64e876a040cce287066487a1bf2780f5.ppt
- Количество слайдов: 58
NEW CMS REIMBURSEMENT REVIEW ENTITIES – The Brave New World of MACs, RACs, PSCs and MICs 2009 AHCA/NCAL Convention ROLAND G. RAPP MARK E. REAGAN EVP, General Counsel, Chief Administrative Officer rrapp@skilledhealthcare. com Skilled Healthcare, LLC 27442 Portola Parkway, Suite 200 Foothill Ranch, California 92610 direct: 949 -282 -5822 fax: 949 -282 -5820 Partner mreagan@health-law. com HOOPER, LUNDY & BOOKMAN, INC. 575 Market Street, Suite 2300 San Francisco, CA 94105 Tel: 415 -875 -8501 Fax: 415 -985 -8519 1
Medicare Administrative Contractors n n The MMA (2003) mandated that a new MAC authority replace current Part A FIs and Part B carriers This Medicare contracting reform must be implemented by 2011 Prior -- 23 FIs and 17 carriers To be replaced by 19 MAC contractors n 15 Part. A/Part B MACs n 4 specialty MACs for DME 2

MAC Benefits (According to CMS) n n n n Serve as single point of contact for providers and suppliers for all claims related business Assist providers and suppliers with obtaining information on behalf of patients about items or services received from another provider or supplier that could affect claims payment Improved provider education and training Role for provider and suppliers in contractor evaluation via surveys Timeliness on claims processing and payment A more even distribution of claims processing Creation of a modernized administrate IT platform that incorporates the latest technological advances and standardization practices 3
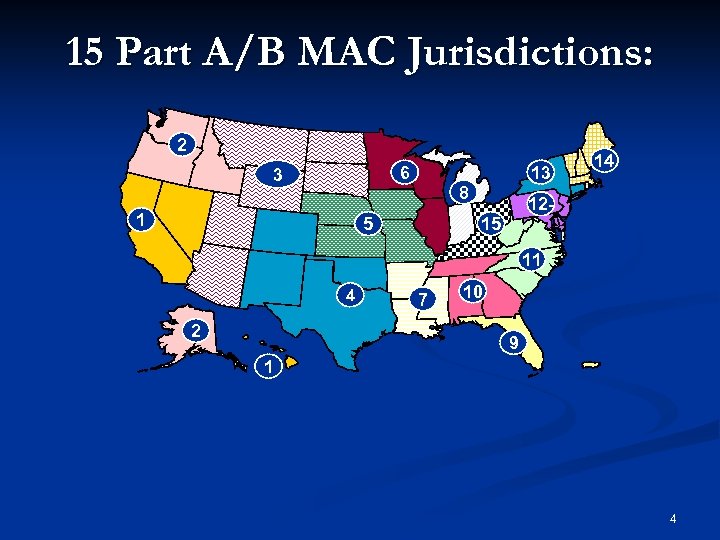
15 Part A/B MAC Jurisdictions: 2 6 3 1 13 8 5 14 12 - 15 11 4 2 7 10 9 1 4
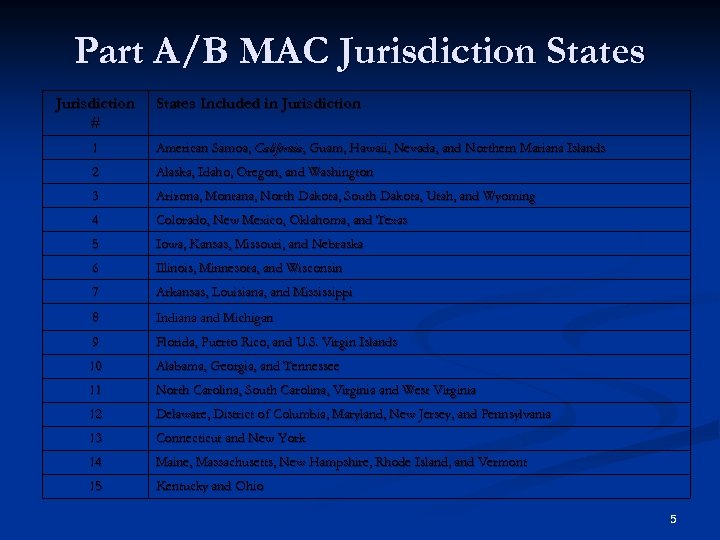
Part A/B MAC Jurisdiction States Jurisdiction # States Included in Jurisdiction 1 American Samoa, California, Guam, Hawaii, Nevada, and Northern Mariana Islands 2 Alaska, Idaho, Oregon, and Washington 3 Arizona, Montana, North Dakota, South Dakota, Utah, and Wyoming 4 Colorado, New Mexico, Oklahoma, and Texas 5 Iowa, Kansas, Missouri, and Nebraska 6 Illinois, Minnesota, and Wisconsin 7 Arkansas, Louisiana, and Mississippi 8 Indiana and Michigan 9 Florida, Puerto Rico, and U. S. Virgin Islands 10 Alabama, Georgia, and Tennessee 11 North Carolina, South Carolina, Virginia and West Virginia 12 Delaware, District of Columbia, Maryland, New Jersey, and Pennsylvania 13 Connecticut and New York 14 Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont 15 Kentucky and Ohio 5
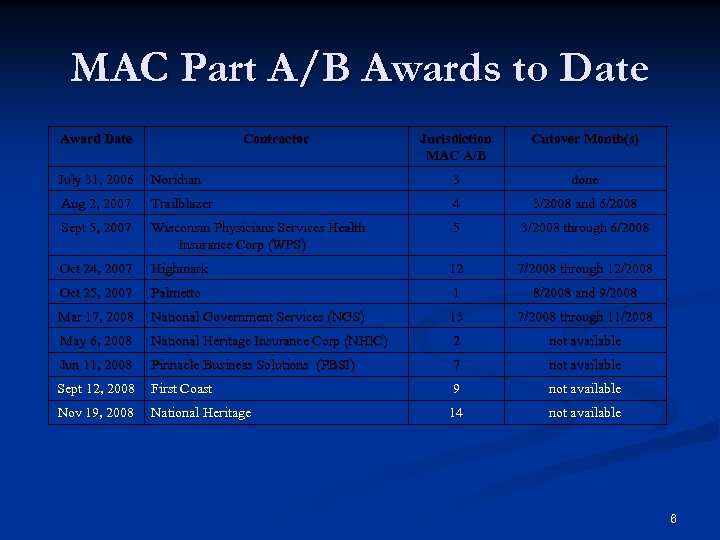
