9696ef3741b445ef6a421a51161ad768.ppt
- Количество слайдов: 56

On Behalf of Baystate Medical Center and The Department of Surgery WELCOME!
Orientation Objectives v v Orient you to Baystate Medical Center Provide essential information and basic resources Clear expectations on vital issues Facilitate earliest possible effectiveness within the health care system
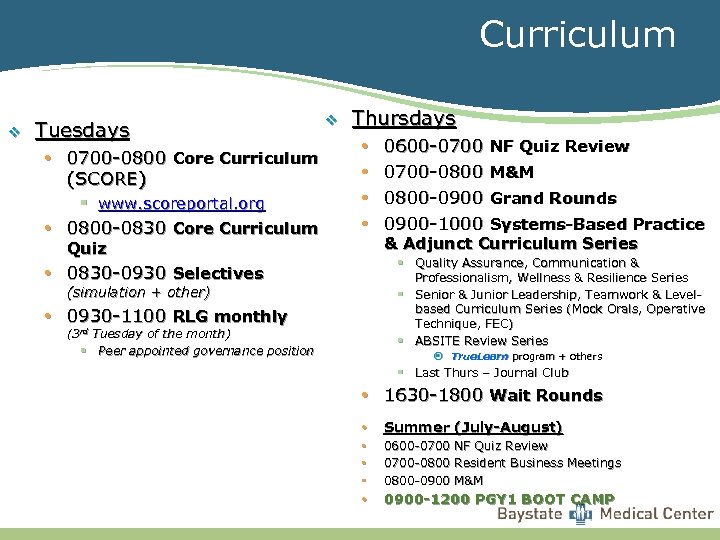
Curriculum v Tuesdays • 0700 -0800 Core Curriculum (SCORE) § www. scoreportal. org • 0800 -0830 Core Curriculum v Thursdays • • Quiz 0600 -0700 NF Quiz Review 0700 -0800 M&M 0800 -0900 Grand Rounds 0900 -1000 Systems-Based Practice & Adjunct Curriculum Series § Quality Assurance, Communication & Professionalism, Wellness & Resilience Series § Senior & Junior Leadership, Teamwork & Levelbased Curriculum Series (Mock Orals, Operative Technique, FEC) § ABSITE Review Series • 0830 -0930 Selectives (simulation + other) • 0930 -1100 RLG monthly (3 rd Tuesday of the month) § Peer appointed governance position ¤ True. Learn program + others § Last Thurs – Journal Club • 1630 -1800 Wait Rounds • Summer (July-August) • • • 0600 -0700 NF Quiz Review 0700 -0800 Resident Business Meetings 0800 -0900 M&M • 0900 -1200 PGY 1 BOOT CAMP
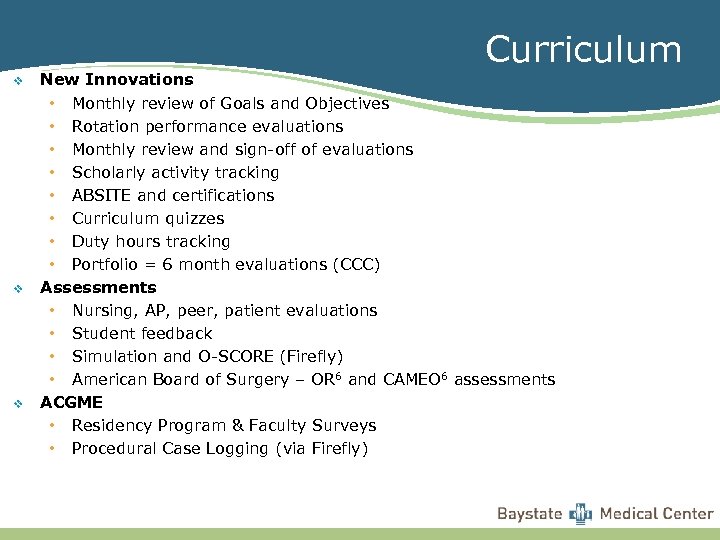
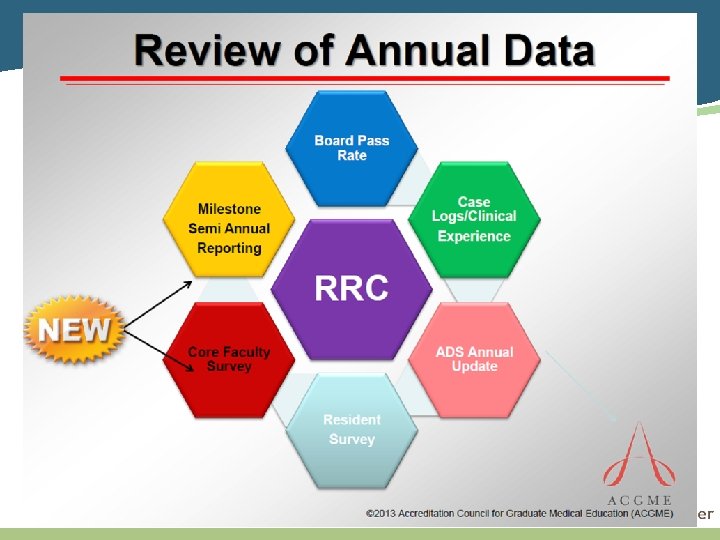
Curriculum v v v New Innovations • Monthly review of Goals and Objectives • Rotation performance evaluations • Monthly review and sign-off of evaluations • Scholarly activity tracking • ABSITE and certifications • Curriculum quizzes • Duty hours tracking • Portfolio = 6 month evaluations (CCC) Assessments • Nursing, AP, peer, patient evaluations • Student feedback • Simulation and O-SCORE (Firefly) • American Board of Surgery – OR 6 and CAMEO 6 assessments ACGME • Residency Program & Faculty Surveys • Procedural Case Logging (via Firefly)
Learning Responsibilities and Habits • Self-directed learning • Prepare for patient care, OR cases, Curriculum, M&Ms, Service rounds • SCORE & True. Learn • • ABSITE Learning Contracts Evaluation and feedback USMLE-3 • Mandatory pass during PG-2 year • • Teaching students and team members (RAT’s) Wellness (RAW)
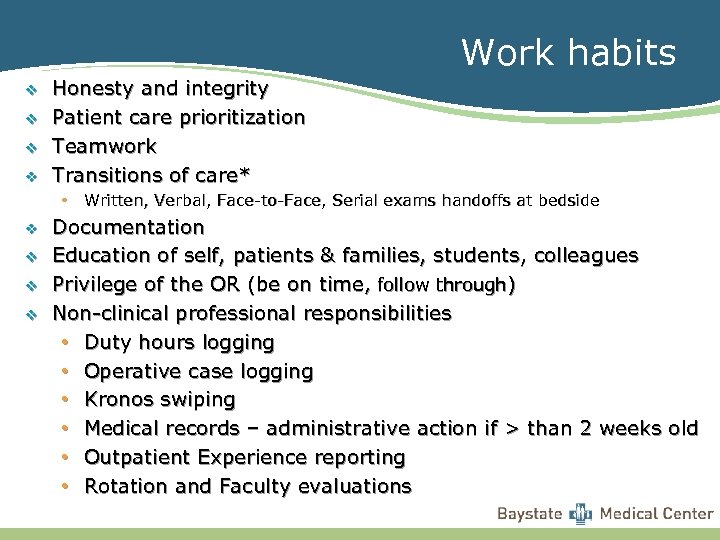
Work habits v v Honesty and integrity Patient care prioritization Teamwork Transitions of care* • Written, Verbal, Face-to-Face, Serial exams handoffs at bedside v v Documentation Education of self, patients & families, students, colleagues Privilege of the OR (be on time, follow through) Non-clinical professional responsibilities • Duty hours logging • Operative case logging • Kronos swiping • Medical records – administrative action if > than 2 weeks old • Outpatient Experience reporting • Rotation and Faculty evaluations
