caf228f2fd7b7740fec149251a2b13f6.ppt
- Количество слайдов: 53
Nutrition and Disease & Injury States Barbara Magnuson, Pharm. D BCNSP Nutrition Support Service
Disease Specific Enteral Products Patient Specific products/modifications l Renal disease l Liver disease l Malabsorption l Surgery, Trauma, Burns l Respiratory l Diabetes
Acute vs. Chronic l Acute Kidney Injury (AKI) – – l Decrease GFR over days – weeks Quick accumulation of creatinine, nitrogen waste (BUN), fluid volume, and electrolytes * * * Etiology – drugs, shock, volume Usually reversible Chronic Kidney Disease – – Structural or functional changes over > 3 months Usually does not improve
AKI Not hypermetabolic by itself l Calories: Assess patient by their primary injury or current nutritional status and needs, @ 2030 kcal/kg l CHO: l – l Often hyperglycemic with insulin resistance Fats: – Often elevated triglycerides (TGLY), monitor levels if receiving IV lipid emulsions
AKI l Protein: – – – l Hypercatabolism – usually b/c of concomitant issues Dose - specific for injury or type of dialysis used BOTH Essential and Non-essential amino acids Fluids: – – May need concentrated nutrition/fluids if low urine output and no other losses (GI) May require high volume replacement if high output, dilute urine
AKI – Electrolytes, TE, MVI Sodium: Often impaired Na elimination l Potassium, Magnesium, & Phosphorus: l – – Accumulates until dialysis Usually restricted or eliminated in TF or TPN until dialysis initiated Trace elements: No adjustments until dialysis l Vitamins: No adjustments until dialysis l
1980’s Historical Perspective HD patients had EXTREME protein restrictions to postpone HD or minimize uremia l TPN and EN provided only essential AA l – – – Lacks arginine (only conditionally essential) Thought was: the body can synthesize all the remaining non-essential amino acids Ammonia elevated & Urea still increased Resulted in protein malnutrition Poor wound healing of diabetic wounds
Nutrition with Hemo. Dialysis (HD) Hemodialysis: 2 -4 hours, 2 -4 times weekly l Calories: l – – – HD itself may slightly increase metabolism 20 -30 kcal/kg, lower end for obesity and higher end if underweight. May need up to 35 kcal/kg if severly malnourished Glucose calories absorbed from dialysate (200600 kcal)
