fbb484de47f8c392474af88bf23605cf.ppt
- Количество слайдов: 19
 On-Time Pressure Ulcer Healing in Long Term Care Track 4: Patient Safety – Improving Quality of Care in Nursing Homes and Long-Term Care Settings September 10, 2008 Presented by Siobhan Sharkey, MBA 1
On-Time Pressure Ulcer Healing in Long Term Care Track 4: Patient Safety – Improving Quality of Care in Nursing Homes and Long-Term Care Settings September 10, 2008 Presented by Siobhan Sharkey, MBA 1
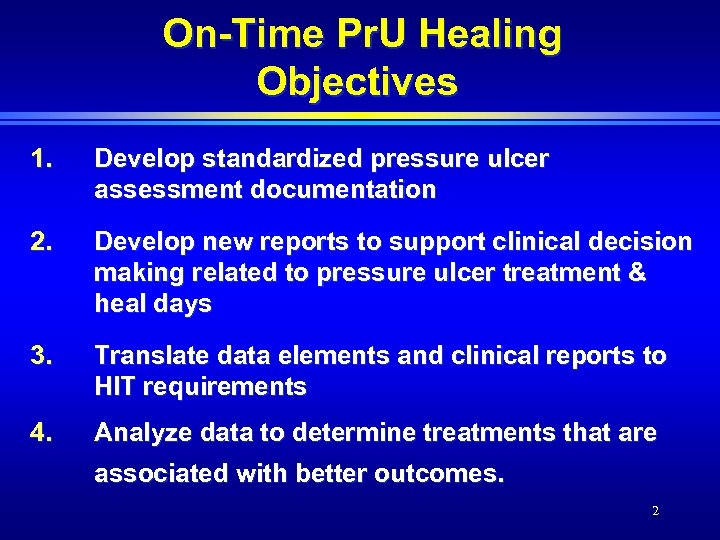 On-Time Pr. U Healing Objectives 1. Develop standardized pressure ulcer assessment documentation 2. Develop new reports to support clinical decision making related to pressure ulcer treatment & heal days 3. Translate data elements and clinical reports to HIT requirements 4. Analyze data to determine treatments that are associated with better outcomes. 2
On-Time Pr. U Healing Objectives 1. Develop standardized pressure ulcer assessment documentation 2. Develop new reports to support clinical decision making related to pressure ulcer treatment & heal days 3. Translate data elements and clinical reports to HIT requirements 4. Analyze data to determine treatments that are associated with better outcomes. 2
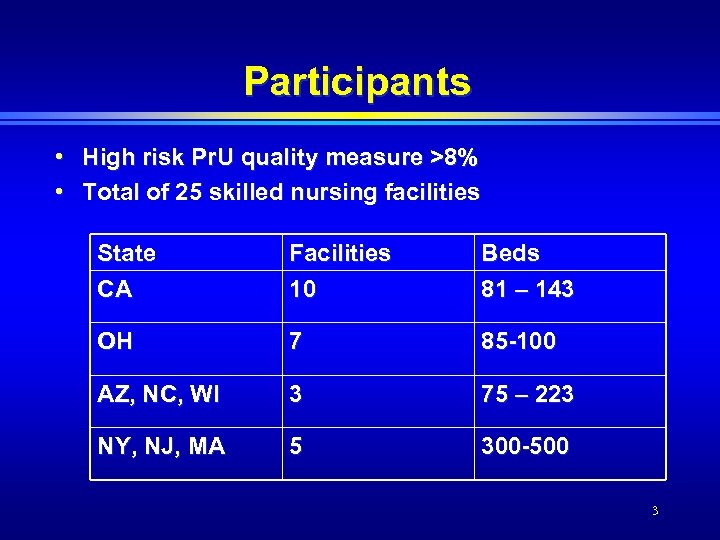 Participants • High risk Pr. U quality measure >8% • Total of 25 skilled nursing facilities State CA Facilities 10 Beds 81 – 143 OH 7 85 -100 AZ, NC, WI 3 75 – 223 NY, NJ, MA 5 300 -500 3
Participants • High risk Pr. U quality measure >8% • Total of 25 skilled nursing facilities State CA Facilities 10 Beds 81 – 143 OH 7 85 -100 AZ, NC, WI 3 75 – 223 NY, NJ, MA 5 300 -500 3
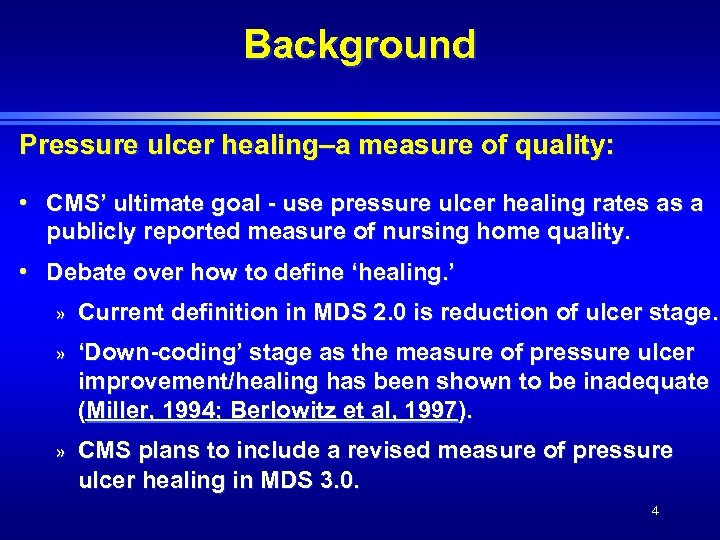 Background Pressure ulcer healing–a measure of quality: • CMS’ ultimate goal - use pressure ulcer healing rates as a publicly reported measure of nursing home quality. • Debate over how to define ‘healing. ’ » Current definition in MDS 2. 0 is reduction of ulcer stage. » ‘Down-coding’ stage as the measure of pressure ulcer improvement/healing has been shown to be inadequate (Miller, 1994; Berlowitz et al, 1997). » CMS plans to include a revised measure of pressure ulcer healing in MDS 3. 0. 4
