2107428fe7b289f91e56b0c35d2a31b4.ppt
- Количество слайдов: 99
 Neuromuscular diseases leading to respiratory failure Jiann-Horng Yeh, M. D. Department of Neurology Shin Kong WHS Memorial Hospital
Neuromuscular diseases leading to respiratory failure Jiann-Horng Yeh, M. D. Department of Neurology Shin Kong WHS Memorial Hospital
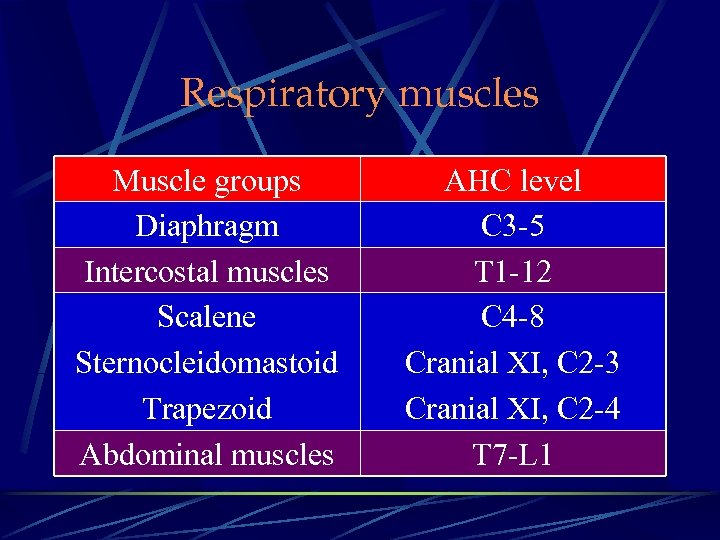 Respiratory muscles Muscle groups Diaphragm Intercostal muscles Scalene Sternocleidomastoid Trapezoid Abdominal muscles AHC level C 3 -5 T 1 -12 C 4 -8 Cranial XI, C 2 -3 Cranial XI, C 2 -4 T 7 -L 1
Respiratory muscles Muscle groups Diaphragm Intercostal muscles Scalene Sternocleidomastoid Trapezoid Abdominal muscles AHC level C 3 -5 T 1 -12 C 4 -8 Cranial XI, C 2 -3 Cranial XI, C 2 -4 T 7 -L 1
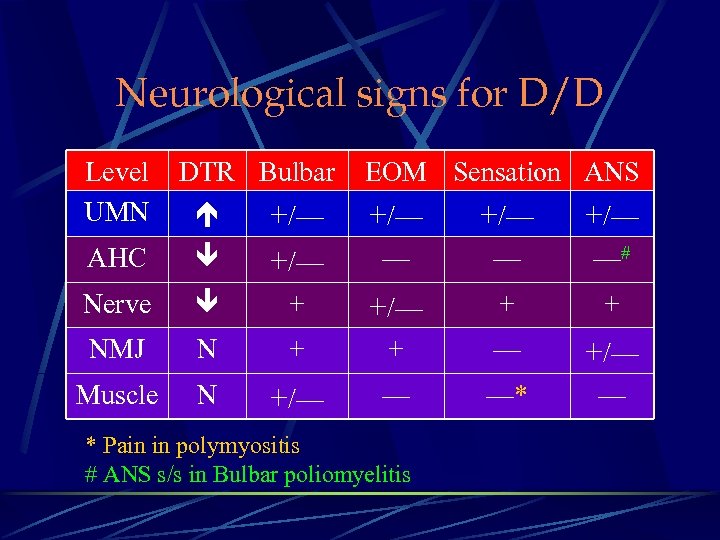 Neurological signs for D/D Level UMN AHC DTR Bulbar +/— EOM Sensation ANS +/— +/— — — —# Nerve + +/— + + NMJ N + + — +/— Muscle N +/— — —* — * Pain in polymyositis # ANS s/s in Bulbar poliomyelitis
Neurological signs for D/D Level UMN AHC DTR Bulbar +/— EOM Sensation ANS +/— +/— — — —# Nerve + +/— + + NMJ N + + — +/— Muscle N +/— — —* — * Pain in polymyositis # ANS s/s in Bulbar poliomyelitis
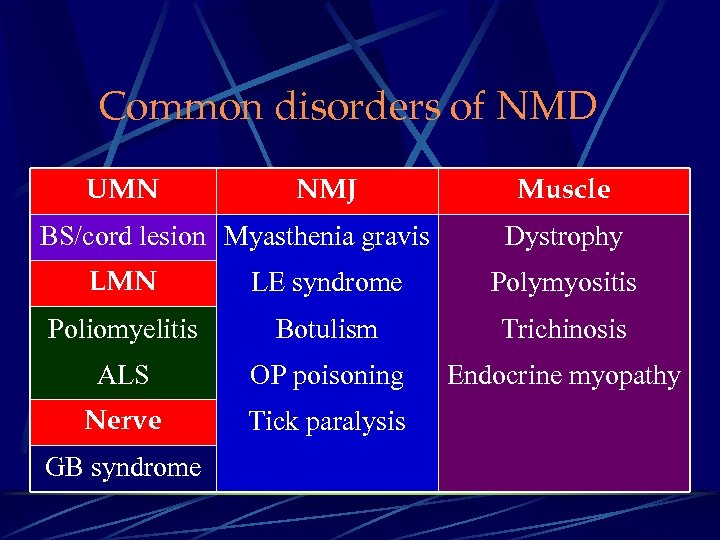 Common disorders of NMD UMN NMJ BS/cord lesion Myasthenia gravis Muscle Dystrophy LMN LE syndrome Polymyositis Poliomyelitis Botulism Trichinosis ALS OP poisoning Endocrine myopathy Nerve Tick paralysis GB syndrome
Common disorders of NMD UMN NMJ BS/cord lesion Myasthenia gravis Muscle Dystrophy LMN LE syndrome Polymyositis Poliomyelitis Botulism Trichinosis ALS OP poisoning Endocrine myopathy Nerve Tick paralysis GB syndrome
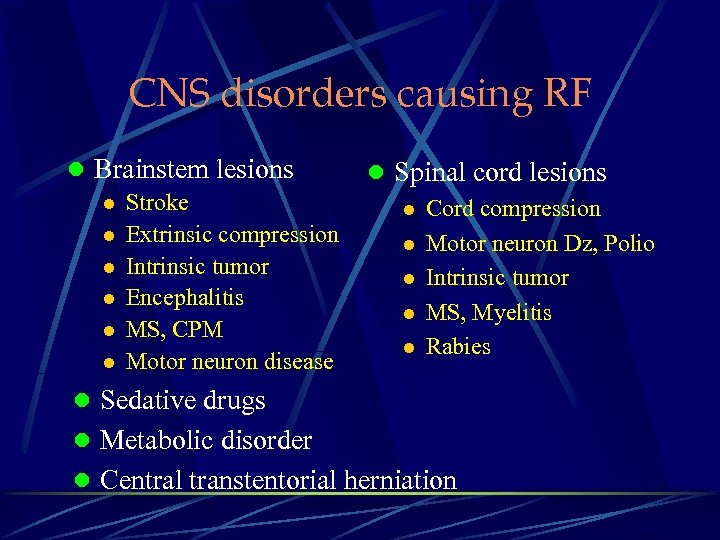 CNS disorders causing RF l Brainstem lesions l Stroke l Extrinsic compression l Intrinsic tumor l Encephalitis l MS, CPM l Motor neuron disease l Spinal cord lesions l Cord compression l Motor neuron Dz, Polio l Intrinsic tumor l MS, Myelitis l Rabies l Sedative drugs l Metabolic disorder l Central transtentorial herniation
CNS disorders causing RF l Brainstem lesions l Stroke l Extrinsic compression l Intrinsic tumor l Encephalitis l MS, CPM l Motor neuron disease l Spinal cord lesions l Cord compression l Motor neuron Dz, Polio l Intrinsic tumor l MS, Myelitis l Rabies l Sedative drugs l Metabolic disorder l Central transtentorial herniation
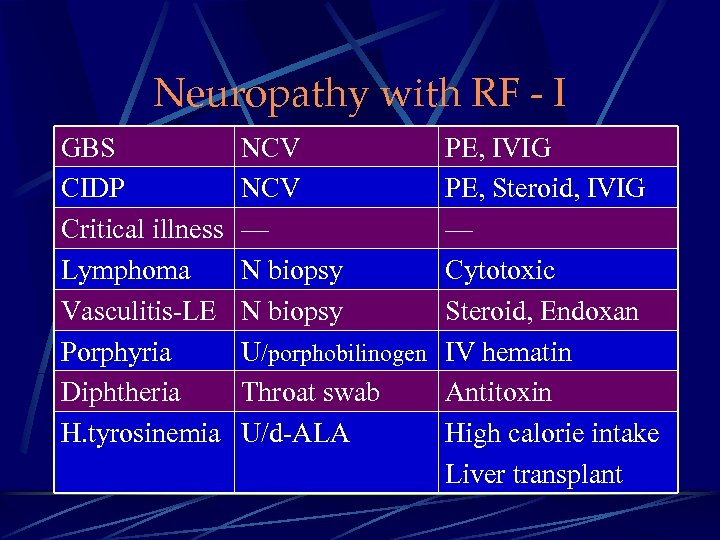 Neuropathy with RF - I GBS CIDP Critical illness Lymphoma Vasculitis-LE Porphyria Diphtheria H. tyrosinemia NCV — N biopsy U/porphobilinogen Throat swab U/d-ALA PE, IVIG PE, Steroid, IVIG — Cytotoxic Steroid, Endoxan IV hematin Antitoxin High calorie intake Liver transplant
Neuropathy with RF - I GBS CIDP Critical illness Lymphoma Vasculitis-LE Porphyria Diphtheria H. tyrosinemia NCV — N biopsy U/porphobilinogen Throat swab U/d-ALA PE, IVIG PE, Steroid, IVIG — Cytotoxic Steroid, Endoxan IV hematin Antitoxin High calorie intake Liver transplant
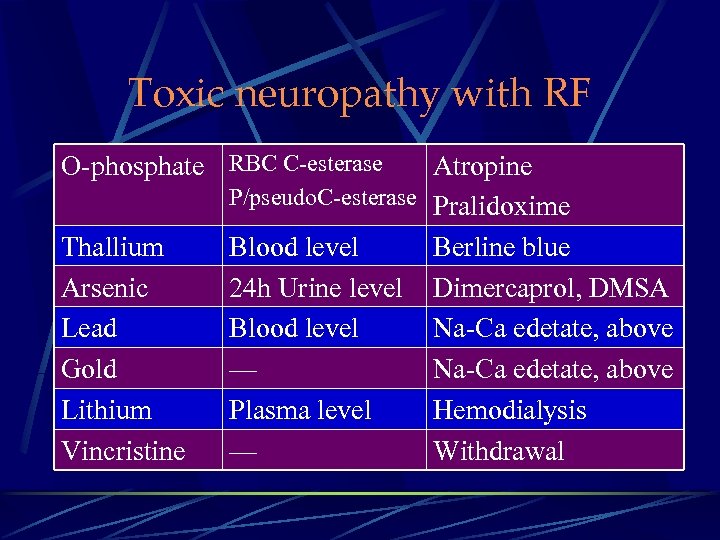 Toxic neuropathy with RF O-phosphate RBC C-esterase Thallium Arsenic Lead Gold Lithium Vincristine Atropine P/pseudo. C-esterase Pralidoxime Blood level Berline blue 24 h Urine level Dimercaprol, DMSA Blood level Na-Ca edetate, above — Na-Ca edetate, above Plasma level Hemodialysis — Withdrawal
Toxic neuropathy with RF O-phosphate RBC C-esterase Thallium Arsenic Lead Gold Lithium Vincristine Atropine P/pseudo. C-esterase Pralidoxime Blood level Berline blue 24 h Urine level Dimercaprol, DMSA Blood level Na-Ca edetate, above — Na-Ca edetate, above Plasma level Hemodialysis — Withdrawal
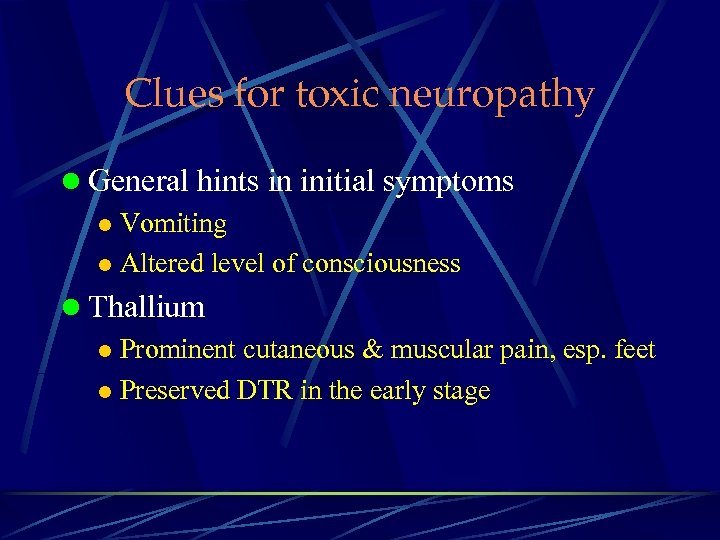 Clues for toxic neuropathy l General hints in initial symptoms l Vomiting l Altered level of consciousness l Thallium l Prominent cutaneous & muscular pain, esp. feet l Preserved DTR in the early stage
Clues for toxic neuropathy l General hints in initial symptoms l Vomiting l Altered level of consciousness l Thallium l Prominent cutaneous & muscular pain, esp. feet l Preserved DTR in the early stage
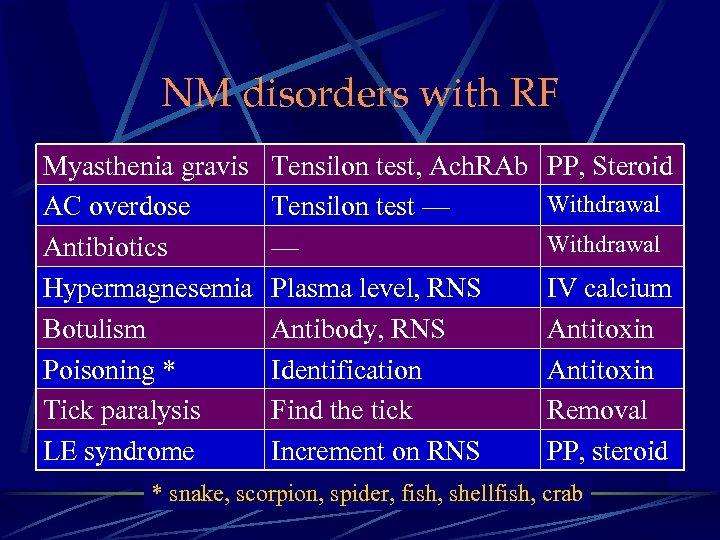 NM disorders with RF Myasthenia gravis AC overdose Antibiotics Hypermagnesemia Botulism Poisoning * Tick paralysis LE syndrome Tensilon test, Ach. RAb Tensilon test — — Plasma level, RNS Antibody, RNS Identification Find the tick Increment on RNS PP, Steroid Withdrawal IV calcium Antitoxin Removal PP, steroid * snake, scorpion, spider, fish, shellfish, crab
NM disorders with RF Myasthenia gravis AC overdose Antibiotics Hypermagnesemia Botulism Poisoning * Tick paralysis LE syndrome Tensilon test, Ach. RAb Tensilon test — — Plasma level, RNS Antibody, RNS Identification Find the tick Increment on RNS PP, Steroid Withdrawal IV calcium Antitoxin Removal PP, steroid * snake, scorpion, spider, fish, shellfish, crab
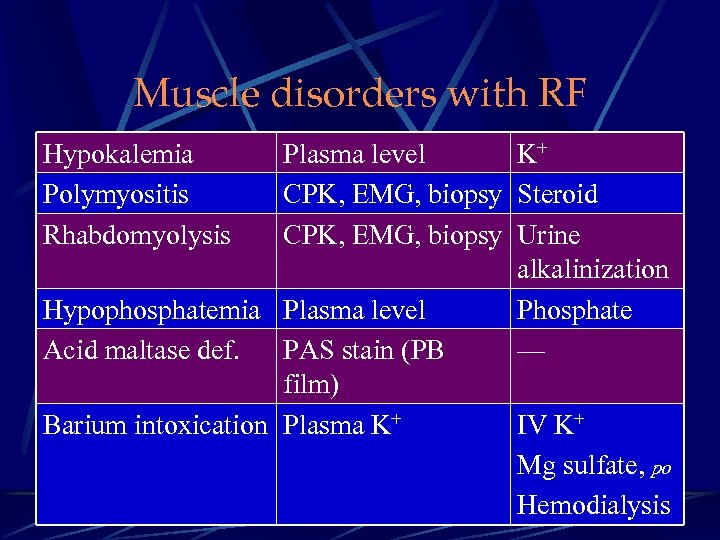 Muscle disorders with RF Hypokalemia Polymyositis Rhabdomyolysis Plasma level K+ CPK, EMG, biopsy Steroid CPK, EMG, biopsy Urine alkalinization Hypophosphatemia Plasma level Phosphate Acid maltase def. PAS stain (PB — film) Barium intoxication Plasma K+ IV K+ Mg sulfate, po Hemodialysis
Muscle disorders with RF Hypokalemia Polymyositis Rhabdomyolysis Plasma level K+ CPK, EMG, biopsy Steroid CPK, EMG, biopsy Urine alkalinization Hypophosphatemia Plasma level Phosphate Acid maltase def. PAS stain (PB — film) Barium intoxication Plasma K+ IV K+ Mg sulfate, po Hemodialysis
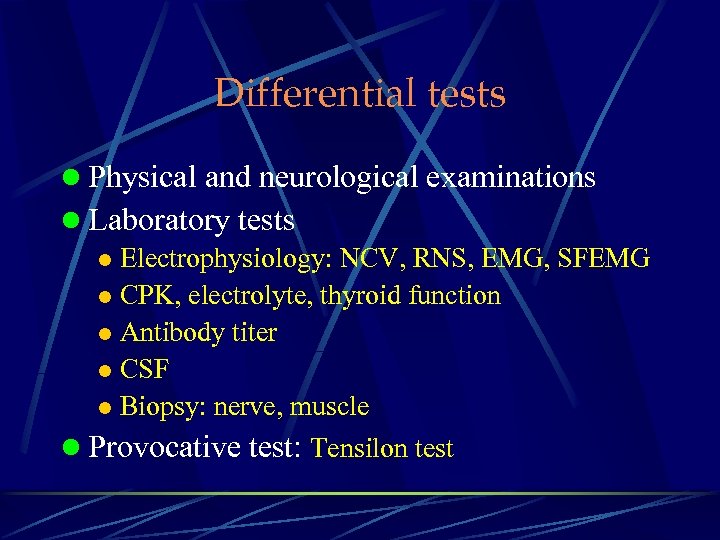 Differential tests l Physical and neurological examinations l Laboratory tests l Electrophysiology: NCV, RNS, EMG, SFEMG l CPK, electrolyte, thyroid function l Antibody titer l CSF l Biopsy: nerve, muscle l Provocative test: Tensilon test
Differential tests l Physical and neurological examinations l Laboratory tests l Electrophysiology: NCV, RNS, EMG, SFEMG l CPK, electrolyte, thyroid function l Antibody titer l CSF l Biopsy: nerve, muscle l Provocative test: Tensilon test
 General Management in ICU
General Management in ICU
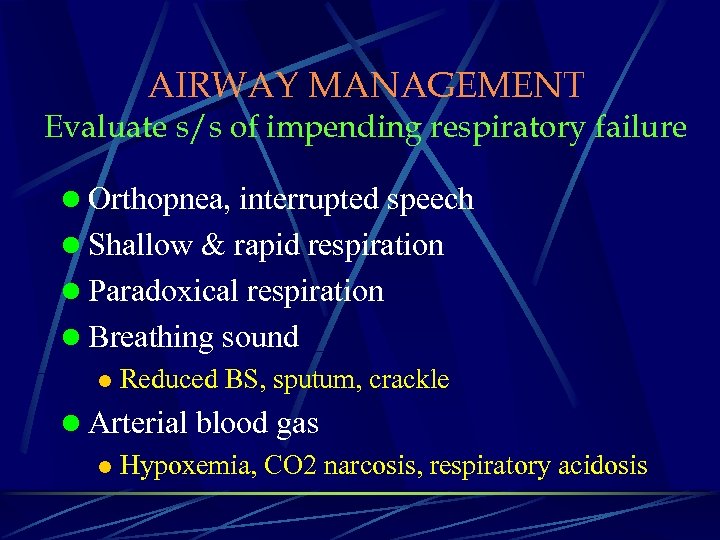 AIRWAY MANAGEMENT Evaluate s/s of impending respiratory failure l Orthopnea, interrupted speech l Shallow & rapid respiration l Paradoxical respiration l Breathing sound l Reduced BS, sputum, crackle l Arterial blood gas l Hypoxemia, CO 2 narcosis, respiratory acidosis
AIRWAY MANAGEMENT Evaluate s/s of impending respiratory failure l Orthopnea, interrupted speech l Shallow & rapid respiration l Paradoxical respiration l Breathing sound l Reduced BS, sputum, crackle l Arterial blood gas l Hypoxemia, CO 2 narcosis, respiratory acidosis
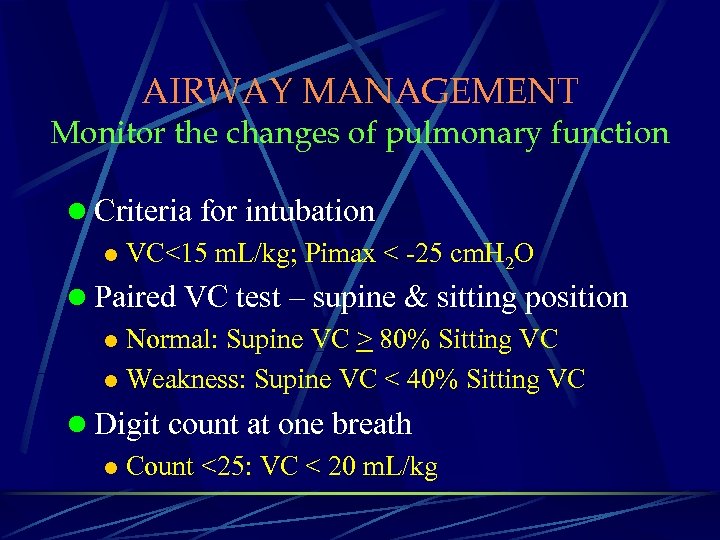 AIRWAY MANAGEMENT Monitor the changes of pulmonary function l Criteria for intubation l VC<15 m. L/kg; Pimax < -25 cm. H 2 O l Paired VC test – supine & sitting position l Normal: Supine VC > 80% Sitting VC l Weakness: Supine VC < 40% Sitting VC l Digit count at one breath l Count <25: VC < 20 m. L/kg