MAC Part A/B Awards to Date Award Date Contractor Jurisdiction MAC A/B Cutover Month(s) July 31, 2006 Noridian 3 done Aug 2, 2007 Trailblazer 4 3/2008 and 6/2008 Sept 5, 2007 Wisconsin Physicians Services Health Insurance Corp (WPS) 5 3/2008 through 6/2008 Oct 24, 2007 Highmark 12 7/2008 through 12/2008 Oct 25, 2007 Palmetto 1 8/2008 and 9/2008 Mar 17, 2008 National Government Services (NGS) 13 7/2008 through 11/2008 May 6, 2008 National Heritage Insurance Corp (NHIC) 2 not available Jun 11, 2008 Pinnacle Business Solutions (PBSI) 7 not available Sept 12, 2008 First Coast 9 not available Nov 19, 2008 National Heritage 14 not available 6
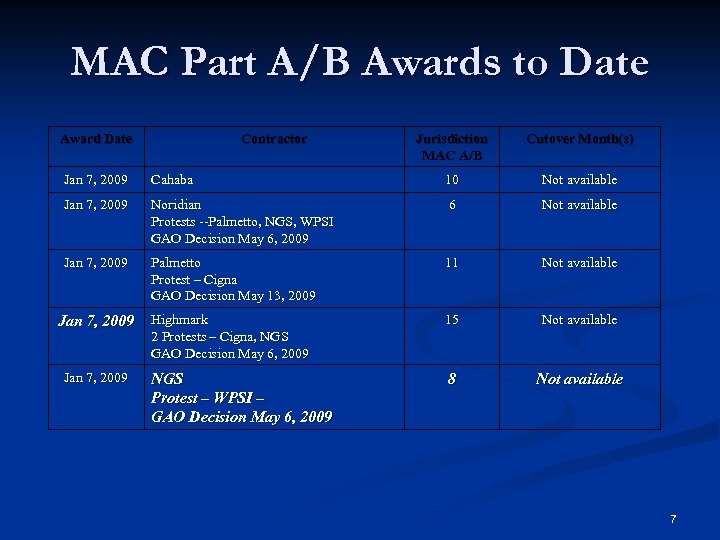
MAC Part A/B Awards to Date Award Date Contractor Jurisdiction MAC A/B Cutover Month(s) Jan 7, 2009 Cahaba 10 Not available Jan 7, 2009 Noridian Protests --Palmetto, NGS, WPSI GAO Decision May 6, 2009 6 Not available Jan 7, 2009 Palmetto Protest – Cigna GAO Decision May 13, 2009 11 Not available Jan 7, 2009 Highmark 2 Protests – Cigna, NGS GAO Decision May 6, 2009 15 Not available NGS Protest – WPSI – GAO Decision May 6, 2009 8 Not available Jan 7, 2009 7

DME MAC Awards Jurisdiction A – National Heritage Insurance Company n Jurisdiction B – Admini. Star Federal Inc. n Jurisdiction C – CIGNA n Jurisdiction D – Noridian n 8
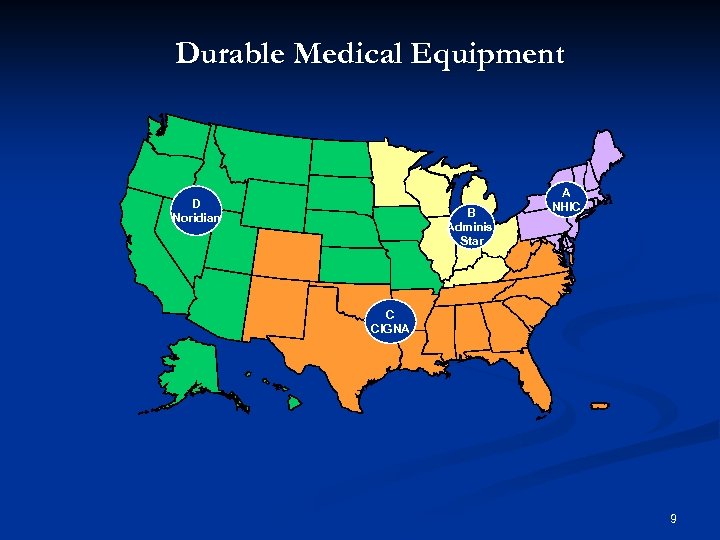
Durable Medical Equipment D Noridian B Adminis. Star A NHIC C CIGNA 9

Geographic Assignment Rule n n Provider’s State -- Providers who are not in a special category will be assigned to the MAC that covers the state where the provider is located. There are two exceptions: Exception 1 for QCP – Home Office State -- A qualified chain provider (QCP) may request that its members providers be served by a single A/B MAC – specifically, the A/B MAC that covers the state where the QCP’s home office is located. QCP is defined as: (42 CFR 421. 404(b)(2) n n Ten or more hospitals, SNFs, and/or critical access hospitals, under common ownership or control, collectively totaling 500 or more certified beds; or Five or more hospitals, SNFs, and/or critical access hospitals, under common ownership or control in three or more contiguous states, collectively totaling 300 or more certified beds CMS may assign non-QCP providers, as well as ESRD providers to an A/B MAC outside of the prevailing geographic assignment rule only to support the implementation of MACs or to serve some other compelling interest of the Medicare program Exception 2 for Provider-based Entities -- – Provider-based entities (e. g. , hospital-based SNF) will be assigned to the MAC that covers the state where the main “parent” provider is assigned. 10

