60db55dce37f7aa319cfb1a84d0f23e1.ppt
- Количество слайдов: 29
 Normal Pressure Hydrocephalus (NPH) Date: 2005/09/27 Speaker: Int. 吳忠泰 Supervisor: V. S. 俞芹英
Normal Pressure Hydrocephalus (NPH) Date: 2005/09/27 Speaker: Int. 吳忠泰 Supervisor: V. S. 俞芹英
 Outlines Definition Epidemiology and etiology Physiology and pathophysiology Diagnosis and differential diagnosis Treatment and complication Prognosis
Outlines Definition Epidemiology and etiology Physiology and pathophysiology Diagnosis and differential diagnosis Treatment and complication Prognosis
 Definition First described in 1965 by Hakim and Adams Normal CSF pressure Ventriculomegaly Clinical triad: Slowly progressive gait disorder Impairment of mental function Sphincteric incontinence
Definition First described in 1965 by Hakim and Adams Normal CSF pressure Ventriculomegaly Clinical triad: Slowly progressive gait disorder Impairment of mental function Sphincteric incontinence
 Epidemiology 1 per 25’ 000 Accounts for approximately 0. 5 -5% (up to 6%) of dementias One of the few treatable causes of dementia Most common in patient > 60 y/o M>F
Epidemiology 1 per 25’ 000 Accounts for approximately 0. 5 -5% (up to 6%) of dementias One of the few treatable causes of dementia Most common in patient > 60 y/o M>F
 Etiology Idiopathic: Elderly, unknown cause, 50% of NPH With a preceding cause: Young Subarachnoid hemorrhage (SAH) Trauma Meningitis (TB, syphilitic, etc. ) Surgery, irradiation Storage disease (mucopolysaccharidosis)
Etiology Idiopathic: Elderly, unknown cause, 50% of NPH With a preceding cause: Young Subarachnoid hemorrhage (SAH) Trauma Meningitis (TB, syphilitic, etc. ) Surgery, irradiation Storage disease (mucopolysaccharidosis)
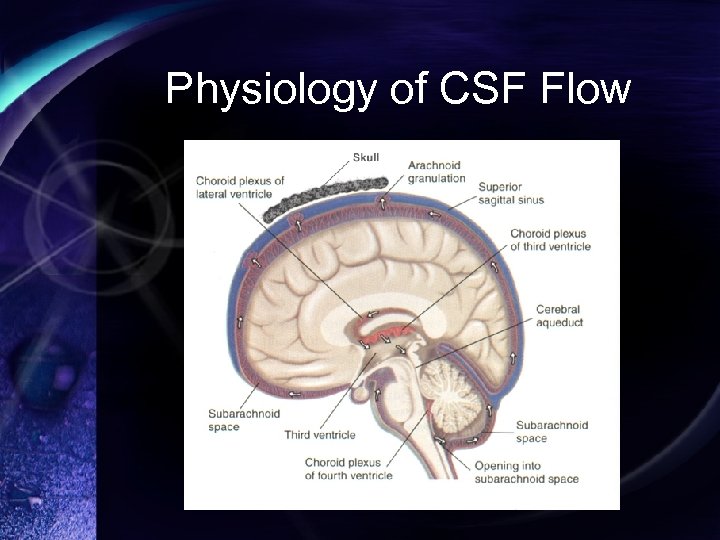 Physiology of CSF Flow
Physiology of CSF Flow
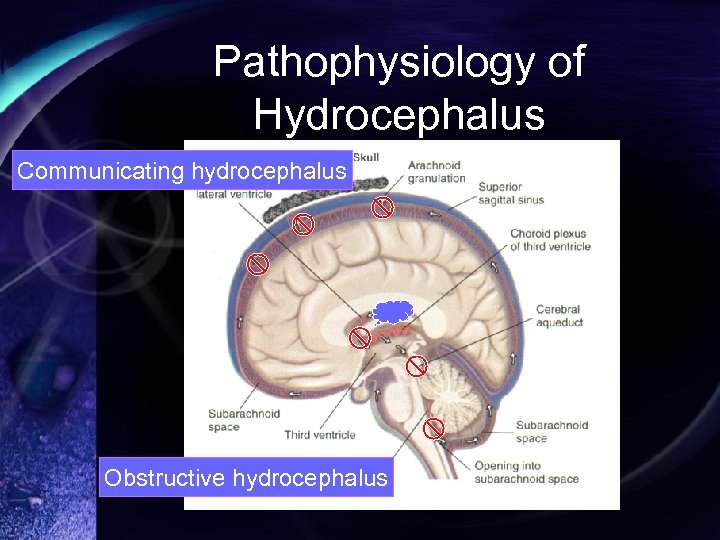 Pathophysiology of Hydrocephalus Communicating hydrocephalus Obstructive hydrocephalus
Pathophysiology of Hydrocephalus Communicating hydrocephalus Obstructive hydrocephalus