AIRWAY MANAGEMENT Monitor the changes of pulmonary function l Criteria for intubation l VC<15 m. L/kg; Pimax < -25 cm. H 2 O l Paired VC test – supine & sitting position l Normal: Supine VC > 80% Sitting VC l Weakness: Supine VC < 40% Sitting VC l Digit count at one breath l Count <25: VC < 20 m. L/kg
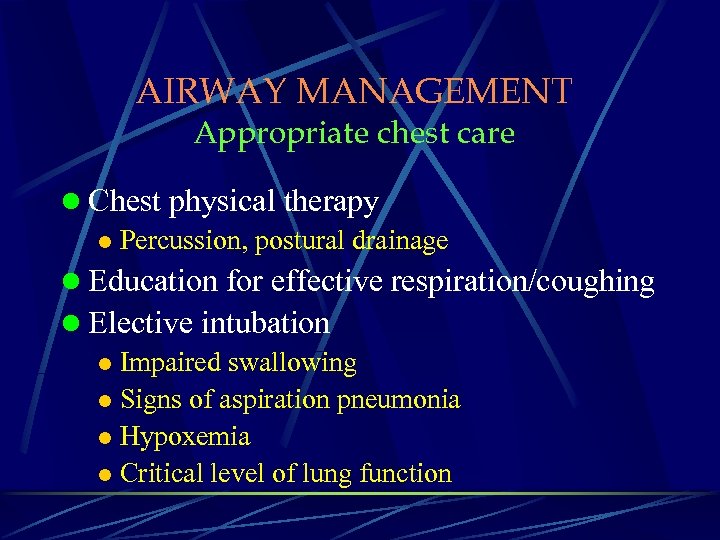 AIRWAY MANAGEMENT Appropriate chest care l Chest physical therapy l Percussion, postural drainage l Education for effective respiration/coughing l Elective intubation l Impaired swallowing l Signs of aspiration pneumonia l Hypoxemia l Critical level of lung function
AIRWAY MANAGEMENT Appropriate chest care l Chest physical therapy l Percussion, postural drainage l Education for effective respiration/coughing l Elective intubation l Impaired swallowing l Signs of aspiration pneumonia l Hypoxemia l Critical level of lung function
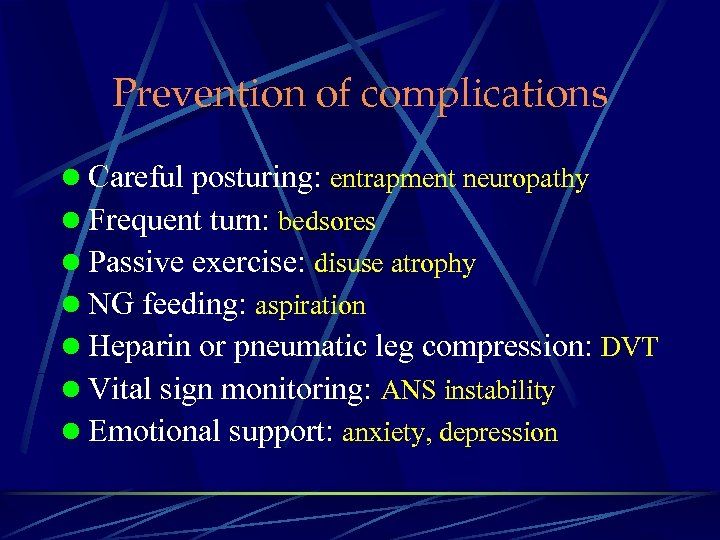 Prevention of complications l Careful posturing: entrapment neuropathy l Frequent turn: bedsores l Passive exercise: disuse atrophy l NG feeding: aspiration l Heparin or pneumatic leg compression: DVT l Vital sign monitoring: ANS instability l Emotional support: anxiety, depression
Prevention of complications l Careful posturing: entrapment neuropathy l Frequent turn: bedsores l Passive exercise: disuse atrophy l NG feeding: aspiration l Heparin or pneumatic leg compression: DVT l Vital sign monitoring: ANS instability l Emotional support: anxiety, depression
 Guillain-Barré syndrome
Guillain-Barré syndrome
 Guillain-Barré Syndrome (Acute inflammatory demyelinating polyneuropathy) l Acute/subacute motor paralysis for days/wks l Arefelexia or hyporeflexia l Mild sensory symptoms or signs l CSF: albuminocytological dissociation l NCV: conduction slowing or block l Pathology l Focal segmental demyelination l Inflammatory cells infiltration
Guillain-Barré Syndrome (Acute inflammatory demyelinating polyneuropathy) l Acute/subacute motor paralysis for days/wks l Arefelexia or hyporeflexia l Mild sensory symptoms or signs l CSF: albuminocytological dissociation l NCV: conduction slowing or block l Pathology l Focal segmental demyelination l Inflammatory cells infiltration
 Clinical course l Course l Progression: 4 wk (90%) l Plateau: 4 wk (85%) l Recovery: 4 -6 months (80%) l Outcome l Permanent residua: 15% l Permanently disabled: 5% l Mortality: 2 -5% l Relapse: 3%
Clinical course l Course l Progression: 4 wk (90%) l Plateau: 4 wk (85%) l Recovery: 4 -6 months (80%) l Outcome l Permanent residua: 15% l Permanently disabled: 5% l Mortality: 2 -5% l Relapse: 3%
 Clinical features - I l Spectrum: mild ataxia to total paralysis l Limb involvement l Leg onset: arm & face are possible l Proximal > distal involvement l Symmetric pattern l Absence of DTR even in minimally involved m. l External urethral sphnicter l 10 -20% l retention > incontinence
Clinical features - I l Spectrum: mild ataxia to total paralysis l Limb involvement l Leg onset: arm & face are possible l Proximal > distal involvement l Symmetric pattern l Absence of DTR even in minimally involved m. l External urethral sphnicter l 10 -20% l retention > incontinence
 Clinical features - II l Cranial N involvement l VII: asymmetric: 50% (esp. upper lip/perioral) l EOM: 10% l Isolated cranial N: 5% l Oropharngeal involvement: 40% (herald of impending respiratory failure) l Respiratory muscle involvement l Major cranial N involvement frequently associated l Weakness of shoulder elevation & neck flexion parallels diaphragmatic weakness & resp. failure
Clinical features - II l Cranial N involvement l VII: asymmetric: 50% (esp. upper lip/perioral) l EOM: 10% l Isolated cranial N: 5% l Oropharngeal involvement: 40% (herald of impending respiratory failure) l Respiratory muscle involvement l Major cranial N involvement frequently associated l Weakness of shoulder elevation & neck flexion parallels diaphragmatic weakness & resp. failure
 Clinical features -III l Autonomic involvement: 65% l Sinus tachycardia: > 50% l SIADH, (DI) l Orthostatic hypotension (20%) & hypertension l Sweating disturbance l Cardiac dysautonomia may correlate with sensory dysfunction ( Raphael JC, 1986 ) l Muscular of neuropathic pain: 30 -55% l follow vigorous exercise (chaley horse) l distributed in thigh, buttock & low back
Clinical features -III l Autonomic involvement: 65% l Sinus tachycardia: > 50% l SIADH, (DI) l Orthostatic hypotension (20%) & hypertension l Sweating disturbance l Cardiac dysautonomia may correlate with sensory dysfunction ( Raphael JC, 1986 ) l Muscular of neuropathic pain: 30 -55% l follow vigorous exercise (chaley horse) l distributed in thigh, buttock & low back
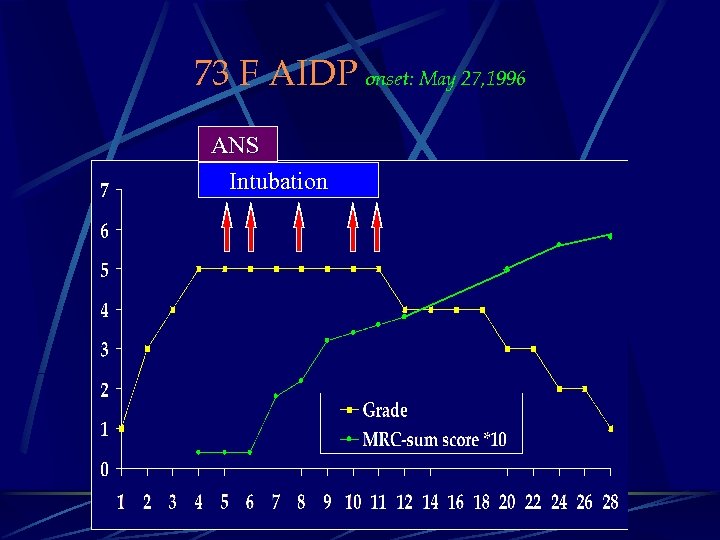 73 F AIDP onset: May 27, 1996 ANS Intubation
73 F AIDP onset: May 27, 1996 ANS Intubation
 GBS之處置 l 呼吸道: 插管 l 肺活量監控, VC<15 m. L/Kg, Pimax < -20 mm. Hg l 輸液: N/S 2 L/天 l 營養: 腸道營養。如有腸堵塞才改靜脈營養 l 特殊處置 l IVIG (免疫球蛋白), 0. 4 g/Kg/天 x 5天 l PE (血漿交換) 隔日一次 x 5次 l 如使用呼吸器或同時使用 aspirin/NSAID病人, 投予Sucralfate 10 m. L bid. l 肌肉疼痛可投予肌肉注射類固醇
GBS之處置 l 呼吸道: 插管 l 肺活量監控, VC<15 m. L/Kg, Pimax < -20 mm. Hg l 輸液: N/S 2 L/天 l 營養: 腸道營養。如有腸堵塞才改靜脈營養 l 特殊處置 l IVIG (免疫球蛋白), 0. 4 g/Kg/天 x 5天 l PE (血漿交換) 隔日一次 x 5次 l 如使用呼吸器或同時使用 aspirin/NSAID病人, 投予Sucralfate 10 m. L bid. l 肌肉疼痛可投予肌肉注射類固醇
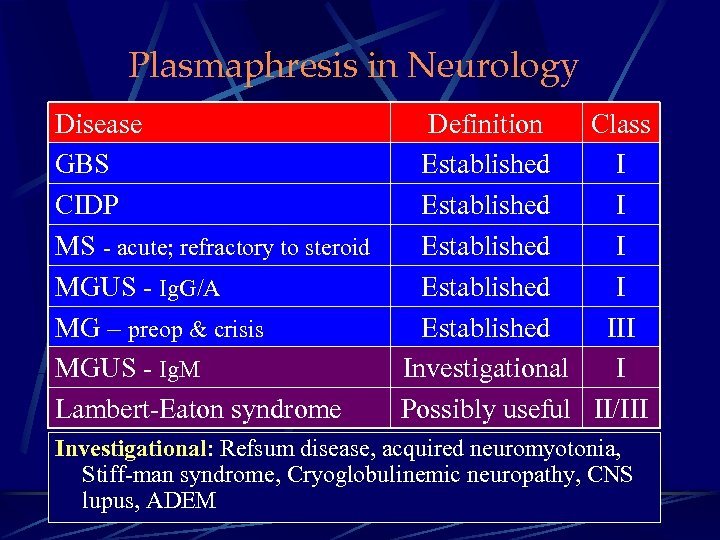 Plasmaphresis in Neurology Disease GBS CIDP MS - acute; refractory to steroid MGUS - Ig. G/A MG – preop & crisis MGUS - Ig. M Lambert-Eaton syndrome Definition Class Established I Established III Investigational I Possibly useful II/III Investigational: Refsum disease, acquired neuromyotonia, Stiff-man syndrome, Cryoglobulinemic neuropathy, CNS lupus, ADEM
Plasmaphresis in Neurology Disease GBS CIDP MS - acute; refractory to steroid MGUS - Ig. G/A MG – preop & crisis MGUS - Ig. M Lambert-Eaton syndrome Definition Class Established I Established III Investigational I Possibly useful II/III Investigational: Refsum disease, acquired neuromyotonia, Stiff-man syndrome, Cryoglobulinemic neuropathy, CNS lupus, ADEM
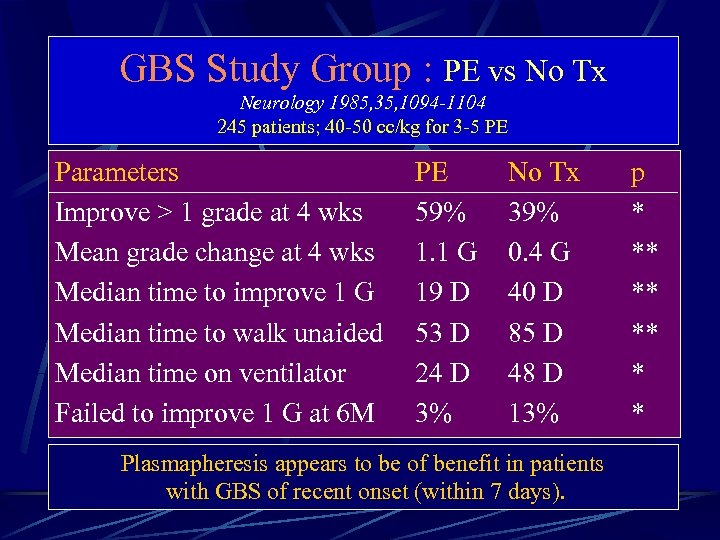 GBS Study Group : PE vs No Tx Neurology 1985, 35, 1094 -1104 245 patients; 40 -50 cc/kg for 3 -5 PE Parameters Improve > 1 grade at 4 wks Mean grade change at 4 wks Median time to improve 1 G Median time to walk unaided Median time on ventilator Failed to improve 1 G at 6 M PE 59% 1. 1 G 19 D 53 D 24 D 3% No Tx 39% 0. 4 G 40 D 85 D 48 D 13% Plasmapheresis appears to be of benefit in patients with GBS of recent onset (within 7 days). p * ** * *
GBS Study Group : PE vs No Tx Neurology 1985, 35, 1094 -1104 245 patients; 40 -50 cc/kg for 3 -5 PE Parameters Improve > 1 grade at 4 wks Mean grade change at 4 wks Median time to improve 1 G Median time to walk unaided Median time on ventilator Failed to improve 1 G at 6 M PE 59% 1. 1 G 19 D 53 D 24 D 3% No Tx 39% 0. 4 G 40 D 85 D 48 D 13% Plasmapheresis appears to be of benefit in patients with GBS of recent onset (within 7 days). p * ** * *
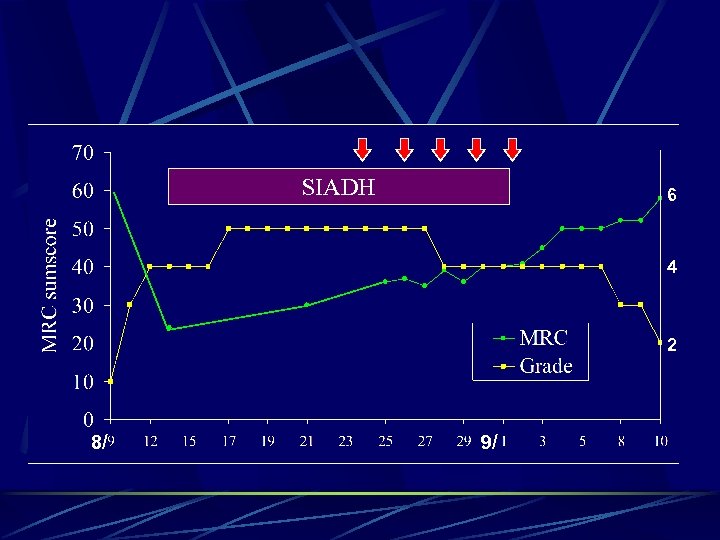
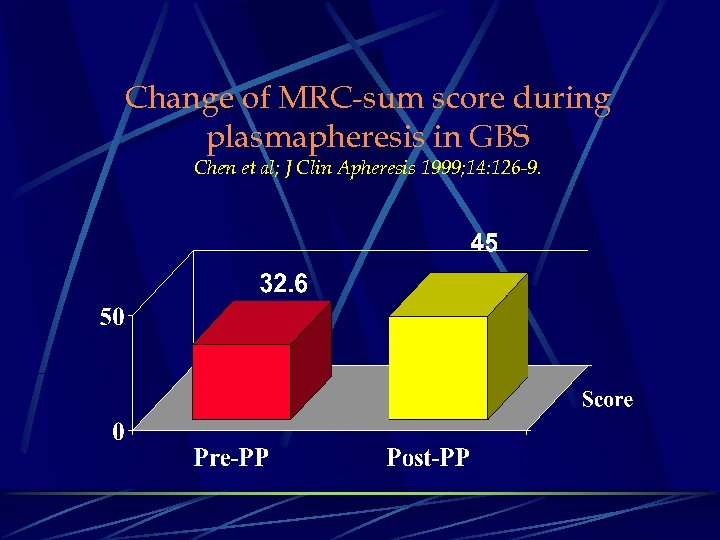 Change of MRC-sum score during plasmapheresis in GBS Chen et al; J Clin Apheresis 1999; 14: 126 -9.
