56b2a2593f94b25d011b9a40086b0a1a.ppt
- Количество слайдов: 37
 One Size Doesn't Fit All: Developing a Model for Integrating Sexual and Reproductive Health and HIV Services in e. Thekwini District, Kwa. Zulu-Natal, South Africa Jenni Smit RHRU, University of the Witwatersrand Columbia U New York Feb 25, 2010
One Size Doesn't Fit All: Developing a Model for Integrating Sexual and Reproductive Health and HIV Services in e. Thekwini District, Kwa. Zulu-Natal, South Africa Jenni Smit RHRU, University of the Witwatersrand Columbia U New York Feb 25, 2010
 Background • The importance of integrating sexual and reproductive health (SRH) and HIV services is widely acknowledged • Growing recognition of the importance of contraception for HIV/AIDS prevention efforts • In particular, repeated calls to strengthen the link between FP and PMTCT • Integration of SRH and HIV services is especially relevant in South Africa: – the highest number of people living with HIV in the world (5. 2 mil) – high contraceptive prevalence, but high unplanned pregnancies and teenage pregnancies 2
Background • The importance of integrating sexual and reproductive health (SRH) and HIV services is widely acknowledged • Growing recognition of the importance of contraception for HIV/AIDS prevention efforts • In particular, repeated calls to strengthen the link between FP and PMTCT • Integration of SRH and HIV services is especially relevant in South Africa: – the highest number of people living with HIV in the world (5. 2 mil) – high contraceptive prevalence, but high unplanned pregnancies and teenage pregnancies 2
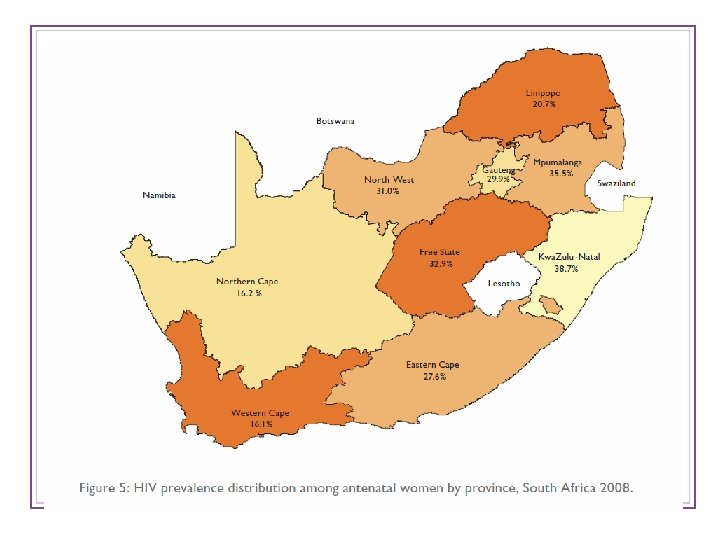 3
3
 HIV Prevalence HSRC community-based survey 2008 Overall prevalence (2+ years): 10. 9% (5. 2 million) • Females 20 -24 years: 21. 1% (males 5. 1%) • Females 25 -29 years: 32. 7% (males 15. 7%) • Prevalence peaks in males in 30 -34 year range: 25. 8% (females 29. 1%) KZN Province highest rates: 15. 8% Condom use at last sex: 64. 8% (67. 4% among males; 62. 5% among females; among youth 15 -24 years: 87. 4% males, 73. 1% females) 4
HIV Prevalence HSRC community-based survey 2008 Overall prevalence (2+ years): 10. 9% (5. 2 million) • Females 20 -24 years: 21. 1% (males 5. 1%) • Females 25 -29 years: 32. 7% (males 15. 7%) • Prevalence peaks in males in 30 -34 year range: 25. 8% (females 29. 1%) KZN Province highest rates: 15. 8% Condom use at last sex: 64. 8% (67. 4% among males; 62. 5% among females; among youth 15 -24 years: 87. 4% males, 73. 1% females) 4
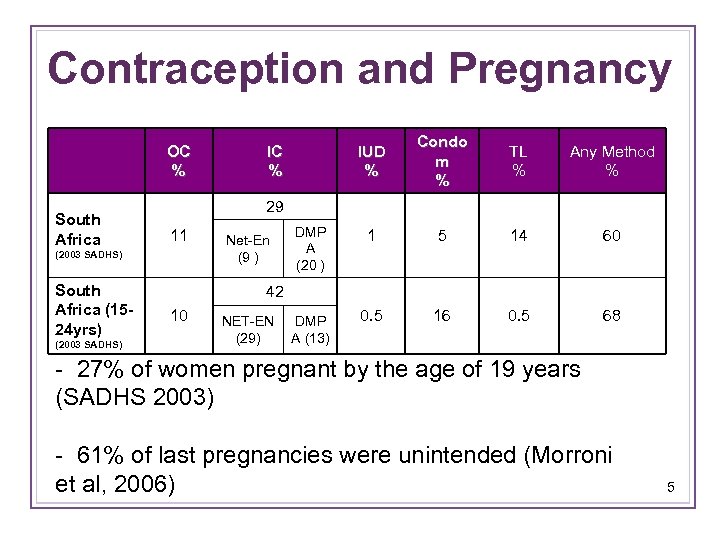 Contraception and Pregnancy OC % South Africa (2003 SADHS) Condo m % TL % Any Method % DMP A (20 ) 1 5 14 60 NET-EN DMP (29) A (13) 0. 5 16 0. 5 68 29 11 (2003 SADHS) South Africa (1524 yrs) IUD % IC % Net-En (9 ) 42 10 - 27% of women pregnant by the age of 19 years (SADHS 2003) - 61% of last pregnancies were unintended (Morroni et al, 2006) 5
Contraception and Pregnancy OC % South Africa (2003 SADHS) Condo m % TL % Any Method % DMP A (20 ) 1 5 14 60 NET-EN DMP (29) A (13) 0. 5 16 0. 5 68 29 11 (2003 SADHS) South Africa (1524 yrs) IUD % IC % Net-En (9 ) 42 10 - 27% of women pregnant by the age of 19 years (SADHS 2003) - 61% of last pregnancies were unintended (Morroni et al, 2006) 5
 Background, cont’d • The primary health care approach (PHC) to service delivery was adopted in South Africa in 1994 • A district health system was put in place with primary care clinics and referral systems to secondary and tertiary care where appropriate • At PHC level, SRH services should be comprehensive, but in reality are limited • Recently, decentralized care has begun for referral of stabilized HIV-infected (on ART), from hospitals to PHC sites 6