Local Coverage Determinations n As is current practice, MACs will be required to develop LCDs in accordance with chapter 13 of the Program Integrity Manual. n As the MACs commence operations in their jurisdictions, each MAC will consolidate all the LCDs for its jurisdiction by selecting the least restrictive LCD from the existing LCDs on the topic. n National coverage decisions will continue to be issued by CMS. 11
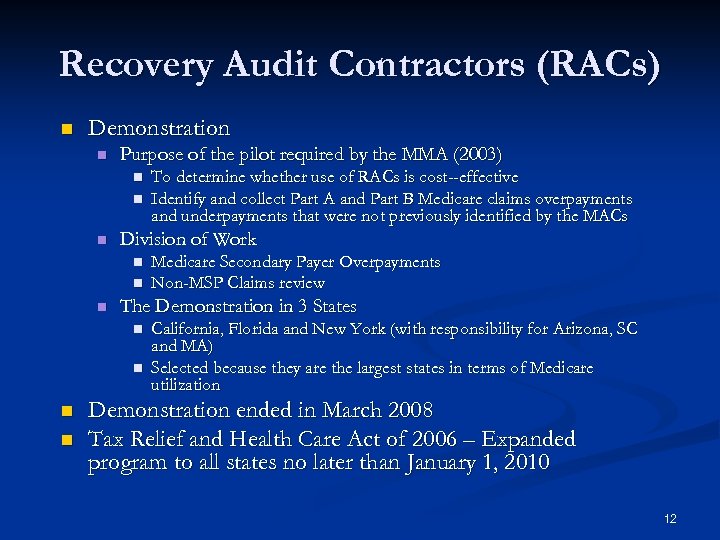
Recovery Audit Contractors (RACs) n Demonstration n Purpose of the pilot required by the MMA (2003) n n n Division of Work n n n Medicare Secondary Payer Overpayments Non-MSP Claims review The Demonstration in 3 States n n To determine whether use of RACs is cost--effective Identify and collect Part A and Part B Medicare claims overpayments and underpayments that were not previously identified by the MACs California, Florida and New York (with responsibility for Arizona, SC and MA) Selected because they are the largest states in terms of Medicare utilization Demonstration ended in March 2008 Tax Relief and Health Care Act of 2006 – Expanded program to all states no later than January 1, 2010 12
Payment to RACs n RAC paid on contingency basis – Starting March 1, 2006, RACs received an equivalent percentage for all underpayment and overpayment identifications 13

Problems Many problems in the California Demonstration n AHCA and California affiliate went to CMS and the Hill n Changes made for the permanent program n 14
CMS Improvements to the RAC Permanent Program n n n Coding experts Physician reviewers RAC physician medical director Credentials of reviewers provided on request Limits on # of medical records requested – CMS to establish limits All new issues a RAC wishes to pursue for overpayments validated by CMS or an independent RAC Validation Contractor Contingency fees to be paid back by RACs when an improper payment determination is overturned at any level of appeal Changing from a 4 -year look-back period to a 3 -year look-back period Maximum look-back date of October 1, 2007 Web-based application that will allow providers to look up the status of medical record reviews Reason for review listed on request for records letters and overpayment letters Public disclosure of RAC contingency fees 15
16
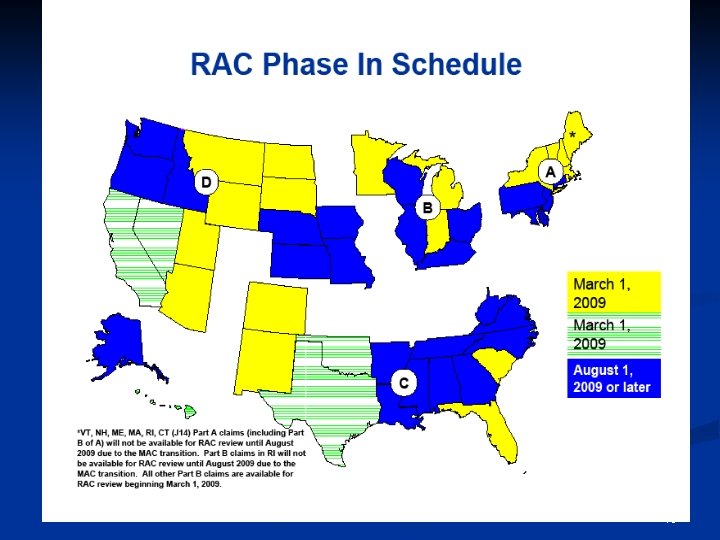
RAC Timetable The RACs have already started recovery audits in Summer/Fall of 2009 n Likely to be only “automated reviews” at first and “complex reviews” likely not to start until late Fall 2009/early 2010 n “Medical necessity” complex reviews likely to begin early 2010 n 17
