afac672cfded332fc4adbe15d4ebc287.ppt
- Количество слайдов: 29
OR Giving our patients the best chance to survive shock Erik Diringer, DO Intensivist – Kenmore Mercy Hospital
Disclosures None
Vasopressors Powerful class of IV medications that induce vasoconstriction Not to be confused with inotropes Surprisingly a dearth of studies exist comparing their use in different shock states 2
Shock States (Adult) “The rude unhinging of the machinery of life” 2 Significant reduction of systemic tissue perfusion Oxygen consumption > Oxygen delivery (VO 2 > DO 2) Cellular effect Systemic effects Cell death, end-organ damage, MSOF, death Often happens prior to hypotension
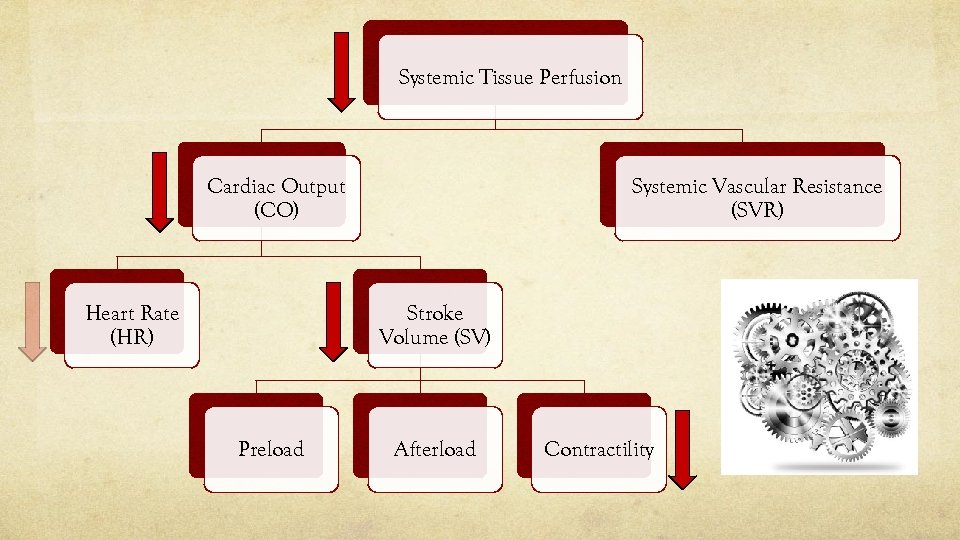
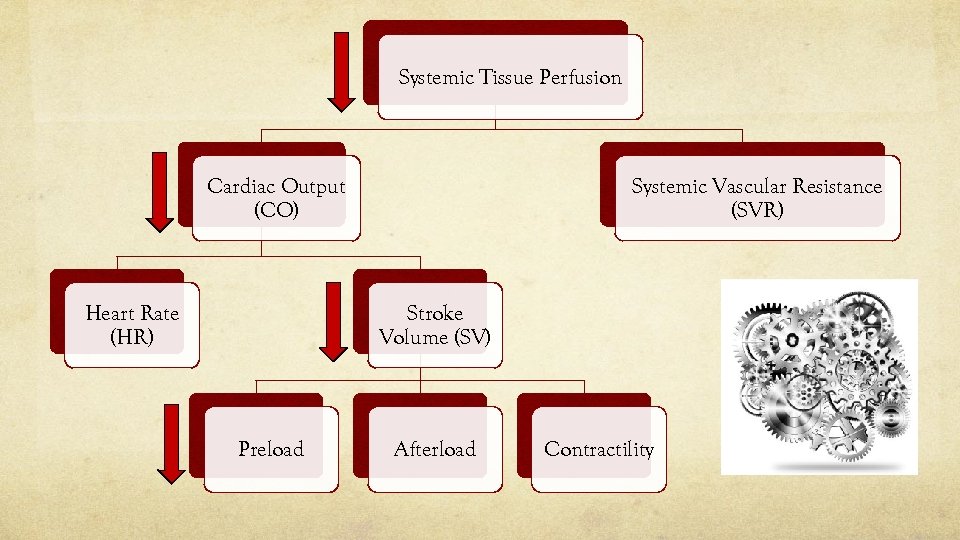
Shock States MAP = (CO x SVR) + CVP CO = HR x SV SV influenced by preload, afterload, contractility
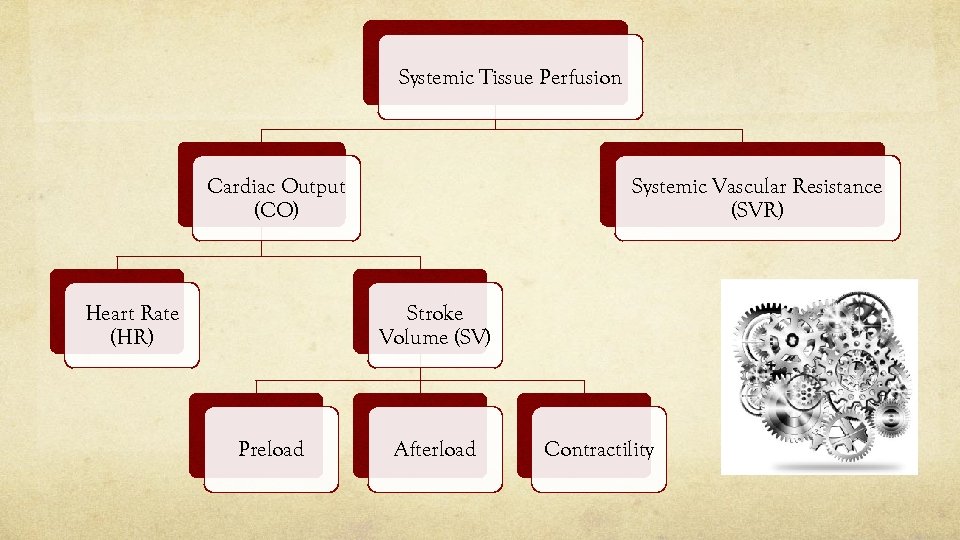
Systemic Tissue Perfusion Systemic Vascular Resistance (SVR) Cardiac Output (CO) Heart Rate (HR) Stroke Volume (SV) Preload Afterload Contractility
Shock States Types: Distributive: dec. SVR Eg) septic shock, SIRS, anaphylaxis, neurogenic, toxins Cardiogenic: dec. contractility (inc. SVR, HR) Eg) CMP, arrhythmia, mechanical, obstructive Hypovolemic: dec. preload (inc. SVR, HR) Eg) fluid loss, hemorrhage
