0c13bf4e5b4718b1ae5c0299b1f9908e.ppt
- Количество слайдов: 26
OB Anesthesia Denise Weiss DO Anesthesiologist
Goals of obstetrics Healthy mom/baby = happy and healthy doctors and nurses, family
OB Anesthesia • NPO guidelines – – Solid food (fatty foods) = 8 hrs Light meal (toast, crackers, etc) = 6 hours Clear liquids =2 hours Breast milk = 4 hours – On L/D clear liquids ok during labor, (often only ice chips allowed) – Stricter adherence to ice chips if higher risk of operative delivery – Scheduled inductions should be instructed to be NPO – All pregnant pts are considered to have full stomachs but the goal is to minimize risk if need for intubation occurs
OB Anesthesia • Reasons for NPO guidelines: – Higher risk of aspiration in pregnant patients (1 in 661 vs 1 in 2131 gen pop) • • • Increased intragastric pressure due to large uterus LES is pushed up and to the left (sim to hiatal hernia) Decreased LES tone secondary to progesterone High incidence of GERD Gastric p. H is more acidic Active phase of labor slows gastric emptying
OB Anesthesia • Higher risk of difficulty in airway management – Morbidity/mortality in pregnant pts have been attributed often to failed or difficulty managing the airway – Airway is more friable and edematous in pregnant pts – Increased breast size can make laryngoscopy very difficult – Decreased FRC so desaturate quickly
OB Anesthesia • p. H less than 2. 5 and gastric volume greater than 25 ml are identified risk factors for aspiration • Pregnant pts going to CS either emergently or scheduled receive pharmacologic prophylaxis (we use reglan and alka selzer gold, bicitra increases p. H without altering volume)
OB Anesthesia • Difficult airway – Incidence of failed intubation in obstetric pts @1: 300 – 1: 2330 in general OR population – Airway complications are the leading cause of anesthesia mortality – Single largest class of injury related claims from the ASA Closed Claims database involves respiratory events
OB Anesthesia • Basic Needs for the OR – Monitors • ECG, NIBP, SPO 2, FHR monitor, suction • Equipment for difficult airway, and emergency drugs • Checked daily
OB Anesthesia for C-Section • • • Spinal Epidural Combined Spinal/epidural General Local
Contraindications for Neuraxial Techniques • Pt refusal or inability to cooperate • Increased ICP secondary to mass lesion • Skin or soft tissue infection at site of needle placement • Coagulopathy • Uncorrected maternal hypovolemia • Low platelets (depends)
Complications with Neuraxial Techniques Infection Postdural Puncture Headache Incomplete or failed block Neurologic injury(incidence is 20 in 1. 2 million for subarachnoid blocks, 20 in 450, 000 for epidurals) • Meningitis or arachnoiditis • Spinal hematoma(sharp back and leg pain-numbness and motor dysfunction(loss of bowel/bladder fxn) • Emergent MRI or CT and referral (6 -12 hr window for decompression) • •
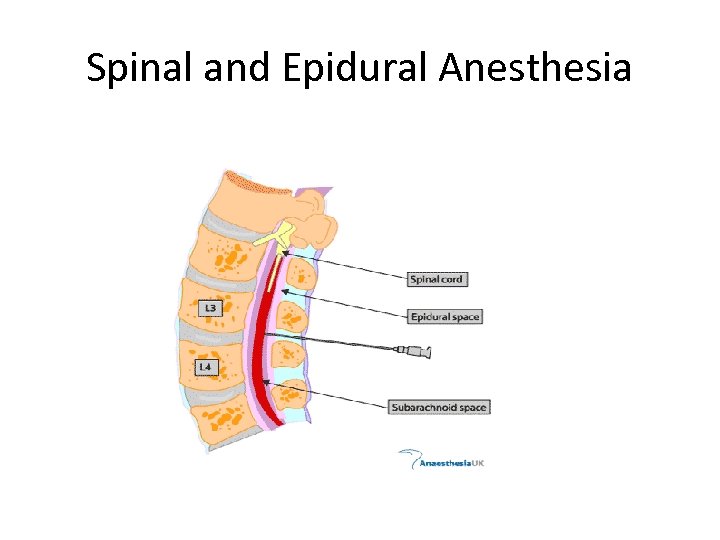
Spinal and Epidural Anesthesia
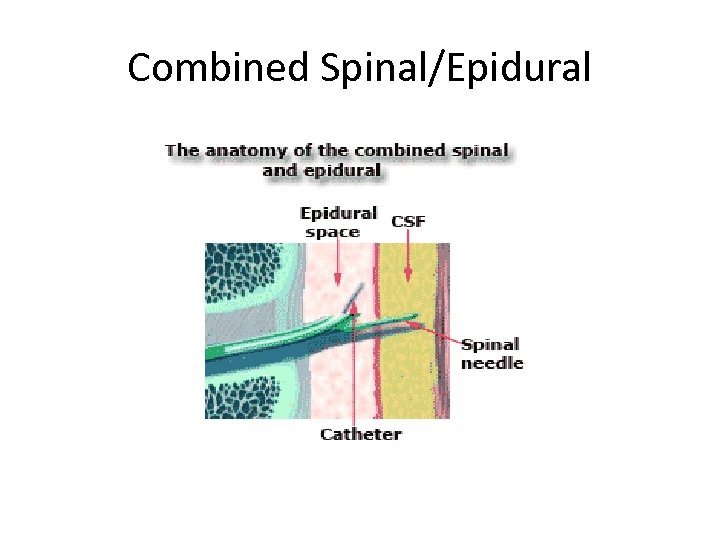
Combined Spinal/Epidural
