e354bc0678b0441c2385a8dab1a229ef.ppt
- Количество слайдов: 113
NH Bureau of EMS & NH 2009 Patient Care Protocol Vicki Blanchard Advanced Life Support Coordinator New Hampshire Department of Safety Division of Fire Standards and Training and EMS
An Overview Of The NH EMS System Division of Fire Standards and Training & Emergency Medical Services
The NH EMS System • • • EMS Laws & Rules The Bureau of EMS Staff Responsibilities Advisory Boards & Associations Resource Hospitals Instructor/Coordinators Regions & Districts Units Providers

Laws and Rules • Laws: Created by the House and Senate. Laws: Also known as RSAs (Revised Statutes Annotated) • Rules: Are the nuts and bolts of the day to day Rules: operation. Also known as NH Code of Administrative Rules
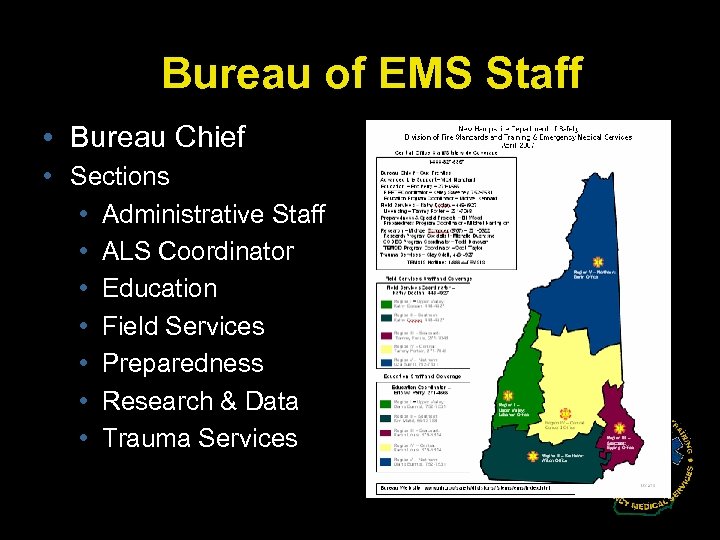
Bureau of EMS Staff • Bureau Chief • Sections • Administrative Staff • ALS Coordinator • Education • Field Services • Preparedness • Research & Data • Trauma Services
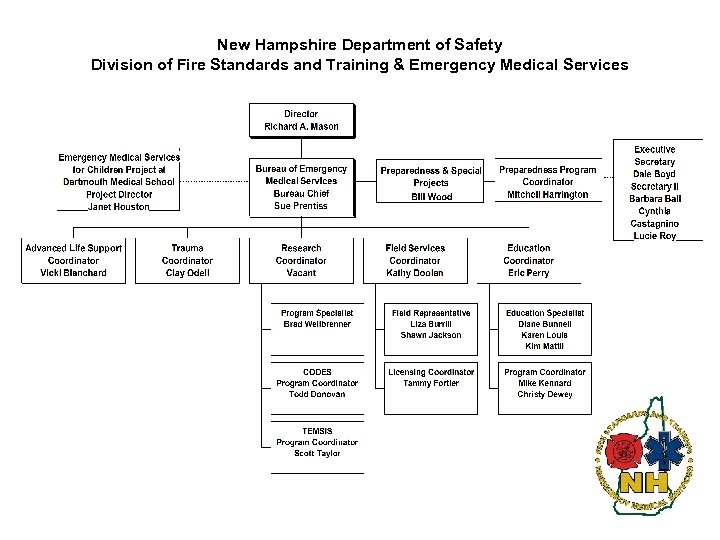
New Hampshire Department of Safety Division of Fire Standards and Training & Emergency Medical Services

Bureau Chief – Sue Prentiss • Overall Oversight & Responsibility
Administrative • Office Management Staff
ALS Coordinator – Vicki Blanchard • Protocols & Process ALS level
Education Coordinator – Eric Perry • Instructors/Testing/Trai ning QA & Standards

Field Services Coordinator Kathy Doolan • Liaison to Units & Hospitals, Licensing, Operations

Research & Quality Management • To create a quality management system for New Hampshire’s EMS system that improves the customer’s experience.
Preparedness & Special Projects Bill Wood • Preparedness • MCI • AEDs
Trauma Coordinator – Clay Odell • Statewide Trauma System and Preparedness Issues
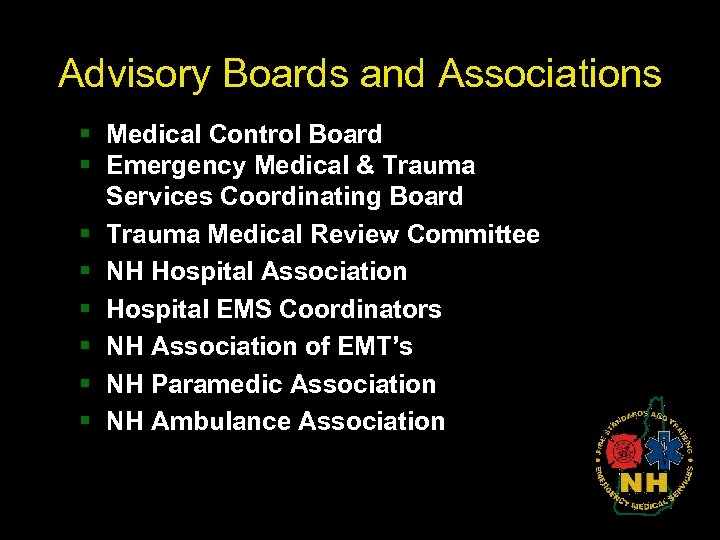
Advisory Boards and Associations § Medical Control Board § Emergency Medical & Trauma Services Coordinating Board § Trauma Medical Review Committee § NH Hospital Association § Hospital EMS Coordinators § NH Association of EMT’s § NH Paramedic Association § NH Ambulance Association
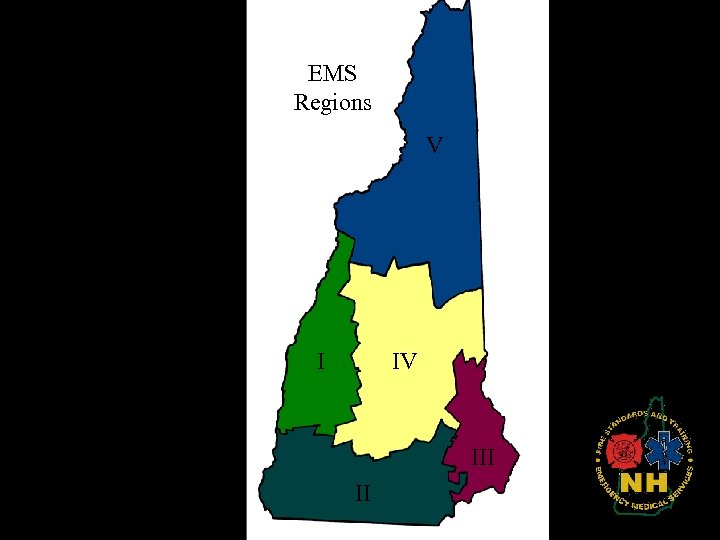
EMS Regions V I IV III II
Medical Control Board • RSA 153 -A: 5 III…duties (c) Serving as a liaison with medical personnel throughout the state. (e) With the concurrence of the state pharmacy board, specifying noncontrolled prescription drugs that emergency medical care providers licensed under this chapter may possess for emergency use as authorized in RSA 318: 42, X. (f) With the concurrence of the state pharmacy board, specifying controlled prescription drugs that advanced emergency medical care providers licensed under this chapter may possess for emergency use as authorized in RSA 318 -B: 10, V. (g) Approving the protocols and procedures to be used by emergency medical care providers under their own licenses or through medical control.
