200f12313127c31bbded88155664eca4.ppt
- Количество слайдов: 36
Non-pharmacological interventions in traumatic brain injury: an update Dr Matt Wiles Department of Neuroanaesthesia & Neurocritical Care Sheffield Teaching Hospitals NHS Foundation Trust, UK @STHJournal. Club sthjournalclub. wordpress. com www. researcherid. com/rid/F-5612 -2015

“…. there are knowns; there are things we know. We also know there are known unknowns; that is to say we know there are some things we do not know. But there also unknowns – the ones we don't know. ” www. esahq. org
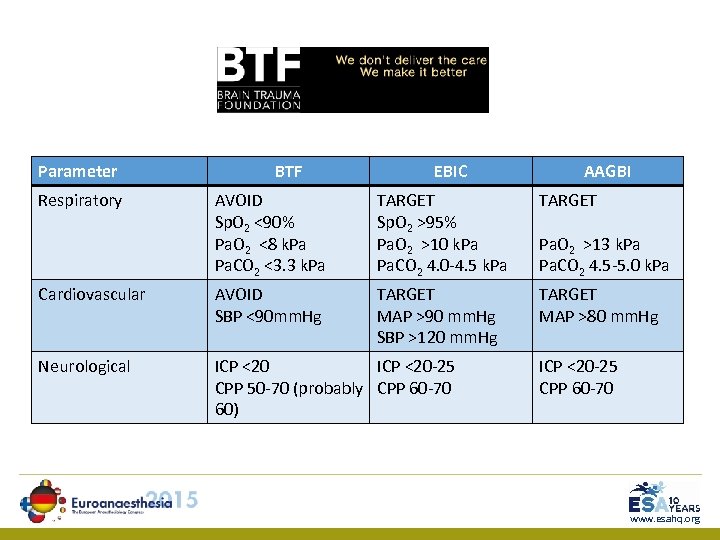
Parameter Respiratory BTF EBIC AAGBI AVOID Sp. O 2 <90% Pa. O 2 <8 k. Pa Pa. CO 2 <3. 3 k. Pa TARGET Sp. O 2 >95% Pa. O 2 >10 k. Pa Pa. CO 2 4. 0 -4. 5 k. Pa TARGET Cardiovascular AVOID SBP <90 mm. Hg TARGET MAP >90 mm. Hg SBP >120 mm. Hg TARGET MAP >80 mm. Hg Neurological ICP <20 -25 CPP 50 -70 (probably CPP 60 -70 60) Pa. O 2 >13 k. Pa Pa. CO 2 4. 5 -5. 0 k. Pa ICP <20 -25 CPP 60 -70 www. esahq. org
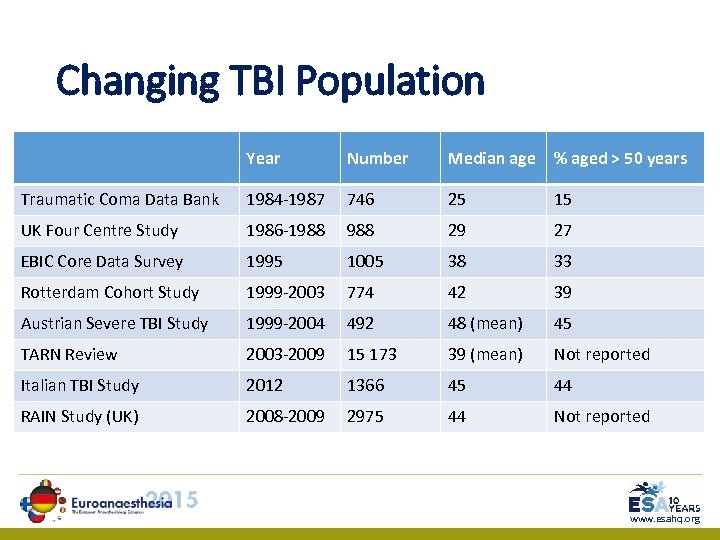