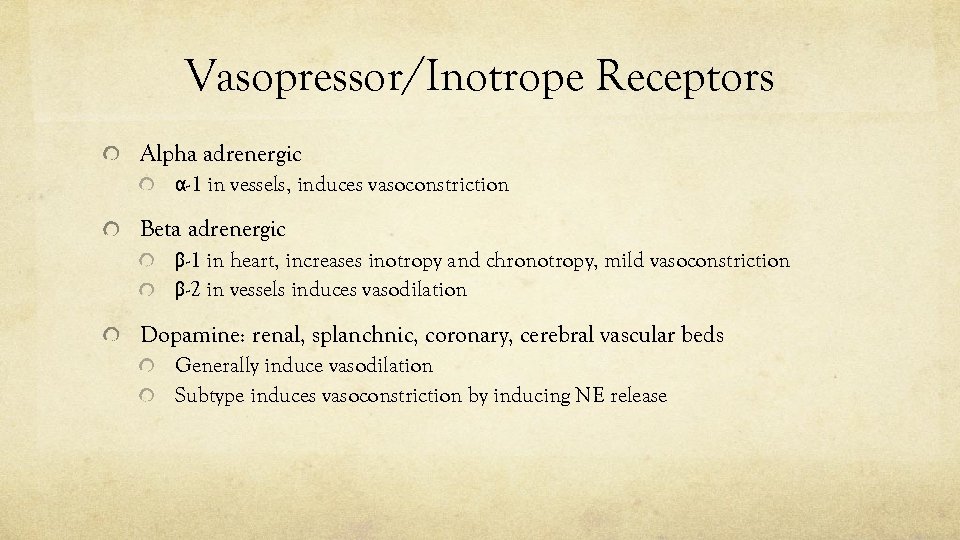
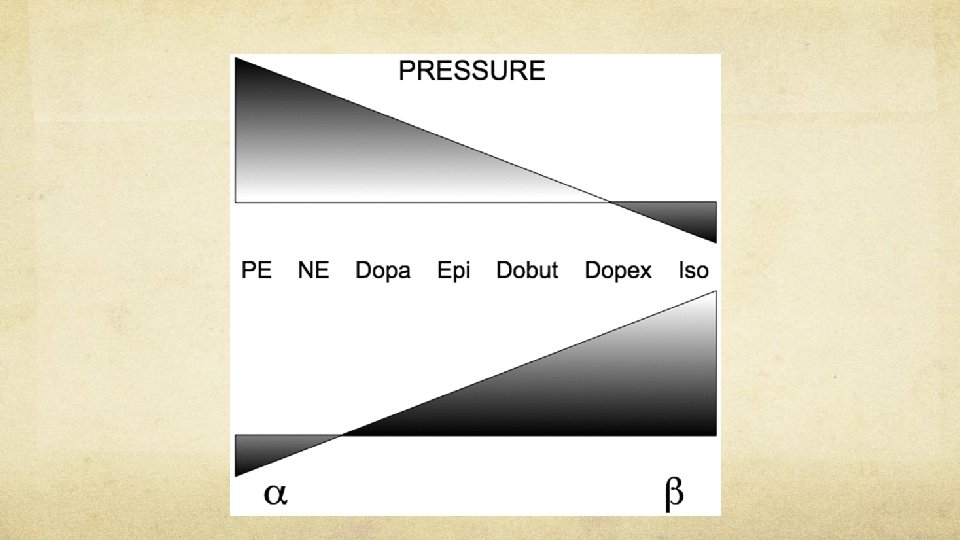
Vasopressor/Inotrope Receptors Alpha adrenergic α-1 in vessels, induces vasoconstriction Beta adrenergic β-1 in heart, increases inotropy and chronotropy, mild vasoconstriction β-2 in vessels induces vasodilation Dopamine: renal, splanchnic, coronary, cerebral vascular beds Generally induce vasodilation Subtype induces vasoconstriction by inducing NE release
Vasopressor Choices Norepinephreine (Levophed) – 0. 02 -1 mcg/kg/min IV α-1 and β-1 activity Potent vasoconstriction, modest inc. CO Phenylephrine (Neo-Synephrine) – 40 -60 mcg/min IV α-1 activity Potent vasoconstriction, dec. SV Epinephrine – 2 -10 mcg/min IV Potent β-1 activity, modest α-1, β-2 inc. CO, dec. SVR α-1 predominates at higher doses Beware of arrhythmias, splanchnic vasoconstriction
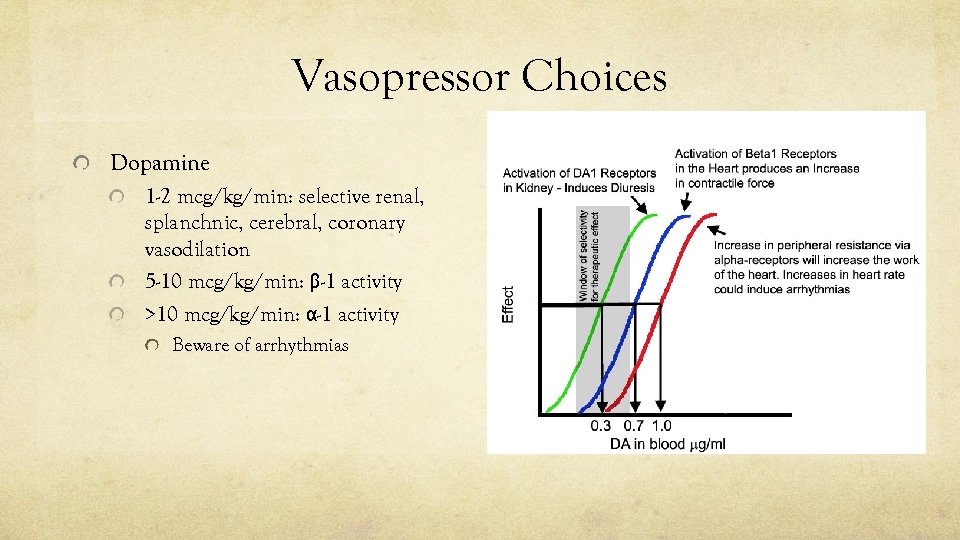
Vasopressor Choices Dopamine 1 -2 mcg/kg/min: selective renal, splanchnic, cerebral, coronary vasodilation 5 -10 mcg/kg/min: β-1 activity >10 mcg/kg/min: α-1 activity Beware of arrhythmias
