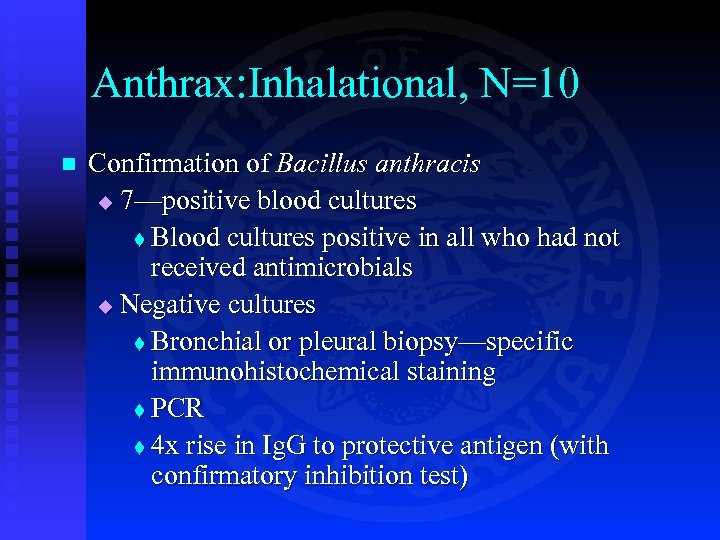
Anthrax: Inhalational, N=10 n Confirmation of Bacillus anthracis u 7—positive blood cultures t Blood cultures positive in all who had not received antimicrobials u Negative cultures t Bronchial or pleural biopsy—specific immunohistochemical staining t PCR t 4 x rise in Ig. G to protective antigen (with confirmatory inhibition test)
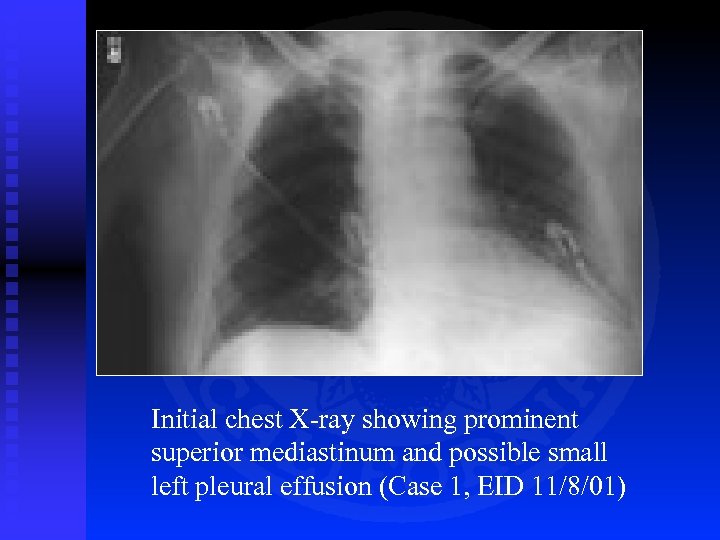
Initial chest X-ray showing prominent superior mediastinum and possible small left pleural effusion (Case 1, EID 11/8/01)
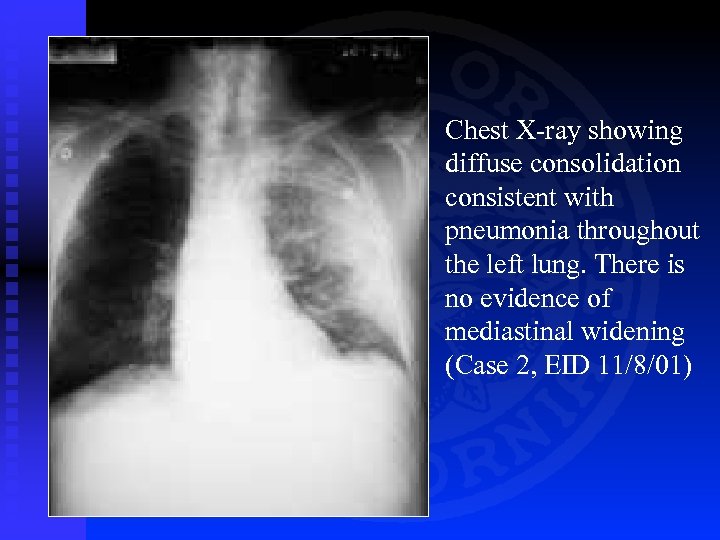
Chest X-ray showing diffuse consolidation consistent with pneumonia throughout the left lung. There is no evidence of mediastinal widening (Case 2, EID 11/8/01)
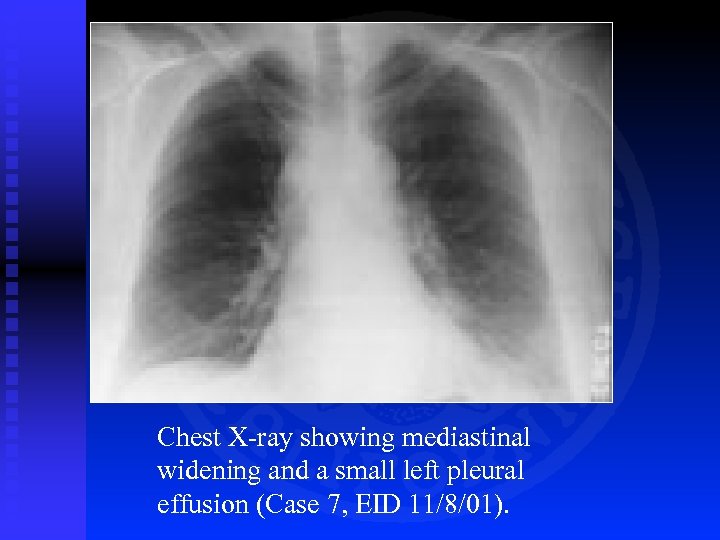
Chest X-ray showing mediastinal widening and a small left pleural effusion (Case 7, EID 11/8/01).