Change of MRC-sum score during plasmapheresis in GBS Chen et al; J Clin Apheresis 1999; 14: 126 -9.
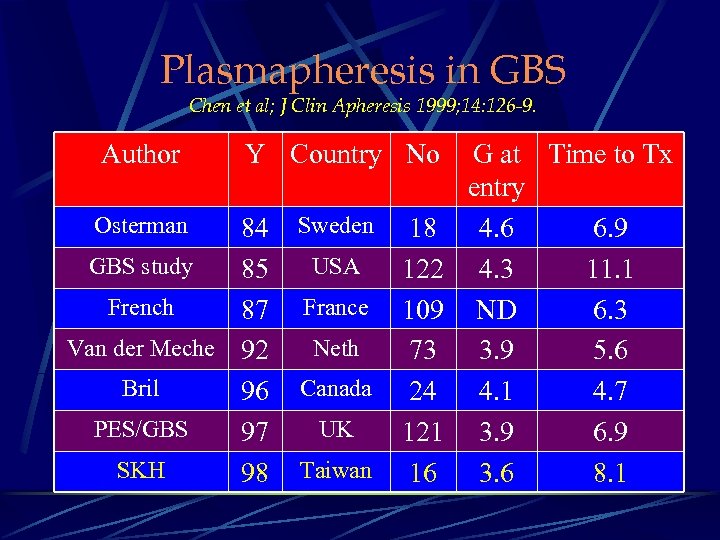 Plasmapheresis in GBS Chen et al; J Clin Apheresis 1999; 14: 126 -9. Author Y Country No Osterman Sweden 84 GBS study 85 French 87 Van der Meche 92 Bril 96 PES/GBS 97 SKH 98 USA France Neth Canada UK Taiwan G at Time to Tx entry 18 4. 6 6. 9 122 4. 3 11. 1 109 ND 6. 3 73 3. 9 5. 6 24 4. 1 4. 7 121 3. 9 6. 9 16 3. 6 8. 1
Plasmapheresis in GBS Chen et al; J Clin Apheresis 1999; 14: 126 -9. Author Y Country No Osterman Sweden 84 GBS study 85 French 87 Van der Meche 92 Bril 96 PES/GBS 97 SKH 98 USA France Neth Canada UK Taiwan G at Time to Tx entry 18 4. 6 6. 9 122 4. 3 11. 1 109 ND 6. 3 73 3. 9 5. 6 24 4. 1 4. 7 121 3. 9 6. 9 16 3. 6 8. 1
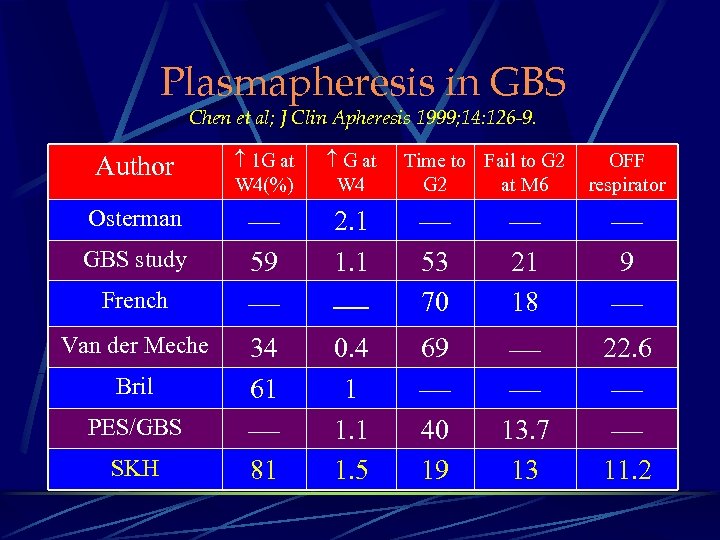 Plasmapheresis in GBS Chen et al; J Clin Apheresis 1999; 14: 126 -9. Author 1 G at W 4(%) G at W 4 Osterman 59 2. 1 1. 1 34 61 81 GBS study French Van der Meche Bril PES/GBS SKH Time to Fail to G 2 at M 6 OFF respirator 53 70 21 18 9 0. 4 1 1. 5 69 40 19 13. 7 13 22. 6 11. 2
Plasmapheresis in GBS Chen et al; J Clin Apheresis 1999; 14: 126 -9. Author 1 G at W 4(%) G at W 4 Osterman 59 2. 1 1. 1 34 61 81 GBS study French Van der Meche Bril PES/GBS SKH Time to Fail to G 2 at M 6 OFF respirator 53 70 21 18 9 0. 4 1 1. 5 69 40 19 13. 7 13 22. 6 11. 2
 GBS病情惡化之成因 l 病情持續惡化 l 病情穩定後再復發(relapse) l 自律神經異常(dysautonomia) l 好發於急速癱瘓且合併眼肌麻痺者 l 血壓不穩 l 心律不整 l 呼吸器相關之併發症
GBS病情惡化之成因 l 病情持續惡化 l 病情穩定後再復發(relapse) l 自律神經異常(dysautonomia) l 好發於急速癱瘓且合併眼肌麻痺者 l 血壓不穩 l 心律不整 l 呼吸器相關之併發症
 Myasthenic Crisis
Myasthenic Crisis
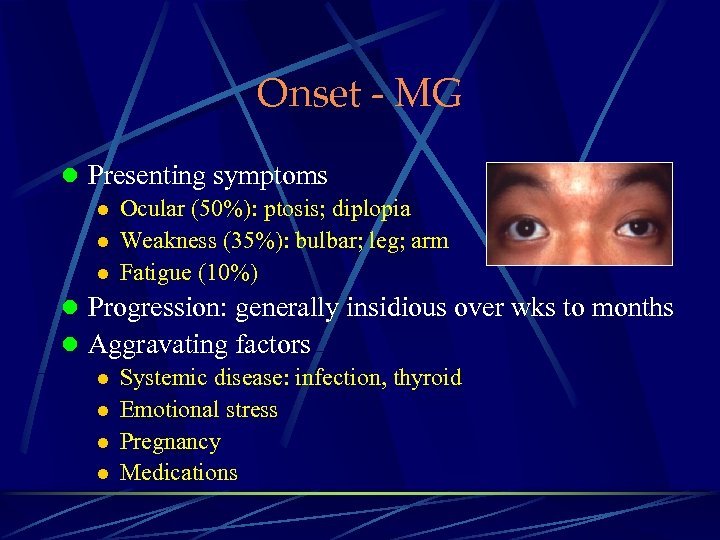 Onset - MG l Presenting symptoms l Ocular (50%): ptosis; diplopia l Weakness (35%): bulbar; leg; arm l Fatigue (10%) l Progression: generally insidious over wks to months l Aggravating factors l Systemic disease: infection, thyroid l Emotional stress l Pregnancy l Medications
Onset - MG l Presenting symptoms l Ocular (50%): ptosis; diplopia l Weakness (35%): bulbar; leg; arm l Fatigue (10%) l Progression: generally insidious over wks to months l Aggravating factors l Systemic disease: infection, thyroid l Emotional stress l Pregnancy l Medications
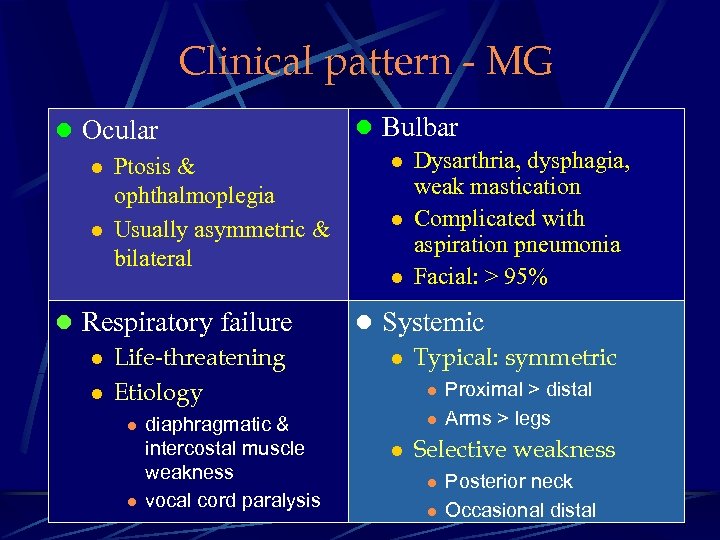 Clinical pattern - MG l Ocular l Ptosis & ophthalmoplegia l Usually asymmetric & bilateral l Bulbar l Dysarthria, dysphagia, weak mastication l Complicated with aspiration pneumonia l Facial: > 95% l Respiratory failure l Life-threatening l Etiology l Systemic l Typical: symmetric l l diaphragmatic & intercostal muscle weakness vocal cord paralysis l l l Proximal > distal Arms > legs Selective weakness l l Posterior neck Occasional distal
Clinical pattern - MG l Ocular l Ptosis & ophthalmoplegia l Usually asymmetric & bilateral l Bulbar l Dysarthria, dysphagia, weak mastication l Complicated with aspiration pneumonia l Facial: > 95% l Respiratory failure l Life-threatening l Etiology l Systemic l Typical: symmetric l l diaphragmatic & intercostal muscle weakness vocal cord paralysis l l l Proximal > distal Arms > legs Selective weakness l l Posterior neck Occasional distal
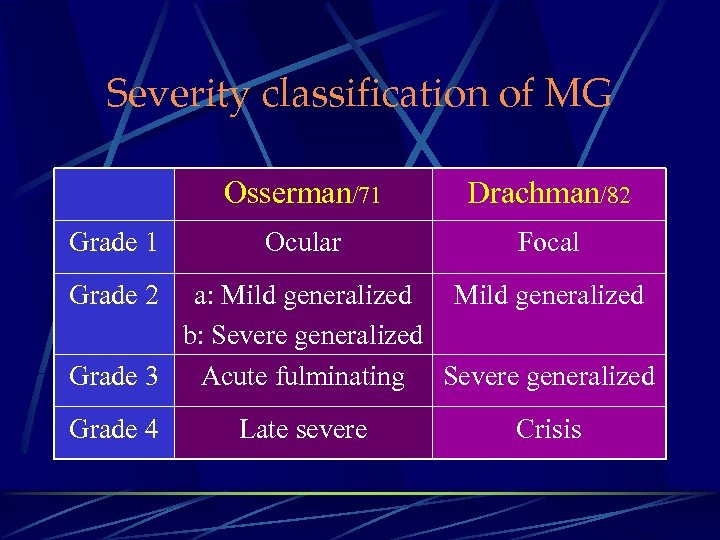 Severity classification of MG Osserman/71 Grade 1 Drachman/82 Ocular Focal Grade 2 a: Mild generalized b: Severe generalized Grade 3 Acute fulminating Severe generalized Grade 4 Late severe Crisis
Severity classification of MG Osserman/71 Grade 1 Drachman/82 Ocular Focal Grade 2 a: Mild generalized b: Severe generalized Grade 3 Acute fulminating Severe generalized Grade 4 Late severe Crisis
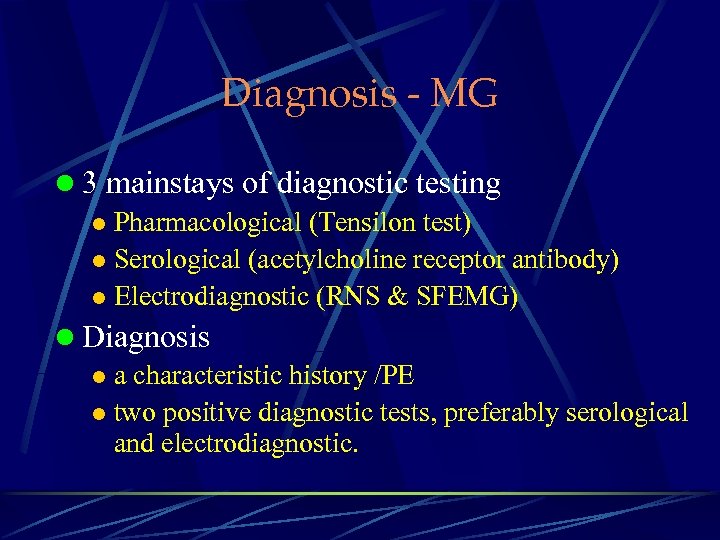 Diagnosis - MG l 3 mainstays of diagnostic testing l Pharmacological (Tensilon test) l Serological (acetylcholine receptor antibody) l Electrodiagnostic (RNS & SFEMG) l Diagnosis l a characteristic history /PE l two positive diagnostic tests, preferably serological and electrodiagnostic.
Diagnosis - MG l 3 mainstays of diagnostic testing l Pharmacological (Tensilon test) l Serological (acetylcholine receptor antibody) l Electrodiagnostic (RNS & SFEMG) l Diagnosis l a characteristic history /PE l two positive diagnostic tests, preferably serological and electrodiagnostic.
