de1d48bc6a841c62d1bd475595c66a5a.ppt
- Количество слайдов: 57
Obstetrical Hemorrhage International Obstetrical Hemorrhage
Obstetrical Hemorrhage International Obstetrical Hemorrhage Principles • Prompt diagnosis • Recognize reserve and ability to compensate • Resuscitate vigorously • Identify underlying cause • Treat underlying cause
Obstetrical Hemorrhage International A 25 year- old G 3 woman presents to the maternity unit with vaginal bleeding. Fetal heart rate is 140/mnt and her BP is 110/60 mm. Hg and her HR 85/mnt. Fundal height is 28 cm. She has been given nothing. What are the possible diagnosis ? -------------------------------How would you distinguish between the diagnosis ? -----------------------
Obstetrical Hemorrhage International
Obstetrical Hemorrhage International Antepartum Hemorrhage
Obstetrical Hemorrhage International Objectives • Definitions and Incidence • Etiology and Risk Factors • Diagnosis • Management - maternal and fetal assessment - appropriate resuscitation - no vaginal exam prior to determining placental location • Individual Causes
Obstetrical Hemorrhage International Definition • vaginal bleeding between 20 weeks and delivery Incidence • 2% to 5% of all pregnancies • various causes of antepartum haemorrhage - abruptio placenta 40% - 1% of pregnancies - unclassified 35% - placenta previa 20% - ½% of pregnancies - lower genital tract lesion 5% - other
Obstetrical Hemorrhage International Etiology of APH • Cervical – contact bleeding (e. g. intercourse, pap, neoplasia, examination – inflammation (e. g. infection) – effacement and dilatation (e. g. labour, cervical incompetence) • Placental – abruptio – previa – marginal sinus rupture • Vasa previa • Other - abnormal coagulation
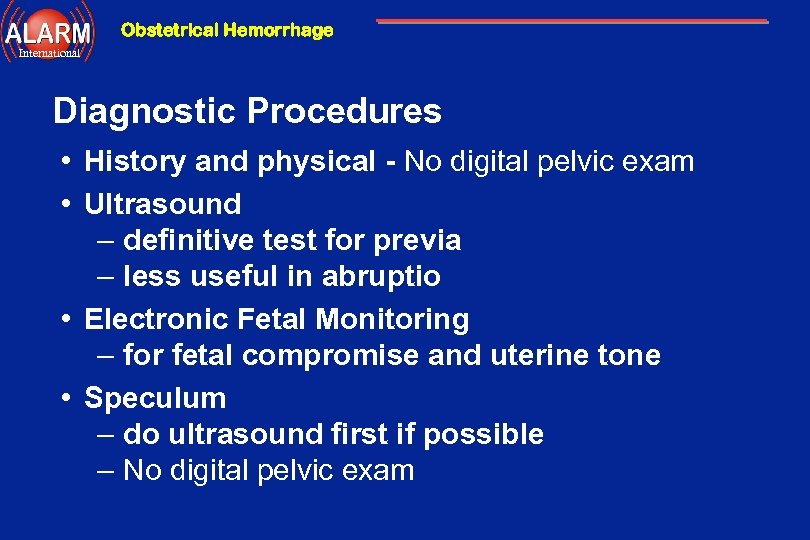
Obstetrical Hemorrhage International Diagnostic Procedures • History and physical - No digital pelvic exam • Ultrasound – definitive test for previa – less useful in abruptio • Electronic Fetal Monitoring – for fetal compromise and uterine tone • Speculum – do ultrasound first if possible – No digital pelvic exam
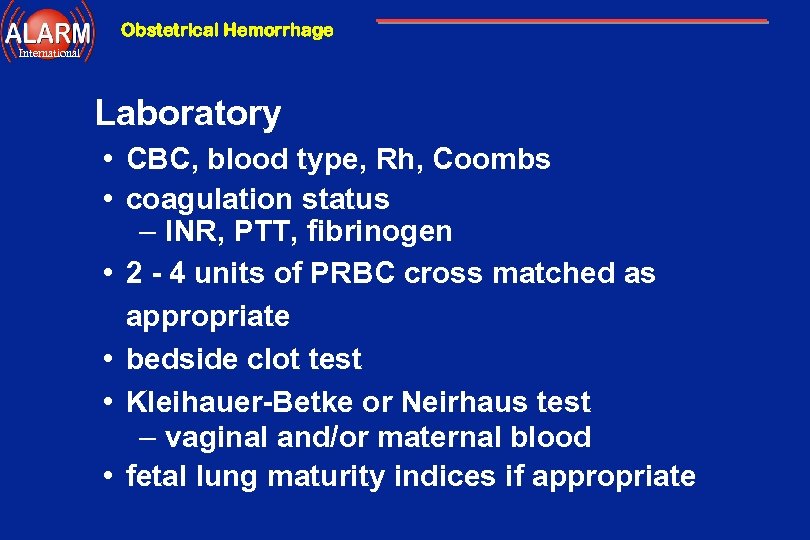
Obstetrical Hemorrhage International Laboratory • CBC, blood type, Rh, Coombs • coagulation status – INR, PTT, fibrinogen • 2 - 4 units of PRBC cross matched as appropriate • bedside clot test • Kleihauer-Betke or Neirhaus test – vaginal and/or maternal blood • fetal lung maturity indices if appropriate
