3086e2cfa72ba4ab4523b06fd3b4e4f4.ppt
- Количество слайдов: 63
ONCOLOGIC EMERGENCIES By: Somar Al. Othman, M. D, 2016


ﺍﻟﻤﺮﻳﺾ ﺣﻴﺎﻥ ﺍﻟﻨﺸﻔﺎﻥ An 83 -year-old man presents to the emergency room with 1 week history of: 1. generalized weakness. 2. progressive change in mental status; confusion. 3. He has a history of diabetes and renal failure, which is well controlled. 4. Neurologic Exam: hyporeflexia, proximal myopathy. 5. GI tract: nausea/vomiting, constipation. 6. G/U Tract: polyuria.
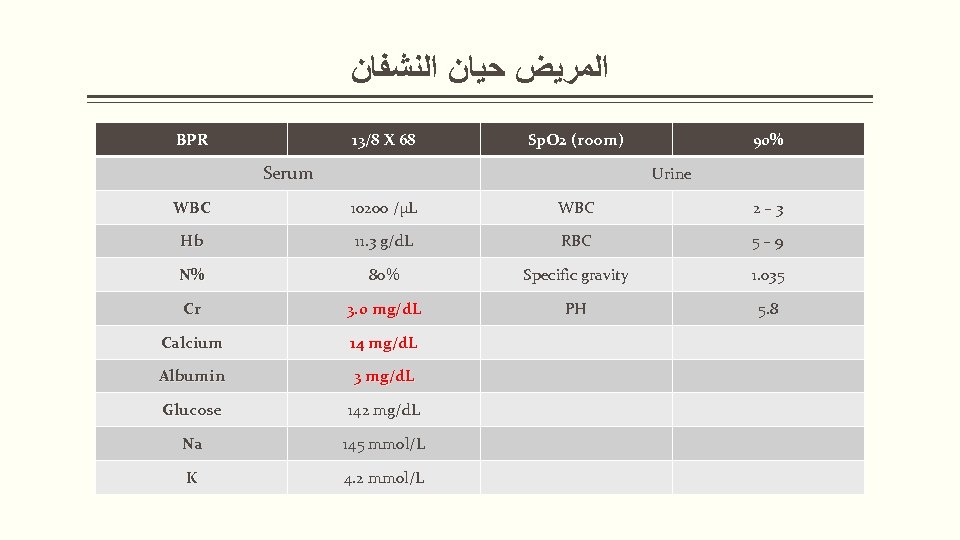
ﺍﻟﻤﺮﻳﺾ ﺣﻴﺎﻥ ﺍﻟﻨﺸﻔﺎﻥ BPR 13/8 X 68 Sp. O 2 (room) Serum 90% Urine WBC 10200 /µL WBC 2– 3 Hb 11. 3 g/d. L RBC 5– 9 N% 80% Specific gravity 1. 035 Cr 3. 0 mg/d. L PH 5. 8 Calcium 14 mg/d. L Albumin 3 mg/d. L Glucose 142 mg/d. L Na 145 mmol/L K 4. 2 mmol/L
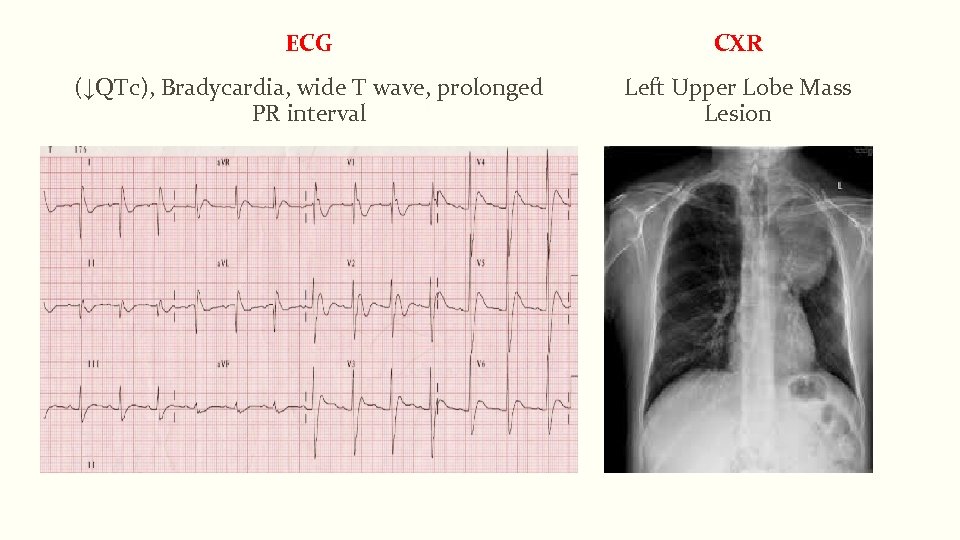
ECG CXR (↓QTc), Bradycardia, wide T wave, prolonged PR interval Left Upper Lobe Mass Lesion
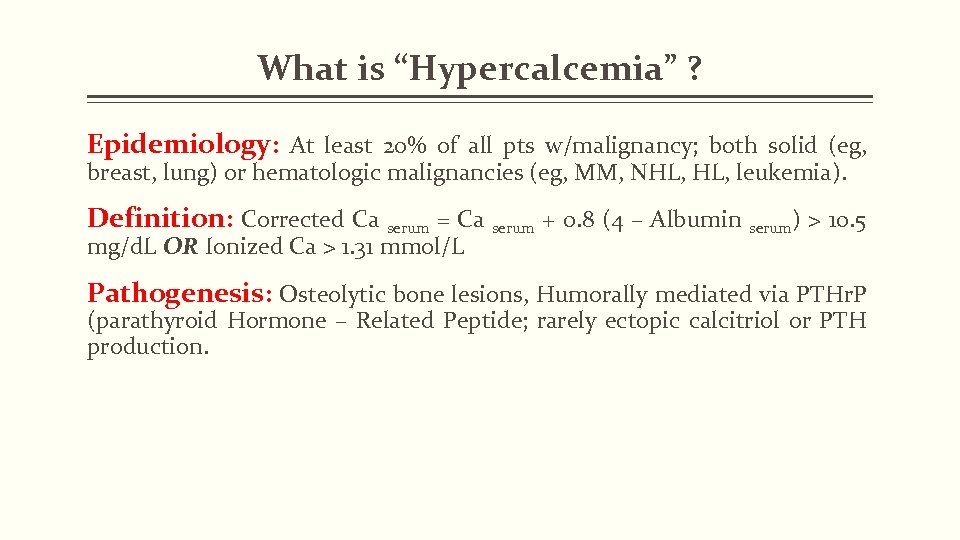
What is “Hypercalcemia” ? Epidemiology: At least 20% of all pts w/malignancy; both solid (eg, breast, lung) or hematologic malignancies (eg, MM, NHL, leukemia). Definition: Corrected Ca serum = Ca serum + 0. 8 (4 – Albumin serum) > 10. 5 mg/d. L OR Ionized Ca > 1. 31 mmol/L Pathogenesis: Osteolytic bone lesions, Humorally mediated via PTHr. P (parathyroid Hormone – Related Peptide; rarely ectopic calcitriol or PTH production.
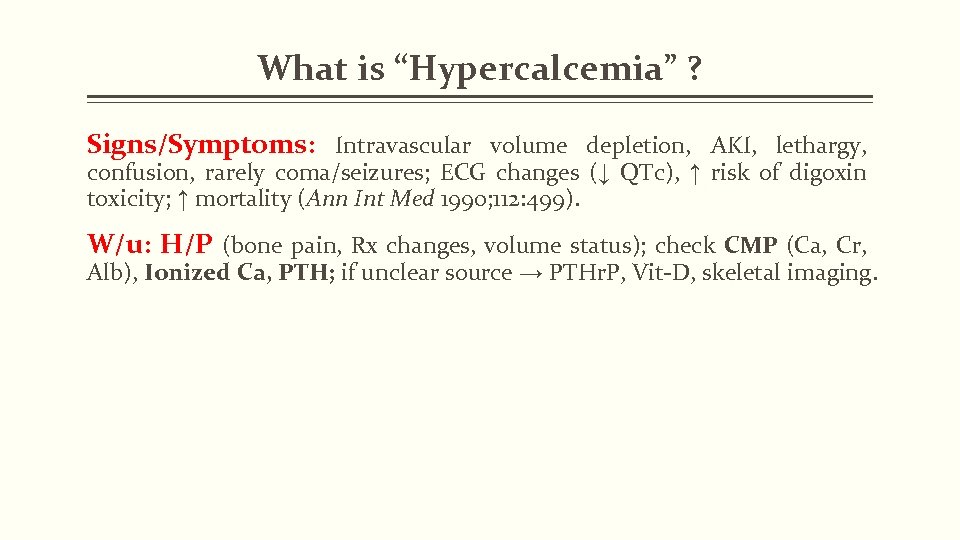
What is “Hypercalcemia” ? Signs/Symptoms: Intravascular volume depletion, AKI, lethargy, confusion, rarely coma/seizures; ECG changes (↓ QTc), ↑ risk of digoxin toxicity; ↑ mortality (Ann Int Med 1990; 112: 499). W/u: H/P (bone pain, Rx changes, volume status); check CMP (Ca, Cr, Alb), Ionized Ca, PTH; if unclear source → PTHr. P, Vit-D, skeletal imaging.