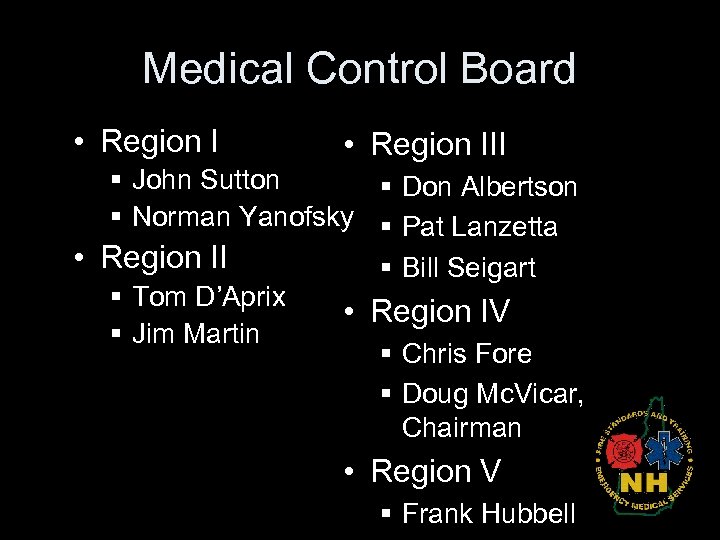
Medical Control Board • Region III § John Sutton § Don Albertson § Norman Yanofsky § Pat Lanzetta • Region II § Bill Seigart § Tom D’Aprix • Region IV § Jim Martin § Chris Fore § Doug Mc. Vicar, Chairman • Region V § Frank Hubbell
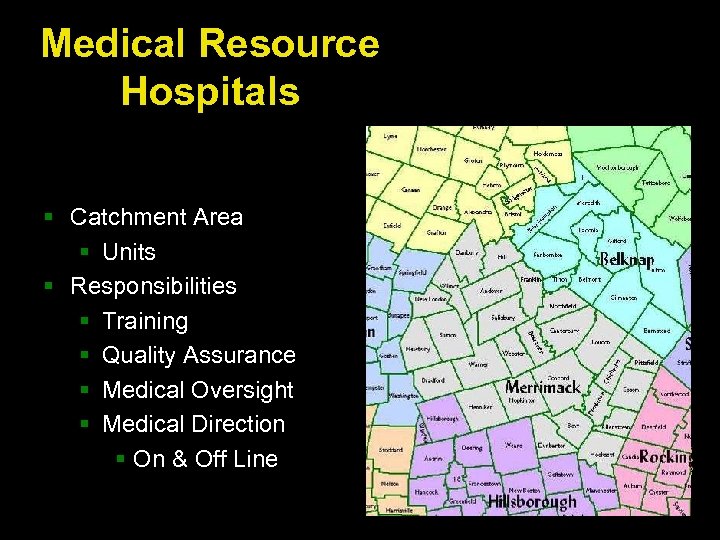
Medical Resource Hospitals § Catchment Area § Units § Responsibilities § Training § Quality Assurance § Medical Oversight § Medical Direction § On & Off Line

Medical Director • • Education Leadership Advice Critiques Performance improvement Medications Treatment modalities
The NH EMS Licensed Provider Levels § § § Apprentice Providers First Responders EMT-Basics EMT-Intermediates EMT-Paramedics PA/RN/MD’s = EMT’s § Other Entities : § National Ski Patrol / Lifeguards and Search & Rescue Agencies
Protocol Process • MCB assigns protocol committee • Committee researches each protocol for evidence based documentation to update or change • Updates/changes brought to MCB for discussion, revisions, approval, or denial • Final approved document
Protocol Process • 2 year cycle § § Through May 2007 – rollout of 07 protocols May 07 – Nov 08 – research/updates Nov 08 – Jan 09 publication/final approval March 2009 – 09 rollouts begin
2009 Protocols

In General • Remove IVs from each individual protocol, as it is already in Routine Patient Care. • Standardize IV fluids throughout the document to read “ 0. 9% Na. Cl (normal saline) • Removed Consider ALS or paramedic intercept and oxygen administration, because this too is in Routine Patient Care
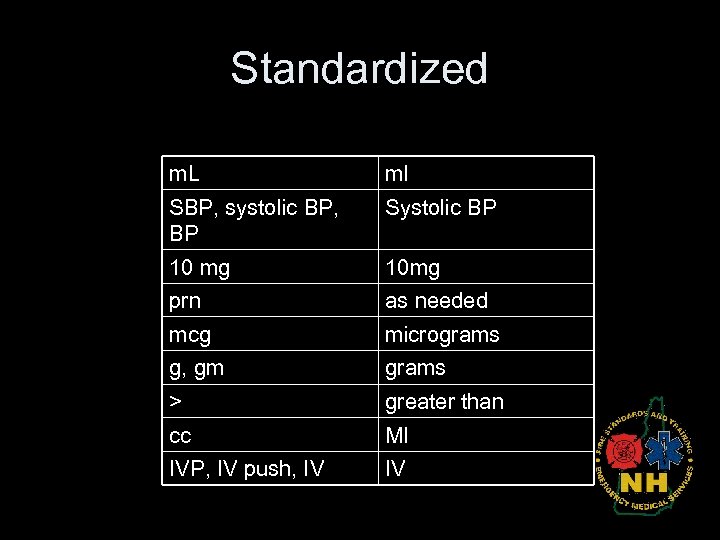
Standardized m. L ml SBP, systolic BP, BP Systolic BP 10 mg 10 mg prn as needed mcg micrograms g, gm grams > greater than cc Ml IVP, IV push, IV IV
Grammar • Examples of grammar: § Their / there § “repeated in 5 minutes, once” vs. “repeated once after 5 minutes. § Administer / give § hepa / HEPA
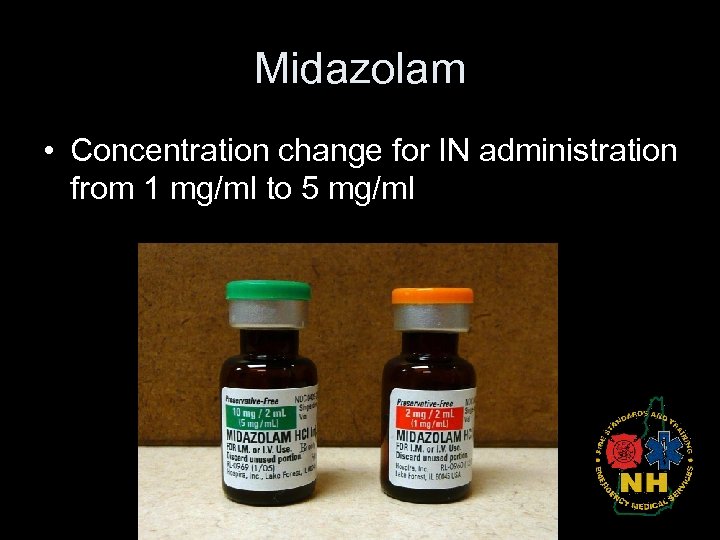
Midazolam • Concentration change for IN administration from 1 mg/ml to 5 mg/ml
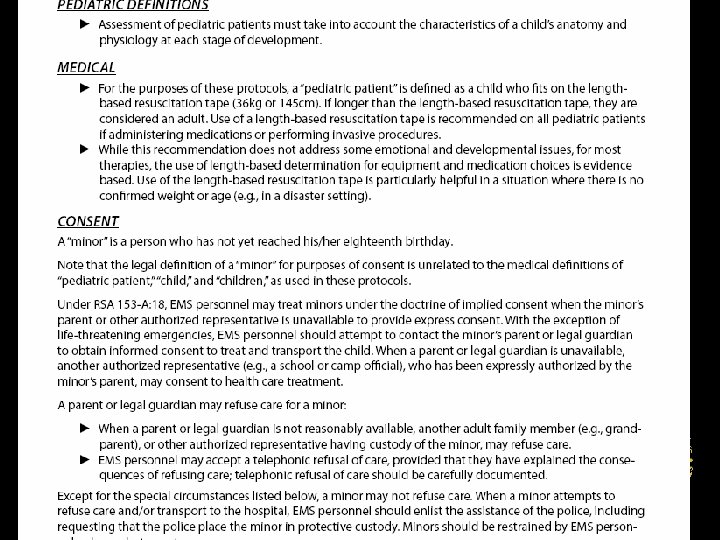
Routine Patient Care • Added tourniquets as a last resort when all other efforts have been exhausted. • Consent section added Sept/ Nov. 07
Apparent Life-Threatening Event • ALTE for children under 2 years was discussed previously in pediatric assessment. It was moved to its own protocol to prevent if from being overlooked. March 08