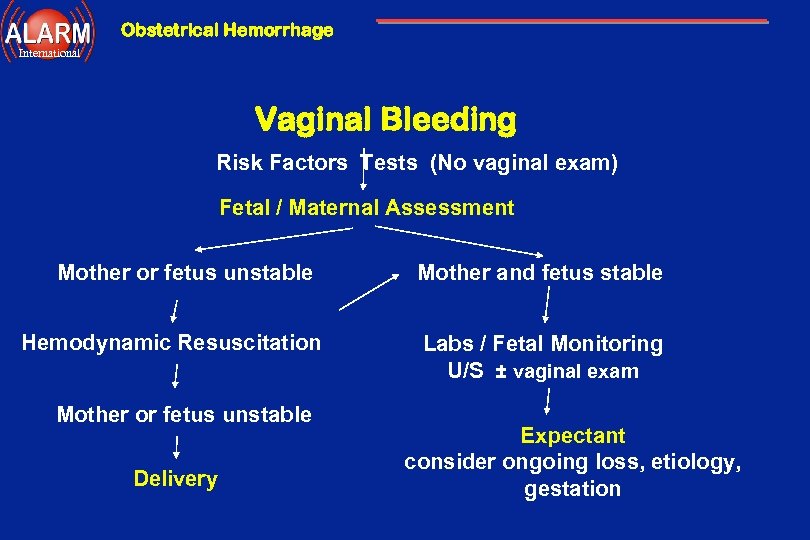
Obstetrical Hemorrhage International Vaginal Bleeding Risk Factors Tests (No vaginal exam) Fetal / Maternal Assessment Mother or fetus unstable Hemodynamic Resuscitation Mother or fetus unstable Delivery Mother and fetus stable Labs / Fetal Monitoring U/S ± vaginal exam Expectant consider ongoing loss, etiology, gestation
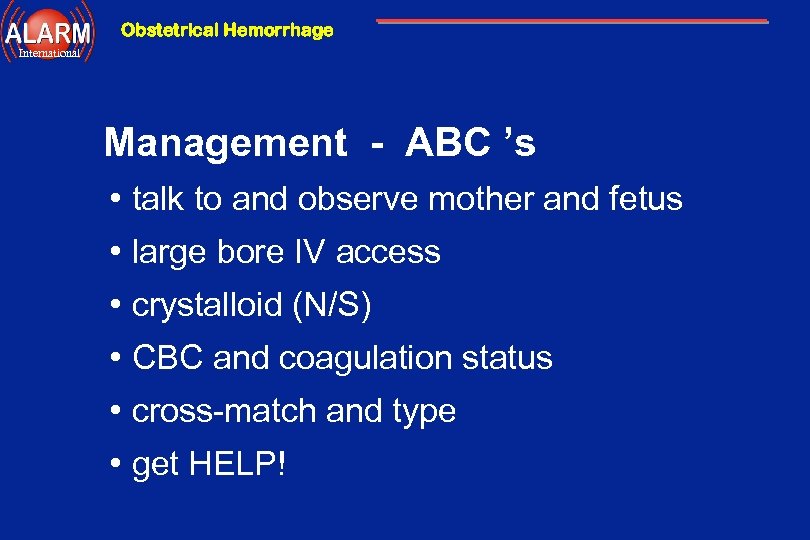
Obstetrical Hemorrhage International Management - ABC ’s • talk to and observe mother and fetus • large bore IV access • crystalloid (N/S) • CBC and coagulation status • cross-match and type • get HELP!
Obstetrical Hemorrhage International Hemodynamic Resuscitation • early aggressive resuscitation to protect fetus and maternal organs from hypoperfusion and to prevent DIC • stabilize vital signs • large bore IV crystalloid infusion, plasma expanders • follow hemoglobin and coagulation status • oxygen consumption is up 20% in pregnancy
Obstetrical Hemorrhage International Fetal Considerations • lateral position increases cardiac output up to 30% • consider amniocentesis for lung indices • external fetal and labor monitoring • Kleihauer-Betke if suspected abruption • post-trauma monitor at least 4 hours for evidence of fetal insult, abruptio, fetal maternal transfusion
Obstetrical Hemorrhage International Abruptio Placenta - Definition • premature separation of normally implanted placenta Abruptio Placenta - Classification • Total fetal death • Partial fetus may tolerate up to 30 -50% abruption
Obstetrical Hemorrhage International Risk Factors for Abruption • • • hypertension: gestational and pre-existing abdominal trauma cocaine or crack abuse previous abruption overdistended uterus – multiple gestation, polyhydramnios • smoking, especially >1 pack/day
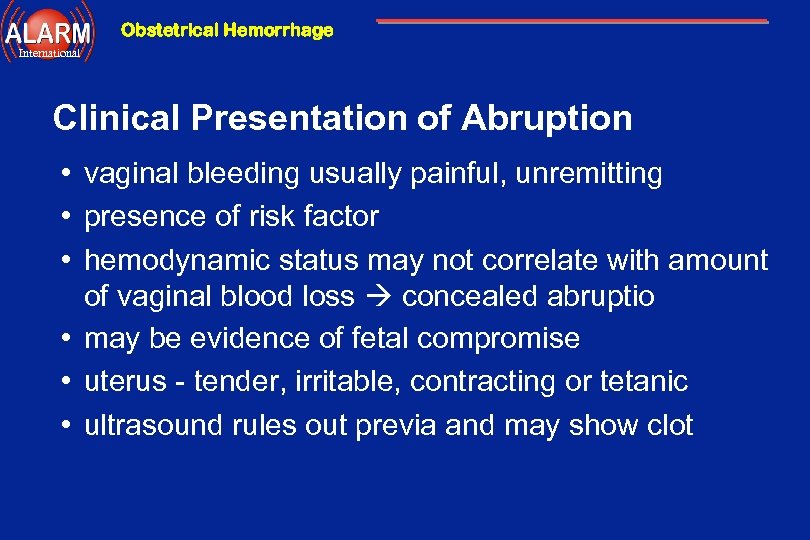
Obstetrical Hemorrhage International Clinical Presentation of Abruption • vaginal bleeding usually painful, unremitting • presence of risk factor • hemodynamic status may not correlate with amount of vaginal blood loss concealed abruptio • may be evidence of fetal compromise • uterus - tender, irritable, contracting or tetanic • ultrasound rules out previa and may show clot
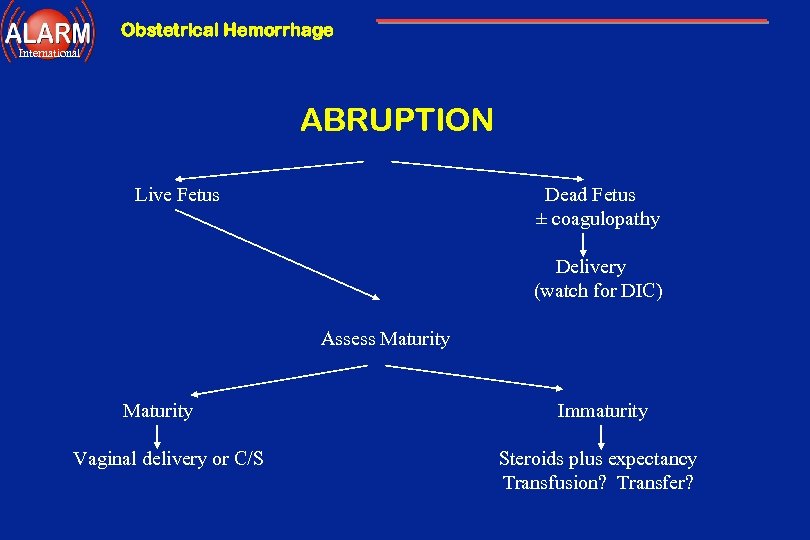
Obstetrical Hemorrhage International ABRUPTION Live Fetus Dead Fetus ± coagulopathy Delivery (watch for DIC) Assess Maturity Vaginal delivery or C/S Immaturity Steroids plus expectancy Transfusion? Transfer?