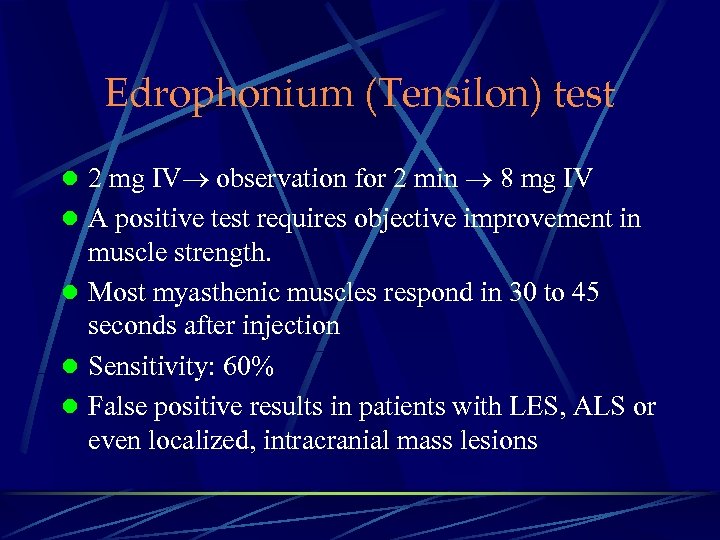 Edrophonium (Tensilon) test l 2 mg IV observation for 2 min 8 mg IV l A positive test requires objective improvement in muscle strength. l Most myasthenic muscles respond in 30 to 45 seconds after injection l Sensitivity: 60% l False positive results in patients with LES, ALS or even localized, intracranial mass lesions
Edrophonium (Tensilon) test l 2 mg IV observation for 2 min 8 mg IV l A positive test requires objective improvement in muscle strength. l Most myasthenic muscles respond in 30 to 45 seconds after injection l Sensitivity: 60% l False positive results in patients with LES, ALS or even localized, intracranial mass lesions
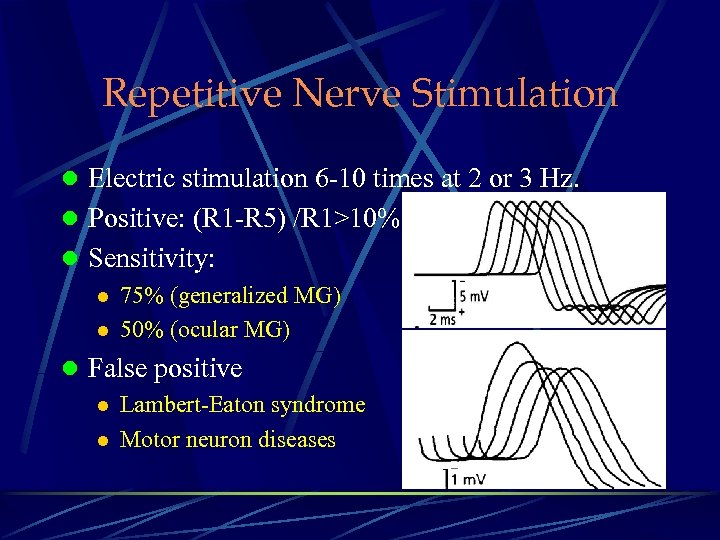 Repetitive Nerve Stimulation l Electric stimulation 6 -10 times at 2 or 3 Hz. l Positive: (R 1 -R 5) /R 1>10% l Sensitivity: l 75% (generalized MG) l 50% (ocular MG) l False positive l Lambert-Eaton syndrome l Motor neuron diseases
Repetitive Nerve Stimulation l Electric stimulation 6 -10 times at 2 or 3 Hz. l Positive: (R 1 -R 5) /R 1>10% l Sensitivity: l 75% (generalized MG) l 50% (ocular MG) l False positive l Lambert-Eaton syndrome l Motor neuron diseases
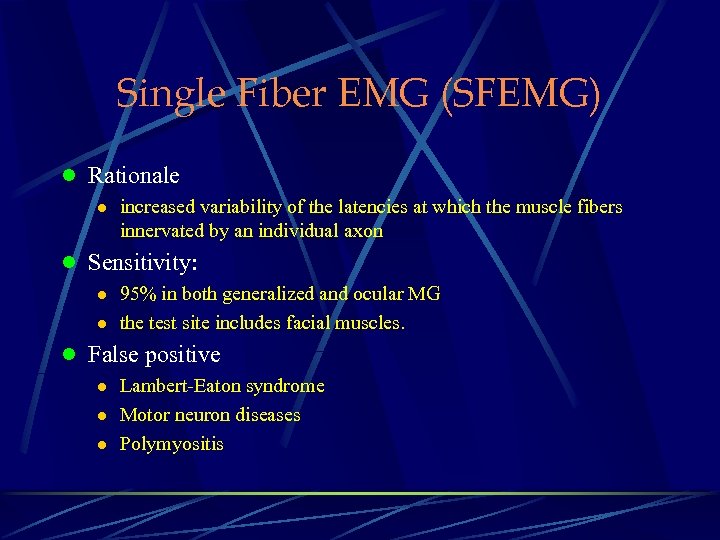 Single Fiber EMG (SFEMG) l Rationale l increased variability of the latencies at which the muscle fibers innervated by an individual axon l Sensitivity: l 95% in both generalized and ocular MG l the test site includes facial muscles. l False positive l Lambert-Eaton syndrome l Motor neuron diseases l Polymyositis
Single Fiber EMG (SFEMG) l Rationale l increased variability of the latencies at which the muscle fibers innervated by an individual axon l Sensitivity: l 95% in both generalized and ocular MG l the test site includes facial muscles. l False positive l Lambert-Eaton syndrome l Motor neuron diseases l Polymyositis
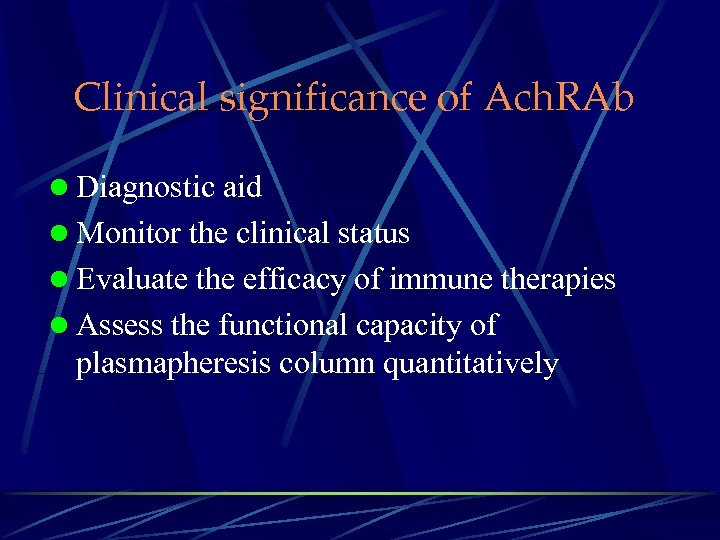 Clinical significance of Ach. RAb l Diagnostic aid l Monitor the clinical status l Evaluate the efficacy of immune therapies l Assess the functional capacity of plasmapheresis column quantitatively
Clinical significance of Ach. RAb l Diagnostic aid l Monitor the clinical status l Evaluate the efficacy of immune therapies l Assess the functional capacity of plasmapheresis column quantitatively
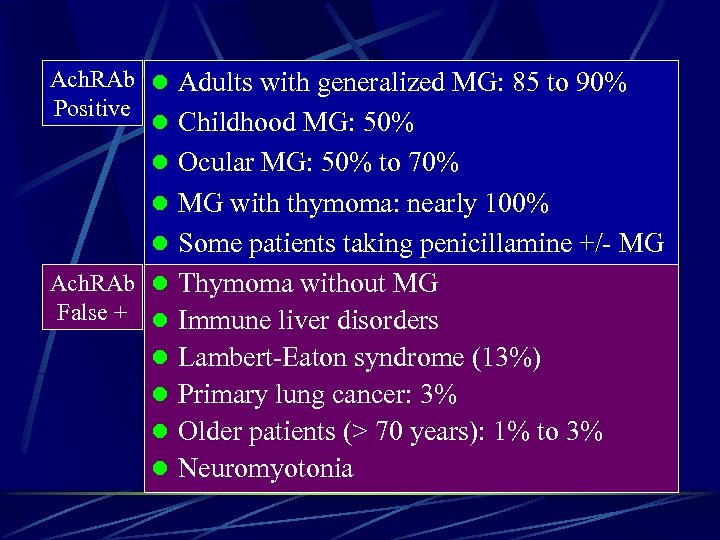 Ach. RAb l Adults with generalized MG: 85 to 90% Positive l Childhood MG: 50% l Ocular MG: 50% to 70% l MG with thymoma: nearly 100% l Some patients taking penicillamine +/- MG Ach. RAb l Thymoma without MG False + l Immune liver disorders l Lambert-Eaton syndrome (13%) l Primary lung cancer: 3% l Older patients (> 70 years): 1% to 3% l Neuromyotonia
Ach. RAb l Adults with generalized MG: 85 to 90% Positive l Childhood MG: 50% l Ocular MG: 50% to 70% l MG with thymoma: nearly 100% l Some patients taking penicillamine +/- MG Ach. RAb l Thymoma without MG False + l Immune liver disorders l Lambert-Eaton syndrome (13%) l Primary lung cancer: 3% l Older patients (> 70 years): 1% to 3% l Neuromyotonia
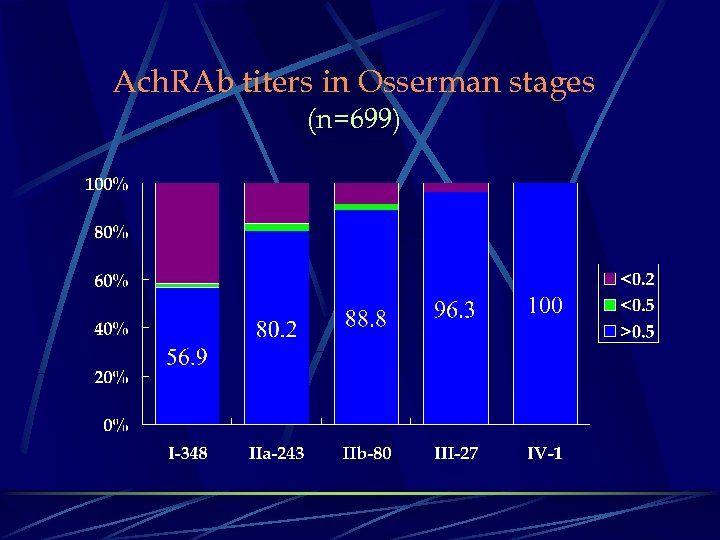 Ach. RAb titers in Osserman stages (n=699)
Ach. RAb titers in Osserman stages (n=699)
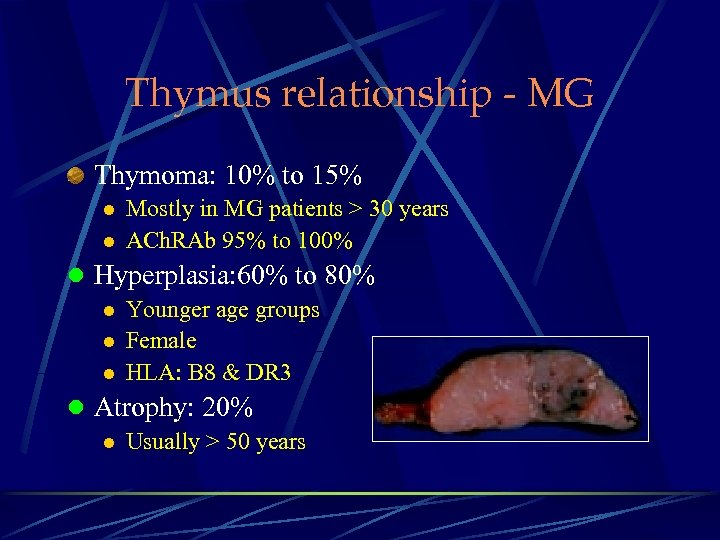 Thymus relationship - MG Thymoma: 10% to 15% l l Mostly in MG patients > 30 years ACh. RAb 95% to 100% l Hyperplasia: 60% to 80% l Younger age groups l Female l HLA: B 8 & DR 3 l Atrophy: 20% l Usually > 50 years
Thymus relationship - MG Thymoma: 10% to 15% l l Mostly in MG patients > 30 years ACh. RAb 95% to 100% l Hyperplasia: 60% to 80% l Younger age groups l Female l HLA: B 8 & DR 3 l Atrophy: 20% l Usually > 50 years
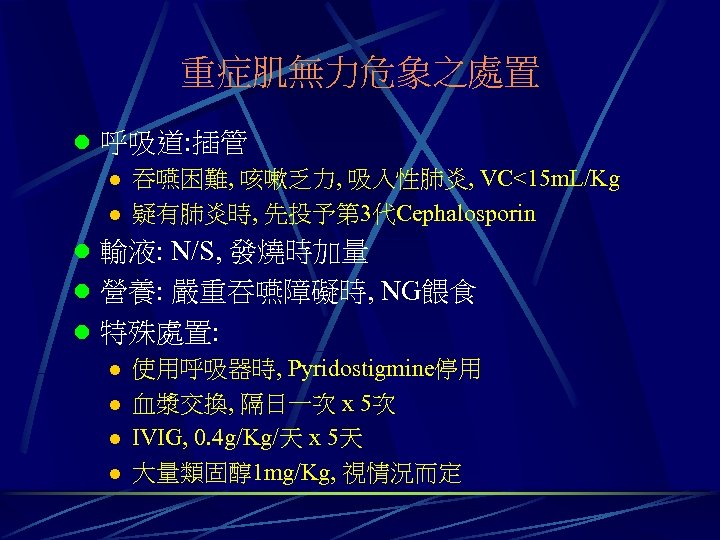 重症肌無力危象之處置 l 呼吸道: 插管 l 吞嚥困難, 咳嗽乏力, 吸入性肺炎, VC<15 m. L/Kg l 疑有肺炎時, 先投予第 3代Cephalosporin l 輸液: N/S, 發燒時加量 l 營養: 嚴重吞嚥障礙時, NG餵食 l 特殊處置: l 使用呼吸器時, Pyridostigmine停用 l 血漿交換, 隔日一次 x 5次 l IVIG, 0. 4 g/Kg/天 x 5天 l 大量類固醇1 mg/Kg, 視情況而定
重症肌無力危象之處置 l 呼吸道: 插管 l 吞嚥困難, 咳嗽乏力, 吸入性肺炎, VC<15 m. L/Kg l 疑有肺炎時, 先投予第 3代Cephalosporin l 輸液: N/S, 發燒時加量 l 營養: 嚴重吞嚥障礙時, NG餵食 l 特殊處置: l 使用呼吸器時, Pyridostigmine停用 l 血漿交換, 隔日一次 x 5次 l IVIG, 0. 4 g/Kg/天 x 5天 l 大量類固醇1 mg/Kg, 視情況而定