Status Determination and Transport Decision • Added definitions to the status categories • Updated the examples Sept. 07
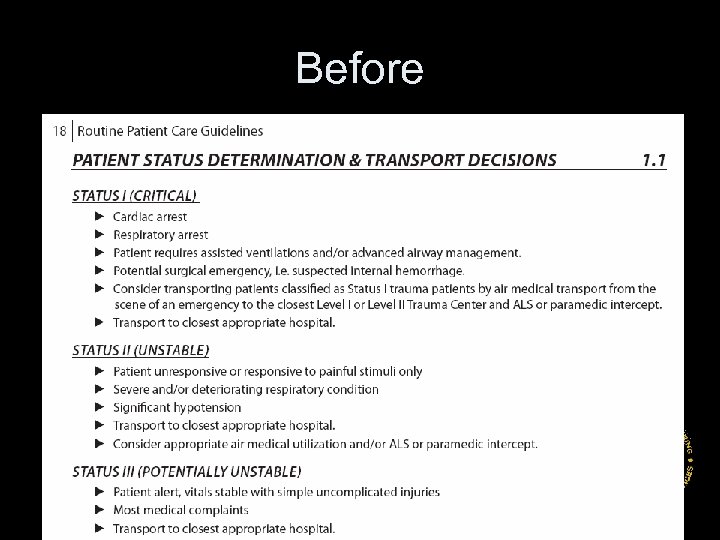
Before
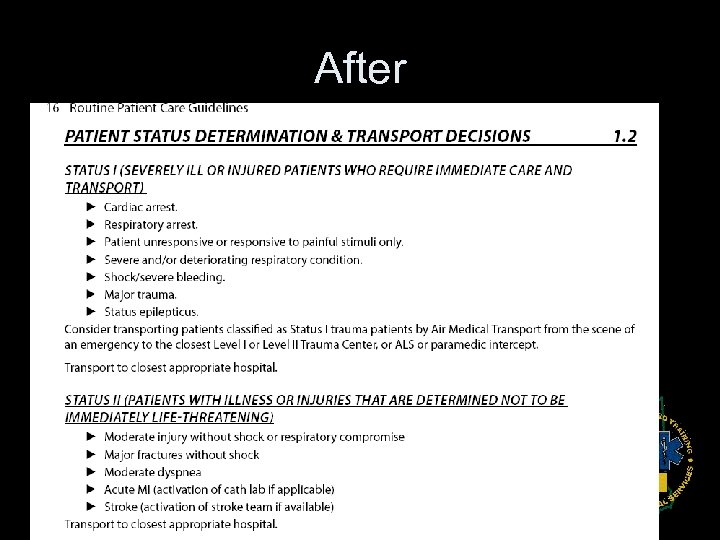
After
No Changes • Air Medical Transport • Communication Failure Sept. 07
Allergic Reaction/Anaphylaxis • Adult Intermediate: albuterol/ ipratropium mix (Duo. Neb ) § This will require a Transition program • Adult Paramedic: Removed the epinephrine infusion Sept/ Nov. 07
Asthma/COPD/RAD Adult & Pediatric Basic (Adult & Pediatric) • Add levalbuterol (Xopenex ) to the list of approved MDI • Change MDI assisting from § 2 puffs; every 5 minutes as needed to § 2 puffs; repeat every 5 minutes up to 3 times, as needed Intermediate (Adult only) • Albuterol/ ipratropium mix (Duo. Neb ) § This will require a transition program Reference: National Heart Lung and Blood Institute, NIH Publication No. 07 -4051 Sept/Nov. 07
Asthma/COPD/RAD Adult & Pediatric Paramedic • Added to the end of paramedic’s levalbuterol, “every 20 minutes up to a total of 4 doses. • Pediatric: similar changes with appropriate dosing • Pediatric: standardized the basic bullets with the adult protocol Reference: National Heart Lung and Blood Institute, NIH Publication No. 07 -4051 Sept/ Nov. 07
Behavioral Adult & Pediatric Paramedic • Changed Haloperidol route per FDA’s recommendation to IM only § Haloperidol 5 mg IM, may repeat once in 5 minutes • Diphenhydramine dose change to a range 25 – 50 mg IV or 50 mg IM Nov. 07

Diabetic Adult • Changed title to Hypoglycemia and Hyperglycemia • Added definition of hyperglycemia: glucose levels > 300 mg/dl with associated altered mental status • Added to oral glucose bullet that “the patient must be alert enough to swallow and protect airway” • Adult: Intermediate/Paramedic: § For hyperglycemia, administer 500 ml bolus 0. 9% Na. Cl (normal saline), then 250 m. L per hour, • Removed Thiamine Nov. 07
Diabetic Pediatric • Pediatric Paramedic: • Hypoglycemic Emergency § Administer dextrose per length-based resuscitation tape. • Hyperglycemic Emergency § 10 m. L/kg bolus in addition to maintaining hemodynamic status Nov. 07
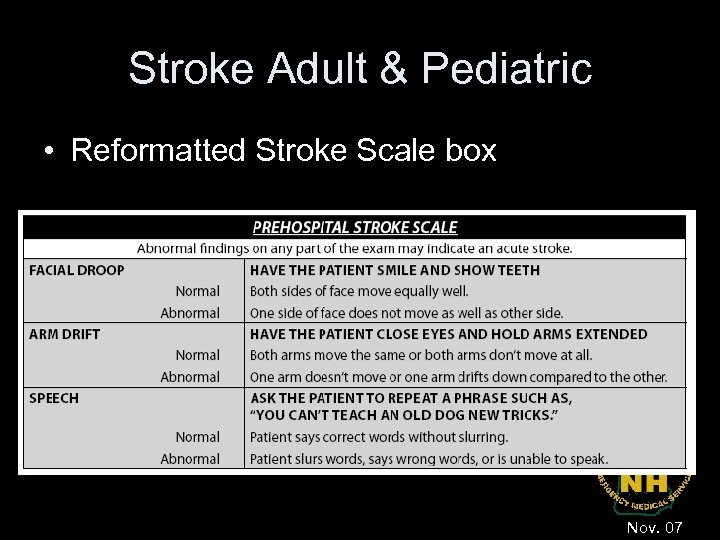
Stroke Adult & Pediatric • Reformatted Stroke Scale box Nov. 07
Hyperthermia Adult & Pediatric • Intermediate Adult: § 500 ml 0. 9% Na. Cl (normal saline) IV fluid bolus for dehydration • Paramedic Pediatric: § 10 – 20 ml/kg 0. 9% Na. Cl (normal saline( IV fluid bolus for dehydration • Bullet link for seizure activity Nov. 07