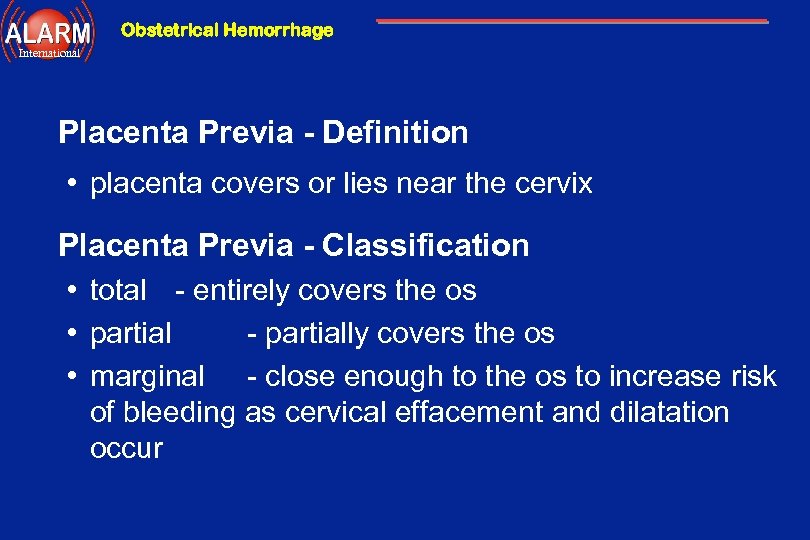
Obstetrical Hemorrhage International Placenta Previa - Definition • placenta covers or lies near the cervix Placenta Previa - Classification • total - entirely covers the os • partial - partially covers the os • marginal - close enough to the os to increase risk of bleeding as cervical effacement and dilatation occur
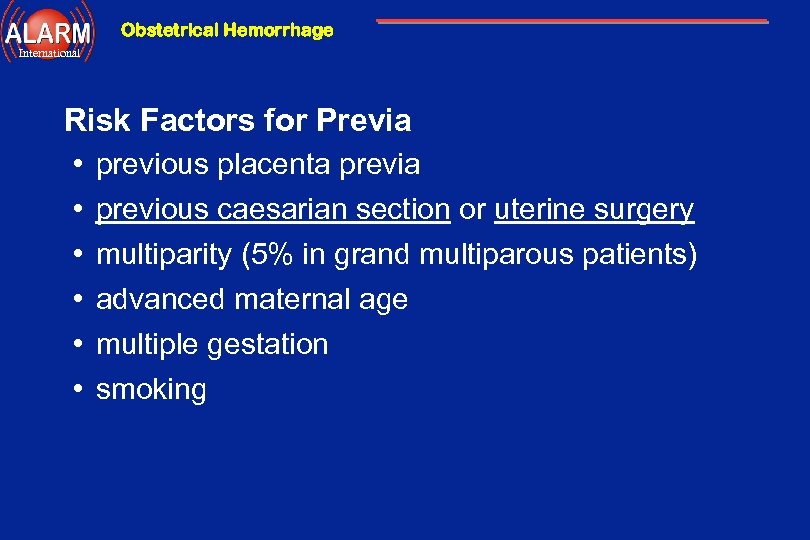
Obstetrical Hemorrhage International Risk Factors for Previa • previous placenta previa • previous caesarian section or uterine surgery • multiparity (5% in grand multiparous patients) • advanced maternal age • multiple gestation • smoking
Obstetrical Hemorrhage International Clinical Presentation of Previa • vaginal bleeding usually painless (unless in labour) • maternal hemodynamic status corresponds to amount of vaginal blood loss • well tolerated by fetus unless maternal instability • uterus - non-tender, not irritable, soft • may have abnormal lie • ultrasound shows previa !
