e2a9f7d98be23c6b8a34d386aa1e029c.ppt
- Количество слайдов: 84
 OPEN LUNG AND LUNG RECRUITMENT PEEP & Oxygenation in Today’s ICU RET 2264 C Dr. J. B. Elsberry Prof. J. M. Newberry Special Thanks to: Susan P. Pilbeam, MS, RRT, FAARC Supported by funds from Maquet (Servo Ventilator) Gary F. Nieman, Asst. Research Professor State University of NY, Upstate Medical Center Joseph E. Previtera, RRT Respiratory Care Department Beth Israel Deaconess Medical Center Boston, MA
OPEN LUNG AND LUNG RECRUITMENT PEEP & Oxygenation in Today’s ICU RET 2264 C Dr. J. B. Elsberry Prof. J. M. Newberry Special Thanks to: Susan P. Pilbeam, MS, RRT, FAARC Supported by funds from Maquet (Servo Ventilator) Gary F. Nieman, Asst. Research Professor State University of NY, Upstate Medical Center Joseph E. Previtera, RRT Respiratory Care Department Beth Israel Deaconess Medical Center Boston, MA
 Open Lung and Protective Lung Strategies 1. History and Definitions – ARDS/ALI 2. Ventilator Induced Lung Injury 3. ARDS Network Study – 4. Lung Protective Strategies 5. Lung Recruitment
Open Lung and Protective Lung Strategies 1. History and Definitions – ARDS/ALI 2. Ventilator Induced Lung Injury 3. ARDS Network Study – 4. Lung Protective Strategies 5. Lung Recruitment
 Historical Perspective on ARDS • Original publication – The Lancet: 1967, Ashbaugh, Bigelow, Petty and Levine. • “The clinical pattern which we will refer to as the respiratory distress syndrome, includes severe dyspnea, tachypnea, cyanosis that is refractory to oxygen therapy, loss of lung compliance and diffuse alveolar infiltration see on chest Xray. ”
Historical Perspective on ARDS • Original publication – The Lancet: 1967, Ashbaugh, Bigelow, Petty and Levine. • “The clinical pattern which we will refer to as the respiratory distress syndrome, includes severe dyspnea, tachypnea, cyanosis that is refractory to oxygen therapy, loss of lung compliance and diffuse alveolar infiltration see on chest Xray. ”
 Identified During Vietnam Conflict • • Da Nang lung Shock lung Pump lung “This disorder is best described as a homogenous acute metabolic malfunction of the lung parenchyma…” Pilbeam, Mechanical Ventilation, 1986. • Is this definition TRUE?
Identified During Vietnam Conflict • • Da Nang lung Shock lung Pump lung “This disorder is best described as a homogenous acute metabolic malfunction of the lung parenchyma…” Pilbeam, Mechanical Ventilation, 1986. • Is this definition TRUE?
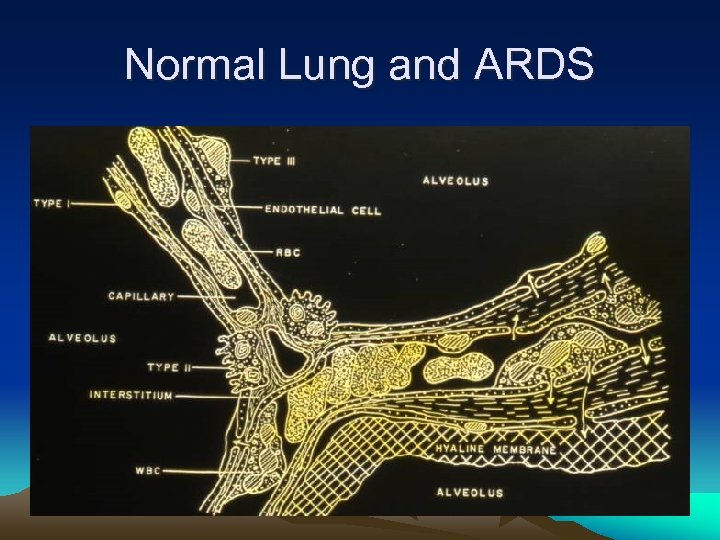 Normal Lung and ARDS
Normal Lung and ARDS
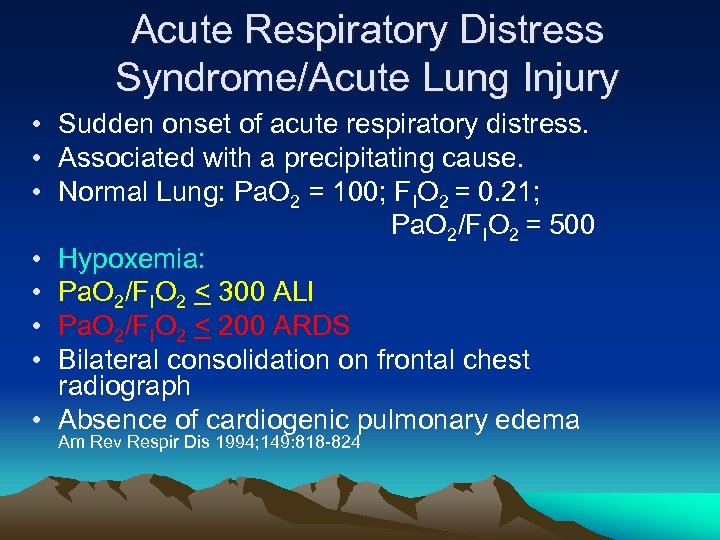 Acute Respiratory Distress Syndrome/Acute Lung Injury • Sudden onset of acute respiratory distress. • Associated with a precipitating cause. • Normal Lung: Pa. O 2 = 100; FIO 2 = 0. 21; Pa. O 2/FIO 2 = 500 • Hypoxemia: • Pa. O 2/FIO 2 < 300 ALI • Pa. O 2/FIO 2 < 200 ARDS • Bilateral consolidation on frontal chest radiograph • Absence of cardiogenic pulmonary edema Am Rev Respir Dis 1994; 149: 818 -824
Acute Respiratory Distress Syndrome/Acute Lung Injury • Sudden onset of acute respiratory distress. • Associated with a precipitating cause. • Normal Lung: Pa. O 2 = 100; FIO 2 = 0. 21; Pa. O 2/FIO 2 = 500 • Hypoxemia: • Pa. O 2/FIO 2 < 300 ALI • Pa. O 2/FIO 2 < 200 ARDS • Bilateral consolidation on frontal chest radiograph • Absence of cardiogenic pulmonary edema Am Rev Respir Dis 1994; 149: 818 -824
 Associated Causes of ARDS • Direct lung injury ( Primary or Pulmonary) • Indirect (Secondary or Extrapulmonary) • Gattinoni, Am J Respir Crit Care med 1998; 158: 3 -11 ARDS Consensus Conference, Am Rev Resp Dis, 1994: 149: 818 -824
Associated Causes of ARDS • Direct lung injury ( Primary or Pulmonary) • Indirect (Secondary or Extrapulmonary) • Gattinoni, Am J Respir Crit Care med 1998; 158: 3 -11 ARDS Consensus Conference, Am Rev Resp Dis, 1994: 149: 818 -824
 DIRECT LUNG INJURY (Causes of ARDS) • • • Also called: Primary or Pulmonary Direct effect on lung parenchyma Infectious pneumonia Aspiration or other chemical pneumonitis Chest wall or lung trauma – lung contusion Near Drowning Journal of Resp. Intensive Care Medicine 1998: 158: 3 -11
DIRECT LUNG INJURY (Causes of ARDS) • • • Also called: Primary or Pulmonary Direct effect on lung parenchyma Infectious pneumonia Aspiration or other chemical pneumonitis Chest wall or lung trauma – lung contusion Near Drowning Journal of Resp. Intensive Care Medicine 1998: 158: 3 -11
 INDIRECT LUNG INJURY (Secondary or Extra-pulmonary) • Nonpulmonary induced ARDS causes: – Sepsis; inflammation – Acute Pancreatitis – Multiple trauma, burns – Shock, hypoperfusion -Journal of Resp. Intensive Care Medicine 2001: 164(9): 1701 -1711
INDIRECT LUNG INJURY (Secondary or Extra-pulmonary) • Nonpulmonary induced ARDS causes: – Sepsis; inflammation – Acute Pancreatitis – Multiple trauma, burns – Shock, hypoperfusion -Journal of Resp. Intensive Care Medicine 2001: 164(9): 1701 -1711
 Clinical Presentation ARDS • Hypoxemia non-responsive to oxygen therapy (I. P. Shunt); perfusion without ventilation. • Increased dead space; ventilation without perfusion. – Requiring high minute ventilation – Hypercapnia • Reduced lung compliance; normal in an intubated person about 50 to 100 m. L/cm H 2 O – Accompanying tachypnea – Dyspnea
Clinical Presentation ARDS • Hypoxemia non-responsive to oxygen therapy (I. P. Shunt); perfusion without ventilation. • Increased dead space; ventilation without perfusion. – Requiring high minute ventilation – Hypercapnia • Reduced lung compliance; normal in an intubated person about 50 to 100 m. L/cm H 2 O – Accompanying tachypnea – Dyspnea
 Pathophysiology of ARDS/ALI • Alveolar-capillary (AC) injury with alteration of the normal endothelial and epithelial barrier • Increased permeability of the AC membrane • Inflammatory response with • Release of chemical mediators – Recruitment of inflammatory cells
Pathophysiology of ARDS/ALI • Alveolar-capillary (AC) injury with alteration of the normal endothelial and epithelial barrier • Increased permeability of the AC membrane • Inflammatory response with • Release of chemical mediators – Recruitment of inflammatory cells
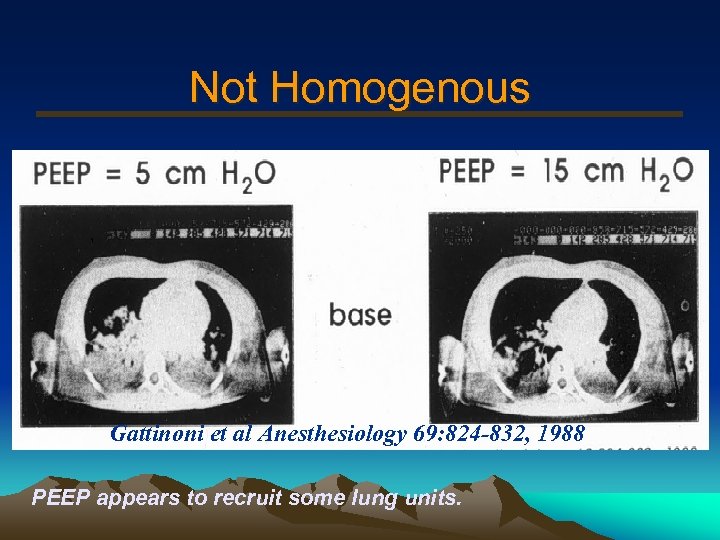 Not Homogenous Gattinoni et al Anesthesiology 69: 824 -832, 1988 PEEP appears to recruit some lung units.