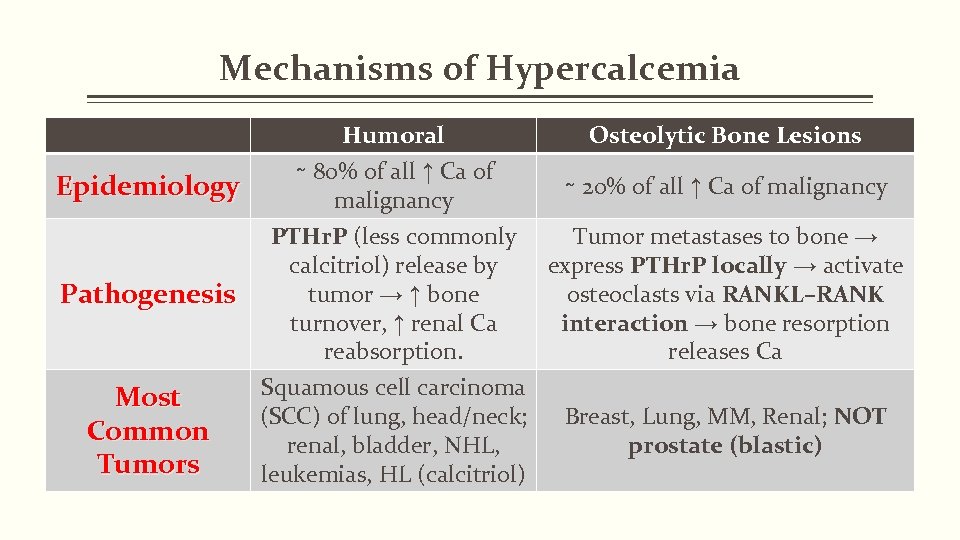
Mechanisms of Hypercalcemia Epidemiology Humoral ∼ 80% of all ↑ Ca of malignancy Osteolytic Bone Lesions ∼ 20% of all ↑ Ca of malignancy PTHr. P (less commonly Tumor metastases to bone → calcitriol) release by express PTHr. P locally → activate tumor → ↑ bone osteoclasts via RANKL–RANK Pathogenesis turnover, ↑ renal Ca interaction → bone resorption reabsorption. releases Ca Squamous cell carcinoma Most (SCC) of lung, head/neck; Breast, Lung, MM, Renal; NOT Common renal, bladder, NHL, prostate (blastic) Tumors leukemias, HL (calcitriol)
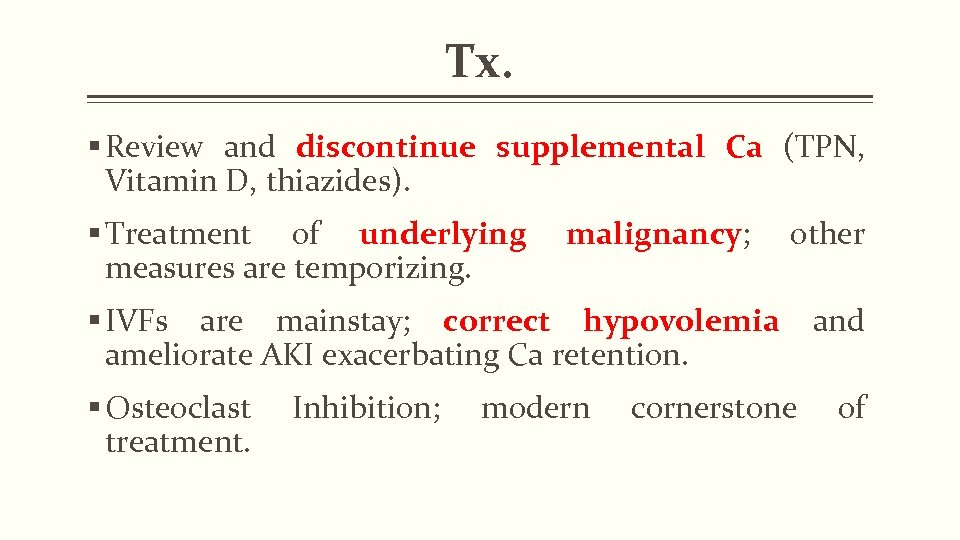
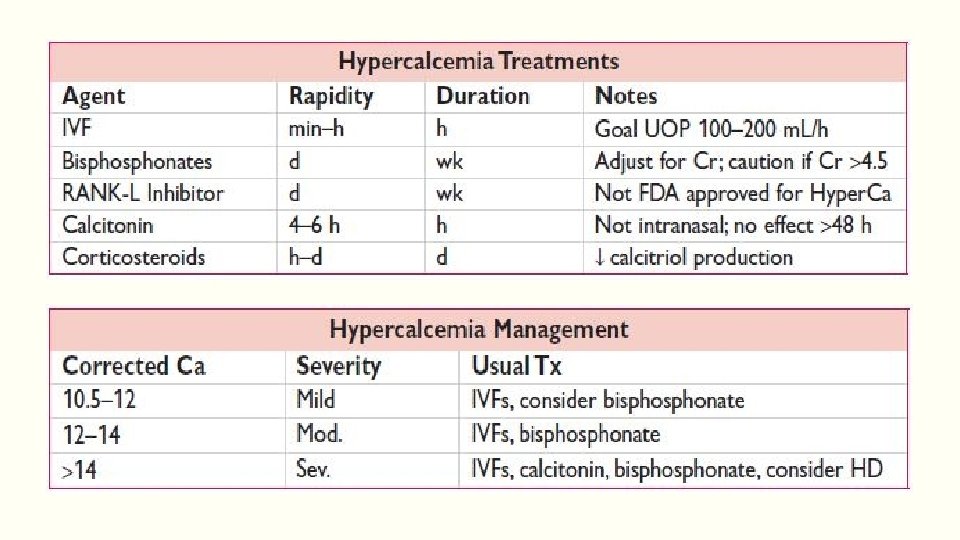
Tx. § Review and discontinue supplemental Ca (TPN, Vitamin D, thiazides). § Treatment of underlying measures are temporizing. malignancy; malignancy other § IVFs are mainstay; correct hypovolemia and ameliorate AKI exacerbating Ca retention. § Osteoclast treatment. Inhibition; modern cornerstone of
Osteoclast Inhibition Bisphonates: Onset 1 day, lasts 1– 2 wks. Zoledronic acid (Zometa®) may be superior to Pamidronate (Aredia®) (JCO 2001; 19: 558) but either acceptable; Zoledronic acid has more risk of worsened AKI than Pamidronate. Both have ↑ risk of ↓ Ca.
Osteoclast Inhibition RANK-L inhibitor: Not FDA approved for ↑Ca treatment, but Denosumab (Prolia®: Xgeva®) may be useful in severe renal failure (Ann Int Med 2012; 156: 96); ↑↑ risk of ↓Ca, especially if recent bisphonate use or prostate cancer with blastic lesions.
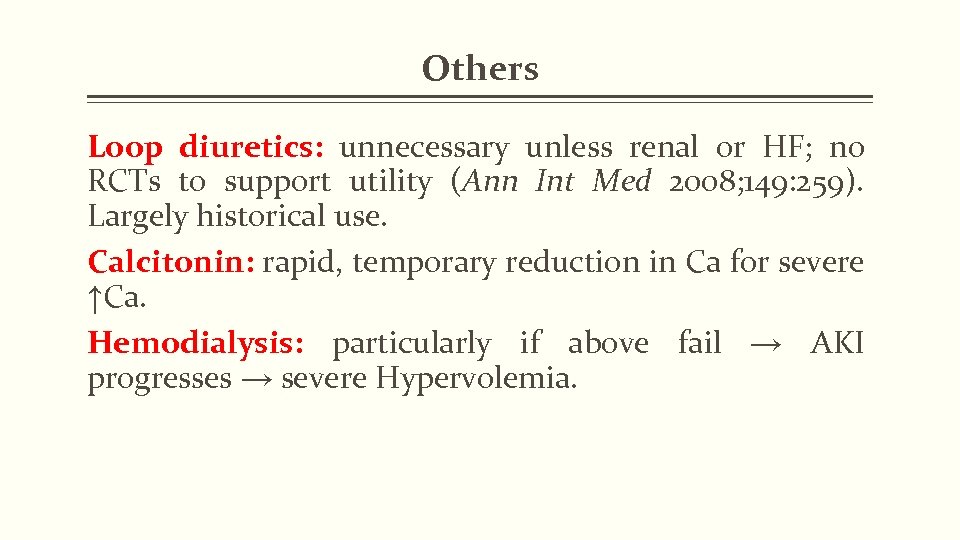
Others Loop diuretics: unnecessary unless renal or HF; no RCTs to support utility (Ann Int Med 2008; 149: 259). Largely historical use. Calcitonin: rapid, temporary reduction in Ca for severe ↑Ca. Hemodialysis: particularly if above fail → AKI progresses → severe Hypervolemia.