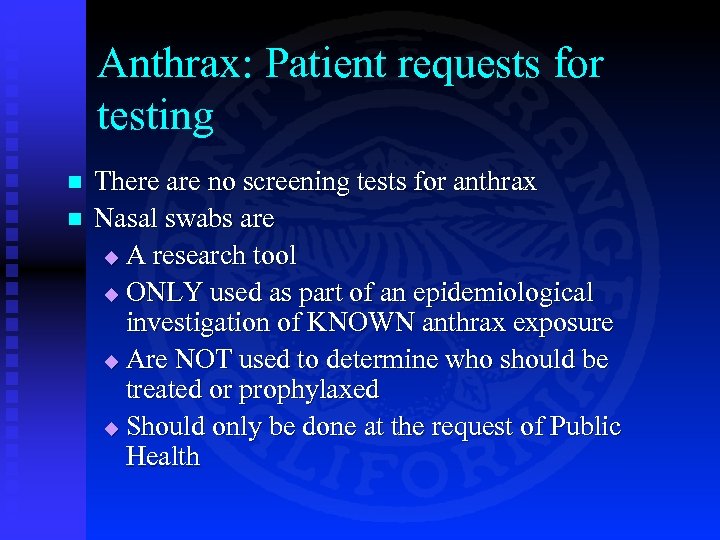
Anthrax: Patient requests for testing n n There are no screening tests for anthrax Nasal swabs are u A research tool u ONLY used as part of an epidemiological investigation of KNOWN anthrax exposure u Are NOT used to determine who should be treated or prophylaxed u Should only be done at the request of Public Health
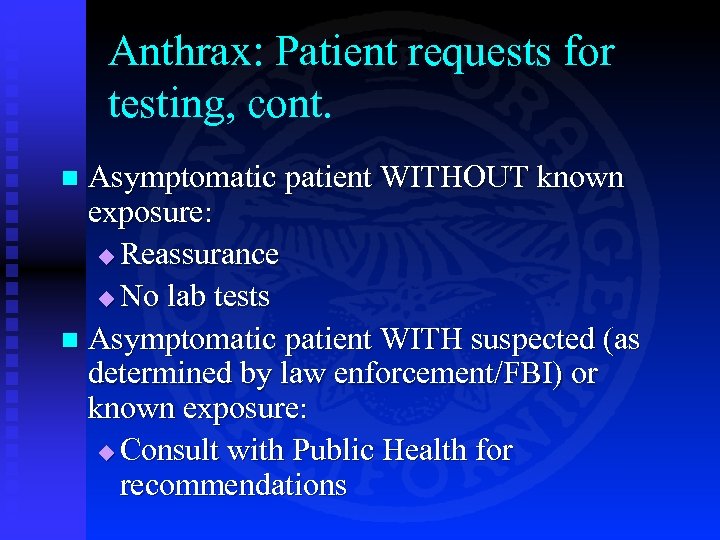
Anthrax: Patient requests for testing, cont. Asymptomatic patient WITHOUT known exposure: u Reassurance u No lab tests n Asymptomatic patient WITH suspected (as determined by law enforcement/FBI) or known exposure: u Consult with Public Health for recommendations n
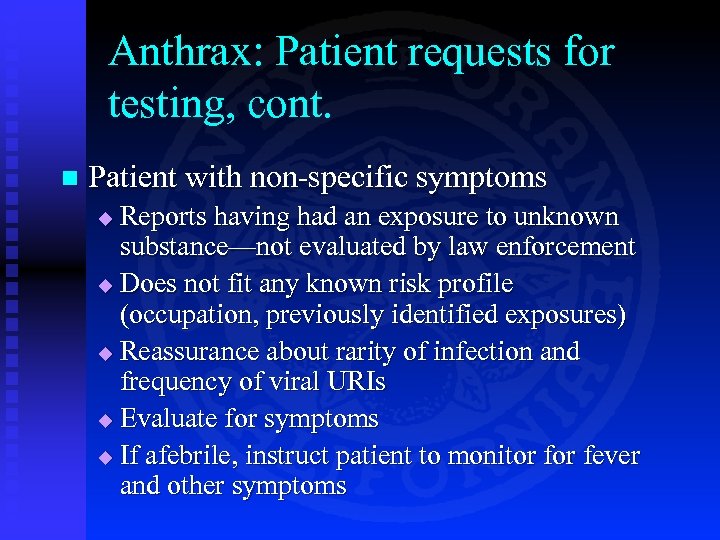
Anthrax: Patient requests for testing, cont. n Patient with non-specific symptoms Reports having had an exposure to unknown substance—not evaluated by law enforcement u Does not fit any known risk profile (occupation, previously identified exposures) u Reassurance about rarity of infection and frequency of viral URIs u Evaluate for symptoms u If afebrile, instruct patient to monitor fever and other symptoms u
