0d53699f73df57550739974160461eb5.ppt
- Количество слайдов: 1
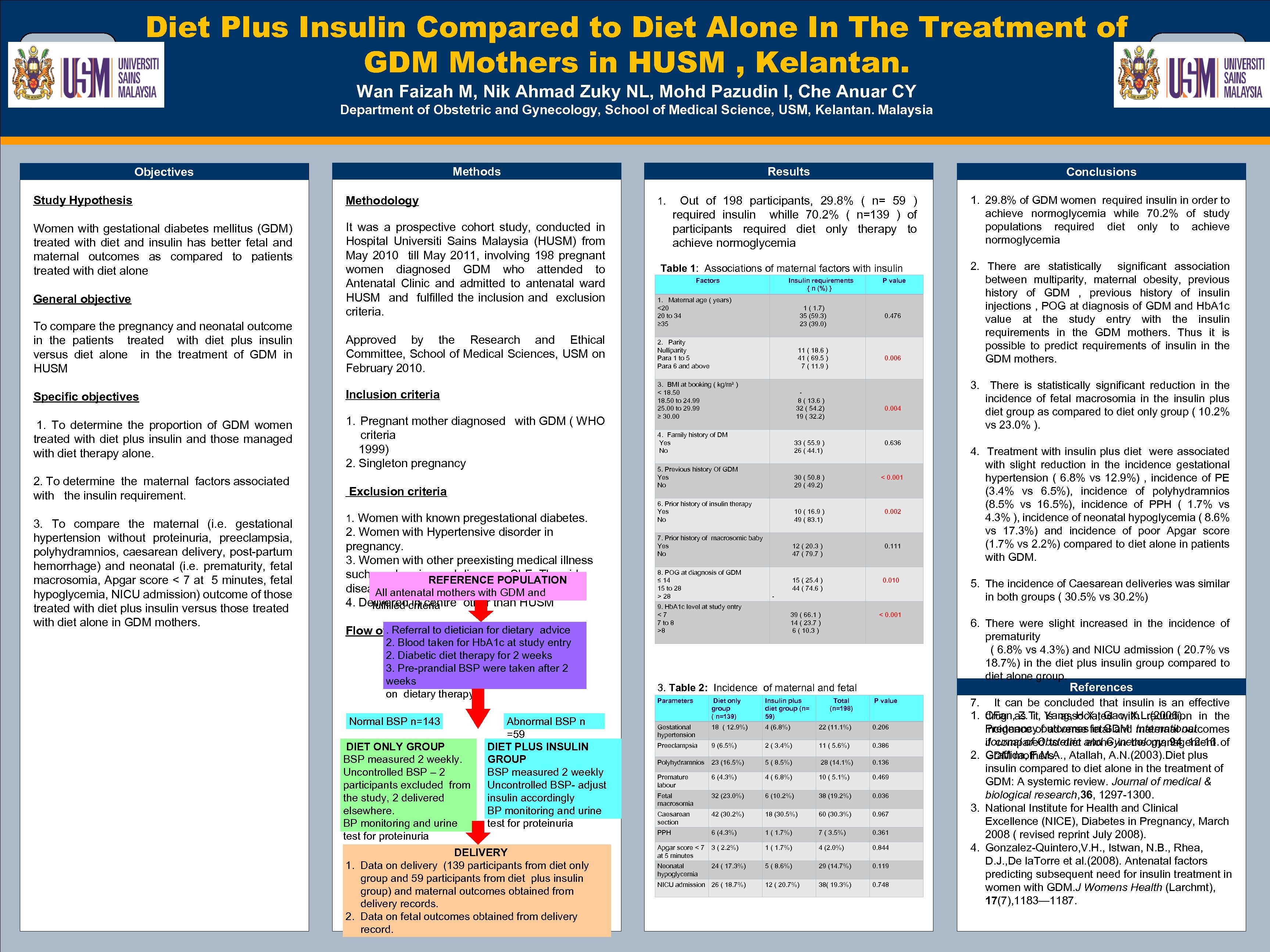 OPTIONAL LOGO HERE Diet Plus Insulin Compared to Diet Alone In The Treatment of GDM Mothers in HUSM , Kelantan. OPTIONAL LOGO HERE Wan Faizah M, Nik Ahmad Zuky NL, Mohd Pazudin I, Che Anuar CY Department of Obstetric and Gynecology, School of Medical Science, USM, Kelantan. Malaysia Methods Objectives Study Hypothesis Conclusions 1. Out of 198 participants, 29. 8% ( n= 59 ) Methodology Results 1. 29. 8% of GDM women required insulin in order to achieve normoglycemia while 70. 2% of study populations required diet only to achieve normoglycemia Women with gestational diabetes mellitus (GDM) treated with diet and insulin has better fetal and maternal outcomes as compared to patients treated with diet alone General objective To compare the pregnancy and neonatal outcome in the patients treated with diet plus insulin versus diet alone in the treatment of GDM in HUSM Specific objectives 1. To determine the proportion of GDM women treated with diet plus insulin and those managed with diet therapy alone. 2. To determine the maternal factors associated with the insulin requirement. 3. To compare the maternal (i. e. gestational hypertension without proteinuria, preeclampsia, polyhydramnios, caesarean delivery, post-partum hemorrhage) and neonatal (i. e. prematurity, fetal macrosomia, Apgar score < 7 at 5 minutes, fetal hypoglycemia, NICU admission) outcome of those treated with diet plus insulin versus those treated with diet alone in GDM mothers. It was a prospective cohort study, conducted in Hospital Universiti Sains Malaysia (HUSM) from May 2010 till May 2011, involving 198 pregnant women diagnosed GDM who attended to Antenatal Clinic and admitted to antenatal ward HUSM and fulfilled the inclusion and exclusion criteria. Approved by the Research and Ethical Committee, School of Medical Sciences, USM on February 2010. Inclusion criteria 1. Pregnant mother diagnosed with GDM ( WHO criteria 1999) 2. Singleton pregnancy Exclusion criteria 1. Women with known pregestational diabetes. 2. Women with Hypertensive disorder in pregnancy. 