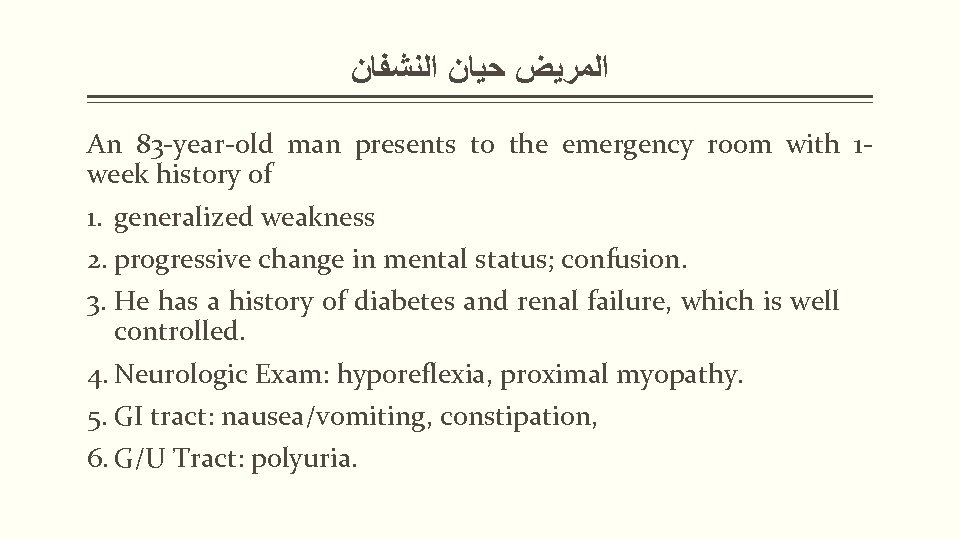
ﺍﻟﻤﺮﻳﺾ ﺣﻴﺎﻥ ﺍﻟﻨﺸﻔﺎﻥ An 83 -year-old man presents to the emergency room with 1 week history of 1. generalized weakness 2. progressive change in mental status; confusion. 3. He has a history of diabetes and renal failure, which is well controlled. 4. Neurologic Exam: hyporeflexia, proximal myopathy. 5. GI tract: nausea/vomiting, constipation, 6. G/U Tract: polyuria.
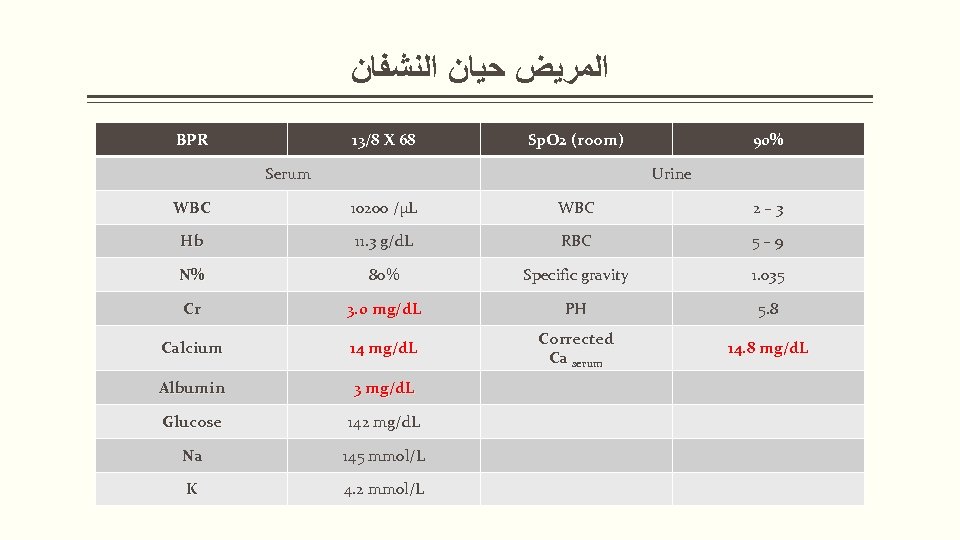
ﺍﻟﻤﺮﻳﺾ ﺣﻴﺎﻥ ﺍﻟﻨﺸﻔﺎﻥ BPR 13/8 X 68 Sp. O 2 (room) Serum 90% Urine WBC 10200 /µL WBC 2– 3 Hb 11. 3 g/d. L RBC 5– 9 N% 80% Specific gravity 1. 035 Cr 3. 0 mg/d. L PH 5. 8 Calcium 14 mg/d. L Corrected Ca serum 14. 8 mg/d. L Albumin 3 mg/d. L Glucose 142 mg/d. L Na 145 mmol/L K 4. 2 mmol/L
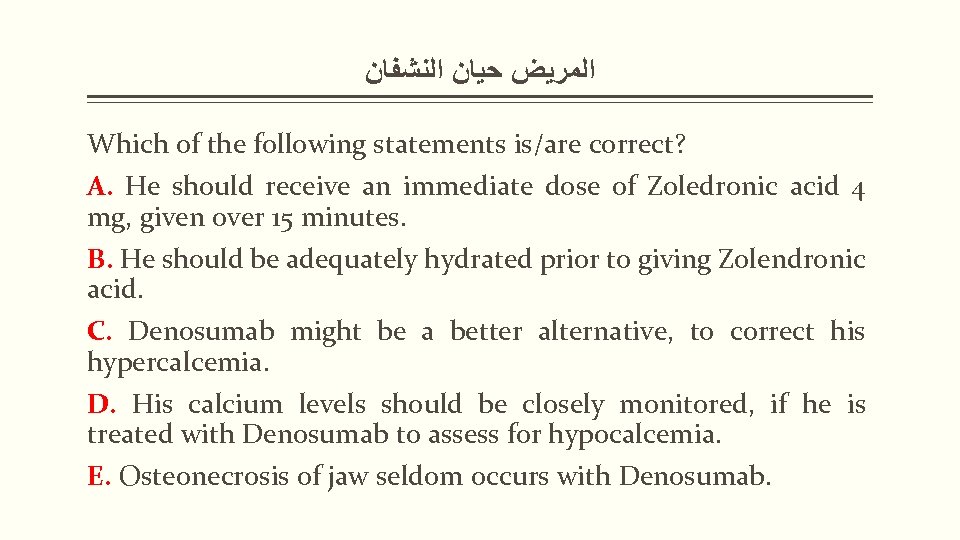
ﺍﻟﻤﺮﻳﺾ ﺣﻴﺎﻥ ﺍﻟﻨﺸﻔﺎﻥ Which of the following statements is/are correct? A. He should receive an immediate dose of Zoledronic acid 4 mg, given over 15 minutes. B. He should be adequately hydrated prior to giving Zolendronic acid. C. Denosumab might be a better alternative, to correct his hypercalcemia. D. His calcium levels should be closely monitored, if he is treated with Denosumab to assess for hypocalcemia. E. Osteonecrosis of jaw seldom occurs with Denosumab.

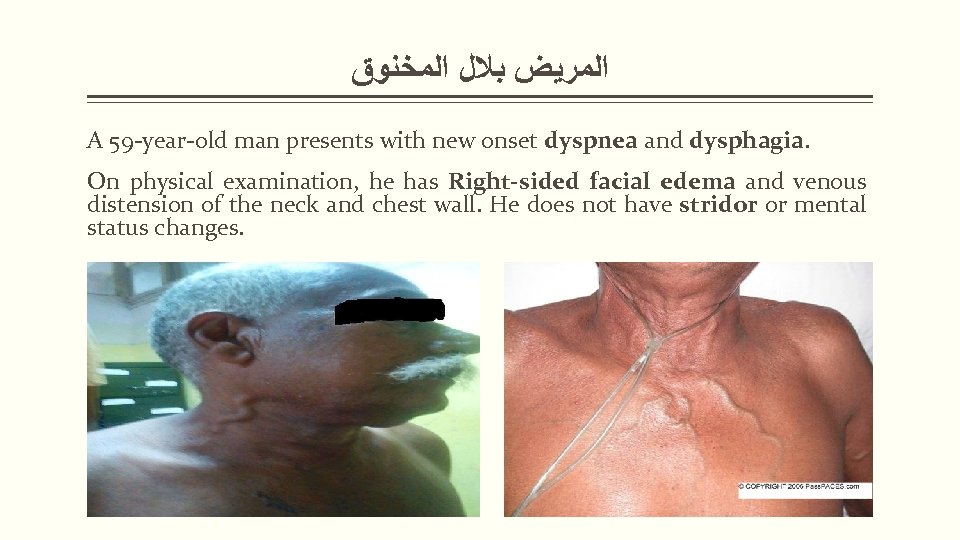
ﺍﻟﻤﺮﻳﺾ ﺑﻼﻝ ﺍﻟﻤﺨﻨﻮﻕ A 59 -year-old man presents with new onset dyspnea and dysphagia. On physical examination, he has Right-sided facial edema and venous distension of the neck and chest wall. He does not have stridor or mental status changes.
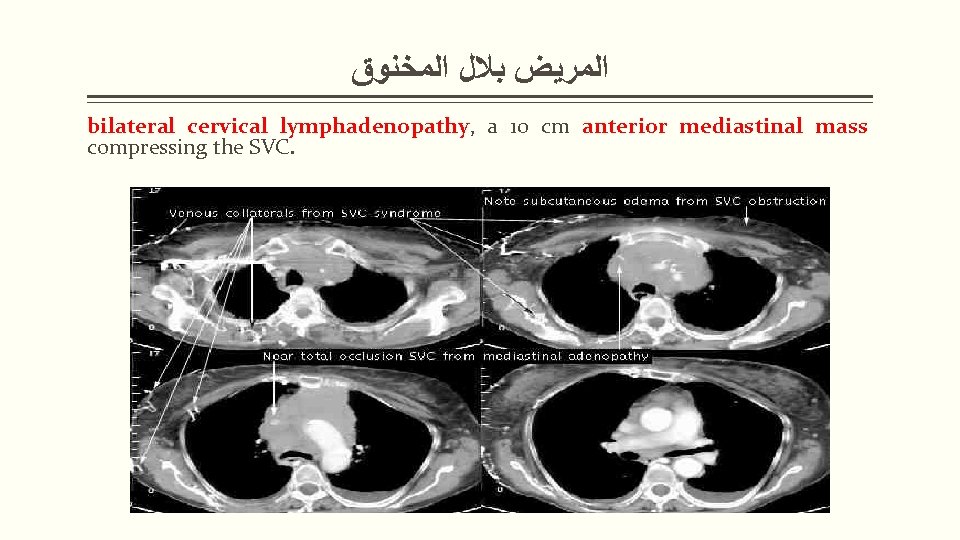
ﺍﻟﻤﺮﻳﺾ ﺑﻼﻝ ﺍﻟﻤﺨﻨﻮﻕ bilateral cervical lymphadenopathy, a 10 cm anterior mediastinal mass compressing the SVC.
