de0490dbff879f41f2ce8e33b83c4622.ppt
- Количество слайдов: 73
Obstructive Sleep Apnea Established and Emerging Treatment Options Dragos Manta, MD Assistant Professor of Medicine Division of Pulmonary, Critical Care and Sleep Medicine
Objectives • Review patho-physiologic mechanisms of obstructive sleep apnea (OSA) • Review the established positive airway pressure, oral appliance and surgical therapy options • Review emerging therapy options
Why OSA? • OSA is the second most common sleep-related breathing disorder after primary snoring. • Prevalence in general populations – up to 9% in women – up to 24% in men • Prevalence of symptomatic OSA – 1 -5% in women – 3 -8% in men
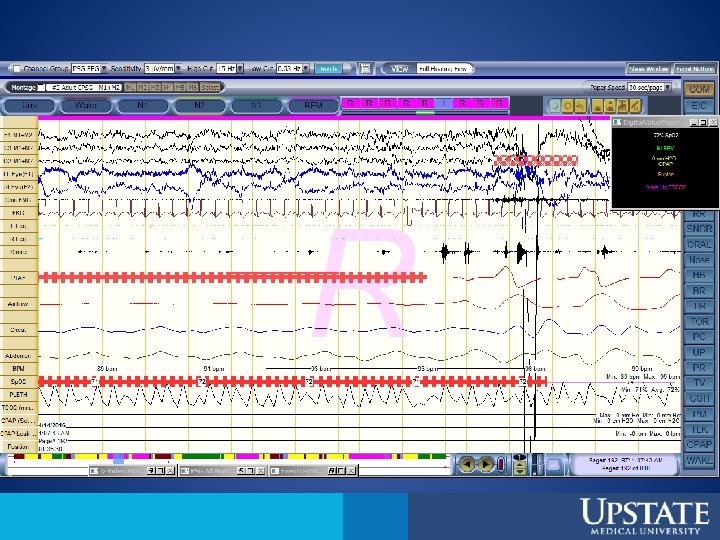
International Classification of Sleep Disorders – 3 rd Edition (ICSD-3) • OSA is characterized by repetitive episodes of complete (apnea) or partial (hypopnea) upper airway obstruction occurring during sleep. • Sleep testing is required for diagnosis – 15 or more predominantly obstructive events per hour of sleep in a asymptomatic patient – 5 or more predominantly obstructive events per hour of sleep in a patient with sleep symptoms or co-morbidities
Risk Factors • Obesity • Upper Airway Size • Sedentary Behavior
Obesity • The single most important risk factor in OSA in middle-age adults • 70% of OSA patients are obese • In a large cohort of adults undergoing bariatric surgery, 80% had OSA (Khan A et al. JCSM. 2013; 9(1): 21 -29) OSA Obesity
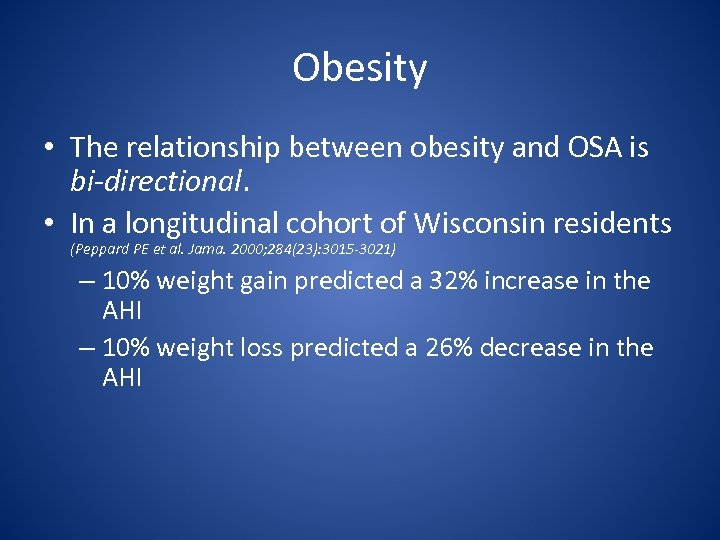
Obesity • The relationship between obesity and OSA is bi-directional. • In a longitudinal cohort of Wisconsin residents (Peppard PE et al. Jama. 2000; 284(23): 3015 -3021) – 10% weight gain predicted a 32% increase in the AHI – 10% weight loss predicted a 26% decrease in the AHI
Obesity • Mediators – Increased neck circumference • Men>17 inches • Women >16 inches – Fat deposition in the tongue – Decreased “tracheal tug” due to decreased functional residual capacity (FRC) (Gifford AH et al. CHEST 2010; 138( 3 ): 704 – 715)
Upper Airway (UAW) Size • The upper airway size of OSA patient is smaller, particularly lateral dimensions – – Heritable factors Developmental Inflammatory Obesity