Changing TBI Population Year Number Median age % aged > 50 years Traumatic Coma Data Bank 1984 -1987 746 25 15 UK Four Centre Study 1986 -1988 29 27 EBIC Core Data Survey 1995 1005 38 33 Rotterdam Cohort Study 1999 -2003 774 42 39 Austrian Severe TBI Study 1999 -2004 492 48 (mean) 45 TARN Review 2003 -2009 15 173 39 (mean) Not reported Italian TBI Study 2012 1366 45 44 RAIN Study (UK) 2008 -2009 2975 44 Not reported www. esahq. org
www. esahq. org
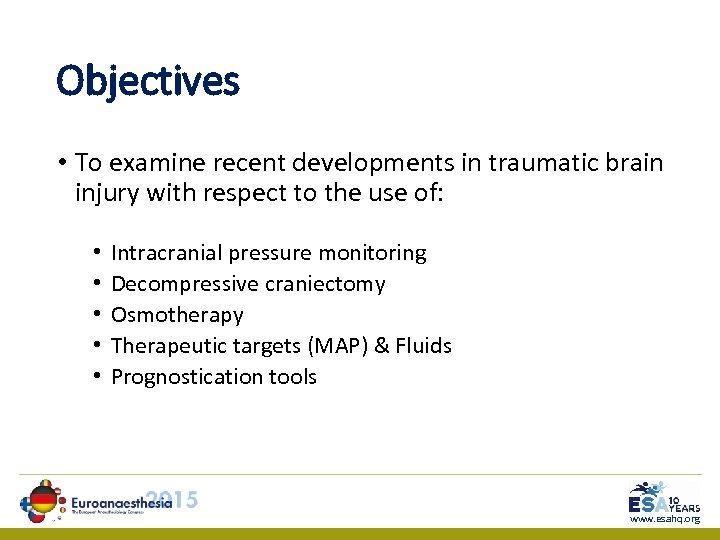
Objectives • To examine recent developments in traumatic brain injury with respect to the use of: • • • Intracranial pressure monitoring Decompressive craniectomy Osmotherapy Therapeutic targets (MAP) & Fluids Prognostication tools www. esahq. org
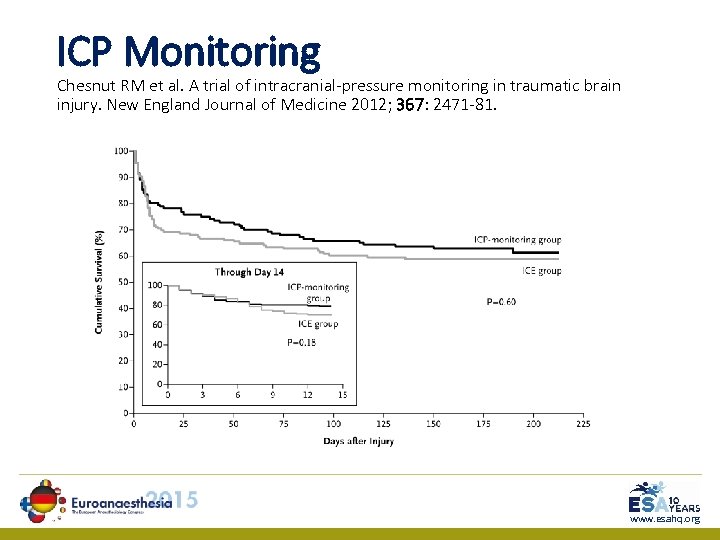
ICP Monitoring Chesnut RM et al. A trial of intracranial-pressure monitoring in traumatic brain injury. New England Journal of Medicine 2012; 367: 2471 -81. www. esahq. org
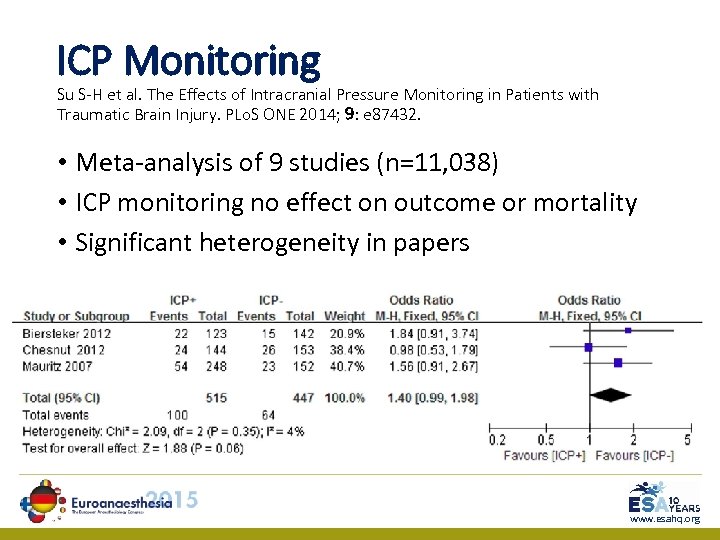
ICP Monitoring Su S-H et al. The Effects of Intracranial Pressure Monitoring in Patients with Traumatic Brain Injury. PLo. S ONE 2014; 9: e 87432. • Meta-analysis of 9 studies (n=11, 038) • ICP monitoring no effect on outcome or mortality • Significant heterogeneity in papers www. esahq. org
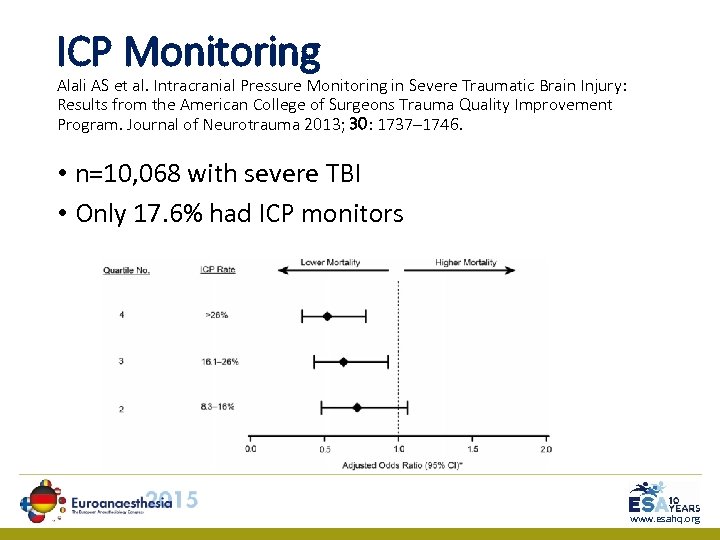