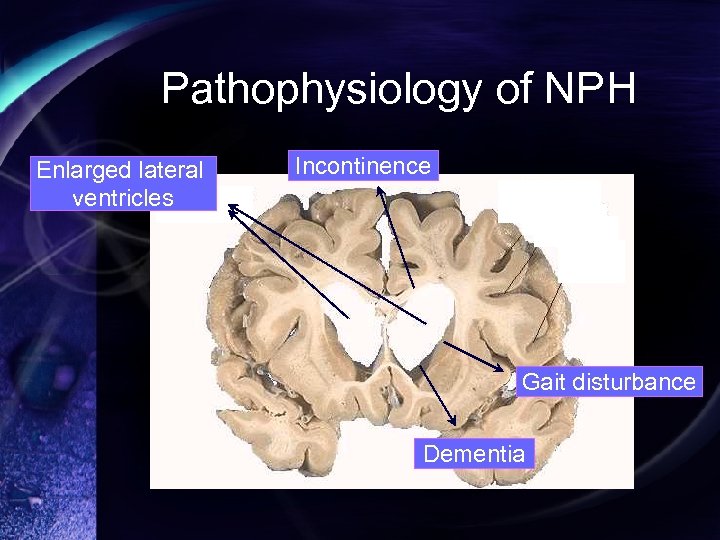 Pathophysiology of NPH Enlarged lateral ventricles Incontinence Gait disturbance Dementia
Pathophysiology of NPH Enlarged lateral ventricles Incontinence Gait disturbance Dementia
 Pathophysiology of NPH On the basis of both dynamic and ischemic factors Ventricular enlargement Vascular stretching → Ischemia Decreased compliance of ventricular wall High pulse pressure Barotrauma or shearing stress
Pathophysiology of NPH On the basis of both dynamic and ischemic factors Ventricular enlargement Vascular stretching → Ischemia Decreased compliance of ventricular wall High pulse pressure Barotrauma or shearing stress
 Dynamics of NPH Transmantle pressure gradient Difference in pressure between ventricle and subarachnoid space Gradient ↑ temporarily → Ventricle↑ B wave (plateau) Transient elevations of mean and pulse pressure Water-hammer effect → Ventricle↑ More than 50% of time
Dynamics of NPH Transmantle pressure gradient Difference in pressure between ventricle and subarachnoid space Gradient ↑ temporarily → Ventricle↑ B wave (plateau) Transient elevations of mean and pulse pressure Water-hammer effect → Ventricle↑ More than 50% of time
 Dynamics of NPH Aqueductal CSF flow void Increased CSF flow velocity Favorable response to CSF diversion Aqueductal CSF stroke volume CSF pulsating back and forth through the aqueduct during systole and diastole Favorable response to shunting Hyperdynamic CSF flow
Dynamics of NPH Aqueductal CSF flow void Increased CSF flow velocity Favorable response to CSF diversion Aqueductal CSF stroke volume CSF pulsating back and forth through the aqueduct during systole and diastole Favorable response to shunting Hyperdynamic CSF flow
 Dynamics of NPH Saline infusion test CSF resorption in NPH is abnormal Arachnoid granulation? Arachnoidal villi? Venous compromise Increased transvenular resistance in superior saggital sinus cause NPH What cause venous compromise? Microangiopathy? Deep white matter ischemia?
