Oral Ulcerations.ppt
- Количество слайдов: 26
Oral Ulcerations Azmi Darwazeh BDS. , MSc. , Ph. D. , FFD RCSI. Professor of Oral Medicine & Pathology Faculty of Dentistry Jordan University of Science & Technology
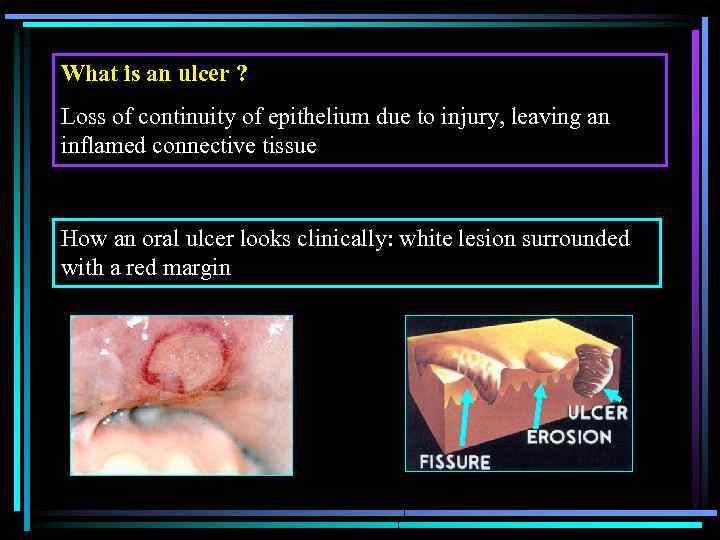
What is an ulcer ? Loss of continuity of epithelium due to injury, leaving an inflamed connective tissue How an oral ulcer looks clinically: white lesion surrounded with a red margin
Traumatic ulceration Mechanichal Chemical Thermal Radiotherapy
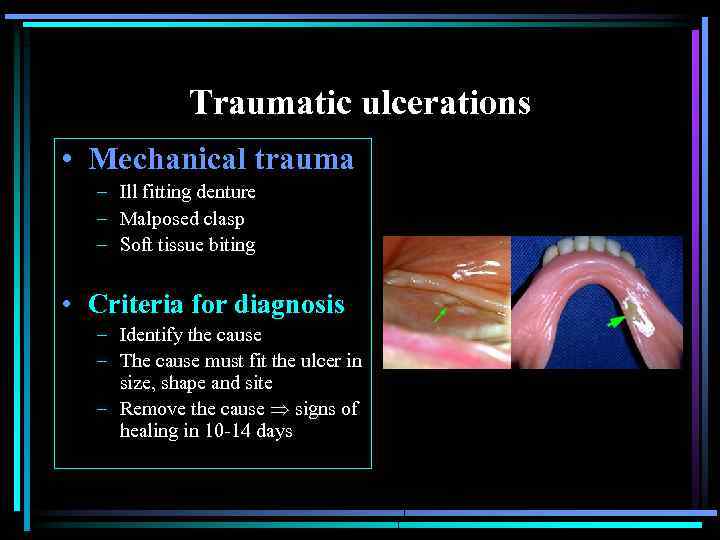
Traumatic ulcerations • Mechanical trauma – Ill fitting denture – Malposed clasp – Soft tissue biting • Criteria for diagnosis – Identify the cause – The cause must fit the ulcer in size, shape and site – Remove the cause signs of healing in 10 -14 days

A traumatic ulcer caused by a cotton roll
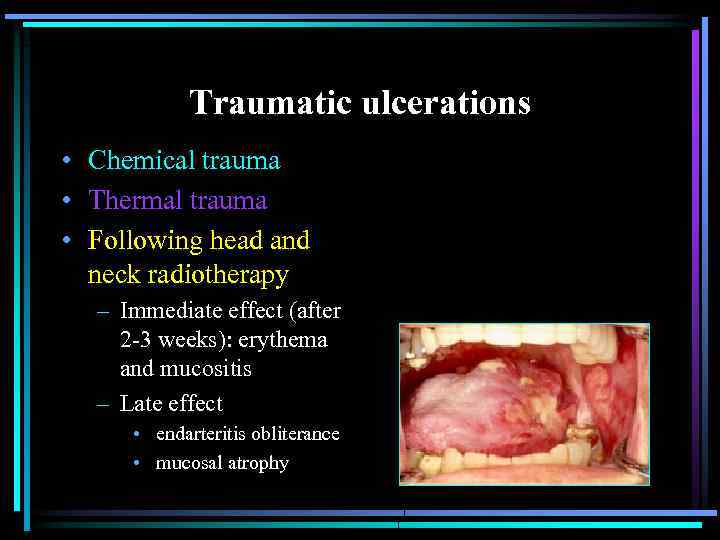
Traumatic ulcerations • Chemical trauma • Thermal trauma • Following head and neck radiotherapy – Immediate effect (after 2 -3 weeks): erythema and mucositis – Late effect • endarteritis obliterance • mucosal atrophy