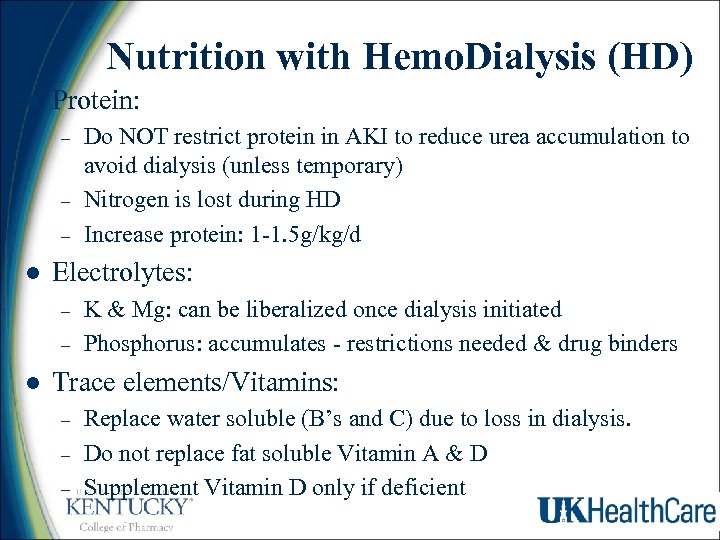
Nutrition with Hemo. Dialysis (HD) l Protein: – – – l Electrolytes: – – l Do NOT restrict protein in AKI to reduce urea accumulation to avoid dialysis (unless temporary) Nitrogen is lost during HD Increase protein: 1 -1. 5 g/kg/d K & Mg: can be liberalized once dialysis initiated Phosphorus: accumulates - restrictions needed & drug binders Trace elements/Vitamins: – – – Replace water soluble (B’s and C) due to loss in dialysis. Do not replace fat soluble Vitamin A & D Supplement Vitamin D only if deficient
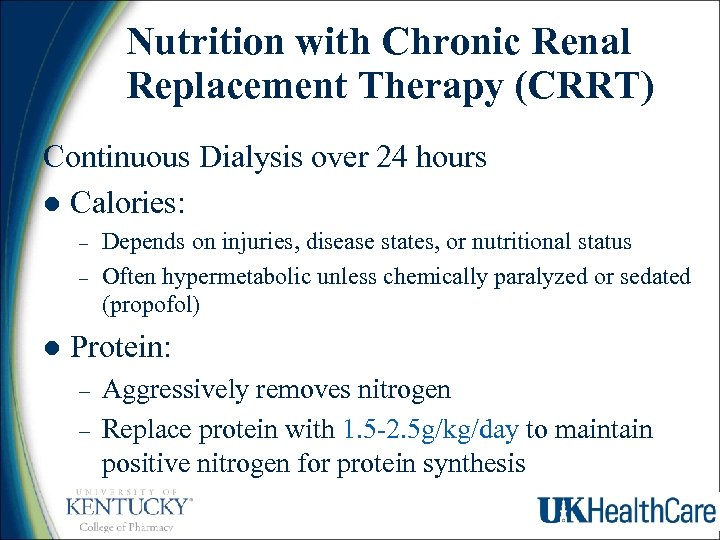
Nutrition with Chronic Renal Replacement Therapy (CRRT) Continuous Dialysis over 24 hours l Calories: – – l Depends on injuries, disease states, or nutritional status Often hypermetabolic unless chemically paralyzed or sedated (propofol) Protein: – – Aggressively removes nitrogen Replace protein with 1. 5 -2. 5 g/kg/day to maintain positive nitrogen for protein synthesis
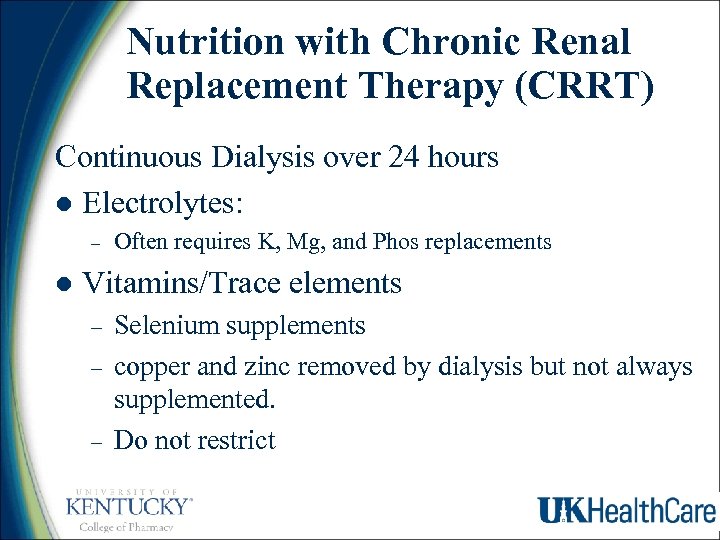
Nutrition with Chronic Renal Replacement Therapy (CRRT) Continuous Dialysis over 24 hours l Electrolytes: – l Often requires K, Mg, and Phos replacements Vitamins/Trace elements – – – Selenium supplements copper and zinc removed by dialysis but not always supplemented. Do not restrict
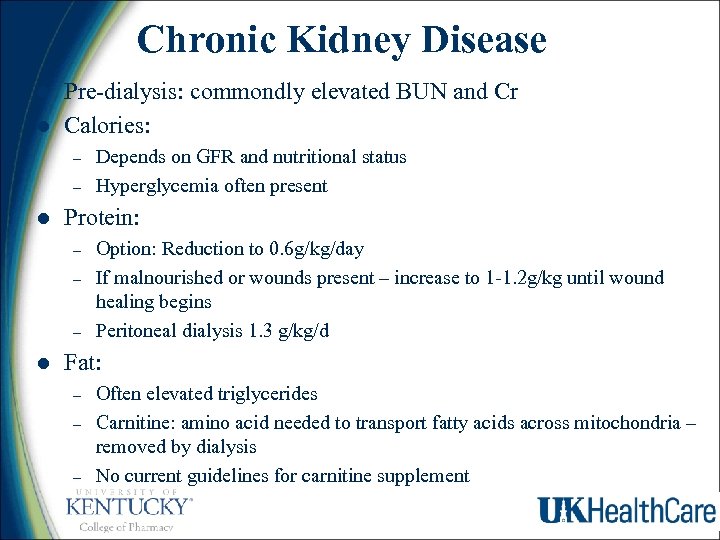
Chronic Kidney Disease l l Pre-dialysis: commondly elevated BUN and Cr Calories: – – l Protein: – – – l Depends on GFR and nutritional status Hyperglycemia often present Option: Reduction to 0. 6 g/kg/day If malnourished or wounds present – increase to 1 -1. 2 g/kg until wound healing begins Peritoneal dialysis 1. 3 g/kg/d Fat: – – – Often elevated triglycerides Carnitine: amino acid needed to transport fatty acids across mitochondria – removed by dialysis No current guidelines for carnitine supplement
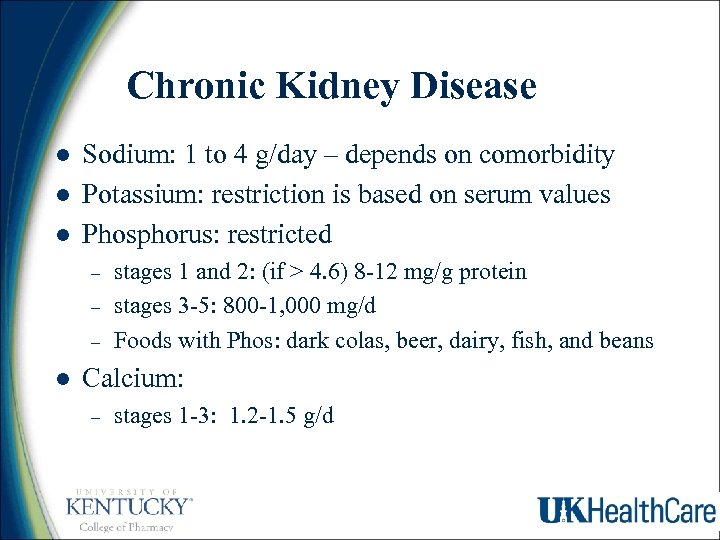