Dynamics of NPH Saline infusion test CSF resorption in NPH is abnormal Arachnoid granulation? Arachnoidal villi? Venous compromise Increased transvenular resistance in superior saggital sinus cause NPH What cause venous compromise? Microangiopathy? Deep white matter ischemia?
 Ischemia of NPH Acetazolamide challenge test Cerebral blood flow (CBF)↑ in normal person Failed to cause CBF↑ in NPH p’t Indicate the arterioles are already maximally dilated because of ischemia CSF diversion → CBF improve and response to acetazolamide
Ischemia of NPH Acetazolamide challenge test Cerebral blood flow (CBF)↑ in normal person Failed to cause CBF↑ in NPH p’t Indicate the arterioles are already maximally dilated because of ischemia CSF diversion → CBF improve and response to acetazolamide
 Ischemia of NPH Compensatory CSF flow Periventricular white matter Increased interstitial fluid Loss of parenchymal compliance
Ischemia of NPH Compensatory CSF flow Periventricular white matter Increased interstitial fluid Loss of parenchymal compliance
 Pathophysiology of NPH Dynamic Hyperdynamic CSF flow Impaired CSF resorption Ischemic Reduced CBF Periventricular white matter lesion
Pathophysiology of NPH Dynamic Hyperdynamic CSF flow Impaired CSF resorption Ischemic Reduced CBF Periventricular white matter lesion