Background Pressure ulcer healing–a measure of quality: • CMS’ ultimate goal - use pressure ulcer healing rates as a publicly reported measure of nursing home quality. • Debate over how to define ‘healing. ’ » Current definition in MDS 2. 0 is reduction of ulcer stage. » ‘Down-coding’ stage as the measure of pressure ulcer improvement/healing has been shown to be inadequate (Miller, 1994; Berlowitz et al, 1997). » CMS plans to include a revised measure of pressure ulcer healing in MDS 3. 0. 4
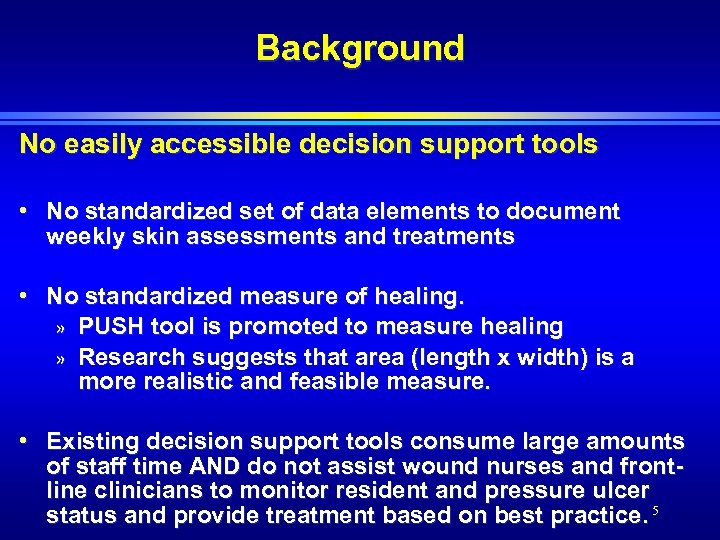 Background No easily accessible decision support tools • No standardized set of data elements to document weekly skin assessments and treatments • No standardized measure of healing. » PUSH tool is promoted to measure healing » Research suggests that area (length x width) is a more realistic and feasible measure. • Existing decision support tools consume large amounts of staff time AND do not assist wound nurses and frontline clinicians to monitor resident and pressure ulcer status and provide treatment based on best practice. 5
Background No easily accessible decision support tools • No standardized set of data elements to document weekly skin assessments and treatments • No standardized measure of healing. » PUSH tool is promoted to measure healing » Research suggests that area (length x width) is a more realistic and feasible measure. • Existing decision support tools consume large amounts of staff time AND do not assist wound nurses and frontline clinicians to monitor resident and pressure ulcer status and provide treatment based on best practice. 5