Background, cont’d • The primary health care approach (PHC) to service delivery was adopted in South Africa in 1994 • A district health system was put in place with primary care clinics and referral systems to secondary and tertiary care where appropriate • At PHC level, SRH services should be comprehensive, but in reality are limited • Recently, decentralized care has begun for referral of stabilized HIV-infected (on ART), from hospitals to PHC sites 6
 Background, cont’d • Health services in South Africa have recently demonstrated: – HIV positive women wish to have babies and need to be supported in this – A number of HIV positive women are entering PMTCT for the 2 nd/greater time, and reporting unplanned pregnancies – Policy makers, managers and providers are requesting training on contraception and HIV and the interaction of the two – The rapidly growing, strongly vertical ARV programme has led to a narrow focus on HIV treatment, creating a strain on other client demands/needs • There is a call to develop and implement policies and programmes to address broad SRH needs of clients. 7
Background, cont’d • Health services in South Africa have recently demonstrated: – HIV positive women wish to have babies and need to be supported in this – A number of HIV positive women are entering PMTCT for the 2 nd/greater time, and reporting unplanned pregnancies – Policy makers, managers and providers are requesting training on contraception and HIV and the interaction of the two – The rapidly growing, strongly vertical ARV programme has led to a narrow focus on HIV treatment, creating a strain on other client demands/needs • There is a call to develop and implement policies and programmes to address broad SRH needs of clients. 7
 President Zuma’s Declaration To be implemented in KZN on 1 April 2010 • All HIV + children < 1 yr to commence on HAART • All HIV + pregnant woman with CD 4 ≤ 350 to commence HAART • All HIV + pregnant woman with CD 4 > 350 to commence Dual (AZT) therapy from 14 weeks gestation, HIV exposed babies will be given NVP for up to 12 months if the mum got dual therapy • All TB/HIV co-infected pts with CD 4≤ 350 to commence HAART • All facilities to have TB/HIV services under one roof (TB at HIV and HIV at TB) • Male Medical Circumcision services to be commenced • All above services to be available at or through all facilities • Infant & Young Child feeding: the plan (but not yet policy) is to stop formula feeding i. e. no more formula [KZN Dept of Health to host a SRH Dialogue with a focus on FP in March, to develop strategies to address low FP uptake in KZN] 8
President Zuma’s Declaration To be implemented in KZN on 1 April 2010 • All HIV + children < 1 yr to commence on HAART • All HIV + pregnant woman with CD 4 ≤ 350 to commence HAART • All HIV + pregnant woman with CD 4 > 350 to commence Dual (AZT) therapy from 14 weeks gestation, HIV exposed babies will be given NVP for up to 12 months if the mum got dual therapy • All TB/HIV co-infected pts with CD 4≤ 350 to commence HAART • All facilities to have TB/HIV services under one roof (TB at HIV and HIV at TB) • Male Medical Circumcision services to be commenced • All above services to be available at or through all facilities • Infant & Young Child feeding: the plan (but not yet policy) is to stop formula feeding i. e. no more formula [KZN Dept of Health to host a SRH Dialogue with a focus on FP in March, to develop strategies to address low FP uptake in KZN] 8