Vasopressor Choices Vasopressin (ADH) Second-line agent in distributive shock Doses >0. 03 U/min associated with coronary and mesenteric ischemia
Inotrope Choices Dobutamine (Dobutrex) β-1 activity: inc. contractility, dec. SVR Isoproterenol (Isuprel) β-1, β-2 activity: inc. HR, dec. SVR Milrinone PDE inhibitor Non-adrenergic, but similar physiological effect to dobutamine
Pre-Pressor Problems ABCs Volume resuscitation Central access, monitoring Why is my patient in shock? What determinant of tissue perfusion is being adversely affected? HR, preload, afterload, contractility, SVR

Distributive Shock
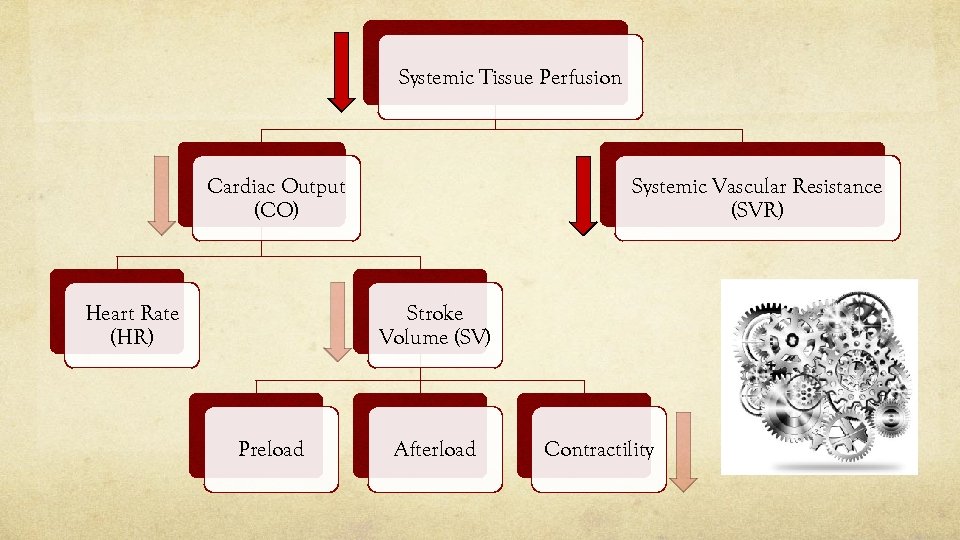
Systemic Tissue Perfusion Systemic Vascular Resistance (SVR) Cardiac Output (CO) Heart Rate (HR) Stroke Volume (SV) Preload Afterload Contractility
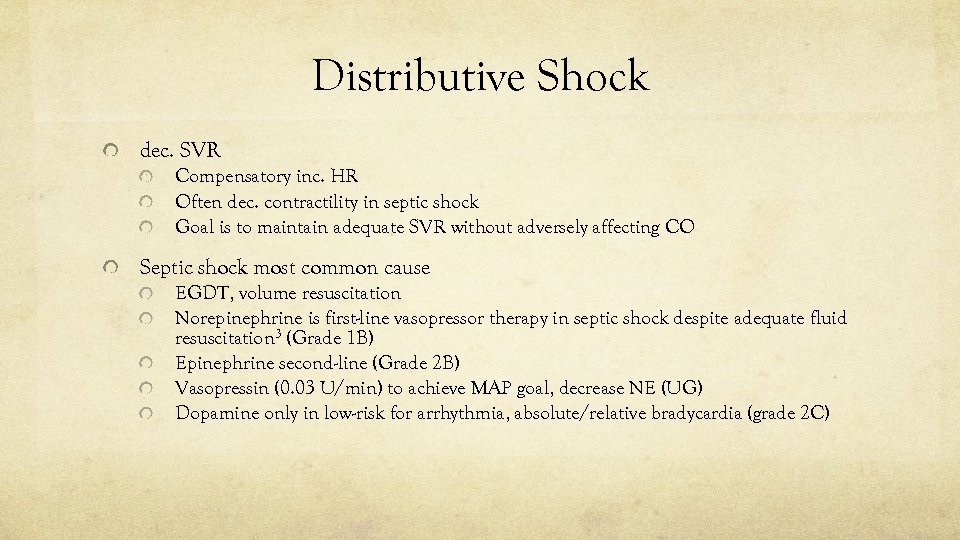
Distributive Shock dec. SVR Compensatory inc. HR Often dec. contractility in septic shock Goal is to maintain adequate SVR without adversely affecting CO Septic shock most common cause EGDT, volume resuscitation Norepinephrine is first-line vasopressor therapy in septic shock despite adequate fluid resuscitation 3 (Grade 1 B) Epinephrine second-line (Grade 2 B) Vasopressin (0. 03 U/min) to achieve MAP goal, decrease NE (UG) Dopamine only in low-risk for arrhythmia, absolute/relative bradycardia (grade 2 C)