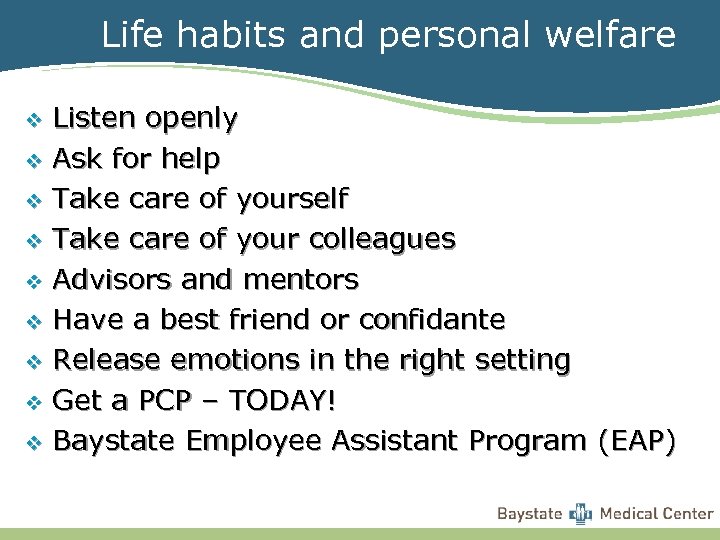
Life habits and personal welfare Listen openly v Ask for help v Take care of yourself v Take care of your colleagues v Advisors and mentors v Have a best friend or confidante v Release emotions in the right setting v Get a PCP – TODAY! v Baystate Employee Assistant Program (EAP) v
Baystate Medical Center Mission Statement Baystate Medical Center affirms its commitment to Graduate Medical Education by providing and maintaining the institutional infrastructure including: personnel, equipment, facilities and resources necessary to support an appropriate learning environment. The educational environment will foster professional and personal development by providing organized educational programs, appropriate guidance and supervision of all residents and fellows and outstanding, compassionate medical care.
The Accreditation Council for Graduate Medical Education (ACGME) v v A private professional organization Responsible for the accreditation of nearly 7, 800 residency education programs One of the largest private accrediting agencies in the country, if not the world Last visited on May 7 th, 2013: 10 year accreditation (with annual reporting and periodic CLER visits)
Institutional Responsibilities v Provide appropriate supervision/support v Ensure that work hours are in compliance with: • duty hour regulations and • educational goals v Work hours are consistent with: • educational needs • patient needs • continuity of care • accountability • supervision
Common Program Requirements VI. A, B & C v v v v Appear for duty appropriately rested and fit to provide the services required by patients Actively participate in interdisciplinary clinical quality improvement and patient safety programs Participation in effective transitions of care to facilitate continuity and patient safety Honestly and accurately report duty hours, patient outcomes, and clinical experience data Recognize impairment, including illness and fatigue, in themselves and in their peers Be familiar with alertness management and fatigue mitigation processes Employee Assistance Program (EAP)
Common Program Requirements Vl. D. , F v Know the limits of his/her scope of authority, and the circumstances under which he/she is permitted to act with conditional independence • PGY 1 supervision must be direct v Work as a member of effective interprofessional teams
Resident Responsibilities Common Program Requirements V. B, C v Submit to the program director at least annually confidential written evaluations of the faculty and program v Participate in surveys v Provide feedback!