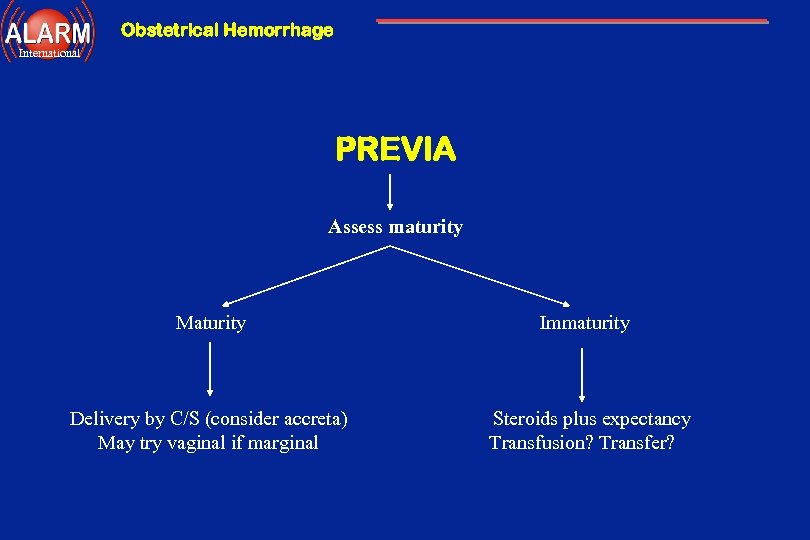
Obstetrical Hemorrhage International PREVIA Assess maturity Maturity Immaturity Delivery by C/S (consider accreta) May try vaginal if marginal Steroids plus expectancy Transfusion? Transfer?
Obstetrical Hemorrhage International Vasa Previa - Definition • blood vessels in the membranes run across the cervix • requires a vellamentous insertion or succenturiate lobe Complication • ex-sanguination following amniotomy or ROM Diagnosis • Apt test or Kleihauer test on vaginal blood • terminal fetal bradycardia ± initial tachycardia or sinusoidal FH Prognosis • fetal mortality as high as 50 -70%
Obstetrical Hemorrhage International Conclusions • • • assess maternal status and stability assess fetal well-being resuscitate appropriately assess cause of bleeding - avoid vaginal exam expectant management if appropriate deliver if indicated based on maternal or fetal status
Obstetrical Hemorrhage International Postpartum Hemorrhage
Obstetrical Hemorrhage International You have just delivered a 37 week twin pregnancy per vagina. The third stage is complicated by post partum hemorrhage unresponsive to uterine message and the use of oxytocin. What would your next management steps be ----------------- ?
Obstetrical Hemorrhage International Objectives • Definition • Etiology • Risk Factors • Prevention • Management
Obstetrical Hemorrhage International Traditional Definition • blood loss of > 500 m. L following vaginal delivery • blood loss of > 1000 m. L following cesarean delivery Functional Definition • any blood loss that has the potential to produce or produces hemodynamic instability Incidence • about 5% of all deliveries
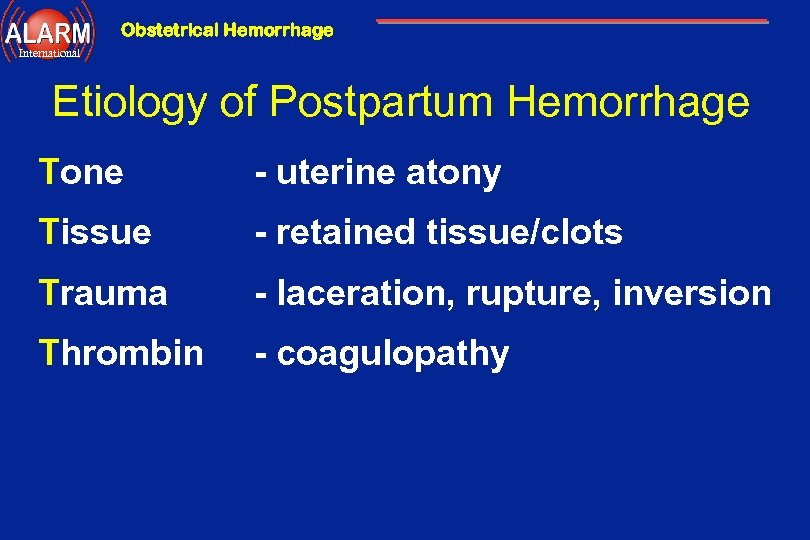
Obstetrical Hemorrhage International Etiology of Postpartum Hemorrhage Tone - uterine atony Tissue - retained tissue/clots Trauma - laceration, rupture, inversion Thrombin - coagulopathy
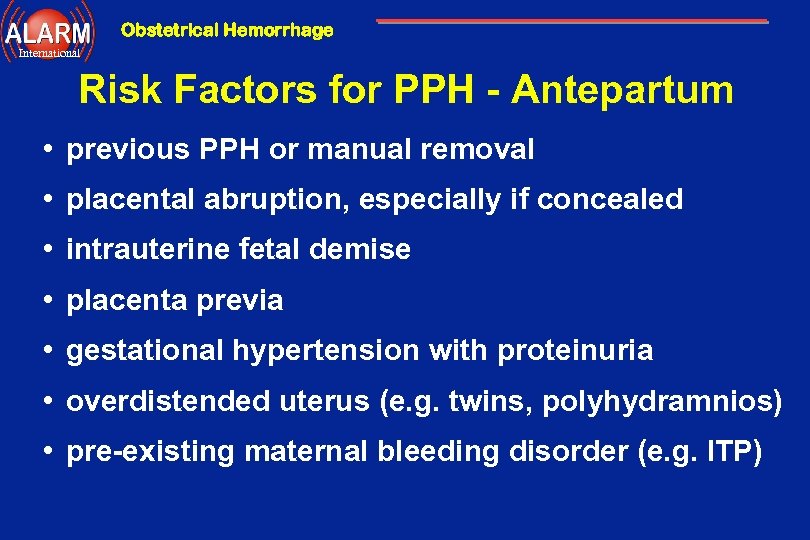
Obstetrical Hemorrhage International Risk Factors for PPH - Antepartum • previous PPH or manual removal • placental abruption, especially if concealed • intrauterine fetal demise • placenta previa • gestational hypertension with proteinuria • overdistended uterus (e. g. twins, polyhydramnios) • pre-existing maternal bleeding disorder (e. g. ITP)