 Diagnosis Clinical symptoms and signs Gait disturbance Dementia Urinary incontinence The moment when highly suspect NPH !! Image MRI (T 2 WI) with CSF flow study CT with lumbar puncture
Diagnosis Clinical symptoms and signs Gait disturbance Dementia Urinary incontinence The moment when highly suspect NPH !! Image MRI (T 2 WI) with CSF flow study CT with lumbar puncture
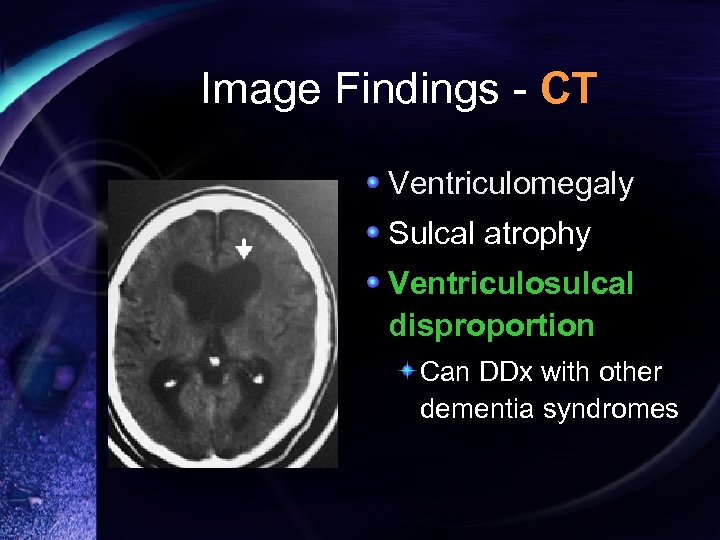 Image Findings - CT Ventriculomegaly Sulcal atrophy Ventriculosulcal disproportion Can DDx with other dementia syndromes
Image Findings - CT Ventriculomegaly Sulcal atrophy Ventriculosulcal disproportion Can DDx with other dementia syndromes
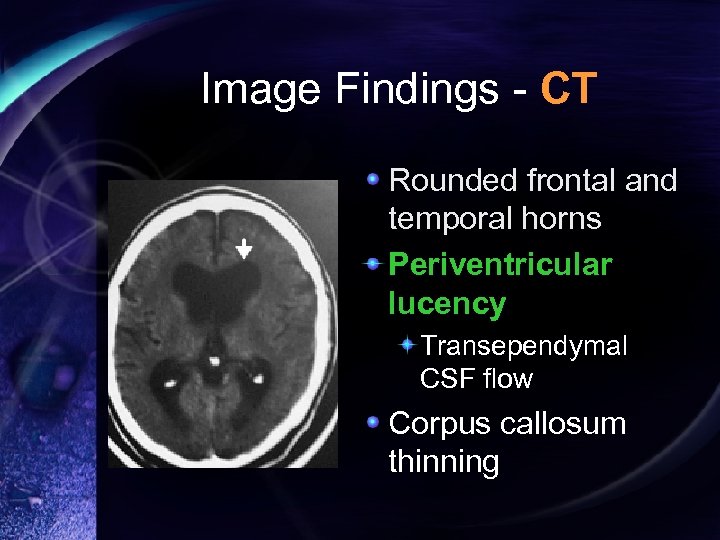 Image Findings - CT Rounded frontal and temporal horns Periventricular lucency Transependymal CSF flow Corpus callosum thinning
Image Findings - CT Rounded frontal and temporal horns Periventricular lucency Transependymal CSF flow Corpus callosum thinning
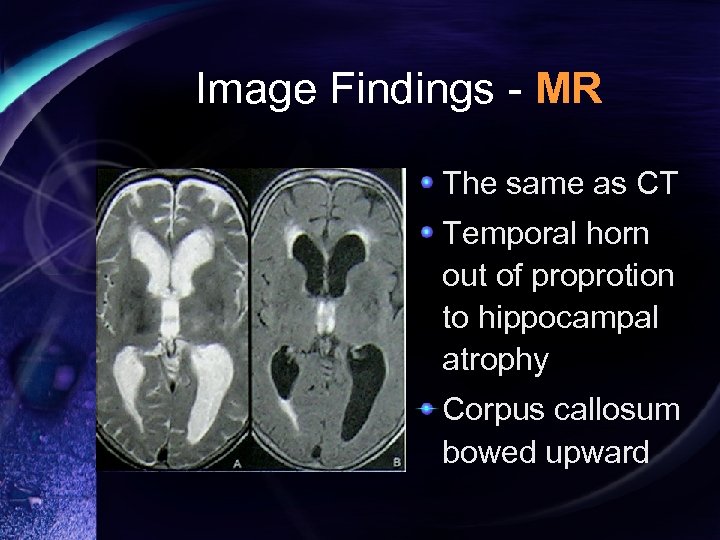 Image Findings - MR The same as CT Temporal horn out of proprotion to hippocampal atrophy Corpus callosum bowed upward
Image Findings - MR The same as CT Temporal horn out of proprotion to hippocampal atrophy Corpus callosum bowed upward
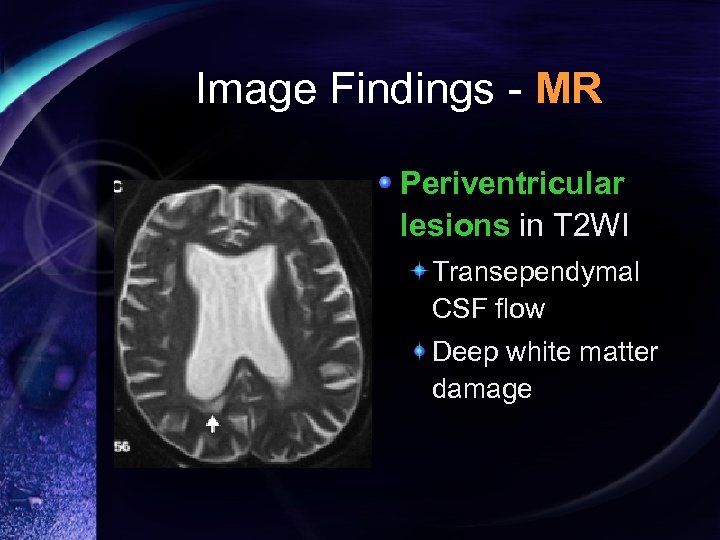 Image Findings - MR Periventricular lesions in T 2 WI Transependymal CSF flow Deep white matter damage