ICP Monitoring Alali AS et al. Intracranial Pressure Monitoring in Severe Traumatic Brain Injury: Results from the American College of Surgeons Trauma Quality Improvement Program. Journal of Neurotrauma 2013; 30: 1737– 1746. • n=10, 068 with severe TBI • Only 17. 6% had ICP monitors www. esahq. org
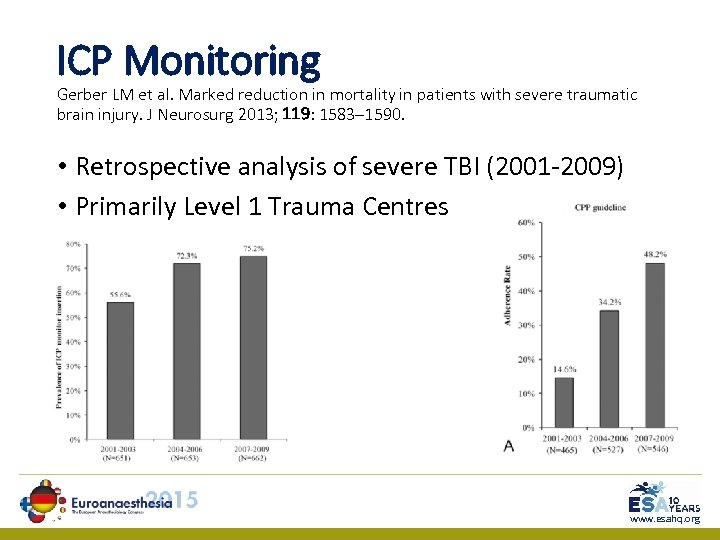
ICP Monitoring Gerber LM et al. Marked reduction in mortality in patients with severe traumatic brain injury. J Neurosurg 2013; 119: 1583– 1590. • Retrospective analysis of severe TBI (2001 -2009) • Primarily Level 1 Trauma Centres www. esahq. org
ICP Monitoring Kosty JA et al. Brief report: a comparison of clinical and research practices in measuring cerebral perfusion pressure: a literature review and practitioner survey. Anesth Analg 2013; 117: 694 -8 • Survey of Neurocritical Care Society • Atrium (74%) • Tragus (16%) • Conflicted (10%) www. esahq. org
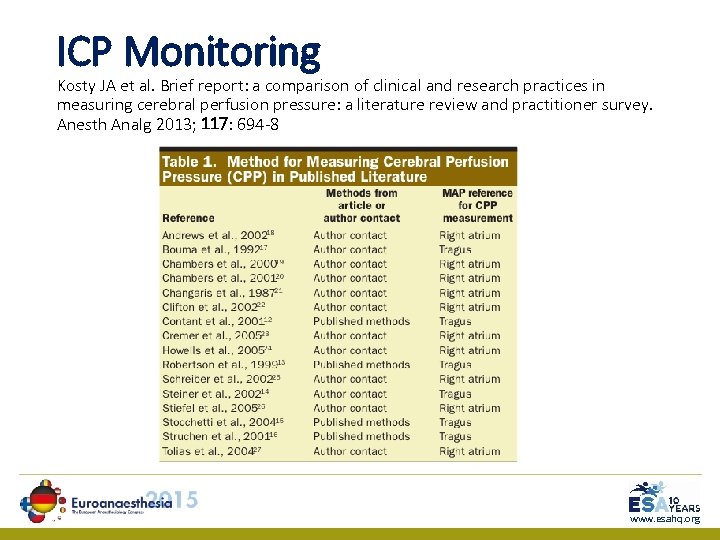
ICP Monitoring Kosty JA et al. Brief report: a comparison of clinical and research practices in measuring cerebral perfusion pressure: a literature review and practitioner survey. Anesth Analg 2013; 117: 694 -8 www. esahq. org
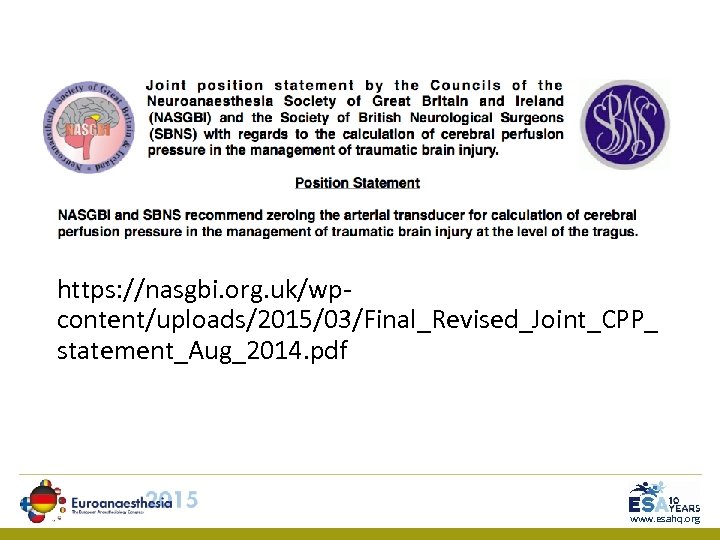