Not Homogenous Gattinoni et al Anesthesiology 69: 824 -832, 1988 PEEP appears to recruit some lung units.
 Part 2 • Lung injuries caused from conventional mechanical ventilation.
Part 2 • Lung injuries caused from conventional mechanical ventilation.
 Ventilator Induced Lung Injury • Studies as early as 1970 showed use of mechanical ventilators injured the lung. • In the 1970 s -1980 s it was not uncommon to see VT of 15 m. L/kg • Not unheard of to see high PIP upwards of 90 -100 cm H 2 O.
Ventilator Induced Lung Injury • Studies as early as 1970 showed use of mechanical ventilators injured the lung. • In the 1970 s -1980 s it was not uncommon to see VT of 15 m. L/kg • Not unheard of to see high PIP upwards of 90 -100 cm H 2 O.
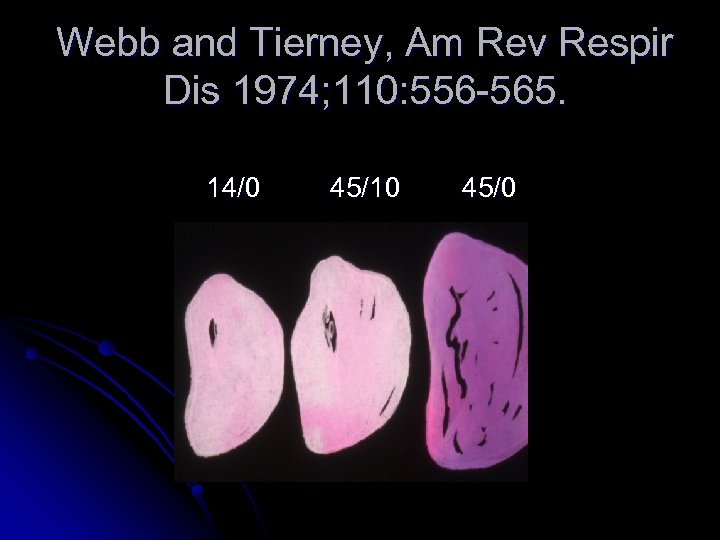 Webb and Tierney, Am Rev Respir Dis 1974; 110: 556 -565. 14/0 45/10 45/0
Webb and Tierney, Am Rev Respir Dis 1974; 110: 556 -565. 14/0 45/10 45/0
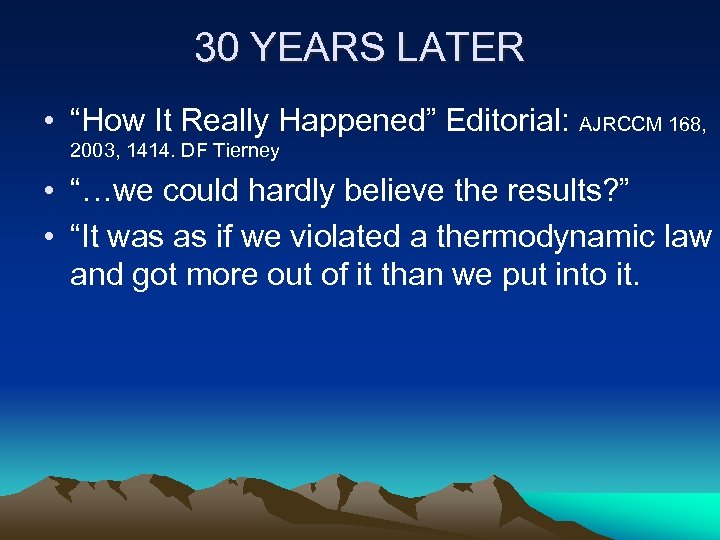 30 YEARS LATER • “How It Really Happened” Editorial: AJRCCM 168, 2003, 1414. DF Tierney • “…we could hardly believe the results? ” • “It was as if we violated a thermodynamic law and got more out of it than we put into it.
30 YEARS LATER • “How It Really Happened” Editorial: AJRCCM 168, 2003, 1414. DF Tierney • “…we could hardly believe the results? ” • “It was as if we violated a thermodynamic law and got more out of it than we put into it.
 “Within minutes the rats were cyanotic and appeared moribund…But were human lungs likely to be injured at all from those pressures? . . It took a decade or two for others to conclude that human lungs could be injured by such ventilation. Our final paragraph 30 years ago suggested management …using protective ventilation and low tidal volumes. -- Tierney
“Within minutes the rats were cyanotic and appeared moribund…But were human lungs likely to be injured at all from those pressures? . . It took a decade or two for others to conclude that human lungs could be injured by such ventilation. Our final paragraph 30 years ago suggested management …using protective ventilation and low tidal volumes. -- Tierney
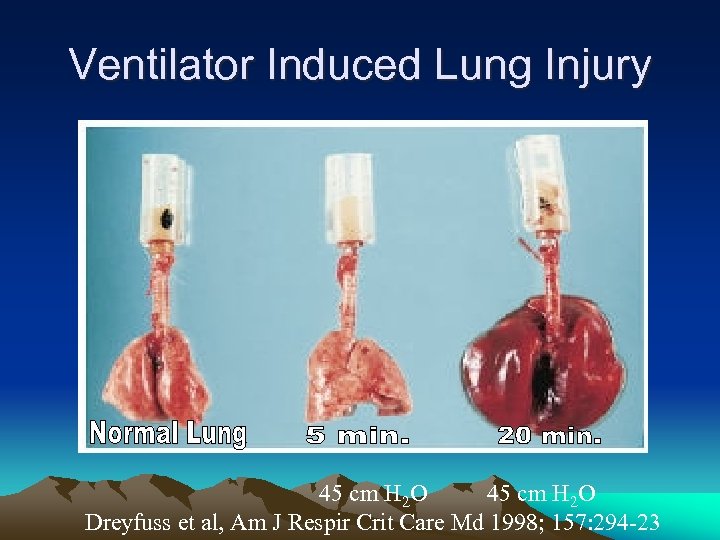 Ventilator Induced Lung Injury 45 cm H 2 O Dreyfuss et al, Am J Respir Crit Care Md 1998; 157: 294 -23
Ventilator Induced Lung Injury 45 cm H 2 O Dreyfuss et al, Am J Respir Crit Care Md 1998; 157: 294 -23
 Ventilator Associated Lung Injury versus Ventilator Induced Lung Injury • VALI -Ventilator associated pneumonias (VAPS) -Oxygen toxicity -Barotrauma (pneumothorax, pneumomediastinum, subcutaneous emphysema, etc) -Over distention of the lung -Collapse of the alveolar units
Ventilator Associated Lung Injury versus Ventilator Induced Lung Injury • VALI -Ventilator associated pneumonias (VAPS) -Oxygen toxicity -Barotrauma (pneumothorax, pneumomediastinum, subcutaneous emphysema, etc) -Over distention of the lung -Collapse of the alveolar units
 Ventilator Induced Lung Injury. Biophysical Injury • VILI • Caused Specifically by Mechanical Ventilation with High Positive Pressures and/or Volumes (animal models) – Altered lung fluid balance – Increased endothelial and epithelial permeability – Severe tissue damage
Ventilator Induced Lung Injury. Biophysical Injury • VILI • Caused Specifically by Mechanical Ventilation with High Positive Pressures and/or Volumes (animal models) – Altered lung fluid balance – Increased endothelial and epithelial permeability – Severe tissue damage
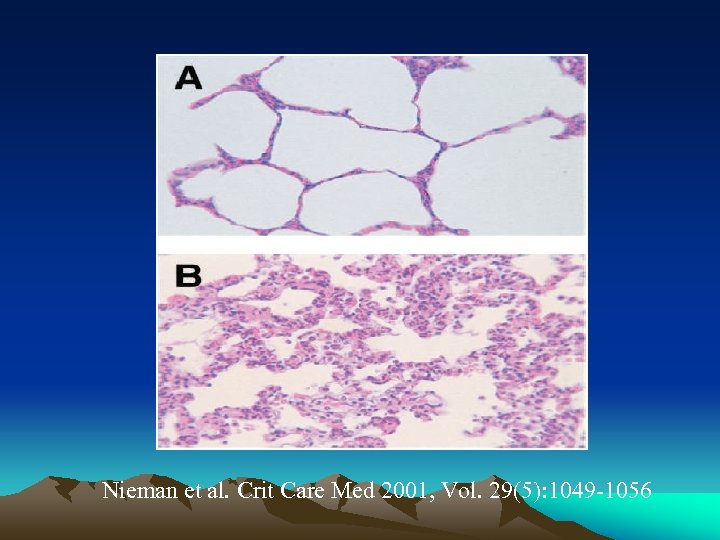 Nieman et al. Crit Care Med 2001, Vol. 29(5): 1049 -1056
Nieman et al. Crit Care Med 2001, Vol. 29(5): 1049 -1056
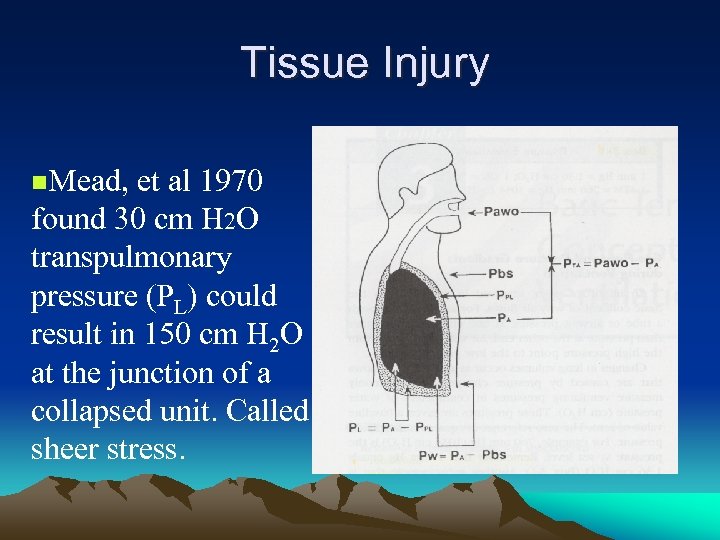 Tissue Injury n. Mead, et al 1970 found 30 cm H 2 O transpulmonary pressure (PL) could result in 150 cm H 2 O at the junction of a collapsed unit. Called sheer stress.