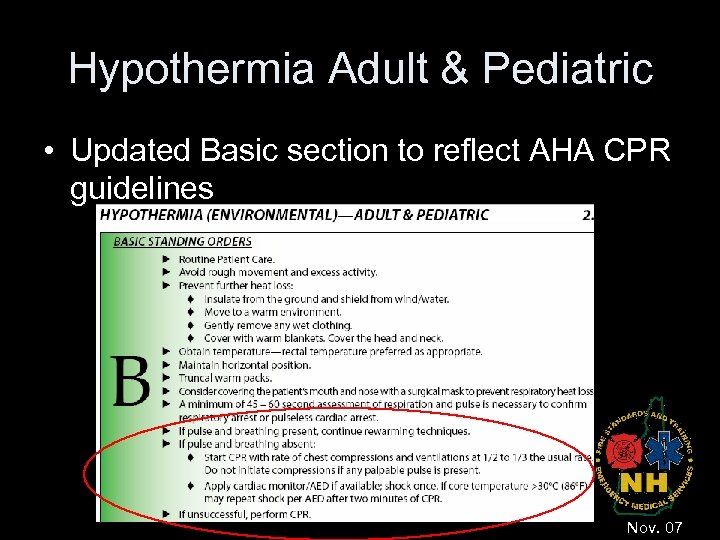
Hypothermia Adult & Pediatric • Updated Basic section to reflect AHA CPR guidelines Insert screen shot Nov. 07
Obstetrical Emergencies • Updated the Contact Medical control list to include § Limb presentation § Nuchal cord • Paramedic: Changed the oxytocin dose to 20 units in 1000 m. L 0. 9% Na. Cl (normal saline) to control post partum hemorrhage at a rate of 200 – 600 m. L/hr. • Paramedic: Added the bullet: Tocolysis for preterm labor: 0. 9% Na. Cl (normal saline) IV bolus 20 m. L/kg prn § Contraindications: Gestation beyond 37 weeks, pre-eclampsia, vaginal bleeding § Tocolysis: Rapid intravascular expansion which can diminish contractions of an irritable uterus Nov. 07
Care of the Newborn • A new protocol for the uncomplicated normal delivery • In the past normal delivery was incorporated into the newborn resuscitation, which is a bit of a contraindication…normal delivery and resuscitation. Nov 08
Newborn Resuscitation • This protocol assumes routine care of the newborn has been performed and reveals a newborn in need of resuscitation. Nov 08
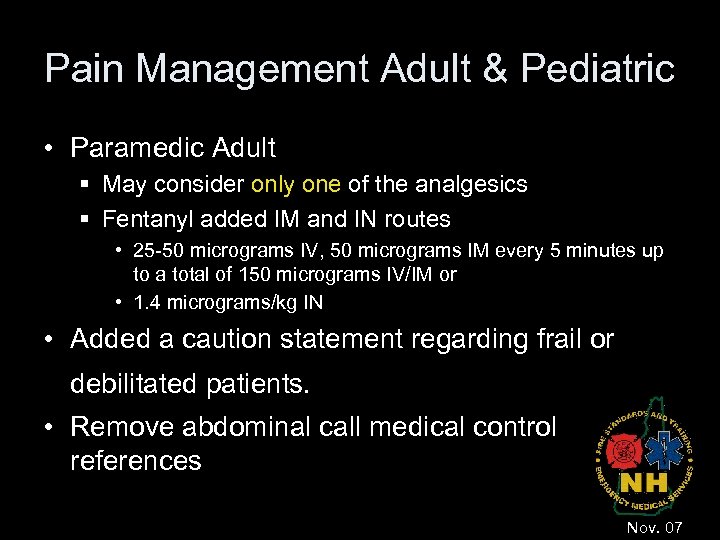
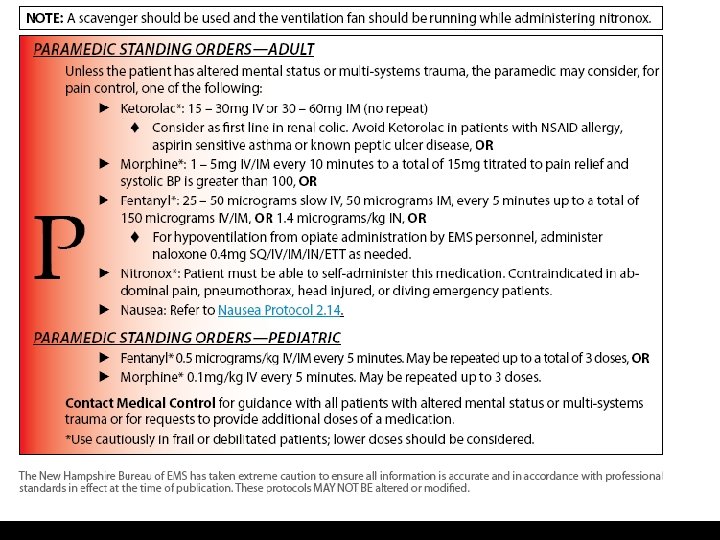
Pain Management Adult & Pediatric • Paramedic Adult § May consider only one of the analgesics § Fentanyl added IM and IN routes • 25 -50 micrograms IV, 50 micrograms IM every 5 minutes up to a total of 150 micrograms IV/IM or • 1. 4 micrograms/kg IN • Added a caution statement regarding frail or debilitated patients. • Remove abdominal call medical control references Nov. 07
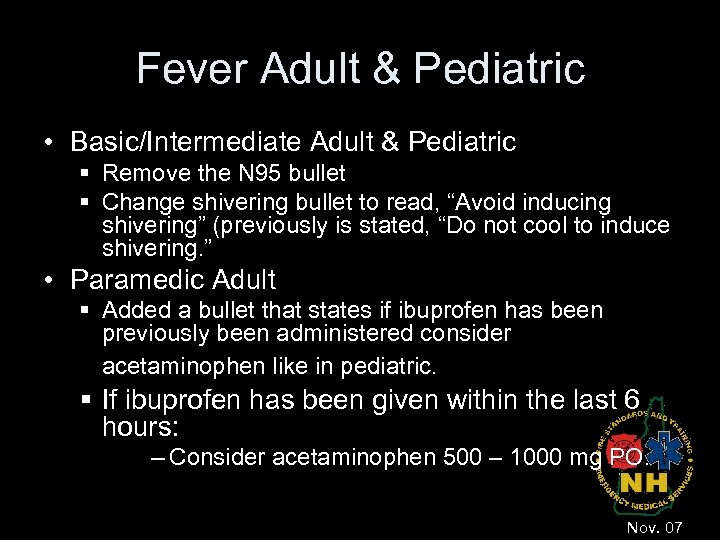
Fever Adult & Pediatric • Basic/Intermediate Adult & Pediatric § Remove the N 95 bullet § Change shivering bullet to read, “Avoid inducing shivering” (previously is stated, “Do not cool to induce shivering. ” • Paramedic Adult § Added a bullet that states if ibuprofen has been previously been administered consider acetaminophen like in pediatric. § If ibuprofen has been given within the last 6 hours: – Consider acetaminophen 500 – 1000 mg PO. Nov. 07
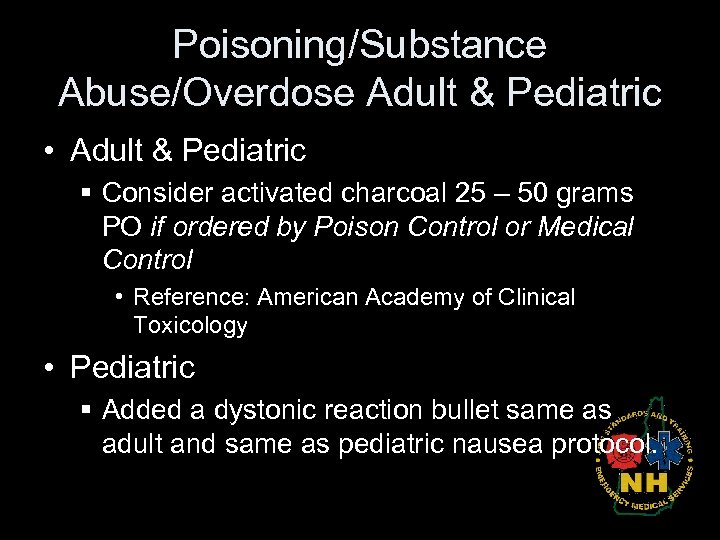
Poisoning/Substance Abuse/Overdose Adult & Pediatric • Adult & Pediatric § Consider activated charcoal 25 – 50 grams PO if ordered by Poison Control or Medical Control • Reference: American Academy of Clinical Toxicology • Pediatric § Added a dystonic reaction bullet same as adult and same as pediatric nausea protocol.