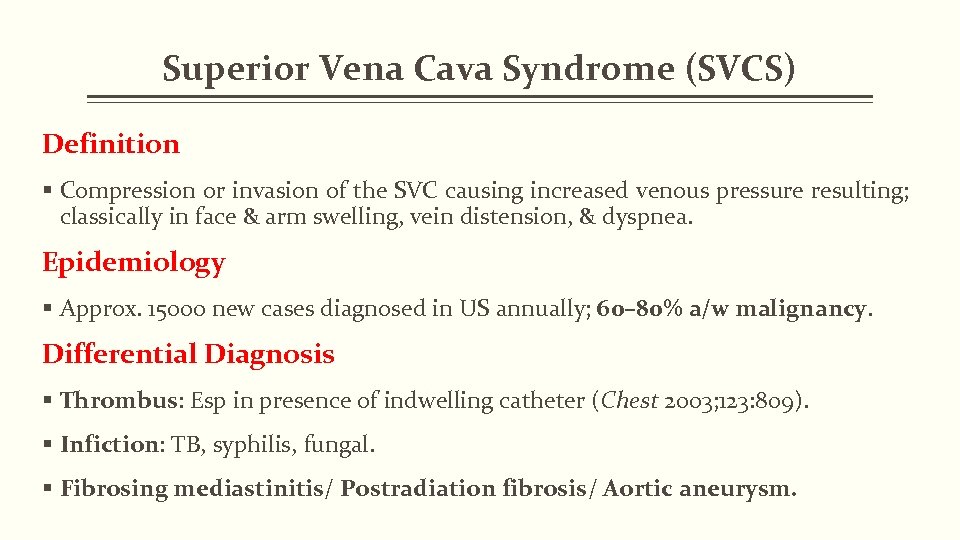
Superior Vena Cava Syndrome (SVCS) Definition § Compression or invasion of the SVC causing increased venous pressure resulting; classically in face & arm swelling, vein distension, & dyspnea. Epidemiology § Approx. 15000 new cases diagnosed in US annually; 60– 80% a/w malignancy. Differential Diagnosis § Thrombus: Esp in presence of indwelling catheter (Chest 2003; 123: 809). § Infiction: TB, syphilis, fungal. § Fibrosing mediastinitis/ Postradiation fibrosis/ Aortic aneurysm.
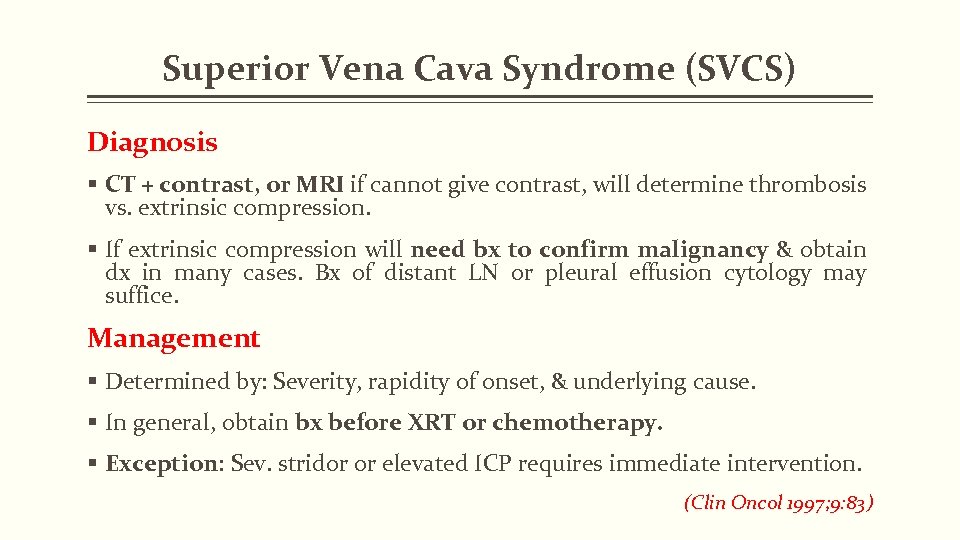
Superior Vena Cava Syndrome (SVCS) Diagnosis § CT + contrast, or MRI if cannot give contrast, will determine thrombosis vs. extrinsic compression. § If extrinsic compression will need bx to confirm malignancy & obtain dx in many cases. Bx of distant LN or pleural effusion cytology may suffice. Management § Determined by: Severity, rapidity of onset, & underlying cause. § In general, obtain bx before XRT or chemotherapy. § Exception: Sev. stridor or elevated ICP requires immediate intervention. (Clin Oncol 1997; 9: 83)
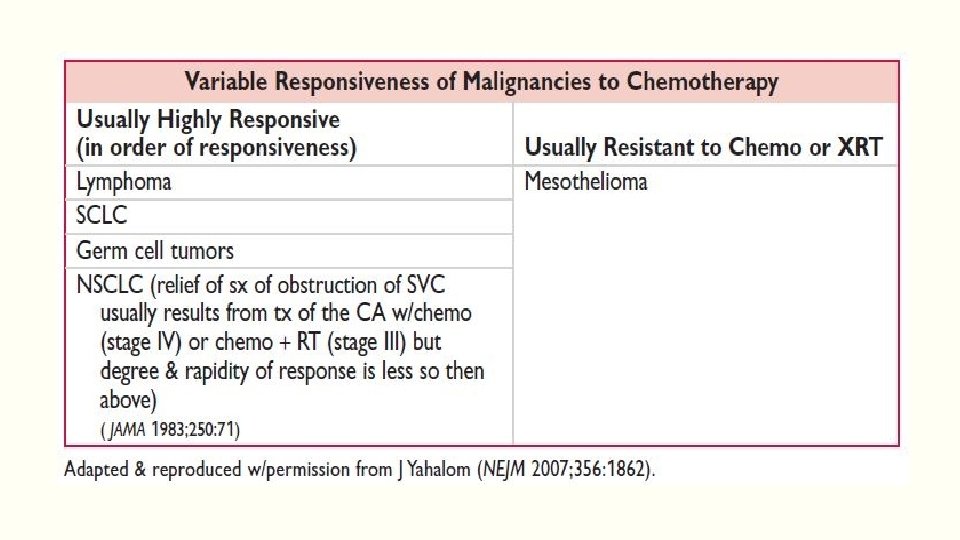
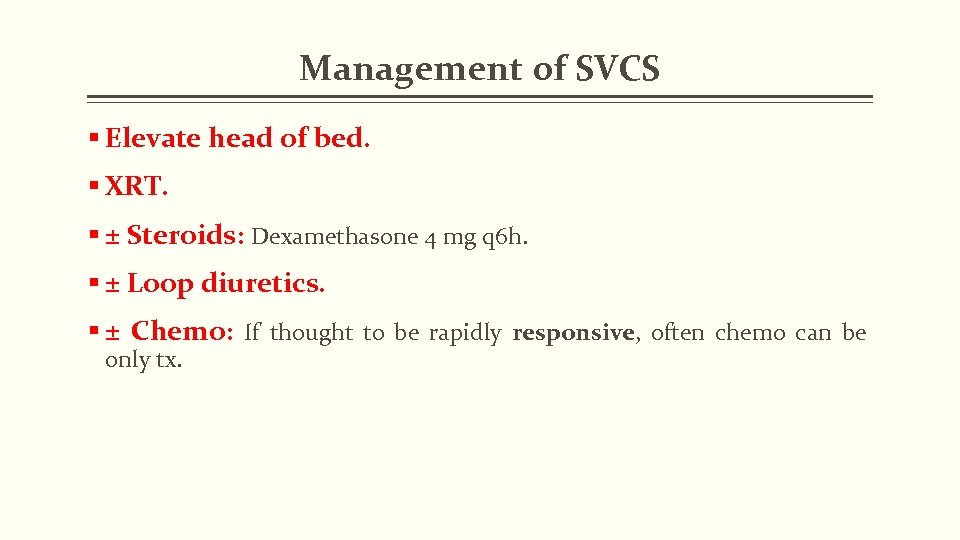
Management of SVCS § Elevate head of bed. § XRT. § ± Steroids: Dexamethasone 4 mg q 6 h. § ± Loop diuretics. § ± Chemo: If thought to be rapidly responsive, often chemo can be only tx.