The six general competencies are: v v v Patient Care Medical Knowledge System-based Practice-based Learning & Improvement Professionalism Interpersonal & Communication Skills
ACGME Core Competencies v Patient Care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health v Medical Knowledge about established and evolving biomedical, clinical, and cognate (e. g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care v Practice-Based Learning and Improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care v Interpersonal and Communication skills that result in effective information exchange and teaming with patients, their families, and other health professionals v Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population v Systems-Based Practice as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value
Academic Performance Actions v Individual Learning Plan (ILP) • Specific skills development • Learning contract (LC) Corrective Action Plan (CAP) v Academic Remediation v Academic Probation* v Employment action* v *Reportable to BORM
ACGME Duty Hours Regulations v Total Weekly Duty Hours • 80 per week average v Consecutive Hours + Post-Call Hours • 24 + 4 v Time Between Duty Periods – Daily • Should be 10 * v Time Between Duty Periods – Post-Call • Should be 14 * v Call Frequency • No more than 1 in 3 days on average v Days Off • 1 in 7 days on average v Minimize Handoffs/Transitions of Care v Supervision • Direct (by Seniors or Attendings) * modifiable for educational clinical experience continuity
ACGME Regulations v PGY-1 supervision must be DIRECT v Outpatient Clinic must attend 4 hours/week v v Transitions of care must be thorough and effective Patient privacy & confidentiality
HIPAA & Corporate Compliance v v v v You only may access Protected Health Information for patients if you need that information to do your job. Limit access to restricted areas Access for any other reason is prohibited and will result in termination. e. g. Chart Checks, Elevator Talk, Cafeteria Chat, Loss of Patient Lists or Stickers Service lists-printouts Locked blue bins only Passwords should NOT be shared Avoid logging onto other pagers & manipulating status
Professionalism v Timeliness (to rounds, OR, appointments, curriculum) v Respectful behavior with team members, consultants, students, patients & families v Verbal and written communications • (Avoid chart wars! These are medicolegal documents!) v Administrative responsibilities v Professional appearance • Baystate Health Appearance Standards
Documentation v Detailed, accurate and timely v No “Cut and Paste” v All medical records are legal documents • No note? ? ? Then you weren’t there. v No phone dictation of consults at PGY 1 level v Medical Records Department memos • Do NOT sign an order which you did NOT give
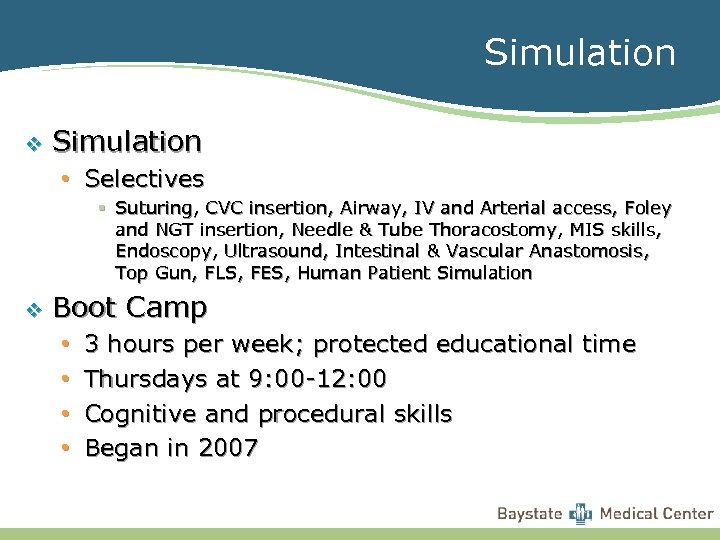
Simulation v Simulation • Selectives § Suturing, CVC insertion, Airway, IV and Arterial access, Foley and NGT insertion, Needle & Tube Thoracostomy, MIS skills, Endoscopy, Ultrasound, Intestinal & Vascular Anastomosis, Top Gun, FLS, FES, Human Patient Simulation v Boot Camp • • 3 hours per week; protected educational time Thursdays at 9: 00 -12: 00 Cognitive and procedural skills Began in 2007
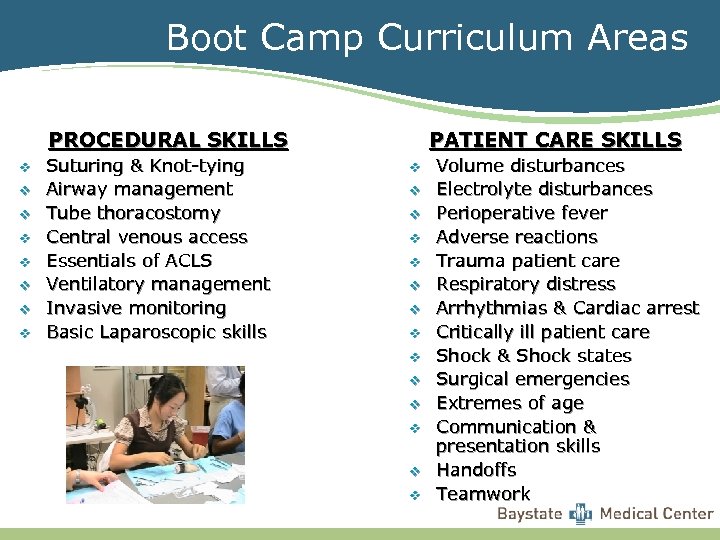
Boot Camp Curriculum Areas PROCEDURAL SKILLS v v v v Suturing & Knot-tying Airway management Tube thoracostomy Central venous access Essentials of ACLS Ventilatory management Invasive monitoring Basic Laparoscopic skills PATIENT CARE SKILLS v v v v Volume disturbances Electrolyte disturbances Perioperative fever Adverse reactions Trauma patient care Respiratory distress Arrhythmias & Cardiac arrest Critically ill patient care Shock & Shock states Surgical emergencies Extremes of age Communication & presentation skills Handoffs Teamwork
Other Important Items v IRB v TEG v Lifeimage LILA v Firefly
ACGME Surgery Milestones As the ACGME began to move toward continuous accreditation, specialty groups developed outcomes-based milestones as a framework for determining resident and fellow performance within the six ACGME Core Competencies. What are Milestones? Simply defined, a milestone is a significant point in development. For accreditation purposes, the Milestones are competency-based developmental outcomes (e. g. , knowledge, skills, attitudes, and performance) that can be demonstrated progressively by residents and fellows from the beginning of their education through graduation to the unsupervised practice of their specialties. What is a Milestone? Skill and knowledge-based developments that commonly occur by a specific time. Specific behaviors, attributes, or outcomes in the six general competency domains to be demonstrated by residents during residency

Milestones – cont’d Why Milestones? First and foremost, the Milestones are designed to help all residencies and fellowships produce highly competent physicians to meet the health and health care needs of the public. Milestones serve important purposes in program accreditation Allow for continuous monitoring of programs and lengthening of site visit cycles Public Accountability – report at a national level on aggregate competency outcomes by specialty Community of practice for evaluation and research, with focus on continuous improvement of graduate medical education For educational (residency/fellowship) programs, the Milestones will: Provide a rich descriptive, developmental framework for clinical competency committees Guide curriculum development of the residency or fellowship Support better assessment practices Enhance opportunities for early identification of struggling residents and fellows And for residents and fellows, the Milestones will: Provide more explicit and transparent expectations of performance Support better self-directed assessment and learning Facilitate better feedback for professional development How will the Milestones be used by the ACGME? Residents’/fellows' performance on the Milestones will become a source of specialty-specific data for the specialty Review Committees to use in assessing the quality of residency and fellowship programs and for facilitating improvements to program curricula and resident performance if and when needed. The Milestones will also be used by the ACGME to demonstrate accountability of the effectiveness of graduate medical education within ACGMEaccredited programs in meeting the needs of the public.