3. Women with other preexisting medical illness such as chronic renal disease , SLE, Thyroid REFERENCE POPULATION disease, epilepsy, blood disorder. All antenatal mothers with GDM and 4. Delivered in centre other than HUSM fulfilled criteria. Referral to dietician for dietary advice Flow of Study 2. Blood taken for Hb. A 1 c at study entry 2. Diabetic diet therapy for 2 weeks 3. Pre-prandial BSP were taken after 2 weeks on dietary therapy. Normal BSP n=143 DIET ONLY GROUP BSP measured 2 weekly. Uncontrolled BSP – 2 participants excluded from the study, 2 delivered elsewhere. BP monitoring and urine test for proteinuria Abnormal BSP n =59 DIET PLUS INSULIN GROUP BSP measured 2 weekly Uncontrolled BSP- adjust insulin accordingly BP monitoring and urine test for proteinuria DELIVERY 1. Data on delivery (139 participants from diet only group and 59 participants from diet plus insulin group) and maternal outcomes obtained from delivery records. 2. Data on fetal outcomes obtained from delivery record. TEMPLATE DESIGN © 2008 www. Poster. Presentations. com required insulin whille 70. 2% ( n=139 ) of participants required diet only therapy to achieve normoglycemia Table 1: Associations of maternal factors with insulin Factors Insulin requirements P value requirements in the treatment of GDM { n (%) } 1. Maternal age ( years) <20 20 to 34 ≥ 35 1 ( 1. 7) 35 (59. 3) 23 (39. 0) 0. 476 2. Parity Nulliparity Para 1 to 5 Para 6 and above 11 ( 18. 6 ) 41 ( 69. 5 ) 7 ( 11. 9 ) 0. 006 3. BMI at booking ( kg/m² ) < 18. 50 to 24. 99 25. 00 to 29. 99 ≥ 30. 00 8 ( 13. 6 ) 32 ( 54. 2) 19 ( 32. 2) 4. Family history of DM Yes No 33 ( 55. 9 ) 26 ( 44. 1) 0. 636 5. Previous history Of GDM Yes No 30 ( 50. 8 ) 29 ( 49. 2) < 0. 001 6. Prior history of insulin therapy Yes No 10 ( 16. 9 ) 49 ( 83. 1) 0. 002 7. Prior history of macrosomic baby Yes No 12 ( 20. 3 ) 47 ( 79. 7 ) 0. 111 8. POG at diagnosis of GDM ≤ 14 15 to 28 > 28 15 ( 25. 4 ) 44 ( 74. 6 ) - 0. 010 9. Hb. A 1 c level at study entry < 7 7 to 8 >8 39 ( 66. 1 ) 14 ( 23. 7 ) 6 ( 10. 3 ) 0. 004 < 0. 001 3. Table 2: Incidence of maternal and fetal Parameters Diet only Insulin plus Total P value complications in GDM mothers treated with insulin plus group diet group (n=198) diet therapy as compared to diet only ( n=139) 59) Gestational hypertension 18 ( 12. 9%) 4 (6. 8%) 22 (11. 1%) 0. 206 Preeclampsia 9 (6. 5%) 2 ( 3. 4%) 11 ( 5. 6%) 0. 386 Polyhydramnios 23 (16. 5%) 5 ( 8. 5%) 28 (14. 1%) 0. 136 Premature labour 6 (4. 3%) 4 ( 6. 8%) 10 ( 5. 1%) 0. 469 Fetal macrosomia 32 (23. 0%) 6 (10. 2%) 38 (19. 2%) 0. 