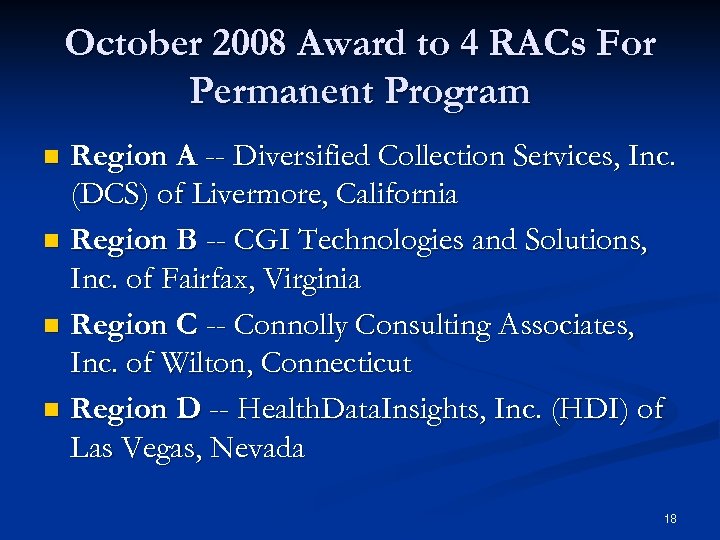
October 2008 Award to 4 RACs For Permanent Program Region A -- Diversified Collection Services, Inc. (DCS) of Livermore, California n Region B -- CGI Technologies and Solutions, Inc. of Fairfax, Virginia n Region C -- Connolly Consulting Associates, Inc. of Wilton, Connecticut n Region D -- Health. Data. Insights, Inc. (HDI) of Las Vegas, Nevada n 18

Contract Protests and Resolution on February 6, 2009 PRG-Schultz, Inc. will serve as subcontractor to HDI, DCS, and CGI in Regions A, B and D (will only be doing home health claims in California) n Viant Payment System, Inc will serve as subcontractor to Connolly Consulting in Region C n 19

RAC Review Process n n RACs review claims on a post payment basis RACs use the same Medicare policies as FIs, Carriers and MACs n n Two types of review: n n n Automated (no medical record needed) Complex (medical record required) RACs will NOT be able to review claims paid prior to October 1, 2007 n n NCDs, LCDs & CMS manuals RACs will be able to look back three years from the date the claim was paid RACs are required to employ a staff consisting of nurses, therapists, certified coders & a physician CMD 20
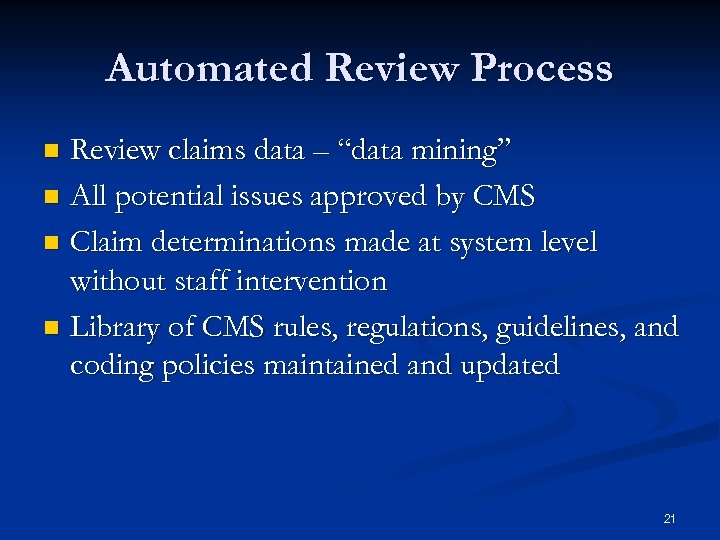
Automated Review Process Review claims data – “data mining” n All potential issues approved by CMS n Claim determinations made at system level without staff intervention n Library of CMS rules, regulations, guidelines, and coding policies maintained and updated n 21
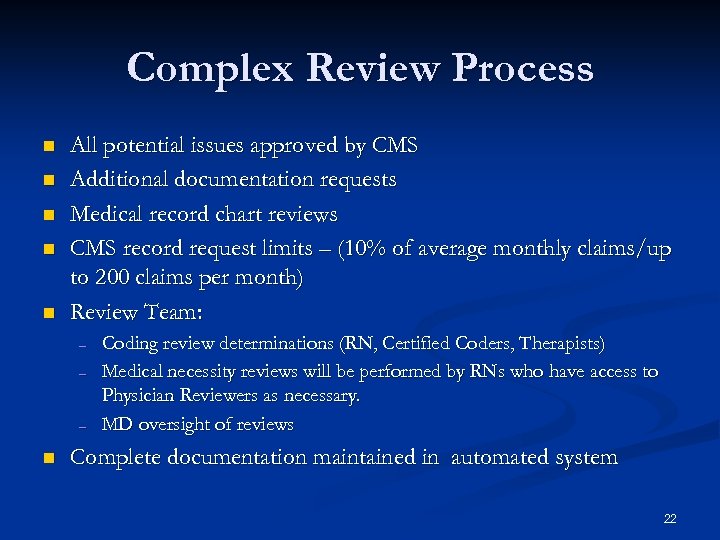
Complex Review Process n n n All potential issues approved by CMS Additional documentation requests Medical record chart reviews CMS record request limits – (10% of average monthly claims/up to 200 claims per month) Review Team: – – – n Coding review determinations (RN, Certified Coders, Therapists) Medical necessity reviews will be performed by RNs who have access to Physician Reviewers as necessary. MD oversight of reviews Complete documentation maintained in automated system 22

Appeal Issues n Strategic Appeal Issues - Redetermination 30 days to stop recoupment n 120 days to request redetermination n 11. 375% interest accrues from date of determination n Cash flow – can extend repayment for 90 days from the date of determination (includes 60 days for redetermination decisions to be issued) n Impact of “rebuttal period” - up to 30 days n 23
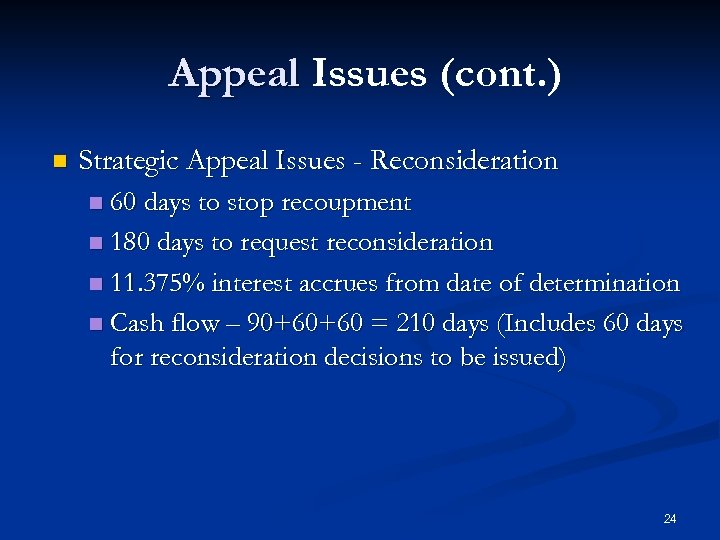