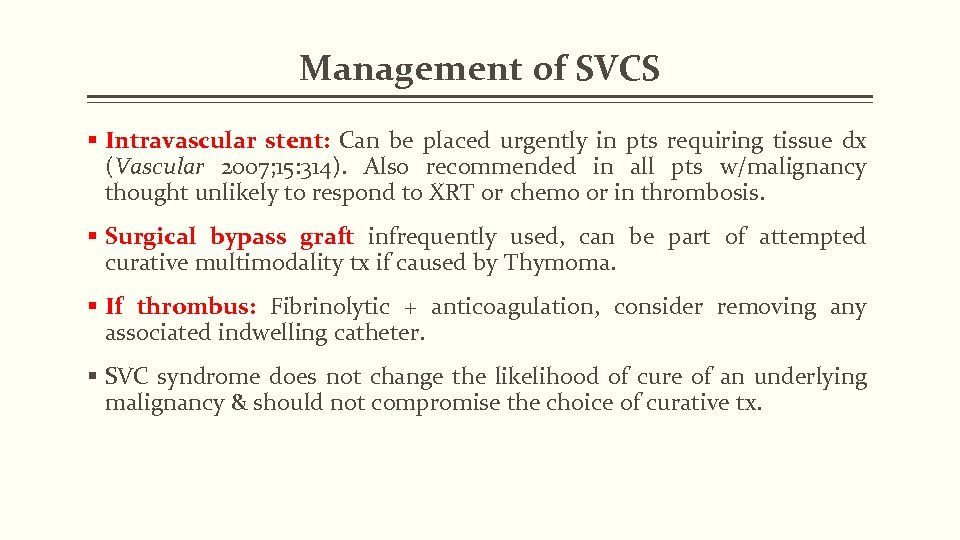
Management of SVCS § Intravascular stent: Can be placed urgently in pts requiring tissue dx (Vascular 2007; 15: 314). Also recommended in all pts w/malignancy thought unlikely to respond to XRT or chemo or in thrombosis. § Surgical bypass graft infrequently used, can be part of attempted curative multimodality tx if caused by Thymoma. § If thrombus: Fibrinolytic + anticoagulation, consider removing any associated indwelling catheter. § SVC syndrome does not change the likelihood of cure of an underlying malignancy & should not compromise the choice of curative tx.
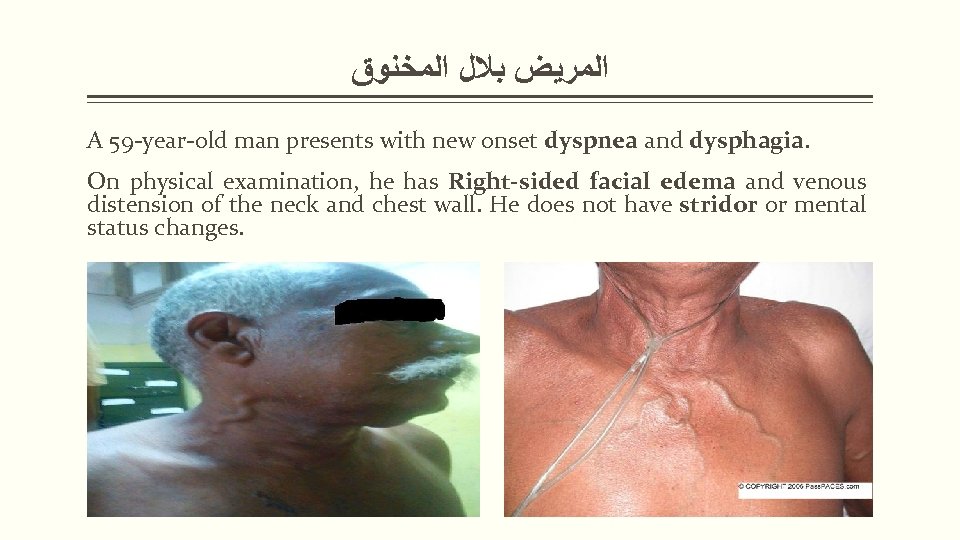
ﺍﻟﻤﺮﻳﺾ ﺑﻼﻝ ﺍﻟﻤﺨﻨﻮﻕ A 59 -year-old man presents with new onset dyspnea and dysphagia. On physical examination, he has Right-sided facial edema and venous distension of the neck and chest wall. He does not have stridor or mental status changes.
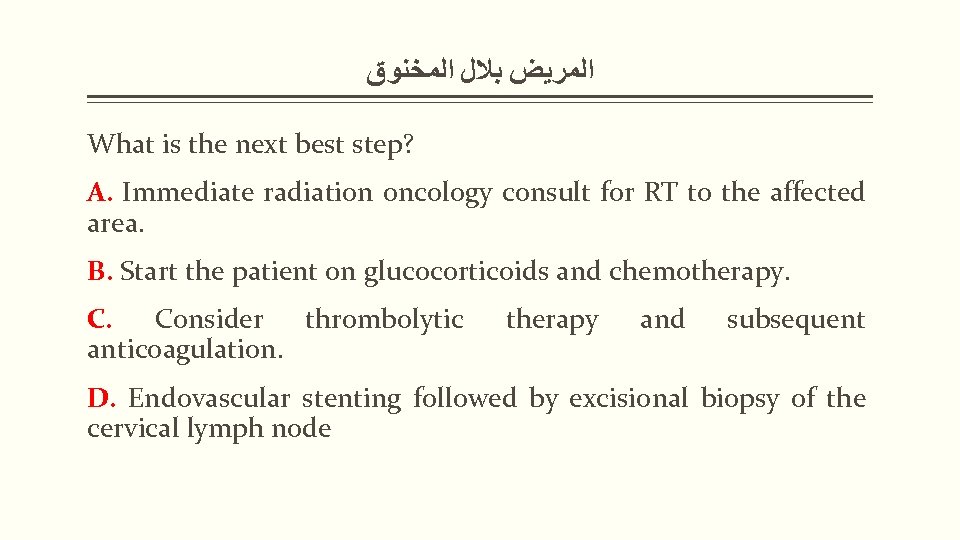
ﺍﻟﻤﺮﻳﺾ ﺑﻼﻝ ﺍﻟﻤﺨﻨﻮﻕ What is the next best step? A. Immediate radiation oncology consult for RT to the affected area. B. Start the patient on glucocorticoids and chemotherapy. C. Consider thrombolytic anticoagulation. therapy and subsequent D. Endovascular stenting followed by excisional biopsy of the cervical lymph node

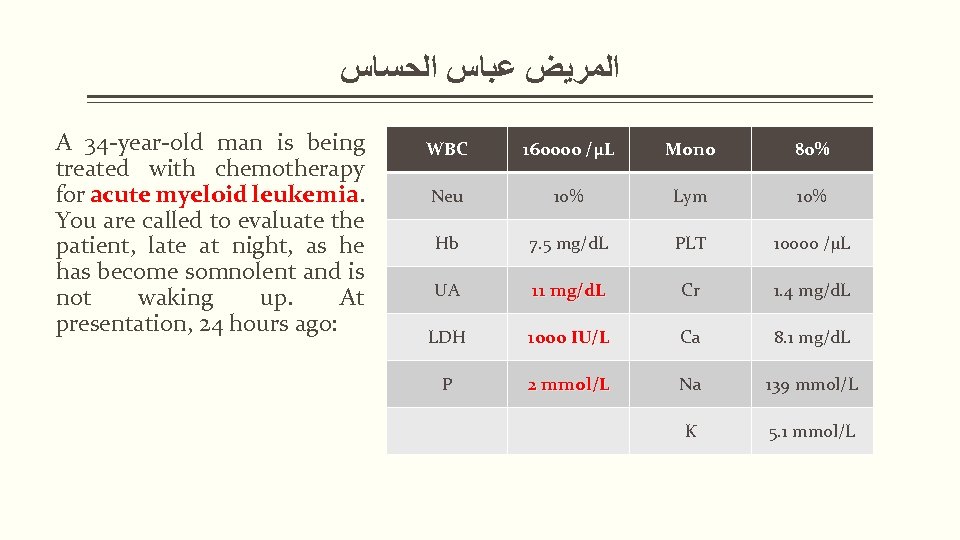
ﺍﻟﻤﺮﻳﺾ ﻋﺒﺎﺱ ﺍﻟﺤﺴﺎﺱ A 34 -year-old man is being treated with chemotherapy for acute myeloid leukemia. You are called to evaluate the patient, late at night, as he has become somnolent and is not waking up. At presentation, 24 hours ago: WBC 160000 /µL Mono 80% Neu 10% Lym 10% Hb 7. 5 mg/d. L PLT 10000 /µL UA 11 mg/d. L Cr 1. 4 mg/d. L LDH 1000 IU/L Ca 8. 1 mg/d. L P 2 mmol/L Na 139 mmol/L K 5. 1 mmol/L
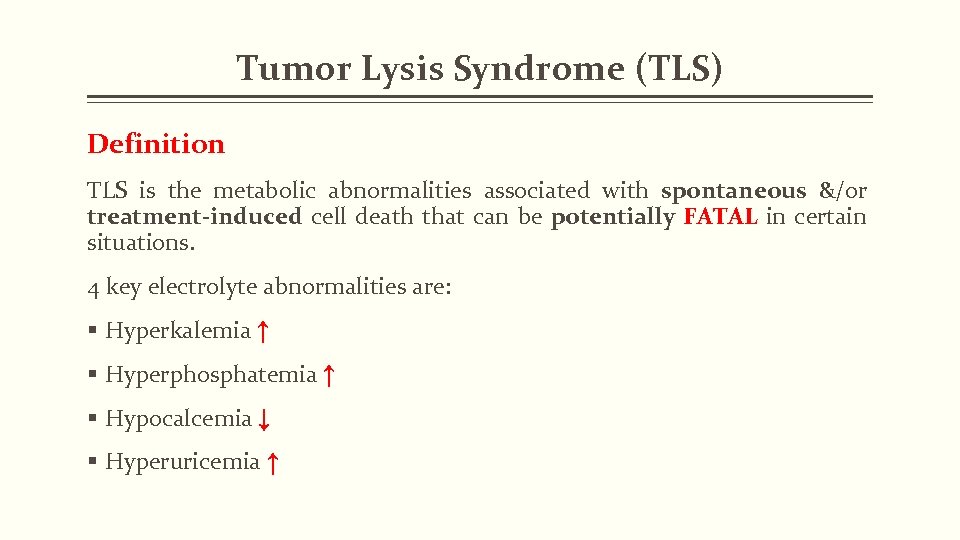
Tumor Lysis Syndrome (TLS) Definition TLS is the metabolic abnormalities associated with spontaneous &/or treatment-induced cell death that can be potentially FATAL in certain situations. 4 key electrolyte abnormalities are: § Hyperkalemia ↑ § Hyperphosphatemia ↑ § Hypocalcemia ↓ § Hyperuricemia ↑
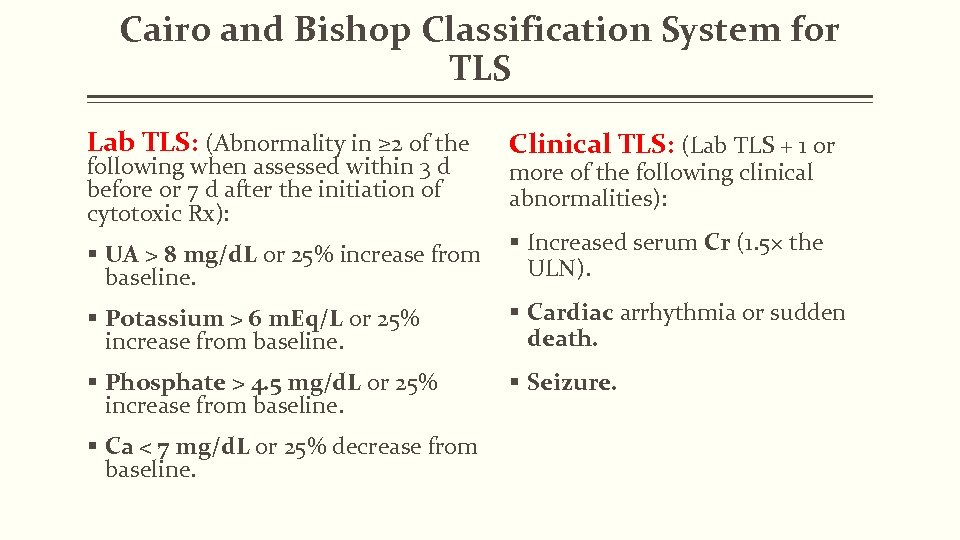
Cairo and Bishop Classification System for TLS Lab TLS: (Abnormality in ≥ 2 of the Clinical TLS: (Lab TLS + 1 or § UA > 8 mg/d. L or 25% increase from baseline. § Increased serum Cr (1. 5× the ULN). § Potassium > 6 m. Eq/L or 25% increase from baseline. § Cardiac arrhythmia or sudden death. § Phosphate > 4. 5 mg/d. L or 25% increase from baseline. § Seizure. following when assessed within 3 d before or 7 d after the initiation of cytotoxic Rx): § Ca < 7 mg/d. L or 25% decrease from baseline. more of the following clinical abnormalities):
Tumor Lysis Syndrome (TLS) Common Malignancies Associated with a High Risk of Developing TLS in Adult Patients: § Acute leukemias (eg, AML & ALL). § High-grade lymphomas such as Burkitt lymphoma & DLBCL. (Of note, indolent lymphomas rarely cause TLS).