Tissue Injury n. Mead, et al 1970 found 30 cm H 2 O transpulmonary pressure (PL) could result in 150 cm H 2 O at the junction of a collapsed unit. Called sheer stress.
 • Transpulmonary Pressure and It’s the Sheer Stress Closing of the Alveoli in between breaths that caused the damage
• Transpulmonary Pressure and It’s the Sheer Stress Closing of the Alveoli in between breaths that caused the damage
 Alveoli Instablity • Instability occurs in ARDS due to absent or altered surfactant. • Also occurs with VILI • Opening and closing of alveoli. – Causing milking out of surfactant and alveolar instability.
Alveoli Instablity • Instability occurs in ARDS due to absent or altered surfactant. • Also occurs with VILI • Opening and closing of alveoli. – Causing milking out of surfactant and alveolar instability.
 Surfactant’s Important Role • Webb and Tierney: AJRCCM 168, 2003, 1414. DF Tierney • “Lipids (sufactant) form a layer one molecule thick between air and liquid. When the area decreases, the molecules can be formed together until some pop out on the surface. Such ‘used’ lipids don’t respread rapidly, although newly secreted surfactant will. ”
Surfactant’s Important Role • Webb and Tierney: AJRCCM 168, 2003, 1414. DF Tierney • “Lipids (sufactant) form a layer one molecule thick between air and liquid. When the area decreases, the molecules can be formed together until some pop out on the surface. Such ‘used’ lipids don’t respread rapidly, although newly secreted surfactant will. ”
 RESULT • “As a consequence, surfactant in the surface may be squeezed out at low lung volumes when the surface area decreases, and then newly secreted surfactant would be required to replace it. ” • “The greater the decrease of surface area (alveolar volume change) during exhalation, the more molecules would leave and need to be replaced by newly secreted surfactant. ”
RESULT • “As a consequence, surfactant in the surface may be squeezed out at low lung volumes when the surface area decreases, and then newly secreted surfactant would be required to replace it. ” • “The greater the decrease of surface area (alveolar volume change) during exhalation, the more molecules would leave and need to be replaced by newly secreted surfactant. ”
 Biochemical Injury • Overinflation of the lungs in animal studies. • Release of inflammatory mediators. – Cytokines – Leukotrienes – Complement prostanoids – Reactive oxygen species – Proteases
Biochemical Injury • Overinflation of the lungs in animal studies. • Release of inflammatory mediators. – Cytokines – Leukotrienes – Complement prostanoids – Reactive oxygen species – Proteases
 Release of Inflammatory Mediators During Mechanical Ventilation • Leak from the lungs during mechanical ventilation and enter the circulation. • Animal study (rat) with cytokines measured. Von Bethmann et al, Am J Respir Crit Care Med 1998; 157: 263. • Mechanical ventilation may contribute to a systemic inflammatory response. • Repeated stretching (high transpulmonary pressure) may increase cytokine release. Tremblay L, et al AJRCCM, 157, 1997, 944. • Repeated opening and closing (dogs) caused release of bacteria from the alveoli to the blood stream. Effect reduced when PEEP of 10 added. (Nahum et al. , CCM, 25, 1997, 1733. )
Release of Inflammatory Mediators During Mechanical Ventilation • Leak from the lungs during mechanical ventilation and enter the circulation. • Animal study (rat) with cytokines measured. Von Bethmann et al, Am J Respir Crit Care Med 1998; 157: 263. • Mechanical ventilation may contribute to a systemic inflammatory response. • Repeated stretching (high transpulmonary pressure) may increase cytokine release. Tremblay L, et al AJRCCM, 157, 1997, 944. • Repeated opening and closing (dogs) caused release of bacteria from the alveoli to the blood stream. Effect reduced when PEEP of 10 added. (Nahum et al. , CCM, 25, 1997, 1733. )
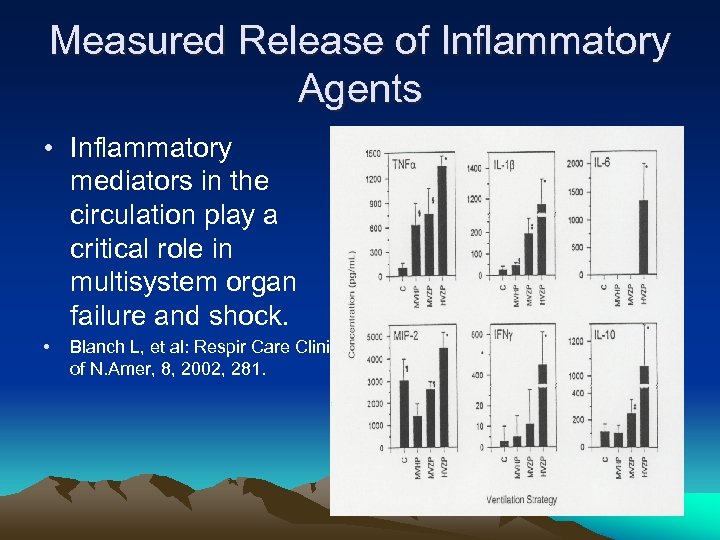 Measured Release of Inflammatory Agents • Inflammatory mediators in the circulation play a critical role in multisystem organ failure and shock. • Blanch L, et al: Respir Care Clinics of N. Amer, 8, 2002, 281.
Measured Release of Inflammatory Agents • Inflammatory mediators in the circulation play a critical role in multisystem organ failure and shock. • Blanch L, et al: Respir Care Clinics of N. Amer, 8, 2002, 281.
 How To Stop the Cytokine Release • Ventilator strategies that promote optimal PEEP to keep open all lung regions can contribute to improved mortality of mechanically ventilated patients. • Potentially, lung recruitment, low tidal volumes and optimal PEEP levels. Blanch L, et al: Respir Care Clinics of N. Amer, 8, 2002, 281.
How To Stop the Cytokine Release • Ventilator strategies that promote optimal PEEP to keep open all lung regions can contribute to improved mortality of mechanically ventilated patients. • Potentially, lung recruitment, low tidal volumes and optimal PEEP levels. Blanch L, et al: Respir Care Clinics of N. Amer, 8, 2002, 281.
 Part 3 • The ARDS net Study • Protecting the Lung
Part 3 • The ARDS net Study • Protecting the Lung
 Landmark ARDS Network Study • Reported May 4, 2000 in NEJM – best evidence of how to set the ventilator. • 861 patients with ARDS/ALI • Randomized to 6 m. L/kg (IBW) or 12 m. L/kg (IBW); A/C Vol; Pplat < 30 cm H 2 O • 25% reduction in mortality with low VT. • Adjusted f to affect p. H goal (7. 30 -7. 45)
Landmark ARDS Network Study • Reported May 4, 2000 in NEJM – best evidence of how to set the ventilator. • 861 patients with ARDS/ALI • Randomized to 6 m. L/kg (IBW) or 12 m. L/kg (IBW); A/C Vol; Pplat < 30 cm H 2 O • 25% reduction in mortality with low VT. • Adjusted f to affect p. H goal (7. 30 -7. 45)
 ARDSnet Study • Patients with 12 ml/kg VT had a better Pa. O 2/FIO 2 ratio; however, • Better clinical numbers (ABG’s etc. ) did not, in this case, lead to a better survival.
ARDSnet Study • Patients with 12 ml/kg VT had a better Pa. O 2/FIO 2 ratio; however, • Better clinical numbers (ABG’s etc. ) did not, in this case, lead to a better survival.
 Open Lung Approach What does it mean? • Prevent repeated opening and closing of alveoli. • Perform a recruitment maneuver. • Maintain high PEEP • Use low distending Pressures • VT < 6 m. L/kg IBW, PC, PIP < 40 cm H 2 O, • Accept Permissive hypercapnia,
Open Lung Approach What does it mean? • Prevent repeated opening and closing of alveoli. • Perform a recruitment maneuver. • Maintain high PEEP • Use low distending Pressures • VT < 6 m. L/kg IBW, PC, PIP < 40 cm H 2 O, • Accept Permissive hypercapnia,
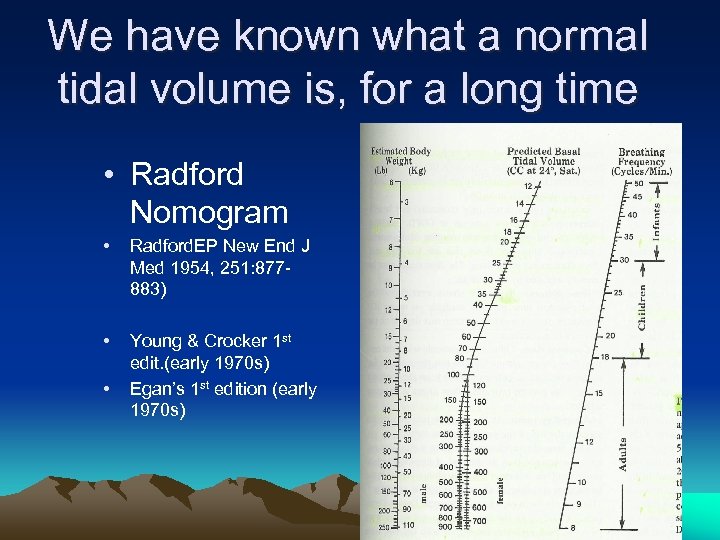 We have known what a normal tidal volume is, for a long time • Radford Nomogram • Radford. EP New End J Med 1954, 251: 877883) • Young & Crocker 1 st edit. (early 1970 s) Egan’s 1 st edition (early 1970 s) •
We have known what a normal tidal volume is, for a long time • Radford Nomogram • Radford. EP New End J Med 1954, 251: 877883) • Young & Crocker 1 st edit. (early 1970 s) Egan’s 1 st edition (early 1970 s) •
 Part 4: Lung Protective Strategies • The importance of PEEP. • Recruiting collapsed alveoli.