Traumatic Ulcer - Management • Identify the cause and remove it • Prevent secondary infection • Review after 10 -14 days If the ulcer is not showing signs of healing then biopsy is a must to exclude malignancy
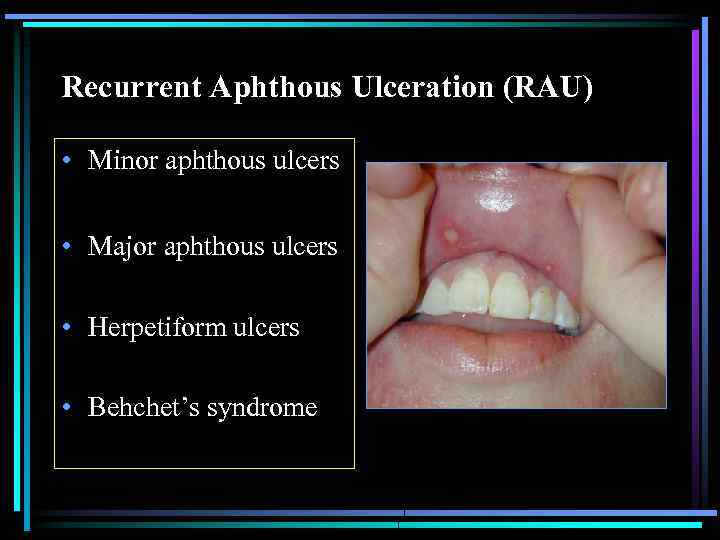
Recurrent Aphthous Ulceration (RAU) • Minor aphthous ulcers • Major aphthous ulcers • Herpetiform ulcers • Behchet’s syndrome
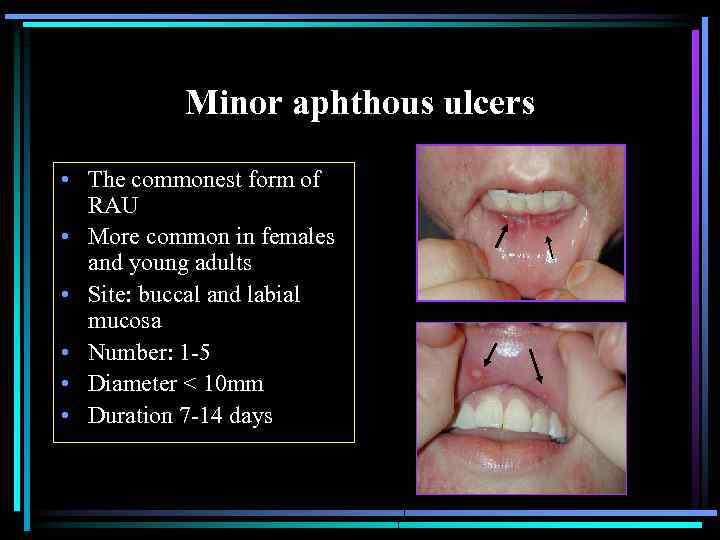
Minor aphthous ulcers • The commonest form of RAU • More common in females and young adults • Site: buccal and labial mucosa • Number: 1 -5 • Diameter < 10 mm • Duration 7 -14 days


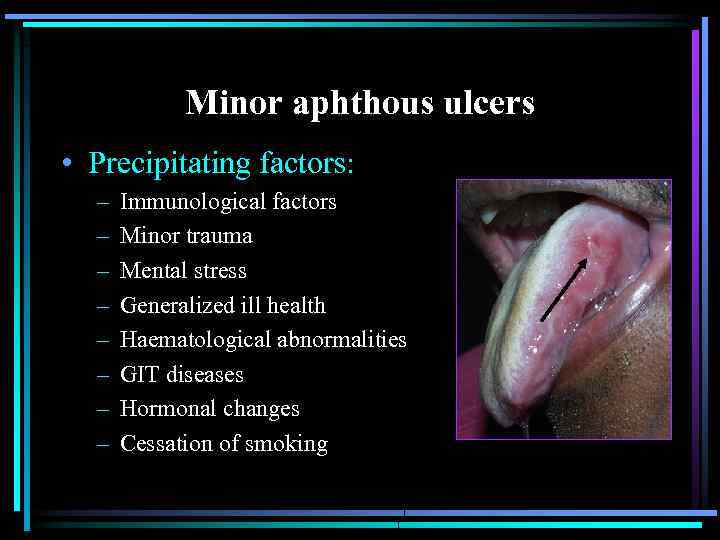
Minor aphthous ulcers • Precipitating factors: – – – – Immunological factors Minor trauma Mental stress Generalized ill health Haematological abnormalities GIT diseases Hormonal changes Cessation of smoking