Risk Factors for TLS Common factors associated with TLS are: § High burden of disease (such as a bulky tumor, extensive met or BM involvement). § Impaired renal function & nephrotoxins. § High proliferation rate of the CA cells. § Sensitivity of the cancer cells to treatment and intensity of initial anticancer Rx. § Volume depletion, acidic urine, Hypotension. (British Journal Haematology 2010; 149: 578; New England Journal Med 2011; 364: 1844)
Monitoring for TLS Monitoring urine output is key along w/maintaining an appropriate fluid balance: § Common labs include: UA, phosphate, potassium, Cr, Ca & LDH. § High-risk pts could be monitored in ICU w/frequent measurements of electrolytes, Cr & UA levels. § Intermediate- or low-risk pts require lab monitoring ever 8– 12 h & daily respectively.
Prophylaxis for TLS Ppx is key: Ppx tx options include the following. § IV hydration: Usually w/NS, rate depends on clinical situation but for high-risk pts, recommended 2500– 3000 m. L/m 2/d or obtain a UOP of 2 m. L/kg/h. § Urinary alkalinization (controversial). § Allopurinol &/or Rasburicase Rx (Rasburicase in high-risk pts only). (De. Vita, Hellman, and Rosenberg’s cancer: Principles & practice of oncology 9 th ed. Lippincott Williams & Wilkins, 2011; Br J Haematol 2011; 154: 3)
Management of TLS Hyperkalemia: Clinical s/s: Asymptomatic, cardiac dysrhythmia or ECG changes, muscle cramps, paresthesias, nausea, vomiting, diarrhea & sudden death Tx Options: § Mod. & asymptomatic, > 6 mmol/L: Sodium polystyrene sulfonate & avoid IV & oral potassium § Sev. (>7 mmol/L) &/or symptomatic: Sodium polystyrene sulfonate, avoid IV & oral potassium, Ca gluconate (100– 200 mg/kg) IV for lifethreatening arrhythmias, regular insulin (0. 1 Unit/kg IV) + D 25 (2 m. L/kg) IV, Na bicarbonate (1– 2 m. Eq/kg IV push), loop diuretics, inh β-agonists & in sev. cases dialysis.
Management of TLS Hyperphosphatemia: Clinical s/s: Asx, acute renal failure, 2° hypocalcemia. Tx Options: § Sevelamer hydroxide, Ca carbonate (should not be used in pts w/elevated Ca), lanthanum carbonate & aluminum hydroxide p. o. 15 m. L (50– 150 mg/kg/24 h) q 6 h & sev. cases might require dialysis (Avoid IV phosphate administration during TLS).
Management of TLS Hypocalcemia: Clinical s/s: Asx, NM irritability (including tetany, paresthesias, muscle twitching or cramping, laryngospasm or bronchospasm), cardiac dysfunction (including dysrhythmia, HF). mental status changes (including confusion, delirium, & hallucinations). seizure & sudden death. Tx Options: Correct hyperphosphatemia & in symptomatic cases Ca gluconate 50– 100 mg/kg IV administered slowly w/ECG monitoring.
