55429c8ce1f1924ac1f94d78ce7efb52.ppt
- Количество слайдов: 57

NUTRITION, MALNUTRITION, AND FEEDING ISSUES
OBJECTIVES Know and understand: • Age-related changes in nutritional health • Nutritional syndromes common in older people • The fundamental clinical approach to difficulties with feeding Slide 2
TOPICS COVERED • Age-related Nutritional Changes and Needs • Screening and Assessment • Nutrition Syndromes • Nutritional Interventions • Oral Health • Dysphagia • Feeding and PEG Tubes Slide 3
AGE-RELATED NUTRITIONAL CHANGES • Body composition • Energy requirements • Macronutrient needs • Micronutrient requirements • Fluid needs Slide 4
CHANGES IN BODY COMPOSITION WITH AGE • Bone mass, lean mass, water content • Total body fat, commonly with intraabdominal fat stores • Cannot generalize well-standardized nutrient requirements of young or middle-aged adults to older adults Slide 5
ENERGY REQUIREMENTS OF OLDER ADULTS • Reduced basal metabolic rate (BMR) in older adults reflects loss of muscle mass • BMR is the principal determinant of total energy expenditure • Estimation of energy needs based on body weight: 25 to 30 kcal/kg/day • Avoid overfeeding, while still meeting basal requirements Slide 6

MACRONUTRIENT NEEDS (1 of 2) Slide 7
MACRONUTRIENT NEEDS (2 of 2) • Protein: 0. 8 g/kg/day (1. 5 g/kg/day under stress) • Fat: 20%– 35% of total energy intake per day, with reduced cholesterol, saturated fat, and trans fatty acids • Carbohydrate: 45%– 65% of total energy intake per day, with complex carbohydrate as the preferred fiber source • Fiber: 30 g/day (men), 21 g/day (women) Slide 8
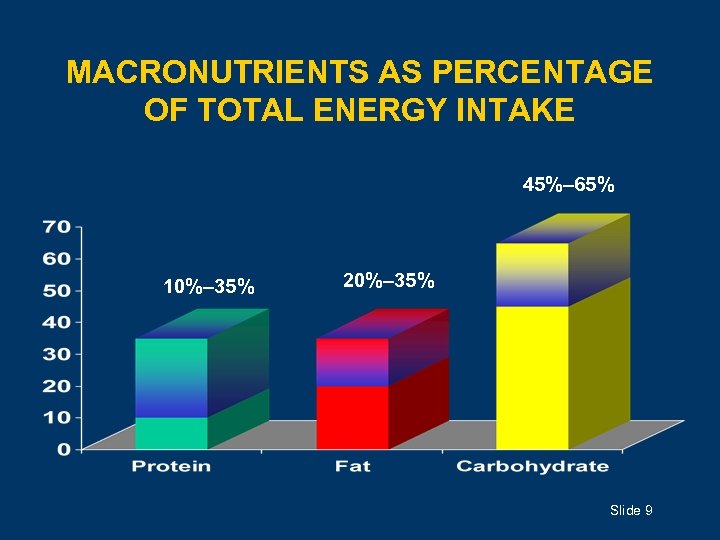
MACRONUTRIENTS AS PERCENTAGE OF TOTAL ENERGY INTAKE 45%– 65% 10%– 35% 20%– 35% Slide 9
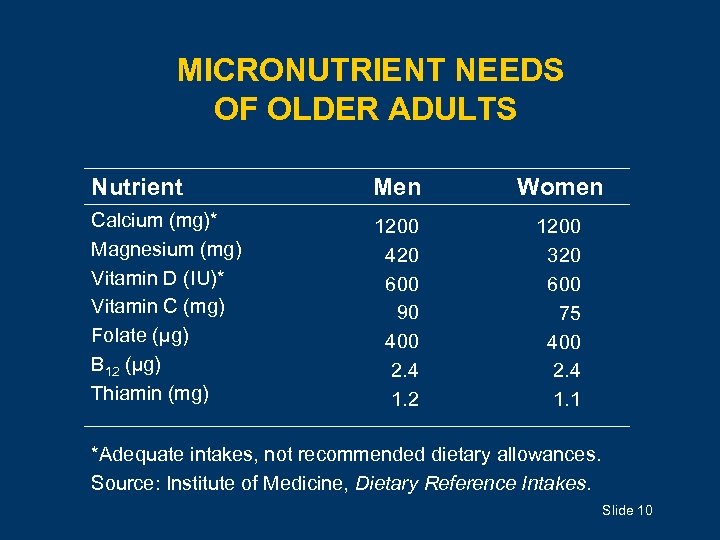
MICRONUTRIENT NEEDS OF OLDER ADULTS Nutrient Men Women Calcium (mg)* Magnesium (mg) Vitamin D (IU)* Vitamin C (mg) Folate (µg) B 12 (µg) Thiamin (mg) 1200 420 600 90 400 2. 4 1. 2 1200 320 600 75 400 2. 4 1. 1 *Adequate intakes, not recommended dietary allowances. Source: Institute of Medicine, Dietary Reference Intakes. Slide 10
FLUID NEEDS OF OLDER ADULTS • Dehydration is the most common fluid or electrolyte disturbance in older adults • Decreased perception of thirst is associated with normal aging • Also associated with normal aging: Ø Decreased response to serum osmolarity Ø Reduced ability to concentrate urine following fluid deprivation • 30 ml/kg/d or 1 ml/kcal ingested Slide 11