https: //nasgbi. org. uk/wpcontent/uploads/2015/03/Final_Revised_Joint_CPP_ statement_Aug_2014. pdf www. esahq. org
ICP Monitoring Stocchetti N et al. Clinical applications of intracranial pressure monitoring in traumatic brain injury. Acta Neurochir 2014; 156: 1615– 1622 • No ICP bolt: • Normal CT brain • ICP bolt: • Cerebral contusions and remained sedated • After decompressive craniectomy • After evacuation of supratentorial haematoma and at risk of raised ICP • GCS ≤ 5, midline shift > 5 mm, abnormal pupils etc. . www. esahq. org
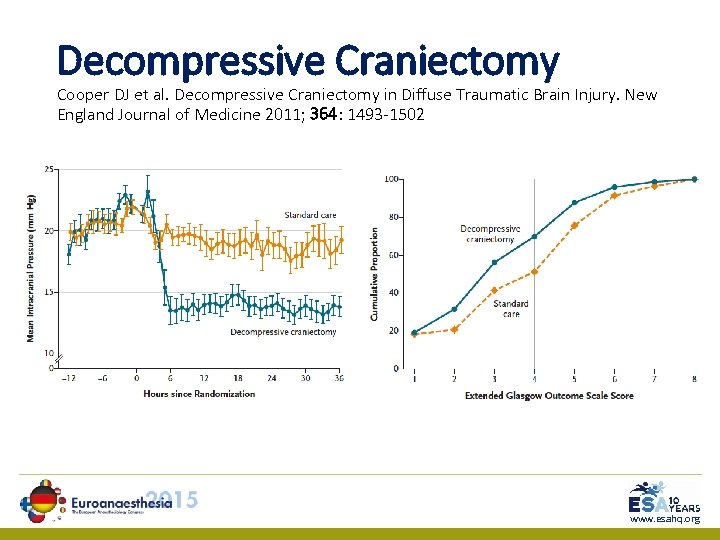
Decompressive Craniectomy Cooper DJ et al. Decompressive Craniectomy in Diffuse Traumatic Brain Injury. New England Journal of Medicine 2011; 364: 1493 -1502 www. esahq. org
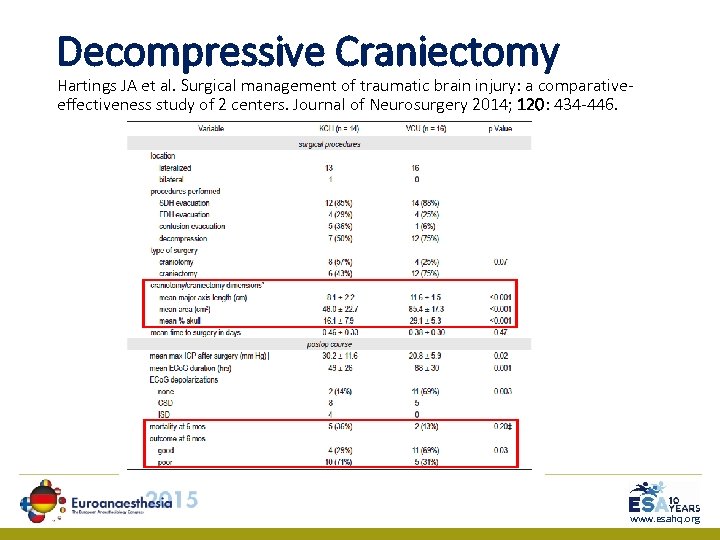
Decompressive Craniectomy Hartings JA et al. Surgical management of traumatic brain injury: a comparativeeffectiveness study of 2 centers. Journal of Neurosurgery 2014; 120: 434 -446. www. esahq. org
www. esahq. org
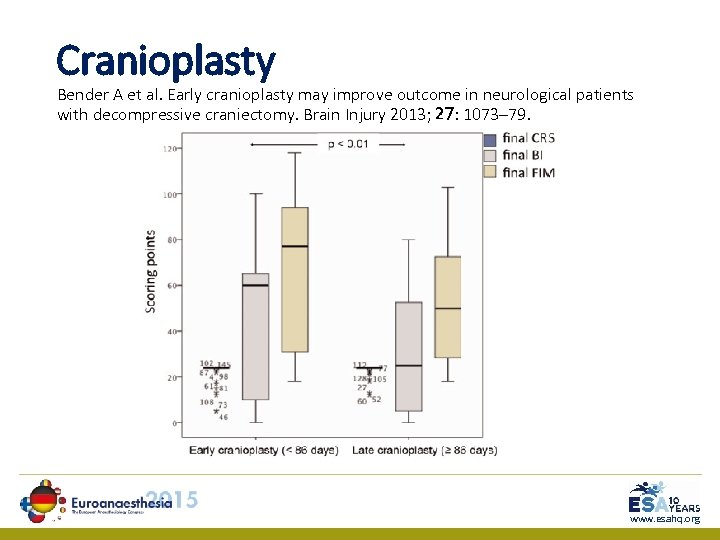
Cranioplasty Bender A et al. Early cranioplasty may improve outcome in neurological patients with decompressive craniectomy. Brain Injury 2013; 27: 1073– 79. www. esahq. org