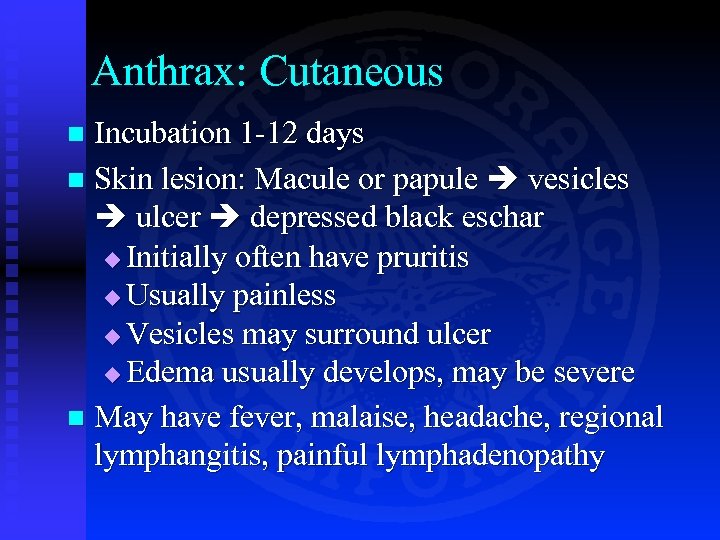
Anthrax: Cutaneous Incubation 1 -12 days n Skin lesion: Macule or papule vesicles ulcer depressed black eschar u Initially often have pruritis u Usually painless u Vesicles may surround ulcer u Edema usually develops, may be severe n May have fever, malaise, headache, regional lymphangitis, painful lymphadenopathy n
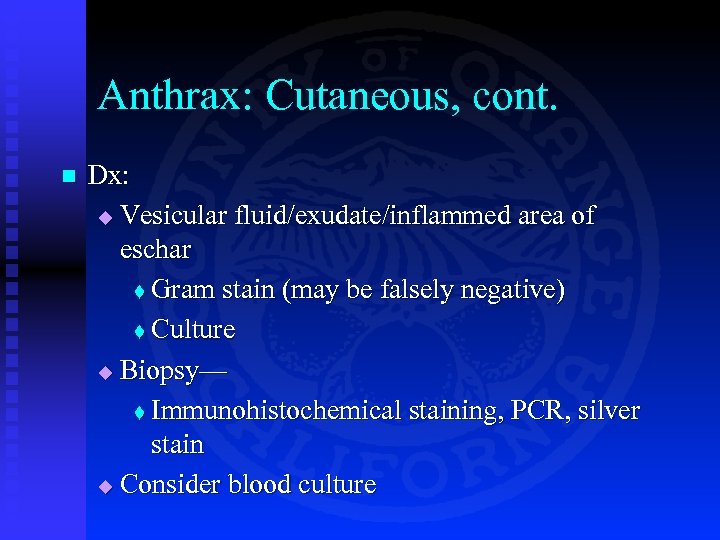
Anthrax: Cutaneous, cont. n Dx: u Vesicular fluid/exudate/inflammed area of eschar t Gram stain (may be falsely negative) t Culture u Biopsy— t Immunohistochemical staining, PCR, silver stain u Consider blood culture

Cutaneous lesion on face Cutaneous lesion: day 11 Cutaneous lesion on neck
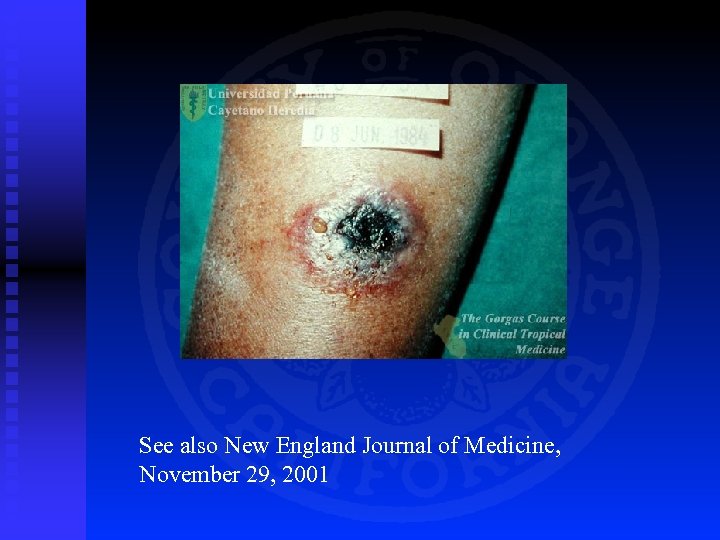
See also New England Journal of Medicine, November 29, 2001