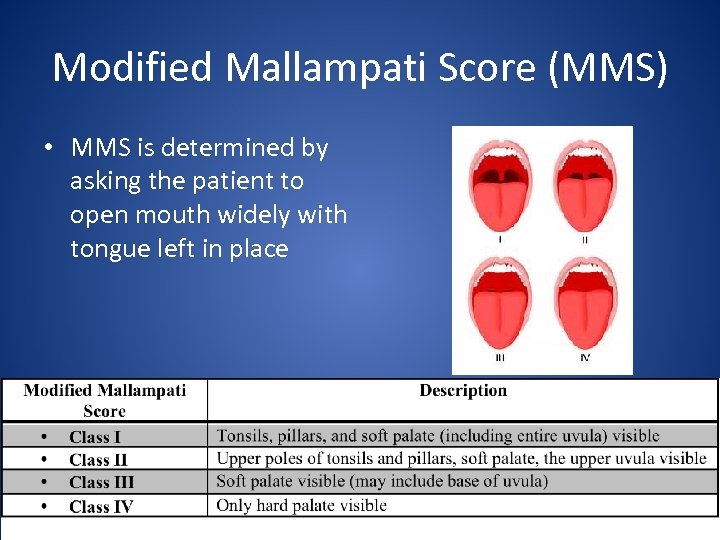
Modified Mallampati Score (MMS) • MMS is determined by asking the patient to open mouth widely with tongue left in place
Other Signs of a Small UAW • • Tongue volume is higher (lateral dental imprints) High arched palate Tonsillar/adenoid hypertrophy Small retrognathic mandible
Upper Airway Abnormalities • Craniofacial syndromes (like Pierre Robin Syndrome) • Soft tissue abnormalities – Increased tongue size ( Down syndrome) – Upper airway tumors
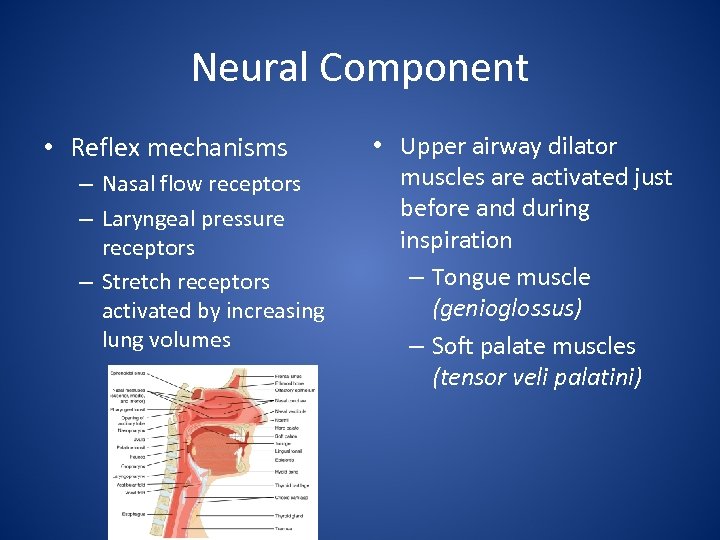
Neural Component • Reflex mechanisms – Nasal flow receptors – Laryngeal pressure receptors – Stretch receptors activated by increasing lung volumes • Upper airway dilator muscles are activated just before and during inspiration – Tongue muscle (genioglossus) – Soft palate muscles (tensor veli palatini)
Pcrit= Critical UAW Pressure • Concept encompasses both passive and active characteristics of the upper airway • Intra-luminal upper airway pressure is subatmospheric during each inspiratory effort • Pcrit= transmural pressure at which the airway collapses
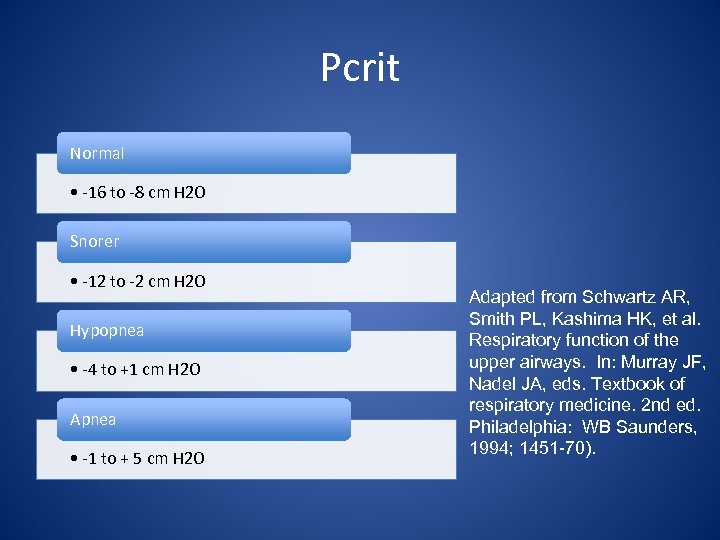
Pcrit Normal • -16 to -8 cm H 2 O Snorer • -12 to -2 cm H 2 O Hypopnea • -4 to +1 cm H 2 O Apnea • -1 to + 5 cm H 2 O Adapted from Schwartz AR, Smith PL, Kashima HK, et al. Respiratory function of the upper airways. In: Murray JF, Nadel JA, eds. Textbook of respiratory medicine. 2 nd ed. Philadelphia: WB Saunders, 1994; 1451 -70).
Fluid Shifts at Night • Observational study of 23 non-obese male subjects referred for evaluation for sleep apnea • Decrease in leg fluid volume at night correlates positively – neck circumference – AHI – a sedentary behavior during the day
Major Pathophysiologic Mechanisms of OSA • Sleep fragmentation causes lighter sleep • Excessive daytime sleepiness • When associated with inability to wake up • Increased risk of postoperative complications • Repetitive arousals/ epinephrine bursts/ cyclical deoxygenation/ reoxygenation (repetitive ischemia/reperfusion) • • Hypertension Cardio- and cerebro-vascular disease Insulin resistance and diabetes Increase mortality
