a77ef78dffdfb53a73c7e37d740d5062.ppt
- Количество слайдов: 44
Obstetric Emergencies Dr Mohamed Abdul Hakim Kotb, MBBCH, MSC, MD Anaesthesia & ICU
Obstetric emergencies Massive obstetric haemorrhage Non-haemorrhagic shock: – – Amniotic fluid embolism Acute uterine inversion Shoulder dystocia Eclampsia Cord prolapse Cardiac Arrest Anaphylaxis TRAUMA
BASIC PRINCIPLES FOR OBSTETRIC EMERGENCIES. Physiological changes in pregnancy modify: • • • Presentation of the problem Normal physiological variables Response to treatment Both mother & fetus are affected by the pathology & subsequent treatment. Mother’s welfare always takes precedence over fetal concerns --Fetal survival is usually dependant on optimal maternal management. •

MASSIVE OBSTETRIC HAEMORRHAGE Major contributor to maternal mortality Definition – Blood loss requiring replacement of patient’s total blood volume – Transfusion requiring > 10 u of blood in 24 hs – 50% replacement of blood vol. <3 hs period Difficult to estimate blood loss Problem of concealed bleeding – Uterus – Broad lig. – Peritoneal cavity
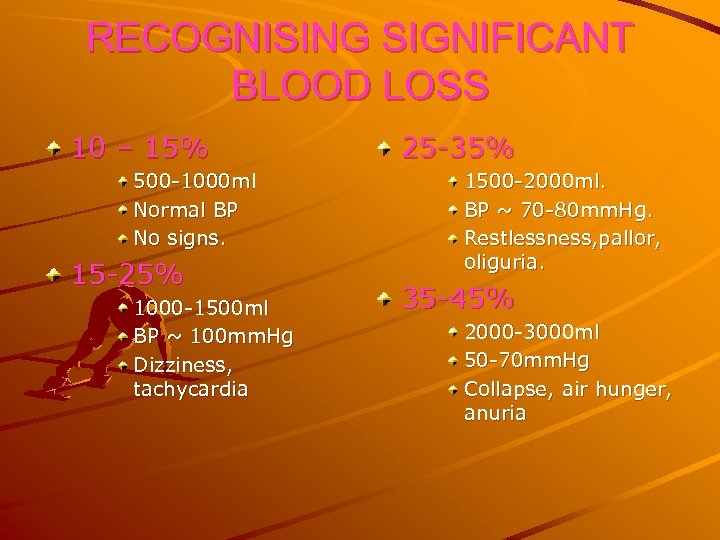
RECOGNISING SIGNIFICANT BLOOD LOSS 10 – 15% 500 -1000 ml Normal BP No signs. 15 -25% 1000 -1500 ml BP ~ 100 mm. Hg Dizziness, tachycardia 25 -35% 1500 -2000 ml. BP ~ 70 -80 mm. Hg. Restlessness, pallor, oliguria. 35 -45% 2000 -3000 ml 50 -70 mm. Hg Collapse, air hunger, anuria
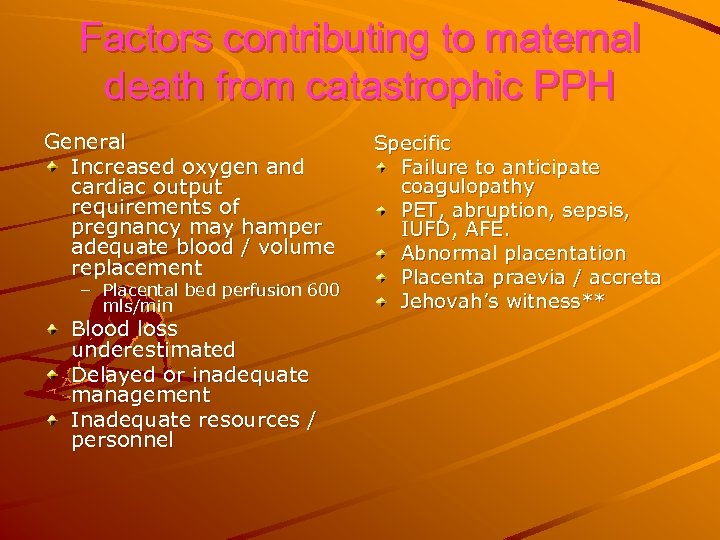
Factors contributing to maternal death from catastrophic PPH General Increased oxygen and cardiac output requirements of pregnancy may hamper adequate blood / volume replacement – Placental bed perfusion 600 mls/min Blood loss underestimated Delayed or inadequate management Inadequate resources / personnel Specific Failure to anticipate coagulopathy PET, abruption, sepsis, IUFD, AFE. Abnormal placentation Placenta praevia / accreta Jehovah’s witness**
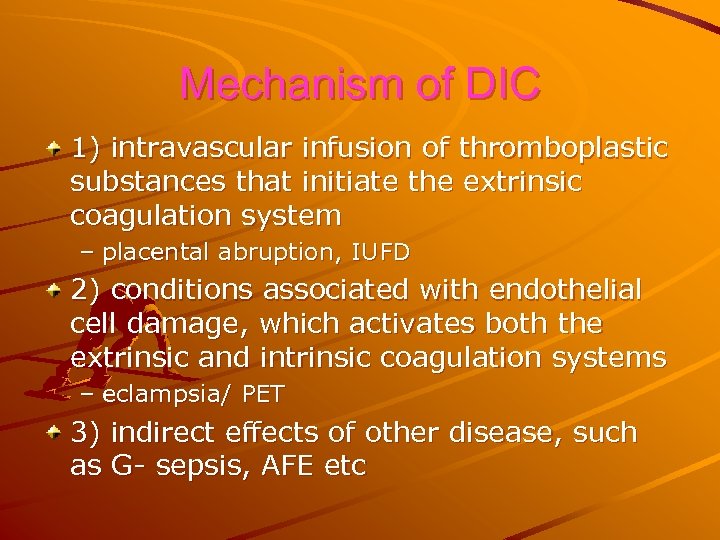
Mechanism of DIC 1) intravascular infusion of thromboplastic substances that initiate the extrinsic coagulation system – placental abruption, IUFD 2) conditions associated with endothelial cell damage, which activates both the extrinsic and intrinsic coagulation systems – eclampsia/ PET 3) indirect effects of other disease, such as G- sepsis, AFE etc

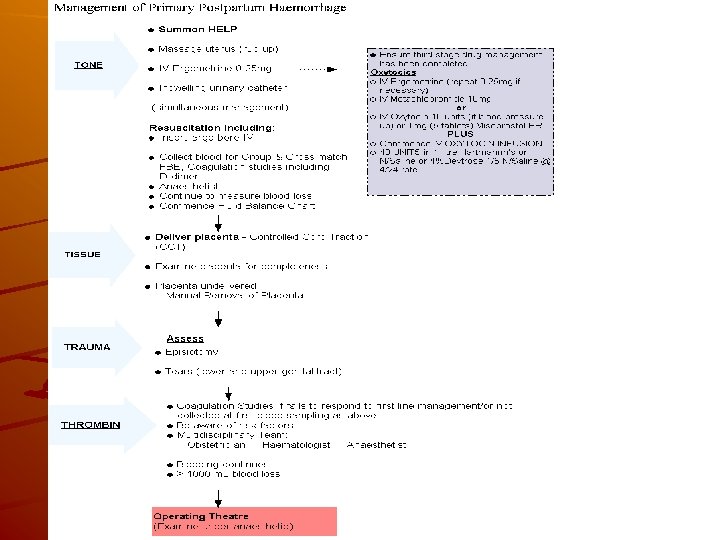