Part 4: Lung Protective Strategies • The importance of PEEP. • Recruiting collapsed alveoli.
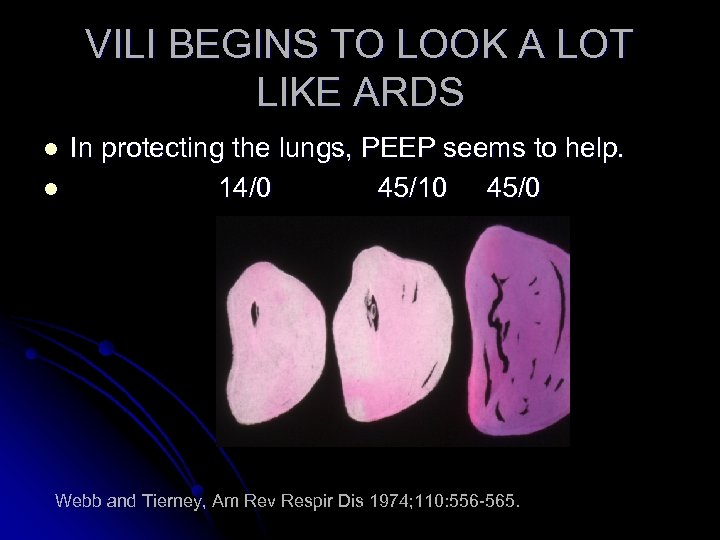 VILI BEGINS TO LOOK A LOT LIKE ARDS l l In protecting the lungs, PEEP seems to help. 14/0 45/10 45/0 Webb and Tierney, Am Rev Respir Dis 1974; 110: 556 -565.
VILI BEGINS TO LOOK A LOT LIKE ARDS l l In protecting the lungs, PEEP seems to help. 14/0 45/10 45/0 Webb and Tierney, Am Rev Respir Dis 1974; 110: 556 -565.
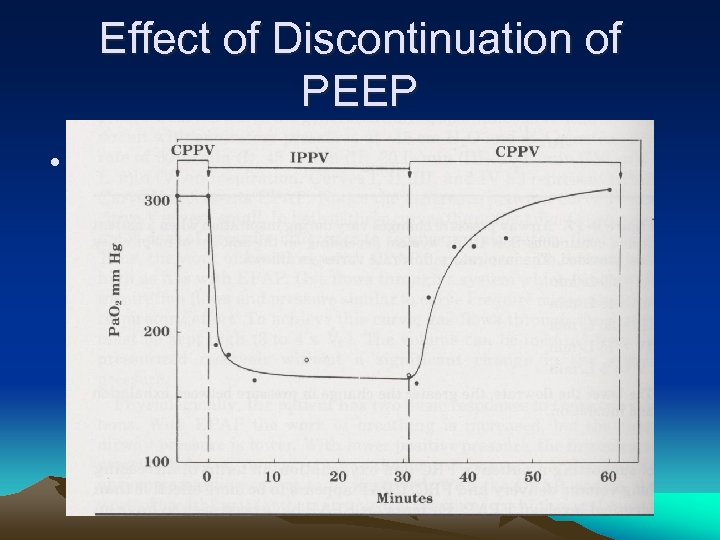 Effect of Discontinuation of PEEP • Kumar et al: NEJM 1970 (283)
Effect of Discontinuation of PEEP • Kumar et al: NEJM 1970 (283)
 Alveolar Stability • In normal lung, alveoli are very stable. • In ARDS, alveoli are unstable. • Some alveoli in ARDS totally collapse on exhalation (type III) and pop open on inspiration. • Repeated Alveolar Collapse and Expansion (RACE)
Alveolar Stability • In normal lung, alveoli are very stable. • In ARDS, alveoli are unstable. • Some alveoli in ARDS totally collapse on exhalation (type III) and pop open on inspiration. • Repeated Alveolar Collapse and Expansion (RACE)
 The Raft Theory • Like balloons in a raft, they inflate. • In normal lungs it is hard to get alveolar overexpansion. • However, if one alveolus collapses, neighbors expand into the void. • Get overinflation and sheer stress of alveoli.
The Raft Theory • Like balloons in a raft, they inflate. • In normal lungs it is hard to get alveolar overexpansion. • However, if one alveolus collapses, neighbors expand into the void. • Get overinflation and sheer stress of alveoli.
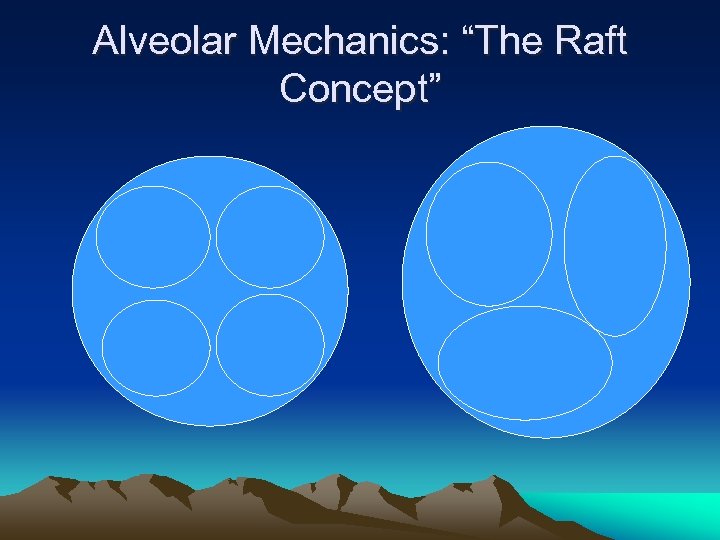 Alveolar Mechanics: “The Raft Concept”
Alveolar Mechanics: “The Raft Concept”
 Part 5 – Lung Recruitment
Part 5 – Lung Recruitment
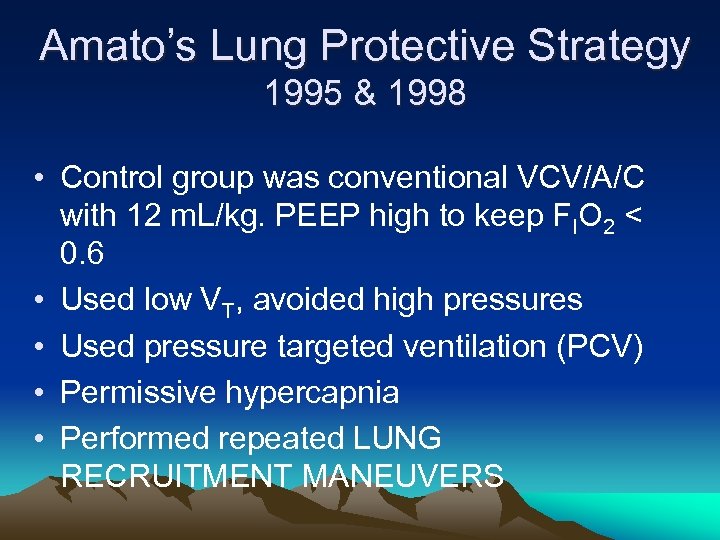 Amato’s Lung Protective Strategy 1995 & 1998 • Control group was conventional VCV/A/C with 12 m. L/kg. PEEP high to keep FIO 2 < 0. 6 • Used low VT, avoided high pressures • Used pressure targeted ventilation (PCV) • Permissive hypercapnia • Performed repeated LUNG RECRUITMENT MANEUVERS
Amato’s Lung Protective Strategy 1995 & 1998 • Control group was conventional VCV/A/C with 12 m. L/kg. PEEP high to keep FIO 2 < 0. 6 • Used low VT, avoided high pressures • Used pressure targeted ventilation (PCV) • Permissive hypercapnia • Performed repeated LUNG RECRUITMENT MANEUVERS
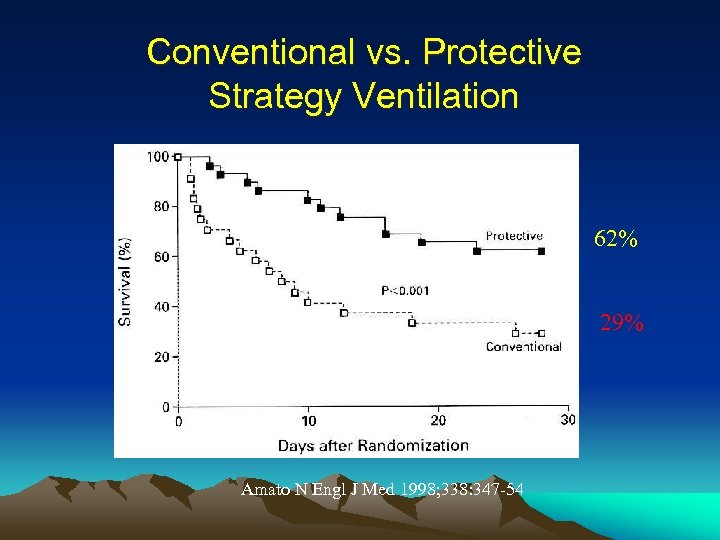 Conventional vs. Protective Strategy Ventilation 62% 29% Amato N Engl J Med 1998; 338: 347 -54
Conventional vs. Protective Strategy Ventilation 62% 29% Amato N Engl J Med 1998; 338: 347 -54