 Study Aims and Objectives To Develop and evaluate a district based model for integrating SRH and HIV services in SA 1. Conduct formative research: KI interviews; baseline assessment at clinic level 2. Develop, implement and evaluate a model of integrated RH services at all levels of health care delivery 3. Develop community advisory structures to support implementation and sustainability of the RH integration model 4. Develop guidelines, tools and methods for an integrated RH service delivery model 5. Formulate policy at district, provincial and national levels based on lessons learned from the project. 9
Study Aims and Objectives To Develop and evaluate a district based model for integrating SRH and HIV services in SA 1. Conduct formative research: KI interviews; baseline assessment at clinic level 2. Develop, implement and evaluate a model of integrated RH services at all levels of health care delivery 3. Develop community advisory structures to support implementation and sustainability of the RH integration model 4. Develop guidelines, tools and methods for an integrated RH service delivery model 5. Formulate policy at district, provincial and national levels based on lessons learned from the project. 9
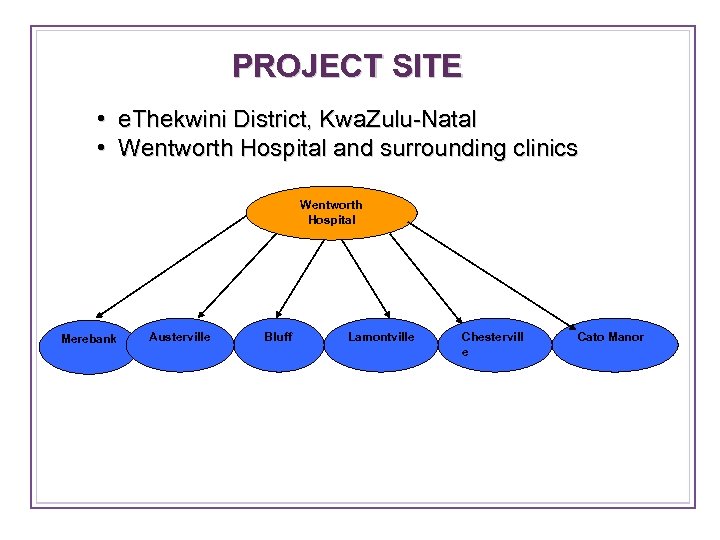 PROJECT SITE • e. Thekwini District, Kwa. Zulu-Natal • Wentworth Hospital and surrounding clinics Wentworth Hospital Merebank Austerville Bluff Lamontville Chestervill e Cato Manor
PROJECT SITE • e. Thekwini District, Kwa. Zulu-Natal • Wentworth Hospital and surrounding clinics Wentworth Hospital Merebank Austerville Bluff Lamontville Chestervill e Cato Manor
 11
11
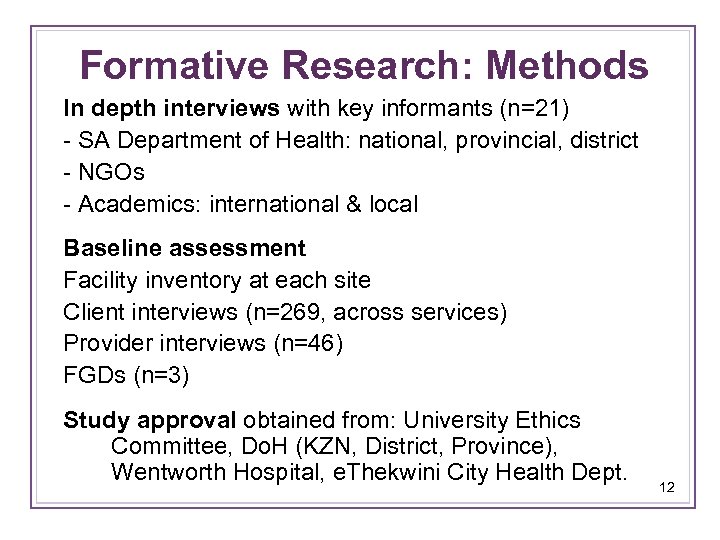 Formative Research: Methods In depth interviews with key informants (n=21) - SA Department of Health: national, provincial, district - NGOs - Academics: international & local Baseline assessment Facility inventory at each site Client interviews (n=269, across services) Provider interviews (n=46) FGDs (n=3) Study approval obtained from: University Ethics Committee, Do. H (KZN, District, Province), Wentworth Hospital, e. Thekwini City Health Dept. 12
Formative Research: Methods In depth interviews with key informants (n=21) - SA Department of Health: national, provincial, district - NGOs - Academics: international & local Baseline assessment Facility inventory at each site Client interviews (n=269, across services) Provider interviews (n=46) FGDs (n=3) Study approval obtained from: University Ethics Committee, Do. H (KZN, District, Province), Wentworth Hospital, e. Thekwini City Health Dept. 12
 Results: Key Informant Interviews
Results: Key Informant Interviews
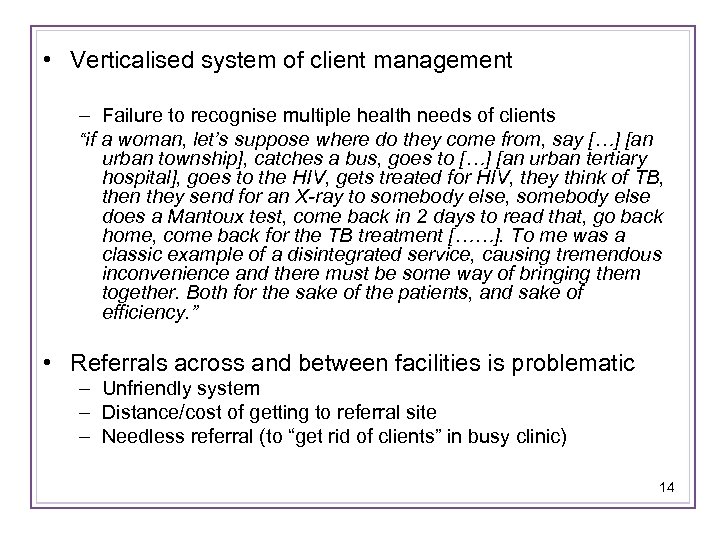 • Verticalised system of client management – Failure to recognise multiple health needs of clients “if a woman, let’s suppose where do they come from, say […] [an urban township], catches a bus, goes to […] [an urban tertiary hospital], goes to the HIV, gets treated for HIV, they think of TB, then they send for an X-ray to somebody else, somebody else does a Mantoux test, come back in 2 days to read that, go back home, come back for the TB treatment [……]. To me was a classic example of a disintegrated service, causing tremendous inconvenience and there must be some way of bringing them together. Both for the sake of the patients, and sake of efficiency. ” • Referrals across and between facilities is problematic – Unfriendly system – Distance/cost of getting to referral site – Needless referral (to “get rid of clients” in busy clinic) 14