COMMON SIGNS OF DEHYDRATION • Decreased urine output • Constipation • Mucosal dryness • Confusion Slide 12
NUTRITION SCREENING AND ASSESSMENT • Anthropometrics • Nutritional intake • Laboratory tests • Drug-nutrient interactions Slide 13
ANTHROPOMETRICS • Includes measures of weight and height Ø Body mass index (BMI) = weight in kg/height in m 2 Ø Risk threshold for low BMI = 18. 5 kg/m 2 • Weight loss of 5% in 1 month or 10% in 6 months is a useful indicator of nutritional risk and morbidity and is predictive of: Ø Functional limitations Ø Health care charges Ø Need for hospitalization Slide 14
NUTRITIONAL INTAKE • Inadequate nutritional intake has been defined as average intake of food groups, nutrients, or energy 25% to 50% below a threshold level of the RDA • Minimum Data Set uses different measure: intake of <75% of food provided triggers nutritional assessment in nursing homes • 5% to 18% of nursing home residents do not meet standards for adequate nutritional intake Slide 15
LABORATORY TESTS: ALBUMIN • A risk indicator for morbidity and mortality; however, lacks sensitivity and specificity as a nutritional indicator • The prognostic value of low albumin (<3. 5 g/d. L) is probably as a marker for injury, disease, or inflammation • Prealbumin may better reflect short-term changes in protein status (because of shorter half-life) but has largely the same limitations as albumin Slide 16
LABORATORY TESTS: SERUM CHOLESTEROL • Acquired hypocholesterolemia (<160 mg/d. L) is a nonspecific feature of poor health status that is independent of nutrient or energy intake • May reflect a proinflammatory condition • Community-dwelling older adults with both low albumin and low cholesterol have higher rates of morbidity and mortality than those with either low albumin or low cholesterol alone Slide 17
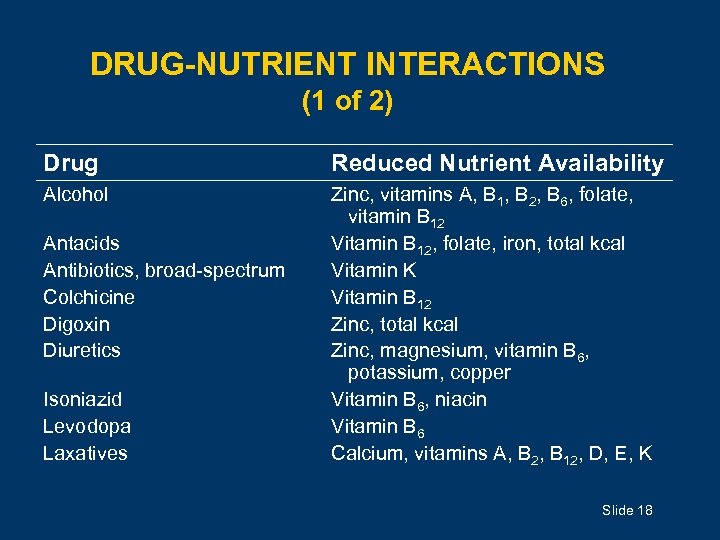
DRUG-NUTRIENT INTERACTIONS (1 of 2) Drug Reduced Nutrient Availability Alcohol Zinc, vitamins A, B 1, B 2, B 6, folate, vitamin B 12 Vitamin B 12, folate, iron, total kcal Vitamin K Vitamin B 12 Zinc, total kcal Zinc, magnesium, vitamin B 6, potassium, copper Vitamin B 6, niacin Vitamin B 6 Calcium, vitamins A, B 2, B 12, D, E, K Antacids Antibiotics, broad-spectrum Colchicine Digoxin Diuretics Isoniazid Levodopa Laxatives Slide 18
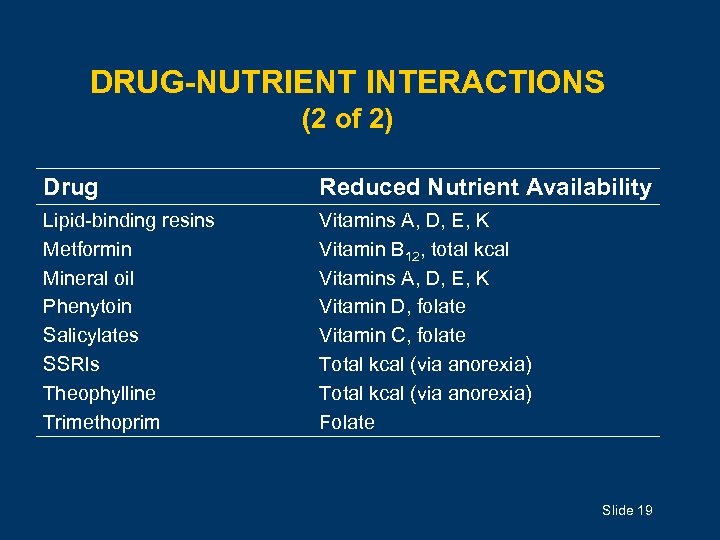
DRUG-NUTRIENT INTERACTIONS (2 of 2) Drug Reduced Nutrient Availability Lipid-binding resins Metformin Mineral oil Phenytoin Salicylates SSRIs Theophylline Trimethoprim Vitamins A, D, E, K Vitamin B 12, total kcal Vitamins A, D, E, K Vitamin D, folate Vitamin C, folate Total kcal (via anorexia) Folate Slide 19