Chronic Kidney Disease l l l Sodium: 1 to 4 g/day – depends on comorbidity Potassium: restriction is based on serum values Phosphorus: restricted – – – l stages 1 and 2: (if > 4. 6) 8 -12 mg/g protein stages 3 -5: 800 -1, 000 mg/d Foods with Phos: dark colas, beer, dairy, fish, and beans Calcium: – stages 1 -3: 1. 2 -1. 5 g/d
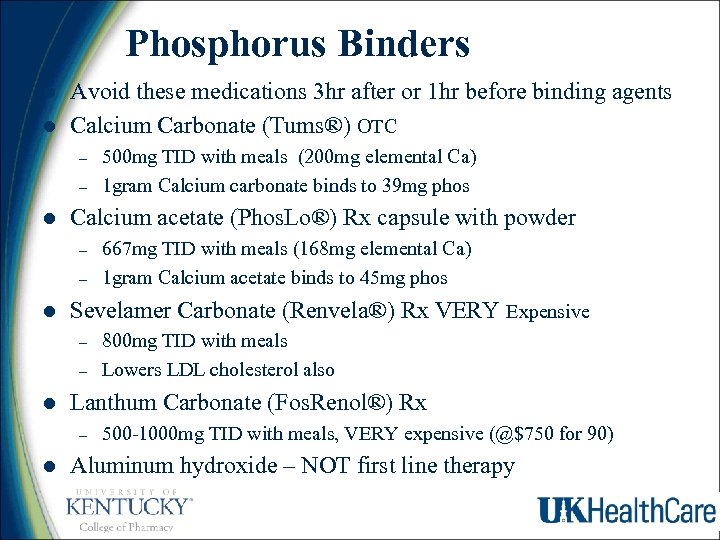
Phosphorus Binders l l Avoid these medications 3 hr after or 1 hr before binding agents Calcium Carbonate (Tums®) OTC – – l Calcium acetate (Phos. Lo®) Rx capsule with powder – – l – 800 mg TID with meals Lowers LDL cholesterol also Lanthum Carbonate (Fos. Renol®) Rx – l 667 mg TID with meals (168 mg elemental Ca) 1 gram Calcium acetate binds to 45 mg phos Sevelamer Carbonate (Renvela®) Rx VERY Expensive – l 500 mg TID with meals (200 mg elemental Ca) 1 gram Calcium carbonate binds to 39 mg phos 500 -1000 mg TID with meals, VERY expensive (@$750 for 90) Aluminum hydroxide – NOT first line therapy
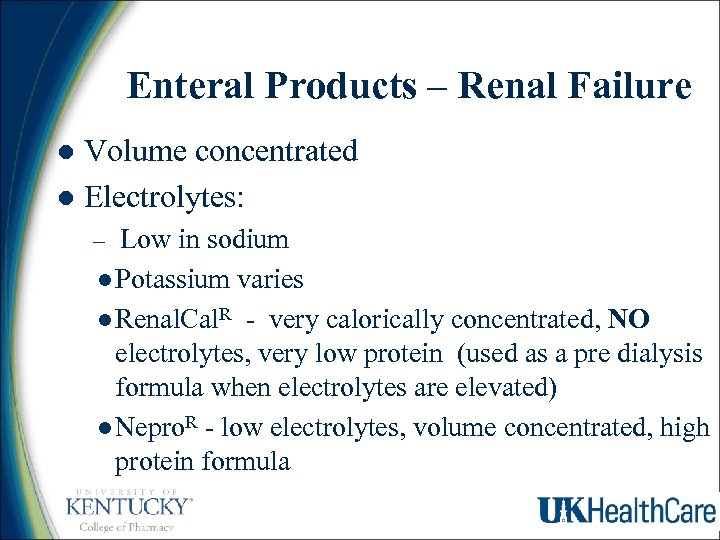
Enteral Products – Renal Failure Volume concentrated l Electrolytes: l Low in sodium l Potassium varies l Renal. Cal. R - very calorically concentrated, NO electrolytes, very low protein (used as a pre dialysis formula when electrolytes are elevated) l Nepro. R - low electrolytes, volume concentrated, high protein formula –
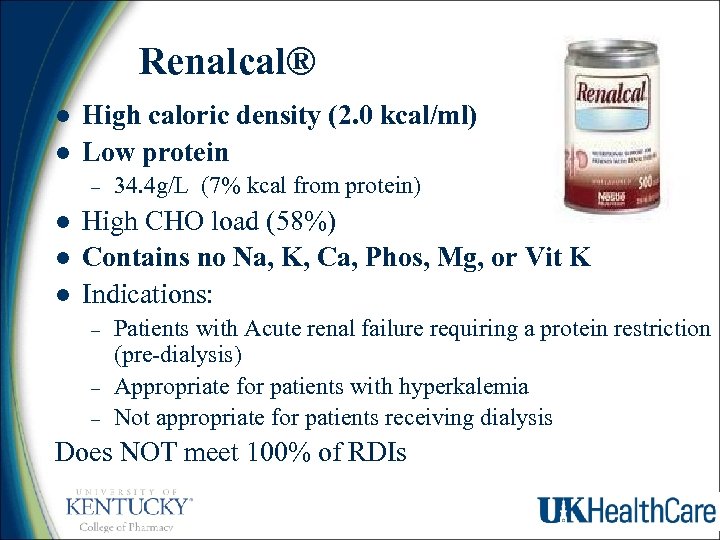
Renalcal® l l High caloric density (2. 0 kcal/ml) Low protein – l l l 34. 4 g/L (7% kcal from protein) High CHO load (58%) Contains no Na, K, Ca, Phos, Mg, or Vit K Indications: – – – Patients with Acute renal failure requiring a protein restriction (pre-dialysis) Appropriate for patients with hyperkalemia Not appropriate for patients receiving dialysis Does NOT meet 100% of RDIs
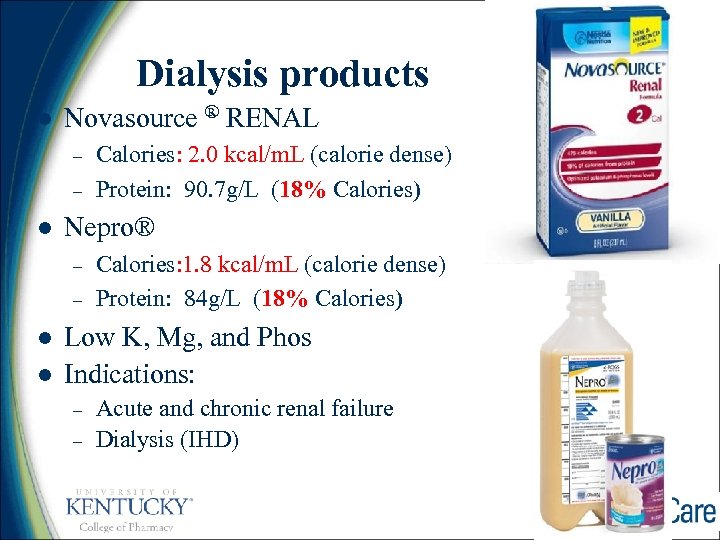
Dialysis products l Novasource ® RENAL – – l Nepro® – – l l Calories: 2. 0 kcal/m. L (calorie dense) Protein: 90. 7 g/L (18% Calories) Calories: 1. 8 kcal/m. L (calorie dense) Protein: 84 g/L (18% Calories) Low K, Mg, and Phos Indications: – – Acute and chronic renal failure Dialysis (IHD)
Nutrition in Liver Disease/Cirrhosis l End Stage Liver Disease: – Impaired detoxification of metabolites – Often malnourished pt. – especially protein and vitamins – Typically poor dietary protein intake – Serum Albumin usually low l poor protein intake l poor synthesis