• Verticalised system of client management – Failure to recognise multiple health needs of clients “if a woman, let’s suppose where do they come from, say […] [an urban township], catches a bus, goes to […] [an urban tertiary hospital], goes to the HIV, gets treated for HIV, they think of TB, then they send for an X-ray to somebody else, somebody else does a Mantoux test, come back in 2 days to read that, go back home, come back for the TB treatment [……]. To me was a classic example of a disintegrated service, causing tremendous inconvenience and there must be some way of bringing them together. Both for the sake of the patients, and sake of efficiency. ” • Referrals across and between facilities is problematic – Unfriendly system – Distance/cost of getting to referral site – Needless referral (to “get rid of clients” in busy clinic) 14
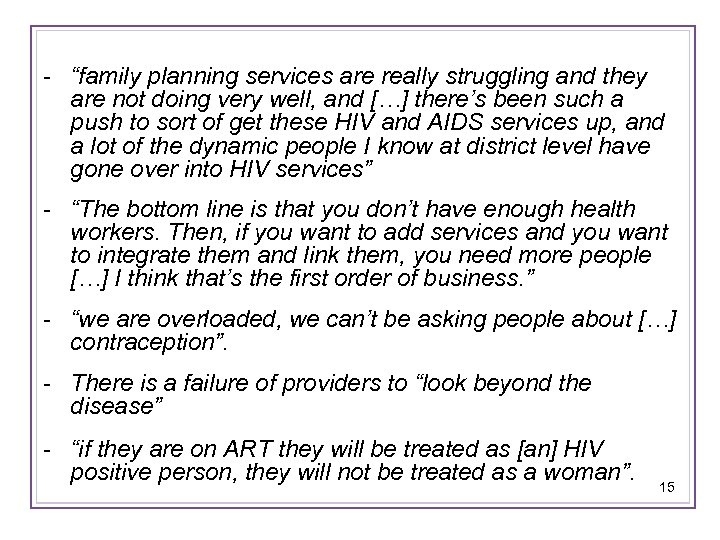 - “family planning services are really struggling and they are not doing very well, and […] there’s been such a push to sort of get these HIV and AIDS services up, and a lot of the dynamic people I know at district level have gone over into HIV services” - “The bottom line is that you don’t have enough health workers. Then, if you want to add services and you want to integrate them and link them, you need more people […] I think that’s the first order of business. ” - “we are overloaded, we can’t be asking people about […] contraception”. - There is a failure of providers to “look beyond the disease” - “if they are on ART they will be treated as [an] HIV positive person, they will not be treated as a woman”. 15
- “family planning services are really struggling and they are not doing very well, and […] there’s been such a push to sort of get these HIV and AIDS services up, and a lot of the dynamic people I know at district level have gone over into HIV services” - “The bottom line is that you don’t have enough health workers. Then, if you want to add services and you want to integrate them and link them, you need more people […] I think that’s the first order of business. ” - “we are overloaded, we can’t be asking people about […] contraception”. - There is a failure of providers to “look beyond the disease” - “if they are on ART they will be treated as [an] HIV positive person, they will not be treated as a woman”. 15
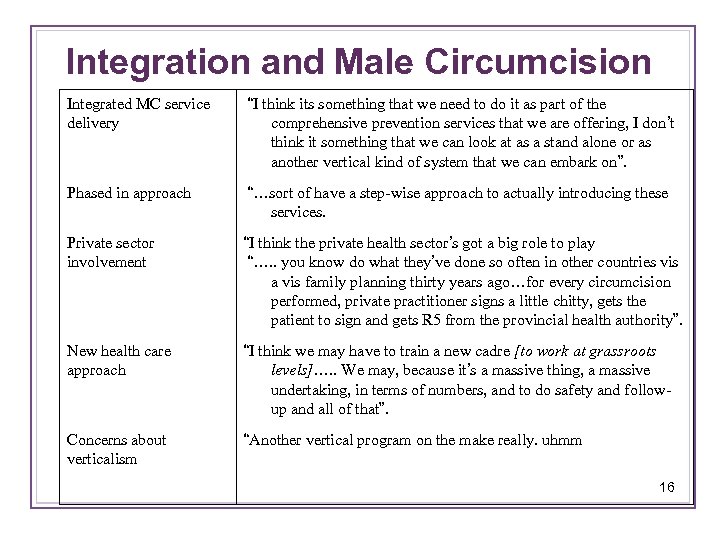 Integration and Male Circumcision Integrated MC service delivery “I think its something that we need to do it as part of the comprehensive prevention services that we are offering, I don’t think it something that we can look at as a stand alone or as another vertical kind of system that we can embark on”. Phased in approach “…sort of have a step-wise approach to actually introducing these services. Private sector involvement “I think the private health sector’s got a big role to play “…. . you know do what they’ve done so often in other countries vis a vis family planning thirty years ago…for every circumcision performed, private practitioner signs a little chitty, gets the patient to sign and gets R 5 from the provincial health authority”. New health care approach “I think we may have to train a new cadre [to work at grassroots levels]…. . We may, because it’s a massive thing, a massive undertaking, in terms of numbers, and to do safety and followup and all of that”. Concerns about verticalism “Another vertical program on the make really. uhmm 16