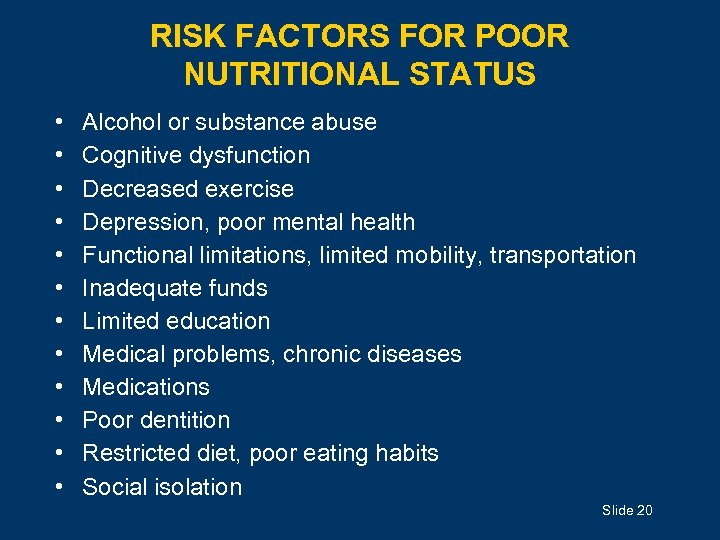
RISK FACTORS FOR POOR NUTRITIONAL STATUS • • • Alcohol or substance abuse Cognitive dysfunction Decreased exercise Depression, poor mental health Functional limitations, limited mobility, transportation Inadequate funds Limited education Medical problems, chronic diseases Medications Poor dentition Restricted diet, poor eating habits Social isolation Slide 20
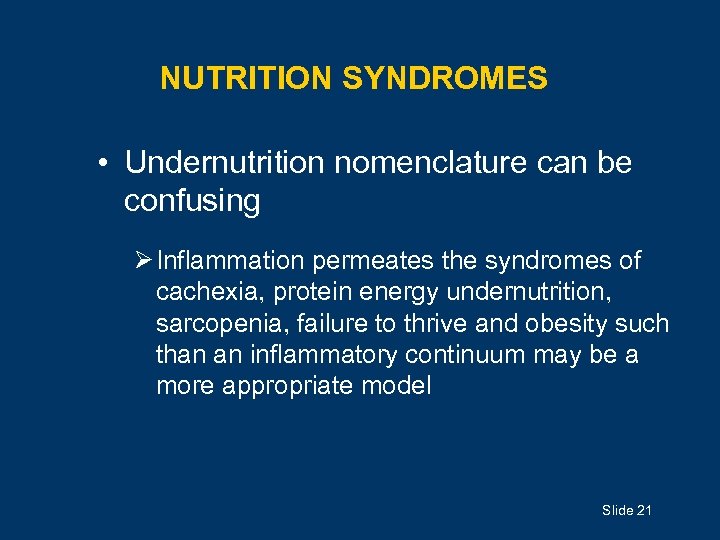
NUTRITION SYNDROMES • Undernutrition nomenclature can be confusing Ø Inflammation permeates the syndromes of cachexia, protein energy undernutrition, sarcopenia, failure to thrive and obesity such than an inflammatory continuum may be a more appropriate model Slide 21
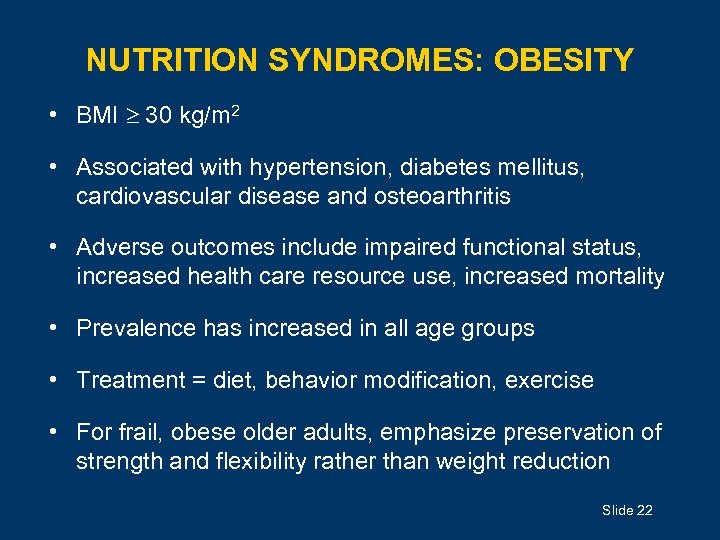
NUTRITION SYNDROMES: OBESITY • BMI 30 kg/m 2 • Associated with hypertension, diabetes mellitus, cardiovascular disease and osteoarthritis • Adverse outcomes include impaired functional status, increased health care resource use, increased mortality • Prevalence has increased in all age groups • Treatment = diet, behavior modification, exercise • For frail, obese older adults, emphasize preservation of strength and flexibility rather than weight reduction Slide 22
PREVENTING UNDERNUTRITION • Cater to patient’s food preferences • Avoid restrictive “therapeutic diets” unless clinical value is certain • Enhance patient’s preparedness for meal; provide assistance if needed • Enhance taste and appearance of food • Enhance social aspect; provide adequate time • Address dental/oral complaints of chewing discomfort/dysfunction Slide 23
DIETARY SUPPLEMENTS • May result in reduced intake of normal diet, but overall effect on nutrient intake unclear • Contain macro- and micronutrients • Available in liquid and bar forms • Most formulas provide 1 to 1. 5 calories/m. L and many are lactose- and gluten-free Slide 24
DRUG TREATMENT FOR UNDERNUTRITION SYNDROMES Appetite stimulants may improve appetite but their effect on weight and meaningful clinical outcomes are unproven. These agents should be used rarely, if ever. Appetite stimulants • Antidepressant: mirtazapine • Cyproheptadine • Megestrol Anabolic agents • Human growth hormone • Testosterone Slide 25

EATING AND NORMAL AGING • Taste sensation but not discrimination is diminished: Ø Tendency to add more salt and sweetener (especially sugar) to food Ø Can still discriminate sweet from salty • Diminished olfactory function further impairs taste sensation Slide 26