Seizure Adult & Pediatric • Updated Vagus Nerve Stimulator Bullets to be more descriptive Nov. 07
Nausea/Vomiting Adult & Pediatric • Intermediate Adult § 500 ml 0. 9% Na. Cl (normal Saline) IV fluid bolus for dehydration IV bullet to 0. 9% Na. Cl (normal saline) IV fluid bolus 10 – 20 ml/kg for dehydration • Under the Paramedic § Prochlorperazine dose increased to 5 mg – 10 mg (was 2. 5 mg) § Removed Promethazine § Changed metoclopramide to just 5 mg IV or IM (was 0. 1 mg/kg up to 5 mg) § Changed the repeat to: May repeat any of the above medications once after 10 minutes if nausea/vomiting persist § Added to granisetron “over 5 minutes” one dose only both adult and pediatric Nov. 07
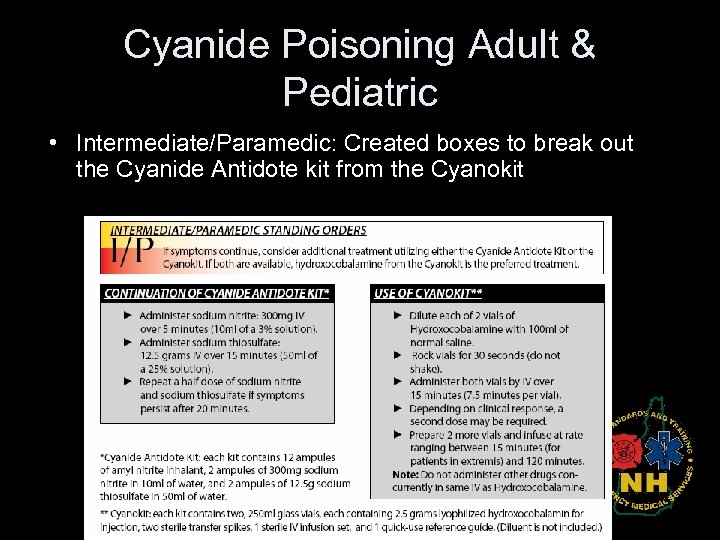
Cyanide Poisoning Adult & Pediatric • Intermediate/Paramedic: Created boxes to break out the Cyanide Antidote kit from the Cyanokit
Bradycardia Adult & Pediatric • Bradycardia – Paramedic Adult § Broke out “Symptomatic and Hemodynamically Unstable” from “Symptomatic, but Hemodynamically Stable” • Bradycardia – Basic/Intermediate Pediatric § added reasons for underlying causes. Jan 08
Tachycardia Adult & Pediatric • Tachycardia – Paramedic Adult § Reordered PSVT, WPW and AF/Aflutter for better flow and added midazolam 2. 5 mg IV, IM, IN under sedation • Tachycardia – Paramedic Pediatric § Broke out “Symptomatic and Hemodynamically Unstable” and “Symptomatic, but Hemodynamically Stable” for continuity. Jan 08
ACS Adult • All patients with complaints of chest pain should not automatically be treated with ASA and NTG. You should consider the likelihood of ACS based on the nature of the symptoms, the patients age, cardiac risk factors, past medical history, etc. ” • Grammatical changes to the Fibrinolytic Questionnaire Box and Cath Lab Activation box. • Changed morphine dose to be consistent with the rest of the document. Jan 08
Congestive Heart Failure (Pulmonary Edema) Adult • Intermediate – Added CPAP § This will require a transition module • Paramedic § Reordered treatment regime • • CPAP (starting at Intermediate level) NTG Furosemide or bumetanide Morphine Nov 07

Cardiac Arrest - Adult • Cardiac Arrest – Adult § Intermediates: • Intraosseous infusion via a commercial IO introduction device (examples EZ-IO, B. I. G. ) This will require a transition program § Paramedic: • Procainimide removed Jan 08
Cardiac Arrest - Pediatric • Basic § Updated the AED bullet to reflect recent approval of AED pads for newborns. • From birth to age eight use pediatric AED pads. – If pediatric AED pads are unavailable, providers may use adult AED pads, provided the pads do not overlap. • Paramedic § Reordered VFib/Pulseless VT and Asystole to be consistent with the Adult protocol. Jan 08
Drowning Adult & Pediatric • Grammatical changes Jan 08
Eye & Dental Injuries Adult & Pediatric • Paramedic § Tetracaine added § Proparacaine or tetracaine 2 drops to affected eye; repeat every 5 minutes as needed Nov 08
Burns Adult & Pediatric • Merged Adult and Pediatric. • Grammatical Jan 08
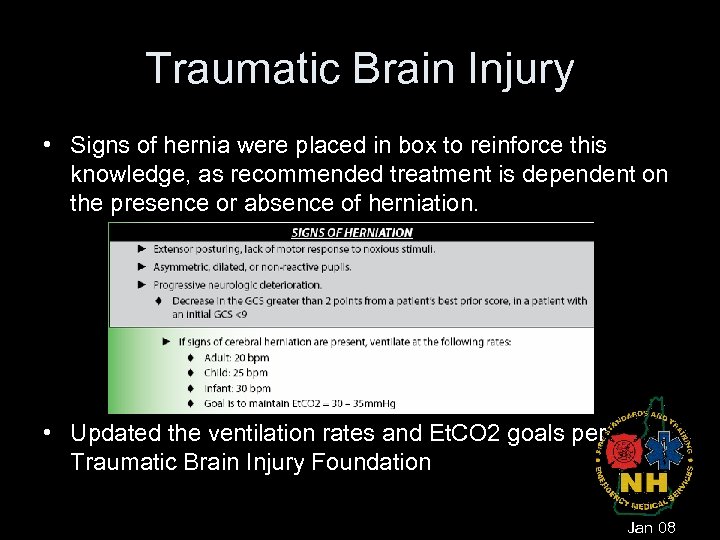
Traumatic Brain Injury • Signs of hernia were placed in box to reinforce this knowledge, as recommended treatment is dependent on the presence or absence of herniation. • Updated the ventilation rates and Et. CO 2 goals per Traumatic Brain Injury Foundation Jan 08