Integration and Male Circumcision Integrated MC service delivery “I think its something that we need to do it as part of the comprehensive prevention services that we are offering, I don’t think it something that we can look at as a stand alone or as another vertical kind of system that we can embark on”. Phased in approach “…sort of have a step-wise approach to actually introducing these services. Private sector involvement “I think the private health sector’s got a big role to play “…. . you know do what they’ve done so often in other countries vis a vis family planning thirty years ago…for every circumcision performed, private practitioner signs a little chitty, gets the patient to sign and gets R 5 from the provincial health authority”. New health care approach “I think we may have to train a new cadre [to work at grassroots levels]…. . We may, because it’s a massive thing, a massive undertaking, in terms of numbers, and to do safety and followup and all of that”. Concerns about verticalism “Another vertical program on the make really. uhmm 16
 Consensus: Integration implies different models depending on need and context • Could be: One provider, internal or external referral “there is no one size fits all” “the best way for one facility may not be the best way for another, depending on client load, and the availability of staff, and the availability of…you know, supplies and equipment. So, I don’t think there’s necessarily one best way” • However, need minimum std of care and principles for consistency • Some services require specialisation (e. g. To. P & violence) • Range in perceptions of complexity of integration: – From simple and “self evident” to the need for a “paradigm shift” in the organisation of care 17
Consensus: Integration implies different models depending on need and context • Could be: One provider, internal or external referral “there is no one size fits all” “the best way for one facility may not be the best way for another, depending on client load, and the availability of staff, and the availability of…you know, supplies and equipment. So, I don’t think there’s necessarily one best way” • However, need minimum std of care and principles for consistency • Some services require specialisation (e. g. To. P & violence) • Range in perceptions of complexity of integration: – From simple and “self evident” to the need for a “paradigm shift” in the organisation of care 17
 Health Sector and Community Entry and Baseline Assessment
Health Sector and Community Entry and Baseline Assessment
 Site Selection • Made with Provincial and District Managers • Based on perceived need for improved service delivery quality &integration • Resources • Feasibility • Willingness of district health sector 19
Site Selection • Made with Provincial and District Managers • Based on perceived need for improved service delivery quality &integration • Resources • Feasibility • Willingness of district health sector 19
 Facility Entry • Formal permission at all levels of health sector • Meetings and workshops with staff at each project facility • Meetings with Community and setting up a Community Advisory Board (CAB) • Setting up an Integration Forum • Setting up a Scientific Advisory Board 20
Facility Entry • Formal permission at all levels of health sector • Meetings and workshops with staff at each project facility • Meetings with Community and setting up a Community Advisory Board (CAB) • Setting up an Integration Forum • Setting up a Scientific Advisory Board 20
 Results & Feedback: Baseline Assessments
Results & Feedback: Baseline Assessments
 • Feedback provided to each site on data collected from that particular site • Following feedback, discussion and interpretation of findings • What do the findings mean for integration at that site? • What strategies could be employed to improve integration at your facility and more widely? • Presentation on integration, its importance and some approaches • Presentation of a scenario to stimulate discussion about integration models • Similar exercise conducted for CAB 22
• Feedback provided to each site on data collected from that particular site • Following feedback, discussion and interpretation of findings • What do the findings mean for integration at that site? • What strategies could be employed to improve integration at your facility and more widely? • Presentation on integration, its importance and some approaches • Presentation of a scenario to stimulate discussion about integration models • Similar exercise conducted for CAB 22
 Scenario: FP clients referral to VCT/STI services • HIV and STI prevalence are high and many women do not know they are infected. • Women may have signs and symptoms of STIs but may not know they need treatment or may be too embarrassed to ask. • In some work RHRU conducted at a Durban clinic in 2007 out of 70 family planning clients who came to the clinic, 20 had Chlamydia and 4 had gonorrhea, these women either did not know or were unsure they had an STI and had come to the clinic for FP and not to seek treatment. • HIV prevalence is 38. 7% in ANC clients in Kwa. Zulu-Natal (Do. H, 2009) and many women found positive in ANC may not have known their status. • Most of your clinic attendees have been tested in the past. • Family planning attendees are an important group to target for testing/re-testing as they come to the clinic regularly and may not know their current HIV status. How can C& be routinely provided in family planning services? 23
Scenario: FP clients referral to VCT/STI services • HIV and STI prevalence are high and many women do not know they are infected. • Women may have signs and symptoms of STIs but may not know they need treatment or may be too embarrassed to ask. • In some work RHRU conducted at a Durban clinic in 2007 out of 70 family planning clients who came to the clinic, 20 had Chlamydia and 4 had gonorrhea, these women either did not know or were unsure they had an STI and had come to the clinic for FP and not to seek treatment. • HIV prevalence is 38. 7% in ANC clients in Kwa. Zulu-Natal (Do. H, 2009) and many women found positive in ANC may not have known their status. • Most of your clinic attendees have been tested in the past. • Family planning attendees are an important group to target for testing/re-testing as they come to the clinic regularly and may not know their current HIV status. How can C& be routinely provided in family planning services? 23
 The Case of X Clinic • 30 clients interviewed from the following services: • • • ANC PHC PNC VCT ARV/HIV wellness STI • 4 Providers interviewed 24
The Case of X Clinic • 30 clients interviewed from the following services: • • • ANC PHC PNC VCT ARV/HIV wellness STI • 4 Providers interviewed 24
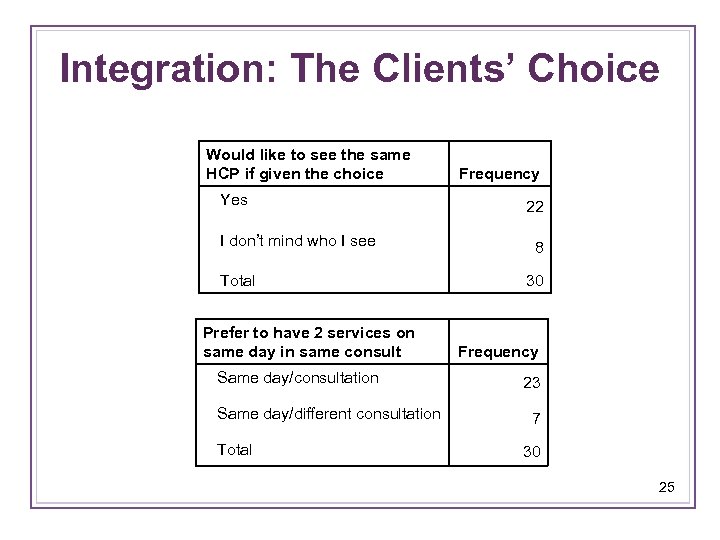 Integration: The Clients’ Choice Would like to see the same HCP if given the choice Yes I don’t mind who I see Total Prefer to have 2 services on same day in same consult Same day/consultation Same day/different consultation Total Frequency 22 8 30 Frequency 23 7 30 25
Integration: The Clients’ Choice Would like to see the same HCP if given the choice Yes I don’t mind who I see Total Prefer to have 2 services on same day in same consult Same day/consultation Same day/different consultation Total Frequency 22 8 30 Frequency 23 7 30 25
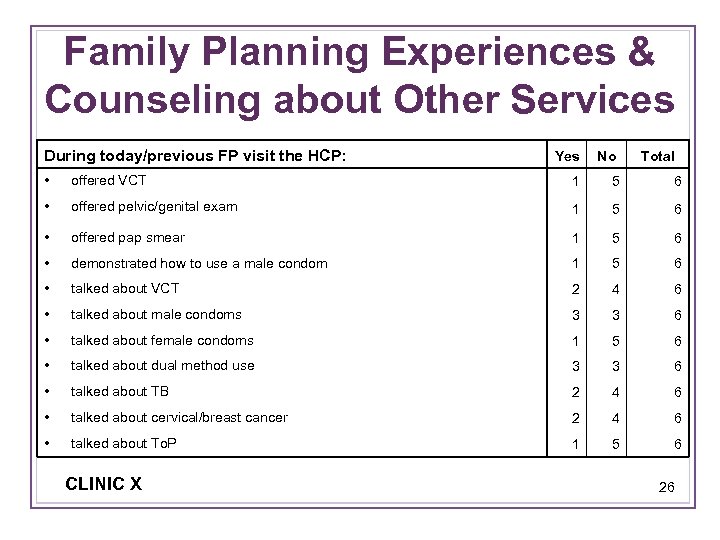 Family Planning Experiences & Counseling about Other Services During today/previous FP visit the HCP: Yes No Total • offered VCT 1 5 6 • offered pelvic/genital exam 1 5 6 • offered pap smear 1 5 6 • demonstrated how to use a male condom 1 5 6 • talked about VCT 2 4 6 • talked about male condoms 3 3 6 • talked about female condoms 1 5 6 • talked about dual method use 3 3 6 • talked about TB 2 4 6 • talked about cervical/breast cancer 2 4 6 • talked about To. P 1 5 6 CLINIC X 26
Family Planning Experiences & Counseling about Other Services During today/previous FP visit the HCP: Yes No Total • offered VCT 1 5 6 • offered pelvic/genital exam 1 5 6 • offered pap smear 1 5 6 • demonstrated how to use a male condom 1 5 6 • talked about VCT 2 4 6 • talked about male condoms 3 3 6 • talked about female condoms 1 5 6 • talked about dual method use 3 3 6 • talked about TB 2 4 6 • talked about cervical/breast cancer 2 4 6 • talked about To. P 1 5 6 CLINIC X 26
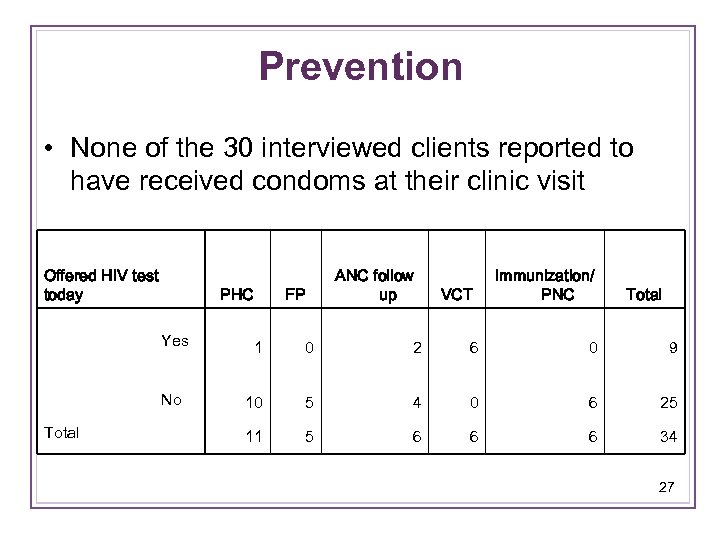 Prevention • None of the 30 interviewed clients reported to have received condoms at their clinic visit Offered HIV test today PHC FP ANC follow up VCT Immunization/ PNC Total Yes Total 1 0 2 6 0 9 No 10 5 4 0 6 25 11 5 6 6 6 34 27
Prevention • None of the 30 interviewed clients reported to have received condoms at their clinic visit Offered HIV test today PHC FP ANC follow up VCT Immunization/ PNC Total Yes Total 1 0 2 6 0 9 No 10 5 4 0 6 25 11 5 6 6 6 34 27
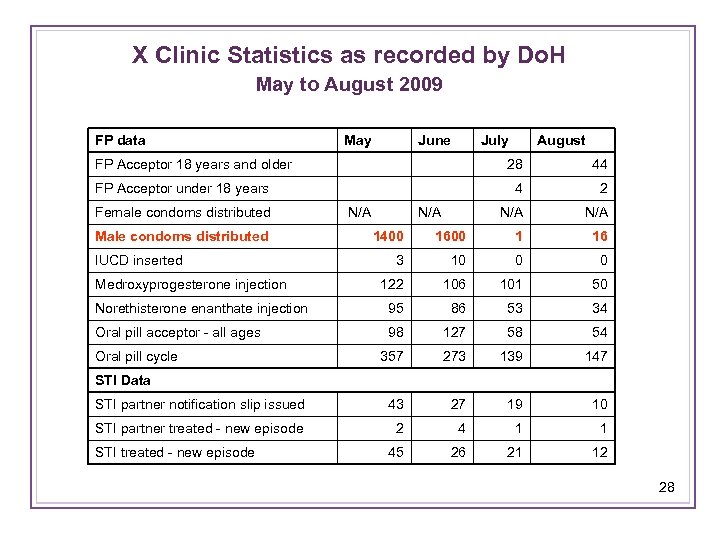 X Clinic Statistics as recorded by Do. H May to August 2009 FP data May June FP Acceptor 18 years and older 28 44 FP Acceptor under 18 years 4 2 Female condoms distributed N/A N/A Male condoms distributed July August 1400 1600 1 16 3 10 0 0 122 106 101 50 Norethisterone enanthate injection 95 86 53 34 Oral pill acceptor - all ages 98 127 58 54 357 273 139 147 IUCD inserted Medroxyprogesterone injection Oral pill cycle STI Data STI partner notification slip issued 43 27 19 10 STI partner treated - new episode 2 4 1 1 45 26 21 12 STI treated - new episode 28
X Clinic Statistics as recorded by Do. H May to August 2009 FP data May June FP Acceptor 18 years and older 28 44 FP Acceptor under 18 years 4 2 Female condoms distributed N/A N/A Male condoms distributed July August 1400 1600 1 16 3 10 0 0 122 106 101 50 Norethisterone enanthate injection 95 86 53 34 Oral pill acceptor - all ages 98 127 58 54 357 273 139 147 IUCD inserted Medroxyprogesterone injection Oral pill cycle STI Data STI partner notification slip issued 43 27 19 10 STI partner treated - new episode 2 4 1 1 45 26 21 12 STI treated - new episode 28
 Some Overall Findings
Some Overall Findings
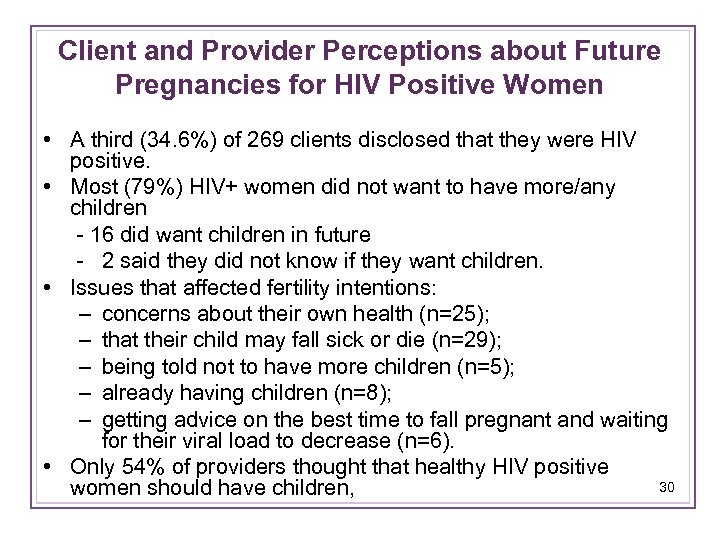 Client and Provider Perceptions about Future Pregnancies for HIV Positive Women • A third (34. 6%) of 269 clients disclosed that they were HIV positive. • Most (79%) HIV+ women did not want to have more/any children - 16 did want children in future - 2 said they did not know if they want children. • Issues that affected fertility intentions: – concerns about their own health (n=25); – that their child may fall sick or die (n=29); – being told not to have more children (n=5); – already having children (n=8); – getting advice on the best time to fall pregnant and waiting for their viral load to decrease (n=6). • Only 54% of providers thought that healthy HIV positive 30 women should have children,
Client and Provider Perceptions about Future Pregnancies for HIV Positive Women • A third (34. 6%) of 269 clients disclosed that they were HIV positive. • Most (79%) HIV+ women did not want to have more/any children - 16 did want children in future - 2 said they did not know if they want children. • Issues that affected fertility intentions: – concerns about their own health (n=25); – that their child may fall sick or die (n=29); – being told not to have more children (n=5); – already having children (n=8); – getting advice on the best time to fall pregnant and waiting for their viral load to decrease (n=6). • Only 54% of providers thought that healthy HIV positive 30 women should have children,
 DEVELOPING THE MODEL What have we learnt? Context specific, flexible approach to achieving integration is favoured One size Doesn’t fit all
DEVELOPING THE MODEL What have we learnt? Context specific, flexible approach to achieving integration is favoured One size Doesn’t fit all
 Systems • Referral systems v poor, frequent losses along the way -- look at health systems navigators • Task- shifting; better use of highly trained staff • Down referral of ARV services • Patient flow • Facility/space restructuring • Data/logistics systems poor • Integration policy lacking 32
Systems • Referral systems v poor, frequent losses along the way -- look at health systems navigators • Task- shifting; better use of highly trained staff • Down referral of ARV services • Patient flow • Facility/space restructuring • Data/logistics systems poor • Integration policy lacking 32
 Services • Attitudes to integration generally very good • Missed opportunities in FP, testing only discussed at first visit, not repeats • “Provider initiated FP” in HIV services • Request for access to female condoms • Need for a male clinic • Need for youth services • Main focus on FP 33
Services • Attitudes to integration generally very good • Missed opportunities in FP, testing only discussed at first visit, not repeats • “Provider initiated FP” in HIV services • Request for access to female condoms • Need for a male clinic • Need for youth services • Main focus on FP 33
 Main Issues: Clients • Clients don’t have time to be counselled about everything – defeats the purpose of a “fast-track” queue • Clients not always amenable to counselling (e. g. drunk clients) • Stigma associated with testing, clients often opt to an NGO for C&T 34
Main Issues: Clients • Clients don’t have time to be counselled about everything – defeats the purpose of a “fast-track” queue • Clients not always amenable to counselling (e. g. drunk clients) • Stigma associated with testing, clients often opt to an NGO for C&T 34
 Training/ Education Training requested on: • Integration for providers • Integration for community health workers • FP for HIV service providers • FP training for enrolled nurses and counsellors • Need for health education in waiting rooms (reintroduce health educators) • Need for more IEC materials 35
Training/ Education Training requested on: • Integration for providers • Integration for community health workers • FP for HIV service providers • FP training for enrolled nurses and counsellors • Need for health education in waiting rooms (reintroduce health educators) • Need for more IEC materials 35
 Next Steps • Convene integration forum • Agree on minimum standard model • Agree on additional integration components at specific facilities • Introduce HSNs • Finalize costing measures • Hold integration SOTA 36
Next Steps • Convene integration forum • Agree on minimum standard model • Agree on additional integration components at specific facilities • Introduce HSNs • Finalize costing measures • Hold integration SOTA 36
 ACKNOWLEDGEMENTS The William & Flora Hewlett Foundation; the KZN Provincial Department of Health; e. Thekwini District and City Health Departments of Health
ACKNOWLEDGEMENTS The William & Flora Hewlett Foundation; the KZN Provincial Department of Health; e. Thekwini District and City Health Departments of Health