Cutaneous Anthrax: D/dx n n n n Ecthyma Folliculitis Brown recluse spider bite Ecthyma gangrenosum Orf Pyoderma gangrenosum Sweet’s syndrome (http: //www. acponline. org American College of Physicians)
Cutaneous Anthrax: Clues to the diagnosis n n n n Usually solitary lesion Initial pruritis Painless Most often on upper extremities Evolution to eschar formation Non-pitting edema Regional adenopathy May be associated with constitutional sx
Anthrax Treatment n Inhalational u Doxycyline or ciprofloxacin, IV u Plus: 1 or 2 other drugs t Rifampin, clindamycin, chloramphenicol, vancomycin, clindamycin u Not cephalosporins or trimethopirmsulfamethoxazole
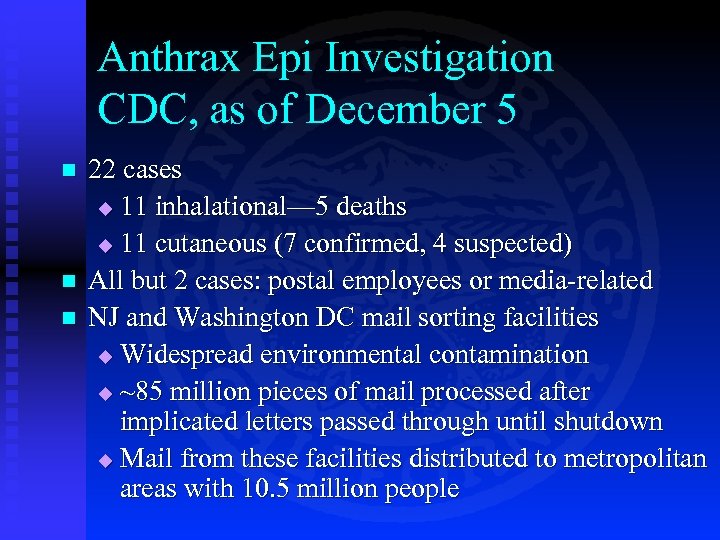
Anthrax Epi Investigation CDC, as of December 5 n n n 22 cases u 11 inhalational— 5 deaths u 11 cutaneous (7 confirmed, 4 suspected) All but 2 cases: postal employees or media-related NJ and Washington DC mail sorting facilities u Widespread environmental contamination u ~85 million pieces of mail processed after implicated letters passed through until shutdown u Mail from these facilities distributed to metropolitan areas with 10. 5 million people