Nutrition in Liver Disease/Cirrhosis l High aldosterone & ADH levels – – l Edema present – – l l Sodium and Water retained Potassium wasted low albumin alkolosis Weight – varies from underweight malnourished, obese, or edematous weight – be cautious Serum ammonia can be elevated – – Nitrogen from protein Nitrogen from endogenous amino acid breakdown
Hepatic Encephalopathy (HE)- Etiology Hepatic encephalopathy is a worsening of brain function that occurs when the liver is no longer able to remove toxic substances in the blood. l Symptoms: Confusion, Altered level of consciousness coma l Causes: Infections, Sepsis, Spontaneous bacterial peritonitis l Ammonia accumulation blood brain barrier – Ammonia glutamine astrocyte swelling HE l
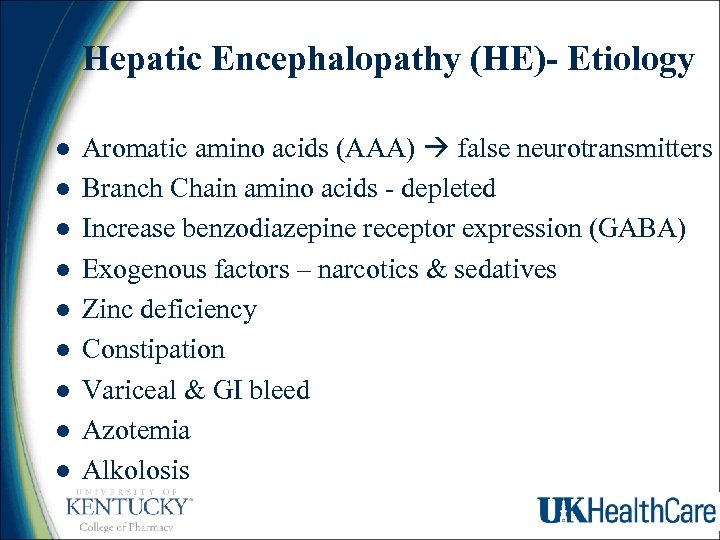
Hepatic Encephalopathy (HE)- Etiology l l l l l Aromatic amino acids (AAA) false neurotransmitters Branch Chain amino acids - depleted Increase benzodiazepine receptor expression (GABA) Exogenous factors – narcotics & sedatives Zinc deficiency Constipation Variceal & GI bleed Azotemia Alkolosis
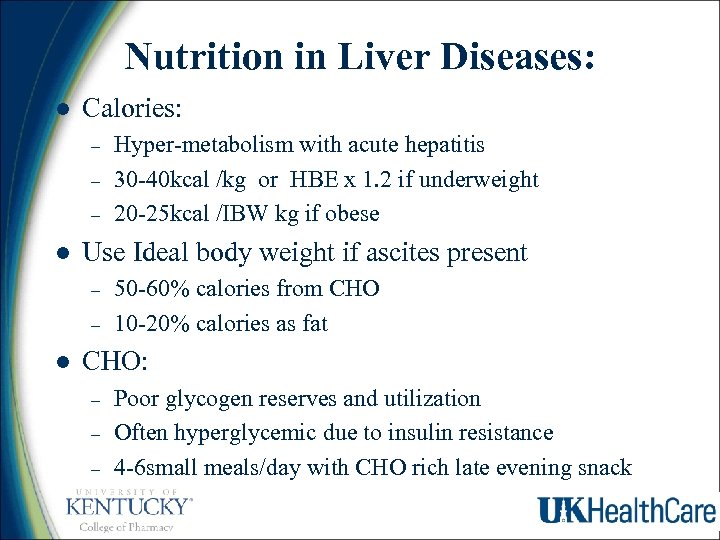
Nutrition in Liver Diseases: l Calories: – – – l Use Ideal body weight if ascites present – – l Hyper-metabolism with acute hepatitis 30 -40 kcal /kg or HBE x 1. 2 if underweight 20 -25 kcal /IBW kg if obese 50 -60% calories from CHO 10 -20% calories as fat CHO: – – – Poor glycogen reserves and utilization Often hyperglycemic due to insulin resistance 4 -6 small meals/day with CHO rich late evening snack
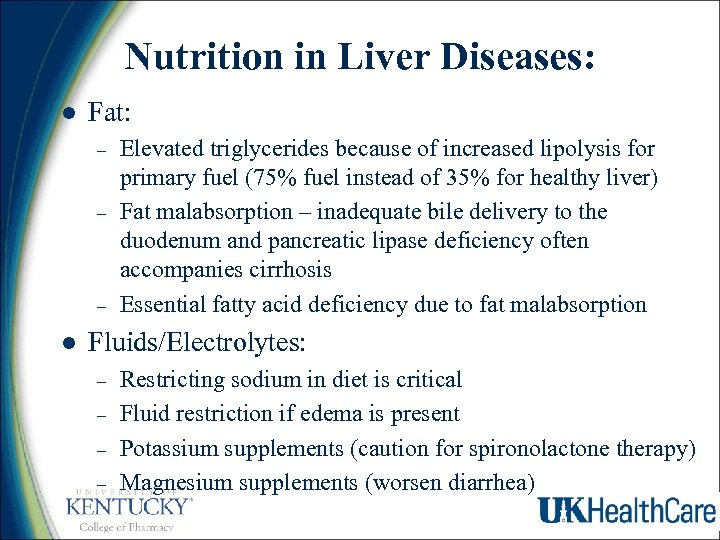
Nutrition in Liver Diseases: l Fat: – – – l Elevated triglycerides because of increased lipolysis for primary fuel (75% fuel instead of 35% for healthy liver) Fat malabsorption – inadequate bile delivery to the duodenum and pancreatic lipase deficiency often accompanies cirrhosis Essential fatty acid deficiency due to fat malabsorption Fluids/Electrolytes: – – Restricting sodium in diet is critical Fluid restriction if edema is present Potassium supplements (caution for spironolactone therapy) Magnesium supplements (worsen diarrhea)