General Anesthesia • Maternal refusal or inability to cooperate with neuraxial tech • Presence of contraindication to neuraxial tech • Insufficient time to induce neuraxial tech(cord prolapse with persistent bradycardia) • Failure of neuraxial technique • Fetal issues (EXIT procedure)
Local Anesthesia • Very rarely used • Dire emergencies when anesthesiologist/CRNA not available • Success dep on avoiding use of retractors, and not exteriorizing the uterus. • After delivery of baby, obtain hemostasis until arrival of anesthesia personnel
Local Anesthesia • 0. 5% lidocaine with epi • 25 g spinal needle to create skin wheal just below umbilicus directed toward symphysis pubis. SQ injection along this full area. • Ideally wait 3 -4 min to take effect • Vertical incision to rectus then local into rectus fascia and muscles. Takes 4 -5 min for anesthesia to be complete
Local Anesthesia • • • Parietal peritoneum infiltration and incision Visceral peritoneum infiltration and incision Paracervical injection Uterine incision and delivery Obtain hemostasis Await availability of general anesthesia
Local Anesthesia • Disadvantages – Pt discomfort – Risk for local anesthetic toxicity (may use up to 100 ml of local – Difficult operating conditions to say the least
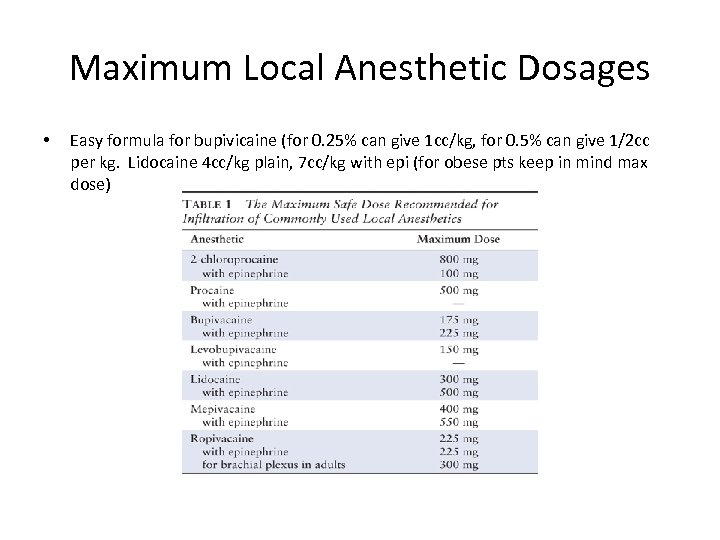
Maximum Local Anesthetic Dosages • Easy formula for bupivicaine (for 0. 25% can give 1 cc/kg, for 0. 5% can give 1/2 cc per kg. Lidocaine 4 cc/kg plain, 7 cc/kg with epi (for obese pts keep in mind max dose)
PCA Fentanyl • Great alternative for pts who cannot have an epidural – All opioids cross placenta by diffusion secondary to lipid solubility – All are associated with neonatal depression – Fentanyl readily crosses placenta but avg umbilical to maternal conc ratio is low at 0. 31 – Studies show reduced FHR variability but difference in APGAR scores, respiratory depression and Neurologic and Adaptive Capacity scores at 2 -4 hrs or 24 hrs compared to infants whose mothers did not have fentanyl(Am Journal of Obst/Gyn; Anesth/Analgesia)
PCA Fentanyl • • • Rapid onset High potency Short duration No active metabolites One of most commonly used for PCA
PCA Fentanyl • • Must have resuscitation equip available Pulse oximetry, +/- et. CO 2 monitoring One/one nursing Education of family members Loading dose (50 -150 mcg Bolus 25 -50 mcg(start at 25, and assess) Lockout 10 min No basal rate
PCA Fentanyl • As labor progresses may need to decrease lockout time to 5 min
OB in Rural Areas • Likely will not have immediately available anesthesia provider • OB nurses can assist with management of epidural infusions • ASA has a consultation program that will help with setting up the anesthesia service to fit the needs of the facility • Consensus of all involved that OB anesthesia is a priority and a worthwhile goal
OB in Rural Areas • Anesthesia provider does NOT have to stay in house during course of epidural infusion • ASA recommends it but recognizes difficulty
Questions? ? ?
0c13bf4e5b4718b1ae5c0299b1f9908e.ppt