What is CLER? Clinical Learning Environment Review (CLER) the ACGME has established the CLER program to assess the graduate medical education (GME) learning environment of each sponsoring institution and its participating sites. CLER emphasizes the responsibility of the sponsoring institution for the quality and safety of the environment for learning and patient care, a key dimension of the 2011 ACGME Common Program Requirements. The intent of CLER is “to generate national data on program and institutional attributes that have a salutary effect on quality and safety in settings where residents learn and on the quality of care rendered after graduation. ” 1 CLER provides frequent on-site sampling of the learning environment that will: increase the educational emphasis on patient safety demanded by the public; and, provide opportunity for sponsoring institutions to demonstrate leadership in patient safety, quality improvement, and reduction in health care disparities The CLER program’s ultimate goal is to move from a major targeted focus on duty hours to that of broader focus on the GME learning environment and how it can deliver both high-quality physicians and higher quality, safer, patient care. In its initial phase, CLER data will not be used in accreditation decisions by the Institutional Review Committee (IRC). CLER consists of three related activities: The CLER site visit program is used solely for providing feedback, learning, and helping to establish baselines for sponsoring institutions, the Evaluation Committee, and the IRC. The first cycle of visit findings will result in dissemination of salutary practices by the Evaluation Committee. The CLER Evaluation Committee includes a broad cross-section of individuals with expertise related to the aim of the CLER program. The Committee provides input to the design and implementation of CLER site visit activities and conducts evaluation review of sponsoring institutions that are visited during each cycle. The ACGME recognizes the great interest by sponsoring institutions to support faculty development in those areas on which the CLER program will focus (e. g. , patient safety, health care quality, transitions of care, etc. ). Therefore, as part of the CLER program, the ACGME will develop a program to support faculty development.

CLER assesses sponsoring institutions in the following 6 focus areas Patient Safety – including opportunities for residents to report errors, unsafe conditions, and near misses, and to participate in inter-professional teams to promote and enhance safe care. Quality Improvement – including how sponsoring institutions engage residents in the use of data to improve systems of care, reduce health care disparities and improve patient outcomes. Transitions in Care – including how sponsoring institutions demonstrate effective standardization and oversight of transitions of care. Supervision – including how sponsoring institutions maintain and oversee policies of supervision concordant with ACGME requirements in an environment at both the institutional and program level that assures the absence of retribution. Duty Hours Oversight, Fatigue Management and Mitigation – including how sponsoring institutions: (i) demonstrate effective and meaningful oversight of duty hours across all residency programs institutionwide; (ii) design systems and provide settings that facilitate fatigue management and mitigation; and (iii) provide effective education of faculty members and residents in sleep, fatigue recognition, and fatigue mitigation. Professionalism—with regard to how sponsoring institutions educate for professionalism, monitor behavior on the part of residents and faculty and respond to issues concerning: (i) accurate reporting of program information; (ii) integrity in fulfilling educational and professional responsibilities; and (iii) veracity in scholarly pursuits.