Septic Shock Phenylephrine is not recommended , except (grade 1 C): When norepinephrine is associated with serious arrhythmias When CO is high and BP persistently low As salvage therapy when combined inotrope/vasopressor drugs and low-dose vasopressin have failed to achieve the MAP target Phenylephrine is an appropriate pressor in neurogenic shock

Cardiogenic Shock
Systemic Tissue Perfusion Systemic Vascular Resistance (SVR) Cardiac Output (CO) Heart Rate (HR) Stroke Volume (SV) Preload Afterload Contractility
Cardiogenic Shock dec. contractility Compensatory inc. SVR and HR Only vasopressors with β activity are indicated! Avoid α-1 agents that only increase SVR Inotropes preferred when BP adequate Sometime secondary to dec. HR Provide optimal supportive care (p. H, temp, O 2) May require device (VA-ECMO, IABP, VAD, TVP)
Cardiogenic Shock – Obstructive Generally no role for vasopressors Treatment aimed specifically at underlying cause Cardiac tamponade, tension pneumothorax, massive PE

Hypovolemic Shock
Systemic Tissue Perfusion Systemic Vascular Resistance (SVR) Cardiac Output (CO) Heart Rate (HR) Stroke Volume (SV) Preload Afterload Contractility
Hypovolemic Shock dec. preload Compensatory inc. SVR and HR Why is my patient hypovolemic? Fluid loss, hemorrhage Treat the underlying cause Generally vasopressors indicated as temporizing support ie) BP support during intubation, procedures Specific cases Esophageal varices: Vasopressin decreases portal blood flow and improves hemostasis
Take Home Messages Shock often occurs before hypotension Oxygen consumption > Oxygen delivery (VO 2 > DO 2) Tissue perfusion influence by CO and SVR CO influenced by HR, preload, afterload and contractility Shock can be distributive, cardiogenic, hypovolemic or a combination Vasopressor choice directed at mechanism of shock
Take Home Messages Always ask “Why? ” Direct your therapy based upon the answer
References 1. Müllner M, Urbanek B, Havel C, et al. Vasopressors for shock. Cochrane Database Syst Rev 2004; : CD 003709. 2. Simeone FA: Shock, trauma and the surgeon. Ann Surg 1963; 158: 759– 774. 3. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012 (http: //www. survivingsepsis. org/Guidelines).
afac672cfded332fc4adbe15d4ebc287.ppt