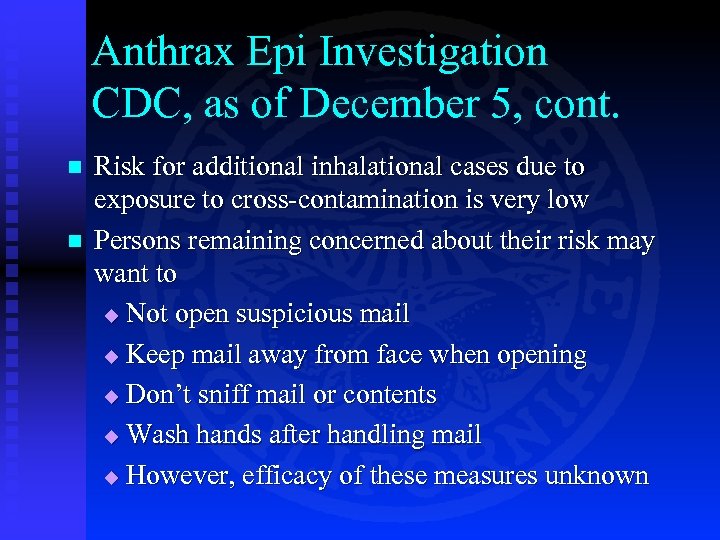
Anthrax Epi Investigation CDC, as of December 5, cont. n n Risk for additional inhalational cases due to exposure to cross-contamination is very low Persons remaining concerned about their risk may want to u Not open suspicious mail u Keep mail away from face when opening u Don’t sniff mail or contents u Wash hands after handling mail u However, efficacy of these measures unknown
Smallpox
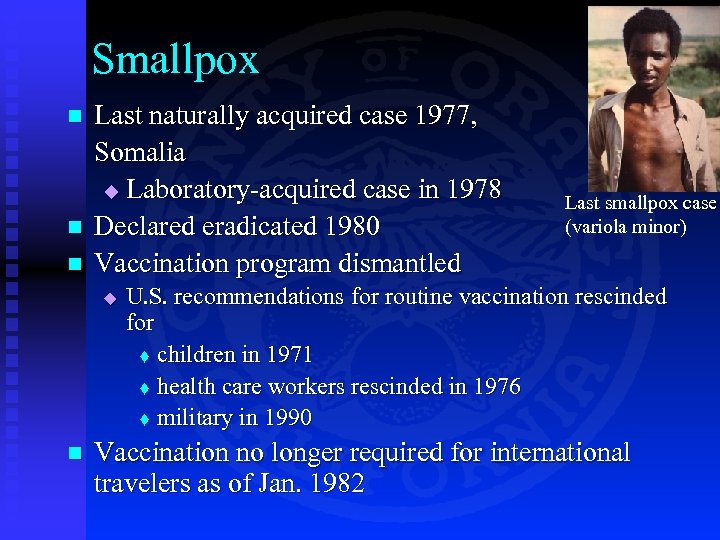
Smallpox n n n Last naturally acquired case 1977, Somalia u Laboratory-acquired case in 1978 Declared eradicated 1980 Vaccination program dismantled u n Last smallpox case (variola minor) U. S. recommendations for routine vaccination rescinded for t children in 1971 t health care workers rescinded in 1976 t military in 1990 Vaccination no longer required for international travelers as of Jan. 1982
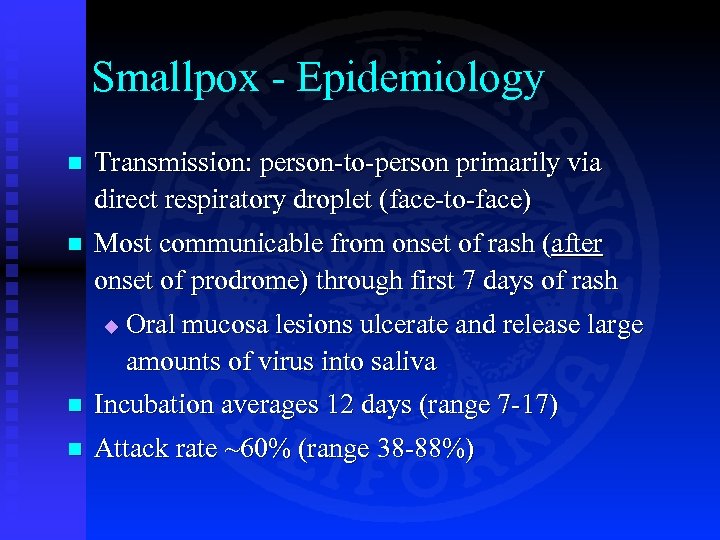