Image Findings - MR Periventricular lesions in T 2 WI Transependymal CSF flow Deep white matter damage
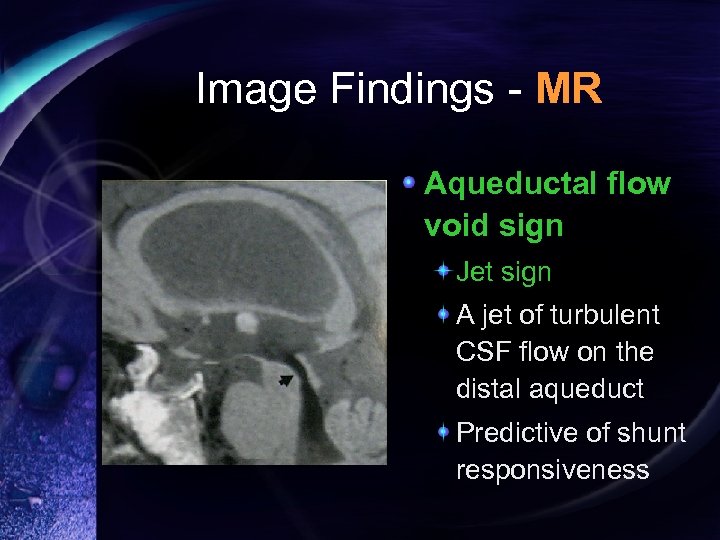 Image Findings - MR Aqueductal flow void sign Jet sign A jet of turbulent CSF flow on the distal aqueduct Predictive of shunt responsiveness
Image Findings - MR Aqueductal flow void sign Jet sign A jet of turbulent CSF flow on the distal aqueduct Predictive of shunt responsiveness
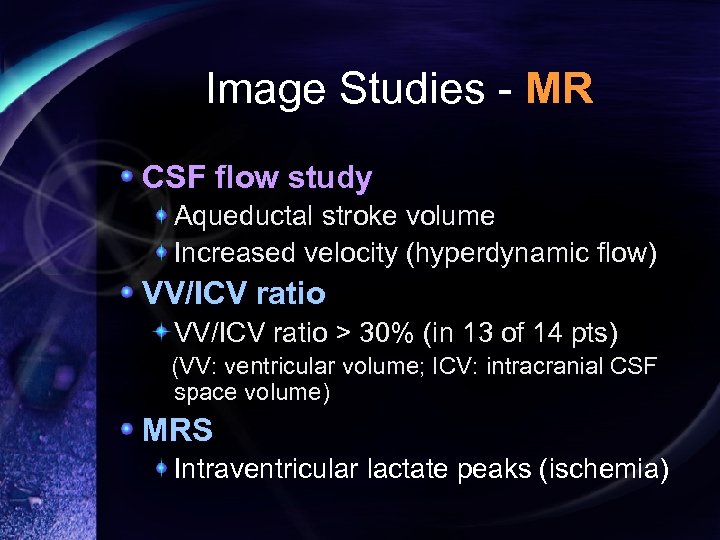 Image Studies - MR CSF flow study Aqueductal stroke volume Increased velocity (hyperdynamic flow) VV/ICV ratio > 30% (in 13 of 14 pts) (VV: ventricular volume; ICV: intracranial CSF space volume) MRS Intraventricular lactate peaks (ischemia)
Image Studies - MR CSF flow study Aqueductal stroke volume Increased velocity (hyperdynamic flow) VV/ICV ratio > 30% (in 13 of 14 pts) (VV: ventricular volume; ICV: intracranial CSF space volume) MRS Intraventricular lactate peaks (ischemia)
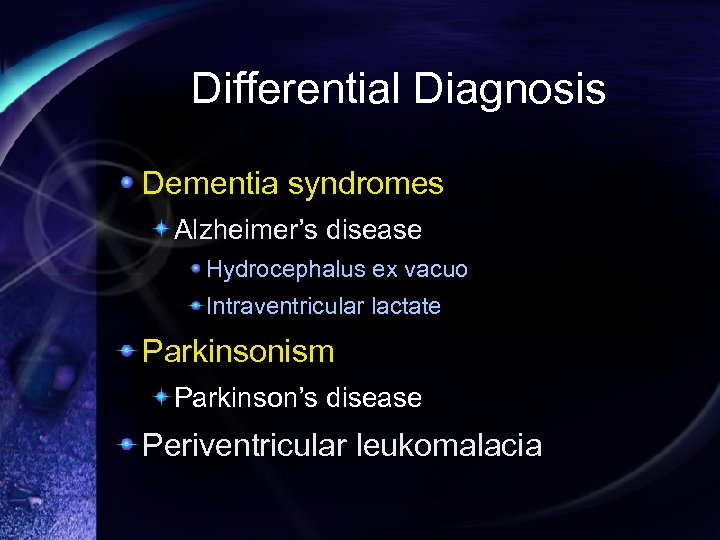 Differential Diagnosis Dementia syndromes Alzheimer’s disease Hydrocephalus ex vacuo Intraventricular lactate Parkinsonism Parkinson’s disease Periventricular leukomalacia
Differential Diagnosis Dementia syndromes Alzheimer’s disease Hydrocephalus ex vacuo Intraventricular lactate Parkinsonism Parkinson’s disease Periventricular leukomalacia