Minor aphthous ulcers • Diagnosis: clinical picture + history • Causes: not determined yet !!! – Infection: herpes virus, S. sanguis, hypersensitivity reaction to microbes – Abnormalities of the immune system: allergy and autoimmunity.
Minor aphthous ulcers • Treatment: • Identify and correct predisposing factor(s) • Strict oral hygiene • Medications: – – – – Covering agents Antiseptic mouth washes Topical antibiotics Topical steroids Hormones Topical anesthetics Other drugs: Na cromoglycate, Prostogflandin, Carbenoxolone

Major aphthous ulcers • Site: as MAU + palate and pharynx • Diameter: >10 mm • Duration >30 days • Number: 1 -10 • More painful • Heals by scaring
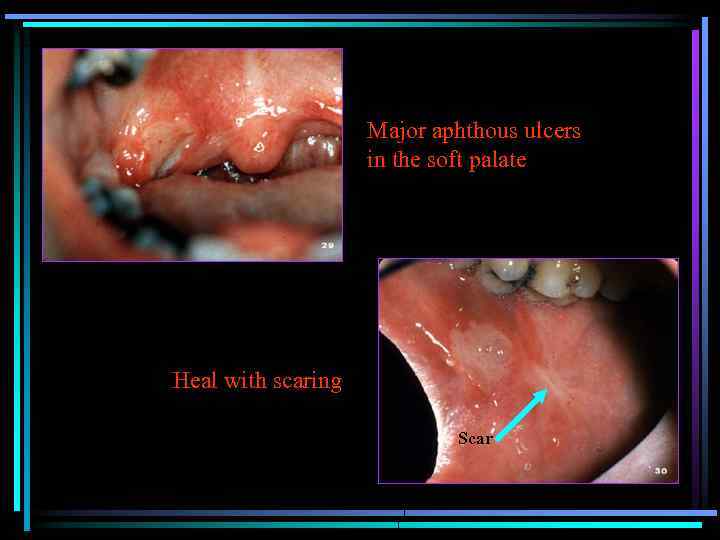
Major aphthous ulcers in the soft palate Heal with scaring Scar
Major aphthous ulcers • Treatment: as MAU + – Systemic steroids: Rx: Prednisolone 40 mg. For 3 days 30 mg. 20 mg. 10 mg. – Intra- or sub-lesional injection of steroids Triamcinolone acetonide susp. – High concentration steroid mouth wash – Steroid sparing drugs: e. g. azathioprine