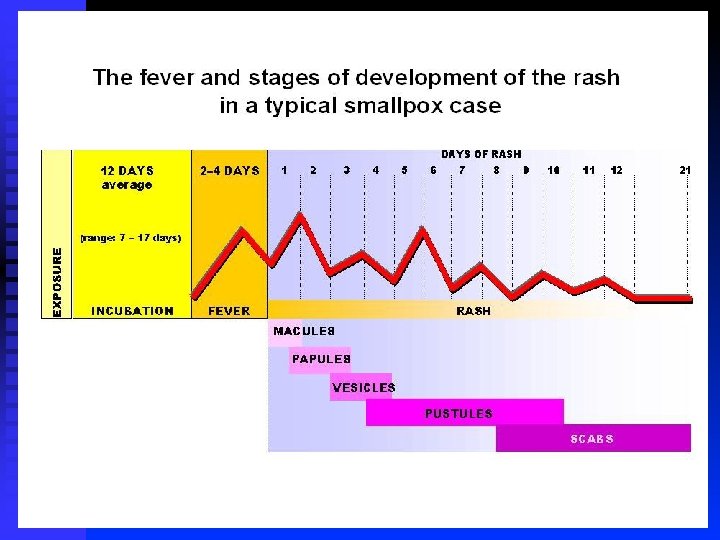
Smallpox - Epidemiology n Transmission: person-to-person primarily via direct respiratory droplet (face-to-face) n Most communicable from onset of rash (after onset of prodrome) through first 7 days of rash u Oral mucosa lesions ulcerate and release large amounts of virus into saliva n Incubation averages 12 days (range 7 -17) n Attack rate ~60% (range 38 -88%)
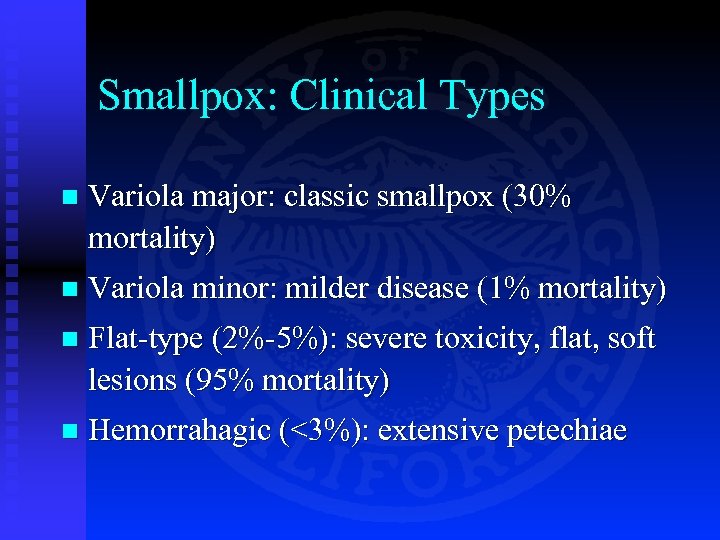
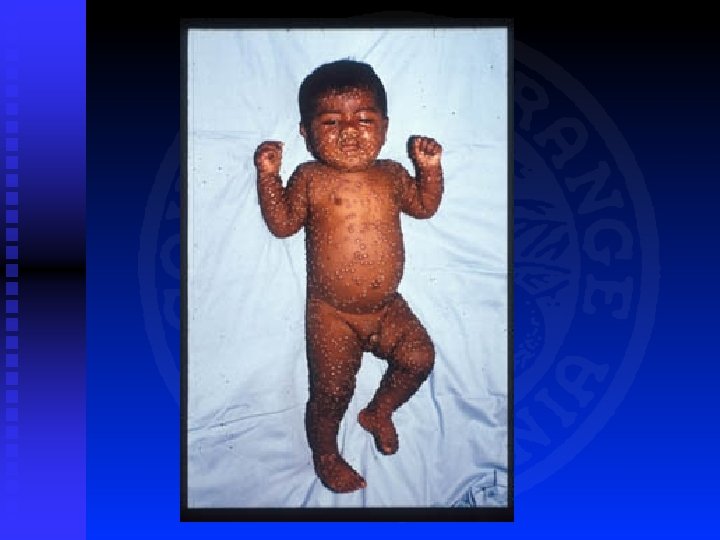
Smallpox: Clinical Types n Variola major: classic smallpox (30% mortality) n Variola minor: milder disease (1% mortality) n Flat-type (2%-5%): severe toxicity, flat, soft lesions (95% mortality) n Hemorrahagic (<3%): extensive petechiae
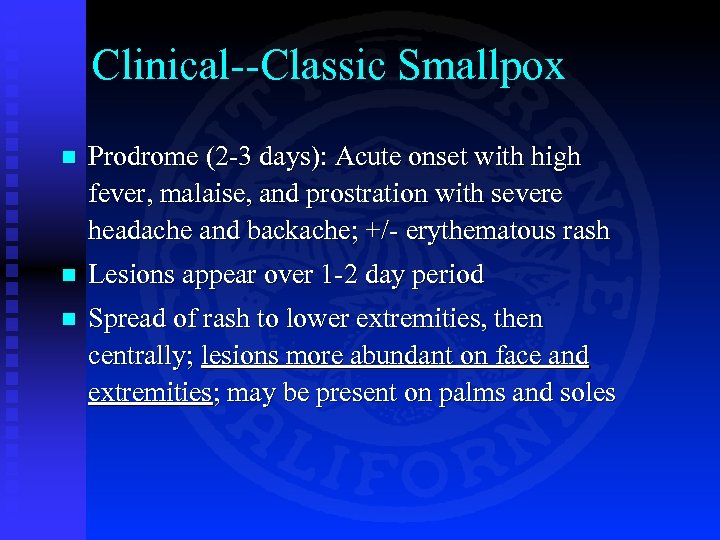
Clinical--Classic Smallpox n Prodrome (2 -3 days): Acute onset with high fever, malaise, and prostration with severe headache and backache; +/- erythematous rash n Lesions appear over 1 -2 day period n Spread of rash to lower extremities, then centrally; lesions more abundant on face and extremities; may be present on palms and soles