CHEMOSENSORY PERCEPTION • Olfactory function declines with age • Changes in perceived degree of saltiness and sweetness • Complaints of taste and smell dysfunction are common in older adults • Drugs may adversely affect smell and taste Slide 27
COMMON BUT NORMAL • Xerostomia (but salivary function not significantly reduced with aging) • Reduced chewing efficiency and efficacy with loss of multiple teeth • Esophageal dysmotility Slide 28
ORAL CAVITY • Dysfunction and disease in the mouth may be important risk factors for nutritional impairment • Increasing age and history of prior restorative dentistry make teeth less sensitive, thereby predisposing to unnoticed and more possibly irreparable tooth destruction • Dry mouth, decay, missing teeth, and periodontal disease are common but do not represent normal aging Slide 29
THREE PHASES OF SWALLOWING • Preparatory or oral phase: Voluntary; includes the complex activities of mastication and propelling the food bolus to the back of the mouth toward the pharynx • Pharyngeal phase: Involuntary initiation of the swallow reflex; food propelled into the esophagus • Esophageal phase: Food propelled down the esophagus by the action of skeletal muscle proximally and smooth muscle distally; regulated by its own intrinsic innervation Slide 30
DYSPHAGIA (difficulty with swallowing) • Oral dysphagia: Difficulty with voluntary transfer of food from mouth to pharynx (eg, due to xerostomia, or in dementia) • Pharyngeal dysphagia: Difficult reflexive transfer of food bolus from pharynx to initiate the involuntary esophageal phase while simultaneously protecting the airway (eg, after stroke) • Esophageal dysphagia: Sensation of food being “stuck” after swallow (eg, in esophageal motility disorder or with mechanical obstruction) Slide 31
ASPIRATION • Defined as misdirection of pharyngeal contents into the airway • Aspiration pneumonia occurs when an inoculum of bacteria large enough to overcome host defenses arrives in the lung Slide 32
SOURCES OF ASPIRATION • Oral and oropharyngeal fauna Ø Exacerbated in case of salivary hypofunction, when intrinsic antimicrobial defenses are diminished • Gastric contents (Mendelson’s syndrome) Ø Usually results in a chemical pneumonitis Ø Usefulness of prophylactic antibiotics questionable • Most often, local host defenses clear the lung of offending aspirate without serious clinical impact Slide 33