036 Caesarean section 42 (30. 2%) 18 (30. 5%) 60 (30. 3%) 0. 967 PPH 6 (4. 3%) 1 ( 1. 7%) 7 ( 3. 5%) 0. 361 Apgar score < 7 3 ( 2. 2%) at 5 minutes 1 ( 1. 7%) 4 (2. 0%) 0. 844 Neonatal hypoglycemia 5 ( 8. 6%) 29 (14. 7%) 0. 119 12 ( 20. 7%) 38( 19. 3%) 0. 748 24 ( 17. 3%) NICU admission 26 ( 18. 7%) 2. There are statistically significant association between multiparity, maternal obesity, previous history of GDM , previous history of insulin injections , POG at diagnosis of GDM and Hb. A 1 c value at the study entry with the insulin requirements in the GDM mothers. Thus it is possible to predict requirements of insulin in the GDM mothers. 3. There is statistically significant reduction in the incidence of fetal macrosomia in the insulin plus diet group as compared to diet only group ( 10. 2% vs 23. 0% ). 4. Treatment with insulin plus diet were associated with slight reduction in the incidence gestational hypertension ( 6. 8% vs 12. 9%) , incidence of PE (3. 4% vs 6. 5%), incidence of polyhydramnios (8. 5% vs 16. 5%), incidence of PPH ( 1. 7% vs 4. 3% ), incidence of neonatal hypoglycemia ( 8. 6% vs 17. 3%) and incidence of poor Apgar score (1. 7% vs 2. 2%) compared to diet alone in patients with GDM. 5. The incidence of Caesarean deliveries was similar in both groups ( 30. 5% vs 30. 2%) 6. There were slight increased in the incidence of prematurity ( 6. 8% vs 4. 3%) and NICU admission ( 20. 7% vs 18. 7%) in the diet plus insulin group compared to diet alone group. References 7. It can be concluded that insulin is an effective 1. drug as it is associated with reduction in the CFan, Z. T. , Yang, H. X. , Gao, X. L. (2006). Pregnancy outcomes in GDM. International incidence of adverse fetal and maternal outcomes Journal of Obstetric alone in the management if compared to diet and Gynecology, 94, 12 -16. of 2. GDM mothers. Graffida, F. M. A. , Atallah, A. N. (2003). Diet plus insulin compared to diet alone in the treatment of GDM: A systemic review. Journal of medical & biological research, 36, 1297 -1300. 3. National Institute for Health and Clinical Excellence (NICE), Diabetes in Pregnancy, March 2008 ( revised reprint July 2008). 4. Gonzalez-Quintero, V. H. , Istwan, N. B. , Rhea, D. J. , De la. Torre et al. (2008). Antenatal factors predicting subsequent need for insulin treatment in women with GDM. J Womens Health (Larchmt), 17(7), 1183— 1187.