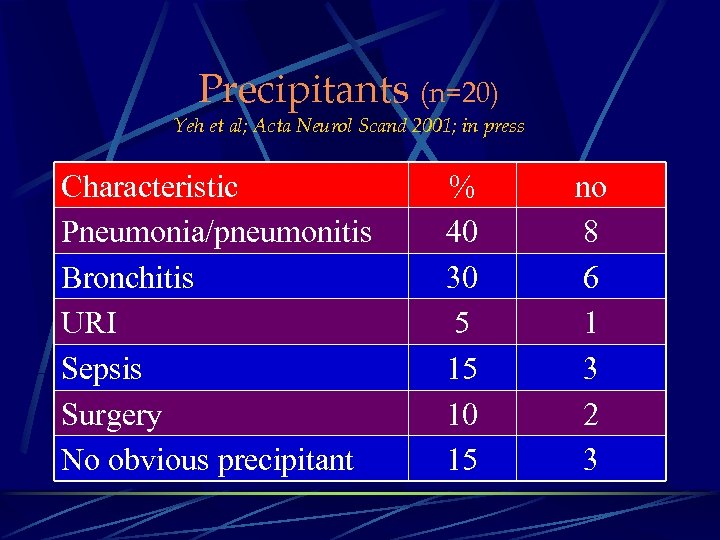 Precipitants (n=20) Yeh et al; Acta Neurol Scand 2001; in press Characteristic Pneumonia/pneumonitis Bronchitis URI Sepsis Surgery No obvious precipitant % 40 30 5 15 10 15 no 8 6 1 3 2 3
Precipitants (n=20) Yeh et al; Acta Neurol Scand 2001; in press Characteristic Pneumonia/pneumonitis Bronchitis URI Sepsis Surgery No obvious precipitant % 40 30 5 15 10 15 no 8 6 1 3 2 3
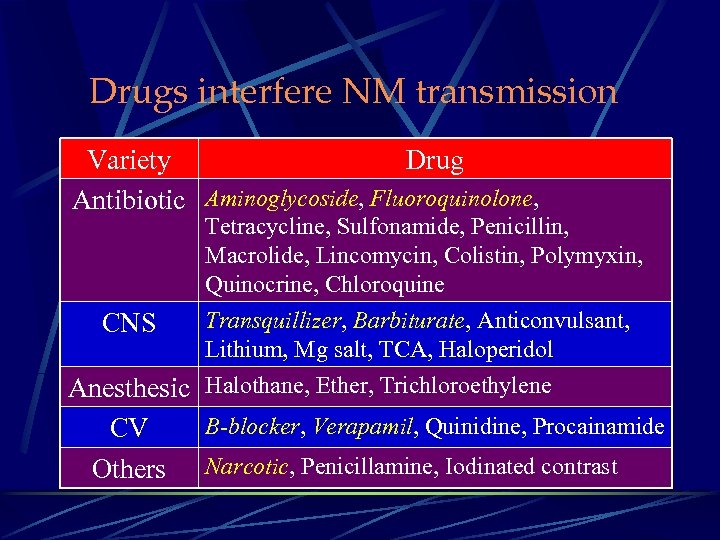 Drugs interfere NM transmission Variety Drug Antibiotic Aminoglycoside, Fluoroquinolone, Tetracycline, Sulfonamide, Penicillin, Macrolide, Lincomycin, Colistin, Polymyxin, Quinocrine, Chloroquine Transquillizer, Barbiturate, Anticonvulsant, Lithium, Mg salt, TCA, Haloperidol Anesthesic Halothane, Ether, Trichloroethylene CNS CV Others B-blocker, Verapamil, Quinidine, Procainamide Narcotic, Penicillamine, Iodinated contrast
Drugs interfere NM transmission Variety Drug Antibiotic Aminoglycoside, Fluoroquinolone, Tetracycline, Sulfonamide, Penicillin, Macrolide, Lincomycin, Colistin, Polymyxin, Quinocrine, Chloroquine Transquillizer, Barbiturate, Anticonvulsant, Lithium, Mg salt, TCA, Haloperidol Anesthesic Halothane, Ether, Trichloroethylene CNS CV Others B-blocker, Verapamil, Quinidine, Procainamide Narcotic, Penicillamine, Iodinated contrast
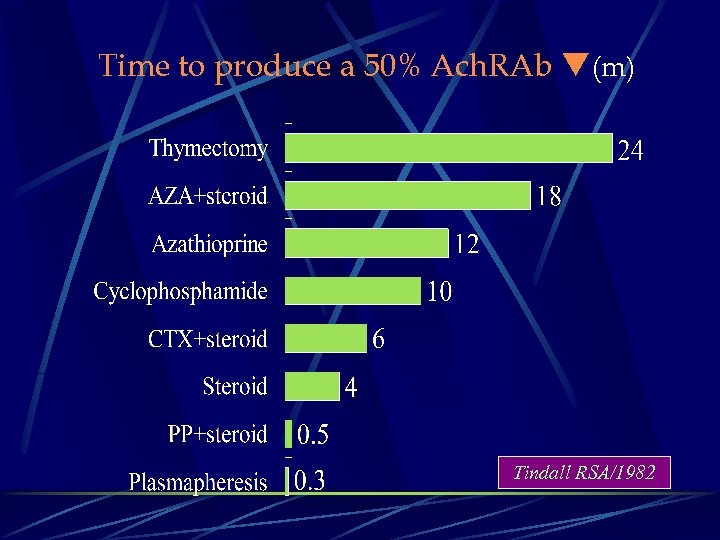 Time to produce a 50% Ach. RAb (m) Tindall RSA/1982
Time to produce a 50% Ach. RAb (m) Tindall RSA/1982
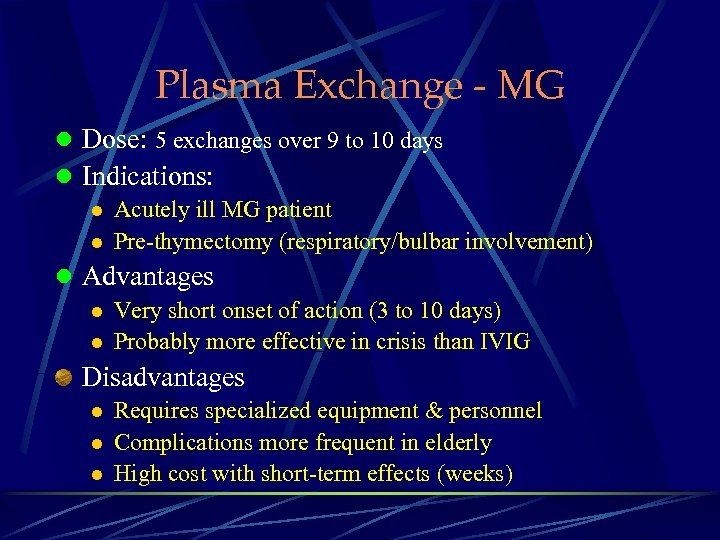 Plasma Exchange - MG l Dose: 5 exchanges over 9 to 10 days l Indications: l Acutely ill MG patient l Pre-thymectomy (respiratory/bulbar involvement) l Advantages l Very short onset of action (3 to 10 days) l Probably more effective in crisis than IVIG Disadvantages l l l Requires specialized equipment & personnel Complications more frequent in elderly High cost with short-term effects (weeks)
Plasma Exchange - MG l Dose: 5 exchanges over 9 to 10 days l Indications: l Acutely ill MG patient l Pre-thymectomy (respiratory/bulbar involvement) l Advantages l Very short onset of action (3 to 10 days) l Probably more effective in crisis than IVIG Disadvantages l l l Requires specialized equipment & personnel Complications more frequent in elderly High cost with short-term effects (weeks)
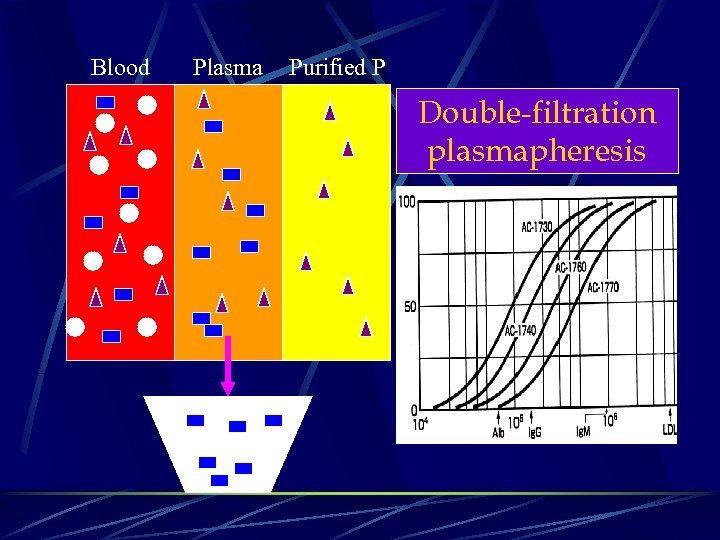 Blood Plasma Purified P Double-filtration plasmapheresis
Blood Plasma Purified P Double-filtration plasmapheresis
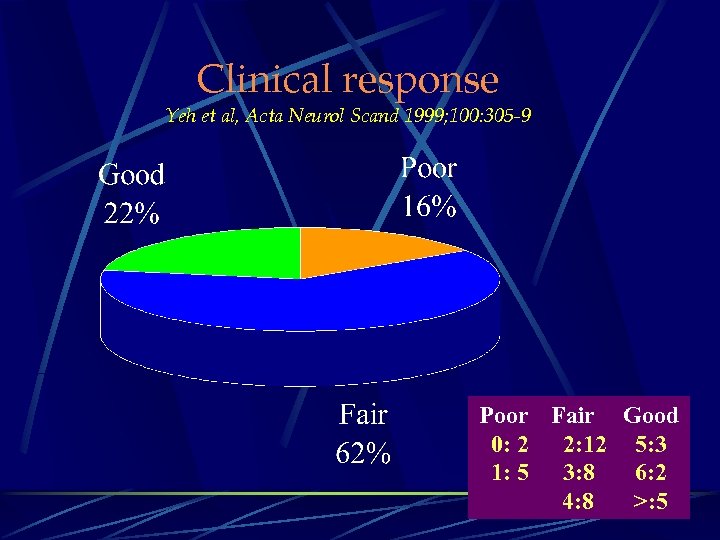 Clinical response Yeh et al, Acta Neurol Scand 1999; 100: 305 -9 Poor Fair Good 0: 2 2: 12 5: 3 1: 5 3: 8 6: 2 4: 8 >: 5
Clinical response Yeh et al, Acta Neurol Scand 1999; 100: 305 -9 Poor Fair Good 0: 2 2: 12 5: 3 1: 5 3: 8 6: 2 4: 8 >: 5
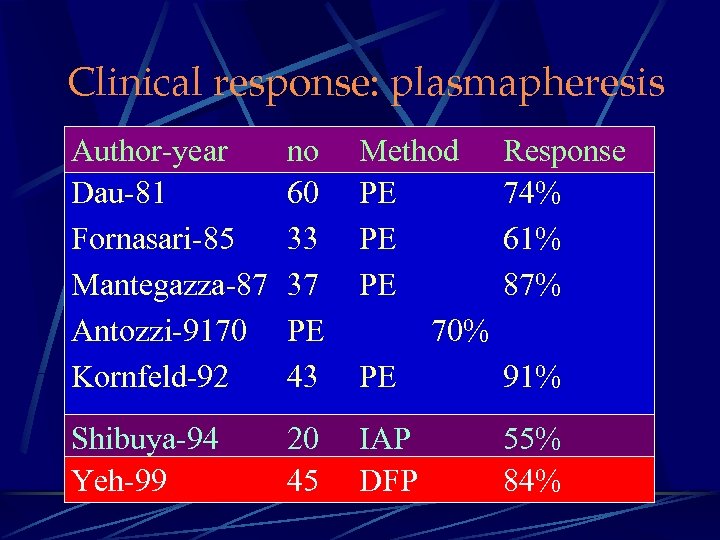 Clinical response: plasmapheresis Author-year Dau-81 Fornasari-85 Mantegazza-87 Antozzi-9170 Kornfeld-92 no 60 33 37 PE 43 Method PE PE PE 70% PE Response 74% 61% 87% Shibuya-94 Yeh-99 20 45 IAP DFP 55% 84% 91%
Clinical response: plasmapheresis Author-year Dau-81 Fornasari-85 Mantegazza-87 Antozzi-9170 Kornfeld-92 no 60 33 37 PE 43 Method PE PE PE 70% PE Response 74% 61% 87% Shibuya-94 Yeh-99 20 45 IAP DFP 55% 84% 91%
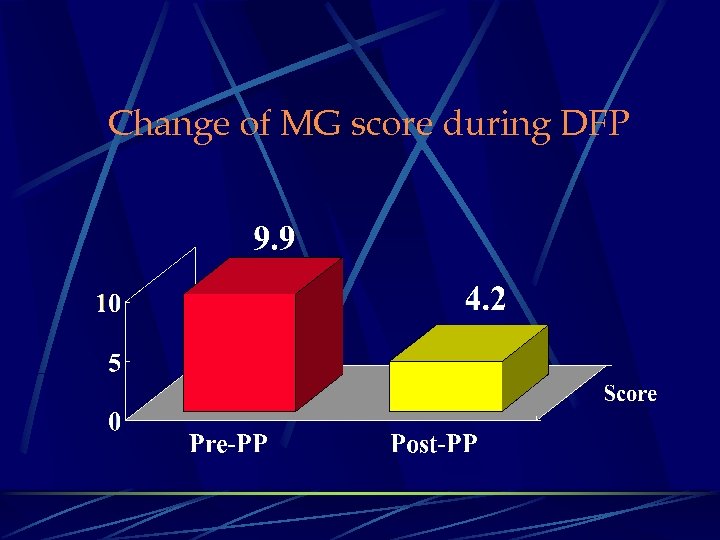 Change of MG score during DFP
Change of MG score during DFP
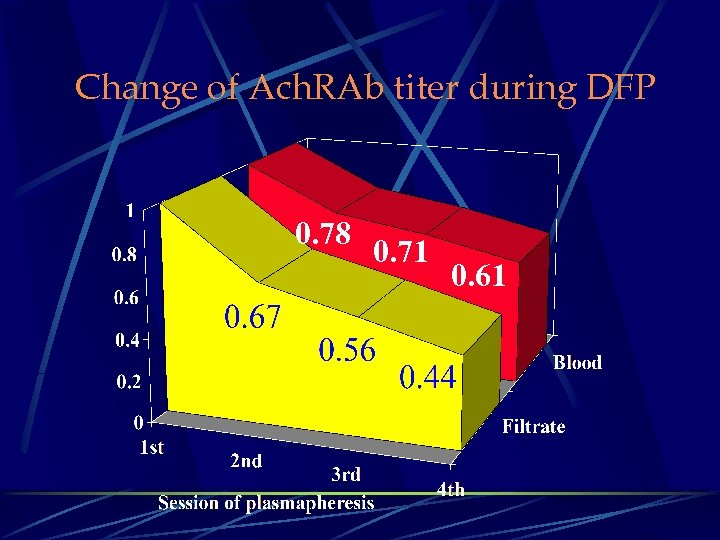 Change of Ach. RAb titer during DFP 0. 78 0. 71 0. 61
Change of Ach. RAb titer during DFP 0. 78 0. 71 0. 61
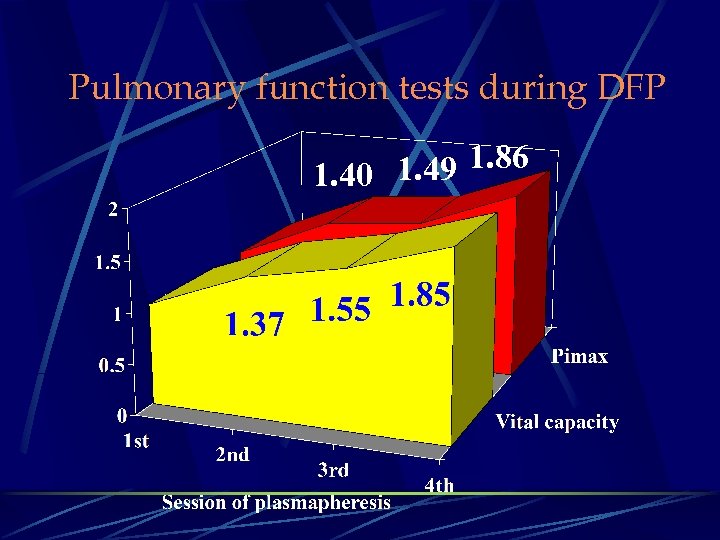 Pulmonary function tests during DFP 1. 49 1. 86 1. 40
Pulmonary function tests during DFP 1. 49 1. 86 1. 40
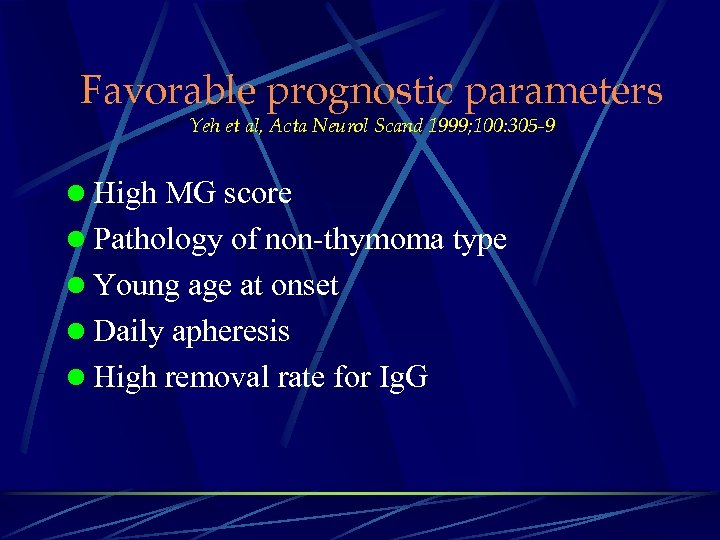 Favorable prognostic parameters Yeh et al, Acta Neurol Scand 1999; 100: 305 -9 l High MG score l Pathology of non-thymoma type l Young age at onset l Daily apheresis l High removal rate for Ig. G
Favorable prognostic parameters Yeh et al, Acta Neurol Scand 1999; 100: 305 -9 l High MG score l Pathology of non-thymoma type l Young age at onset l Daily apheresis l High removal rate for Ig. G
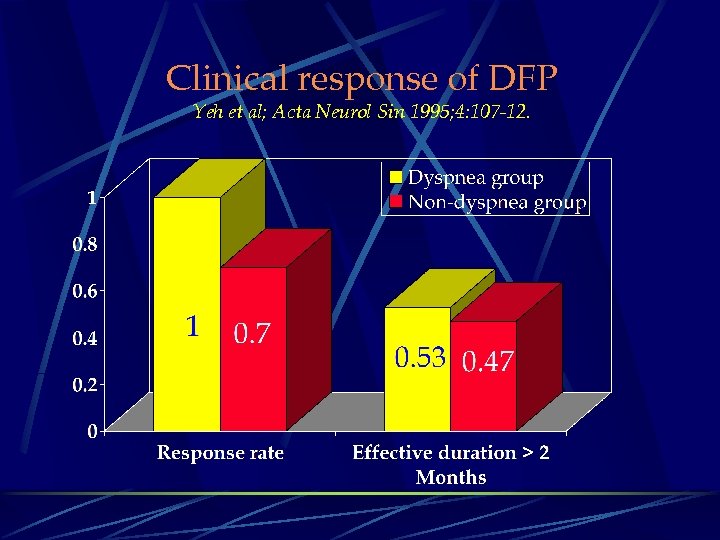 Clinical response of DFP Yeh et al; Acta Neurol Sin 1995; 4: 107 -12.
Clinical response of DFP Yeh et al; Acta Neurol Sin 1995; 4: 107 -12.