Appeal Issues (cont. ) n Strategic Appeal Issues - Reconsideration 60 days to stop recoupment n 180 days to request reconsideration n 11. 375% interest accrues from date of determination n Cash flow – 90+60+60 = 210 days (Includes 60 days for reconsideration decisions to be issued) n 24
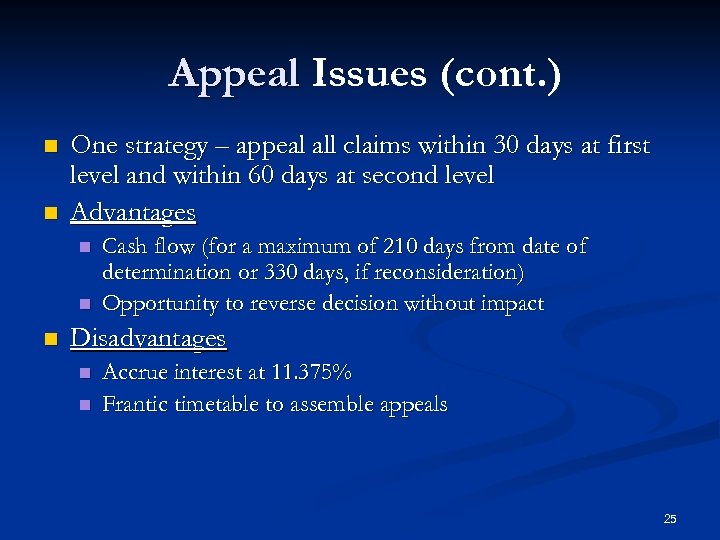
Appeal Issues (cont. ) n n One strategy – appeal all claims within 30 days at first level and within 60 days at second level Advantages n n n Cash flow (for a maximum of 210 days from date of determination or 330 days, if reconsideration) Opportunity to reverse decision without impact Disadvantages n n Accrue interest at 11. 375% Frantic timetable to assemble appeals 25
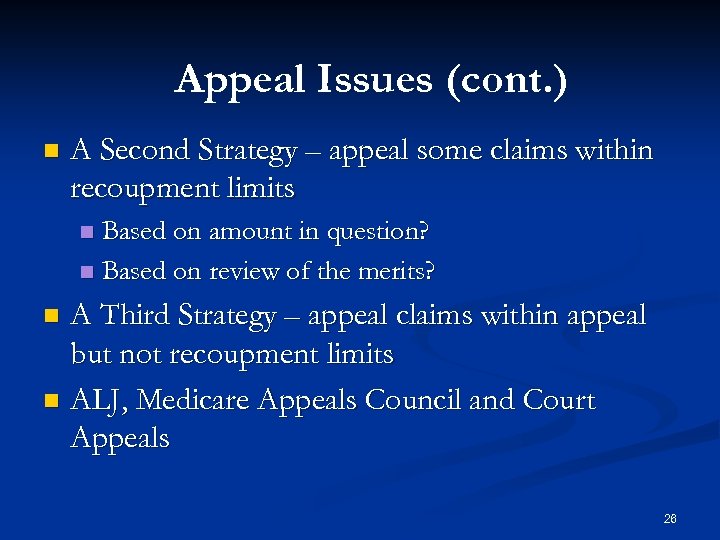
Appeal Issues (cont. ) n A Second Strategy – appeal some claims within recoupment limits Based on amount in question? n Based on review of the merits? n A Third Strategy – appeal claims within appeal but not recoupment limits n ALJ, Medicare Appeals Council and Court Appeals n 26
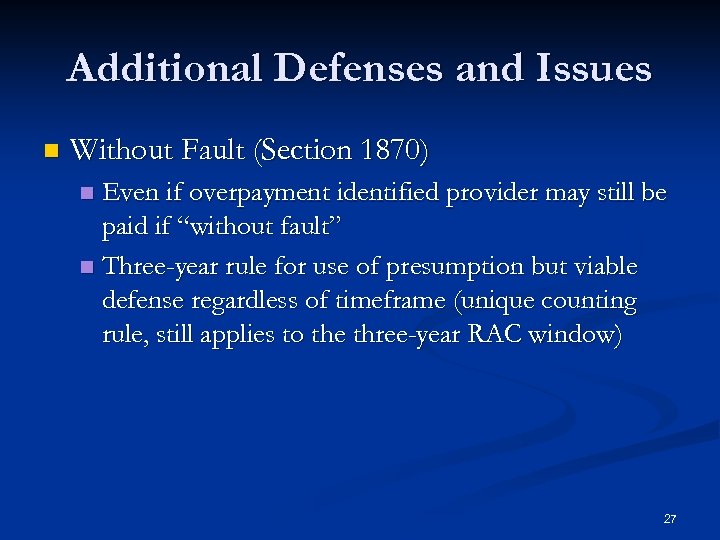
Additional Defenses and Issues n Without Fault (Section 1870) Even if overpayment identified provider may still be paid if “without fault” n Three-year rule for use of presumption but viable defense regardless of timeframe (unique counting rule, still applies to the three-year RAC window) n 27
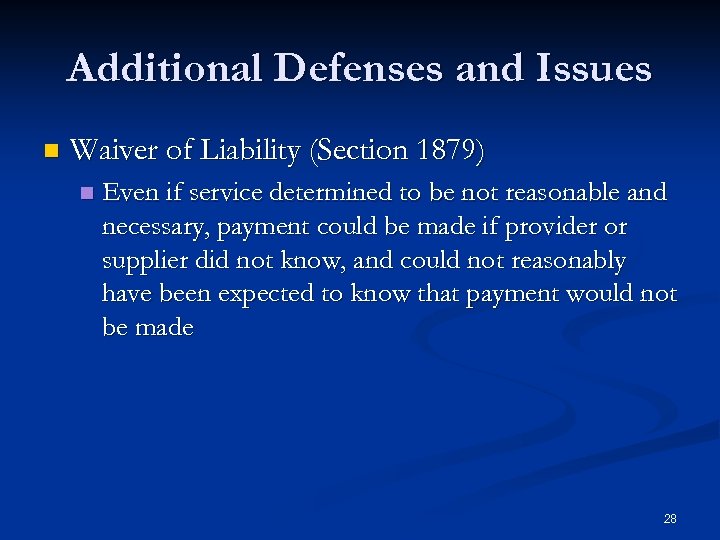
Additional Defenses and Issues n Waiver of Liability (Section 1879) n Even if service determined to be not reasonable and necessary, payment could be made if provider or supplier did not know, and could not reasonably have been expected to know that payment would not be made 28
Additional Defenses and Issues n Timing of Reopening “Good Cause” 42 C. F. R. 405. 980 Medicare Appeals Council Decisions involving hospitals and skilled nursing facilities n Decisions by Appeals Council and the ALJ lack jurisdiction to decide contested reopenings under the Medicare appeals process n Impact of raising “good cause” n 29
Additional Defenses and Issues n Timing of Reopening/”Good Cause” n n n MAC Decision Palomar Medical Center v. Johnson, S. D. Cal. No. 3: 09 -cv-00605 -BEN-NLS (S. D. Cal. Complaint filed 3/24/09) Challenges RAC reopening of two year old hospital claim ALJ determined RAC had not shown “good cause” for reopening MAC reversed ALJ finding ALJ lacked jurisdiction to determine whether reopening was lawful Court challenge to jurisdictional argument and due process CMS Transmittal 1671 (February 16, 2009) – RAC data analysis is “good cause” and ALJ has no jurisdiction 30
Additional Defenses and Issues n Credentials of reviewer Can request a copy of credentials n Medical Director n Coding Experts n 31