Thoracic Injuries Adult & Pediatric • Added bullet stating, “Do not splint the chest” • Updated signs of tension pneumothorax to include tracheal deviation March 08
Airway Management Protocols • • Airway Management – No change Gum Elastic Bougies – No change Orotracheal Intubation – No change Nasotracheal Intubation – Minor change removed pediatric redundancy March 08
Rapid Sequence Intubation • Maximum doses added: Etomidate (40 mg) and Succinylcholine (150 mg) • Cricoid pressure bullet changed to “maintained until proof of placement “ March 08
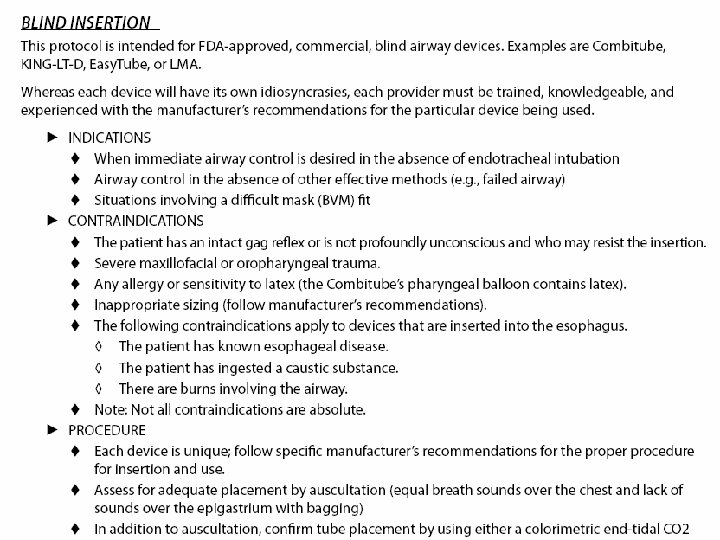
Blind Insertion Airways (King LT-D, Combi-tube, LMA) • Created a single generic blind insertion airway protocol which states “see manufacturer’s instructions” for individual March 08
Cricothyrotomy • Commercial device only • Age-appropriate commercial devices using technique of needle and guide-wire followed by dilatation. (like the Melker) March 08 & May 08
No Changes • Advanced Suctioning • Tracheostomy Care March 08
Intraosseous Access • Intermediate adult patients in cardiac arrest, commercial intraosseous introduction device • This will require a transition program • Lidocaine concentration changed to include 2% July & Nov 08
Umbilical Vein Cannulation • Grammatical March 08
No Changes • Vascular Access via Central Catheter • Immunization March 08
Bloodborne/Airborne Pathogens • Complete re-write incorporating updated standards from the Center of Disease Control and OSHA. • CDC & OSHA’s Bloodborne pathogens Standards 29 CFR – 1910. 1030 May 08
Crime Scene/Preservation of Evidence • No Change March 08
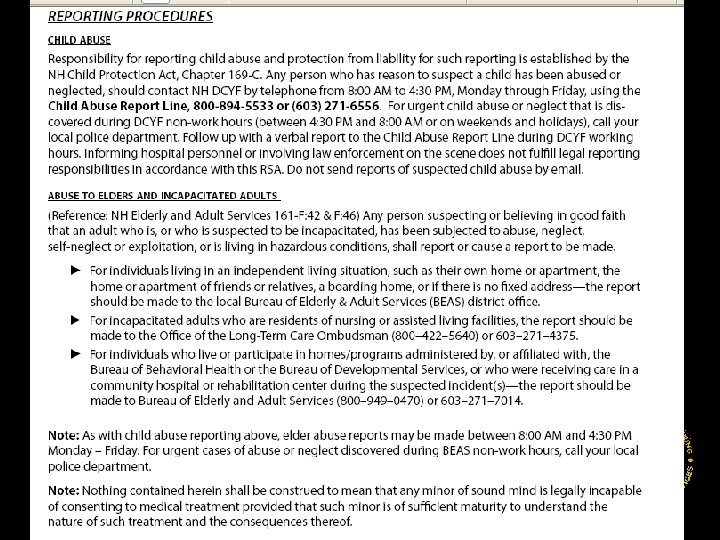
Abuse and Neglect • Reporting procedures section added. • The reporting section strengthened by adding language from applicable NH RSA. May 08
Response to Domestic Violence • Rewritten to heighten awareness of the potential dangers associated with domestic violence calls, and provider safety considerations. • Reference section added. May 08
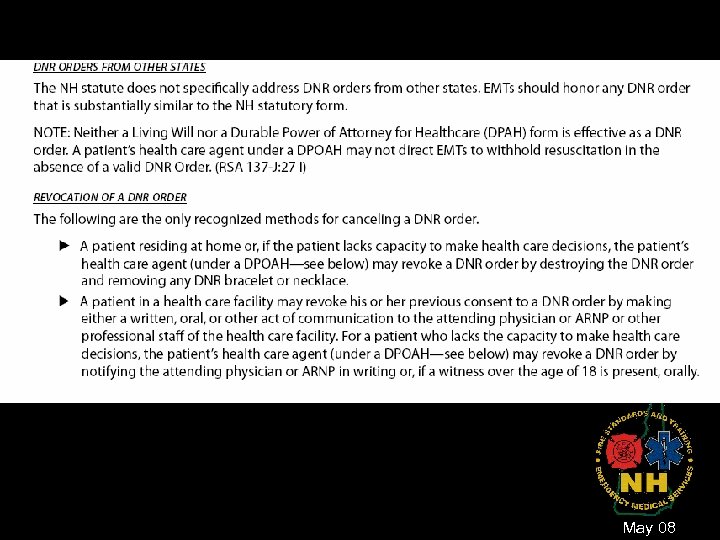
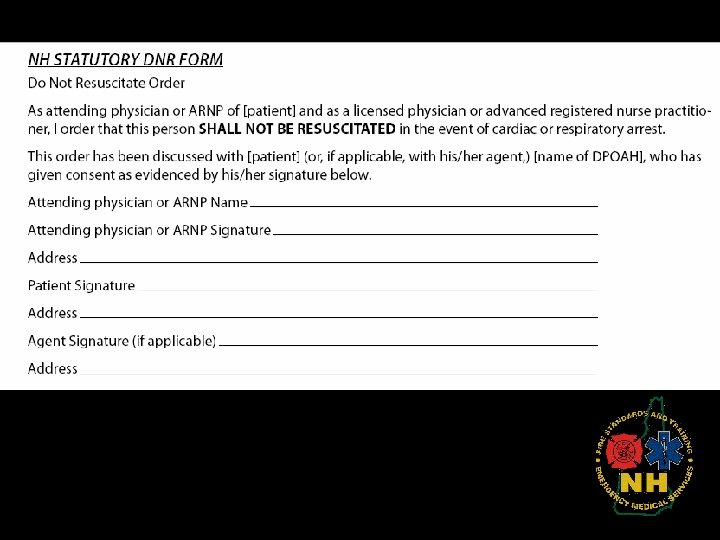
DNR • Clarified the duties of the Durable Power of Attorney for Healthcare. • Clarified revocation of a DNR. • Procedures section made more descriptive. May 08
May 08
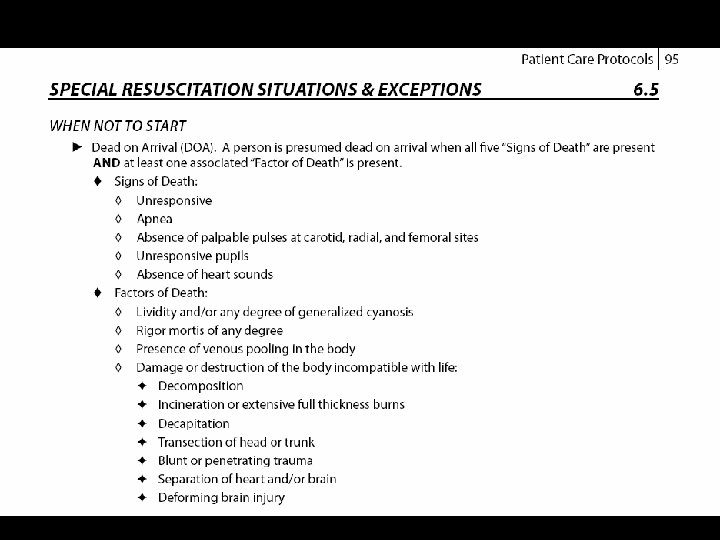
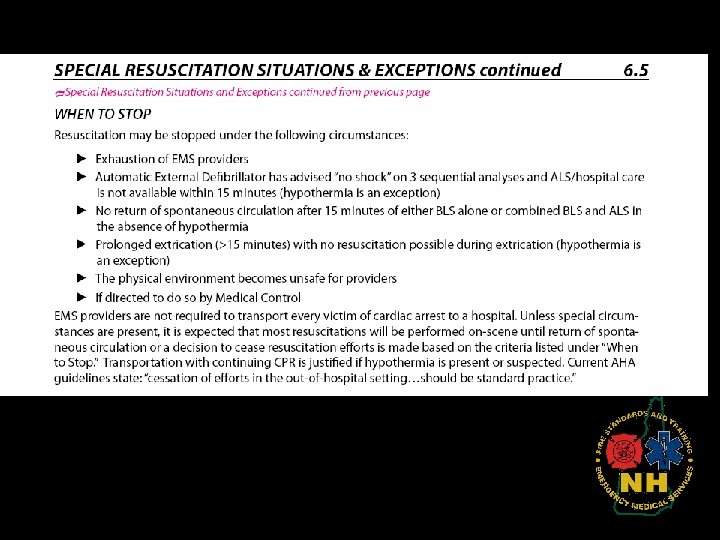
Special Resuscitation Situations and Exceptions • Signs of Death” updated and “Factors of Death” • Following the new AHA standard, EMS providers are not required to transport every victim of cardiac arrest to a hospital. • Keeping in mind the risk involved to the EMS provider of performing resuscitation efforts in the back of a moving ambulance, the protocol was updated to reflect AHA’s recommendation that “it is expected that most resuscitations will be performed on-scene until return of spontaneous circulation or a decision to cease resuscitation efforts is made based on the criteria listed under “When to Stop””. March 08
No Changes • Advanced Spinal Assessment • On-Scene Medical Personnel March 08