 Treatment Surgical shunting VP shunt Lumbar puncture Miller Fisher test: Gait assessment before and after 30 m. L CSF drainage (high rate of false negative) Continuous CSF drainage of 200 m. L per day for 3 -5 days
Treatment Surgical shunting VP shunt Lumbar puncture Miller Fisher test: Gait assessment before and after 30 m. L CSF drainage (high rate of false negative) Continuous CSF drainage of 200 m. L per day for 3 -5 days
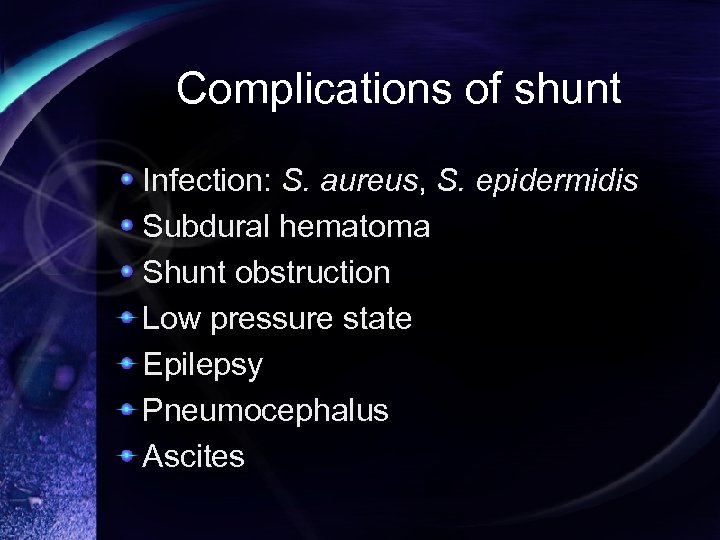 Complications of shunt Infection: S. aureus, S. epidermidis Subdural hematoma Shunt obstruction Low pressure state Epilepsy Pneumocephalus Ascites
Complications of shunt Infection: S. aureus, S. epidermidis Subdural hematoma Shunt obstruction Low pressure state Epilepsy Pneumocephalus Ascites
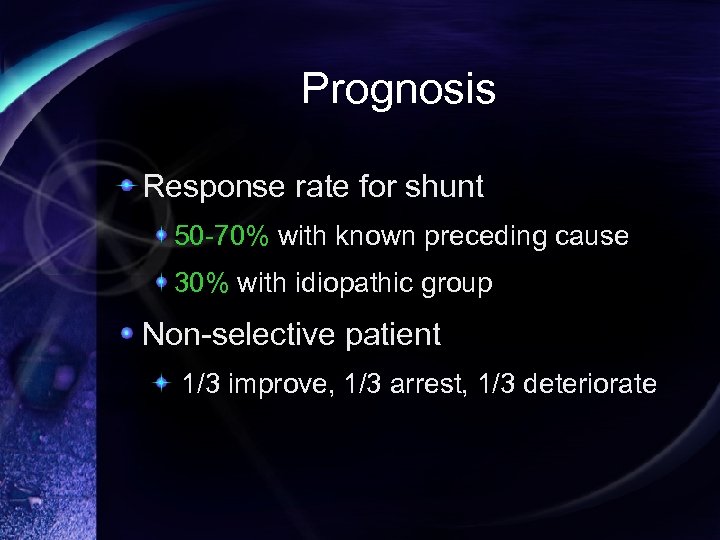 Prognosis Response rate for shunt 50 -70% with known preceding cause 30% with idiopathic group Non-selective patient 1/3 improve, 1/3 arrest, 1/3 deteriorate
Prognosis Response rate for shunt 50 -70% with known preceding cause 30% with idiopathic group Non-selective patient 1/3 improve, 1/3 arrest, 1/3 deteriorate
 Prognosis Positive response to shunting: Absence of central atrophy or ischemia Gait apraxia as dominant symptoms Prominent CSF flow void (stroke volume > 42 m. L) Known history of cause (nonidiopathic type)
