dbaad45cf0181096c38b4030e4f6776e.ppt
- Количество слайдов: 44
Neurosurgical Emergencies Craig Goldberg, MD Chief, Division of Neurosurgery Bassett Healthcare
Overview • Defining “rural” • Evidence-based guidelines for TBI treatment • Brain surgery for the general surgeon • Head CT basics • A few words on spine (if there is time)
Defining Rural China Utah Las Vegas Chicago Jersey March 29, 1976 by Saul Steinberg
Defining Rural “I know it when I see it. ” Potter Stewart, Associate Justice of the United States Supreme Court Wikipedia. com
Defining Rural The author has no financial arrangements with this souvenir stand to report
Guidelines for the Management of Severe Traumatic Brain Injury May 2007 Journal of Neurotrauma www. braintrauma. org • With supplementation from additional literature
Why focus on this study?
Airway, Breathing, and Circulation
Hyperventilation • Level II - prophylactic hyperventilation NOT recommended • IS recommended as a temporizing measure for the reduction of high ICP, but should be avoided in the first 24 hours after injury and should have Sj. O 2 or Pbr. O 2 monitors
BP and O 2
CPP Thresholds • Level II: > 70 mm. Hg can lead to CHF, ARDS • Level III: 50 -70 mm. Hg is target
Infection Prophylaxis • Level II: – Antibiotics for intubation – Early tracheostomy and extubation • Level III: – Early extubation – Abx and ventriculostomy rotation NOT recommended
Hyperosmolar therapy
DVT Prophylaxis • Level III: – use SCDs – use SQ heparin but • no data on dose or timing • does increase hematoma

Additional Treatments
Steroids • Level I: In patients with moderate or severe traumatic brain injury (TBI), high-dose methylprednisolone is associated with increased mortality and is CONTRAINDICATED • This is the ONLY standard in these recommendations.
Seizure Prophylaxis • Level II: – For EARLY (first week) seizure prevention – Not good for late
Hypothermia “only given to patients in a randomised (sic) controlled trial” Cochrane Library Vol(1) 2009
Nutrition • Level II: – Full caloric intake by day 7 “Patients who were not fed within 5 and 7 days after TBI had a 2 - and 4 -fold increased likelihood of death, respectively. ” Journal of Neurosurgery Jul 2008, Vol. 109, No. 1, Pages 50 -56: 50 -56.
Chemical Coma • Level II - prophylactic barbiturates NOT recommended • but barbiturates ARE recommended to control refractory ICP • Propofol can control ICP but has not shown improvement in mortatlity or 6 month outcome
Indications for ICP monitoring • Level II: Salvageable with GCS 3 -8 and abnormal CT (start to treat @ ICP 20) • Level III: normal CT with GCS 3 -8 and 2 of the following – age >40 – SBP < 90 – posturing – (start to treat clinically)
Not a first choice • The issue of non-neurosurgeons doing emergency craniotomies and burr holes was brought up. The consensus of the Committee is that neurosurgeons themselves should be the ones doing these operations. We do all acknowledge, however, that there are extreme circumstances in rural America where general surgeons that are properly trained might be able to perform a lifesaving cranial procedure when other alternatives are not available. The Committee, therefore, is not totally opposed to such a concept. • From Council of State Neurosurgical Societies Neurotrauma Committee Meeting, April 25, 2003
Intracranial Pressure Monitoring • Devices – Ventriculostomy • • • Still “gold standard” Ventricles sometimes hard to cannulate Can get obstructed with debris Costs less Can be recalibrated – Fiber optic monitors • • Diagnostic, not therapeutic Readings can drift Doesn’t go through the brain Easier to insert
Anatomy • The skull is approx 1 cm thick • The ventricles are approx 6 cm deep to the outer surface of the skull