Additional Defenses and Issues n Review criteria used n n n Must be Medicare policy, National Coverage Determinations, Local Coverage Determinations What was in effect at time Is Medicare policy applied correctly Can any of the coverage determinations be used as a defense? Incorrect application of statutes n n Medical records standards Physician testimony/declaration Standard of care evidence Peer-reviewed science 32
Additional Defenses and Issues n Sampling Extrapolation PIM (CMS Pub 100 -08) Chapter 3 n 3. 10. 1 -3. 10. 11. 2 n Challenge statistical analysis n 33
Provider Preparation n n n Know where previous improper payments have been found (OIG, CERT, Demo RAC Reports) New issues are posted to the web – CMS appeal process RAC claim status web interface (2010) Detailed review results letter and denial letter following all complex reviews – “discussion period” opportunity/does not impact appeal deadlines Prepare to respond to RAC medical record requests – 45 day window Keep/submit proper documentation – point of contact/team building/organizational issues resolved Appeal when necessary - know timelines for appeal AND timelines to stop recoupment (e. g. , 120 days v. 30 days for first level appeal and 180 days v. 60 days for second level appeal) 34
Program Safeguard Contractors n n n n Like RACs, PSCs are part of the Medicare Integrity Program Not contingency fee contractors Function like RACs in the area of “complex review” Requirements for Medical Records – 45 -day window Ability to cause recoupments (like RACs) Organize like RAC activities Activities have focused on Part A and Part B (MDS and therapy) 35
Medicare Integrity Program (“MIP”) n n n Created by Deficit Reduction Act (“DRA”) in 2005 Establishes the federal government’s role in combating Medicaid fraud, waste and abuse Effective support and assistance to States Formation of Medicaid Integrity Group (“MIG”) Creation of Medicaid Integrity Contractors (“MICs”) Goal of the MICs: n Identifying and recovering overpayments 36

The World of Medicaid Integrity Contractors (“MICs”) n Review MICs - data analysis n Audit MICs – post-payment audits n Educate MICs – educate providers 37
MIC Audit Process n ID of potential audits through data analysis by review MICs n Vetting potential audits with State and law enforcement n Audit MIC receive assignment n Contact with provider and scheduling of the entrance conference n Currently in 20 states – Florida, South Carolina, Pennsylvania, Delaware, Georgia, Alabama, North Carolina, District of Columbia, Virginia, Kentucky, Maryland, Texas, Arkansas, Louisiana, New Mexico, Colorado, Oklahoma, California, Nevada, Idaho 38