Prognosis Positive response to shunting: Absence of central atrophy or ischemia Gait apraxia as dominant symptoms Prominent CSF flow void (stroke volume > 42 m. L) Known history of cause (nonidiopathic type)
 References Raymond D. Adams, Maurice Victor. Principles of Neurology, 5 th edition: 545 -6 Roger N. Rosenberg et al. The Clinical Neuroscience – Neurology/ Neurosurgery: 1205 -19 Kenneth W. Lindsay, Ian Bone. Neurology and Neurosurgery Illustrated, 4 th edition: 128 -9, 370 -3 Anne G. Osborn et al. Pocket Radiologist – Brain Top 100 Diagnosis: 228 -30 William G. Bradley. Normal Pressure Hydrocephalus: New Concepts on Etiology and Diagnosis. AJNR 2000; 21: 158690 e. Medicine: http: //www. emedicine. com/neuro/topic 277. htm http: //www. emedicine. com/radio/topic 479. htm
References Raymond D. Adams, Maurice Victor. Principles of Neurology, 5 th edition: 545 -6 Roger N. Rosenberg et al. The Clinical Neuroscience – Neurology/ Neurosurgery: 1205 -19 Kenneth W. Lindsay, Ian Bone. Neurology and Neurosurgery Illustrated, 4 th edition: 128 -9, 370 -3 Anne G. Osborn et al. Pocket Radiologist – Brain Top 100 Diagnosis: 228 -30 William G. Bradley. Normal Pressure Hydrocephalus: New Concepts on Etiology and Diagnosis. AJNR 2000; 21: 158690 e. Medicine: http: //www. emedicine. com/neuro/topic 277. htm http: //www. emedicine. com/radio/topic 479. htm
 Thanks for Your Attendance…
Thanks for Your Attendance…