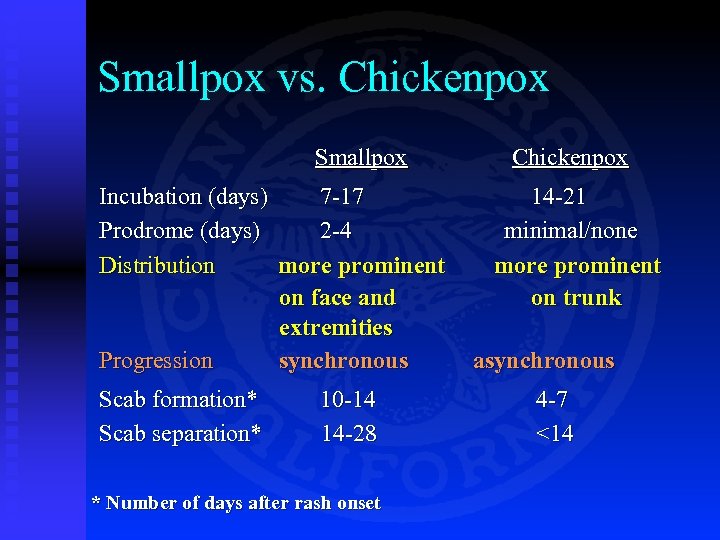
Smallpox vs. Chickenpox Smallpox Incubation (days) 7 -17 Prodrome (days) 2 -4 Distribution more prominent on face and extremities Progression synchronous Scab formation* Scab separation* 10 -14 14 -28 * Number of days after rash onset Chickenpox 14 -21 minimal/none more prominent on trunk asynchronous 4 -7 <14
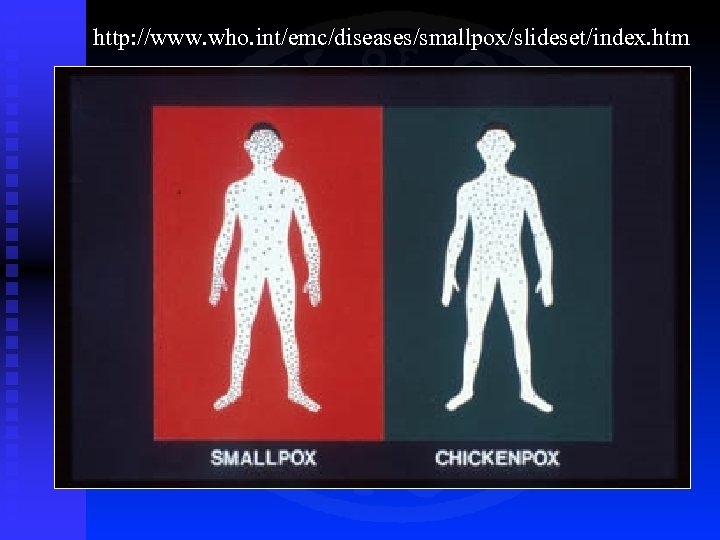
http: //www. who. int/emc/diseases/smallpox/slideset/index. htm

Day 2 of rash Day 5 of rash

Day 4 of rash Day 5 of rash Day 6 of rash

Day 7 Days 8 -9

Days 10 -14 Day 20
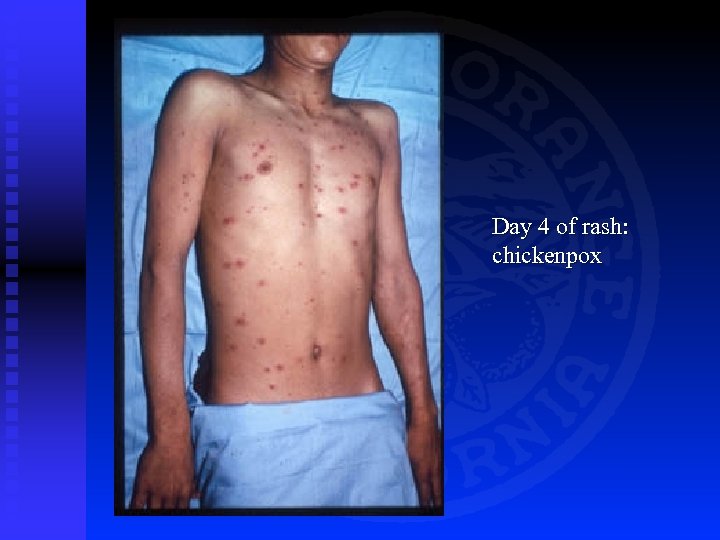
Day 4 of rash: chickenpox
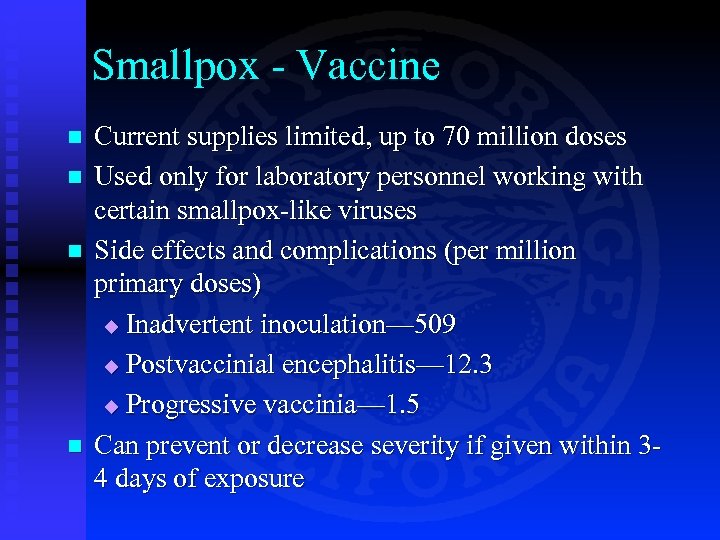
Smallpox - Vaccine n n Current supplies limited, up to 70 million doses Used only for laboratory personnel working with certain smallpox-like viruses Side effects and complications (per million primary doses) u Inadvertent inoculation— 509 u Postvaccinial encephalitis— 12. 