ASSESSMENT OF OROPHARYNGEAL DYSPHAGIA • Full bedside evaluation • Video-fluoroscopic deglutition examination (VDE) by a speech-language pathologist Ø A variant of the modified barium swallow Ø Data conflict regarding usefulness of VDE and subsequent treatment Slide 34
INTERVENTIONS FOR DYSPHAGIA • Swallow therapy: Ø Compensatory (eg, turn head toward weaker side while swallowing) Ø Indirect (eg, exercises to improve the strength of the involved muscles) Ø Direct (eg, exercises to perform while swallowing, such as swallowing multiple times per bolus) • Diet modification: altering bolus size or consistency Slide 35
TUBE FEEDING • Indications not clearly established • Routes: nasoenteric, percutaneous endoscopic gastrostomy (PEG), jejunostomy tubes • Requires high level of care • Selection of formula depends on multiple factors • Aspiration is the most serious common complaint; occurs in 23%– 58% with PEG • Most older people require 1500– 2400 m. L of 1 kcal/m. L solution over 24 h to meet nutritional needs Slide 36
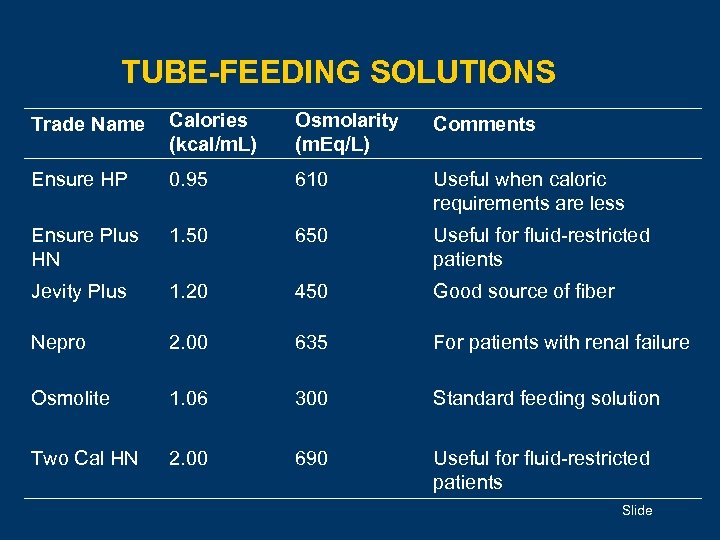
TUBE-FEEDING SOLUTIONS Trade Name Calories (kcal/m. L) Osmolarity (m. Eq/L) Comments Ensure HP 0. 95 610 Useful when caloric requirements are less Ensure Plus HN 1. 50 650 Useful for fluid-restricted patients Jevity Plus 1. 20 450 Good source of fiber Nepro 2. 00 635 For patients with renal failure Osmolite 1. 06 300 Standard feeding solution Two Cal HN 2. 00 690 Useful for fluid-restricted patients Slide
PARENTERAL NUTRITION • Indications not clearly established • A consideration only when GI tract cannot be used for extended period • Older people tolerate total parenteral nutrition as well as younger patients • Fluid issues and dextrose tolerance may be of concern Slide 38
REFEEDING SYNDROME • Results from overzealous enteral or parenteral feedings following severe undernutrition • Characterized by severe electrolyte abnormalities and fluid retention • Avoid by cautiously advancing nutritional therapy and closely monitoring fluid and electrolyte status Slide 39
FEEDING • When older adults experience difficulty eating, the two main approaches are: Ø Careful feeding by hand: Labor intensive Ø Tube feeding: Invasive intervention with its own risks • Data about either are limited; no randomized controlled trials have compared the two directly Slide 40