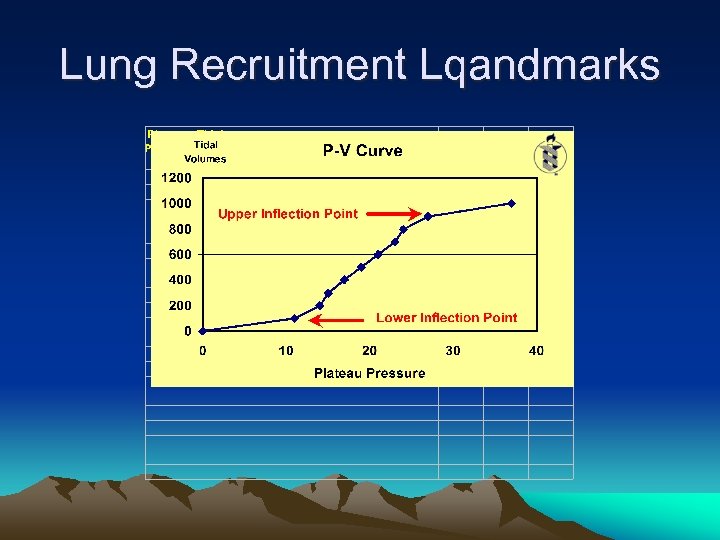 Lung Recruitment Lqandmarks
Lung Recruitment Lqandmarks
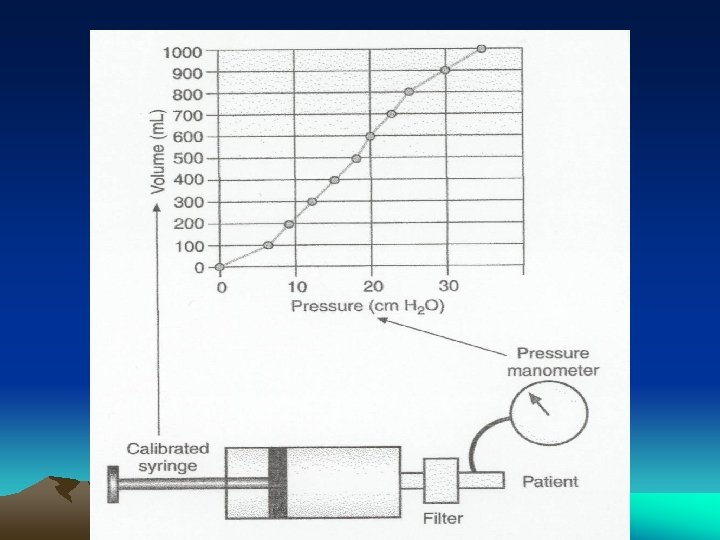
 Evaluating Opening and Closing Pressures to Set PEEP • Use of Pressure/Volume loop – slow progressive addition of volume – Requires sedation and sometimes paralysis – Requires large volume syringe and adaptors – Amato did once per patient in study group to establish high and low inflection points. – PEEP set at 16 cm H 2 O if no Pflex-low obtained.
Evaluating Opening and Closing Pressures to Set PEEP • Use of Pressure/Volume loop – slow progressive addition of volume – Requires sedation and sometimes paralysis – Requires large volume syringe and adaptors – Amato did once per patient in study group to establish high and low inflection points. – PEEP set at 16 cm H 2 O if no Pflex-low obtained.
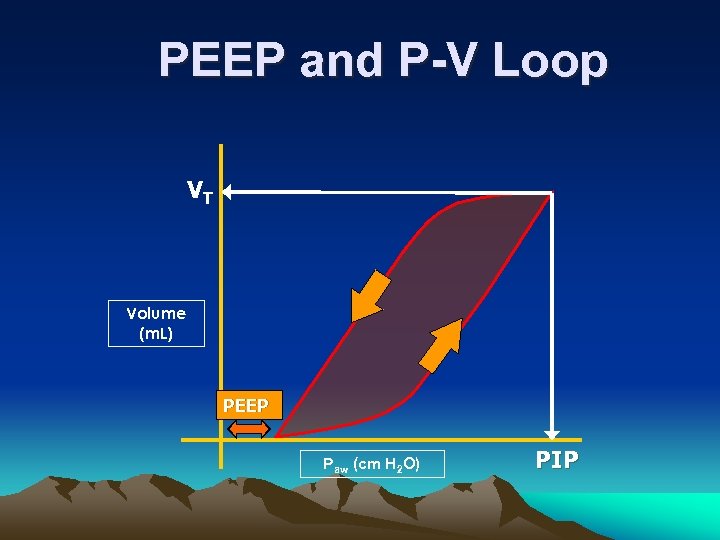 PEEP and P-V Loop VT Volume (m. L) PEEP Paw (cm H 2 O) PIP
PEEP and P-V Loop VT Volume (m. L) PEEP Paw (cm H 2 O) PIP
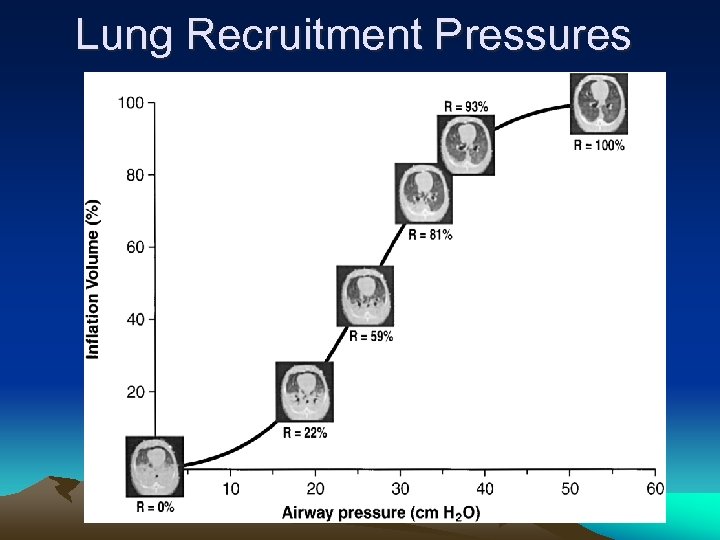 Lung Recruitment Pressures
Lung Recruitment Pressures

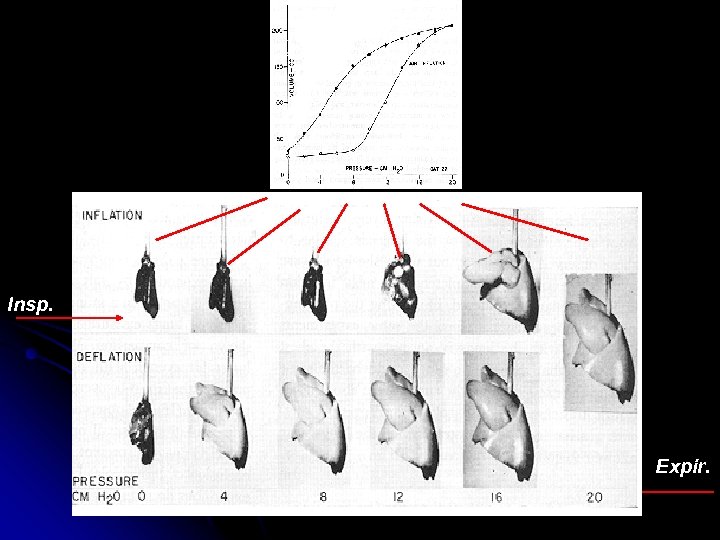 Insp. Expir.
Insp. Expir.
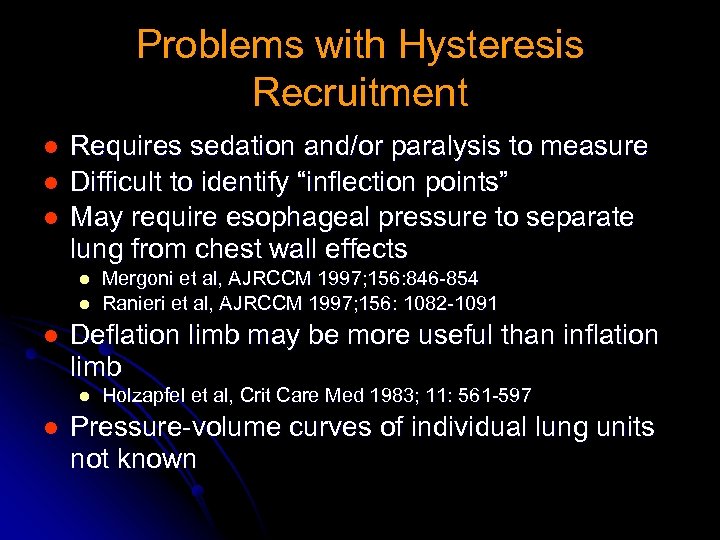 Problems with Hysteresis Recruitment l l l Requires sedation and/or paralysis to measure Difficult to identify “inflection points” May require esophageal pressure to separate lung from chest wall effects l l l Deflation limb may be more useful than inflation limb l l Mergoni et al, AJRCCM 1997; 156: 846 -854 Ranieri et al, AJRCCM 1997; 156: 1082 -1091 Holzapfel et al, Crit Care Med 1983; 11: 561 -597 Pressure-volume curves of individual lung units not known
Problems with Hysteresis Recruitment l l l Requires sedation and/or paralysis to measure Difficult to identify “inflection points” May require esophageal pressure to separate lung from chest wall effects l l l Deflation limb may be more useful than inflation limb l l Mergoni et al, AJRCCM 1997; 156: 846 -854 Ranieri et al, AJRCCM 1997; 156: 1082 -1091 Holzapfel et al, Crit Care Med 1983; 11: 561 -597 Pressure-volume curves of individual lung units not known
 Patient Selection Pulmonary vs. Extra-Pulmonary ARDS: Gattinoni, Am J Respir Crit Care Med 1998; 158: 3 -11 l Pulmonary ARDS (ARDSP) l Largely consolidation l Little atelectasis l l i. e. pneumonia, aspiration, diffuse pulmonary infection, neardrowning, toxic inhalation, lung contusion, etc Extra-pulmonary ARDS (ARDSEX) l Predominately l atelectasis i. e. sepsis, nonthoracic trauma, pancreatitis, transfusion related injury, etc.