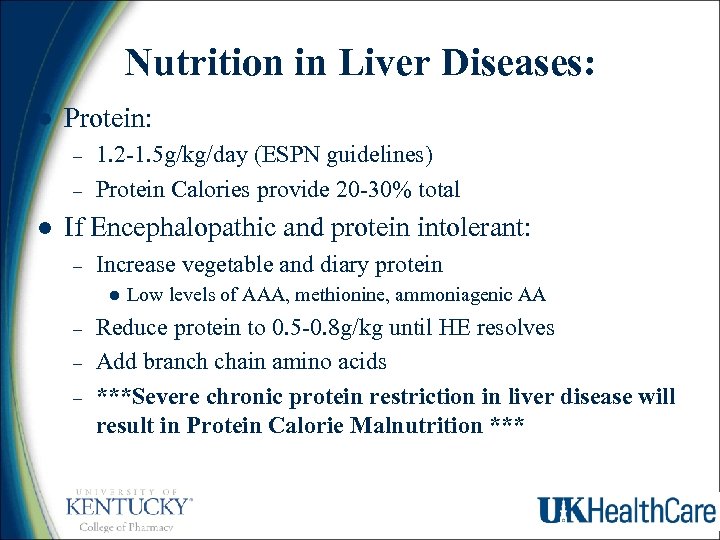
Nutrition in Liver Diseases: l Protein: – – l 1. 2 -1. 5 g/kg/day (ESPN guidelines) Protein Calories provide 20 -30% total If Encephalopathic and protein intolerant: – Increase vegetable and diary protein l – – – Low levels of AAA, methionine, ammoniagenic AA Reduce protein to 0. 5 -0. 8 g/kg until HE resolves Add branch chain amino acids ***Severe chronic protein restriction in liver disease will result in Protein Calorie Malnutrition ***
Liver Disease & Micronutrients l l l l At risk for folate and magnesium deficiency Thiamine deficiency Wernicke’s encephalopathy Vitamin A, D, & E deficiency: Fat malabsorption – due to pancreatic exocrine insufficiency & cholestasis Zinc deficiency: diuretics, protein restrictions, diarrhea Zn and Mg deficiency distorted taste sensation (dysgeusia) Zinc – supplement 600 mg/day – may improve amino acid metabolism and HE grade Selenium - Supplement 40 mcg/day Manganese & Copper o Elimination via the bile o If cholestasis present - reduce or eliminate from TPN
Branch Chain Amino Acids l Essential AA are depleted – l l l l Normalization promotes protein synthesis and reduces ammonia concentrations Aromatic Amino Acids – elevated BCAA – possibly compete with AAA to cross the BBB Leucine potent stimulator of HGF (Human Growth Factor) production & hepatic regeneration Possibly improves protein catabolism in cirrhosis ESPEN – recommends BCAA for decompensated liver cirrhosis Unpalatable & Costly Fail to consistently improve HE
Enteral Nutrition Liver Disease ? ? ? efficacy – – – – Low Sodium formulas Low protein (11% of calories) Added Branch Chain amino acids Low aromatic amino acids Low fat Medium Chain Triglycerides Ex. Hepatic. Aid IIR, Nutra. Hep. R
TPN: Liver Disease l Hepat. Amine 8% – – Mixture of essential and nonessential amino acids High concentrations of the BCAA Low concentrations of methionine and AAA The rationale for Hepat. Amine is based on observations of plasma amino acid imbalances and on theories which postulate that these abnormal patterns are causally related to the development of hepatic encephalopathy.