Refusal of Care • Rewrite of the competence section • Added a procedural section • Who is a patient? § Those people you, as an EMS provider, feel should go to the hospital, and the person is refusing to go. It is not for the person who is not hurt or injured. How can someone refuse care when no care was required. July 08
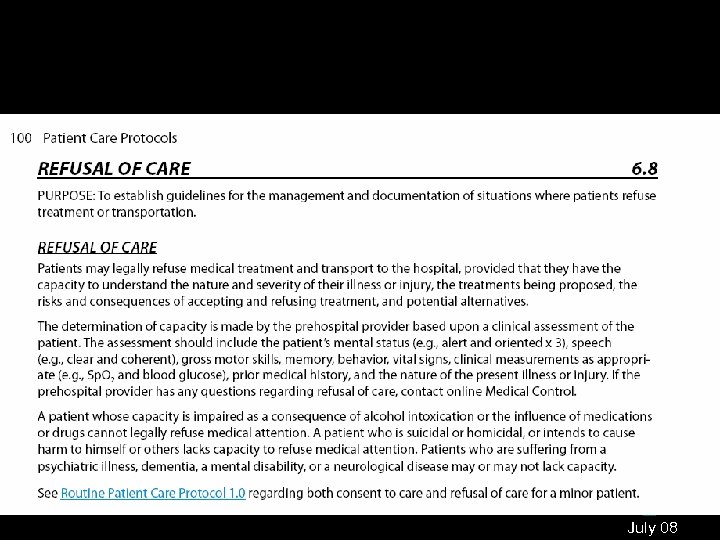
July 08
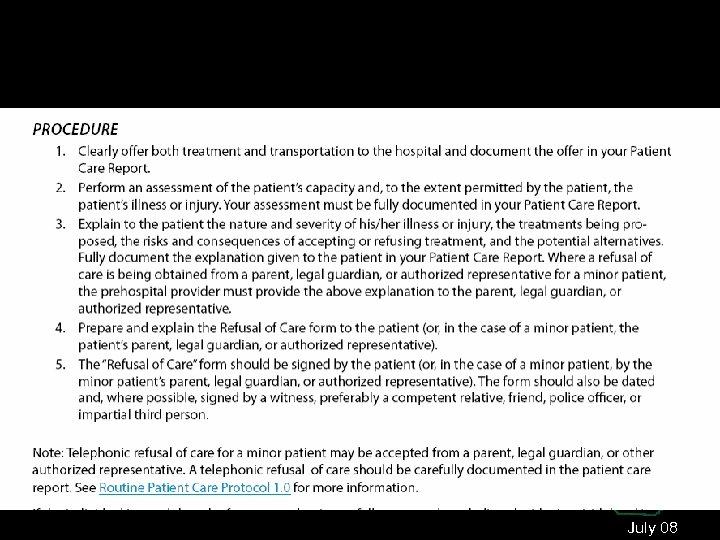
July 08
Pediatric Restraint • NH Law reference to seatbelt use in pediatrics • Updated to include 5 point restraints and isolette recommendations. • Added size limits to various types of car seats • Added examples of various car seats • Reference: Position Statement of Association of Air Medical Services, “Improved Restraint Usage for Infant and Pediatric Patients in Ground Ambulances through Education and Policy Development, May 08
Pediatric Restraint • Changed “Transport of Well Child” to “Non-Patient” to correctly discuss the transport of a child who is not a patient. • For those ill children who need to be placed directly on the cot so that appropriate care may be rendered: • Belting child directly to cot in manner to prevent ramping or sliding in a crash § Loop narrow belts over each shoulder and under arms, attaching to a non-sliding cot member § Use soft, sliding or breakaway connector to hold shoulder straps together on chest § Anchor belt to non-sliding cot member and rout over thighs, not around waist. May 08
Interfacility Transfers • NH Protocol enables paramedics to continue medications that are not within their routine scope of practice, during an interfacility transport, provided that the medication was ordered and initiated prior to transport. The paramedic must proactively obtain working knowledge and education of any such medication –through such means as medication manuals or software, discussion with sending clinicians, discussion with medical director, etc. – prior to transporting the patient. Those medications identified by the NH EMS Medical Control Board as posing an increased risk of untoward effects such as paralytics, some sedatives, and vasoactive medications will also require completion of a NHBEMS approved education program. Paramedics must refuse to transport patients that have a level of acuity and/or medication regimen that the paramedic is not comfortable with, and work with the sending facility to acquire optimal staffing (such as sending nursing staff). • Stable patients with low risk of deterioration (Intermediate level) § Any crystalloid infusion containing less than 10 meq/lt Sept & Nov 08
Interfacility Transfer Medications • Training is available through your Medical Resource Hospital. Contact your EMS Hospital Coordinator • EMS Units are required to ensure their paramedics have this training • Paramedics are responsible for obtaining this training. • Encourage Units to purchase a good medication reference resource
No Changes • Hazardous Materials Exposure • Mass/Multiple Casualty Triage July 08
Nerve Agents & Organophosphates MCI • Duo. Dote Injectors and matrix box for ease of reading. • In addition, because an MCI could involve hours or days, the albuterol dose was changed from a total of 3 nebulizers to “as needed. ” July 08

July 08

Radiation Injuries MCI Adult and Pediatric • No change July 08