Mortality • Untreated OSA is associated with increased mortality – Largely in patients with severe OSA – Independent of sleepiness in patients with severe OSA • Driven mostly by increased mortality in those younger than 65
Diagnosis • Subjective clinical impression that OSA is likely present has a sensitivity of 60% and specificity 63%. (Hoffstein V, et al. Sleep. 1993; 16(2): 118 -122) • Nocturnal pulse oximetry lacks sufficient sensitivity and specificity for diagnosis (Gyulay S et al. The Am rev of res dis. 1993; 147(1): 50 -53) • Attended Polysomnogram • Ambulatory testing or un-attended portable monitors
Treatment of OSA • • • PAP (positive airway pressure) Oral Appliances Surgery Adjunctive therapies Emerging therapies
PAP • Most efficacious option • Continuous PAP (or CPAP) is most commonly prescribed • Acts as a “pneumatic splint” splinting the upper airway and preventing airway collapse during sleep. • Improves PSG (AHI, etc. ) • Improves quality of life , daytime sleepiness • Improves hypertension control • Improves glycemic control in patients with diabetes
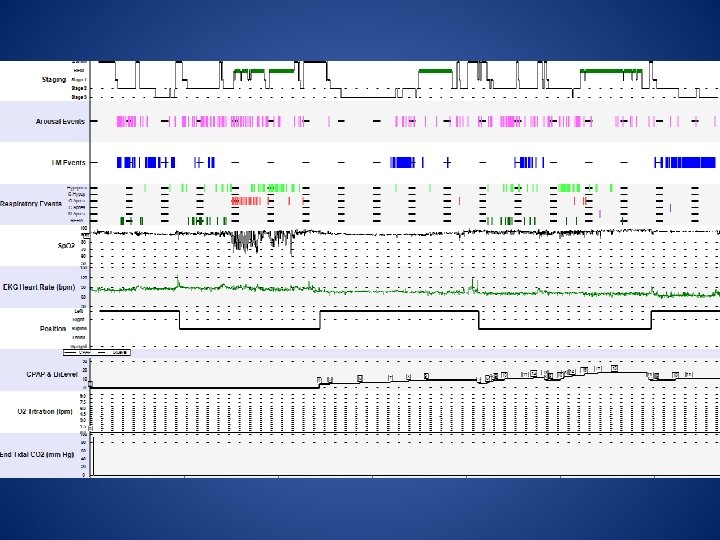
PAP Prescription • Titration during monitored overnight PSG • Auto-CPAP trial
CPAP pressure • • Severity of OSA Body position Weight Sleep stage ( N 2 and REM sleep require highest pressures)
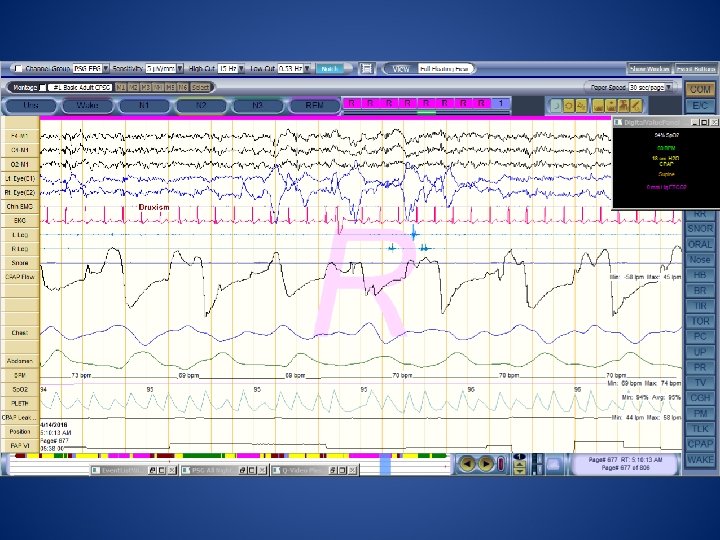
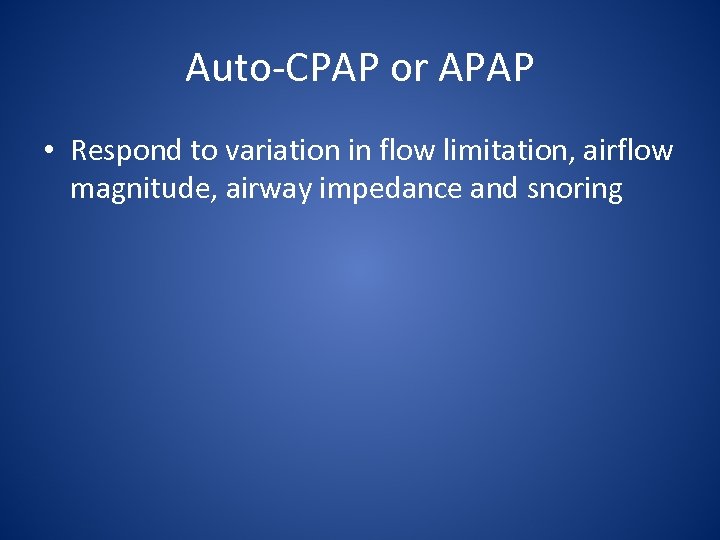
Auto-CPAP or APAP • Respond to variation in flow limitation, airflow magnitude, airway impedance and snoring
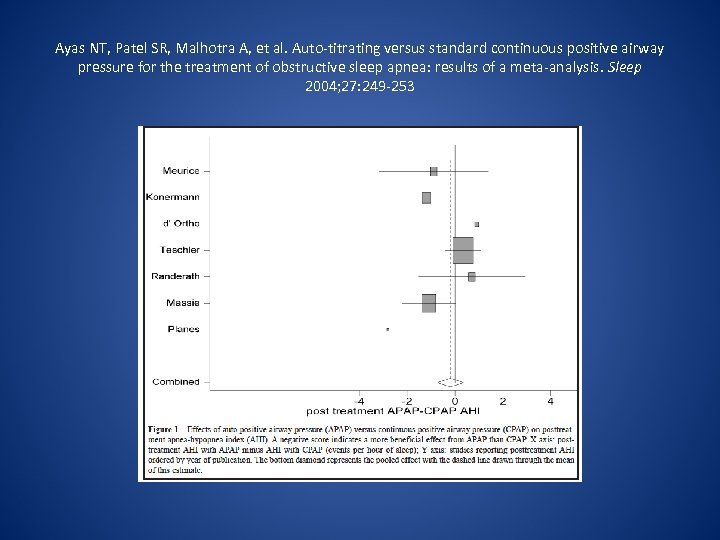
Ayas NT, Patel SR, Malhotra A, et al. Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep 2004; 27: 249 -253
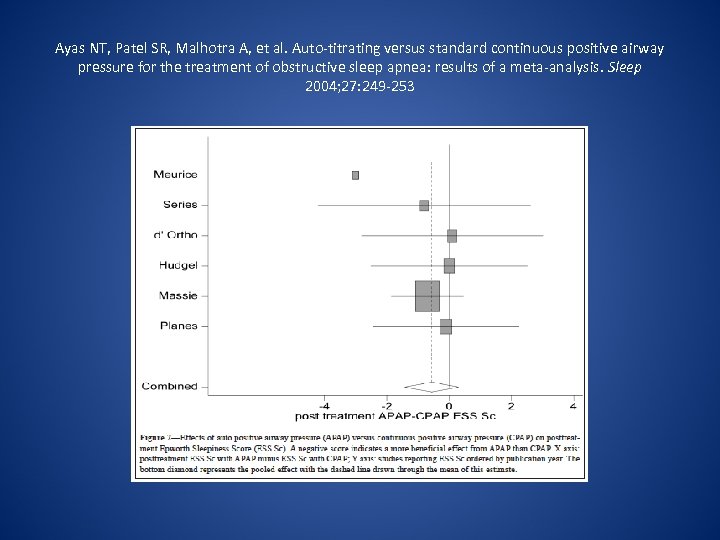
Ayas NT, Patel SR, Malhotra A, et al. Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep 2004; 27: 249 -253
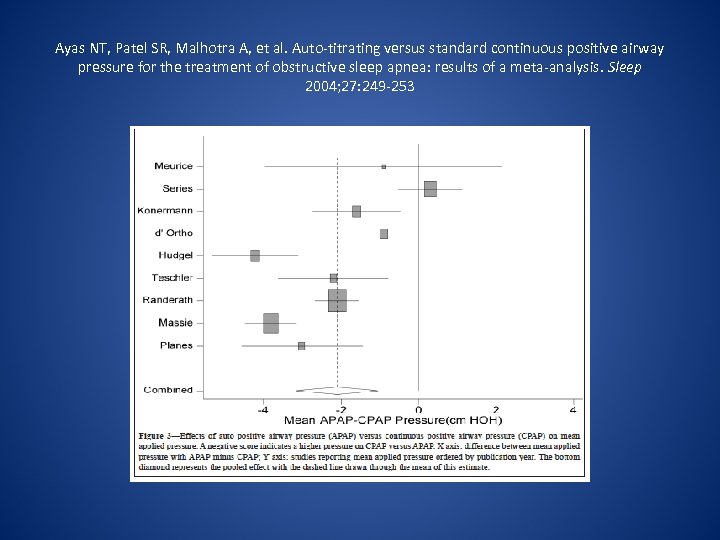
Ayas NT, Patel SR, Malhotra A, et al. Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep 2004; 27: 249 -253
Auto-CPAP for Failed Fixed CPAP • For high pressure intolerance • For OSA concentrated by – sleep stage (N 2, REM) – position (supine)
Morgenthaler TI et al. Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep. 2008; 31(1): 141 -147. • Certain APAP devices may be initiated and used in the self-adjusting mode for unattended treatment of patients with moderate to severe OSA without significant comorbidities (Option)