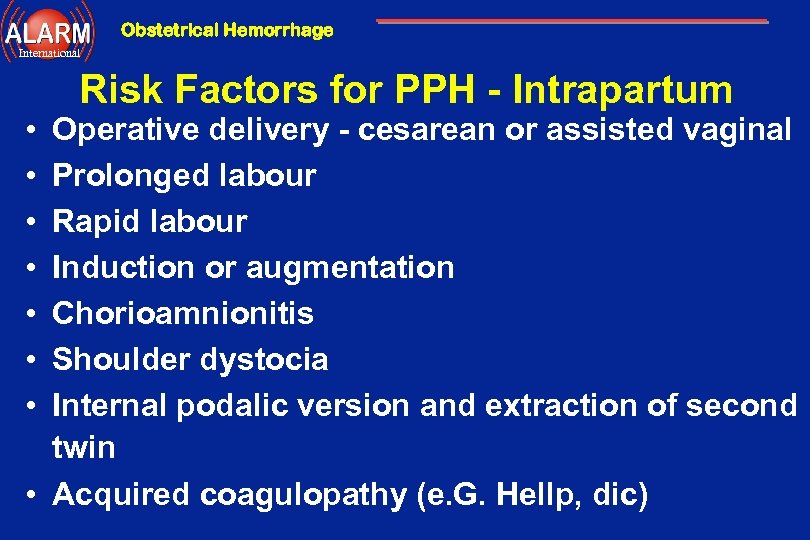
Obstetrical Hemorrhage International • • Risk Factors for PPH - Intrapartum Operative delivery - cesarean or assisted vaginal Prolonged labour Rapid labour Induction or augmentation Chorioamnionitis Shoulder dystocia Internal podalic version and extraction of second twin • Acquired coagulopathy (e. G. Hellp, dic)
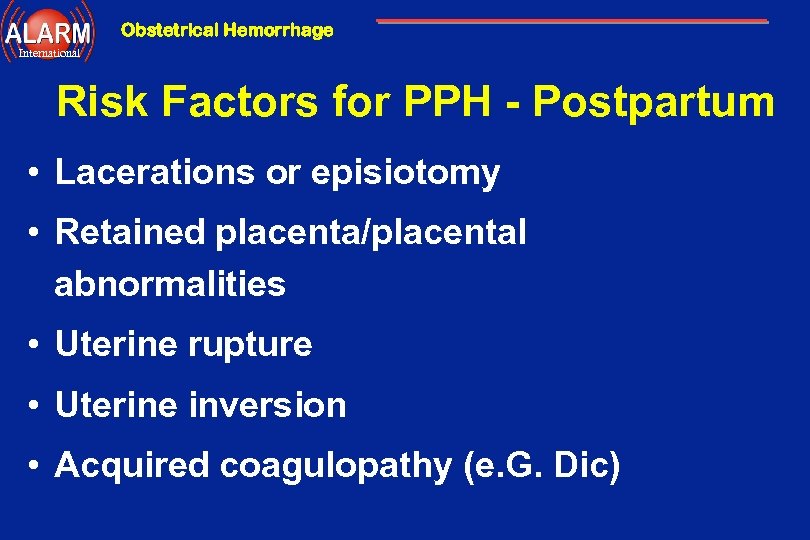
Obstetrical Hemorrhage International Risk Factors for PPH - Postpartum • Lacerations or episiotomy • Retained placenta/placental abnormalities • Uterine rupture • Uterine inversion • Acquired coagulopathy (e. G. Dic)
Obstetrical Hemorrhage International Prevention • be prepared • active management of the third stage • prophylactic oxytocin with delivery or with delivery of anterior shoulder - 10 U IM or 5 U IV bolus - 20 U/L N/S IV run rapidly • early cord clamping and cutting • gentle cord traction with suprapubic countertraction
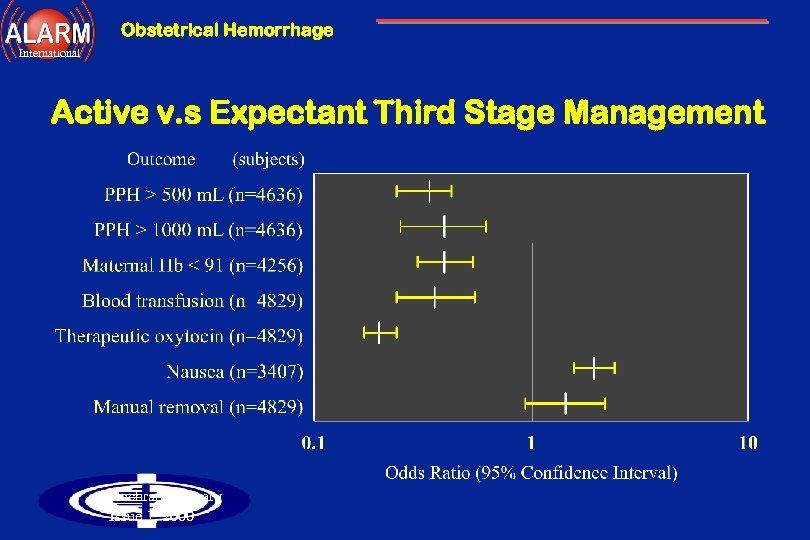
Obstetrical Hemorrhage International Active v. s Expectant Third Stage Management Cochrane Library Issue 1, 2000
Obstetrical Hemorrhage International Postpartum Hemorrhage Diagnosis - Is this a PPH? • consider risk factors • observe vaginal loss • express blood from vagina following C/S • REMEMBER - blood loss is consistently underestimated - ongoing trickling can lead to significant blood loss - blood loss is generally well tolerated to a point
Obstetrical Hemorrhage International Diagnosis - What is the cause? • Assess the fundus • Inspect the lower genital tract • Explore the uterus • Retained placental fragments • Uterine rupture • Uterine inversion • Assess coagulation
Obstetrical Hemorrhage International Postpartum Hemorrhage C B A A = airway B = breathing C = circulation
Obstetrical Hemorrhage International Management - ABC ’s • talk to and observe patient • large bore IV access ( Nr. 16 gauge) • crystalloid - lots! • CBC • cross-match and type • get HELP!