Special Disease States Chronic Malabsorption l Short bowel syndrome l Radiation enteritis l Enteric fistulas l Inflammatory Bowel Disease l
Short Bowel Syndrome l Short bowel syndrome – – Must have 100 cm of small bowel Must have 60 cm of small bowel & colon TPN may need to be used for weeks to months following resection of ischemic or diseased bowel l Enteral nutrition should be initiated as soon as the bowel is healthy enough to feed l
Short Bowel Syndrome l Calories: – – l 25 -30 kcal/kg (less if obese) If the bowel is diseased, it may take 50 kcal/kg ingested to absorb 50% CHO: – – AVOID Simple sugars create a high osmotic load diarrhea Fiber short chain fatty acids in the colon for energy flatulence
Short Bowel Syndrome l Fat: – – l Malabsorption due to low pancreatic enzymes and bile salt malabsorption in the ileum No dietary fat restrictions if lacking a colon and more ileum (absorption site) Fat restriction and supplemental complex CHO if colon is present Supplement Medium Chain Triglycerides Protein – – Single amino acids – saturate absorption Peptides and Standard Protein - optimal
Short Bowel Syndrome l Fluids & Electrolytes: – – – l High losses of most all electrolytes, and water (2 -4 L/day diarrhea) Supplement Na, K, & Mg (caution: supplements may exacerbate diarrhea) Unabsorbed fatty acids bind calcium in the GI Elevated oxylates absorption (because GI calcium unavialable to bind) may increase renal oxylate stones Vitamin D deficiency exacerbates calcium deficiency Vitamins & Trace elements: – – – Supplement trace elements in TPN & may need extra zinc Vitamin B 12 injections may be necessary montly Oral multivitamin with minerals is critical
Semi-elemental Formulas – – – – Simple and small carbohydrates Low residue – no fiber (some EN has fiber) Small di and tri-peptides (best absorbed) Low total fat (long chain fatty acids) Supplemented with medium chain fatty acids Preferred products for malabsorption or short bowel syndrome, radiation enteritis, or chronic diarrhea Example: Peptamen® Vital HN ®
Peptamen 1. 5 • • l 1. 5 kcal/ml 67. 6 g/L protein (18% kcal from protein) 1500 kcal meets 100% of RDIs – 77 % Free Water Contains no fiber l Semi-Elemental formula – uses: – GI impaired patients with malabsorption Chylothorax or chylo-acsitis Transitioning patients from TPN to enteral nutrition – – – l l l Peptide-based formula with whey protein MCT oil for easy absorption. May be consumed orally with flavor packets
Short Bowel Syndrome l l l Transitioning from TPN or EN Small volumes every 2 -3 hr with oral rehydration solutions No sugar sodas Sodium and potassium often necessary to add to sports drinks Medications – NO SORBITOL! – – – Loperamide and lomotil may be life-time requirements PPI or H 2 RA – reduces gastric acid hypersecretion rh. GH and glutamine – enhance bowel adaptation
Surgery, Trauma, Burns Hypermetabolic – high calories (25 -35 kcal/kg) l Hypercatabolic & wound healing: very high protein (1. 5 -2. 5 g/kg) l High potassium & phosphorus needs for burns l Supplemented: vitamin C, glutamine, arginine, selenium, branch chain amino acids l Increased zinc for wound healing l
Immunonutrition/Pharm aconutrition l Supplemented arginine: – – l Supplemented glutamine: – – l Enterocytes utilize for fuel Enhances cellular immune Supplemented Omega 3 fatty acids – l Restores T-cell function Pathway to nitric oxide low inflammatory component Improves postooerative outcomes in GI surgery – Imapact AR® - given TID preop x 5 days
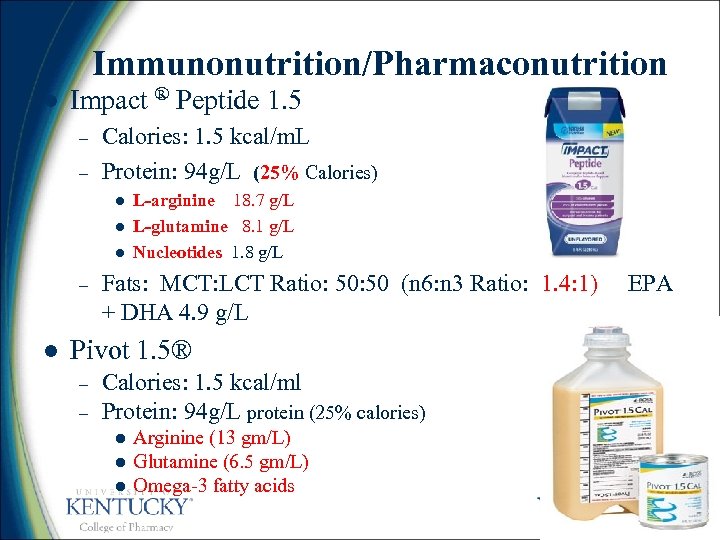
Immunonutrition/Pharmaconutrition l Impact ® Peptide 1. 5 – – Calories: 1. 5 kcal/m. L Protein: 94 g/L (25% Calories) l l l – l L-arginine 18. 7 g/L L-glutamine 8. 1 g/L Nucleotides 1. 8 g/L Fats: MCT: LCT Ratio: 50 (n 6: n 3 Ratio: 1. 4: 1) EPA + DHA 4. 9 g/L Pivot 1. 5® – – Calories: 1. 5 kcal/ml Protein: 94 g/L protein (25% calories) l l l Arginine (13 gm/L) Glutamine (6. 5 gm/L) Omega-3 fatty acids