Preventative Management PPH · Detect and treat antenatal anaemia · Active Management of Third Stage · Administration of a prophylactic oxytocin · Early cord clamping · Controlled cord traction of the umbilical cord. Advantage of active management = reduction in the incidence of PPH by 40% IV access plus collect blood for grouping and cross matching if assessed as at risk.
Available from Royal Women’s Hospital, Carlton, Clinical Practice Guidelines: http: //www. rwh. org. au/rwhcpg/womenshealth. cfm? doc_id= 3333
Management Principles Organisation restoration of blood volume correction of coagulopathy evaluating response to treatment monitoring PR, BP, CVP, ABG, UOP If resuscitation is adequate P & BP should return to normal treat the cause abruption placenta praevia uterine rupture placenta accreta
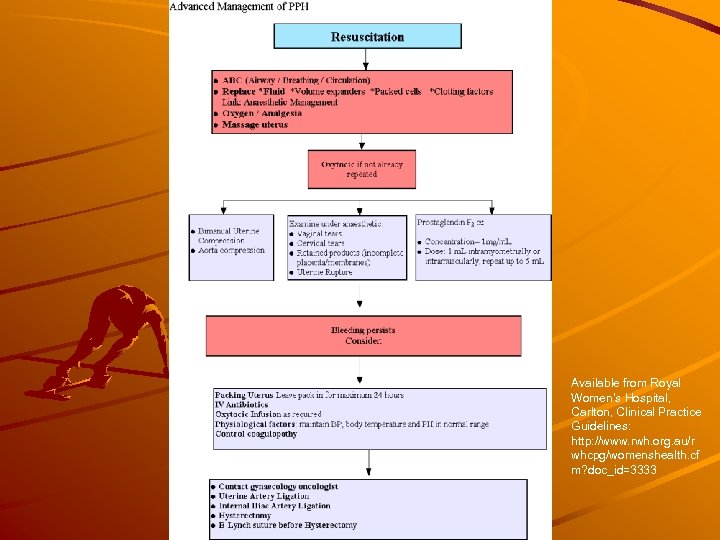
Available from Royal Women’s Hospital, Carlton, Clinical Practice Guidelines: http: //www. rwh. org. au/r whcpg/womenshealth. cf m? doc_id=3333
NON-HAEMORRHAGIC OBSTETRIC SHOCK Uncommon but responsible for majority of maternal deaths in developed countries. -Amniotic fluid embolus -Acute uterine inversion
Amniotic Fluid Embolism – – – Passage of amniotic fluid debris into maternal circulation Obstructs pulmonary circulation Cardio-respiratory arrest
AMNIOTIC FLUID EMBOLISM Clinical features – Multiparous women – Precipitous labour – Presence of intact membranes – Sudden dyspnea – Hypotension – Seizure activity not uncommon – If survive initial insult 70% suffer non-cardiogenic pulmonary oedema ARDS
AMNIOTIC FLUID EMBOLISM Diagnosis – Consider in all obstetric patients with sudden collapse. – Differential PTE Septic shock MI Aspiration pneumonia Allergy to drug
Management Secure airway treat cardiovascular collapse central venous line acute left ventricular failure: digoxin dopamine correct coagulopathy treat metabolic/electrolyte abnormalities

Acute Uterine Inversion Most commonly arises from mismanaged 3 rd stage
Presentation Sudden collapse in 3 rd stage Degree of shock inconsistent with blood loss Shock is neurogenic in nature Traction on infundibular pelvic ligament May be no palpable fundus Mass in vagina/introitus
Management Avoid mismanagement of 3 rd stage of labour Once occurs – Anti-shock measures – If placenta still attached remove after uterus is replaced – Manual replacement of uterus – O’Sullivans hydrostatic pressure – Surgical correction