PERCUTANEOUS ENDOSCOPIC GASTROSTOMY (PEG) TUBES • Low procedure-related complication rates; however, long-term studies reveal substantial mortality • No studies demonstrate improved survival, reduced incidence of pneumonia or other infections, improved symptoms or function, or reduced incidence of pressure sores • Median survival after PEG is < 1 year • Complications include risk of aspiration pneumonia, metabolic disturbances, local cellulitis, diarrhea, diminished social contact Slide 41
DECISIONS ABOUT ARTIFICIAL NUTRITION • Artificial feeding may be withheld or terminated in accordance with a patient’s wishes, with careful consideration of additional comorbidities and futility • Patient and surrogate should have appropriate counseling of the consequences of various options for care Slide 42
SUMMARY • Nutritional concerns affect many aspects of health and disease in older adults • Swallowing is an important and complex task that can be affected by both normal aging and diseases that are common in older adults Slide 43
CASE 1 (1 of 4) • An 83 -year-old nursing home resident with advanced Alzheimer’s disease has steadily lost nearly 8. 2 kg (18 lb), or 11% of his weight, over 11 months. • His current weight is 66. 2 kg (146 lb; body mass index, 22 kg/m 2). • He gained about 8. 2 kg (18 lb) 6 years ago, after he entered the nursing home, and maintained his weight until this year. • He has not had any hospitalizations, acute infections, or other serious medical problems in the last 20 months. Since his admission, he has had a slow, steady decline in cognitive function. Slide 44
CASE 1 (2 of 4) • The patient is fully ambulatory and attends most meals in the residents’ dining hall; he needs minimal feeding assistance (set-up only). • He is on a 2, 600 -kcal regular diet that was modified to include finger foods and nightly snacks. • According to chart documentation, he only rarely consumes <75% of the food served, but a 2 -day calorie count indicates that his consumption is closer to 40% of what he is served. Slide 45
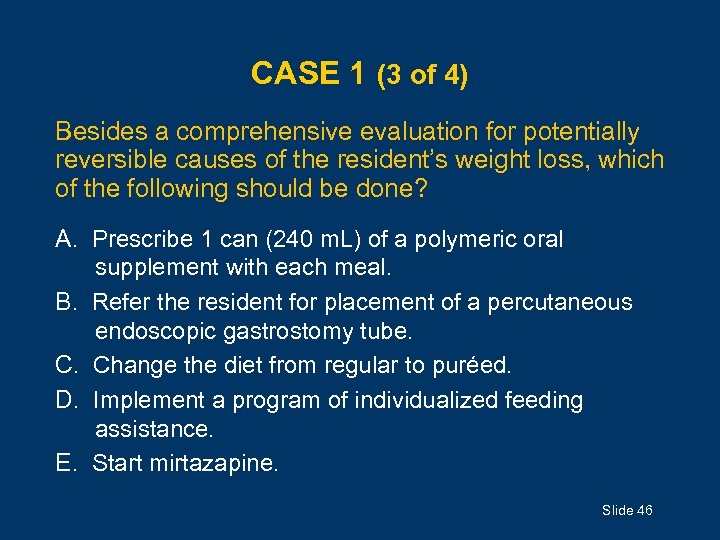
CASE 1 (3 of 4) Besides a comprehensive evaluation for potentially reversible causes of the resident’s weight loss, which of the following should be done? A. Prescribe 1 can (240 m. L) of a polymeric oral supplement with each meal. B. Refer the resident for placement of a percutaneous endoscopic gastrostomy tube. C. Change the diet from regular to puréed. D. Implement a program of individualized feeding assistance. E. Start mirtazapine. Slide 46
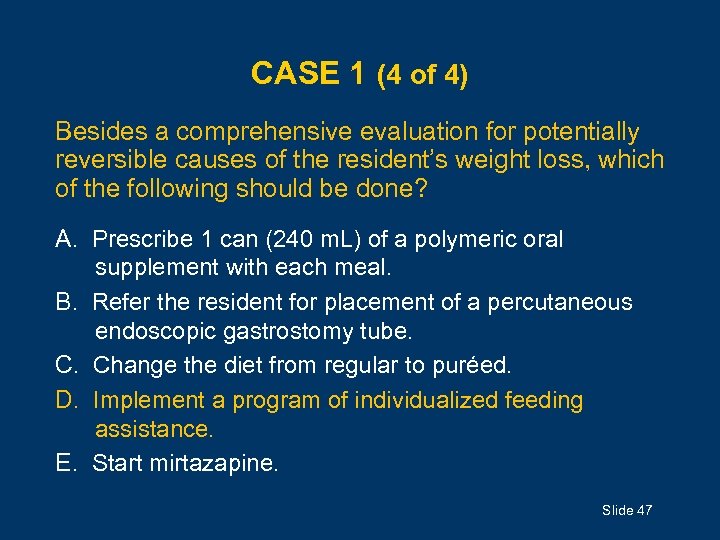