The initial round of CLER evaluations will seek answers to the following central questions: Who and what form the infrastructure of a Sponsoring Institution’s clinical learning environment? What organizational structures and administrative and clinical processes do the SI and its major participating sites have in place to support GME learning in each of the six focus areas? How integrated is the GME leadership and faculty within the SI’s current clinical learning environment infrastructure? What is the role of GME leadership and faculty to support resident and fellow learning in each of the six areas? How engaged are the residents and fellows in using the SI’s current clinical learning environment infrastructure? How comprehensive is the involvement of residents and fellows in using these structures and processes to support their learning in each of the six areas? How does the SI determine the success of its efforts to integrate GME into the quality infrastructure? From the perspective of the SI and its major participating sites, what are the measures of success in using this infrastructure and what was the level of success? What areas have the Sponsoring Institution identified as opportunities for improvement? From the perspective of the SI and its major participating sites (if different), what are seen as the opportunities for improving the quality and value of the current clinical learning environment infrastructure to support the six focus areas? 1 Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system--rationale and benefits. N Engl J Med. 2012; 366(11): 1051 -1056. [Epub 2012 Feb 22. ] 06/10/2012 Ver. 1. 0
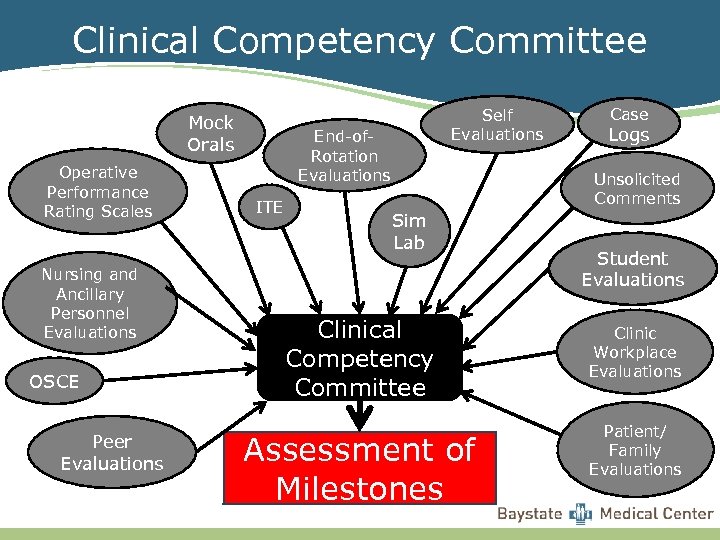
Clinical Competency Committee Mock Orals Operative Performance Rating Scales Nursing and Ancillary Personnel Evaluations OSCE Peer Evaluations Self Evaluations End-of. Rotation Evaluations ITE Case Logs Unsolicited Comments Sim Lab Clinical Competency Committee Assessment of Milestones Student Evaluations Clinic Workplace Evaluations Patient/ Family Evaluations
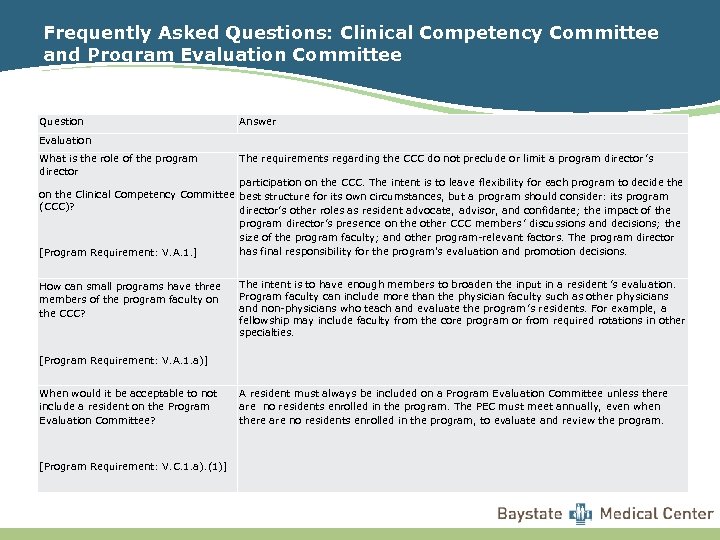
Frequently Asked Questions: Clinical Competency Committee and Program Evaluation Committee Question Answer Evaluation What is the role of the program director The requirements regarding the CCC do not preclude or limit a program director ’s participation on the CCC. The intent is to leave flexibility for each program to decide the on the Clinical Competency Committee best structure for its own circumstances, but a program should consider: its program (CCC)? director’s other roles as resident advocate, advisor, and confidante; the impact of the [Program Requirement: V. A. 1. ] How can small programs have three members of the program faculty on the CCC? program director’s presence on the other CCC members ’ discussions and decisions; the size of the program faculty; and other program-relevant factors. The program director has final responsibility for the program's evaluation and promotion decisions. The intent is to have enough members to broaden the input in a resident ’s evaluation. Program faculty can include more than the physician faculty such as other physicians and non-physicians who teach and evaluate the program ’s residents. For example, a fellowship may include faculty from the core program or from required rotations in other specialties. [Program Requirement: V. A. 1. a)] When would it be acceptable to not include a resident on the Program Evaluation Committee? [Program Requirement: V. C. 1. a). (1)] A resident must always be included on a Program Evaluation Committee unless there are no residents enrolled in the program. The PEC must meet annually, even when there are no residents enrolled in the program, to evaluate and review the program.
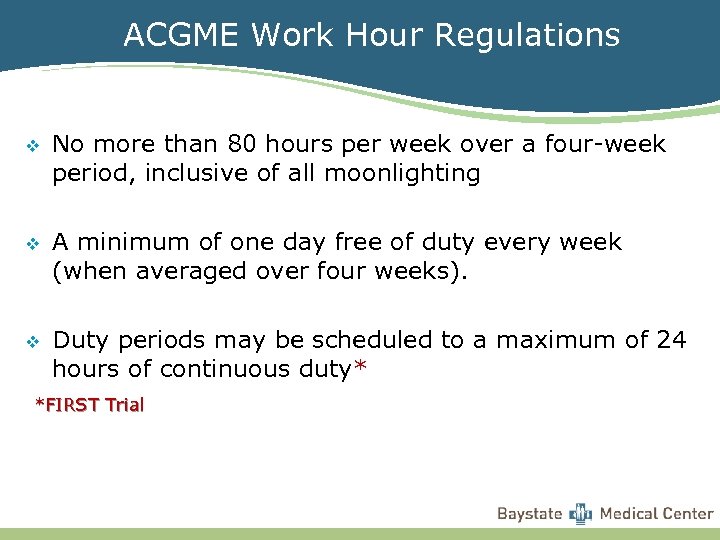
ACGME Work Hour Regulations v No more than 80 hours per week over a four-week period, inclusive of all moonlighting v A minimum of one day free of duty every week (when averaged over four weeks). v Duty periods may be scheduled to a maximum of 24 hours of continuous duty* *FIRST Trial
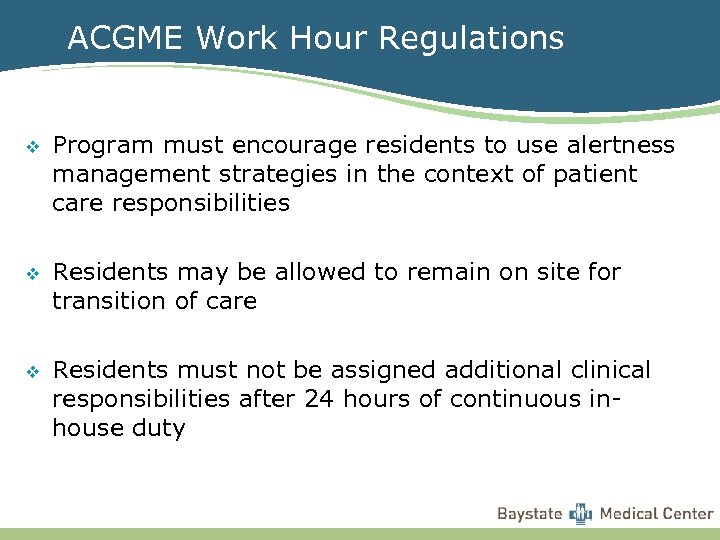
ACGME Work Hour Regulations v Program must encourage residents to use alertness management strategies in the context of patient care responsibilities v Residents may be allowed to remain on site for transition of care v Residents must not be assigned additional clinical responsibilities after 24 hours of continuous inhouse duty