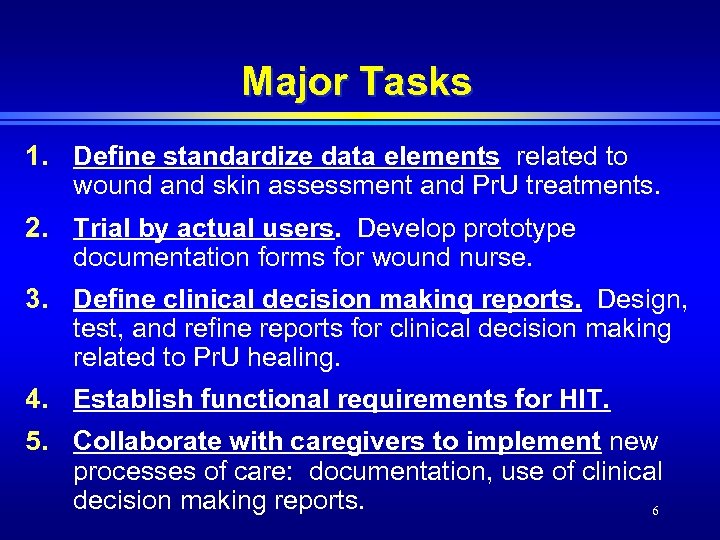 Major Tasks 1. Define standardize data elements related to wound and skin assessment and Pr. U treatments. 2. Trial by actual users. Develop prototype documentation forms for wound nurse. 3. Define clinical decision making reports. Design, test, and refine reports for clinical decision making related to Pr. U healing. 4. Establish functional requirements for HIT. 5. Collaborate with caregivers to implement new processes of care: documentation, use of clinical decision making reports. 6
Major Tasks 1. Define standardize data elements related to wound and skin assessment and Pr. U treatments. 2. Trial by actual users. Develop prototype documentation forms for wound nurse. 3. Define clinical decision making reports. Design, test, and refine reports for clinical decision making related to Pr. U healing. 4. Establish functional requirements for HIT. 5. Collaborate with caregivers to implement new processes of care: documentation, use of clinical decision making reports. 6
 Standardized Data Elements: Wound Assessment • • • • Ulcer Dimensions Wound Edges Undermining Tunneling Necrotic Tissue Type Necrotic Tissue Amount Drainage/ Exudate Type Drainage/ Exudate Amount Peri Wound Area Peri Wound Edema Peri Wound Induration Granulation Epithelialization Pain • • • Treatments Adjunctive Therapies Interventions Consultation Follow up Ulcer Status Current Visualization Ulcer Stage • Resident Disposition 7
Standardized Data Elements: Wound Assessment • • • • Ulcer Dimensions Wound Edges Undermining Tunneling Necrotic Tissue Type Necrotic Tissue Amount Drainage/ Exudate Type Drainage/ Exudate Amount Peri Wound Area Peri Wound Edema Peri Wound Induration Granulation Epithelialization Pain • • • Treatments Adjunctive Therapies Interventions Consultation Follow up Ulcer Status Current Visualization Ulcer Stage • Resident Disposition 7
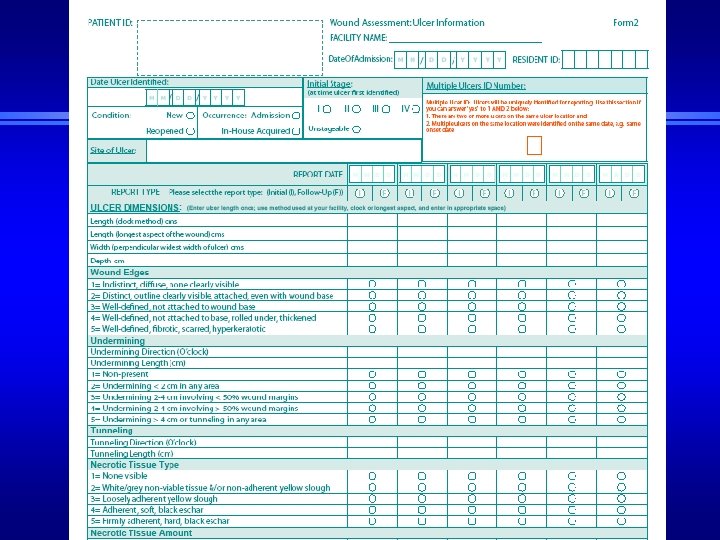 8
8