Shoulder Dystocia
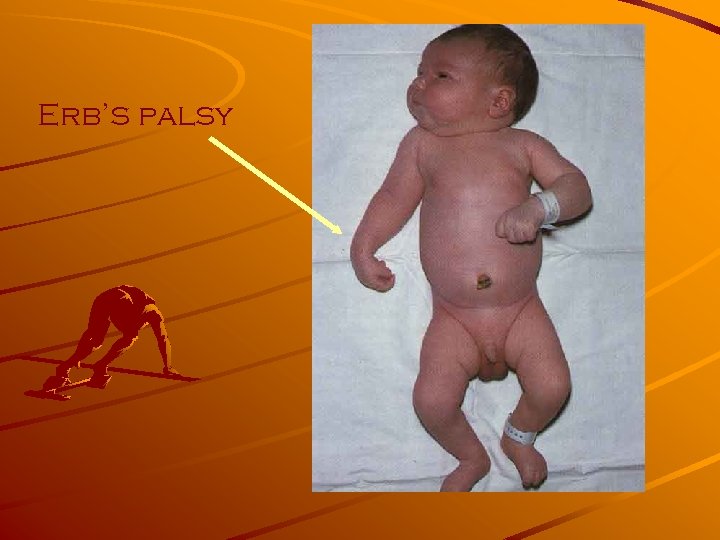
Erb’s palsy
‘It all comes, ’ said Pooh crossly, ‘of not having front doors big enough’
‘It all comes’, said Rabbit sternly, ‘of eating too much’
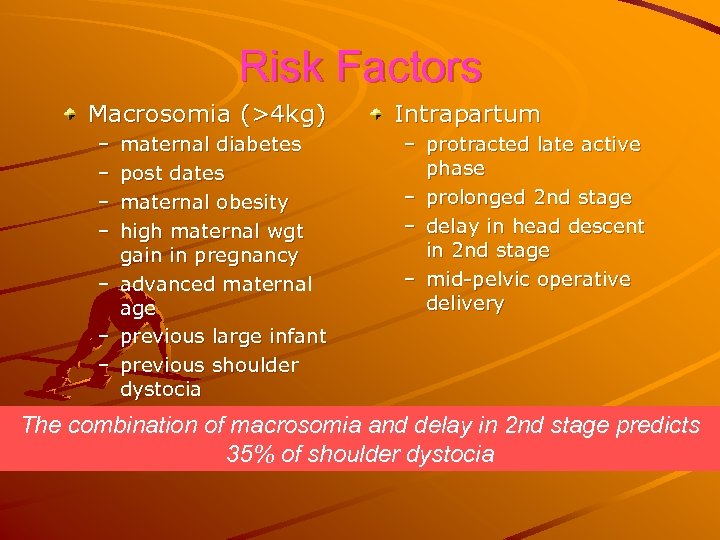
Risk Factors Macrosomia (>4 kg) – – – – maternal diabetes post dates maternal obesity high maternal wgt gain in pregnancy advanced maternal age previous large infant previous shoulder dystocia Intrapartum – protracted late active phase – prolonged 2 nd stage – delay in head descent in 2 nd stage – mid-pelvic operative delivery The combination of macrosomia and delay in 2 nd stage predicts 35% of shoulder dystocia
Eclampsia 1/1500
Complications Cerebrovascular injury pulmonary oedema coagulopathy maternal/fetal death HELLP syndrome
Presentation Hypertension, hyperreflexia, clonus, headache, visual changes, seizure 20% have diastolic BP<90, normal reflexes, and urinary protein <2+ 70% of deaths due to intracerebral haemorrhage
Management • Goals: – Stabilization of the mother/seizure control • Mg. SO 4 therapy: 4 -6 g over 20 min followed by infusion of 1 -3 g/hr, OR • Thiopental or diazepam followed by Mg. SO 4 infusion – Airway management – Avoiding aspiration
Prolapsed Cord 1/500 deliveries Most occur during ARM
Presentation Cord visible outside the introitus CTG abnormalities appear – variable decelerations – fetal bradycardia Note: fetal or maternal injury due to hasty intervention

Management Keep cord warm - replacing in vagina may help Keep pressure off cord by gloved hand in vagina lifting fetal part off the cord Positioning, Maternal O 2, IV access If fetus is alive, operative delivery CS if not able to deliver vaginally If fetus is dead, vaginal delivery if presentation allows
Anaphylaxis vasodilatation, smooth muscle contraction, glandular secretion, increased capillary permeability Management: – oxygen – colloid – bronchodilator – adrenaline (despite Ux stimulatory effect) – anti-histamine (if angioneurotic oedema) – steroid (for refractory bronchospasm)
Maternal cardiac emergency Acute: – AMI – Tocolytic therapy – Aortic dissecting aneurysm – Peripartum cardiomyopathy: 1 in 50000, 50% progress to end-stage heart failure (heart Tx), 50% recurrence. Suspect if acute SOB, chest pain, ab. N ECG, signs LVF/RVF – Traumatic myocardial contusion: ie: MCA