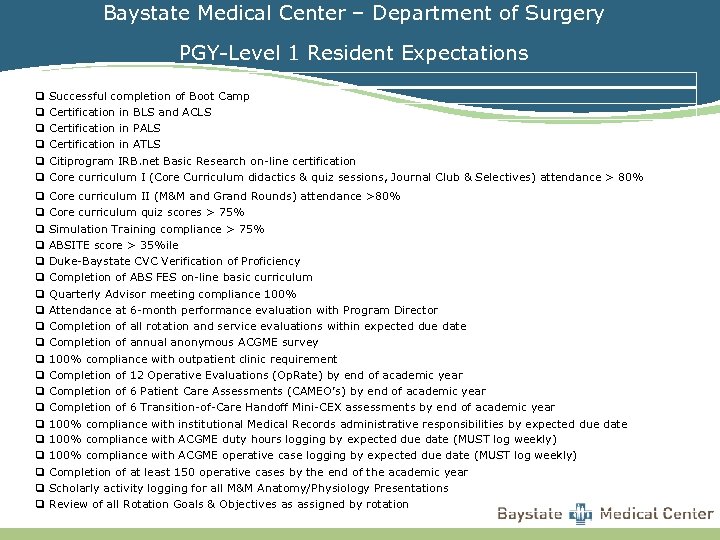
Baystate Medical Center – Department of Surgery PGY-Level 1 Resident Expectations q Successful completion of Boot Camp q Certification in BLS and ACLS q Certification in PALS q Certification in ATLS q Citiprogram IRB. net Basic Research on-line certification q Core curriculum I (Core Curriculum didactics & quiz sessions, Journal Club & Selectives) attendance > 80% q Core curriculum II (M&M and Grand Rounds) attendance >80% q Core curriculum quiz scores > 75% q Simulation Training compliance > 75% q ABSITE score > 35%ile q Duke-Baystate CVC Verification of Proficiency q Completion of ABS FES on-line basic curriculum q Quarterly Advisor meeting compliance 100% q Attendance at 6 -month performance evaluation with Program Director q Completion of all rotation and service evaluations within expected due date q Completion of annual anonymous ACGME survey q 100% compliance with outpatient clinic requirement q Completion of 12 Operative Evaluations (Op. Rate) by end of academic year q Completion of 6 Patient Care Assessments (CAMEO’s) by end of academic year q Completion of 6 Transition-of-Care Handoff Mini-CEX assessments by end of academic year q 100% compliance with institutional Medical Records administrative responsibilities by expected due date q 100% compliance with ACGME duty hours logging by expected due date (MUST log weekly) q 100% compliance with ACGME operative case logging by expected due date (MUST log weekly) q Completion of at least 150 operative cases by the end of the academic year q Scholarly activity logging for all M&M Anatomy/Physiology Presentations q Review of all Rotation Goals & Objectives as assigned by rotation
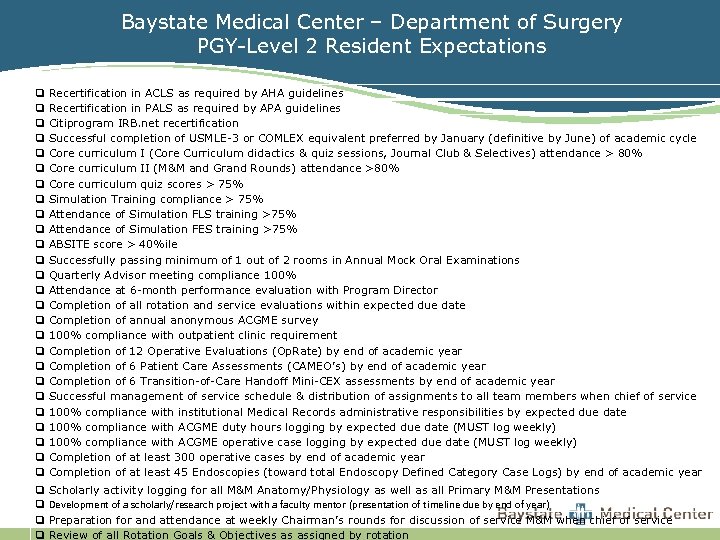
Baystate Medical Center – Department of Surgery PGY-Level 2 Resident Expectations q Recertification in ACLS as required by AHA guidelines q Recertification in PALS as required by APA guidelines q Citiprogram IRB. net recertification q Successful completion of USMLE-3 or COMLEX equivalent preferred by January (definitive by June) of academic cycle q Core curriculum I (Core Curriculum didactics & quiz sessions, Journal Club & Selectives) attendance > 80% q Core curriculum II (M&M and Grand Rounds) attendance >80% q Core curriculum quiz scores > 75% q Simulation Training compliance > 75% q Attendance of Simulation FLS training >75% q Attendance of Simulation FES training >75% q ABSITE score > 40%ile q Successfully passing minimum of 1 out of 2 rooms in Annual Mock Oral Examinations q Quarterly Advisor meeting compliance 100% q Attendance at 6 -month performance evaluation with Program Director q Completion of all rotation and service evaluations within expected due date q Completion of annual anonymous ACGME survey q 100% compliance with outpatient clinic requirement q Completion of 12 Operative Evaluations (Op. Rate) by end of academic year q Completion of 6 Patient Care Assessments (CAMEO’s) by end of academic year q Completion of 6 Transition-of-Care Handoff Mini-CEX assessments by end of academic year q Successful management of service schedule & distribution of assignments to all team members when chief of service q 100% compliance with institutional Medical Records administrative responsibilities by expected due date q 100% compliance with ACGME duty hours logging by expected due date (MUST log weekly) q 100% compliance with ACGME operative case logging by expected due date (MUST log weekly) q Completion of at least 300 operative cases by end of academic year q Completion of at least 45 Endoscopies (toward total Endoscopy Defined Category Case Logs) by end of academic year q Scholarly activity logging for all M&M Anatomy/Physiology as well as all Primary M&M Presentations q Development of a scholarly/research project with a faculty mentor (presentation of timeline due by end of year) q Preparation for and attendance at weekly Chairman’s rounds for discussion of service M&M when chief of service q Review of all Rotation Goals & Objectives as assigned by rotation