Obstetrical Hemorrhage International Postpartum Hemorrhage Management - Assess the fundus • simultaneous with ABC ’s • atony is the leading cause of PPH • if boggy bimanual massage - rules out uterine inversion - may feel lower tract injury - evacuate clot from vagina and/or cervix - may consider manual exploration at this time
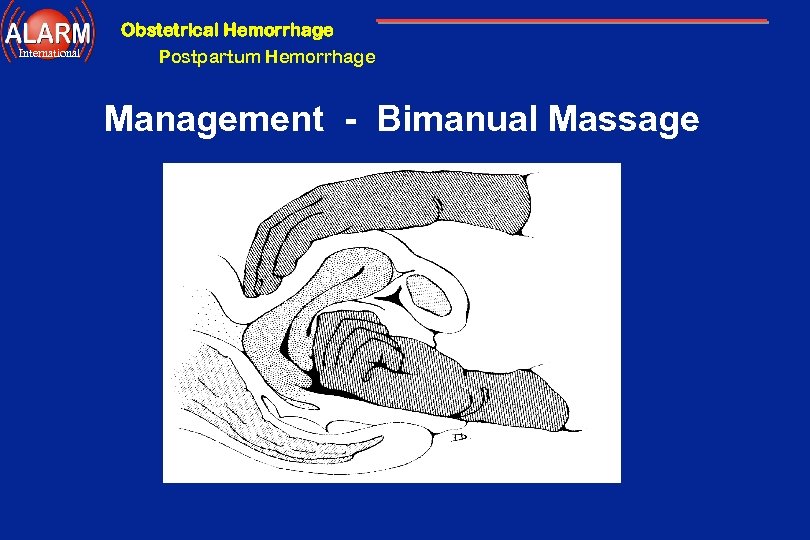
Obstetrical Hemorrhage International Postpartum Hemorrhage Management - Bimanual Massage
Obstetrical Hemorrhage International Postpartum Hemorrhage Management - Oxytocin • 5 units IV bolus • 20 units per L N/S IV wide open • 10 units directly into the uterus if no I. V access
Obstetrical Hemorrhage International Management - Manual Exploration • if no response to bimanual massage and oxytocin then proceed to exploration • manual exploration will: - rule out uterine inversion - palpate cervical injury - remove retained placenta or clot from uterus - rule out uterine rupture or dehiscence
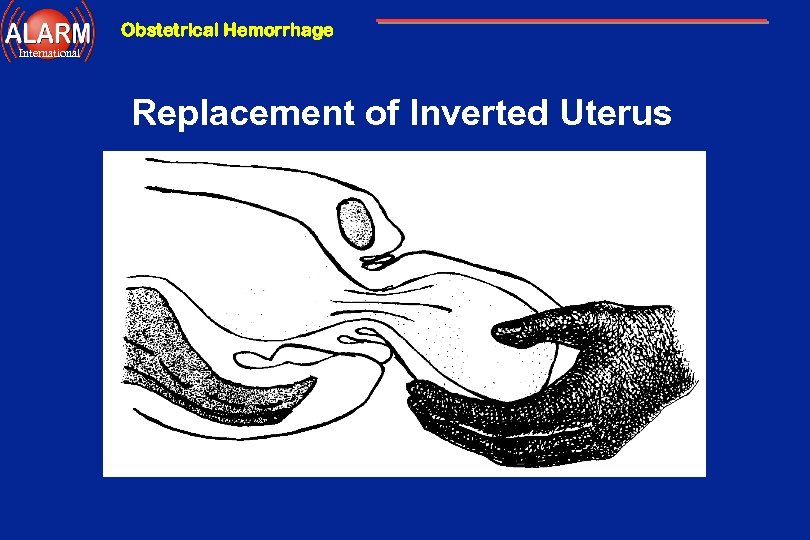
Obstetrical Hemorrhage International Replacement of Inverted Uterus
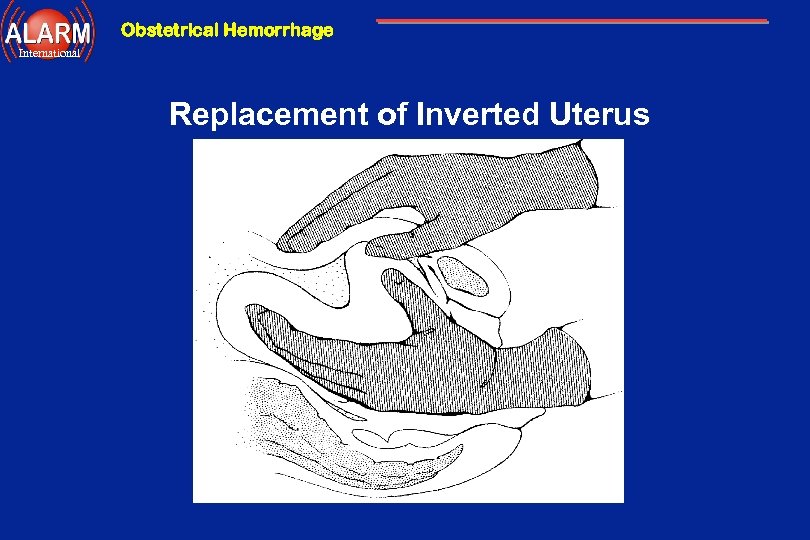
Obstetrical Hemorrhage International Replacement of Inverted Uterus
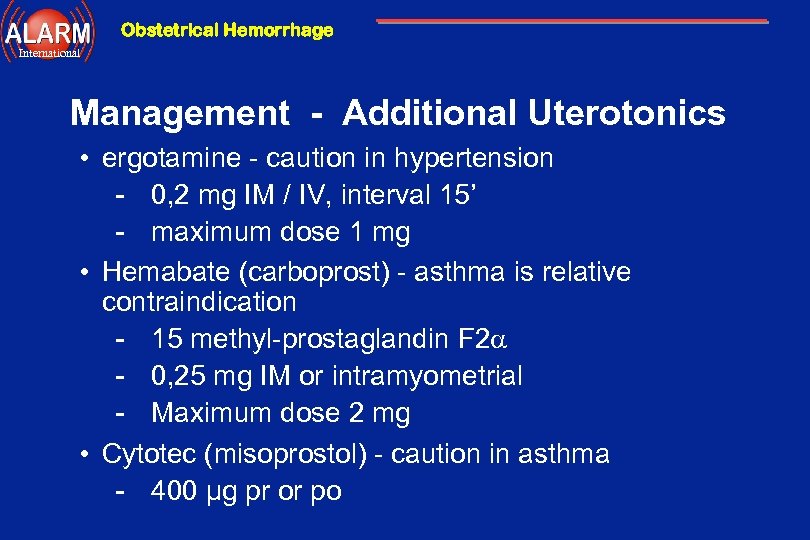