CASE 1 (4 of 4) Besides a comprehensive evaluation for potentially reversible causes of the resident’s weight loss, which of the following should be done? A. Prescribe 1 can (240 m. L) of a polymeric oral supplement with each meal. B. Refer the resident for placement of a percutaneous endoscopic gastrostomy tube. C. Change the diet from regular to puréed. D. Implement a program of individualized feeding assistance. E. Start mirtazapine. Slide 47
CASE 2 (1 of 5) • An 88 -year-old man comes to the clinic for the first time in 18 months, accompanied by his son. • The patient says he has no active medical problems. He has lived alone since his wife’s death 10 years ago. He is not sexually active and does not smoke or drink alcohol. • The son says his father has lost weight, is less active socially than formerly, has little energy or endurance, and spends most of his time reading or watching television. • On detailed questioning, the patient says he often skips meals but otherwise feels his appetite is unchanged. He does all his own cooking. His son notes that when his dad comes to his house on weekends, he eats well. Slide 48
CASE 2 (2 of 5) • The patient says he does not have problems sleeping, swallowing, or voiding. He has had no change in bowel habits, no incontinence, and no depressive symptoms. • History includes early-stage prostate cancer, for which he had a prostatectomy 8 years ago; at follow-up 1 year ago, his urologist told him there was no evidence of recurrence. Screening colonoscopy done 2 year ago was normal. The patient takes a daily multivitamin. • The patient weighs 62. 6 kg (138 lb; body mass index, 22 kg/m 2), which, according to medical records, is 13% less than he weighed 18 months ago. The rest of his physical exam is normal. Slide 49
CASE 2 (3 of 5) • His score on the Mini–Mental State Examination is 29/30; his score on the Yesavage Geriatric Depression Scale– Short Form is 2/15. • Fecal guaiac is negative. Urinalysis, CBC, electrolytes, vitamin B 12, and liver, renal, and thyroid function tests are normal, and prostate-specific antigen is undetectable. • ECG reveals normal sinus rhythm, and chest radiography is normal. Slide 50
CASE 2 (4 of 5) Which of the following is the most appropriate next step? (A) CT of the chest, abdomen, and pelvis (B) Upper and lower endoscopy (C) Upper GI series with small-bowel follow-through (D) Complete radiographic bone survey (E) No further diagnostic testing Slide 51
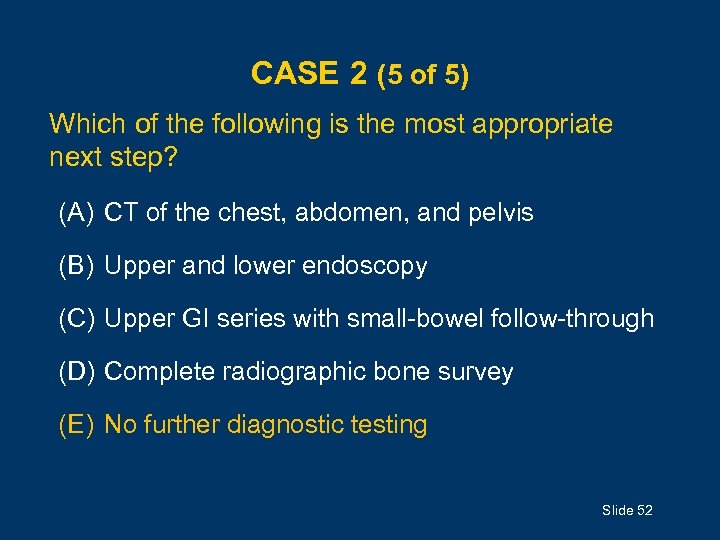