OPTIONAL LOGO HERE Diet Plus Insulin Compared to Diet Alone In The Treatment of GDM Mothers in HUSM , Kelantan. OPTIONAL LOGO HERE Wan Faizah M, Nik Ahmad Zuky NL, Mohd Pazudin I, Che Anuar CY Department of Obstetric and Gynecology, School of Medical Science, USM, Kelantan. Malaysia Methods Objectives Study Hypothesis Conclusions 1. Out of 198 participants, 29. 8% ( n= 59 ) Methodology Results 1. 29. 8% of GDM women required insulin in order to achieve normoglycemia while 70. 2% of study populations required diet only to achieve normoglycemia Women with gestational diabetes mellitus (GDM) treated with diet and insulin has better fetal and maternal outcomes as compared to patients treated with diet alone General objective To compare the pregnancy and neonatal outcome in the patients treated with diet plus insulin versus diet alone in the treatment of GDM in HUSM Specific objectives 1. To determine the proportion of GDM women treated with diet plus insulin and those managed with diet therapy alone. 2. To determine the maternal factors associated with the insulin requirement. 3. To compare the maternal (i. e. gestational hypertension without proteinuria, preeclampsia, polyhydramnios, caesarean delivery, post-partum hemorrhage) and neonatal (i. e. prematurity, fetal macrosomia, Apgar score < 7 at 5 minutes, fetal hypoglycemia, NICU admission) outcome of those treated with diet plus insulin versus those treated with diet alone in GDM mothers. It was a prospective cohort study, conducted in Hospital Universiti Sains Malaysia (HUSM) from May 2010 till May 2011, involving 198 pregnant women diagnosed GDM who attended to Antenatal Clinic and admitted to antenatal ward HUSM and fulfilled the inclusion and exclusion criteria. Approved by the Research and Ethical Committee, School of Medical Sciences, USM on February 2010. Inclusion criteria 1. Pregnant mother diagnosed with GDM ( WHO criteria 1999) 2. Singleton pregnancy Exclusion criteria 1. Women with known pregestational diabetes. 2. Women with Hypertensive disorder in pregnancy. 3. Women with other preexisting medical illness such as chronic renal disease , SLE, Thyroid REFERENCE POPULATION disease, epilepsy, blood disorder. All antenatal mothers with GDM and 4. Delivered in centre other than HUSM fulfilled criteria. Referral to dietician for dietary advice Flow of Study 2. Blood taken for Hb. A 1 c at study entry 2. Diabetic diet therapy for 2 weeks 3. Pre-prandial BSP were taken after 2 weeks on dietary therapy. Normal BSP n=143 DIET ONLY GROUP BSP measured 2 weekly. Uncontrolled BSP – 2 participants excluded from the study, 2 delivered elsewhere. BP monitoring and urine test for proteinuria Abnormal BSP n =59 DIET PLUS INSULIN GROUP BSP measured 2 weekly Uncontrolled BSP- adjust insulin accordingly BP monitoring and urine test for proteinuria DELIVERY 1. Data on delivery (139 participants from diet only group and 59 participants from diet plus insulin group) and maternal outcomes obtained from delivery records. 2. Data on fetal outcomes obtained from delivery record. TEMPLATE DESIGN © 2008 www. Poster. Presentations. com required insulin whille 70. 2% ( n=139 ) of participants required diet only therapy to achieve normoglycemia Table 1: Associations of maternal factors with insulin Factors Insulin requirements P value requirements in the treatment of GDM { n (%) } 1. Maternal age ( years) <20 20 to 34 ≥ 35 1 ( 1. 7) 35 (59. 3) 23 (39. 0) 0. 476 2. Parity Nulliparity Para 1 to 5 Para 6 and above 11 ( 18. 