Juven® l Supplements enteral feeds or PO diet – – l Arginine (7 gm) and Glutamine (7 gm) Orange and Fruit juice flavors Not a complete protein supplement To drink or administer via FT Used to promote wound healing. – – Appropriate for trauma, burns, and skin breakdown Helps build and maintain lean body mass
Chronic Obstructive Pulmonary Disease (COPD) l Emphysema/COPD - the walls between the air sacs are damaged and destroyed leading to fewer and larger air sacs instead of many tiny ones – Reduced gas exchange & Accumulation of CO 2 l CHO – metabolized primarily to CO 2 Low CHO diet– to decrease CO 2 accumulation l Calories – HBE x 1. 3 or 25 kcal/kg unless obese l – – Challenge to increase calories without excessive CHO Overfeeding increased CHO CO 2
Chronic Obstructive Pulmonary Disease (COPD) Fat least amount of CO 2 l Enteral products with Low CHO l – – Remaining calories - high fat Example: Pulmocare® - 55. 2% fat ? ? Efficacy, Massive diarrhea l Protein – dosed for nutritional status l Ventilator Dependant Bedridden l – Decrease calories but maintain high protein diet
Acute Respiratory Distress Syndrome l ARDS: – – – l Poor oxygenation Life threatening Severe inflammatory process Calories & Protein – – – Likely extremely hypermetabolic & hypercatabolic unless pharmacologic paralysis or sedation 25 -30 kcal/kg 1. 5 g/kg/day protein
Acute Respiratory Distress Syndrome Theory: l Decrease or eliminate pro-inflammatory precursors: ie. Omega 6 Fatty acids l Supplement Omega 3 fatty acids l Recent Study showed increase mortality with Oxepa compared to Two. Cal HN, ? ? Study design and propofol used for sedation – Example: Oxepa®

Oxepa® l l Moderate kcal (1. 5 kcal/ml) Moderate protein – l l Contains a unique fat blend of high Omega-3 fatty acids to modulate the inflammatory response. Low Omega-6 fatty acids ONLY Indication: – l 62. 7 g/L (16. 7% kcal from protein) ventilated patients with ARDS (possibly SIRS and Sepsis) 1420 kcal meets 100% of RDIs – – Contains no fiber 79% Free Water
Diabetes l Carbohydrate Consistent diets l Less total CHO and simple sugars l More complex carbohydrates & fiber l Supplement or Substitute meal? ? ? l Avoid excess calories and excess total carbohydrates for overweight patients! – Ex. Glucerna® – 22% protein (high), 45% fat, complex CHO
Glucerna 1. 5 ® Calorically dense (1. 5 Cal/m. L) l High protein 82. 5 g/L protein (22% of calories) l Prebiotics - sc. FOS® (2. 4 g/8 fl oz) l omega-3 fatty acids from canola oil (3 g of ALA per 1500 Cal), AHA recommendations l Beneficial for diabetics or hyperglycemia in ICU patients requiring high protein doses l
TPN Case TF CD is a 35 yo male, 5'10", 80 kg admitted to UKMC for severe dehydration. l CD has excessive drainage from a duodenal fistula resultant from a gun shot wound to the abdomen he received 3 months ago. l Transitioning from TPN to Enteral Nutrition l Which formula type is optimal? l What rate will meet his needs? l Needs: 2089 - 2263 Kcal/day, 112 g/d - 128 g/d l
TPN Case TF Transitioning from TPN to Enteral Nutrition l Which formula type is optimal? l A semi-elemental product is likely to be best tolerated after 3 months of bowel rest l Ex. Peptamen 1. 5 l Rate @ 60 ml/hr provides 2160 kcal & 97 g/day protein l Add 2 beneprotein daily (12 g/day & 50 kcal) l Or 2 Juven daily (28 g or glutamine & Arginine) l
Case #2 l AJ is a 20 yo, 86 kg, 75” multi-fracture trauma patient in the ICU and requires: – – 2150 -2580 kcal/d 120 -150 g/d of protein l Which of the given example enteral products and rate will best meet his needs?