Patient Selection Pulmonary vs. Extra-Pulmonary ARDS: Gattinoni, Am J Respir Crit Care Med 1998; 158: 3 -11 l Pulmonary ARDS (ARDSP) l Largely consolidation l Little atelectasis l l i. e. pneumonia, aspiration, diffuse pulmonary infection, neardrowning, toxic inhalation, lung contusion, etc Extra-pulmonary ARDS (ARDSEX) l Predominately l atelectasis i. e. sepsis, nonthoracic trauma, pancreatitis, transfusion related injury, etc.
 Part 6: Lung Recruitment Maneuvers l l Amato et al performed a recruitment maneuver whenever ventilation was discontinued in the study group. Amato used CPAP of 35 -40 cm H 2 O for 40 seconds.
Part 6: Lung Recruitment Maneuvers l l Amato et al performed a recruitment maneuver whenever ventilation was discontinued in the study group. Amato used CPAP of 35 -40 cm H 2 O for 40 seconds.
 Once Recruited • Requires high PEEP (16 cm H 2 O, Amato; or PEEP plus auto-PEEP) to keep lungs open. • PEEP does not recruit! • Lapinsky et al used 35 -40 m H 2 O for 20 sec. Found that multiple RM might be required. . Lapinsky SE, et al Int. Care Med, 1999: 25, 1297. • Another group used 35 cm H 2 O for 90 sec RM lasted up to 60 min. and no injury observed in ARDS patients. • PEEP prevents alveolar collapse (derecruitment) – Lim CM, Jung H, Koh Y; Crit Care Med, 2001 31: 411 -418.
Once Recruited • Requires high PEEP (16 cm H 2 O, Amato; or PEEP plus auto-PEEP) to keep lungs open. • PEEP does not recruit! • Lapinsky et al used 35 -40 m H 2 O for 20 sec. Found that multiple RM might be required. . Lapinsky SE, et al Int. Care Med, 1999: 25, 1297. • Another group used 35 cm H 2 O for 90 sec RM lasted up to 60 min. and no injury observed in ARDS patients. • PEEP prevents alveolar collapse (derecruitment) – Lim CM, Jung H, Koh Y; Crit Care Med, 2001 31: 411 -418.
 Complications and Implications • Recruitment maneuvers shown to produce small pneumothorax and subcutaneous emphysema in one case. • Does not benefit unilateral lung conditions. • May not benefit primary ARDS such as in pneumonia. • Should not be used in a patient with bullous lung disease or known blebs.
Complications and Implications • Recruitment maneuvers shown to produce small pneumothorax and subcutaneous emphysema in one case. • Does not benefit unilateral lung conditions. • May not benefit primary ARDS such as in pneumonia. • Should not be used in a patient with bullous lung disease or known blebs.
 Evaluating Opening and Closing Pressures • Use of tracking software • Effective in recruiting alveoli in patients with ARDS and improving oxygenation. • Procedure simulates a slow P-V loop to determine over distention and lower inflection point determination. • Papadakos PJ, Lachmann B: Mount Sinai J Med, Jan/March, 2002, 73 -77
Evaluating Opening and Closing Pressures • Use of tracking software • Effective in recruiting alveoli in patients with ARDS and improving oxygenation. • Procedure simulates a slow P-V loop to determine over distention and lower inflection point determination. • Papadakos PJ, Lachmann B: Mount Sinai J Med, Jan/March, 2002, 73 -77
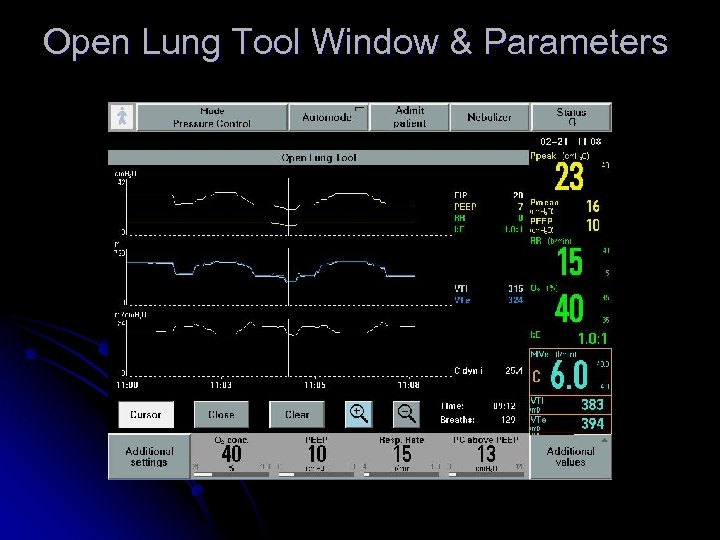 Open Lung Tool Window & Parameters
Open Lung Tool Window & Parameters
 Pig Lung Model
Pig Lung Model
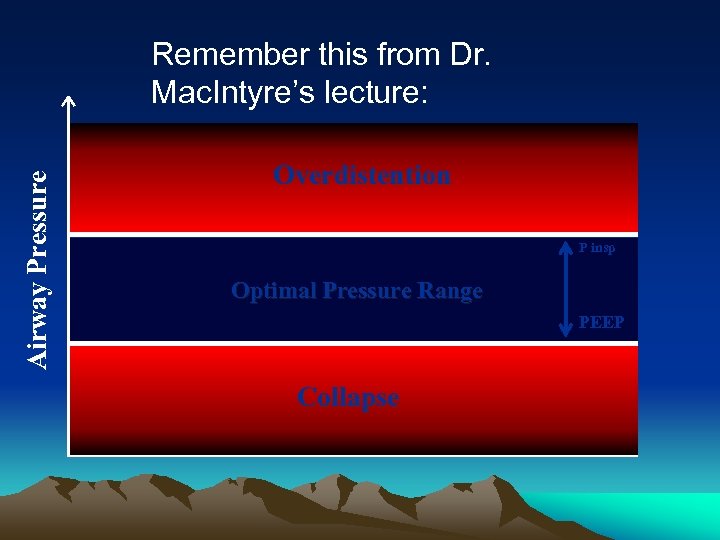 Airway Pressure Remember this from Dr. Mac. Intyre’s lecture: Overdistention P insp Optimal Pressure Range PEEP Collapse
Airway Pressure Remember this from Dr. Mac. Intyre’s lecture: Overdistention P insp Optimal Pressure Range PEEP Collapse
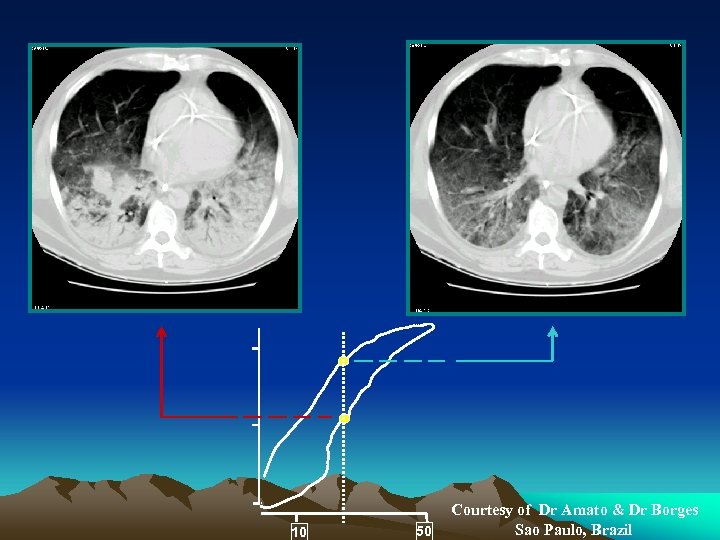 10 50 Courtesy of Dr Amato & Dr Borges Sao Paulo, Brazil
10 50 Courtesy of Dr Amato & Dr Borges Sao Paulo, Brazil
 Summarizing the Problem … Atelectasis is bad. Over inflation is bad. Alveolar collapse on exhalation is bad. The ARDS lung is not uniform. High PEEP is scary. Auto-PEEP is evil.
Summarizing the Problem … Atelectasis is bad. Over inflation is bad. Alveolar collapse on exhalation is bad. The ARDS lung is not uniform. High PEEP is scary. Auto-PEEP is evil.
 So What Are The Best Strategies For Lung Protection in ARDS? • Use low Vt < 6 m. L/Kg IBW • Keep plateau pressures low (< 30 cm H 2 O); but, maybe higher if chest wall is rigid or abdomen is rigid. • Recruit the lung and keep it open. • Keep the PEEP high (16 -20 or at low Pflex point on expiratory curve) • Monitor carefully.
So What Are The Best Strategies For Lung Protection in ARDS? • Use low Vt < 6 m. L/Kg IBW • Keep plateau pressures low (< 30 cm H 2 O); but, maybe higher if chest wall is rigid or abdomen is rigid. • Recruit the lung and keep it open. • Keep the PEEP high (16 -20 or at low Pflex point on expiratory curve) • Monitor carefully.