Timing of Audits Should be at least two weeks notice before audit to begin n Records request/preparation time (all over the place - 10 to 45 days) n Desk or field audit n Entrance conference (phone or in-person) n 39
Look-Back Period Not set by MIG n Relates to maximum period under state law n Not always clear under state law n Need to know/analyze state law n 40
Audit Process (cont. ) Intake questionnaire (work in process) n Entrance conference n Audit n Review of preliminary audit findings and tentative conclusions n Opportunity for provider to comment and provide additional information n 41
Audit Process (cont. ) Draft audit report to CMS and State for review and comments along with provider n If revised, further review with State n Draft audit report finalized n CMS issues final report to State n State has 60 days to repay federal government for its share n 42
Audit Process (cont. ) State issues final report to provider and begins overpayment recovery process n Provider rights of appeal are those available under State law n Settlement made complicated by feds recoupment from states n If provider wins, what happens to state loss? n 43
Relevant Issues n n n Standards applied – known? Audit according to General Accepted Government Auditing Standards (“GAGAS”) Adequate time to produce all records Ability to stay recoupment Payment plan available? Timely Appeal Process/Overburdened State Appeal Process/Due Process 44
MIC PROGRAM No Record Request Limitations n n No Limits on the Number of Medical Records a MIC can Request per Month Unlike RAC program Basic problem with MIP/MICs – no formal structure to program Compare and contrast to RAC 45
MIC Application of Standards Uncertain n Push MIC to identify substantive standards utilized n 46
Identified Audit Process Issues Requests for information outside of the scope of the audit (intake questionnaire) n Short timeframe n Looking back up to 5 years n Duplicative of other audits n Federal/State conflicts n 47
Areas of Focus in LTC Accuracy of patient responsibility/share of cost n Deceased patients n Duplicative payment issues/impact of retro Medicaid rate changes can make it look like duplicate claims n Bed-hold rate limitations n 48
Prepare for RACs/MICs n n n Establish internal team Interdisciplinary Team: Legal, Finance, Clinical, Compliance, IT Identify point of contact for internal and external communications Develop central tracking mechanisms/database for all Incoming and Outgoing Coordinate the tracking mechanism with communications structure – record reviews, and appeal of recoupment deadlines 49