6 ) 41 ( 69. 5 ) 7 ( 11. 9 ) 0. 006 3. BMI at booking ( kg/m² ) < 18. 50 to 24. 99 25. 00 to 29. 99 ≥ 30. 00 8 ( 13. 6 ) 32 ( 54. 2) 19 ( 32. 2) 4. Family history of DM Yes No 33 ( 55. 9 ) 26 ( 44. 1) 0. 636 5. Previous history Of GDM Yes No 30 ( 50. 8 ) 29 ( 49. 2) < 0. 001 6. Prior history of insulin therapy Yes No 10 ( 16. 9 ) 49 ( 83. 1) 0. 002 7. Prior history of macrosomic baby Yes No 12 ( 20. 3 ) 47 ( 79. 7 ) 0. 111 8. POG at diagnosis of GDM ≤ 14 15 to 28 > 28 15 ( 25. 4 ) 44 ( 74. 6 ) - 0. 010 9. Hb. A 1 c level at study entry < 7 7 to 8 >8 39 ( 66. 1 ) 14 ( 23. 7 ) 6 ( 10. 3 ) 0. 004 < 0. 001 3. Table 2: Incidence of maternal and fetal Parameters Diet only Insulin plus Total P value complications in GDM mothers treated with insulin plus group diet group (n=198) diet therapy as compared to diet only ( n=139) 59) Gestational hypertension 18 ( 12. 9%) 4 (6. 8%) 22 (11. 1%) 0. 206 Preeclampsia 9 (6. 5%) 2 ( 3. 4%) 11 ( 5. 6%) 0. 386 Polyhydramnios 23 (16. 5%) 5 ( 8. 5%) 28 (14. 1%) 0. 136 Premature labour 6 (4. 3%) 4 ( 6. 8%) 10 ( 5. 1%) 0. 469 Fetal macrosomia 32 (23. 0%) 6 (10. 2%) 38 (19. 2%) 0. 036 Caesarean section 42 (30. 2%) 18 (30. 5%) 60 (30. 3%) 0. 967 PPH 6 (4. 3%) 1 ( 1. 7%) 7 ( 3. 5%) 0. 361 Apgar score < 7 3 ( 2. 2%) at 5 minutes 1 ( 1. 7%) 4 (2. 0%) 0. 844 Neonatal hypoglycemia 5 ( 8. 6%) 29 (14. 7%) 0. 119 12 ( 20. 7%) 38( 19. 3%) 0. 748 24 ( 17. 3%) NICU admission 26 ( 18. 7%) 2. There are statistically significant association between multiparity, maternal obesity, previous history of GDM , previous history of insulin injections , POG at diagnosis of GDM and Hb. A 1 c value at the study entry with the insulin requirements in the GDM mothers. Thus it is possible to predict requirements of insulin in the GDM mothers. 3. There is statistically significant reduction in the incidence of fetal macrosomia in the insulin plus diet group as compared to diet only group ( 10. 2% vs 23. 0% ). 4. Treatment with insulin plus diet were associated with slight reduction in the incidence gestational hypertension ( 6. 8% vs 12. 9%) , incidence of PE (3. 4% vs 6. 5%), incidence of polyhydramnios (8. 5% vs 16. 5%), incidence of PPH ( 1. 7% vs 4. 3% ), incidence of neonatal hypoglycemia ( 8. 6% vs 17. 3%) and incidence of poor Apgar score (1. 7% vs 2. 2%) compared to diet alone in patients with GDM. 5. The incidence of Caesarean deliveries was similar in both groups ( 30. 5% vs 30. 2%) 6. There were slight increased in the incidence of prematurity ( 6. 8% vs 4. 3%) and NICU admission ( 20. 7% vs 18. 7%) in the diet plus insulin group compared to diet alone group. References 7. It can be concluded that insulin is an effective 1. drug as it is associated with reduction in the CFan, Z. T. , Yang, H. X. , Gao, X. L. (2006). Pregnancy outcomes in GDM. International incidence of adverse fetal and maternal outcomes Journal of Obstetric alone in the management if compared to diet and Gynecology, 94, 12 -16. of 2. GDM mothers. Graffida, F. M. A. , Atallah, A. N. (2003). Diet plus insulin compared to diet alone in the treatment of GDM: A systemic review. Journal of medical & biological research, 36, 1297 -1300. 3. National Institute for Health and Clinical Excellence (NICE), Diabetes in Pregnancy, March 2008 ( revised reprint July 2008). 4. Gonzalez-Quintero, V. H. , Istwan, N. B. , Rhea, D. J. , De la. Torre et al. (2008). Antenatal factors predicting subsequent need for insulin treatment in women with GDM. J Womens Health (Larchmt), 17(7), 1183— 1187.