Drug Overdose Illicit drugs: heroin, cocaine and amphetamines (these 2 can cause hypertension, ^ C. O. , decrease Uterine blood flow, APH, cerebral haemorrhage, convulsions, arrhythmias). Drug overdose Drug error Anaphylaxis Hypermagnesaemia: – wide QRS on ECG, 5 -6 mmol/l lose tendon reflex – resp. paralysis, SA and AV node block – cardiac arrest. Treatment: Ca. Gluconate 10% 10 ml slow IV
CARDIO-PULMONARY ARREST Cardiac arrest rare in pregnancy (1 in 30000 deliveries) Usually associated with particular obstetric complications like amniotic fluid embolism, drug toxicity from Magnesium sulphate & local anesthetics.
Technique for external cardiac massage: External cardiac massage in non-obstetric patient provides 30% cardiac output. After 20 weeks reduced further due to veno-caval compression. Relief of aorto-caval compression part of BLS: û û û left lateral tilt --- decreased efficacy of compressions wedge 270 angle allows 80% of maximal force to be dissipated rescuer’s thigh as wedge. Sodium bicarbonate controversial as it leads to fetal acidosis but p. H has to be kept above 7. 30 to prevent uterine vasoconstriction. International Liaison Committee on Resuscitation (ILCOR) “ if there is no response to ALS, peri-mortem caesarean delivery should be made within 5 minutes of arrest”
TRAUMA Occurs in 6 -7% of all pregnancies. Hospital admissions only 0. 3 - 0. 4 % of all pregnancies. 1% of all trauma cases are pregnant. Maternal deaths associated most commonly with head injuries & severe hemorrhage. Fetal deaths associated with placental abruption & maternal death.
Management Initial resuscitation should follow normal plan of ABC. Hypotension may not be present until 35% or more blood volume is lost. Aorto-caval compression release Rule out pelvic fractures, uterine injury & retro -peritoneal hemorrhage Fetal monitoring with cardio-tocographic monitor Rh immunoglobulin – within 72 hours. Radiation hazards: 1 st trimester >5 rads Chest x-ray < 5 rads Pelvic film <1 rads Abdomino-pelvic CT scan 5 -10 rads
BURNS Increased levels of prostaglandins predispose to pre-term labour. Replacement of fluids vis-à-vis increased volumes in pregnancy. Inhalational injury- hypoxia & carbon monoxide poisoning Infections- prophylactic antibiotics controversial Topical Povodine iodine- affects fetal thyroid functions


a77ef78dffdfb53a73c7e37d740d5062.ppt