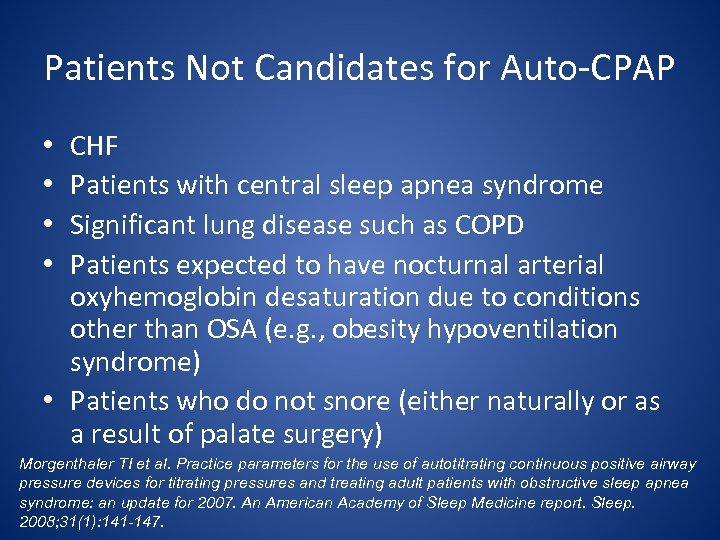
Patients Not Candidates for Auto-CPAP CHF Patients with central sleep apnea syndrome Significant lung disease such as COPD Patients expected to have nocturnal arterial oxyhemoglobin desaturation due to conditions other than OSA (e. g. , obesity hypoventilation syndrome) • Patients who do not snore (either naturally or as a result of palate surgery) • • Morgenthaler TI et al. Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep. 2008; 31(1): 141 -147.
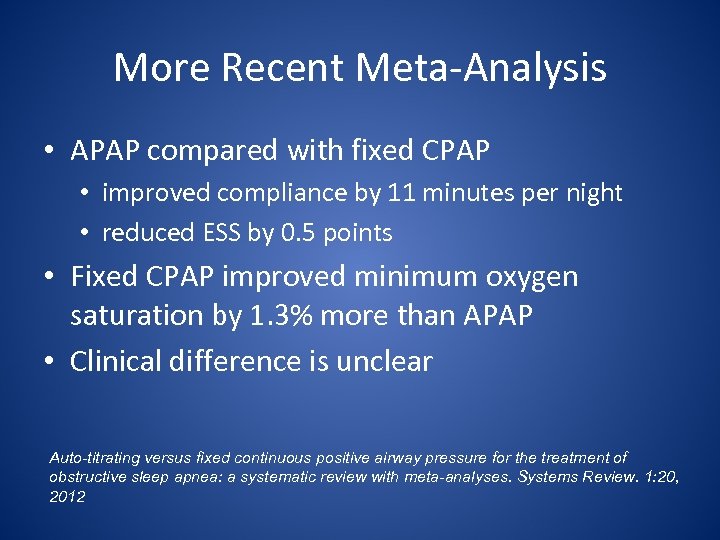
More Recent Meta-Analysis • APAP compared with fixed CPAP • improved compliance by 11 minutes per night • reduced ESS by 0. 5 points • Fixed CPAP improved minimum oxygen saturation by 1. 3% more than APAP • Clinical difference is unclear Auto-titrating versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: a systematic review with meta-analyses. Systems Review. 1: 20, 2012
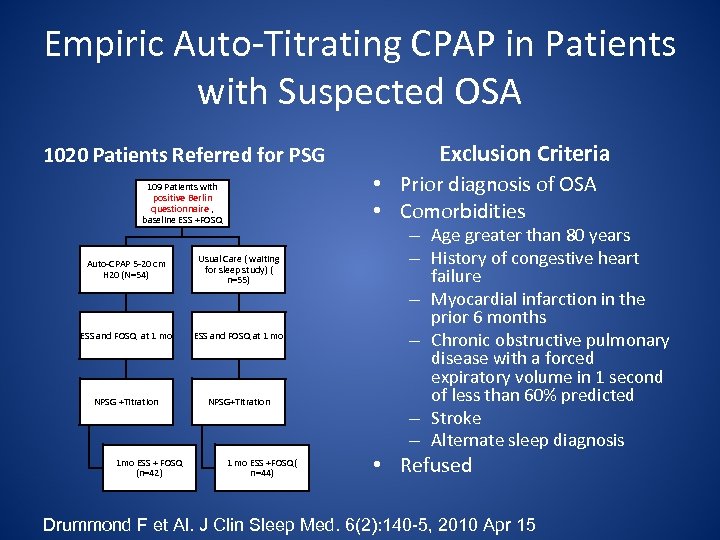
Empiric Auto-Titrating CPAP in Patients with Suspected OSA 1020 Patients Referred for PSG • Prior diagnosis of OSA • Comorbidities 109 Patients with positive Berlin questionnaire , baseline ESS +FOSQ Auto-CPAP 5 -20 cm H 20 (N=54) Usual Care ( waiting for sleep study) ( n=55) ESS and FOSQ at 1 mo NPSG +Titration NPSG+Titration 1 mo ESS + FOSQ (n=42) Exclusion Criteria 1 mo ESS +FOSQ( n=44) – Age greater than 80 years – History of congestive heart failure – Myocardial infarction in the prior 6 months – Chronic obstructive pulmonary disease with a forced expiratory volume in 1 second of less than 60% predicted – Stroke – Alternate sleep diagnosis • Refused Drummond F et Al. J Clin Sleep Med. 6(2): 140 -5, 2010 Apr 15
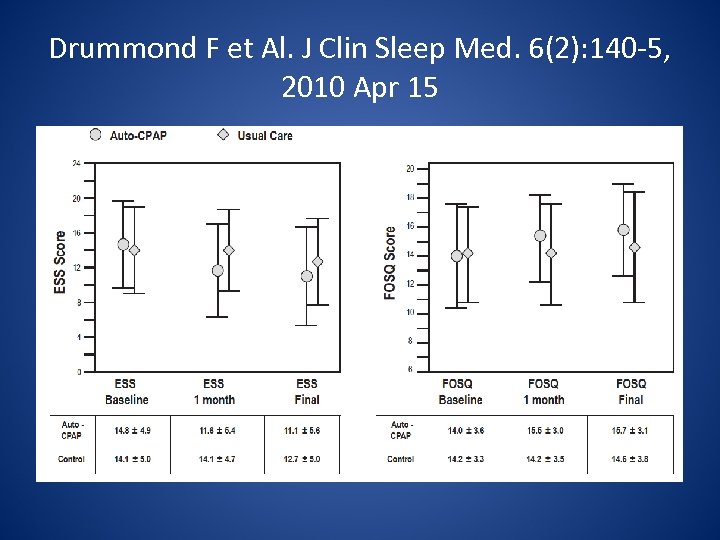
Drummond F et Al. J Clin Sleep Med. 6(2): 140 -5, 2010 Apr 15
Drummond F et Al. J Clin Sleep Med. 6(2): 140 -5, 2010 Apr 15 • Safety And Complications of Auto-CPAP Trial • No adverse events were observed. • No subject deaths or cerebrovascular accidents • No motor vehicle crashes or other catastrophic adverse events • Five patients (12%) in the auto-CPAP group and 4 (9%) in the usual-care group were admitted to the hospital for chest pain.