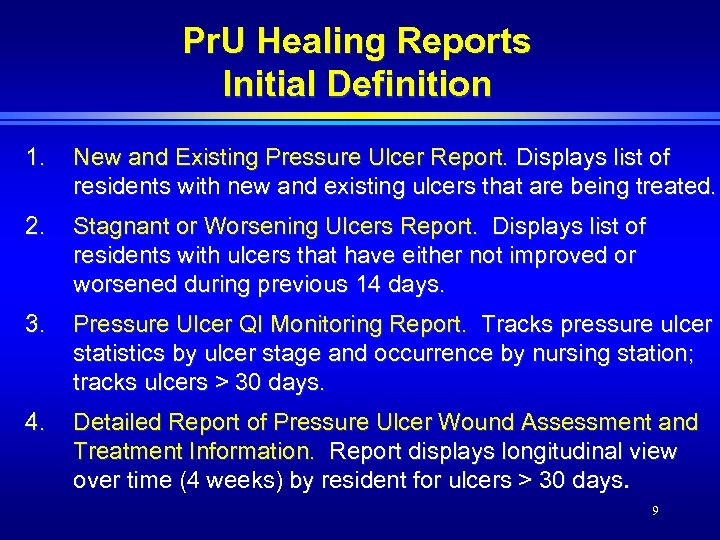 Pr. U Healing Reports Initial Definition 1. New and Existing Pressure Ulcer Report. Displays list of residents with new and existing ulcers that are being treated. 2. Stagnant or Worsening Ulcers Report. Displays list of residents with ulcers that have either not improved or worsened during previous 14 days. 3. Pressure Ulcer QI Monitoring Report. Tracks pressure ulcer statistics by ulcer stage and occurrence by nursing station; tracks ulcers > 30 days. 4. Detailed Report of Pressure Ulcer Wound Assessment and Treatment Information. Report displays longitudinal view over time (4 weeks) by resident for ulcers > 30 days. 9
Pr. U Healing Reports Initial Definition 1. New and Existing Pressure Ulcer Report. Displays list of residents with new and existing ulcers that are being treated. 2. Stagnant or Worsening Ulcers Report. Displays list of residents with ulcers that have either not improved or worsened during previous 14 days. 3. Pressure Ulcer QI Monitoring Report. Tracks pressure ulcer statistics by ulcer stage and occurrence by nursing station; tracks ulcers > 30 days. 4. Detailed Report of Pressure Ulcer Wound Assessment and Treatment Information. Report displays longitudinal view over time (4 weeks) by resident for ulcers > 30 days. 9
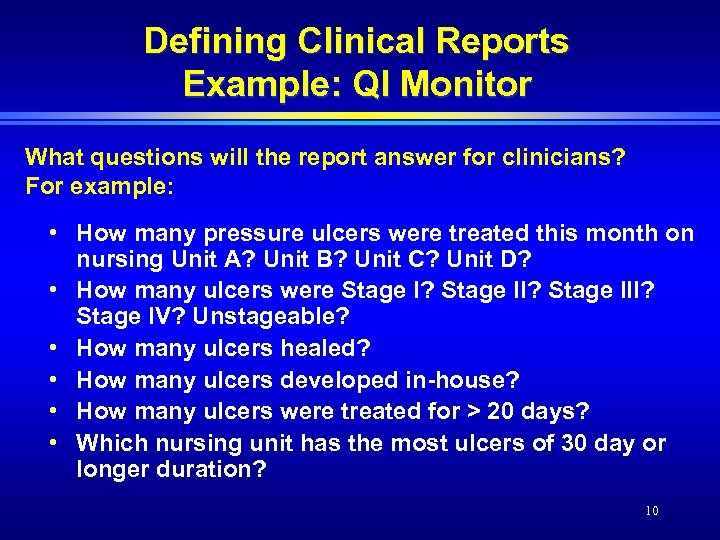 Defining Clinical Reports Example: QI Monitor What questions will the report answer for clinicians? For example: • How many pressure ulcers were treated this month on nursing Unit A? Unit B? Unit C? Unit D? • How many ulcers were Stage I? Stage III? Stage IV? Unstageable? • How many ulcers healed? • How many ulcers developed in-house? • How many ulcers were treated for > 20 days? • Which nursing unit has the most ulcers of 30 day or longer duration? 10