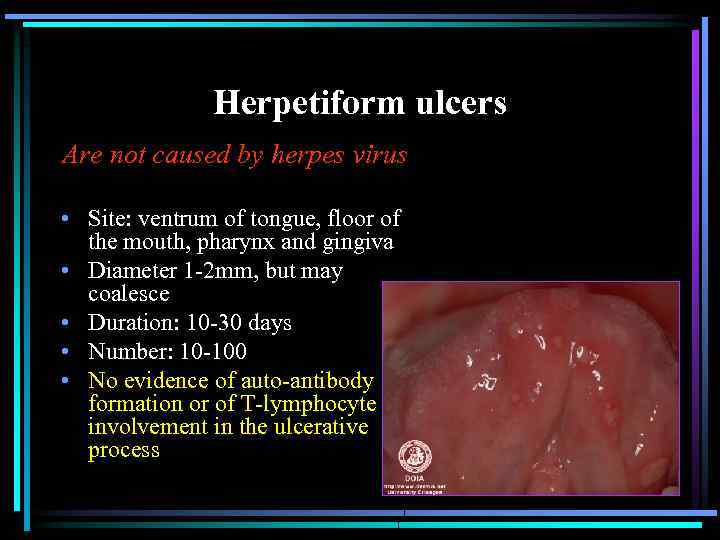
Herpetiform ulcers Are not caused by herpes virus • Site: ventrum of tongue, floor of the mouth, pharynx and gingiva • Diameter 1 -2 mm, but may coalesce • Duration: 10 -30 days • Number: 10 -100 • No evidence of auto-antibody formation or of T-lymphocyte involvement in the ulcerative process
Herpetiform ulcers • Treatment: As MUA – Steroids are ineffective – 2% chlor-tetracycline mouth wash – ? Gluten-free diet.
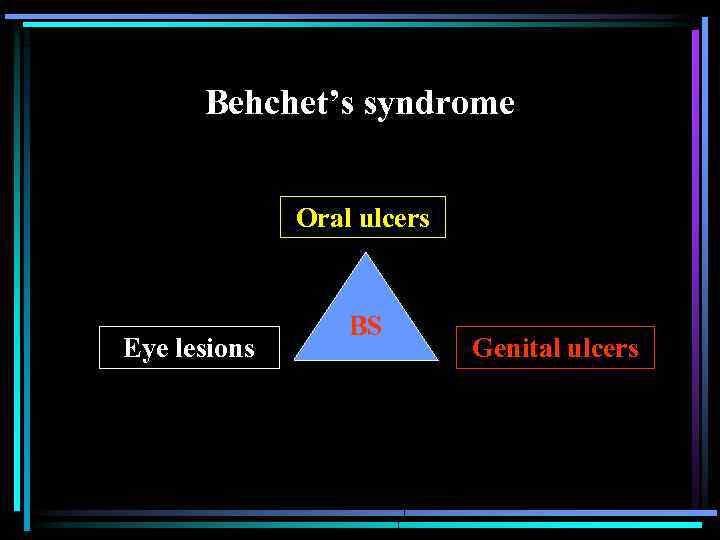
Behchet’s syndrome Oral ulcers Eye lesions BS Genital ulcers
Behchet’s syndrome • Immunological crossreactivity between mucosal epithelia of the : – – – Mouth Pharynx Oesophagus Vagina Conjunctiva Skin
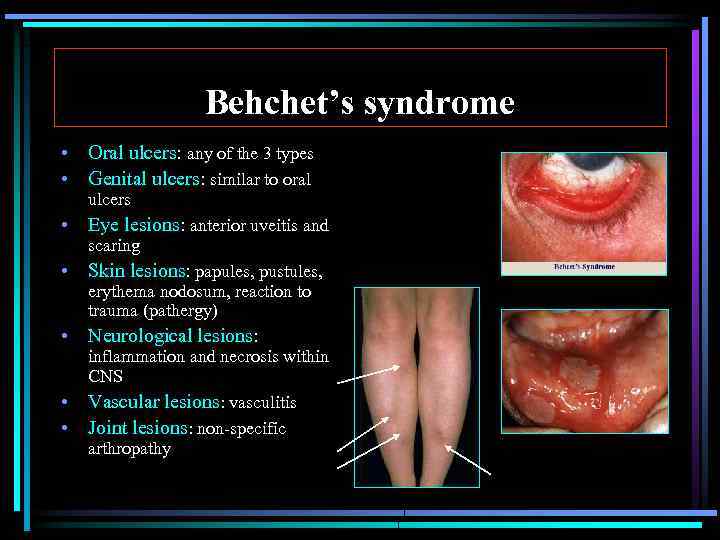
Behchet’s syndrome • Oral ulcers: any of the 3 types • Genital ulcers: similar to oral ulcers • Eye lesions: anterior uveitis and scaring • Skin lesions: papules, pustules, erythema nodosum, reaction