BIPAP S • Offers no significant advantage over CPAP for OSA patients (Gay PC et al. Sleep. 2003; 26(7): 864 -869) • For patients that require high pressures of CPAP > 15 cm H 2 O • For patients intolerant to CPAP due to perceived difficulties with exhalation • For patients with OSA and OHS or COPD • Back-up rate usually not required ( no BIPAP S/T )
Masks Interfaces • Nasal masks are the standard of care • Nasal inserts (“pillows”) are popular • Nasal-oral ( full face) masks
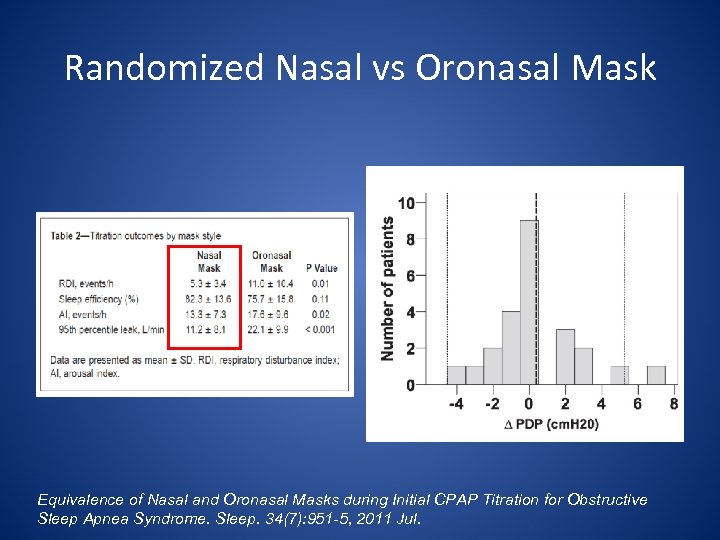
Randomized Nasal vs Oronasal Mask Equivalence of Nasal and Oronasal Masks during Initial CPAP Titration for Obstructive Sleep Apnea Syndrome. Sleep. 34(7): 951 -5, 2011 Jul.
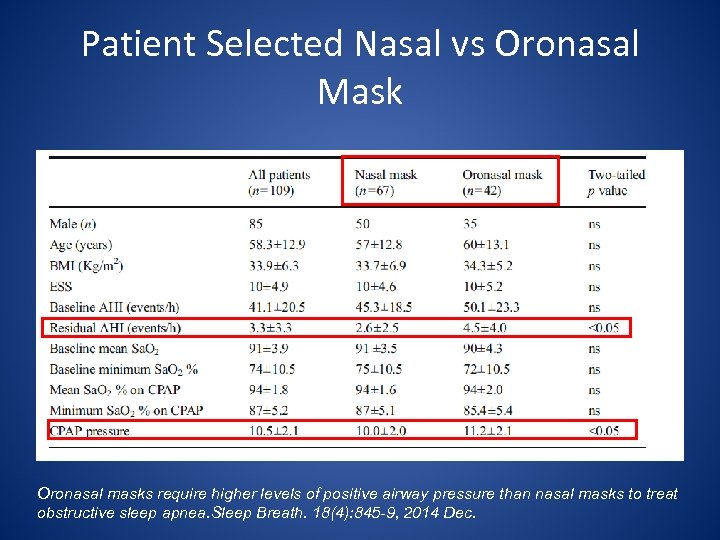
Patient Selected Nasal vs Oronasal Mask Oronasal masks require higher levels of positive airway pressure than nasal masks to treat obstructive sleep apnea. Sleep Breath. 18(4): 845 -9, 2014 Dec.
Follow Up after Initiation of PAP • Office visit • Data Download – Compliance – Residual AHI – Mask Leaks
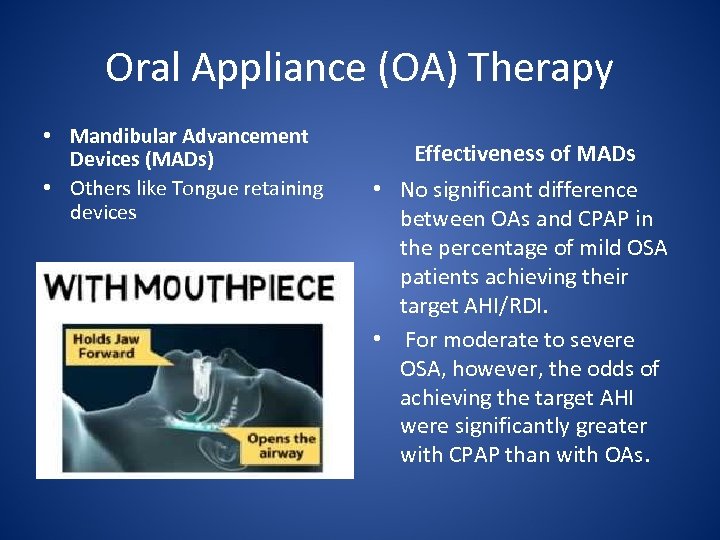
Oral Appliance (OA) Therapy • Mandibular Advancement Devices (MADs) • Others like Tongue retaining devices Effectiveness of MADs • No significant difference between OAs and CPAP in the percentage of mild OSA patients achieving their target AHI/RDI. • For moderate to severe OSA, however, the odds of achieving the target AHI were significantly greater with CPAP than with OAs.