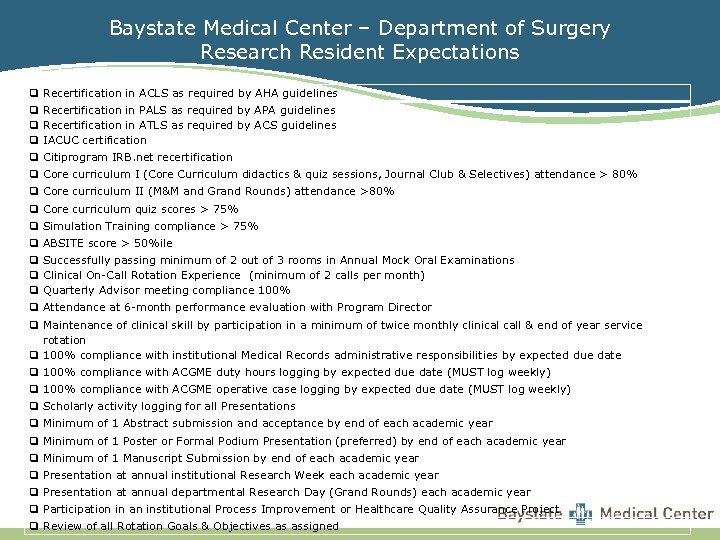
Baystate Medical Center – Department of Surgery Research Resident Expectations q Recertification in ACLS as required by AHA guidelines q Recertification in PALS as required by APA guidelines q Recertification in ATLS as required by ACS guidelines q IACUC certification q Citiprogram IRB. net recertification q Core curriculum I (Core Curriculum didactics & quiz sessions, Journal Club & Selectives) attendance > 80% q Core curriculum II (M&M and Grand Rounds) attendance >80% q Core curriculum quiz scores > 75% q Simulation Training compliance > 75% q ABSITE score > 50%ile q Successfully passing minimum of 2 out of 3 rooms in Annual Mock Oral Examinations q Clinical On-Call Rotation Experience (minimum of 2 calls per month) q Quarterly Advisor meeting compliance 100% q Attendance at 6 -month performance evaluation with Program Director q Maintenance of clinical skill by participation in a minimum of twice monthly clinical call & end of year service rotation q 100% compliance with institutional Medical Records administrative responsibilities by expected due date q 100% compliance with ACGME duty hours logging by expected due date (MUST log weekly) q 100% compliance with ACGME operative case logging by expected due date (MUST log weekly) q Scholarly activity logging for all Presentations q Minimum of 1 Abstract submission and acceptance by end of each academic year q Minimum of 1 Poster or Formal Podium Presentation (preferred) by end of each academic year q Minimum of 1 Manuscript Submission by end of each academic year q Presentation at annual institutional Research Week each academic year q Presentation at annual departmental Research Day (Grand Rounds) each academic year q Participation in an institutional Process Improvement or Healthcare Quality Assurance Project q Review of all Rotation Goals & Objectives as assigned
Scholarly Activity Research v Case reports v Quality Assurance & Process Improvement v Mentors v Department of Surgery Research Office v Academic Research Week v Regional and National Conferences v
Schedules Rotation assignments v Vacation v Certifications and exams not allowed on the following services: v • SICU, NF, Chief of Service Call Schedule generally not modifiable v Special requests must be approved one month in advance (Gold Chief, Service Chief and Administration) v
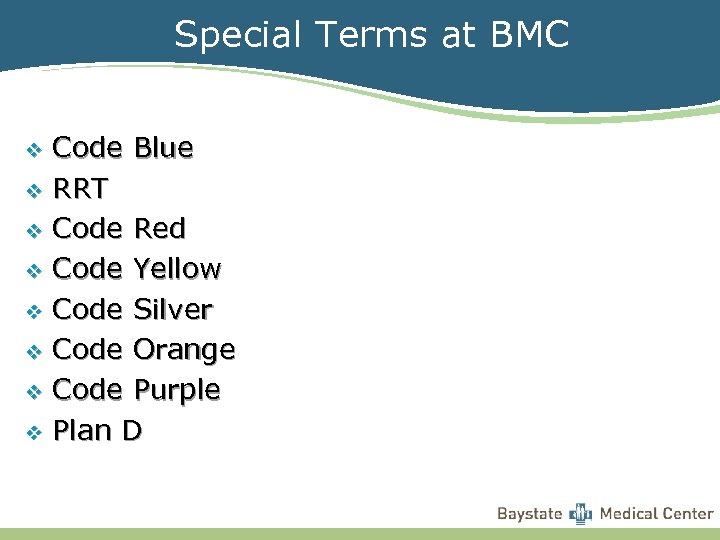
Special Terms at BMC Code Blue v RRT v Code Red v Code Yellow v Code Silver v Code Orange v Code Purple v Plan D v
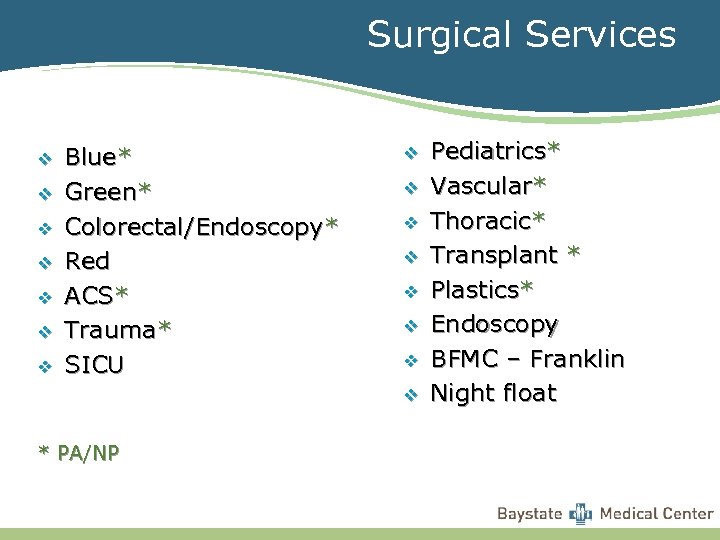
Surgical Services v v v v Blue* Green* Colorectal/Endoscopy* Red ACS* Trauma* SICU v v v v * PA/NP Pediatrics* Vascular* Thoracic* Transplant * Plastics* Endoscopy BFMC – Franklin Night float
Advisors Quarterly Meetings v Documented – Advisor Note worksheet v Mandatory v
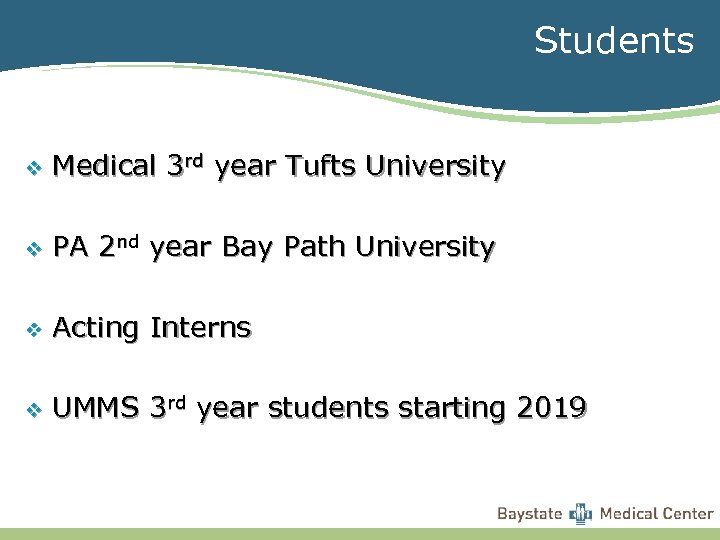
Students v Medical 3 rd year Tufts University v PA 2 nd year Bay Path University v Acting Interns v UMMS 3 rd year students starting 2019
Important Items v Lockers – will be assigned and available Monday v ID Badge – $100 per mo. meal allotment v Pagers – log in and out v Kronos – swipe in daily (green slip if missed)
Video taping v Cortext only for images No video recording v Patients and families recording you v • “I am not comfortable and have not consented to being recorded. I am happy to share information with you but do not consent to recording. ”
Pagers v Personal pager blocking and unblocking v Service pagers can NOT be blocked
Teaching Responsibilities v Team members v Nurses and ancillary care providers v Patients v Students (medical, PA)
BE A TEAM PLAYER You are in the trenches with your fellow interns and residents. So take care of each other. You will carry each other through residency. Do not dump your work on others, and be willing to help each other even if it isn't your problem. Do NOT try to take cases away from a fellow intern or scut them out. Remember: we don’t get much free time. Prioritize your colleagues – they will be much more willing to do you a favor if you have already done for them.