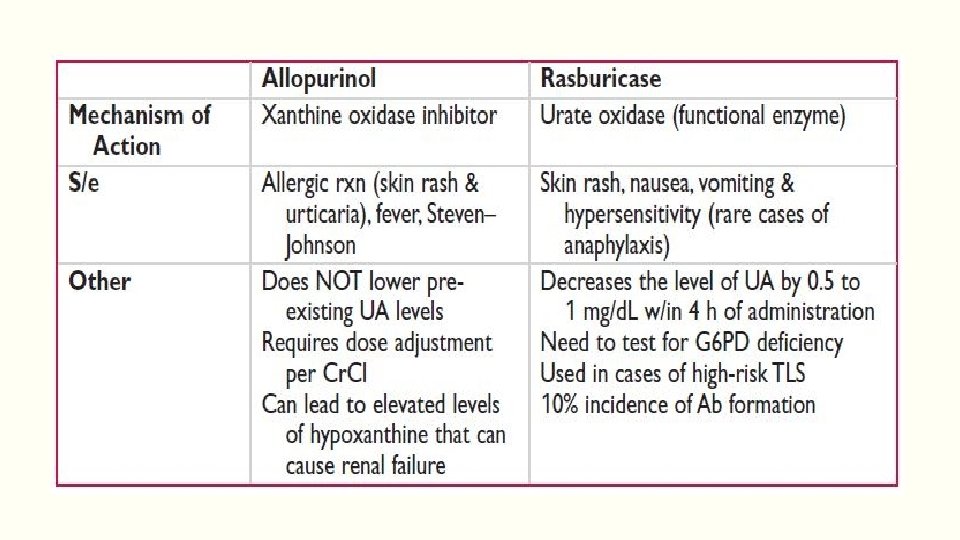
Management of TLS Hyperuricemia: § Clinical s/s: Asx, acute renal failure § Tx Options: Allopurinol vs. Rasburicase & in sev. cases Hemodialysis
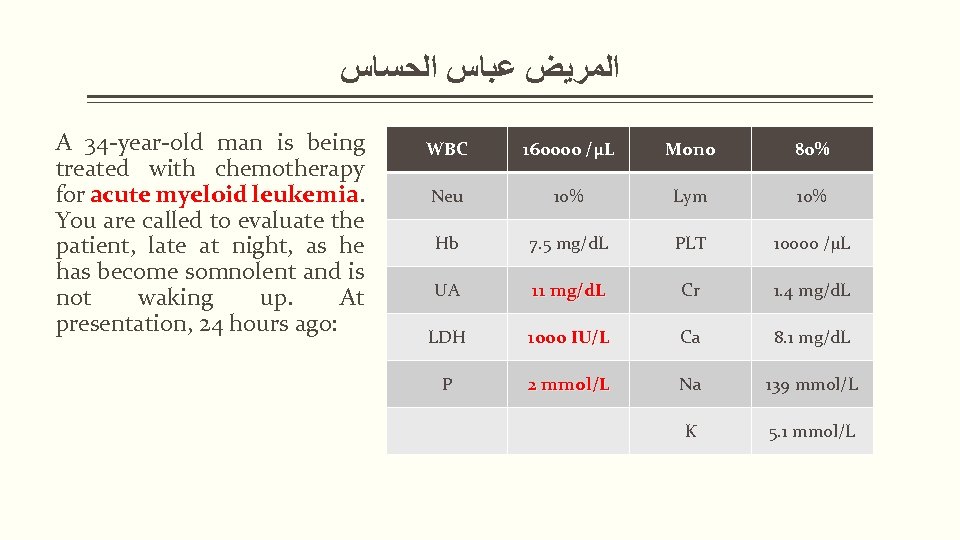
ﺍﻟﻤﺮﻳﺾ ﻋﺒﺎﺱ ﺍﻟﺤﺴﺎﺱ A 34 -year-old man is being treated with chemotherapy for acute myeloid leukemia. You are called to evaluate the patient, late at night, as he has become somnolent and is not waking up. At presentation, 24 hours ago: WBC 160000 /µL Mono 80% Neu 10% Lym 10% Hb 7. 5 mg/d. L PLT 10000 /µL UA 11 mg/d. L Cr 1. 4 mg/d. L LDH 1000 IU/L Ca 8. 1 mg/d. L P 2 mmol/L Na 139 mmol/L K 5. 1 mmol/L
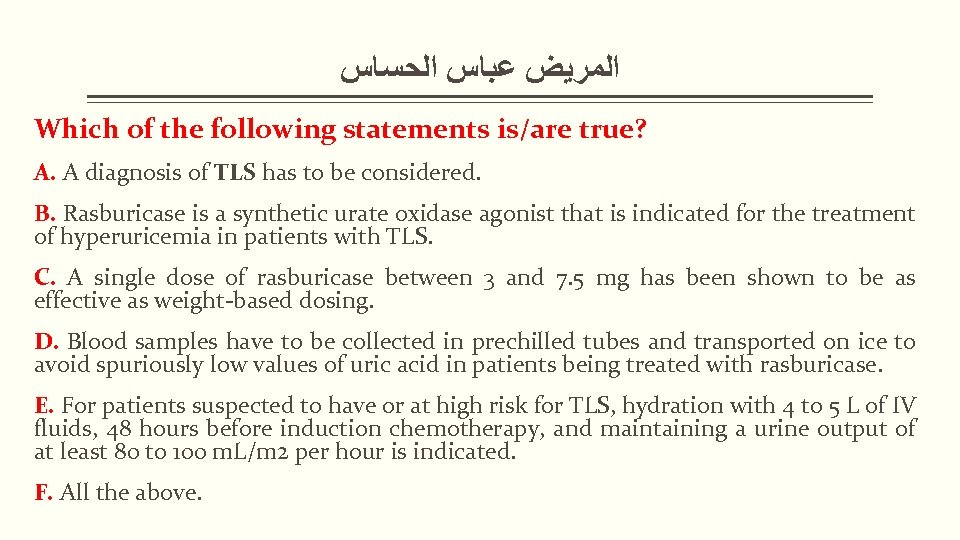
ﺍﻟﻤﺮﻳﺾ ﻋﺒﺎﺱ ﺍﻟﺤﺴﺎﺱ Which of the following statements is/are true? A. A diagnosis of TLS has to be considered. B. Rasburicase is a synthetic urate oxidase agonist that is indicated for the treatment of hyperuricemia in patients with TLS. C. A single dose of rasburicase between 3 and 7. 5 mg has been shown to be as effective as weight-based dosing. D. Blood samples have to be collected in prechilled tubes and transported on ice to avoid spuriously low values of uric acid in patients being treated with rasburicase. E. For patients suspected to have or at high risk for TLS, hydration with 4 to 5 L of IV fluids, 48 hours before induction chemotherapy, and maintaining a urine output of at least 80 to 100 m. L/m 2 per hour is indicated. F. All the above.

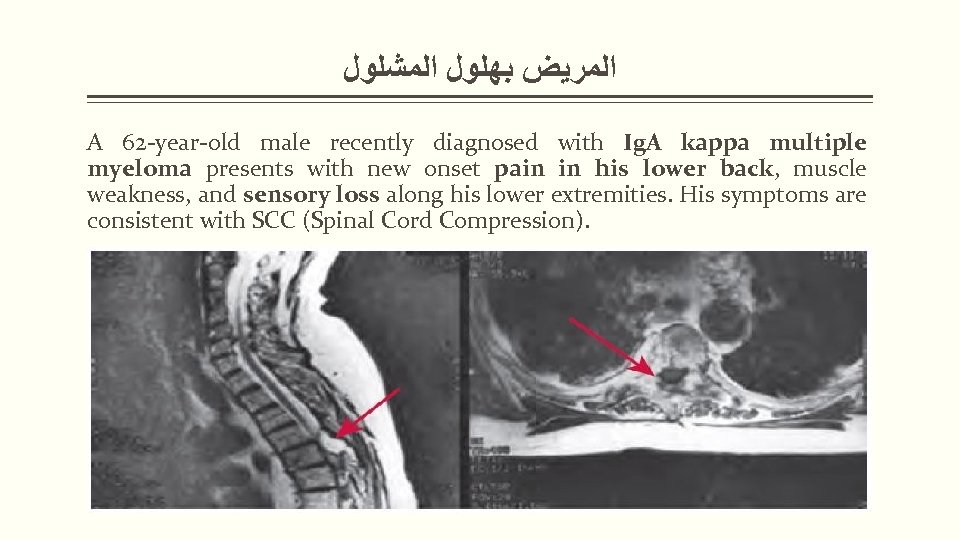
ﺍﻟﻤﺮﻳﺾ ﺑﻬﻠﻮﻝ ﺍﻟﻤﺸﻠﻮﻝ A 62 -year-old male recently diagnosed with Ig. A kappa multiple myeloma presents with new onset pain in his lower back, muscle weakness, and sensory loss along his lower extremities. His symptoms are consistent with SCC (Spinal Cord Compression).
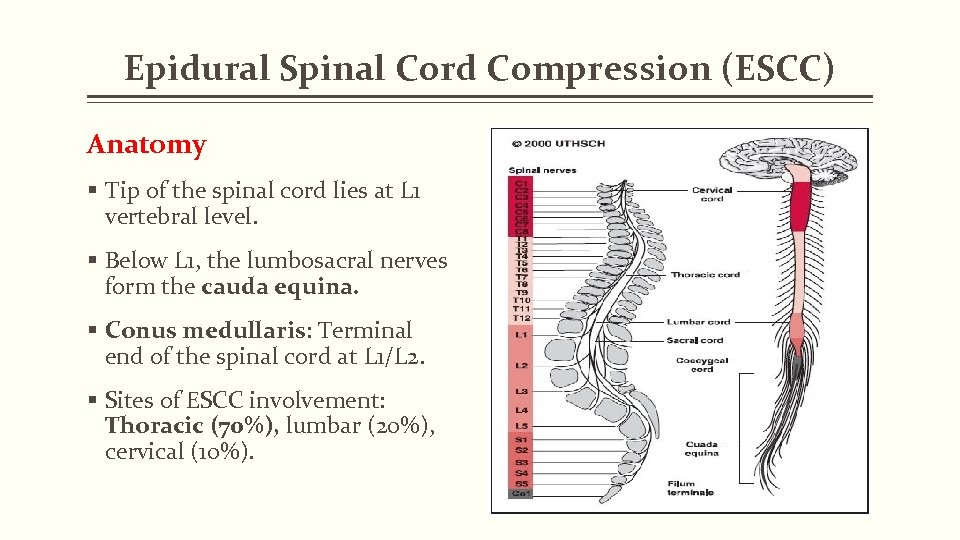
Epidural Spinal Cord Compression (ESCC) Anatomy § Tip of the spinal cord lies at L 1 vertebral level. § Below L 1, the lumbosacral nerves form the cauda equina. § Conus medullaris: Terminal end of the spinal cord at L 1/L 2. § Sites of ESCC involvement: Thoracic (70%), lumbar (20%), cervical (10%).
Epidural Spinal Cord Compression (ESCC) Definition/Risk Factors § Mets on the vertebral body extend, invades the epidural space, compressing thecal sac → causing ESCC → lead to infarction of spinal cord & irreversible loss of neurologic function. § Conus medullaris syndrome: Symmetric saddle anesthesia, bladder & bowel dysfunction), absent bulbocavernosus & anal reflexes. § Cauda equina syndrome: Sev. back pain, leg weakness, &/or sensory loss ± ↓ reflexes in lower extremities, relative sparing of bowel & bladder function. § Met tumor from any 1° site can cause ESCC; most common CA include: Lung, breast, prostate, RCC, NHL, MM. § Neuro-oncologic emergency.
Clinical Manifestations of (ESCC) S/s depending on location & degree of thecal sac compression § Back pain (96%), LE weakness. %) § Autonomic dysfunction (urinary retention/incontinence, decreased anal sphincter tone → bowel incontinence). § Sensory loss (medial thigh), Ataxia, Bilateral Babinski responses. Note: Pain on movement only suggests spinal instability, Abrupt worsening of pain may indicate a pathologic compression fracture. § If acute: Flaccid paraparesis & absent reflexes, If subacute to chronic: Spastic paraparesis & hyperactive reflexes. § Posterior column dysfunction in legs (loss of vibratory sense or proprioception).