Osmotherapy: Mannitol Wakai A et al. Mannitol for acute traumatic brain injury. Cochrane Database Syst Rev. 2013; 8: CD 001049. • Only able to identify 4 trials (n=197) • Insufficient reliable evidence to make recommendations for its use in TBI • Further high-quality RCTs needed despite the widespread use of mannitol www. esahq. org
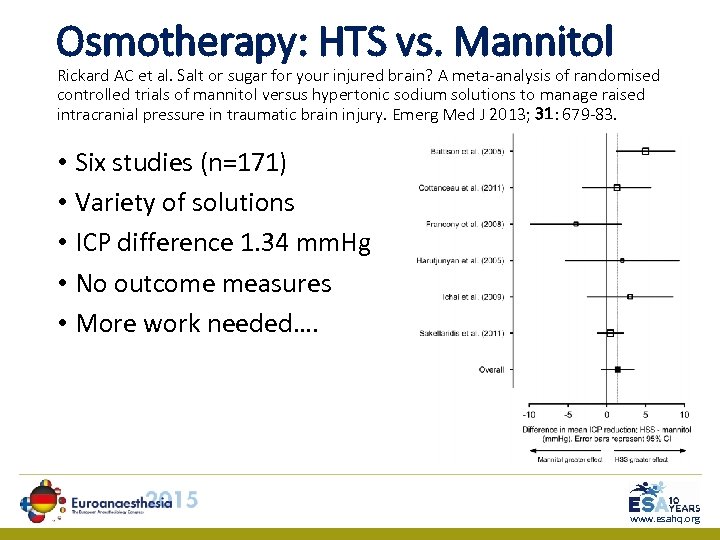
Osmotherapy: HTS vs. Mannitol Rickard AC et al. Salt or sugar for your injured brain? A meta-analysis of randomised controlled trials of mannitol versus hypertonic sodium solutions to manage raised intracranial pressure in traumatic brain injury. Emerg Med J 2013; 31: 679 -83. • Six studies (n=171) • Variety of solutions • ICP difference 1. 34 mm. Hg • No outcome measures • More work needed…. www. esahq. org
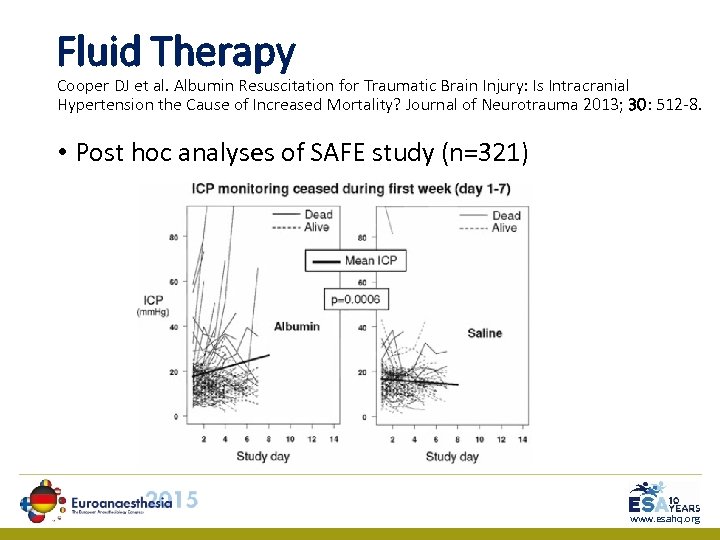
Fluid Therapy Cooper DJ et al. Albumin Resuscitation for Traumatic Brain Injury: Is Intracranial Hypertension the Cause of Increased Mortality? Journal of Neurotrauma 2013; 30: 512 -8. • Post hoc analyses of SAFE study (n=321) www. esahq. org
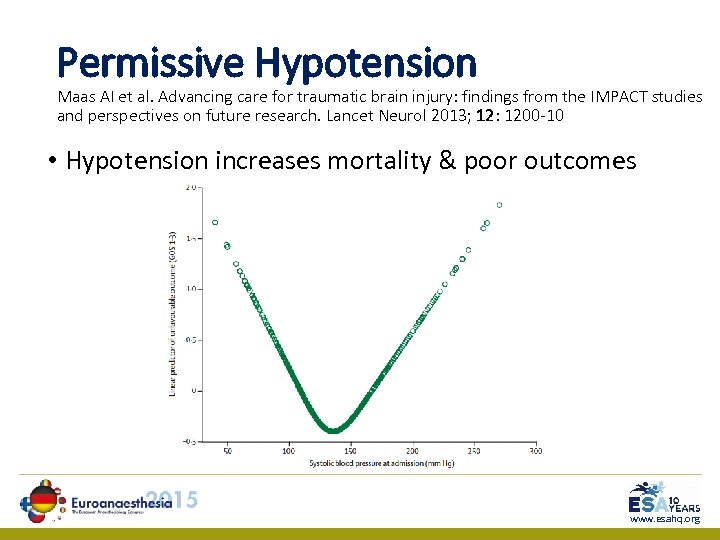