 Botulism
Botulism
 Botulinum Toxin l Clostridium botulinum l Gram positive bacilli l Spore producing l Anaerobic: obligate l Botulinum Toxin l Sequence homology (30% to 40%) to tetanus toxin l Produced as a protoxin with. MW 150 k. Da l 7 types of neurotoxin: A-G
Botulinum Toxin l Clostridium botulinum l Gram positive bacilli l Spore producing l Anaerobic: obligate l Botulinum Toxin l Sequence homology (30% to 40%) to tetanus toxin l Produced as a protoxin with. MW 150 k. Da l 7 types of neurotoxin: A-G
 Clinical Features - Botulism Type A l l l Most common outbreaks in Rocky Mountains & West Ca++ level in synaptosomes overcomes blockade More severe & long-lasting paralysis: 67% intubation Type B l l Most common outbreaks in East, especially Allegheny Has most structural homology to tetanus toxin Require assembled intracellular microtubule for action Somewhat less severe paralysis than Type A
Clinical Features - Botulism Type A l l l Most common outbreaks in Rocky Mountains & West Ca++ level in synaptosomes overcomes blockade More severe & long-lasting paralysis: 67% intubation Type B l l Most common outbreaks in East, especially Allegheny Has most structural homology to tetanus toxin Require assembled intracellular microtubule for action Somewhat less severe paralysis than Type A
 Clinical Features - Botulism Time course Incubation period: average: 18 to 38 hours l Extremes: 2 hours to 1 week l Weakness Diffuse; Usually symmetric; Proximal > distal l Bulbar: dysphagia; dysarthria l Extraocular: ptosis; EOM weakness Sensory loss: never prominent l Tendon reflexes: reduced
Clinical Features - Botulism Time course Incubation period: average: 18 to 38 hours l Extremes: 2 hours to 1 week l Weakness Diffuse; Usually symmetric; Proximal > distal l Bulbar: dysphagia; dysarthria l Extraocular: ptosis; EOM weakness Sensory loss: never prominent l Tendon reflexes: reduced
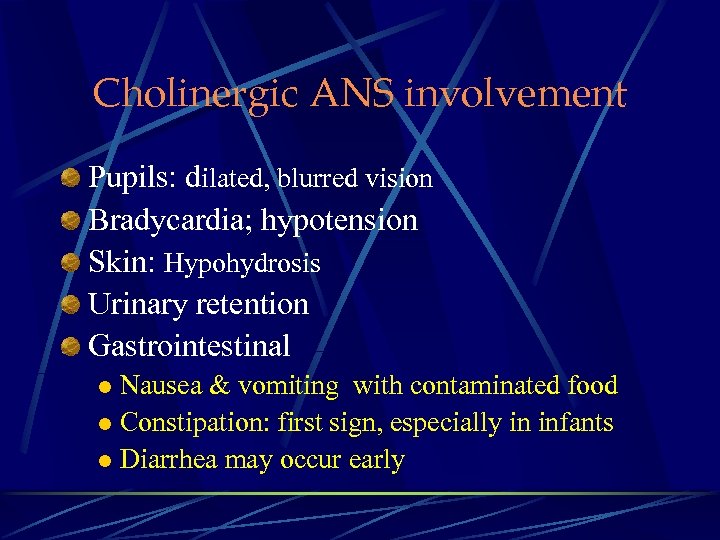 Cholinergic ANS involvement Pupils: dilated, blurred vision Bradycardia; hypotension Skin: Hypohydrosis Urinary retention Gastrointestinal Nausea & vomiting with contaminated food l Constipation: first sign, especially in infants l Diarrhea may occur early l
Cholinergic ANS involvement Pupils: dilated, blurred vision Bradycardia; hypotension Skin: Hypohydrosis Urinary retention Gastrointestinal Nausea & vomiting with contaminated food l Constipation: first sign, especially in infants l Diarrhea may occur early l
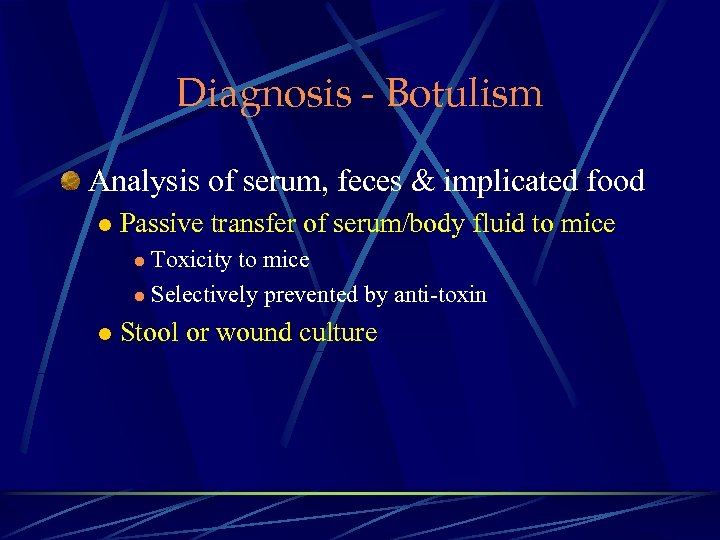 Diagnosis - Botulism Analysis of serum, feces & implicated food l Passive transfer of serum/body fluid to mice Toxicity to mice l Selectively prevented by anti-toxin l l Stool or wound culture
Diagnosis - Botulism Analysis of serum, feces & implicated food l Passive transfer of serum/body fluid to mice Toxicity to mice l Selectively prevented by anti-toxin l l Stool or wound culture
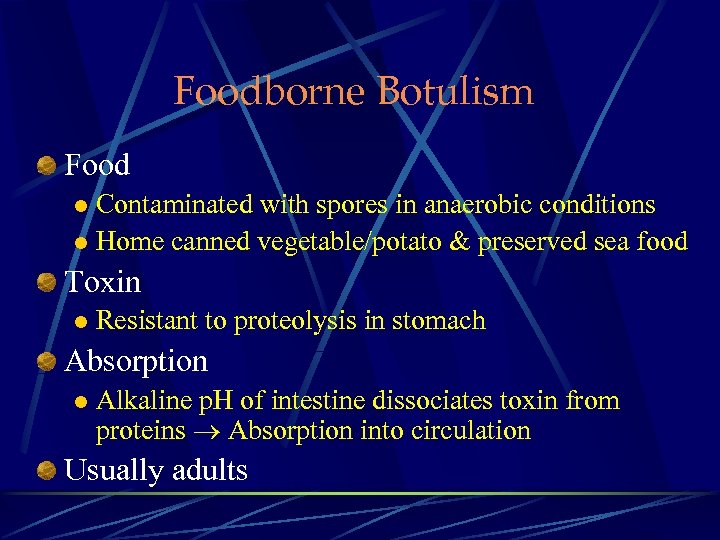 Foodborne Botulism Food Contaminated with spores in anaerobic conditions l Home canned vegetable/potato & preserved sea food l Toxin l Resistant to proteolysis in stomach Absorption l Alkaline p. H of intestine dissociates toxin from proteins Absorption into circulation Usually adults
Foodborne Botulism Food Contaminated with spores in anaerobic conditions l Home canned vegetable/potato & preserved sea food l Toxin l Resistant to proteolysis in stomach Absorption l Alkaline p. H of intestine dissociates toxin from proteins Absorption into circulation Usually adults
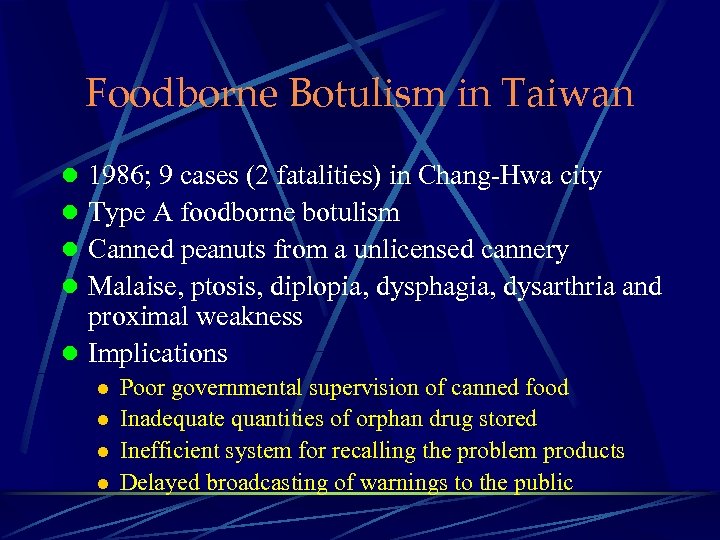 Foodborne Botulism in Taiwan l 1986; 9 cases (2 fatalities) in Chang-Hwa city l Type A foodborne botulism l Canned peanuts from a unlicensed cannery l Malaise, ptosis, diplopia, dysphagia, dysarthria and proximal weakness l Implications l l Poor governmental supervision of canned food Inadequate quantities of orphan drug stored Inefficient system for recalling the problem products Delayed broadcasting of warnings to the public
Foodborne Botulism in Taiwan l 1986; 9 cases (2 fatalities) in Chang-Hwa city l Type A foodborne botulism l Canned peanuts from a unlicensed cannery l Malaise, ptosis, diplopia, dysphagia, dysarthria and proximal weakness l Implications l l Poor governmental supervision of canned food Inadequate quantities of orphan drug stored Inefficient system for recalling the problem products Delayed broadcasting of warnings to the public
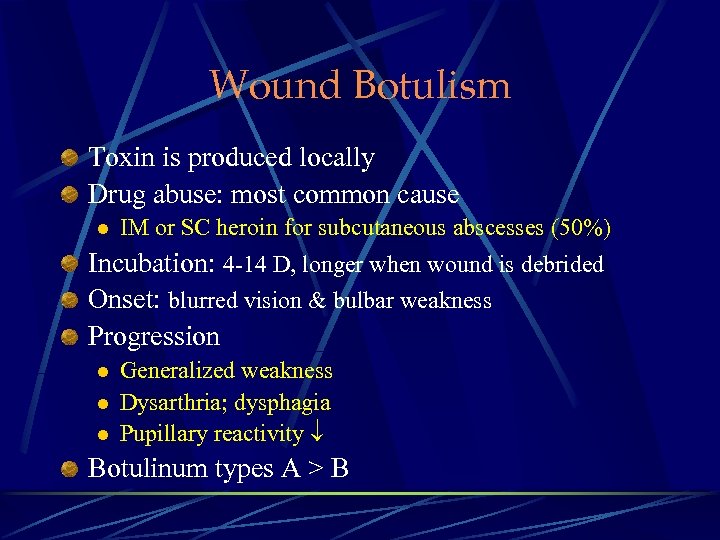 Wound Botulism Toxin is produced locally Drug abuse: most common cause l IM or SC heroin for subcutaneous abscesses (50%) Incubation: 4 -14 D, longer when wound is debrided Onset: blurred vision & bulbar weakness Progression l l l Generalized weakness Dysarthria; dysphagia Pupillary reactivity Botulinum types A > B
Wound Botulism Toxin is produced locally Drug abuse: most common cause l IM or SC heroin for subcutaneous abscesses (50%) Incubation: 4 -14 D, longer when wound is debrided Onset: blurred vision & bulbar weakness Progression l l l Generalized weakness Dysarthria; dysphagia Pupillary reactivity Botulinum types A > B
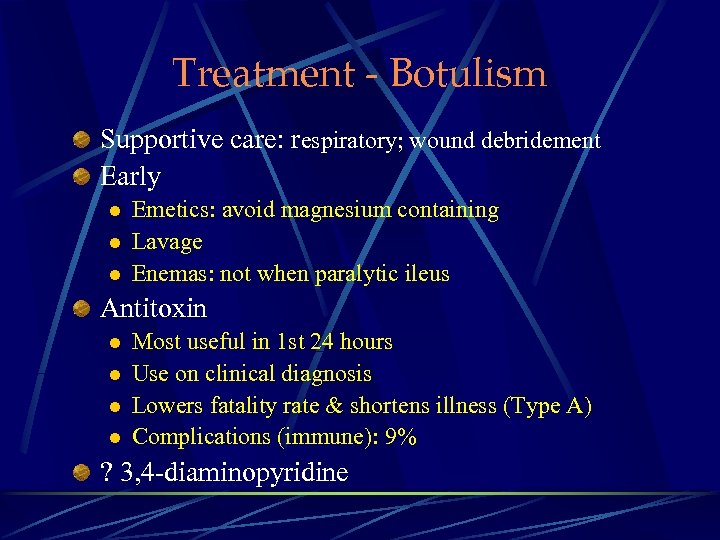 Treatment - Botulism Supportive care: respiratory; wound debridement Early l l l Emetics: avoid magnesium containing Lavage Enemas: not when paralytic ileus Antitoxin l l Most useful in 1 st 24 hours Use on clinical diagnosis Lowers fatality rate & shortens illness (Type A) Complications (immune): 9% ? 3, 4 -diaminopyridine
Treatment - Botulism Supportive care: respiratory; wound debridement Early l l l Emetics: avoid magnesium containing Lavage Enemas: not when paralytic ileus Antitoxin l l Most useful in 1 st 24 hours Use on clinical diagnosis Lowers fatality rate & shortens illness (Type A) Complications (immune): 9% ? 3, 4 -diaminopyridine
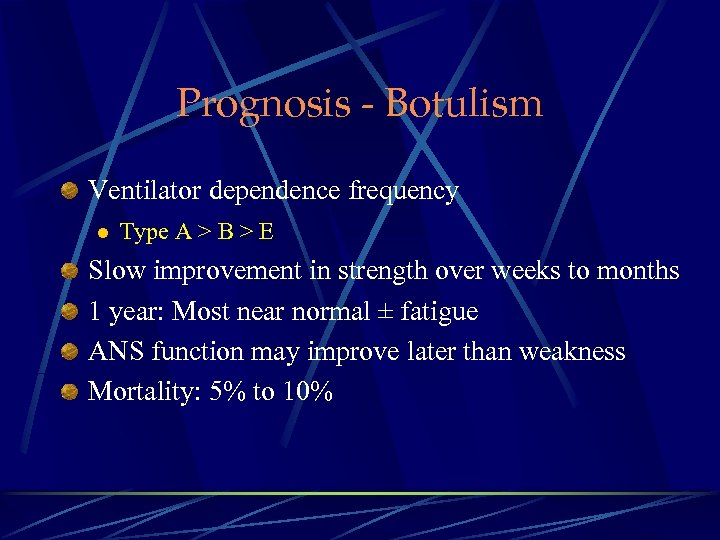 Prognosis - Botulism Ventilator dependence frequency l Type A > B > E Slow improvement in strength over weeks to months 1 year: Most near normal ± fatigue ANS function may improve later than weakness Mortality: 5% to 10%
Prognosis - Botulism Ventilator dependence frequency l Type A > B > E Slow improvement in strength over weeks to months 1 year: Most near normal ± fatigue ANS function may improve later than weakness Mortality: 5% to 10%
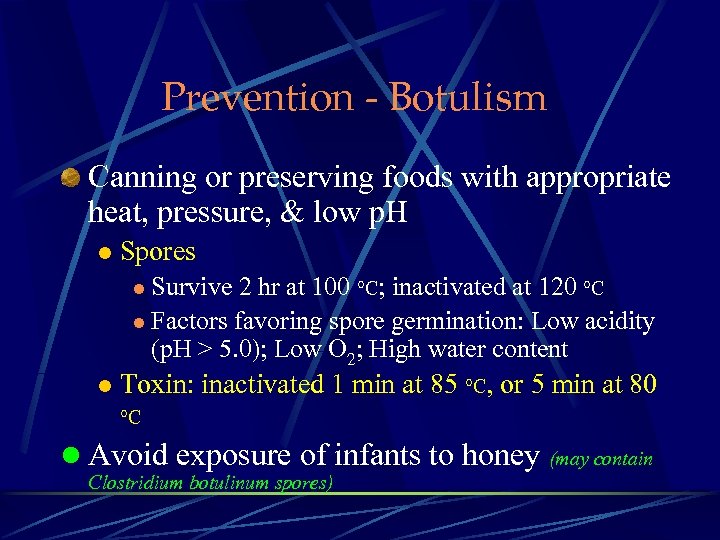 Prevention - Botulism Canning or preserving foods with appropriate heat, pressure, & low p. H l Spores l Survive 2 hr at 100 °C; inactivated at 120 °C l Factors favoring spore germination: Low acidity (p. H > 5. 0); Low O 2; High water content l Toxin: inactivated 1 min at 85 °C, or 5 min at 80 °C l Avoid exposure of infants to honey (may contain Clostridium botulinum spores)
Prevention - Botulism Canning or preserving foods with appropriate heat, pressure, & low p. H l Spores l Survive 2 hr at 100 °C; inactivated at 120 °C l Factors favoring spore germination: Low acidity (p. H > 5. 0); Low O 2; High water content l Toxin: inactivated 1 min at 85 °C, or 5 min at 80 °C l Avoid exposure of infants to honey (may contain Clostridium botulinum spores)