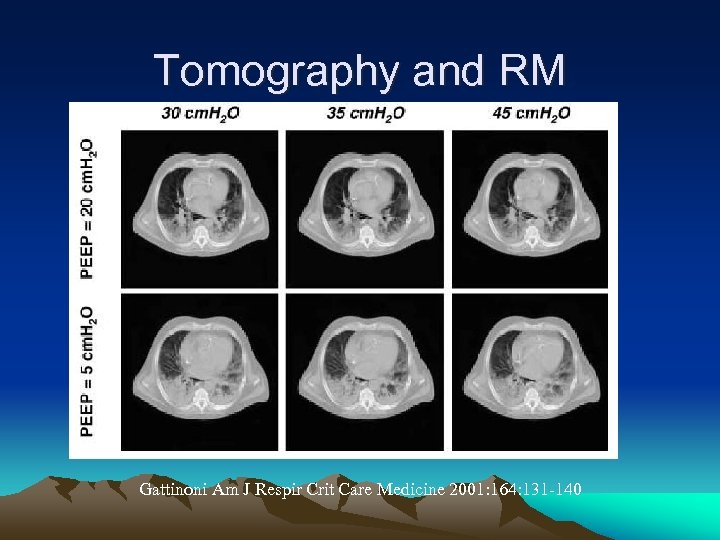 Tomography and RM Gattinoni Am J Respir Crit Care Medicine 2001: 164: 131 -140
Tomography and RM Gattinoni Am J Respir Crit Care Medicine 2001: 164: 131 -140
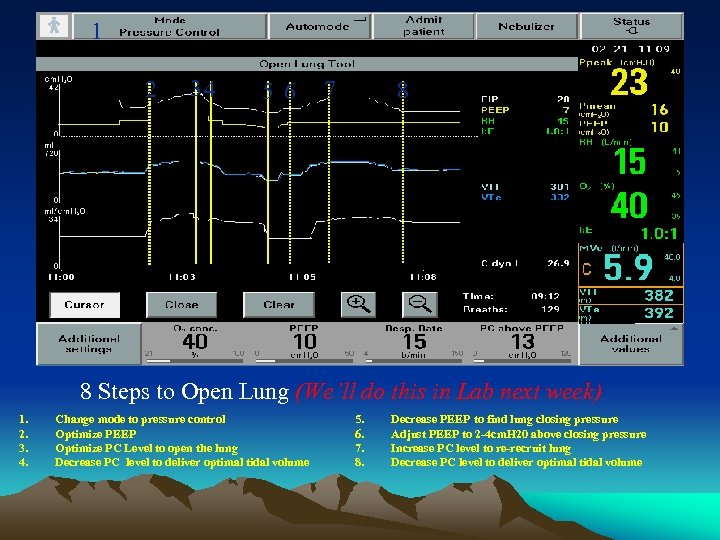 1 2 34 5 6 7 8 8 Steps to Open Lung (We’ll do this in Lab next week) 1. 2. 3. 4. Change mode to pressure control Optimize PEEP Optimize PC Level to open the lung Decrease PC level to deliver optimal tidal volume 5. 6. 7. 8. Decrease PEEP to find lung closing pressure Adjust PEEP to 2 -4 cm. H 20 above closing pressure Increase PC level to re-recruit lung Decrease PC level to deliver optimal tidal volume
1 2 34 5 6 7 8 8 Steps to Open Lung (We’ll do this in Lab next week) 1. 2. 3. 4. Change mode to pressure control Optimize PEEP Optimize PC Level to open the lung Decrease PC level to deliver optimal tidal volume 5. 6. 7. 8. Decrease PEEP to find lung closing pressure Adjust PEEP to 2 -4 cm. H 20 above closing pressure Increase PC level to re-recruit lung Decrease PC level to deliver optimal tidal volume
 Work Done by Tusma, Bohm et al • Study of patients under general anesthesia. • Purpose to open atelectatic lungs. • Study group had PEEP = 15 cm H 2 O applied (increments of 5) • At PEEP = 15 cm H 2 O, VT increased in steps to a maximum of 18 m. L/kg. Study group had better oxygenation than no PEEP or PEEP only with no recruitment. • Tusma G, Bohm SH, Vazquez de Anda GF, et al: ‘Alveolar recruitment strategy improves arterial oxygenation during general anaesthesia. Brit. J Anaesth 1999; 82: 8 -13
Work Done by Tusma, Bohm et al • Study of patients under general anesthesia. • Purpose to open atelectatic lungs. • Study group had PEEP = 15 cm H 2 O applied (increments of 5) • At PEEP = 15 cm H 2 O, VT increased in steps to a maximum of 18 m. L/kg. Study group had better oxygenation than no PEEP or PEEP only with no recruitment. • Tusma G, Bohm SH, Vazquez de Anda GF, et al: ‘Alveolar recruitment strategy improves arterial oxygenation during general anaesthesia. Brit. J Anaesth 1999; 82: 8 -13
 Post Operative Atelectasis – Revisited Again • A study showed reduced shunting, increased oxygenation in postsurgical patients when deep breaths (about 30 seconds) given periodically. • Attributed to reduced atelectasis. • Bendixen H et al: NEJM, 69, 1963, 991.
Post Operative Atelectasis – Revisited Again • A study showed reduced shunting, increased oxygenation in postsurgical patients when deep breaths (about 30 seconds) given periodically. • Attributed to reduced atelectasis. • Bendixen H et al: NEJM, 69, 1963, 991.
 Study from ARDS Network • Crit Care Med 2003 31(11), 2592 -2597 • Sp. O 2 improved after lung recruitment maneuver (35 cm H 2 O CPAP progressively increase 5 -10 sec sustained for 30 seconds. ) • LRM the most likely cause of improvement in venous admixture and oxygenation.
Study from ARDS Network • Crit Care Med 2003 31(11), 2592 -2597 • Sp. O 2 improved after lung recruitment maneuver (35 cm H 2 O CPAP progressively increase 5 -10 sec sustained for 30 seconds. ) • LRM the most likely cause of improvement in venous admixture and oxygenation.
 Procedure in Open Lung Recruitment- Lachman, et al 1. Initially, set to pressure control to 20 PEEP = 15 (range 10 - 20 cm H 2 O), I: E = 1: 1 (range 1: 2 -2: 1), rate = 10 - 15 2. Slowly increase PC (above PEEP) to a minimum of 40 cm H 2 O (PIP 55 cm H 2 O) over a minimum of 10 breaths (range 1030 breaths/min). 3. Monitor for CV side effects, breath sounds, and ventilator parameters, especially dynamic compliance.
Procedure in Open Lung Recruitment- Lachman, et al 1. Initially, set to pressure control to 20 PEEP = 15 (range 10 - 20 cm H 2 O), I: E = 1: 1 (range 1: 2 -2: 1), rate = 10 - 15 2. Slowly increase PC (above PEEP) to a minimum of 40 cm H 2 O (PIP 55 cm H 2 O) over a minimum of 10 breaths (range 1030 breaths/min). 3. Monitor for CV side effects, breath sounds, and ventilator parameters, especially dynamic compliance.
 Procedure in Open Lung Recruitment (cont. ) 4. If stable, when dynamic compliance decrease, note airway pressures. 5. Begin to reduce PC levels until desired VT delivery achieved, e. g. VT 6 m. L/kg (IBW). 6. Decrease PEEP levels until lungs derecruit (Cdyn will again decrease). 7. Note pressure of de-recruitment. 8. Recruit lungs again then ventilate between upper and lower pressure points.
Procedure in Open Lung Recruitment (cont. ) 4. If stable, when dynamic compliance decrease, note airway pressures. 5. Begin to reduce PC levels until desired VT delivery achieved, e. g. VT 6 m. L/kg (IBW). 6. Decrease PEEP levels until lungs derecruit (Cdyn will again decrease). 7. Note pressure of de-recruitment. 8. Recruit lungs again then ventilate between upper and lower pressure points.
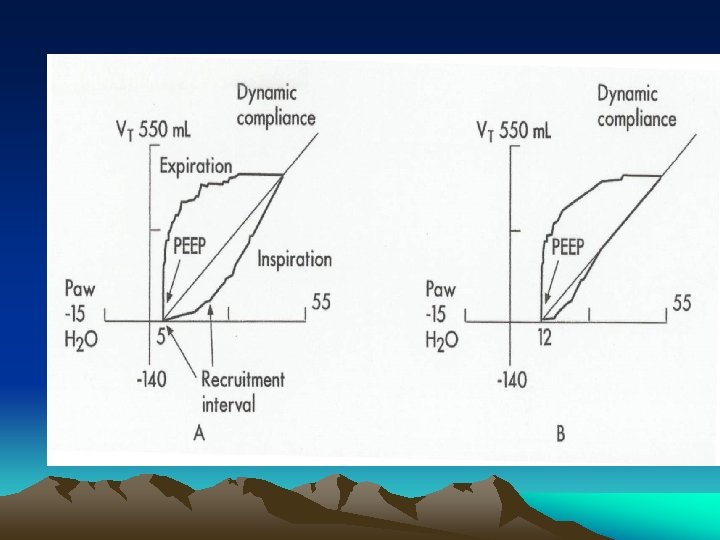
 General Approach to Open Lung Technique • Recruit the lung by applying a plateau pressure that can inflate the lung to TLC. • Provide the recruitment pressure for an adequate period of time. • Maintain the lung by not allowing the lung to derecruit on exhalation. • Coming down to the maintenance PEEP level achieves higher lung volumes than titrating up to the maintenance PEEP level.
General Approach to Open Lung Technique • Recruit the lung by applying a plateau pressure that can inflate the lung to TLC. • Provide the recruitment pressure for an adequate period of time. • Maintain the lung by not allowing the lung to derecruit on exhalation. • Coming down to the maintenance PEEP level achieves higher lung volumes than titrating up to the maintenance PEEP level.
 Apneic Lung Recruitment Technique A “Conservative” Approach? • • Sedation ? Pre-oxygenation. CPAP of 30 cm H 2 O for 30 - 40 seconds. Monitor Vt and oxygenation for 15 - 30 min. • If unresponsive, repeat at CPAP of 35 to 40 cm H 2 O.
Apneic Lung Recruitment Technique A “Conservative” Approach? • • Sedation ? Pre-oxygenation. CPAP of 30 cm H 2 O for 30 - 40 seconds. Monitor Vt and oxygenation for 15 - 30 min. • If unresponsive, repeat at CPAP of 35 to 40 cm H 2 O.