CASE 2 (5 of 5) Which of the following is the most appropriate next step? (A) CT of the chest, abdomen, and pelvis (B) Upper and lower endoscopy (C) Upper GI series with small-bowel follow-through (D) Complete radiographic bone survey (E) No further diagnostic testing Slide 52
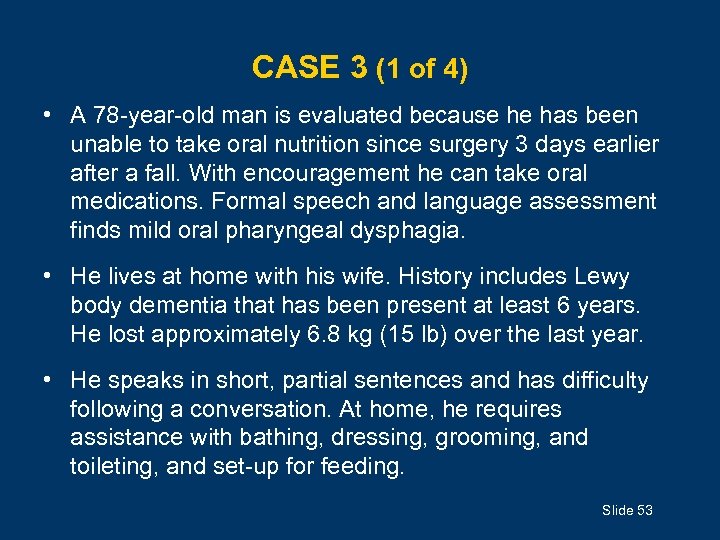
CASE 3 (1 of 4) • A 78 -year-old man is evaluated because he has been unable to take oral nutrition since surgery 3 days earlier after a fall. With encouragement he can take oral medications. Formal speech and language assessment finds mild oral pharyngeal dysphagia. • He lives at home with his wife. History includes Lewy body dementia that has been present at least 6 years. He lost approximately 6. 8 kg (15 lb) over the last year. • He speaks in short, partial sentences and has difficulty following a conversation. At home, he requires assistance with bathing, dressing, grooming, and toileting, and set-up for feeding. Slide 53
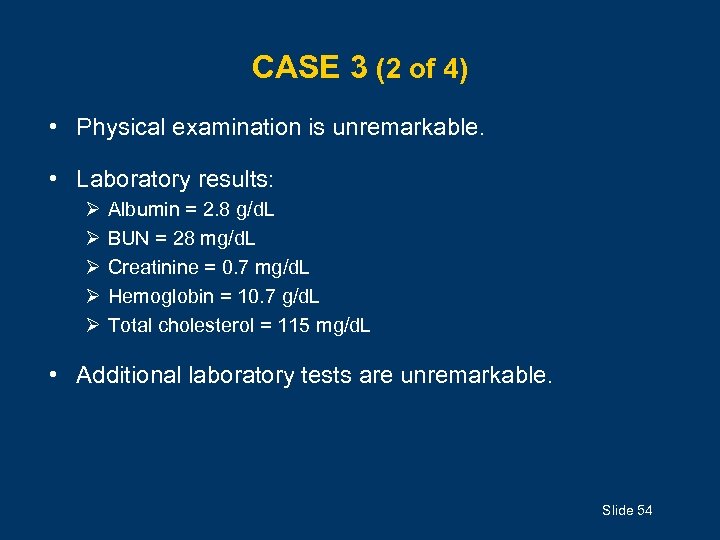
CASE 3 (2 of 4) • Physical examination is unremarkable. • Laboratory results: Ø Ø Ø Albumin = 2. 8 g/d. L BUN = 28 mg/d. L Creatinine = 0. 7 mg/d. L Hemoglobin = 10. 7 g/d. L Total cholesterol = 115 mg/d. L • Additional laboratory tests are unremarkable. Slide 54
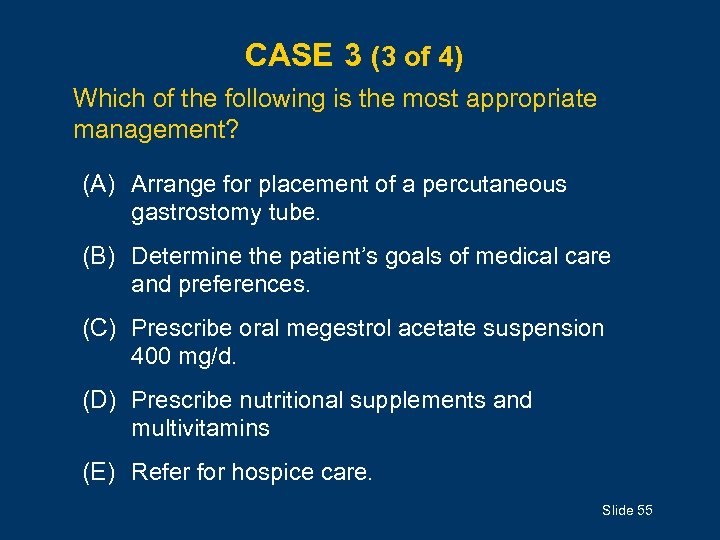
CASE 3 (3 of 4) Which of the following is the most appropriate management? (A) Arrange for placement of a percutaneous gastrostomy tube. (B) Determine the patient’s goals of medical care and preferences. (C) Prescribe oral megestrol acetate suspension 400 mg/d. (D) Prescribe nutritional supplements and multivitamins (E) Refer for hospice care. Slide 55
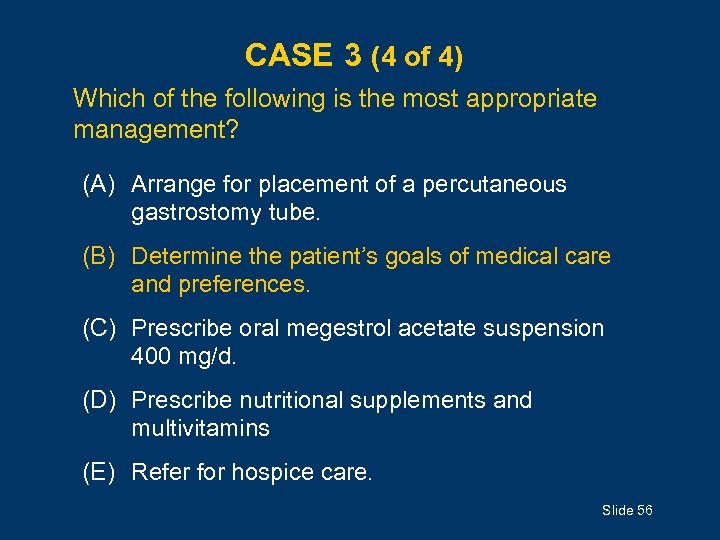
CASE 3 (4 of 4) Which of the following is the most appropriate management? (A) Arrange for placement of a percutaneous gastrostomy tube. (B) Determine the patient’s goals of medical care and preferences. (C) Prescribe oral megestrol acetate suspension 400 mg/d. (D) Prescribe nutritional supplements and multivitamins (E) Refer for hospice care. Slide 56
ACKNOWLEDGMENTS Editors: Annette Medina-Walpole, MD GRS 7 Chapter Authors: Colleen Christmas, MD Gordon L. Jensen, MD, Ph. D Paige E. Miller, MS James S. Powers, MD GRS 7 Question Writers: Daniel Mendelson, MD Dennis H. Sullivan, MD Pharmacotherapy Editor: Judith L. Beizer, Pharm. D Medical Writers: Beverly A. Caley, Faith Reidenbach Managing Editor: Andrea N. Sherman, MS Copyright © 2010 American Geriatrics Society Slide 57
55429c8ce1f1924ac1f94d78ce7efb52.ppt