Obstetrical Hemorrhage International Management - Additional Uterotonics • ergotamine - caution in hypertension - 0, 2 mg IM / IV, interval 15’ - maximum dose 1 mg • Hemabate (carboprost) - asthma is relative contraindication - 15 methyl-prostaglandin F 2 - 0, 25 mg IM or intramyometrial - Maximum dose 2 mg • Cytotec (misoprostol) - caution in asthma - 400 µg pr or po
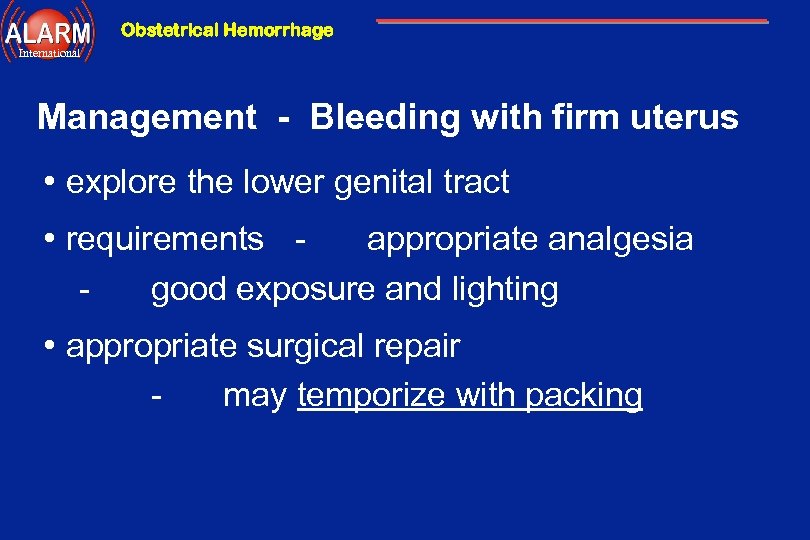
Obstetrical Hemorrhage International Management - Bleeding with firm uterus • explore the lower genital tract • requirements appropriate analgesia good exposure and lighting • appropriate surgical repair may temporize with packing
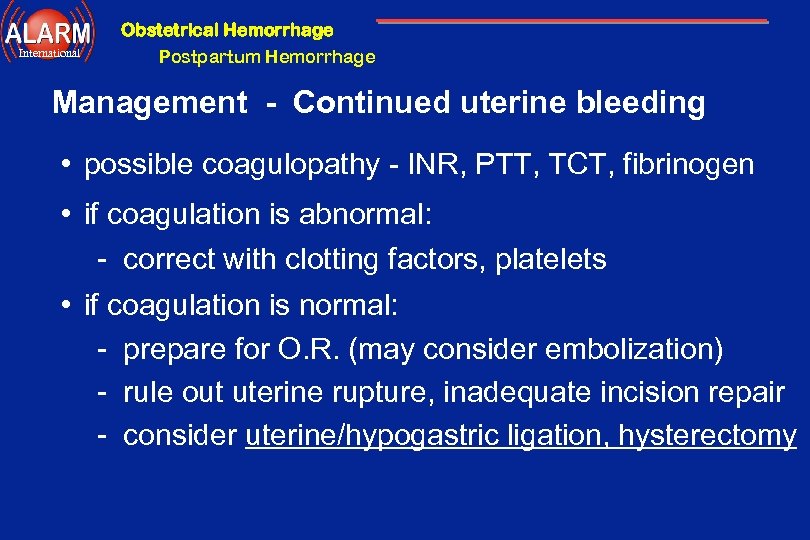
Obstetrical Hemorrhage International Postpartum Hemorrhage Management - Continued uterine bleeding • possible coagulopathy - INR, PTT, TCT, fibrinogen • if coagulation is abnormal: - correct with clotting factors, platelets • if coagulation is normal: - prepare for O. R. (may consider embolization) - rule out uterine rupture, inadequate incision repair - consider uterine/hypogastric ligation, hysterectomy
Obstetrical Hemorrhage International Management - ABC ’s ENSURE that you are always ahead with your resuscitation!!! • consider need for Foley catheter, CVP, arterial line, etc • consider need for more expert help
Obstetrical Hemorrhage International Conclusions • • be prepared practice prevention assess the loss assess maternal status resuscitate vigorously and appropriately diagnose the cause treat the cause