Prepare for RACs/MICs (cont. ) Conduct self audits to identify potential problems n Participate in trainings and outreach n. Monitor news sources, CMS, associations, and your own reports to stay abreast of trends n If desired, development of unique forms for appeal levels once issues identified n 50
Responding to Record Requests: n Stamp date and Time Received Push for 45 calendar days from date of letter for MICs (already established for RACs) n Can request an extension n Notify if significant discrepancy between date of letter and date of receipt n Identify any internal issues in expeditiously getting the mail for processing n 51
Responding to Record Requests: n Was the request sent to the right place? n n Notify Contractor of the contact person with contact information Did the Contractor exceed a reasonable number of record requests under the circumstances? 52
Responding to Record Requests: n Copying of Record and Others Ensure entire record is copied n Include copies of substantive coverage materials n n Review of all records before they are released Permits early identification of issues n Establishes priority for appeals n Intensive work n 53
Responding to Record Requests: Has the claim already been subject to audit by another contractor n Who is this request from? n n Confusion with so many different contractors 54
Responding to Record Requests: n Document Management? Stamp number (Bates Stamp) on bottom of each page produced n Scan everything produced n Include cover letter itemizing contents of box of documents or CD n Send certified mail or, if regular mail, complete affidavit of service by mail n 55
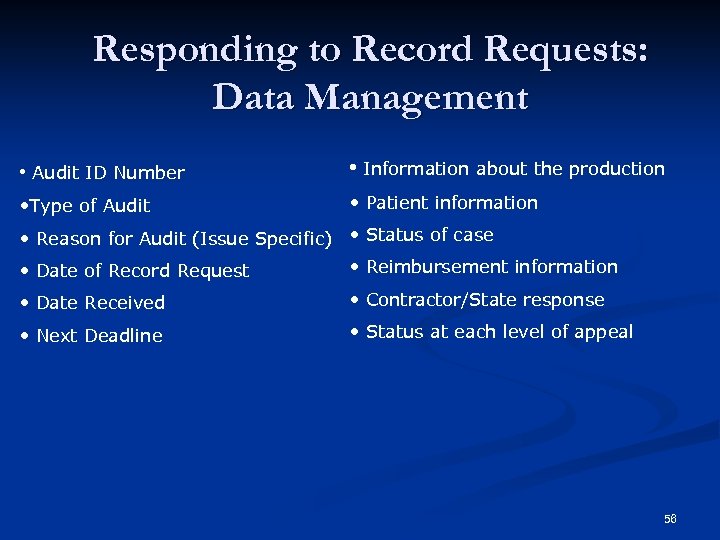
Responding to Record Requests: Data Management • Audit ID Number • Information about the production • Type of Audit • Patient information • Reason for Audit (Issue Specific) • Status of case • Date of Record Request • Reimbursement information • Date Received • Contractor/State response • Next Deadline • Status at each level of appeal 56
Determinations n Stamp the date received n Determine Appeal period 57
Additional Defenses and Issues n n Review criteria used n What was it and is it subject to attack? n What was in effect at time? n Is Medicaid policy applied correctly? Incorrect application n Medical records standards n Physician testimony/declaration n Standard of care evidence n Peer-reviewed science 58
64e876a040cce287066487a1bf2780f5.ppt