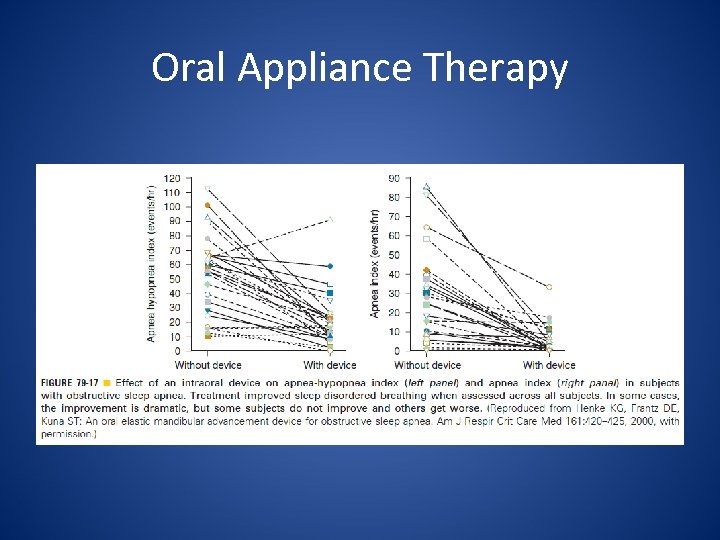
Oral Appliance Therapy
OAs • No factors consistently predicted treatment success • Sleep studies with oral appliance in place are essential as some patients do not respond • Despite reduction of OSA indeces, sleep efficiency and architecture are not improved • Result in an improvement in ESS and quality of life.
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD. Clinical practice guideline forthe treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med 2015; 11(7): 773– 827.
Summary of Recommendations • OAs are recommended for – primary snoring after OSA is ruled out by sleep physician – Patients with OSA who are intolerant of CPAP therapy or prefer alternate therapy • Qualified dentist use a custom, titratable appliance over non-custom oral devices – Custom/titratable >> custom/non-titratable > noncustom • Sleep physicians and qualified dentists provide follow up
Summary of Recommendations • Sleep physicians conduct follow-up sleep testing – To document or improve treatment efficacy – If patients develop recurrent symptoms – If substantial weight gain – With diagnoses of comorbidities relevant to OSA • Impact of OAs on resistant HTN not well studied
Contraindications of MADs • Poor dentition • Temporo-mandibular joint (TMJ) disorders
Surgical Treatment • Apart from tracheostomy, surgery is less predictable and effective • Counseling about alternative therapies, success rates and complications • Can be considered for selected patients that failed or not willing to consider PAP and OA therapy • Further research is needed to clarify patient selection, safety and efficacy of surgical approaches for OSA
Surgical Treatment • Not generally effective and not recommended – Uvulo-palatopaharyngoplasty (UPPP) – Laser-assisted uvulopalatoplasty (LAUP) • Can be considered – Radio-frequency ablation (RFA) for mild-moderate OSA – Palatal implants for mild OSA • Relief of nasal obstruction in order to increase CPAP tolerance is helpful in selected cases • Maxillo-mandibular advancement (MMA) – Has been performed as phase 2 or phase 1 – Is effective in patients with severe OSA – Invasive (entails maxillary and mandibular osteotomies)
