d14936a0ce3579c361d32437a3cd20f4.ppt
- Количество слайдов: 34

NICE’s role in establishing guidelines and Quality standards Dr Françoise Cluzeau, Associate Director, NICE International Dr Ryan Li, Adviser, NICE International

Overview • NICE, its role, structure, funding & governance • Guidelines & Quality Standards process and methods • Enhancing guidance implementation and pay for performance • How does the work of NICE improve care quality? • Learning from other countries

NICE…. what is it ? The National Institute for Health & Care Excellence (NICE) is the independent organisation responsible for providing national guidance and advice to improve health and social care

NICE as an organisation

Roles of NICE

Range & products • medicines, treatments, procedures, diagnostics & devices • clinical guidelines & pathways • Quality Standards, performance metrics and a range of information services for those providing commissioning and managing services across the spectrum of health and social care. Shared Learning Awards

Centres & support services Clinical Practice Clinical Guidelines Medicines and Prescribing Centre Safe staffing guidelines Health Technology Evaluation Technology Appraisals Surgical interventions Health & Social Care Quality Standards Implementation NICE pathways Devices and Diagnostics Social Care PASL Scientific Advice Prevention NICE International R&D Accreditation Communication Business, Planning & resources Evidence Resources Public involvement

Funding & expenditure Funding Expenditure National Institute for Health and Care Excellence Annual Report and Accounts 2013/14

NICE’s core principles Scientific Rigour Inclusiveness Timeliness Support for implementation Accountabilit y for reasonablen ess Review Transparency Independence Challenge

NICE GUIDELINES AND QUALITY STANDARDS 10

Why NICE clinical guidelines and quality standards? • Variation in care and health outcomes across the country – “postcode lottery” – “Different organisations set different standards, using different methods [and] evidence… not clear which standards must be followed and which are optional” Sir Liam Donaldson, previous Chief Medical Officer • NICE given responsibility to develop guidance: – To promote cost-effective use of NHS resources – Based on best available evidence and participatory process 11

What are NICE Clinical Guidelines? • Broad guidance covering management of a particular condition • Considers clinical and costeffectiveness, and patient/carer perspective • Incorporates other relevant NICE guidance (e. g. Technology Appraisals for specific drugs) • Recommendations are advisory, not mandatory… but can be used to develop quality standards

What are NICE guidelines and quality standards? A comprehensive set of recommendations for a particular disease or condition Evidence (e. g. clinical trials, health economic studies) Evidence-based Clinical Guidelines Quality Standards A prioritised, concise set of statements (usually 6 -8) with associated measurable indicators, chosen and adapted from the Clinical Guideline recommendations

NICE quality standards define best practice, not minimum standards NICE quality standards CQC- Registration requirements Proportion of services Standard of services Unsafe Substandard Adequate Good Excellent Quality standards complement regulatory or other minimum requirements

Example: Quality standard for stroke developed from NICE guideline NICE clinical guideline recommendation (2008) Brain imaging should be performed immediately* for people with acute stroke if any of the [indications] apply. *’Immediately’ is defined as ‘ideally the next slot and definitely within 1 hour, whichever is sooner’ Quality standard (NICE 2010) Patients with acute stroke receive brain imaging within 1 hour of admission if they meet any of the indications for immediate imaging. Indications for immediate brain imaging: • Indications for thrombolysis or early anticoagulation treatment • On anticoagulant treatment • Known bleeding tendency • Depressed level of consciousness (Glasgow Coma Score < 13) • Unexplained progressive or fluctuating symptoms • Papilloedema, neck stiffness or fever • Severe headache at onset of stroke symptoms. 15
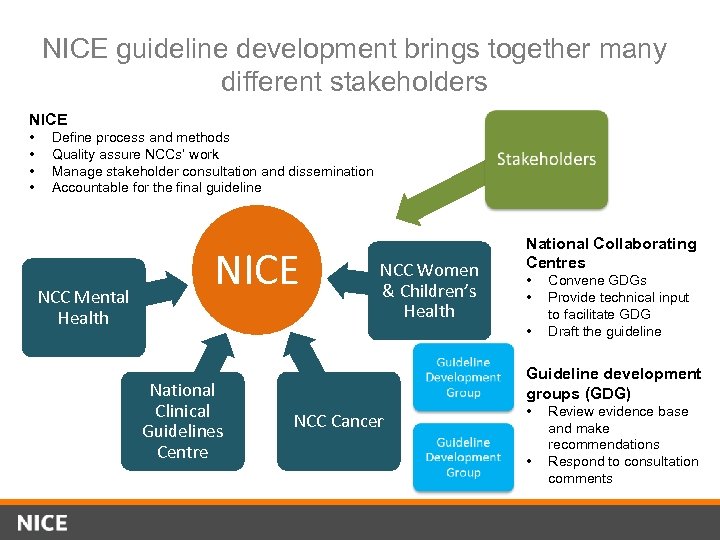
NICE guideline development brings together many different stakeholders NICE • • Define process and methods Quality assure NCCs’ work Manage stakeholder consultation and dissemination Accountable for the final guideline NCC Mental Health NICE NCC Women & Children’s Health National Collaborating Centres • • • National Clinical Guidelines Centre Convene GDGs Provide technical input to facilitate GDG Draft the guideline Guideline development groups (GDG) NCC Cancer • • Review evidence base and make recommendations Respond to consultation comments

Guideline development is a systematic process with stakeholder participation throughout Draft scope 4 months Stakeholder comments Final scope 13 -16 months GDG develops guideline Scoping Development Consultation on draft guideline Stakeholder comments Consultation on draft guideline 9 months Revise guideline after comments Pre-publication check Prepare and publish guideline Final guideline published Validation Publication and dissemination