Defining Clinical Reports Example: QI Monitor What questions will the report answer for clinicians? For example: • How many pressure ulcers were treated this month on nursing Unit A? Unit B? Unit C? Unit D? • How many ulcers were Stage I? Stage III? Stage IV? Unstageable? • How many ulcers healed? • How many ulcers developed in-house? • How many ulcers were treated for > 20 days? • Which nursing unit has the most ulcers of 30 day or longer duration? 10
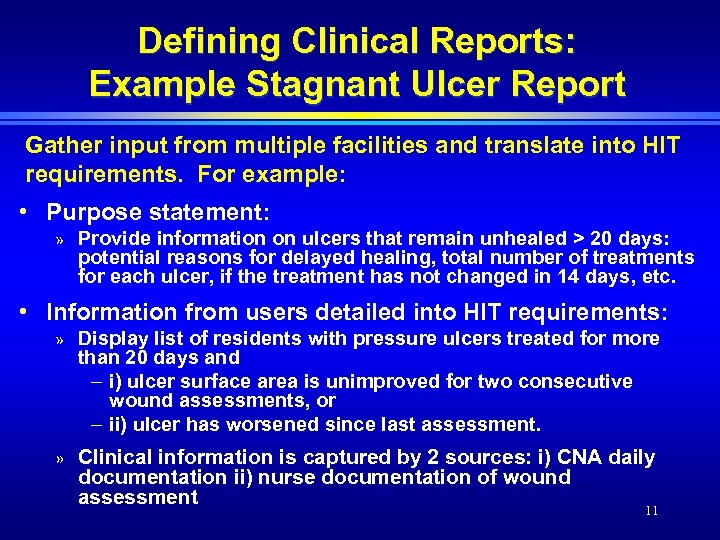 Defining Clinical Reports: Example Stagnant Ulcer Report Gather input from multiple facilities and translate into HIT requirements. For example: • Purpose statement: » Provide information on ulcers that remain unhealed > 20 days: potential reasons for delayed healing, total number of treatments for each ulcer, if the treatment has not changed in 14 days, etc. • Information from users detailed into HIT requirements: » Display list of residents with pressure ulcers treated for more than 20 days and – i) ulcer surface area is unimproved for two consecutive wound assessments, or – ii) ulcer has worsened since last assessment. » Clinical information is captured by 2 sources: i) CNA daily documentation ii) nurse documentation of wound assessment 11
Defining Clinical Reports: Example Stagnant Ulcer Report Gather input from multiple facilities and translate into HIT requirements. For example: • Purpose statement: » Provide information on ulcers that remain unhealed > 20 days: potential reasons for delayed healing, total number of treatments for each ulcer, if the treatment has not changed in 14 days, etc. • Information from users detailed into HIT requirements: » Display list of residents with pressure ulcers treated for more than 20 days and – i) ulcer surface area is unimproved for two consecutive wound assessments, or – ii) ulcer has worsened since last assessment. » Clinical information is captured by 2 sources: i) CNA daily documentation ii) nurse documentation of wound assessment 11