Permissive Hypotension Maas AI et al. Advancing care for traumatic brain injury: findings from the IMPACT studies and perspectives on future research. Lancet Neurol 2013; 12: 1200 -10 • Hypotension increases mortality & poor outcomes www. esahq. org
Permissive Hypotension Wiles MD. Blood pressure management in trauma: from feast to famine? Anaesthesia 2013; 68: 445– 452 • “Trials” of permissive hypotension excluded patients with TBI • Evidence of reduction in haemorrhage with permissive hypotension is lacking in clinical studies • Much (all) is extrapolated from animal models www. esahq. org
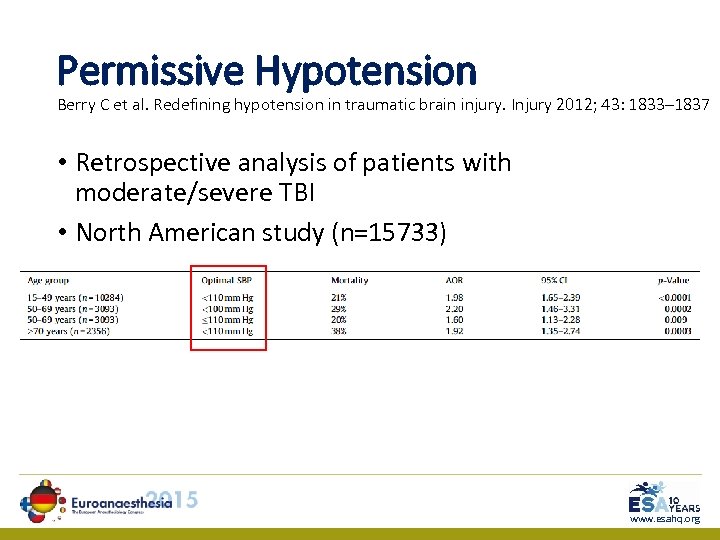
Permissive Hypotension Berry C et al. Redefining hypotension in traumatic brain injury. Injury 2012; 43: 1833– 1837 • Retrospective analysis of patients with moderate/severe TBI • North American study (n=15733) www. esahq. org
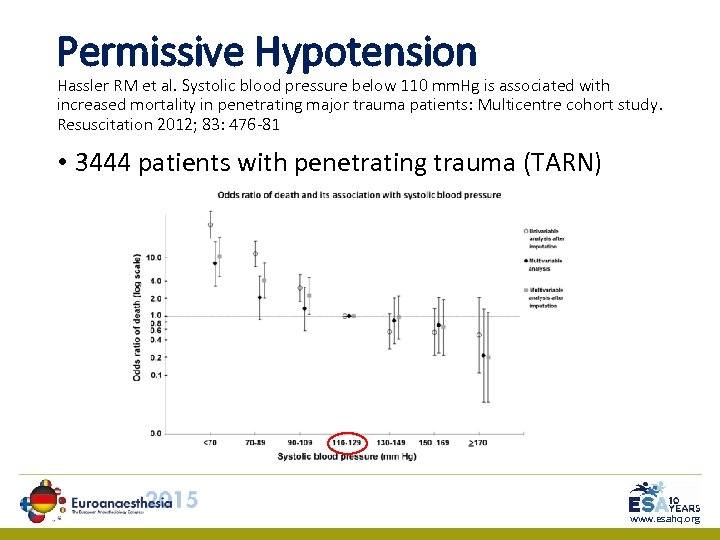
Permissive Hypotension Hassler RM et al. Systolic blood pressure below 110 mm. Hg is associated with increased mortality in penetrating major trauma patients: Multicentre cohort study. Resuscitation 2012; 83: 476 -81 • 3444 patients with penetrating trauma (TARN) 1 www. esahq. org
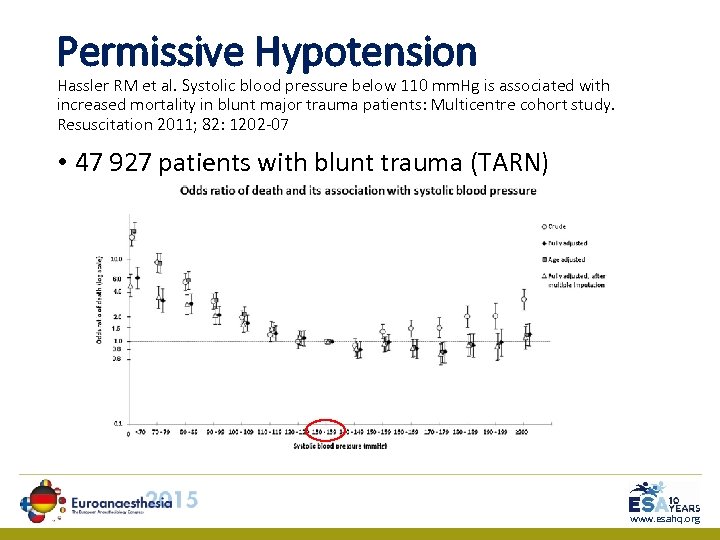