OWN YOUR EDUCATION While much of your time as an intern will be spent gathering information and passing it along to others, always remember that your primary reason for being here is to learn to be an outstanding physician and surgeon. Therefore, always keep in mind that you (yes, YOU) can use the information you gather to make decisions and formulate plans for your patients. In other words, synthesize those vitals with your physical exam, lab values and x-rays and all of a sudden, it is clear what is wrong with your patient and what you need to do. Then, when informing your chief about a patient's recent deterioration, instead of rambling off a load of digits and then pausing for a response, you can state what you think is going on and what you want to do about it. Also remember that what on the surface appears as "scut" is often an educational opportunity. Your practice in surgery begins now.
PLAY NICE WITH OTHERS Every year, interns get into trouble with nurses and ancillary staff for behavior that they perceive as disrespectful. People will address you as “Doctor, ” then ask you to perform duties that are beneath your level of education, training and dignity. At times what you are asked to do is frustrating, demeaning and belittling. Remember that respect breeds respect. So, rather than yell at the nurse who calls you at 03: 00 to tell you that a patient wants to resume her birth control pills, just say, "I'll take care of it, " and move on to the next page. Getting mad wastes your energy. Worse, you will soon acquire a reputation among the nurses for being a Big Pompous Jerk (BPJ). And there are those among the nursing staff who delight in calling Big Pompous Jerk all night and torturing them with trivia. If you must do something to reclaim your sanity when paged with yet another ridiculous request, reciprocate by creating more work for the perpetrator. Ask them for up-to-date vitals, orthostatics, and In ’s & Out’s; make them work for that midnight Simethicone.
In contrast, if you treat everyone gently and correctly, someday, someone will remember who you are, and they will go out of their way to do nice things for you. They will feed you late at night, your STAT labs will get drawn super STAT, and people will smile at you and thank you. They might even throw you a farewell party at the end of your rotation (yes, it has happened). v. Remember, most nurses have been here a lot longer than you and what they say about you to the faculty can carry a lot of weight. More importantly, they can really help you too. We all get angry and lose it sometimes. Just remember that we are all working together as a team to deliver the best patient care possible. v. Good manners also extend to fellow interns and residents, perhaps more so than anyone else. The medical world is small—everyone knows everyone and institutional memories are long. Remember that "please, " and "thank you, " always go a long way.
BE PREPARED You are expected to gather the vitals and In’s & Out’s prior to morning and afternoon team rounds, and make sure that they are correct, despite what careconnect spits out. You need to be prepared for afternoon rounds, i. e. follow up on what was ordered in the morning. You need to follow up on studies & consult recommendations prior to afternoon rounds. Did the patient eat okay? Did he urinate after the Foley was removed? Did he respond to fluid boluses? And so on. Prepare for afternoon rounds just like you prepare for morning rounds. If you changed diet orders on a patient at 7 am, by the time you round again at 4: 30 pm, you should know whether the patient tolerated his or her diet. You should know your patients better than anyone else on your service. You are expected to know not only their post-op/hospital day, diet, and antibiotics, but also their current medications and labs. When you complete your morning tasks, go through each of your patients to check their medication lists, make sure they are on their home medications (if applicable), check if any new culture results are available, check the final radiology reads for radiographic studies that you’ve reviewed as a team (CXRs), and read consult notes from other services.
BE PREPARED – cont’d Be organized: You do not need to memorize everything, but you should have your way of keep track of all patient information. Your system can be your own, as long as it works. v. If you know ahead of time you will be operating, review the patient’s history, labs and imaging. Know what operation you are doing, review the relevant anatomy and know how the operation is done. The goal is to be as prepared as possible and to always do what’s best for the patient and demonstrate that you care. The priority is to mention the key facts and be succinct.
BE EFFICIENT Learn to prioritize and multi-task. Some things are not important, while others are life-and-death. For example, you should probably check the CXR on the patient with the decreasing O 2 sats before you take the staples out of Mr. Bill's abdominal incision. It will take some time, but these things become clear. Also, it is important to take care of tasks early if they require follow-up. Ordering a CXR after writing all of your notes does not make much sense. Figure out how to arrange your work so that there are other tasks to do while waiting for results. The following list is a reasonable order for conducting your work. Group tasks together, so you don't have to go back to do things. In general, your priorities should be: 1. Discharges, 2. Same day studies/consults, 3. Notes, routine patient care, dictations, 4. Logs
SCUT! The Art of Prioritizing One of the most important skills you will develop this year is the ability to prioritize: 1. Consults 2. Radiology Studies 3. Discharges (goal to have patients discharged before 10 am) 4. Labs/other routine orders 5. Administrative responsibilities
READING There will be time to read and read you must v Doctors must be in large part self-taught v None of us could have come so far without the ability to direct our own learning v Read a little each day. Try to read for at least 15 minutes during the day, and do this while at the hospital (between cases, while waiting for studies, any free time). v
9696ef3741b445ef6a421a51161ad768.ppt