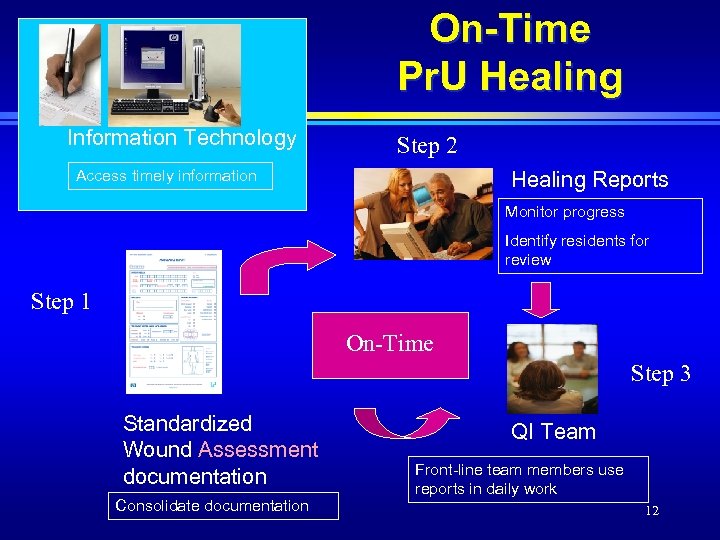 On-Time Pr. U Healing Information Technology Step 2 Access timely information Healing Reports Monitor progress Identify residents for review Step 1 On-Time Step 3 Standardized Wound Assessment documentation Consolidate documentation QI Team Front-line team members use reports in daily work 12
On-Time Pr. U Healing Information Technology Step 2 Access timely information Healing Reports Monitor progress Identify residents for review Step 1 On-Time Step 3 Standardized Wound Assessment documentation Consolidate documentation QI Team Front-line team members use reports in daily work 12
 Facility Implementation Steps • • • Implement standardized assessment facility-wide Confirm in-service strategy Confirm completeness and accuracy: participate in documentation audit with clinical expert Coordinate with project facilitators to confirm HIT vendor meeting requirements Engage multiple disciplines, including rehab, dieticians, quality improvement team Establish plan to use reports: link with workflow 13
Facility Implementation Steps • • • Implement standardized assessment facility-wide Confirm in-service strategy Confirm completeness and accuracy: participate in documentation audit with clinical expert Coordinate with project facilitators to confirm HIT vendor meeting requirements Engage multiple disciplines, including rehab, dieticians, quality improvement team Establish plan to use reports: link with workflow 13
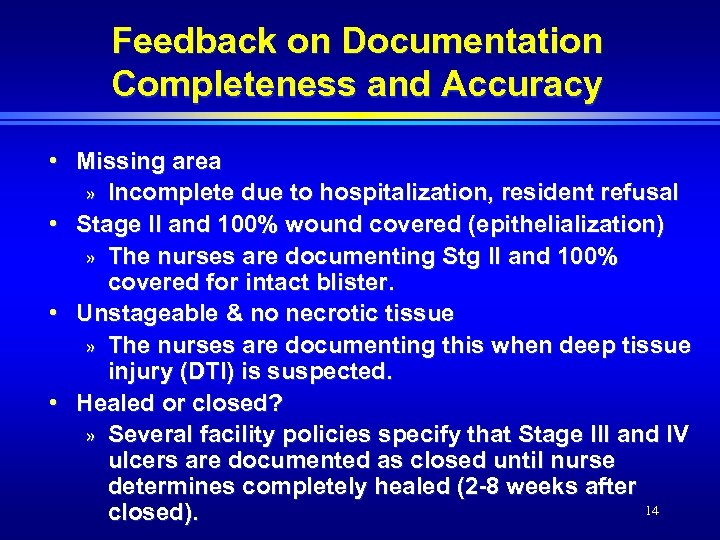 Feedback on Documentation Completeness and Accuracy • Missing area » Incomplete due to hospitalization, resident refusal • Stage II and 100% wound covered (epithelialization) » The nurses are documenting Stg II and 100% covered for intact blister. • Unstageable & no necrotic tissue » The nurses are documenting this when deep tissue injury (DTI) is suspected. • Healed or closed? » Several facility policies specify that Stage III and IV ulcers are documented as closed until nurse determines completely healed (2 -8 weeks after 14 closed).