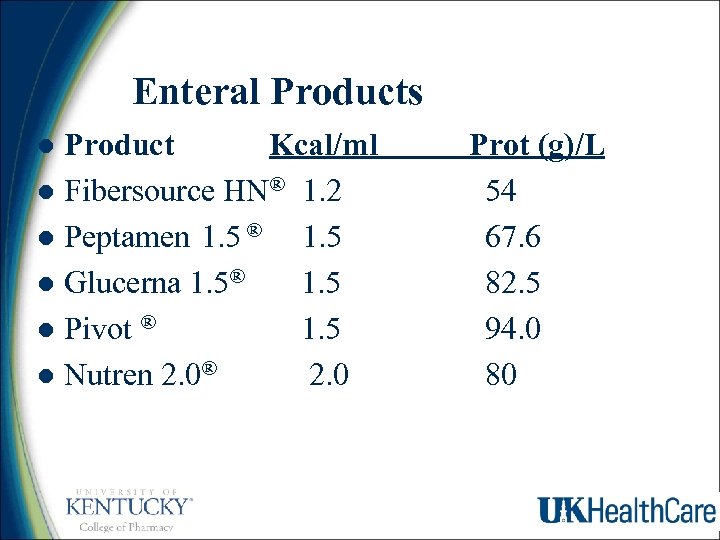
Enteral Products Product Kcal/ml l Fibersource HN® 1. 2 l Peptamen 1. 5 ® 1. 5 l Glucerna 1. 5® 1. 5 l Pivot ® 1. 5 l Nutren 2. 0® 2. 0 l Prot (g)/L 54 67. 6 82. 5 94. 0 80
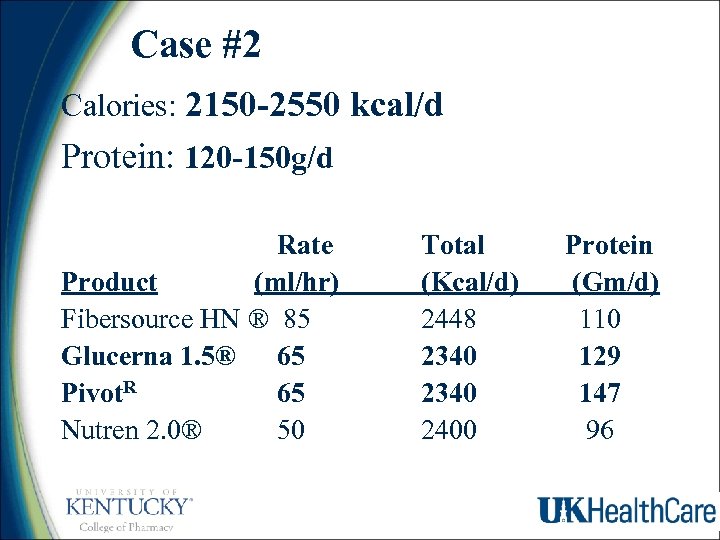
Case #2 Calories: 2150 -2550 kcal/d Protein: 120 -150 g/d Rate Product (ml/hr) Fibersource HN ® 85 Glucerna 1. 5® 65 Pivot. R 65 Nutren 2. 0® 50 Total (Kcal/d) 2448 2340 2400 Protein (Gm/d) 110 129 147 96
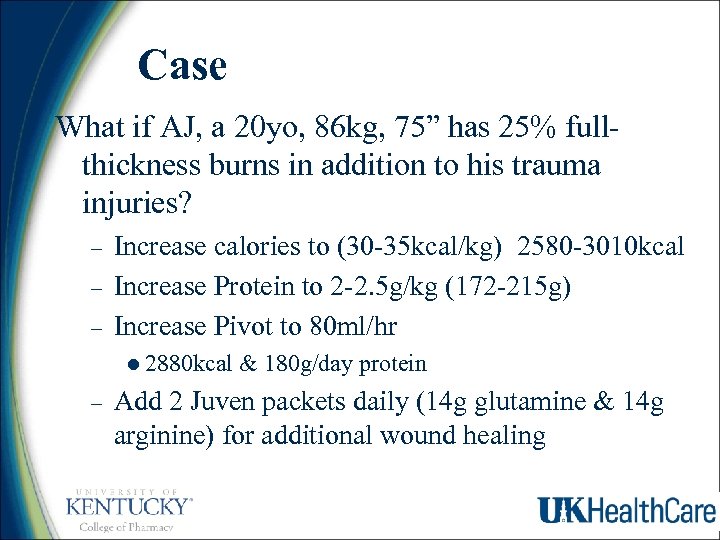
Case What if AJ, a 20 yo, 86 kg, 75” has 25% fullthickness burns in addition to his trauma injuries? – – – Increase calories to (30 -35 kcal/kg) 2580 -3010 kcal Increase Protein to 2 -2. 5 g/kg (172 -215 g) Increase Pivot to 80 ml/hr l 2880 kcal & 180 g/day protein – Add 2 Juven packets daily (14 g glutamine & 14 g arginine) for additional wound healing
caf228f2fd7b7740fec149251a2b13f6.ppt