Permissive Hypotension Hassler RM et al. Systolic blood pressure below 110 mm. Hg is associated with increased mortality in blunt major trauma patients: Multicentre cohort study. Resuscitation 2011; 82: 1202 -07 • 47 927 patients with blunt trauma (TARN) 1 www. esahq. org
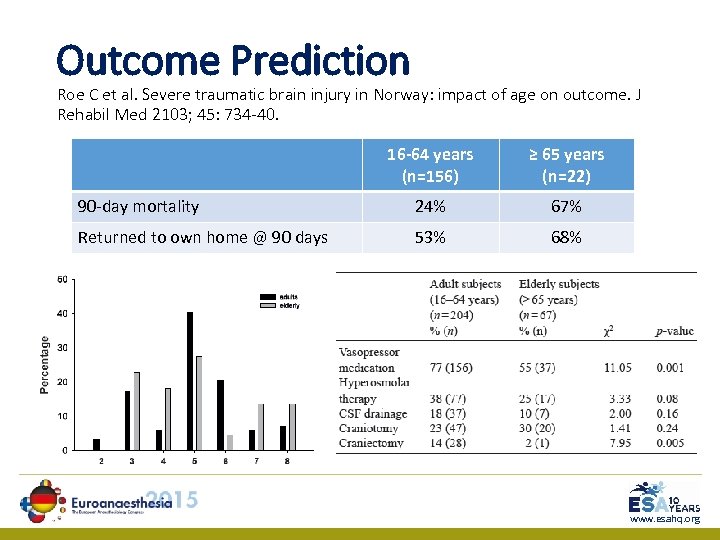
Outcome Prediction Roe C et al. Severe traumatic brain injury in Norway: impact of age on outcome. J Rehabil Med 2103; 45: 734 -40. 16 -64 years (n=156) ≥ 65 years (n=22) 90 -day mortality 24% 67% Returned to own home @ 90 days 53% 68% www. esahq. org
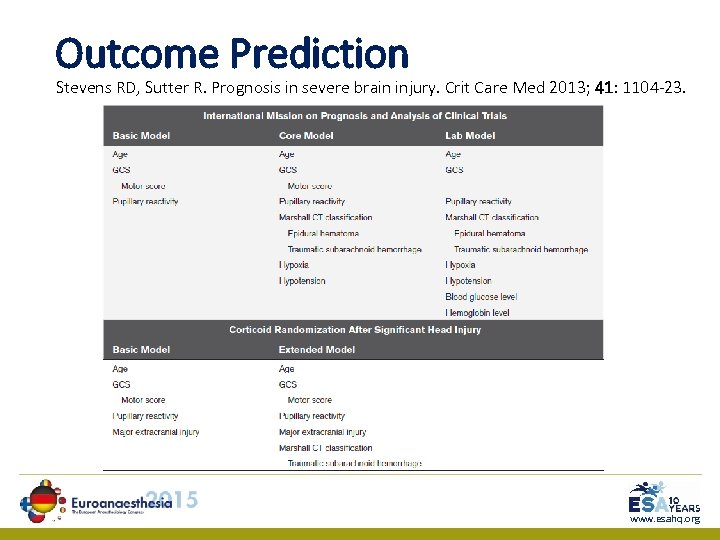
Outcome Prediction Stevens RD, Sutter R. Prognosis in severe brain injury. Crit Care Med 2013; 41: 1104 -23. www. esahq. org
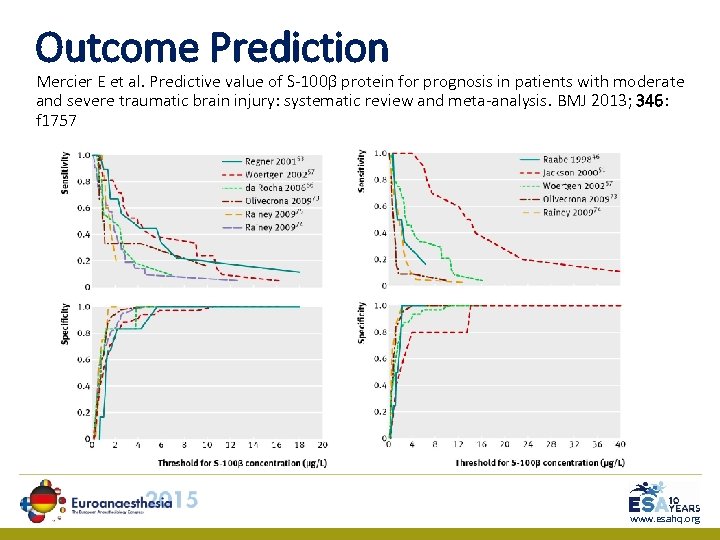
Outcome Prediction Mercier E et al. Predictive value of S-100β protein for prognosis in patients with moderate and severe traumatic brain injury: systematic review and meta-analysis. BMJ 2013; 346: f 1757 www. esahq. org
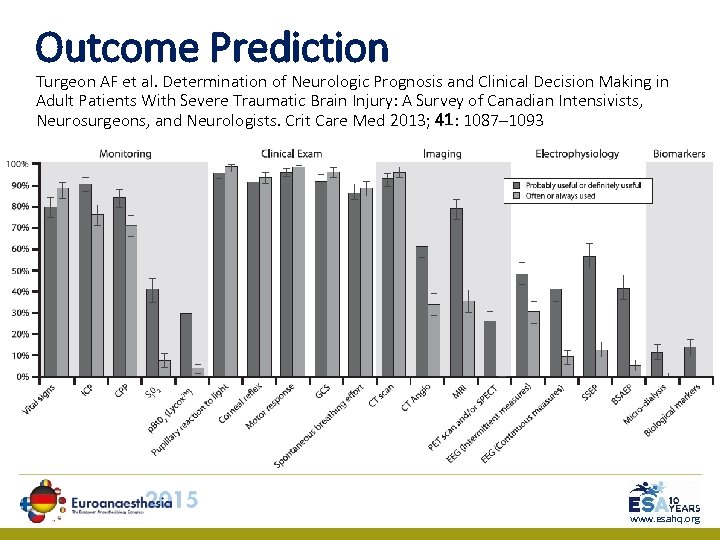
Outcome Prediction Turgeon AF et al. Determination of Neurologic Prognosis and Clinical Decision Making in Adult Patients With Severe Traumatic Brain Injury: A Survey of Canadian Intensivists, Neurosurgeons, and Neurologists. Crit Care Med 2013; 41: 1087– 1093 www. esahq. org