Obstetrical Hemorrhage International Postpartum Hemorrhage Management - Evolution Panic Hysterectomy Pitocin Prostaglandins Happiness

Obstetrical Hemorrhage International

Obstetrical Hemorrhage International Kleihauer-Betke Indications • Measures fetal cells in maternal circulation • Used in assessing for Rh Sensitization • Maternal blood Rh negative • Large antepartum bleed Mechanism • Blood Film stained with acid elution • Fetal Hb. F more acid resistant • Fetal RBC darkly stained, Maternal RBC "ghosts" Technique • Count Fetal cells per 50 low power fields • Five cells per 50 (lpf) = 0. 5 ml bleed
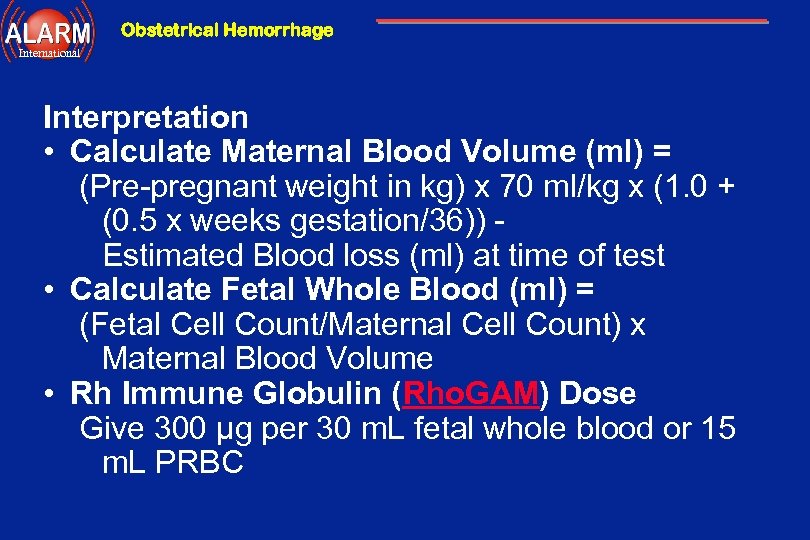
Obstetrical Hemorrhage International Interpretation • Calculate Maternal Blood Volume (ml) = (Pre-pregnant weight in kg) x 70 ml/kg x (1. 0 + (0. 5 x weeks gestation/36)) Estimated Blood loss (ml) at time of test • Calculate Fetal Whole Blood (ml) = (Fetal Cell Count/Maternal Cell Count) x Maternal Blood Volume • Rh Immune Globulin (Rho. GAM) Dose Give 300 μg per 30 m. L fetal whole blood or 15 m. L PRBC
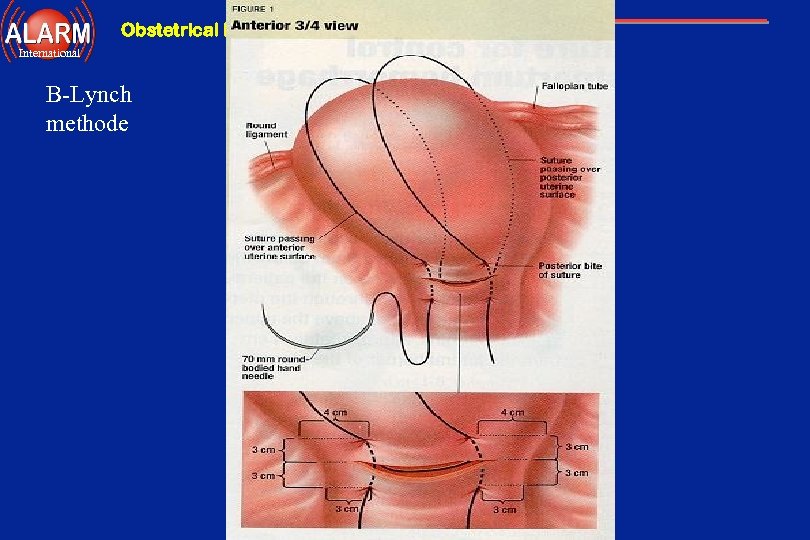
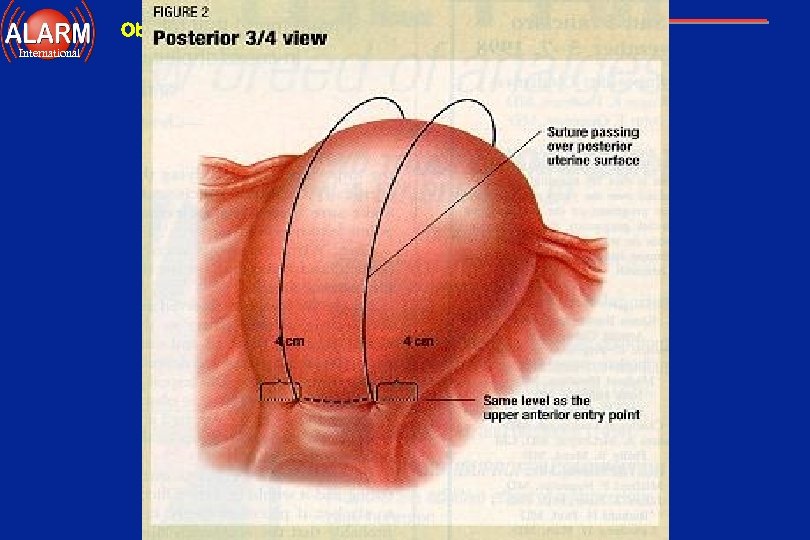
Obstetrical Hemorrhage International B-Lynch methode
Obstetrical Hemorrhage International
Obstetrical Hemorrhage International Medical Anti Schock Trouser & Penekan Infus
Obstetrical Hemorrhage International Postpartum Hemorrhage Keep your bloody fingers off the cervix!
de1d48bc6a841c62d1bd475595c66a5a.ppt