Diagnostic Evaluation of (ESCC) § Do not wait for neurologic signs to develop! § Most important prognostic factor for regaining neurologic function is pre-tx neurologic status (Ann Neurol 1978; 3: 40). § Obtain a STAT whole spine MRI as multiple spinal epidural mets may be found (AJR 1987; 149: 1241). § If cannot do MRI, obtain a CT myelogram. Other diagnostic radiographic myelogram modalities: CT whole spine, plain spine films, bone scans. spine films § If symptoms of Headache, meningismus, obtain CSF for evaluation; however, meningismus spinal cord compression evaluation takes precedence over investigation of leptomeningeal involvement. § Consult Radiation Oncology & Neurosurgical services
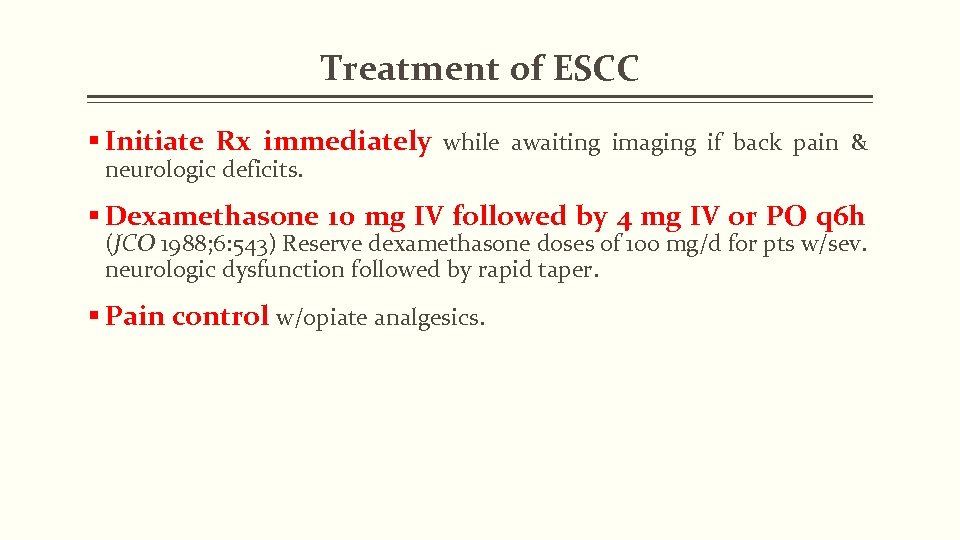
Treatment of ESCC § Initiate Rx immediately while awaiting imaging if back pain & neurologic deficits. § Dexamethasone 10 mg IV followed by 4 mg IV or PO q 6 h (JCO 1988; 6: 543) Reserve dexamethasone doses of 100 mg/d for pts w/sev. neurologic dysfunction followed by rapid taper. § Pain control w/opiate analgesics.
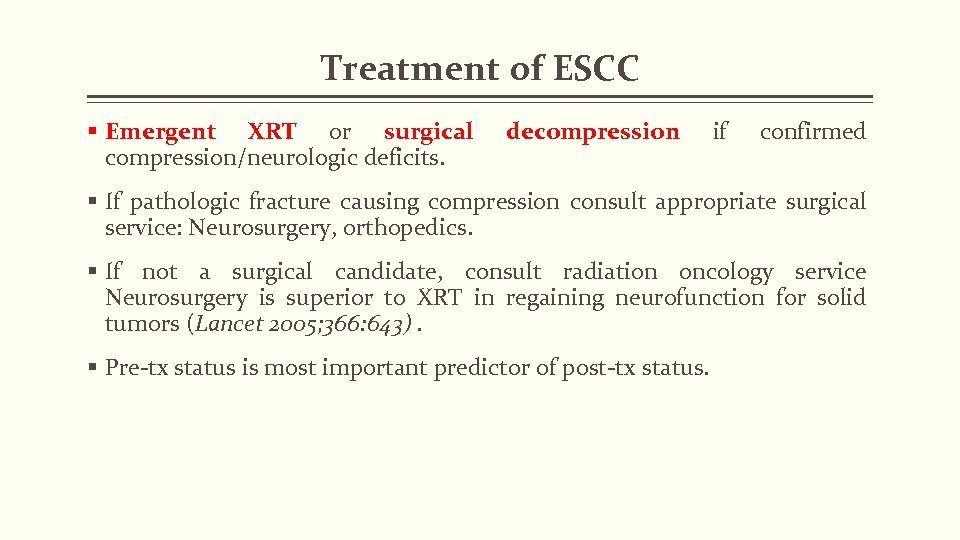
Treatment of ESCC § Emergent XRT or surgical compression/neurologic deficits. decompression if confirmed § If pathologic fracture causing compression consult appropriate surgical service: Neurosurgery, orthopedics. § If not a surgical candidate, consult radiation oncology service Neurosurgery is superior to XRT in regaining neurofunction for solid tumors (Lancet 2005; 366: 643). § Pre-tx status is most important predictor of post-tx status.
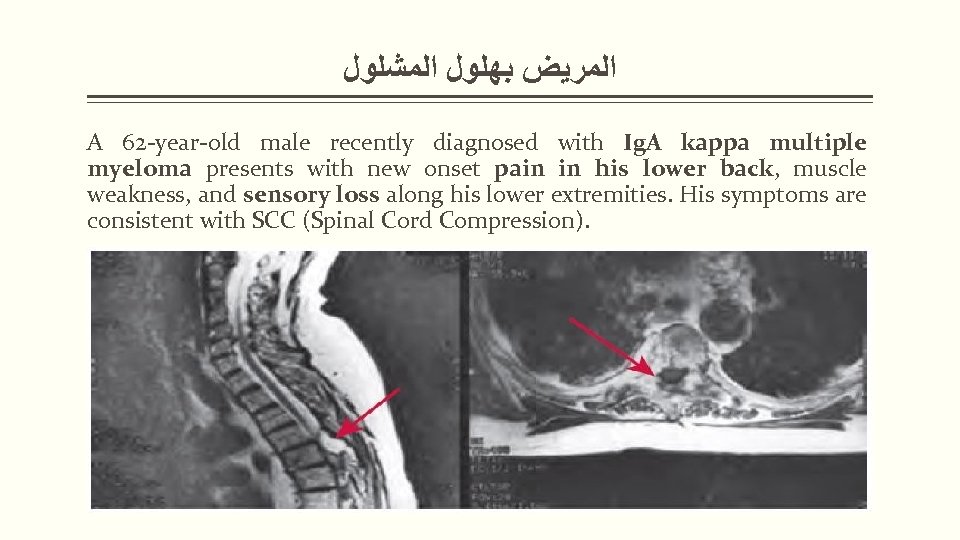
ﺍﻟﻤﺮﻳﺾ ﺑﻬﻠﻮﻝ ﺍﻟﻤﺸﻠﻮﻝ A 62 -year-old male recently diagnosed with Ig. A kappa multiple myeloma presents with new onset pain in his lower back, muscle weakness, and sensory loss along his lower extremities. His symptoms are consistent with SCC (Spinal Cord Compression).
ﺍﻟﻤﺮﻳﺾ ﺑﻬﻠﻮﻝ ﺍﻟﻤﺸﻠﻮﻝ All of the following statements are accurate about ESCC except for A. ESCC most often involves the lumbosacral spine. B. The three most common underlying cancer diagnoses associated with ESCC are lung cancer, breast cancer, and multiple myeloma. C. Pain is usually the first symptom of ESCC, often worse with recumbency. D. MRI of the entire thecal sac is the preferred modality for initial evaluation of a patient with suspected ESCC. E. The most important prognostic factor for regaining ambulation after treatment of ESCC is pretreatment neurologic status.

GOOD NIGHT SHIFT Thank you!
Superior Vena Cava Syndrome (SVCS) Definition § Compression or invasion of the SVC causing increased venous pressure resulting; classically in face & arm swelling, vein distension, & dyspnea. Epidemiology § Approx. 15000 new cases diagnosed in US annually; 60– 80% a/w malignancy. Differential Diagnosis § Thrombus: Esp in presence of indwelling catheter (Chest 2003; 123: 809) § Infxn: TB, syphilis, fungal § Fibrosing mediastinitis § Postradiation fibrosis § Aortic aneurysm
Superior Vena Cava Syndrome (SVCS) Definition § Compression or invasion of the SVC causing increased venous pressure resulting; classically in face & arm swelling, vein distension, & dyspnea. Epidemiology § Approx. 15000 new cases diagnosed in US annually; 60– 80% a/w malignancy. Differential Diagnosis § Thrombus: Esp in presence of indwelling catheter (Chest 2003; 123: 809) § Infxn: TB, syphilis, fungal § Fibrosing mediastinitis § Postradiation fibrosis § Aortic aneurysm
Title and Content Layout with Chart
Title and Content Layout with List § Add your first bullet point here § Add your second bullet point here § Add your third bullet point here
Two Content Layout with Table § First bullet point here Group 1 Group 2 § Second bullet point here Class 1 82 95 § Third bullet point here Class 2 76 88 Class 3 84 90
Title and Content Layout with Smart. Art
Picture with Caption Layout Caption

3086e2cfa72ba4ab4523b06fd3b4e4f4.ppt