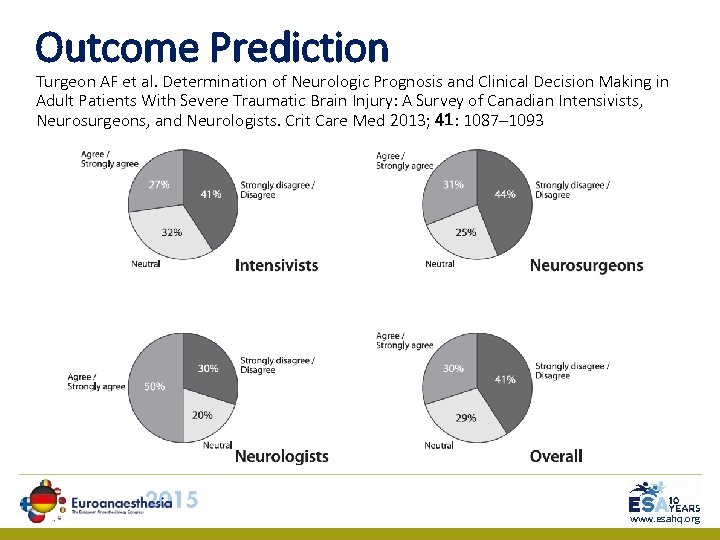
Outcome Prediction Turgeon AF et al. Determination of Neurologic Prognosis and Clinical Decision Making in Adult Patients With Severe Traumatic Brain Injury: A Survey of Canadian Intensivists, Neurosurgeons, and Neurologists. Crit Care Med 2013; 41: 1087– 1093 www. esahq. org
“The lack of improvement in head injured patients is typified by the apparent overall lack of progress in head injury care, which is suggested by the failure to identify a single therapy to improve outcome despite over 250 randomised controlled trials. However, several studies have shown that the institution of packages of specialist neurosurgical or neurocritical care is associated with improved outcomes. ” www. esahq. org
Summary • Therapeutic targets • Hypotension still bad for brains • Intracranial pressure monitoring • Just a number but (probably) useful as part of neurocritical care package • Decompressive craniectomy • Size may matter; await RESCUEICP • Osmotherapy • HTS or mannitol will lower ICP but not alter outcomes • Prognostication • S-100β protein shows promise www. esahq. org
200f12313127c31bbded88155664eca4.ppt