Basic Changes • Tourniquet for bleeding control as a last resort • Levalbuterol added to MDI list • Activated Charcoal only with advice from Poison Control or Medical Control • AEDs can be used on newborns
Intermediate Changes • Albuterol/ ipratropium mix (Duo. Neb ) for Adult Anaphylaxis and Asthma protocols § Requires transition program • CPAP for CHF/Pulmonary Edema § Requires transition program • Commercial Intraosseous introduction device (example: EZ-IO) § Requires transition program
Intermediate Changes • 500 ml bolus 0. 9% Na. Cl for hyperglycemia and dehydration (hyperthermia, fever, nausea/vomiting protocols) • No more thiamine • Intrafacility Transfer: Crystalloids containing less than 10 meq/lt of potassium
Paramedic Changes • Levalbuterol maximum use: four doses • Removed epinephrine infusion from adult anaphylaxis • Removed the IV route of administration from haloperidol administration. • Diphenhydramine dose change from 50 mg IV to 25 - 50 mg IV • Pediatric dextrose dose based on length based resuscitation tape
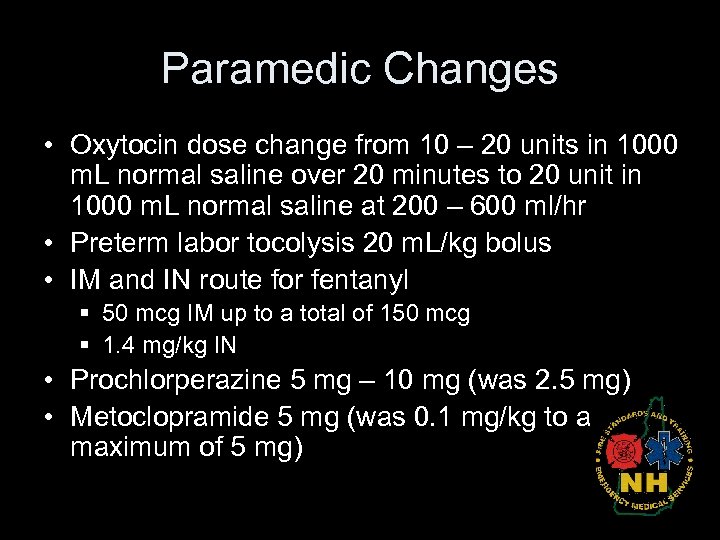
Paramedic Changes • Oxytocin dose change from 10 – 20 units in 1000 m. L normal saline over 20 minutes to 20 unit in 1000 m. L normal saline at 200 – 600 ml/hr • Preterm labor tocolysis 20 m. L/kg bolus • IM and IN route for fentanyl § 50 mcg IM up to a total of 150 mcg § 1. 4 mg/kg IN • Prochlorperazine 5 mg – 10 mg (was 2. 5 mg) • Metoclopramide 5 mg (was 0. 1 mg/kg to a maximum of 5 mg)
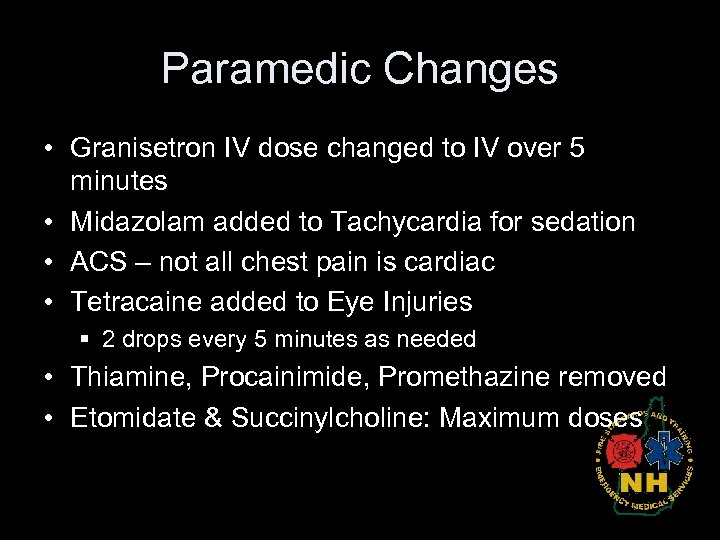
Paramedic Changes • Granisetron IV dose changed to IV over 5 minutes • Midazolam added to Tachycardia for sedation • ACS – not all chest pain is cardiac • Tetracaine added to Eye Injuries § 2 drops every 5 minutes as needed • Thiamine, Procainimide, Promethazine removed • Etomidate & Succinylcholine: Maximum doses
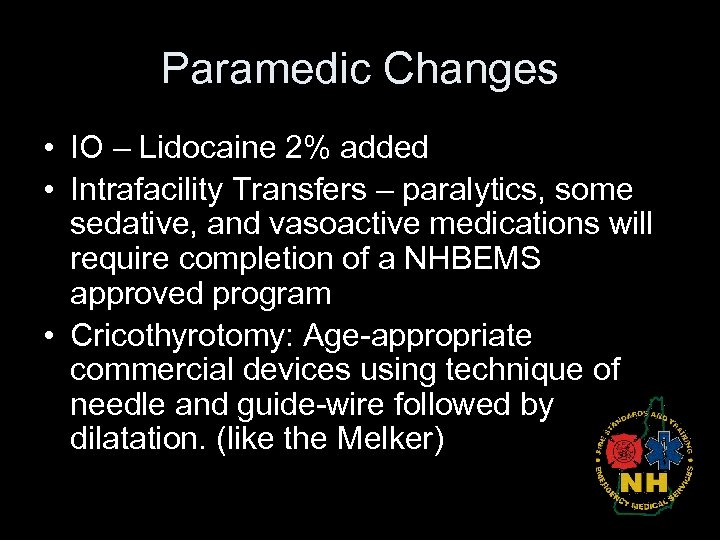
Paramedic Changes • IO – Lidocaine 2% added • Intrafacility Transfers – paralytics, some sedative, and vasoactive medications will require completion of a NHBEMS approved program • Cricothyrotomy: Age-appropriate commercial devices using technique of needle and guide-wire followed by dilatation. (like the Melker)
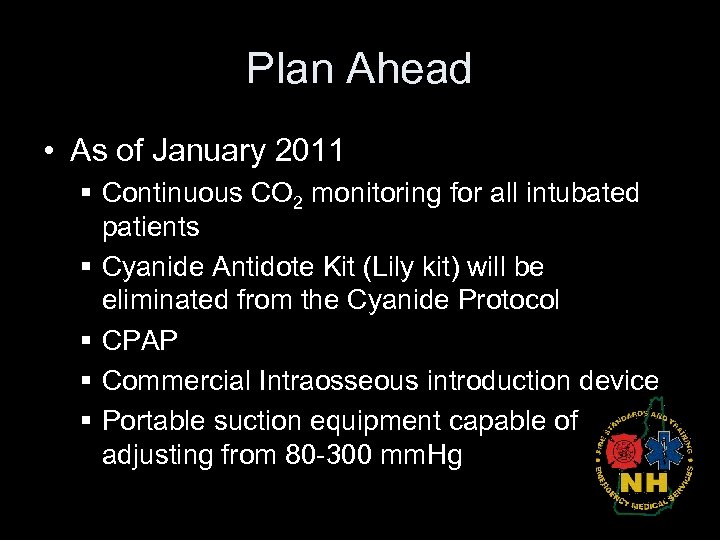
Plan Ahead • As of January 2011 § Continuous CO 2 monitoring for all intubated patients § Cyanide Antidote Kit (Lily kit) will be eliminated from the Cyanide Protocol § CPAP § Commercial Intraosseous introduction device § Portable suction equipment capable of adjusting from 80 -300 mm. Hg
National Scope of Practice • Defines and describes four levels of EMS certification/licensure nationally. • Outlines the skills set and knowledge base required to competently function in the EMS system • Foster greater mobility and reciprocity from state to state and other allied health disciplines
National Education Standards • 2009 Transition Program § Procedures above and beyond the current curriculum • National Education Standards § 2010 – 2012 § Name changes • • First Responder – Emergency Responder EMT Basic – EMT Intermediate – Advanced EMT Paramedic - Paramedic

Questions? Vicki Blanchard ALS Coordinator 223 -4215 vicki. blanchard@dos. nh. gov
e354bc0678b0441c2385a8dab1a229ef.ppt