Adjunctive Therapies • Weight loss should be advised for all obese patients with OSA – Caveat: the magnitude of correlation of OSA severity and weight is greater with weight gain rather than weight loss • Bariatric surgery related weight loss provides either resolution of OSA (around 40%) or major improvements of AHI, sleep architecture, CPAP requirements and daytime sleepiness
Adjunctive Therapies • Exercise • Avoidance of alcohol or sedatives before bedtime
Positional Therapy • For purely positional (supine) apnea • Tennis ball sawn in a back pajama pocket • Commercially available devices that prevents rolling to supine position • Objectively document effectiveness with position monitor
Central Nervous System Stimulants • Persistent symptoms of daytime sleepiness • After objectively documented compliance with CPAP • Modafinil or the longer acting analogue armodafinil
Emerging Therapies • Nasal expiratory PAP devices (Nasal EPAP) • Oral pressure therapy (OPT) • Electrical Stimulation (ES)
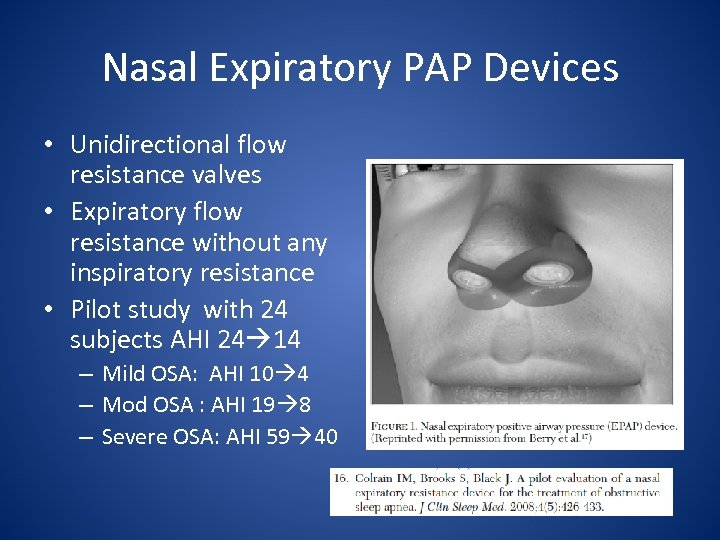
Nasal Expiratory PAP Devices • Unidirectional flow resistance valves • Expiratory flow resistance without any inspiratory resistance • Pilot study with 24 subjects AHI 24 14 – Mild OSA: AHI 10 4 – Mod OSA : AHI 19 8 – Severe OSA: AHI 59 40
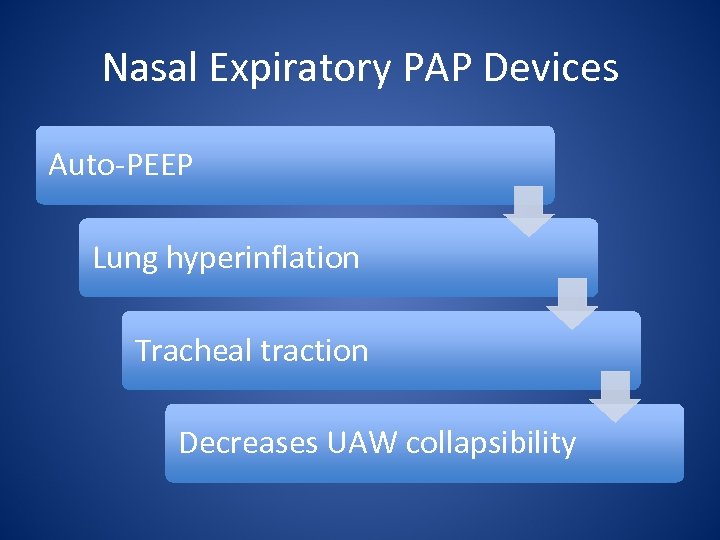
Nasal Expiratory PAP Devices Auto-PEEP Lung hyperinflation Tracheal traction Decreases UAW collapsibility
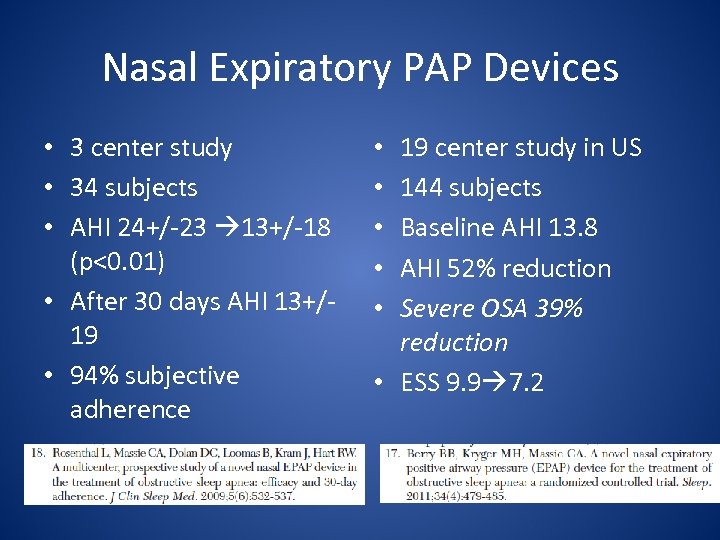
Nasal Expiratory PAP Devices • 3 center study • 34 subjects • AHI 24+/-23 13+/-18 (p<0. 01) • After 30 days AHI 13+/19 • 94% subjective adherence 19 center study in US 144 subjects Baseline AHI 13. 8 AHI 52% reduction Severe OSA 39% reduction • ESS 9. 9 7. 2 • • •
Nasal Expiratory PAP Devices • Excluded patients – Nasal blockage – Nasal allergies/sinusitis – Severe nocturnal desaturations – Use of sedating medications • Testing is required to document effectiveness – Special nasal pressure transducer • Valves are single use night
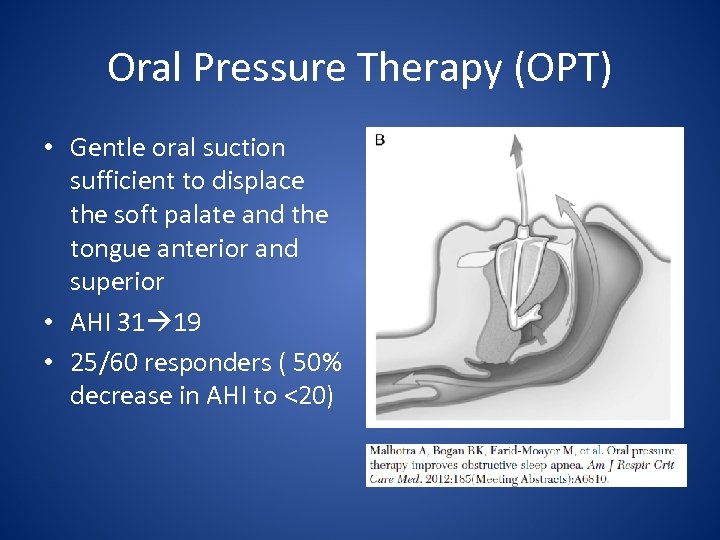
Oral Pressure Therapy (OPT) • Gentle oral suction sufficient to displace the soft palate and the tongue anterior and superior • AHI 31 19 • 25/60 responders ( 50% decrease in AHI to <20)
Oral Pressure Therapy (OPT) • MRI imaging revel 75% increase in retro-palatal airway space • FDA approved