Feedback on Documentation Completeness and Accuracy • Missing area » Incomplete due to hospitalization, resident refusal • Stage II and 100% wound covered (epithelialization) » The nurses are documenting Stg II and 100% covered for intact blister. • Unstageable & no necrotic tissue » The nurses are documenting this when deep tissue injury (DTI) is suspected. • Healed or closed? » Several facility policies specify that Stage III and IV ulcers are documented as closed until nurse determines completely healed (2 -8 weeks after 14 closed).
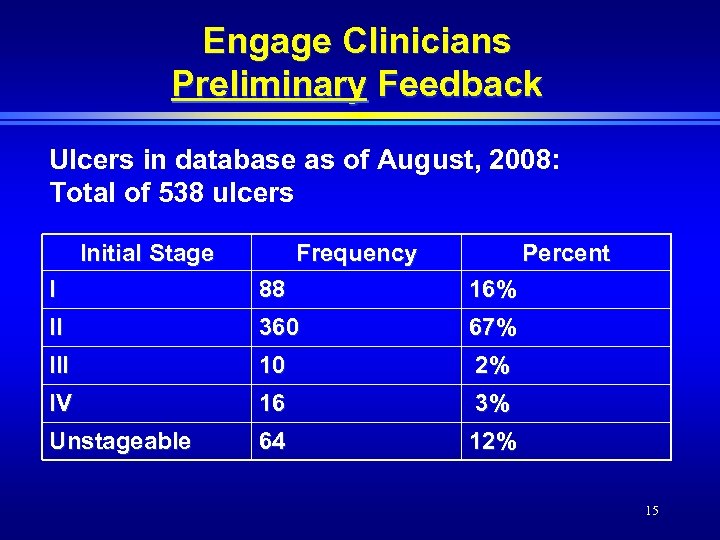 Engage Clinicians Preliminary Feedback Ulcers in database as of August, 2008: Total of 538 ulcers Initial Stage Frequency Percent I 88 16% II 360 67% III 10 2% IV 16 3% Unstageable 64 12% 15
Engage Clinicians Preliminary Feedback Ulcers in database as of August, 2008: Total of 538 ulcers Initial Stage Frequency Percent I 88 16% II 360 67% III 10 2% IV 16 3% Unstageable 64 12% 15
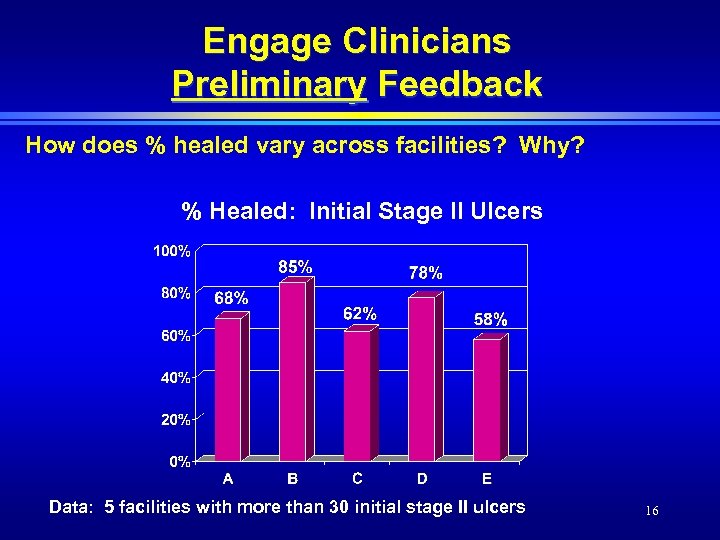 Engage Clinicians Preliminary Feedback How does % healed vary across facilities? Why? % Healed: Initial Stage II Ulcers Data: 5 facilities with more than 30 initial stage II ulcers 16