3 u Progressive vaccinia— 1. 5 Can prevent or decrease severity if given within 34 days of exposure
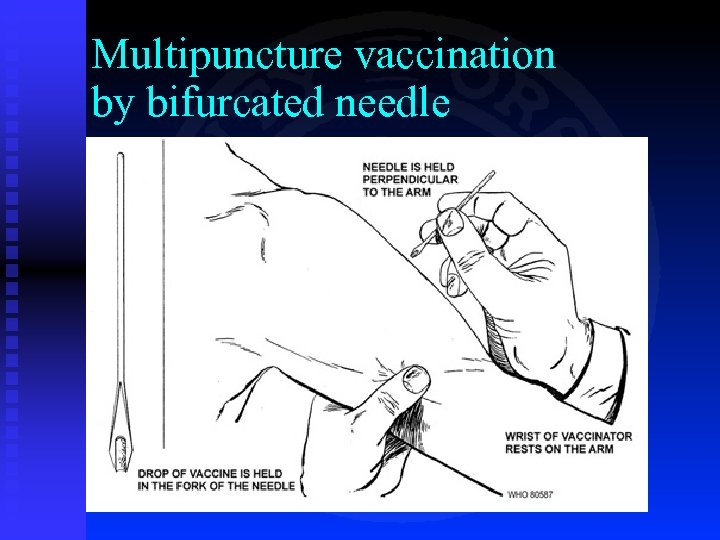
Multipuncture vaccination by bifurcated needle
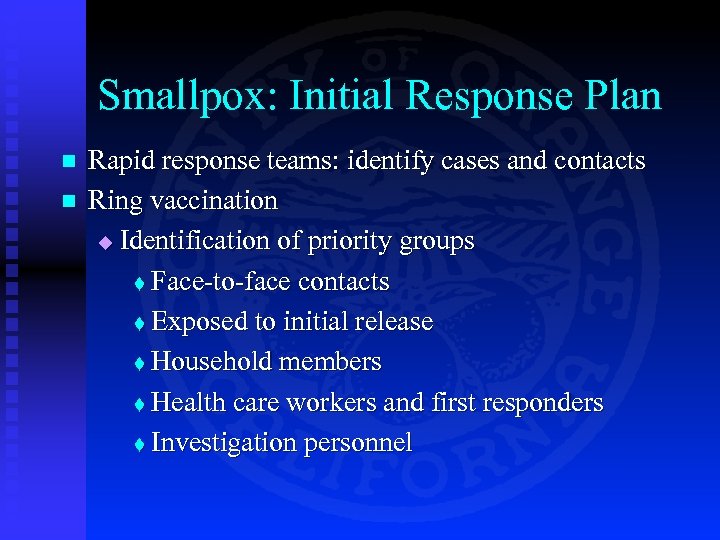
Smallpox: Initial Response Plan n n Rapid response teams: identify cases and contacts Ring vaccination u Identification of priority groups t Face-to-face contacts t Exposed to initial release t Household members t Health care workers and first responders t Investigation personnel
Web Resources n n n CDC Bioterrorism site: http: //www. bt. cdc. gov List of reportable diseases: http: //www. oc. ca. gov/hca/docs/forms/diseases. pdf Confidential morbidity reporting form http: //www. oc. ca. gov/hca/docs/forms/morbidrep. pdf World Health Organization http: //www. who. int/emc/deliberate_epi. html JAMA articles on bioterrorism (scroll down): http: //jama. ama-assn. org/
08adc53229afab3805756dfe87f91e13.ppt