to trauma (pathergy) • Neurological lesions: • • inflammation and necrosis within CNS Vascular lesions: vasculitis Joint lesions: non-specific arthropathy
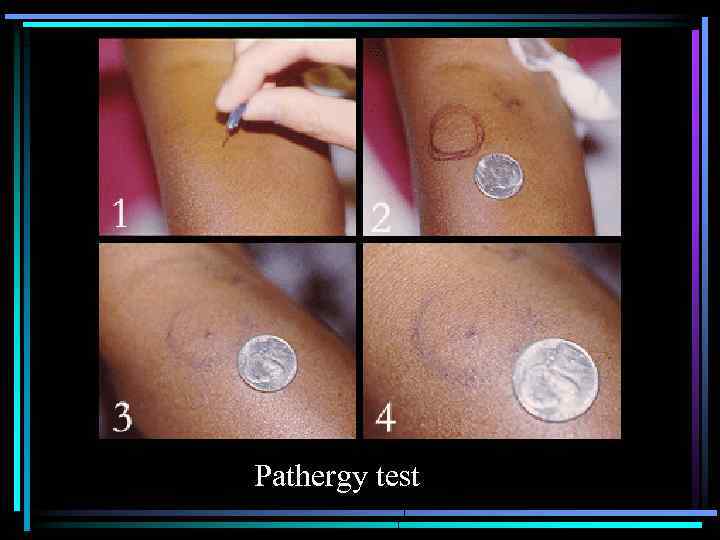
Pathergy test
Behchet’s syndrome - Diagnosis • Major criteria: – Oral ulcers – Genital ulcers – Eye lesions • Minor criteria: – – CNS Vascular lesions Joint lesions others
Behchet’s Syndrome - Management • Oral lesions: As other forms of RAU • Generalized manifestations: – – – – Systemic steroids Azathioprine Cyclosporine Thalidomide (teratogenic effect) Penicillamine Colchicine Chlorambucil
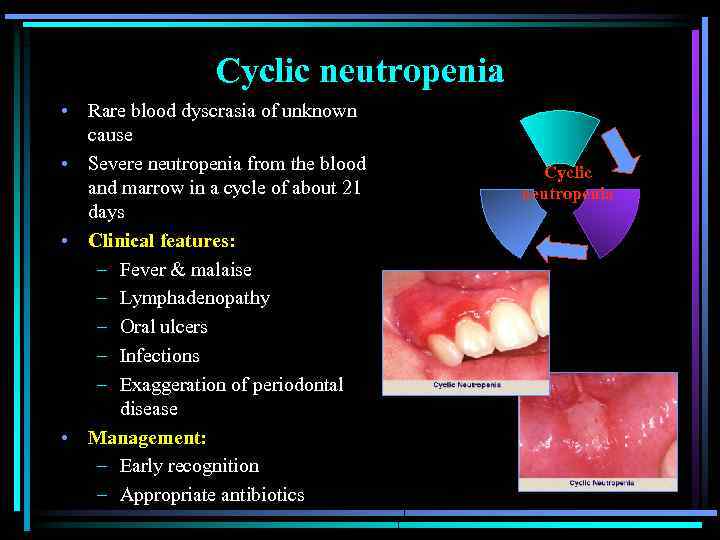
Cyclic neutropenia • Rare blood dyscrasia of unknown cause • Severe neutropenia from the blood and marrow in a cycle of about 21 days • Clinical features: – Fever & malaise – Lymphadenopathy – Oral ulcers – Infections – Exaggeration of periodontal disease • Management: – Early recognition – Appropriate antibiotics Cyclic neutropenia
Oral Ulcerations.ppt