 Periodic Paralysis
Periodic Paralysis
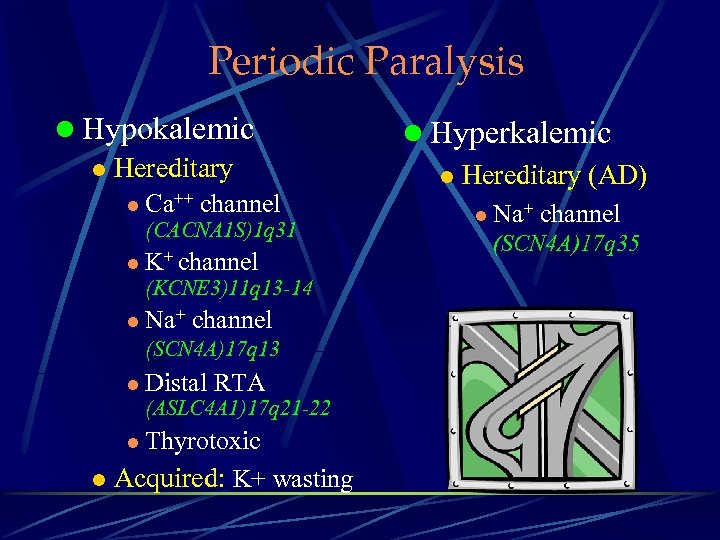 Periodic Paralysis l Hypokalemic l Hereditary l Ca++ channel (CACNA 1 S)1 q 31 l K+ channel (KCNE 3)11 q 13 -14 l Na+ channel (SCN 4 A)17 q 13 l Distal RTA (ASLC 4 A 1)17 q 21 -22 l Thyrotoxic l Acquired: K+ wasting l Hyperkalemic l Hereditary (AD) l Na+ channel (SCN 4 A)17 q 35
Periodic Paralysis l Hypokalemic l Hereditary l Ca++ channel (CACNA 1 S)1 q 31 l K+ channel (KCNE 3)11 q 13 -14 l Na+ channel (SCN 4 A)17 q 13 l Distal RTA (ASLC 4 A 1)17 q 21 -22 l Thyrotoxic l Acquired: K+ wasting l Hyperkalemic l Hereditary (AD) l Na+ channel (SCN 4 A)17 q 35
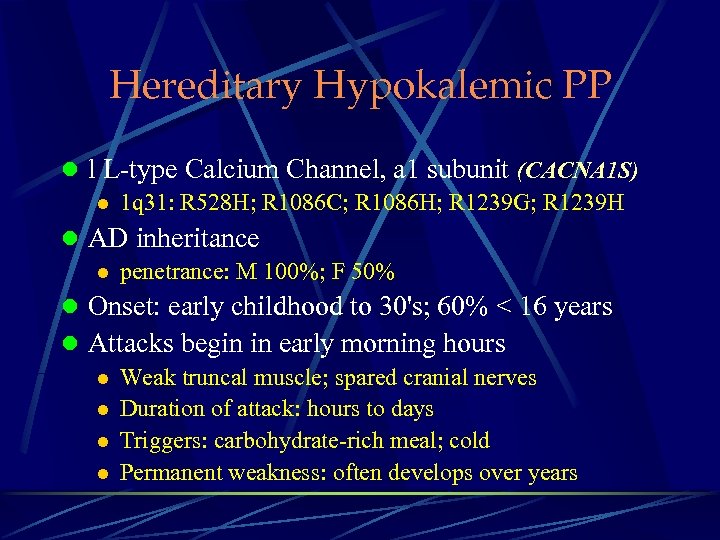 Hereditary Hypokalemic PP l l L-type Calcium Channel, a 1 subunit (CACNA 1 S) l 1 q 31: R 528 H; R 1086 C; R 1086 H; R 1239 G; R 1239 H l AD inheritance l penetrance: M 100%; F 50% l Onset: early childhood to 30's; 60% < 16 years l Attacks begin in early morning hours l Weak truncal muscle; spared cranial nerves l Duration of attack: hours to days l Triggers: carbohydrate-rich meal; cold l Permanent weakness: often develops over years
Hereditary Hypokalemic PP l l L-type Calcium Channel, a 1 subunit (CACNA 1 S) l 1 q 31: R 528 H; R 1086 C; R 1086 H; R 1239 G; R 1239 H l AD inheritance l penetrance: M 100%; F 50% l Onset: early childhood to 30's; 60% < 16 years l Attacks begin in early morning hours l Weak truncal muscle; spared cranial nerves l Duration of attack: hours to days l Triggers: carbohydrate-rich meal; cold l Permanent weakness: often develops over years
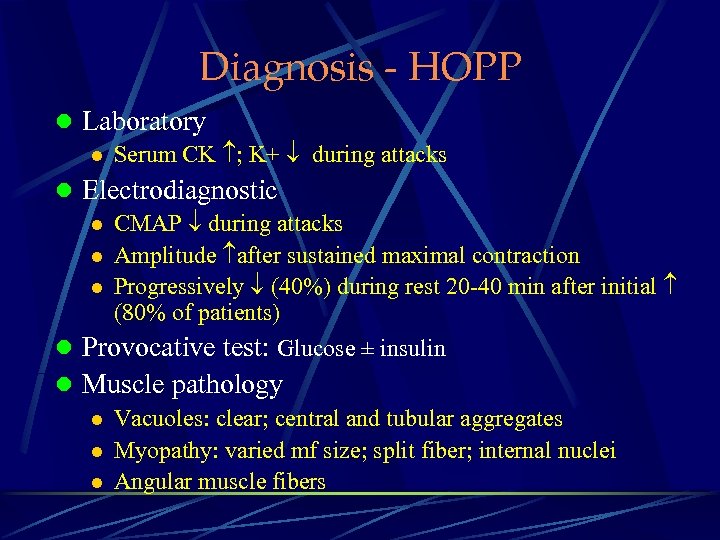 Diagnosis - HOPP l Laboratory l Serum CK ; K+ during attacks l Electrodiagnostic l CMAP during attacks l Amplitude after sustained maximal contraction l Progressively (40%) during rest 20 -40 min after initial (80% of patients) l Provocative test: Glucose ± insulin l Muscle pathology l Vacuoles: clear; central and tubular aggregates l Myopathy: varied mf size; split fiber; internal nuclei l Angular muscle fibers
Diagnosis - HOPP l Laboratory l Serum CK ; K+ during attacks l Electrodiagnostic l CMAP during attacks l Amplitude after sustained maximal contraction l Progressively (40%) during rest 20 -40 min after initial (80% of patients) l Provocative test: Glucose ± insulin l Muscle pathology l Vacuoles: clear; central and tubular aggregates l Myopathy: varied mf size; split fiber; internal nuclei l Angular muscle fibers
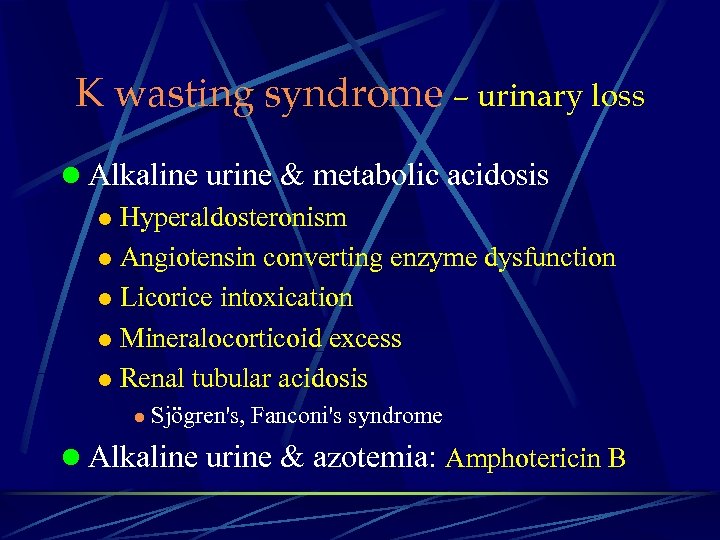 K wasting syndrome – urinary loss l Alkaline urine & metabolic acidosis l Hyperaldosteronism l Angiotensin converting enzyme dysfunction l Licorice intoxication l Mineralocorticoid excess l Renal tubular acidosis l Sjögren's, Fanconi's syndrome l Alkaline urine & azotemia: Amphotericin B
K wasting syndrome – urinary loss l Alkaline urine & metabolic acidosis l Hyperaldosteronism l Angiotensin converting enzyme dysfunction l Licorice intoxication l Mineralocorticoid excess l Renal tubular acidosis l Sjögren's, Fanconi's syndrome l Alkaline urine & azotemia: Amphotericin B
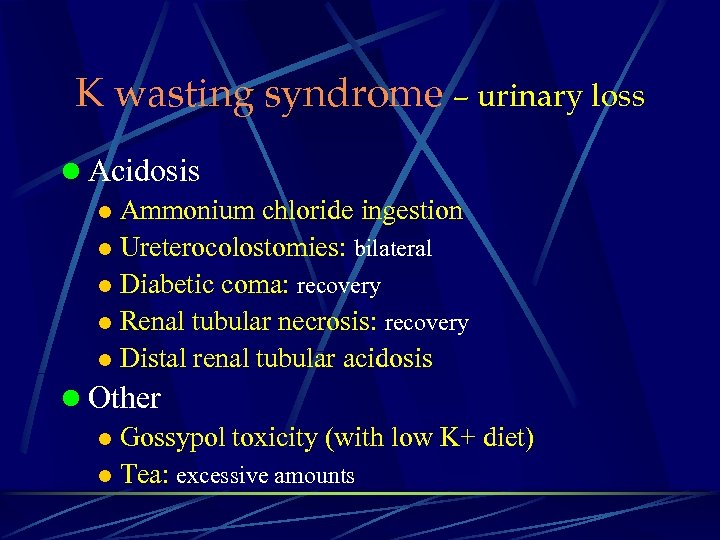 K wasting syndrome – urinary loss l Acidosis l Ammonium chloride ingestion l Ureterocolostomies: bilateral l Diabetic coma: recovery l Renal tubular necrosis: recovery l Distal renal tubular acidosis l Other l Gossypol toxicity (with low K+ diet) l Tea: excessive amounts
K wasting syndrome – urinary loss l Acidosis l Ammonium chloride ingestion l Ureterocolostomies: bilateral l Diabetic coma: recovery l Renal tubular necrosis: recovery l Distal renal tubular acidosis l Other l Gossypol toxicity (with low K+ diet) l Tea: excessive amounts
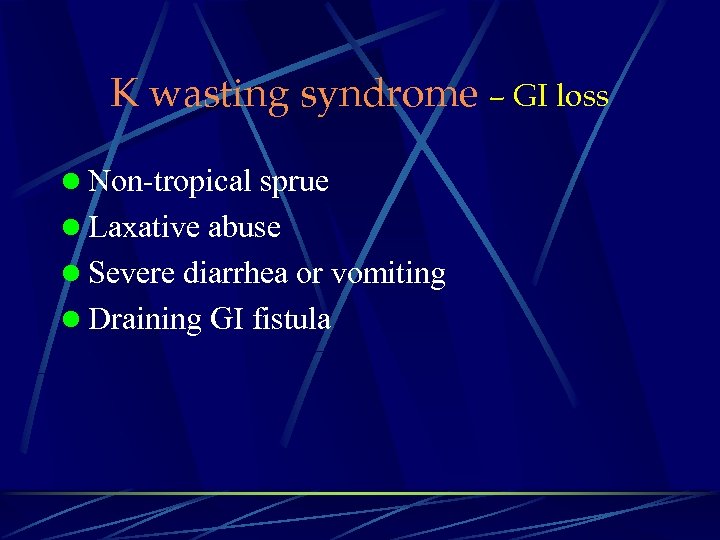 K wasting syndrome – GI loss l Non-tropical sprue l Laxative abuse l Severe diarrhea or vomiting l Draining GI fistula
K wasting syndrome – GI loss l Non-tropical sprue l Laxative abuse l Severe diarrhea or vomiting l Draining GI fistula
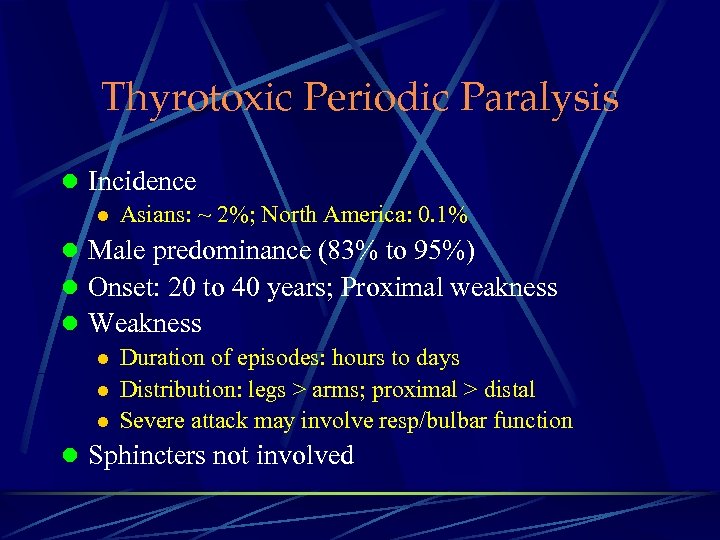 Thyrotoxic Periodic Paralysis l Incidence l Asians: ~ 2%; North America: 0. 1% l Male predominance (83% to 95%) l Onset: 20 to 40 years; Proximal weakness l Weakness l Duration of episodes: hours to days l Distribution: legs > arms; proximal > distal l Severe attack may involve resp/bulbar function l Sphincters not involved
Thyrotoxic Periodic Paralysis l Incidence l Asians: ~ 2%; North America: 0. 1% l Male predominance (83% to 95%) l Onset: 20 to 40 years; Proximal weakness l Weakness l Duration of episodes: hours to days l Distribution: legs > arms; proximal > distal l Severe attack may involve resp/bulbar function l Sphincters not involved
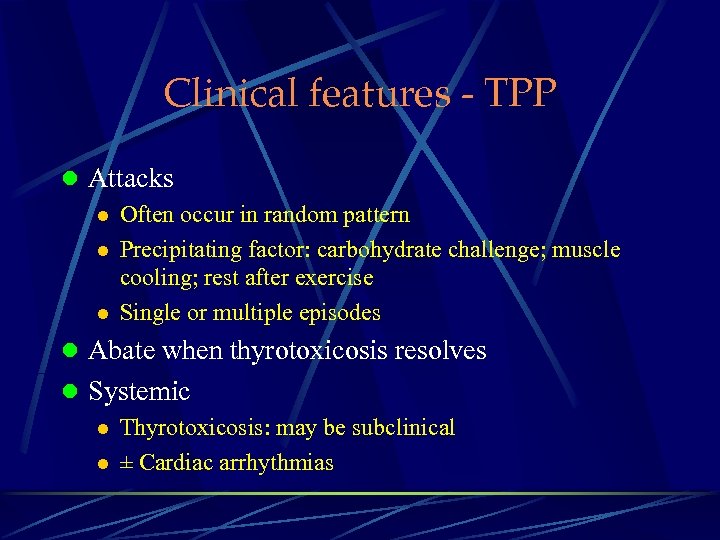 Clinical features - TPP l Attacks l Often occur in random pattern l Precipitating factor: carbohydrate challenge; muscle cooling; rest after exercise l Single or multiple episodes l Abate when thyrotoxicosis resolves l Systemic l Thyrotoxicosis: may be subclinical l ± Cardiac arrhythmias
Clinical features - TPP l Attacks l Often occur in random pattern l Precipitating factor: carbohydrate challenge; muscle cooling; rest after exercise l Single or multiple episodes l Abate when thyrotoxicosis resolves l Systemic l Thyrotoxicosis: may be subclinical l ± Cardiac arrhythmias
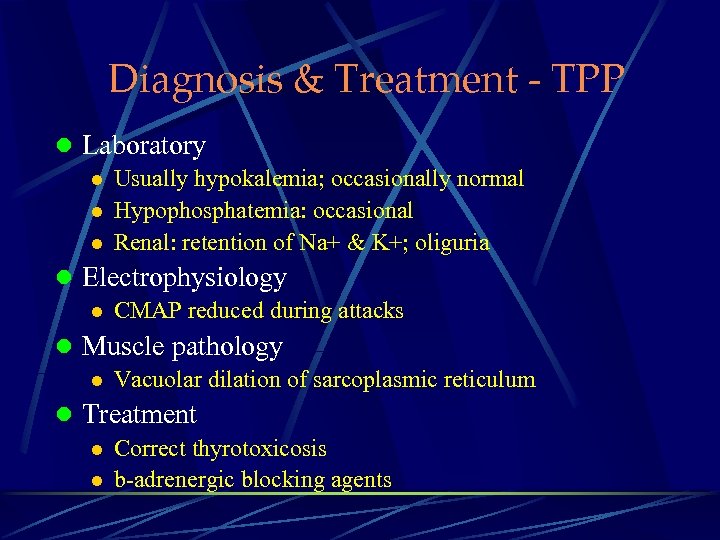 Diagnosis & Treatment - TPP l Laboratory l Usually hypokalemia; occasionally normal l Hypophosphatemia: occasional l Renal: retention of Na+ & K+; oliguria l Electrophysiology l CMAP reduced during attacks l Muscle pathology l Vacuolar dilation of sarcoplasmic reticulum l Treatment l Correct thyrotoxicosis l b-adrenergic blocking agents
Diagnosis & Treatment - TPP l Laboratory l Usually hypokalemia; occasionally normal l Hypophosphatemia: occasional l Renal: retention of Na+ & K+; oliguria l Electrophysiology l CMAP reduced during attacks l Muscle pathology l Vacuolar dilation of sarcoplasmic reticulum l Treatment l Correct thyrotoxicosis l b-adrenergic blocking agents
 Polymyositis
Polymyositis
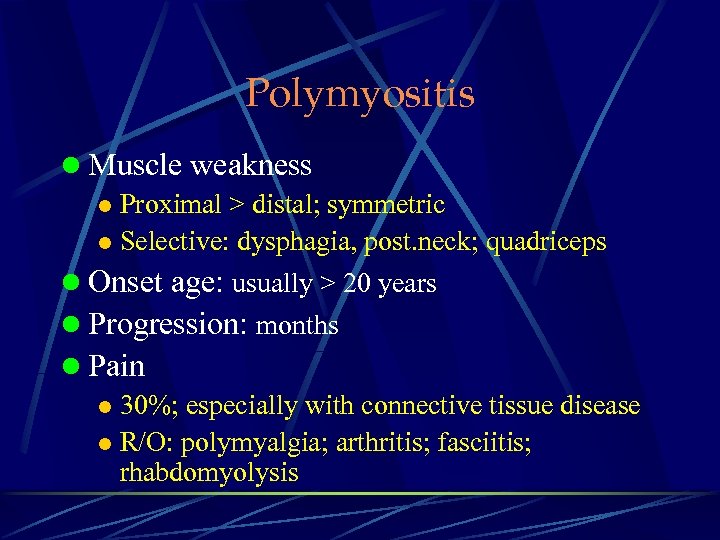 Polymyositis l Muscle weakness l Proximal > distal; symmetric l Selective: dysphagia, post. neck; quadriceps l Onset age: usually > 20 years l Progression: months l Pain l 30%; especially with connective tissue disease l R/O: polymyalgia; arthritis; fasciitis; rhabdomyolysis
Polymyositis l Muscle weakness l Proximal > distal; symmetric l Selective: dysphagia, post. neck; quadriceps l Onset age: usually > 20 years l Progression: months l Pain l 30%; especially with connective tissue disease l R/O: polymyalgia; arthritis; fasciitis; rhabdomyolysis