The Guideline Development Group (GDG) is crucial to each guideline • Multi-disciplinary committee consisting of – Chair: usually highly experienced and respected clinical leader – Clinical and academic experts – Patients, carers and lay members – NCC technical team • GDG members bring their own expertise from different perspectives, but do not represent particular organisations • All members have equal status

Key role of the GDG is to make judgements based on the evidence Effectiveness Costeffectiveness Legal and policy constraints Extent of uncertainty & Irreversibility of decision NICE DECISIONS Practicalities of implementation Other social values: ethics, equity, rights

Developing guidelines – some challenges…. • Scope – What to include/exclude? • Timeliness • Taking into account cost-effectiveness – Selecting topics for economic modelling – When to rely on published data • Keeping guidelines up to date

Helping compliance /implementation – Baseline assessment/audit tools – Cost impact tools – Online educational tools – Local practice improvement – Financial incentives – Do they work? – What is the impact of NICE guidance Shared Learning Awards

Baseline assessment tool • Used to evaluate current practice and plan activity to meet NICE recommendations • Can serve to audit practice • Always used in conjunction with the guidelines they relate to

Cost Impact Statement Advise pregnant women with type 2 diabetes or gestational diabetes who are on a multiple daily insulin injection regimen to test their fasting, pre-meal, 1 -hour post-meal and bedtime blood glucose levels daily during pregnancy. (recommendation 1. 3. 2) Expert clinical opinion: recommendation could potentially double the number of testing strips being used by pregnant women with type 2 or gestational diabetes box of 50 testing strips costs £ 2. 29 (NHS electronic Drug Tariff). Expert clinical opinion suggests approximately 80% to 90% (1, 400) of women with type 2 diabetes and 20% (5, 600) of women with gestational diabetes are on a multiple daily insulin injection regimen


Local Practice improvement case studies_shared learning • Antibiotic prescribing for coughs reduced from 54. 5% to 37. 7% over 3 months • Antibiotic prescribing for URTI reduced from 32. 6% to 19. 7% over 3 months • In January alone, 67 patients avoided unnecessary prescription of antibiotics (over 700 fewer prescriptions in 1 year) Lessons • Buy-in of staff from across the practice • reinforcing the message to clinicians • Involving reception staff from the early stages as first contact with patients on the phone.

Pay for Performance in Primary Care Quality Outcomes Framework (QOF) • Introduced in 2004 – voluntary annual incentive scheme that rewards family doctors in the UK for improving care. • GPs get achievement points for: - Managing common diseases (asthma/diabetes) - Implementing preventative measures (blood pressure checks) - Targeting hard to reach / at risk groups (vaccinations and screening) • There are 75 indicators across 25 disease areas • NICE develops indicators, based on NICE guidelines/Quality Standards

How does the QOF work? • Point system: GP practices are scored against indicators across various domains • Higher score Higher GP income (adjusted for caseload and casemix) Significant expenditure and a significant incentive: £ 670 Million per year 15% of NHS primary care costs 15% of GP practice income

Does QOF improve outcomes? • Recording? – definitely • Process? – mostly yes • Intermediate/proxy outcomes? – yes for some but not for others • Clinical outcomes? – unclear – Strong evidence of initially improved health outcomes for a limited number of conditions but subsequently fell to the pre-existing trend; “limited impact on improving health outcomes due to its focus on process-based indicators. . . ” (Langdown et al. 2014, J Pub Health) – Some evidence that the poorest performing practices have improved the most with narrowing of inequalities in care (Gillam et al. 2012, Annals Fam Med)

Preventing VTEs üAn estimated 25, 000 people die from DVT each year. üMinisters said trusts that fail to act on the guidelines are likely to face financial penalties. üHospitals that fail to screen at least 90% of their patients will be penalised by withholding payments. üFrom 1 April 2010, a hospital could stand to lose 0. 3% of its income through the new Department of Health commissioning for quality and innovation framework.

VTE impact assessment: mandatory quarterly data collection by all acute care providers NICE guidance The documentation of risk assessment improved following the implementation of NICE guidance; it is questionable, however, whether this led to improved patient safety with respect to prescribing appropriate prophylaxis. Bateman et al. The implementation of nice guidance on venous thromboembolism risk assessment and prophylaxis: a before-after observational study to assess the impact on patient safety across four hospitals in England BMC Health Services Research 2013, 13: 203 • There has been a steady increase in the proportion of adult admissions risked assessed for VTE in all providers of NHS funded acute care, from 47% in July 2010 to 94% in December 2012.

NICE International is NICE’s non-profit programme since 2008 • Supporting foreign governments to make better policy decisions for better health o Technical support: HTA, guidelines and quality standards o Advice on process and governance: transparency, public and stakeholder involvement • Practical support projects (clinical pathways, quality standards) with country partners, including: China, India, Vietnam

Vietnam: QS for Stroke developed over 14 month, countryowned process Undertake situation analysis Define the topic for the QS Recruit a QS Committee Select relevant clinical guideline/pathway Develop the QS (3 workshops) Approve final draft and publish

MOH policymakers and clinicians across Vietnam engaged in deliberative process • Selected relevant recommendations to address high-priority clinical areas • Developed quality statements and measures, appropriate to Vietnamese context • Final product approved by Vice Minister 33

QS: a model of national/international partnership? • Effective partnership – Convened policymakers and stroke clinicians for the first time with direct policy impact • Stronger institutions – Mo. H incorporated QS in Hospital Quality Criteria – Pilot QS implementation funded through World Bank project • Better decisions – Focus on low cost, high impact interventions: prevention, joint working across disciplines, early diagnosis and rehabilitation – Full implementation could lead to improved care for 115, 000 patients, and net savings of US$2. 8 m per year 34
d14936a0ce3579c361d32437a3cd20f4.ppt