Anatomy • The most common entry point is – 10 -12 cm back from the glabella – Then lateral approx 2 -3 cm to the mid-pupillary line • The most common target point is – The foramen of Monro (connects the lateral ventricle to the third ventricle which is past the choroid plexus)
Procedure • Often done at bedside in ER or ICU – (rarely on floor, in emergency, then immediate transfer to ICU likely) • Patient supine, head elevated to 30 degrees or more • Analgesia, sedation, paralysis (if intubated) • Right side of head shaved
Procedure • Cranial access kit, ventriculostomy tube and drainage bag opened • Local anesthetic instilled • Small linear (A-P) incision made • Self-retaining retractor inserted • Burr hole drilled • Bone dust cleared
Procedure • • • Dura punctured Tube inserted to approx 6 cm depth CSF pressure measured, specimen collected Tube tunneled postero-laterally Tube secured, wound closed Tube attached to drainage bag and set to desired level (usually 10 cm above pts ear)
CSF Dynamics • When tube attached to transducer – Triphasic waveform, with second wave corresponding to dicrotic notch on a-line – Please do NOT use heparin • Normal ICP 5 -15 mm. Hg = 7 -20 cm H 2 O • Autoregulatory range (Monro-Kelly doctrine) • Small changes in volume lead to little or no changes in pressure
CSF Dynamics • Normal CSF volume: – 50 cc in ventricles, 150 cc total • CSF volume is replenished 3 times per day (approx 400 -500 cc per day) • Typical drainage volumes are 5 -20 cc/hr • There will usually be an initial highpressure gush. ICP can be measured
Transport • Clamp off (no drainage) for transport – Bed to stretcher to ambulance to other hospital if patient can tolerate – Trying to avoid overdrainage – Do NOT leave open and below head – May need to be opened, either intermittently or continuously for lengthy transport – Pressure changes with air travel further complicate the issue
Head CT Basics
Classification • Morphology – Intracranial lesions • Focal – Epidural hematomas – Subdural hematomas – Intracerebral hematomas • Diffuse – Concussion - usually non-structural – Diffuse axonal injury (DAI)
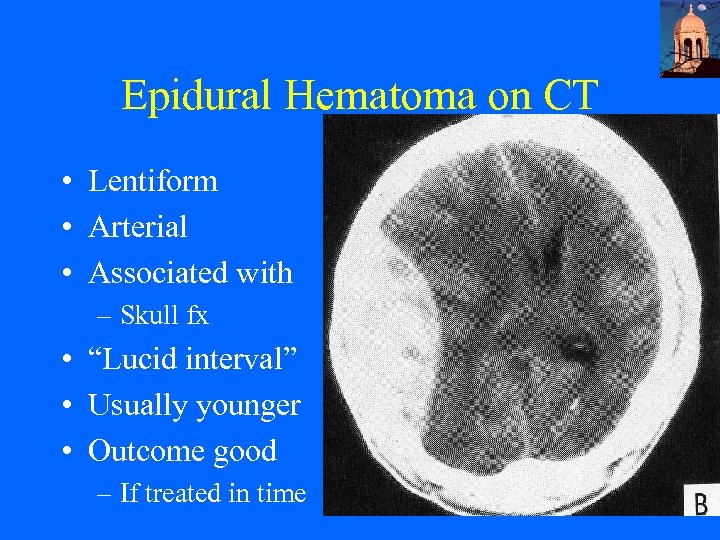
Epidural Hematoma on CT • Lentiform • Arterial • Associated with – Skull fx • “Lucid interval” • Usually younger • Outcome good – If treated in time
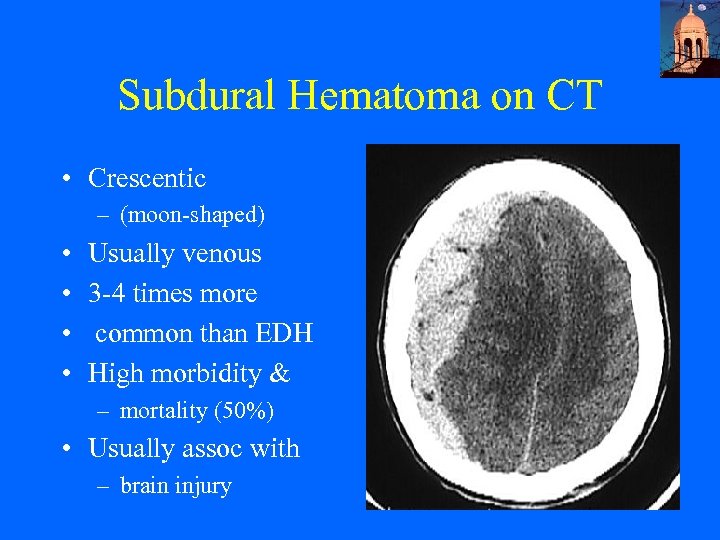
Subdural Hematoma on CT • Crescentic – (moon-shaped) • • Usually venous 3 -4 times more common than EDH High morbidity & – mortality (50%) • Usually assoc with – brain injury
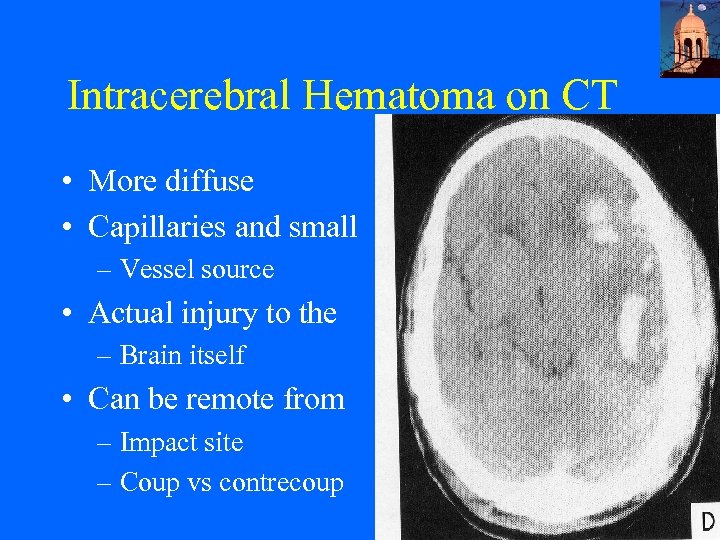
Intracerebral Hematoma on CT • More diffuse • Capillaries and small – Vessel source • Actual injury to the – Brain itself • Can be remote from – Impact site – Coup vs contrecoup
Craniotomy 101 • Verify the correct side on imaging – if no imaging, go with the side of the blown pupil – if both pupils are blown, go with the side that blew first – if you don’t know, go in on the left first
Spine
Spine • Steroids • Treatment with methylprednisolone for either 24 or 48 hours is recommended as an option in the treatment of patients with acute spinal cord injuries that should be undertaken only with the knowledge that the evidence suggesting harmful side effects is more consistent than any suggestion of clinical benefit. • Neurosurgery supplement to March 2002, Vol 50#3, p. S 63
Spine • Solumedrol protocol – bolus 30 mg/kg IV over 15 min – 45 min pause – 5. 4 mg/kg/hr X 23 hrs if < 3 hrs from injury – X 47 hrs if < 8 hrs from injury
Spine • Hypothermia – unproven and experimental
Conclusions • Rural is rural • Don’t treat TBI with steroids • Do keep the patient oxygenating and perfusing • Many treatments to try with suspected or documented high ICP
Conclusions • Steroids in spine are an option, hypothermia has no proven benefit (yet? ) • If there is a possibility that you might find yourself doing brain surgery, this lecture is not enough
Questions?
dbaad45cf0181096c38b4030e4f6776e.ppt