Electrical Stimulation (ES) • • Percutaneous genioglossus muscle stimulation Trigger: decrease in tracheal breath sounds Six subjects AHI 39 11. 7
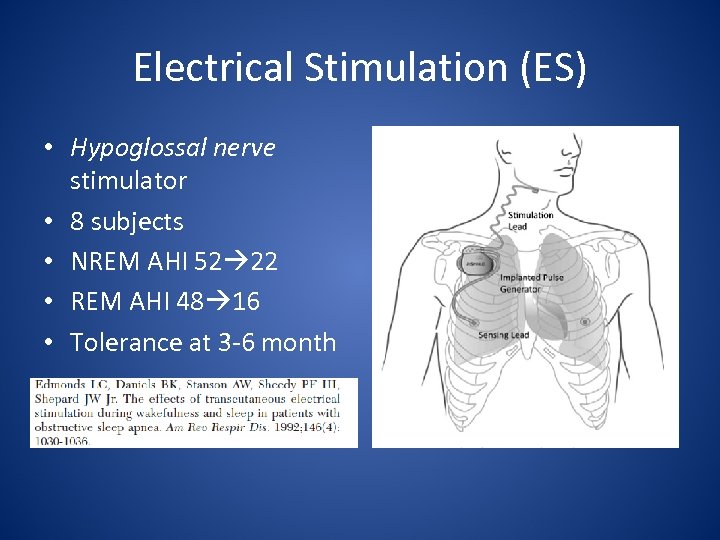
Electrical Stimulation (ES) • Hypoglossal nerve stimulator • 8 subjects • NREM AHI 52 22 • REM AHI 48 16 • Tolerance at 3 -6 month
Electrical Stimulation • Multicenter trial • 21 patients • Respiratory sensing uses thoracic bioimpedance • AHI 43 19 • MIF 215 509 m. L/s • Pain/numbness at insertion site
Choosing the Right Candidates • Prospective validation of positive predictors factors – BMI<32 – AHI<50 – Lack of concentric palatal collapse during druginduced sleep endoscopy • 7/8 patients had a 50% decrease of AHI to <20
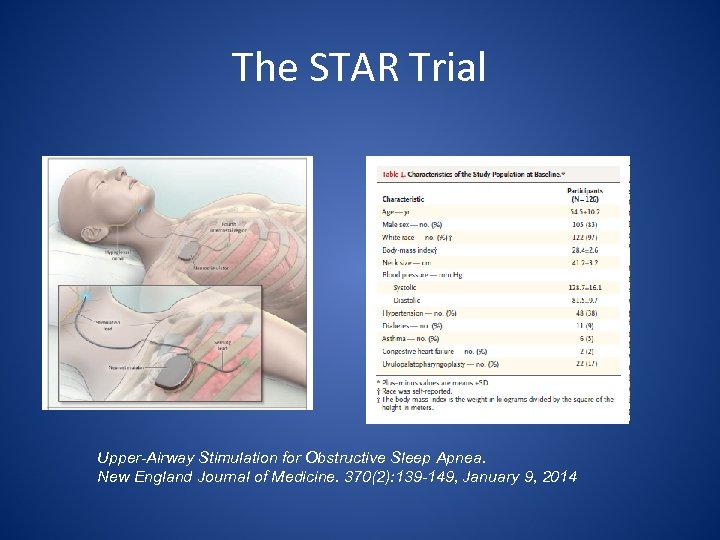
The STAR Trial Upper-Airway Stimulation for Obstructive Sleep Apnea. New England Journal of Medicine. 370(2): 139 -149, January 9, 2014
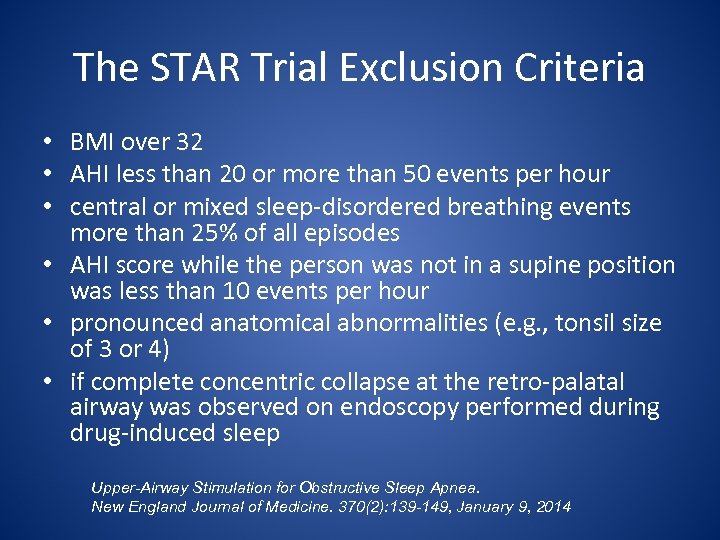
The STAR Trial Exclusion Criteria • BMI over 32 • AHI less than 20 or more than 50 events per hour • central or mixed sleep-disordered breathing events more than 25% of all episodes • AHI score while the person was not in a supine position was less than 10 events per hour • pronounced anatomical abnormalities (e. g. , tonsil size of 3 or 4) • if complete concentric collapse at the retro-palatal airway was observed on endoscopy performed during drug-induced sleep Upper-Airway Stimulation for Obstructive Sleep Apnea. New England Journal of Medicine. 370(2): 139 -149, January 9, 2014
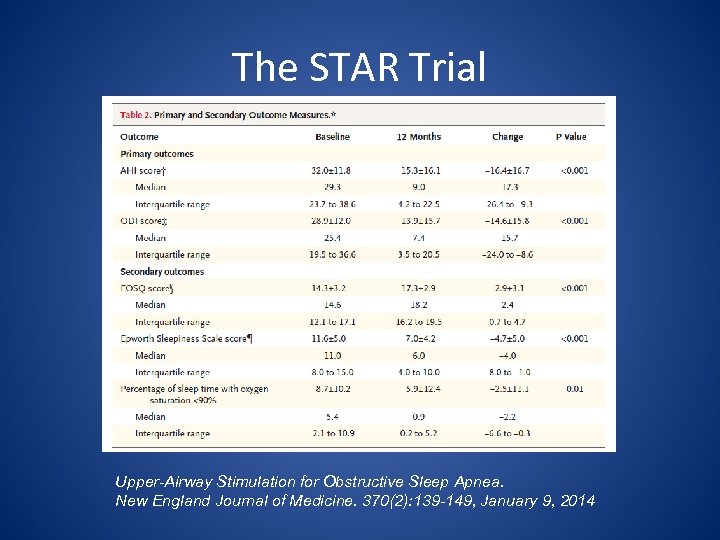
The STAR Trial Upper-Airway Stimulation for Obstructive Sleep Apnea. New England Journal of Medicine. 370(2): 139 -149, January 9, 2014
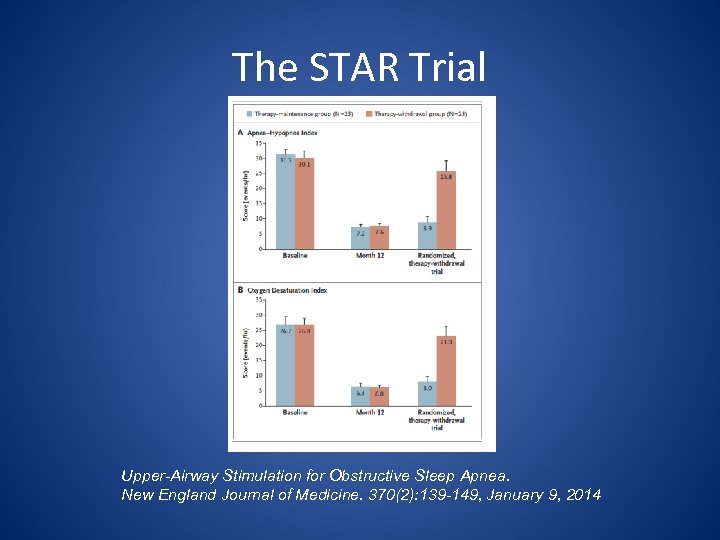
The STAR Trial Upper-Airway Stimulation for Obstructive Sleep Apnea. New England Journal of Medicine. 370(2): 139 -149, January 9, 2014
Electrical Stimulation (ES) • Promising for moderate and severe OSA in non -obese patients • Adherence was improved • For selected patients • ? Long term efficacy and side effects
Thank You! • Review patho-physiologic mechanisms of obstructive sleep apnea (OSA) • Review the established positive airway pressure, oral appliance and surgical therapy options • Review emerging therapy options
de0490dbff879f41f2ce8e33b83c4622.ppt