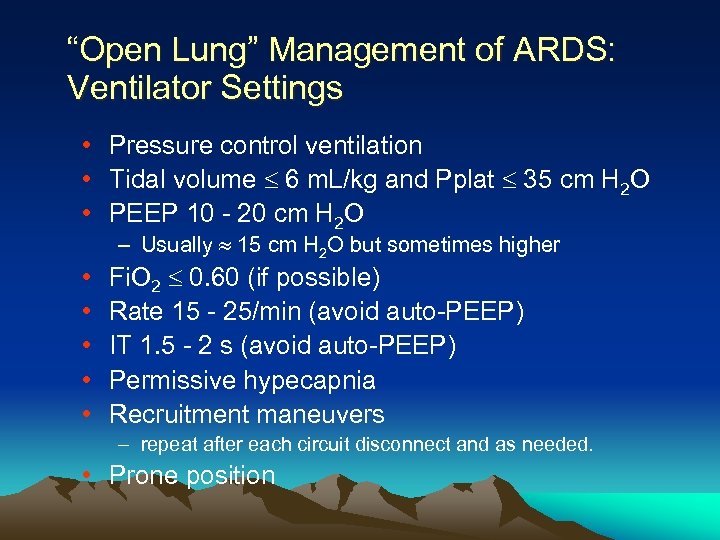 “Open Lung” Management of ARDS: Ventilator Settings • Pressure control ventilation • Tidal volume 6 m. L/kg and Pplat 35 cm H 2 O • PEEP 10 - 20 cm H 2 O – Usually 15 cm H 2 O but sometimes higher • • • Fi. O 2 0. 60 (if possible) Rate 15 - 25/min (avoid auto-PEEP) IT 1. 5 - 2 s (avoid auto-PEEP) Permissive hypecapnia Recruitment maneuvers – repeat after each circuit disconnect and as needed. • Prone position
“Open Lung” Management of ARDS: Ventilator Settings • Pressure control ventilation • Tidal volume 6 m. L/kg and Pplat 35 cm H 2 O • PEEP 10 - 20 cm H 2 O – Usually 15 cm H 2 O but sometimes higher • • • Fi. O 2 0. 60 (if possible) Rate 15 - 25/min (avoid auto-PEEP) IT 1. 5 - 2 s (avoid auto-PEEP) Permissive hypecapnia Recruitment maneuvers – repeat after each circuit disconnect and as needed. • Prone position
 Approaches to Maintain the Recruited Lung Volume • Adequate PEEP • Prone positioning • Sighs
Approaches to Maintain the Recruited Lung Volume • Adequate PEEP • Prone positioning • Sighs
 Other Options used today are APRV and Proning… Has always worked for Bears
Other Options used today are APRV and Proning… Has always worked for Bears
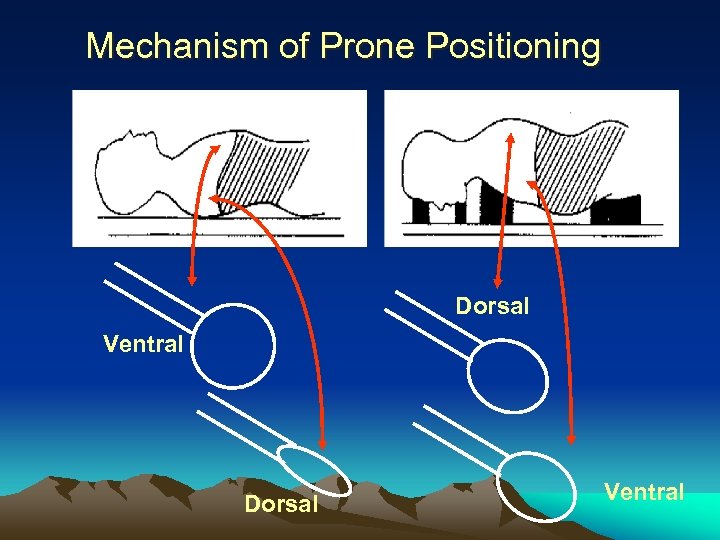 Mechanism of Prone Positioning Dorsal Ventral
Mechanism of Prone Positioning Dorsal Ventral
 PRONE POSITION in ARDS Proposed Explanations • Increased FRC • Blood Flow Redistribution • Changes in Diaphragmatic Motion • Improved Secretion Removal
PRONE POSITION in ARDS Proposed Explanations • Increased FRC • Blood Flow Redistribution • Changes in Diaphragmatic Motion • Improved Secretion Removal
 Prone Positioning: Procedure • Appropriate staff to manage patient and “tubes”. – 2 - 3 for Airway, IV’s, chest tubes, etc. – 2 - 3 for pt. • Minimize abdominal pressure. – Support hips/chest with pillows or deflate abdominal portion of “air bed”. • Maintain pt in Swimming position (one arm extended over head, head turned to that side) – Alternate head/arm Q 2 o hrs. . • Sedation generally required.
Prone Positioning: Procedure • Appropriate staff to manage patient and “tubes”. – 2 - 3 for Airway, IV’s, chest tubes, etc. – 2 - 3 for pt. • Minimize abdominal pressure. – Support hips/chest with pillows or deflate abdominal portion of “air bed”. • Maintain pt in Swimming position (one arm extended over head, head turned to that side) – Alternate head/arm Q 2 o hrs. . • Sedation generally required.
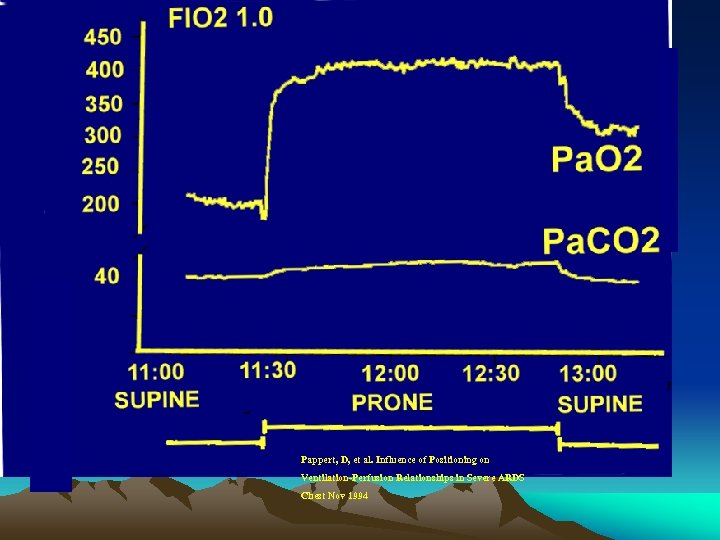 Pappert, D, et al. Influence of Positioning on Ventilation-Perfusion Relationships in Severe ARDS Chest Nov 1994
Pappert, D, et al. Influence of Positioning on Ventilation-Perfusion Relationships in Severe ARDS Chest Nov 1994
 Why is Proning a Good Idea? • Advantages – Limited Technology – Reduction of Pulmonary Compression – V/Q matching – Relief to LL compression • Disadvantages – A Regional Approach – Staff Coordination and Cooperation
Why is Proning a Good Idea? • Advantages – Limited Technology – Reduction of Pulmonary Compression – V/Q matching – Relief to LL compression • Disadvantages – A Regional Approach – Staff Coordination and Cooperation
 The Use of Sighs to Maintain the Open Lung Pelosi, et al. A, J Respir Crit Care Med 1999; 159: 872 -880. • 3/hr. at a Vt which produces a Pplat of 45 cm H 2 O. • May open units with opening pressures > than 35 cm H 2 O. • May resolve absorption atelectasis in poorly ventilated units.
The Use of Sighs to Maintain the Open Lung Pelosi, et al. A, J Respir Crit Care Med 1999; 159: 872 -880. • 3/hr. at a Vt which produces a Pplat of 45 cm H 2 O. • May open units with opening pressures > than 35 cm H 2 O. • May resolve absorption atelectasis in poorly ventilated units.
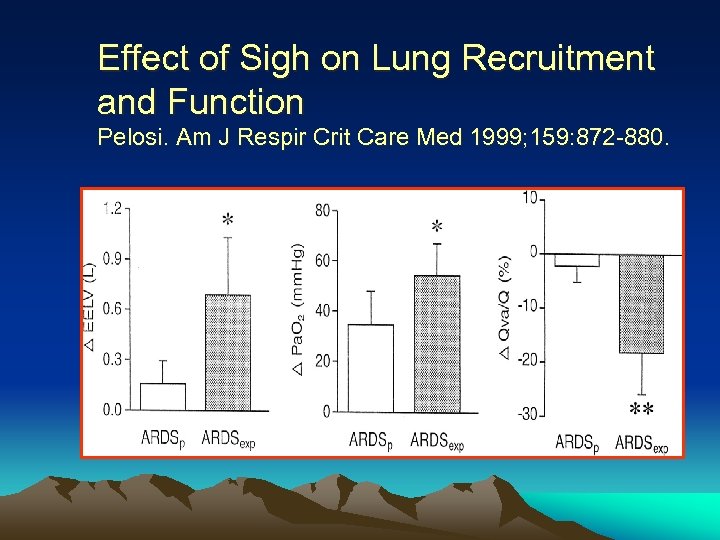 Effect of Sigh on Lung Recruitment and Function Pelosi. Am J Respir Crit Care Med 1999; 159: 872 -880.
Effect of Sigh on Lung Recruitment and Function Pelosi. Am J Respir Crit Care Med 1999; 159: 872 -880.
 Open Lung Ventilation Summary • Treatment of atelectasis, derecruitment and preventing over-distension in ARDS require careful planning. • Best RM techniques may vary for different patients. • Maintenance PEEP is difficult to determine in advance. • Low VT is widely accepted for lung protection:
Open Lung Ventilation Summary • Treatment of atelectasis, derecruitment and preventing over-distension in ARDS require careful planning. • Best RM techniques may vary for different patients. • Maintenance PEEP is difficult to determine in advance. • Low VT is widely accepted for lung protection:


