482a18ba8be055dd6f60b23c85d6f4c5.ppt
- Количество слайдов: 13
 One Person, One Digital Record Our Local Digital Roadmap Janet Fitzgerald Director of Corporate Governance
One Person, One Digital Record Our Local Digital Roadmap Janet Fitzgerald Director of Corporate Governance
 Context National context: • By 2020 – all patient and care records will be interoperable and real time • Between April 2016 and March 2018 – 10 universal priorities to make significant progress on • Scope is to include paper-free at the point of care, digitally enabled self care, real-time data analytics at the point of care, whole systems intelligence to support population health management and commissioning informed by local priorities Local context: • STP and Success Regime – how do we deploy technology to accelerate change? • Model of care – person, past middle age, 3 long term conditions The local digital roadmap needs to describe how we achieve all this.
Context National context: • By 2020 – all patient and care records will be interoperable and real time • Between April 2016 and March 2018 – 10 universal priorities to make significant progress on • Scope is to include paper-free at the point of care, digitally enabled self care, real-time data analytics at the point of care, whole systems intelligence to support population health management and commissioning informed by local priorities Local context: • STP and Success Regime – how do we deploy technology to accelerate change? • Model of care – person, past middle age, 3 long term conditions The local digital roadmap needs to describe how we achieve all this.
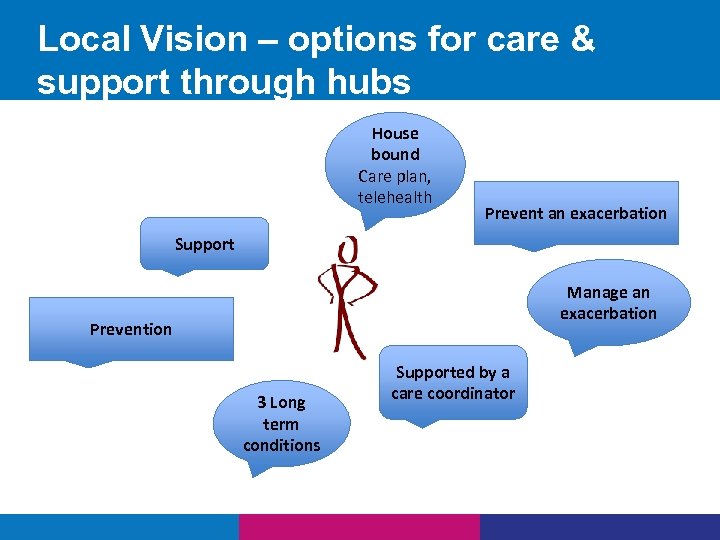 Local Vision – options for care & support through hubs House bound Care plan, telehealth Prevent an exacerbation Support Manage an exacerbation Prevention 3 Long term conditions Supported by a care coordinator
Local Vision – options for care & support through hubs House bound Care plan, telehealth Prevent an exacerbation Support Manage an exacerbation Prevention 3 Long term conditions Supported by a care coordinator
 Progress • Peninsula approach • 3 CCGs working together • 19 other stakeholders - Local Authorities and providers • Agreed set of principles • Used the “I” statements to develop a series of outcomes relating to • Identified 12 Peninsula wide projects
Progress • Peninsula approach • 3 CCGs working together • 19 other stakeholders - Local Authorities and providers • Agreed set of principles • Used the “I” statements to develop a series of outcomes relating to • Identified 12 Peninsula wide projects
 Our Principles o Optimise and make best use of any funding sources to ensure that we maximise income within this programme of work o Work collaboratively and apply our “Do It Once” methodology across the Peninsula o Make the best use of national systems o Ensure that all our work meets common standards, both technical and information standards o Make best use of our combined procurement power to ensure financial sustainability
Our Principles o Optimise and make best use of any funding sources to ensure that we maximise income within this programme of work o Work collaboratively and apply our “Do It Once” methodology across the Peninsula o Make the best use of national systems o Ensure that all our work meets common standards, both technical and information standards o Make best use of our combined procurement power to ensure financial sustainability
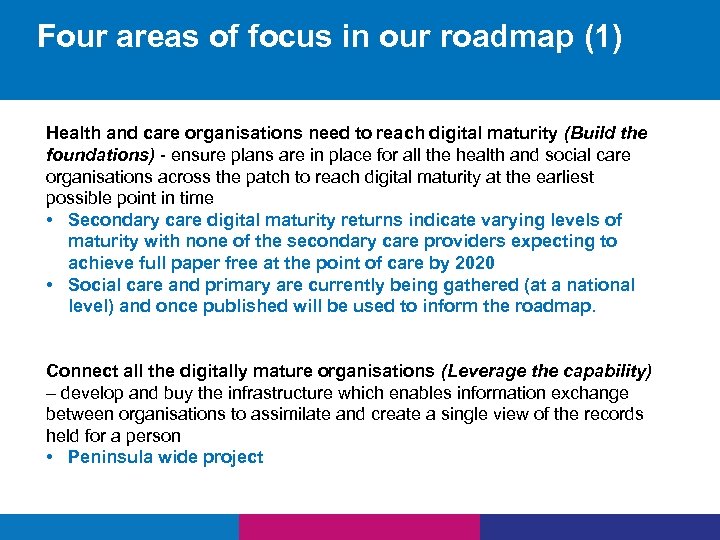 Four areas of focus in our roadmap (1) Health and care organisations need to reach digital maturity (Build the foundations) - ensure plans are in place for all the health and social care organisations across the patch to reach digital maturity at the earliest possible point in time • Secondary care digital maturity returns indicate varying levels of maturity with none of the secondary care providers expecting to achieve full paper free at the point of care by 2020 • Social care and primary are currently being gathered (at a national level) and once published will be used to inform the roadmap. Connect all the digitally mature organisations (Leverage the capability) – develop and buy the infrastructure which enables information exchange between organisations to assimilate and create a single view of the records held for a person • Peninsula wide project
Four areas of focus in our roadmap (1) Health and care organisations need to reach digital maturity (Build the foundations) - ensure plans are in place for all the health and social care organisations across the patch to reach digital maturity at the earliest possible point in time • Secondary care digital maturity returns indicate varying levels of maturity with none of the secondary care providers expecting to achieve full paper free at the point of care by 2020 • Social care and primary are currently being gathered (at a national level) and once published will be used to inform the roadmap. Connect all the digitally mature organisations (Leverage the capability) – develop and buy the infrastructure which enables information exchange between organisations to assimilate and create a single view of the records held for a person • Peninsula wide project
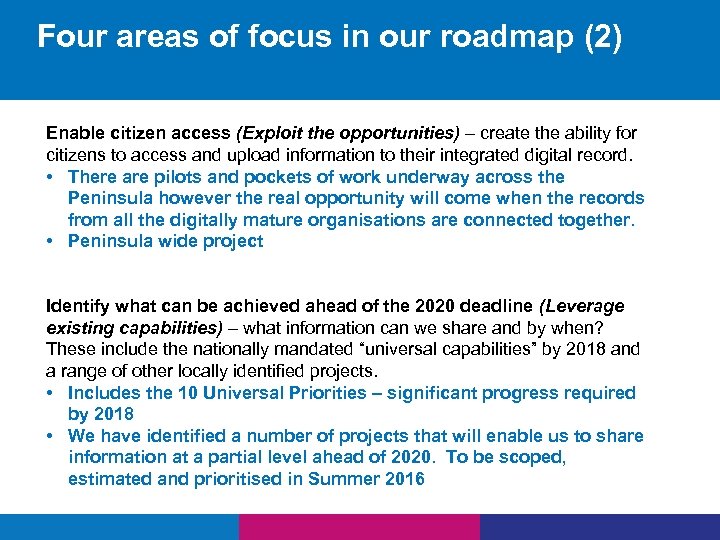 Four areas of focus in our roadmap (2) Enable citizen access (Exploit the opportunities) – create the ability for citizens to access and upload information to their integrated digital record. • There are pilots and pockets of work underway across the Peninsula however the real opportunity will come when the records from all the digitally mature organisations are connected together. • Peninsula wide project Identify what can be achieved ahead of the 2020 deadline (Leverage existing capabilities) – what information can we share and by when? These include the nationally mandated “universal capabilities” by 2018 and a range of other locally identified projects. • Includes the 10 Universal Priorities – significant progress required by 2018 • We have identified a number of projects that will enable us to share information at a partial level ahead of 2020. To be scoped, estimated and prioritised in Summer 2016
Four areas of focus in our roadmap (2) Enable citizen access (Exploit the opportunities) – create the ability for citizens to access and upload information to their integrated digital record. • There are pilots and pockets of work underway across the Peninsula however the real opportunity will come when the records from all the digitally mature organisations are connected together. • Peninsula wide project Identify what can be achieved ahead of the 2020 deadline (Leverage existing capabilities) – what information can we share and by when? These include the nationally mandated “universal capabilities” by 2018 and a range of other locally identified projects. • Includes the 10 Universal Priorities – significant progress required by 2018 • We have identified a number of projects that will enable us to share information at a partial level ahead of 2020. To be scoped, estimated and prioritised in Summer 2016
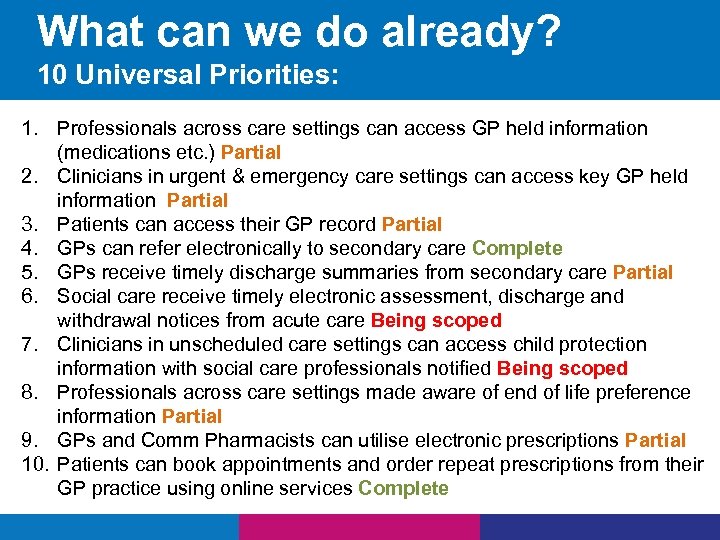 What can we do already? 10 Universal Priorities: 1. Professionals across care settings can access GP held information (medications etc. ) Partial 2. Clinicians in urgent & emergency care settings can access key GP held information Partial 3. Patients can access their GP record Partial 4. GPs can refer electronically to secondary care Complete 5. GPs receive timely discharge summaries from secondary care Partial 6. Social care receive timely electronic assessment, discharge and withdrawal notices from acute care Being scoped 7. Clinicians in unscheduled care settings can access child protection information with social care professionals notified Being scoped 8. Professionals across care settings made aware of end of life preference information Partial 9. GPs and Comm Pharmacists can utilise electronic prescriptions Partial 10. Patients can book appointments and order repeat prescriptions from their GP practice using online services Complete
What can we do already? 10 Universal Priorities: 1. Professionals across care settings can access GP held information (medications etc. ) Partial 2. Clinicians in urgent & emergency care settings can access key GP held information Partial 3. Patients can access their GP record Partial 4. GPs can refer electronically to secondary care Complete 5. GPs receive timely discharge summaries from secondary care Partial 6. Social care receive timely electronic assessment, discharge and withdrawal notices from acute care Being scoped 7. Clinicians in unscheduled care settings can access child protection information with social care professionals notified Being scoped 8. Professionals across care settings made aware of end of life preference information Partial 9. GPs and Comm Pharmacists can utilise electronic prescriptions Partial 10. Patients can book appointments and order repeat prescriptions from their GP practice using online services Complete
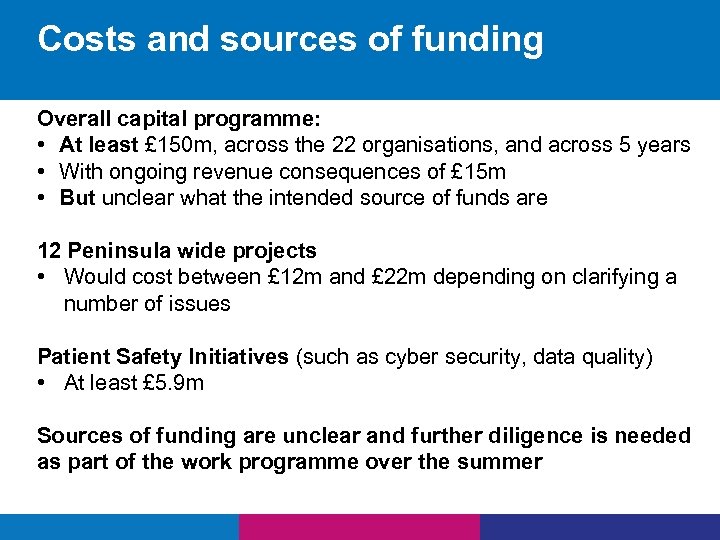 Costs and sources of funding Overall capital programme: • At least £ 150 m, across the 22 organisations, and across 5 years • With ongoing revenue consequences of £ 15 m • But unclear what the intended source of funds are 12 Peninsula wide projects • Would cost between £ 12 m and £ 22 m depending on clarifying a number of issues Patient Safety Initiatives (such as cyber security, data quality) • At least £ 5. 9 m Sources of funding are unclear and further diligence is needed as part of the work programme over the summer
Costs and sources of funding Overall capital programme: • At least £ 150 m, across the 22 organisations, and across 5 years • With ongoing revenue consequences of £ 15 m • But unclear what the intended source of funds are 12 Peninsula wide projects • Would cost between £ 12 m and £ 22 m depending on clarifying a number of issues Patient Safety Initiatives (such as cyber security, data quality) • At least £ 5. 9 m Sources of funding are unclear and further diligence is needed as part of the work programme over the summer
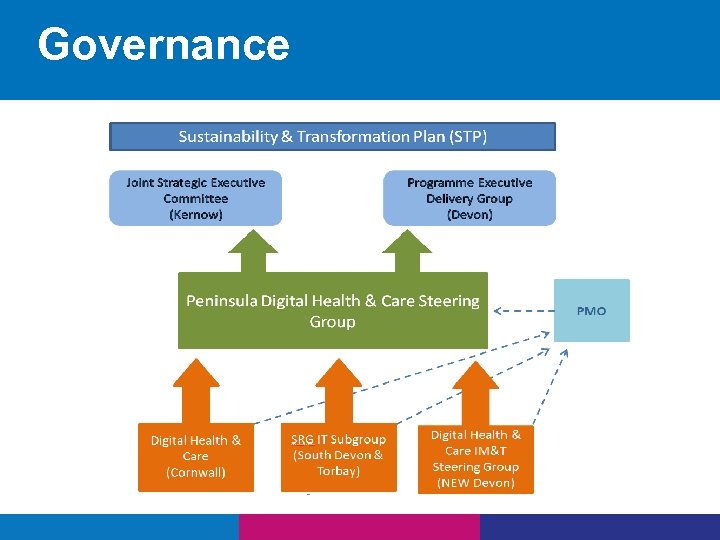 Governance
Governance
 Risks • Greater clinical involvement and capacity – CCIO capacity • We will need to consider how we engage patients and public as we scope each project • Investment – not all of this has funding identified across the system • Scale and pace • Approvals process very tight
Risks • Greater clinical involvement and capacity – CCIO capacity • We will need to consider how we engage patients and public as we scope each project • Investment – not all of this has funding identified across the system • Scale and pace • Approvals process very tight
 Next steps Stakeholder organisations 25 th May – mid June 2016 sign off Local Digital Roadmap CCG Executive Committee Final Scrutiny – Chief Officer and Chief Finance Officer 15 th June 2016 Finance Committee Submission to NHS England 23 rd June 2016 30 th June 2016
Next steps Stakeholder organisations 25 th May – mid June 2016 sign off Local Digital Roadmap CCG Executive Committee Final Scrutiny – Chief Officer and Chief Finance Officer 15 th June 2016 Finance Committee Submission to NHS England 23 rd June 2016 30 th June 2016