Engage Clinicians Preliminary Feedback How does % healed vary across facilities? Why? % Healed: Initial Stage II Ulcers Data: 5 facilities with more than 30 initial stage II ulcers 16
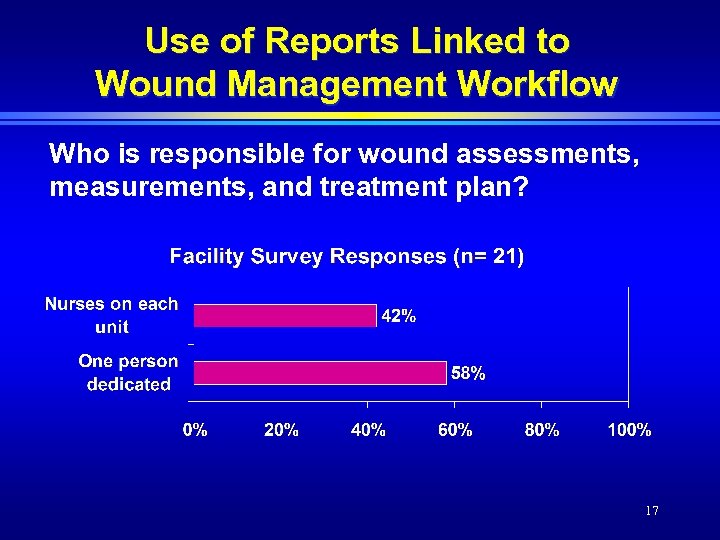 Use of Reports Linked to Wound Management Workflow Who is responsible for wound assessments, measurements, and treatment plan? 17
Use of Reports Linked to Wound Management Workflow Who is responsible for wound assessments, measurements, and treatment plan? 17
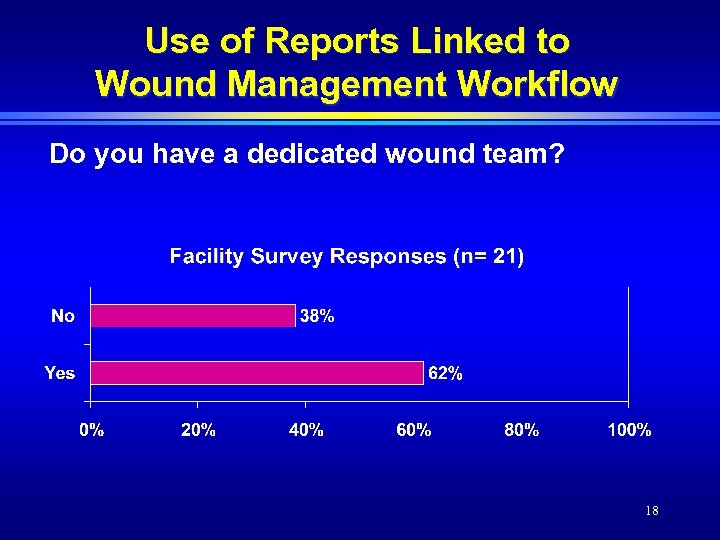 Use of Reports Linked to Wound Management Workflow Do you have a dedicated wound team? 18
Use of Reports Linked to Wound Management Workflow Do you have a dedicated wound team? 18
 Next Steps • Establish plan to use reports » Link reports with existing and new processes • Engage multiple disciplines, including rehab, dieticians, quality improvement team 19
Next Steps • Establish plan to use reports » Link reports with existing and new processes • Engage multiple disciplines, including rehab, dieticians, quality improvement team 19