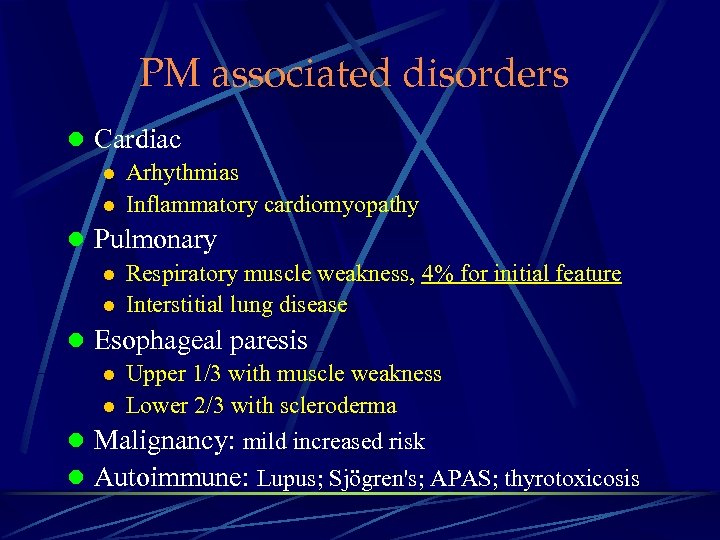 PM associated disorders l Cardiac l Arhythmias l Inflammatory cardiomyopathy l Pulmonary l Respiratory muscle weakness, 4% for initial feature l Interstitial lung disease l Esophageal paresis l Upper 1/3 with muscle weakness l Lower 2/3 with scleroderma l Malignancy: mild increased risk l Autoimmune: Lupus; Sjögren's; APAS; thyrotoxicosis
PM associated disorders l Cardiac l Arhythmias l Inflammatory cardiomyopathy l Pulmonary l Respiratory muscle weakness, 4% for initial feature l Interstitial lung disease l Esophageal paresis l Upper 1/3 with muscle weakness l Lower 2/3 with scleroderma l Malignancy: mild increased risk l Autoimmune: Lupus; Sjögren's; APAS; thyrotoxicosis
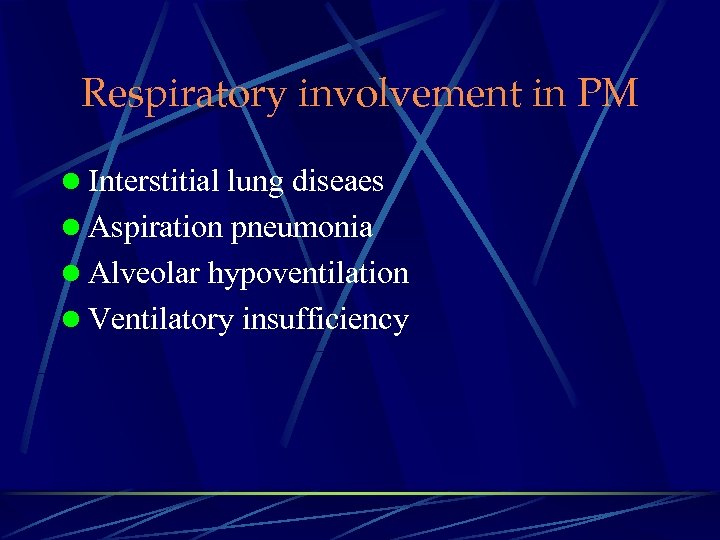 Respiratory involvement in PM l Interstitial lung diseaes l Aspiration pneumonia l Alveolar hypoventilation l Ventilatory insufficiency
Respiratory involvement in PM l Interstitial lung diseaes l Aspiration pneumonia l Alveolar hypoventilation l Ventilatory insufficiency
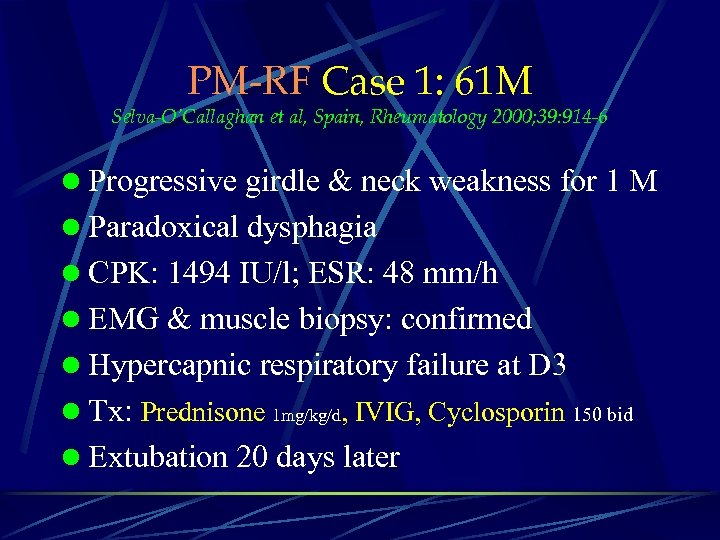 PM-RF Case 1: 61 M Selva-O’Callaghan et al, Spain, Rheumatology 2000; 39: 914 -6 l Progressive girdle & neck weakness for 1 M l Paradoxical dysphagia l CPK: 1494 IU/l; ESR: 48 mm/h l EMG & muscle biopsy: confirmed l Hypercapnic respiratory failure at D 3 l Tx: Prednisone 1 mg/kg/d, IVIG, Cyclosporin 150 bid l Extubation 20 days later
PM-RF Case 1: 61 M Selva-O’Callaghan et al, Spain, Rheumatology 2000; 39: 914 -6 l Progressive girdle & neck weakness for 1 M l Paradoxical dysphagia l CPK: 1494 IU/l; ESR: 48 mm/h l EMG & muscle biopsy: confirmed l Hypercapnic respiratory failure at D 3 l Tx: Prednisone 1 mg/kg/d, IVIG, Cyclosporin 150 bid l Extubation 20 days later
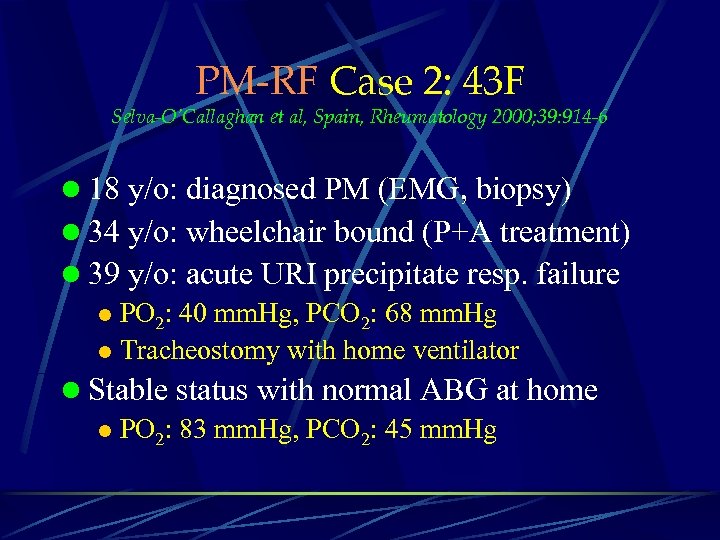 PM-RF Case 2: 43 F Selva-O’Callaghan et al, Spain, Rheumatology 2000; 39: 914 -6 l 18 y/o: diagnosed PM (EMG, biopsy) l 34 y/o: wheelchair bound (P+A treatment) l 39 y/o: acute URI precipitate resp. failure l PO 2: 40 mm. Hg, PCO 2: 68 mm. Hg l Tracheostomy with home ventilator l Stable status with normal ABG at home l PO 2: 83 mm. Hg, PCO 2: 45 mm. Hg
PM-RF Case 2: 43 F Selva-O’Callaghan et al, Spain, Rheumatology 2000; 39: 914 -6 l 18 y/o: diagnosed PM (EMG, biopsy) l 34 y/o: wheelchair bound (P+A treatment) l 39 y/o: acute URI precipitate resp. failure l PO 2: 40 mm. Hg, PCO 2: 68 mm. Hg l Tracheostomy with home ventilator l Stable status with normal ABG at home l PO 2: 83 mm. Hg, PCO 2: 45 mm. Hg
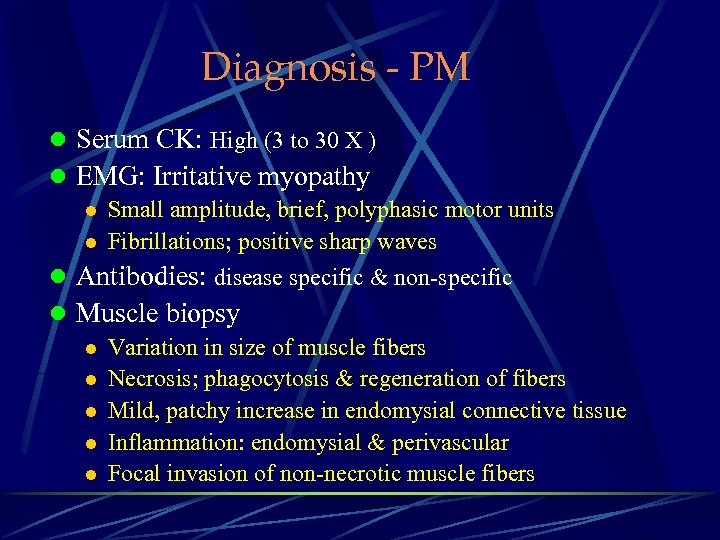 Diagnosis - PM l Serum CK: High (3 to 30 X ) l EMG: Irritative myopathy l Small amplitude, brief, polyphasic motor units l Fibrillations; positive sharp waves l Antibodies: disease specific & non-specific l Muscle biopsy l Variation in size of muscle fibers l Necrosis; phagocytosis & regeneration of fibers l Mild, patchy increase in endomysial connective tissue l Inflammation: endomysial & perivascular l Focal invasion of non-necrotic muscle fibers
Diagnosis - PM l Serum CK: High (3 to 30 X ) l EMG: Irritative myopathy l Small amplitude, brief, polyphasic motor units l Fibrillations; positive sharp waves l Antibodies: disease specific & non-specific l Muscle biopsy l Variation in size of muscle fibers l Necrosis; phagocytosis & regeneration of fibers l Mild, patchy increase in endomysial connective tissue l Inflammation: endomysial & perivascular l Focal invasion of non-necrotic muscle fibers
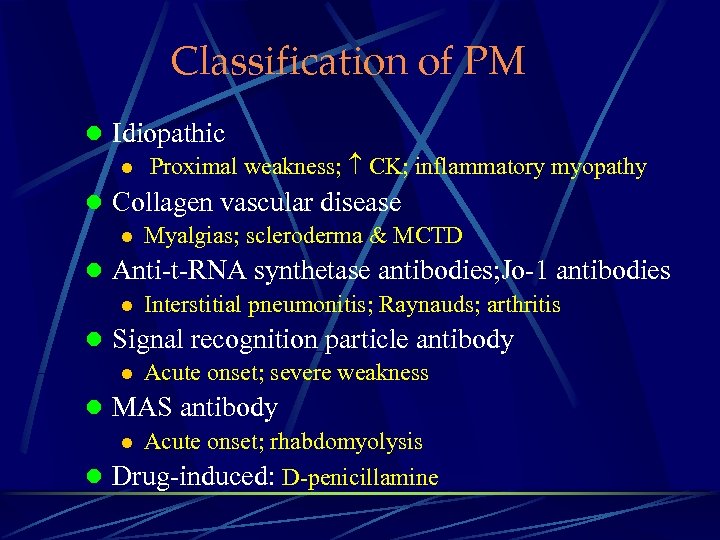 Classification of PM l Idiopathic l Proximal weakness; CK; inflammatory myopathy l Collagen vascular disease l Myalgias; scleroderma & MCTD l Anti-t-RNA synthetase antibodies; Jo-1 antibodies l Interstitial pneumonitis; Raynauds; arthritis l Signal recognition particle antibody l Acute onset; severe weakness l MAS antibody l Acute onset; rhabdomyolysis l Drug-induced: D-penicillamine
Classification of PM l Idiopathic l Proximal weakness; CK; inflammatory myopathy l Collagen vascular disease l Myalgias; scleroderma & MCTD l Anti-t-RNA synthetase antibodies; Jo-1 antibodies l Interstitial pneumonitis; Raynauds; arthritis l Signal recognition particle antibody l Acute onset; severe weakness l MAS antibody l Acute onset; rhabdomyolysis l Drug-induced: D-penicillamine
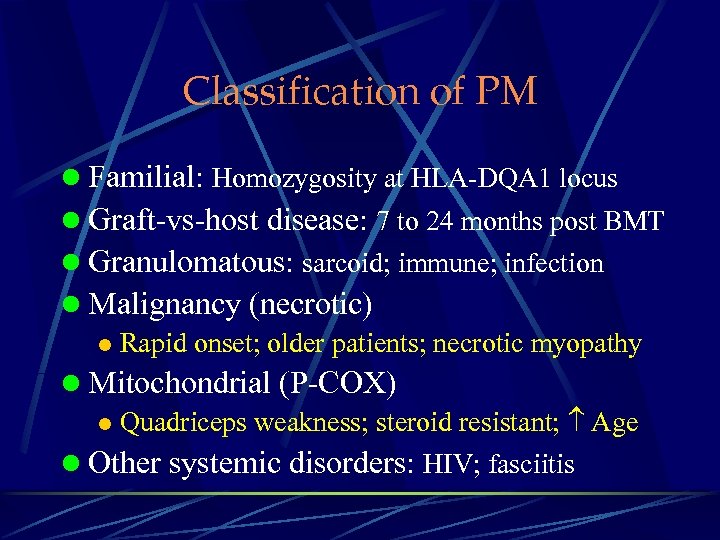 Classification of PM l Familial: Homozygosity at HLA-DQA 1 locus l Graft-vs-host disease: 7 to 24 months post BMT l Granulomatous: sarcoid; immune; infection l Malignancy (necrotic) l Rapid onset; older patients; necrotic myopathy l Mitochondrial (P-COX) l Quadriceps weakness; steroid resistant; Age l Other systemic disorders: HIV; fasciitis
Classification of PM l Familial: Homozygosity at HLA-DQA 1 locus l Graft-vs-host disease: 7 to 24 months post BMT l Granulomatous: sarcoid; immune; infection l Malignancy (necrotic) l Rapid onset; older patients; necrotic myopathy l Mitochondrial (P-COX) l Quadriceps weakness; steroid resistant; Age l Other systemic disorders: HIV; fasciitis
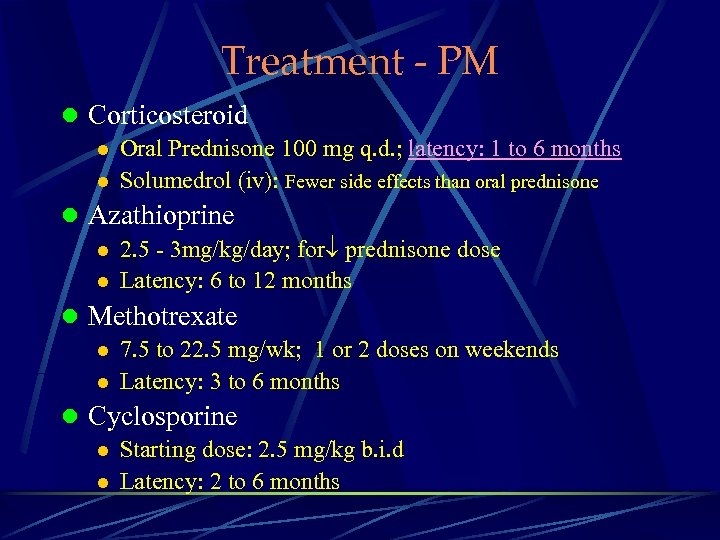 Treatment - PM l Corticosteroid l Oral Prednisone 100 mg q. d. ; latency: 1 to 6 months l Solumedrol (iv): Fewer side effects than oral prednisone l Azathioprine l 2. 5 - 3 mg/kg/day; for prednisone dose l Latency: 6 to 12 months l Methotrexate l 7. 5 to 22. 5 mg/wk; 1 or 2 doses on weekends l Latency: 3 to 6 months l Cyclosporine l Starting dose: 2. 5 mg/kg b. i. d l Latency: 2 to 6 months
Treatment - PM l Corticosteroid l Oral Prednisone 100 mg q. d. ; latency: 1 to 6 months l Solumedrol (iv): Fewer side effects than oral prednisone l Azathioprine l 2. 5 - 3 mg/kg/day; for prednisone dose l Latency: 6 to 12 months l Methotrexate l 7. 5 to 22. 5 mg/wk; 1 or 2 doses on weekends l Latency: 3 to 6 months l Cyclosporine l Starting dose: 2. 5 mg/kg b. i. d l Latency: 2 to 6 months
 Case Demonstration
Case Demonstration
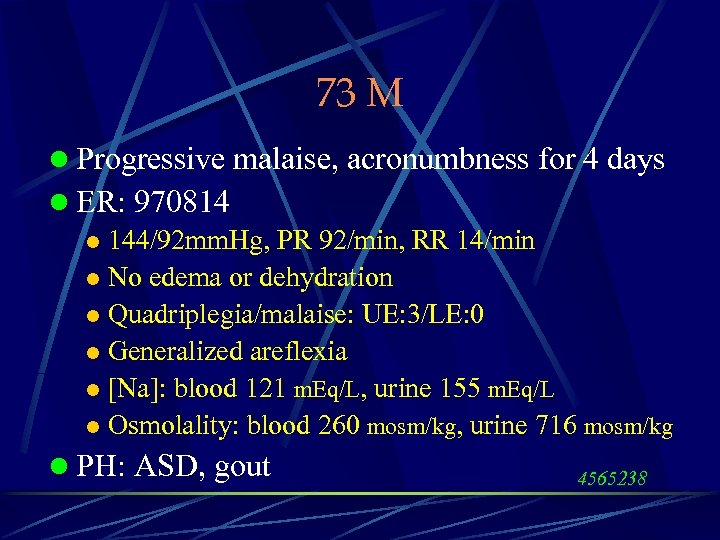 73 M l Progressive malaise, acronumbness for 4 days l ER: 970814 l 144/92 mm. Hg, PR 92/min, RR 14/min l No edema or dehydration l Quadriplegia/malaise: UE: 3/LE: 0 l Generalized areflexia l [Na]: blood 121 m. Eq/L, urine 155 m. Eq/L l Osmolality: blood 260 mosm/kg, urine 716 mosm/kg l PH: ASD, gout 4565238
73 M l Progressive malaise, acronumbness for 4 days l ER: 970814 l 144/92 mm. Hg, PR 92/min, RR 14/min l No edema or dehydration l Quadriplegia/malaise: UE: 3/LE: 0 l Generalized areflexia l [Na]: blood 121 m. Eq/L, urine 155 m. Eq/L l Osmolality: blood 260 mosm/kg, urine 716 mosm/kg l PH: ASD, gout 4565238
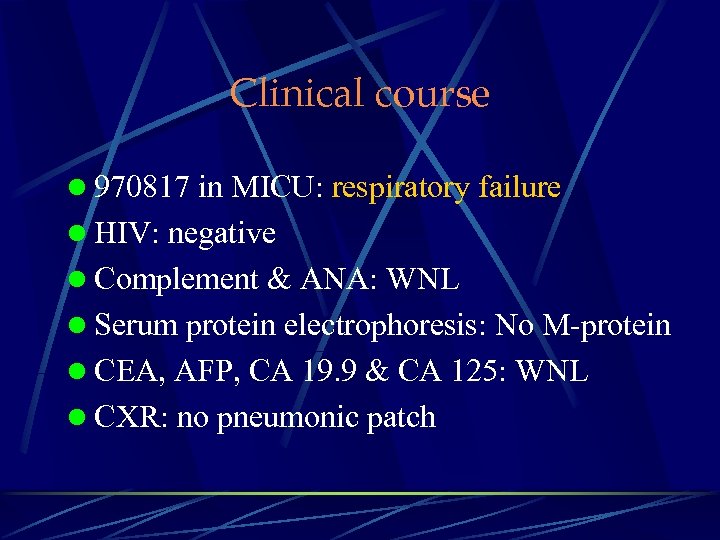 Clinical course l 970817 in MICU: respiratory failure l HIV: negative l Complement & ANA: WNL l Serum protein electrophoresis: No M-protein l CEA, AFP, CA 19. 9 & CA 125: WNL l CXR: no pneumonic patch
Clinical course l 970817 in MICU: respiratory failure l HIV: negative l Complement & ANA: WNL l Serum protein electrophoresis: No M-protein l CEA, AFP, CA 19. 9 & CA 125: WNL l CXR: no pneumonic patch
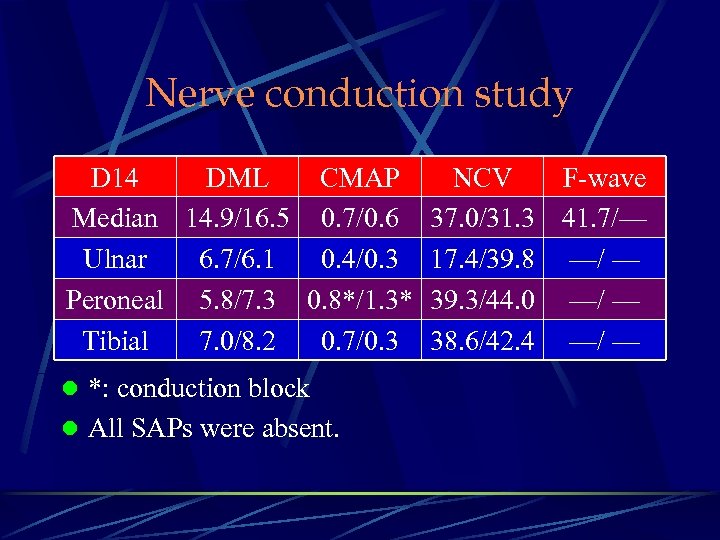 Nerve conduction study D 14 DML CMAP NCV F-wave Median 14. 9/16. 5 0. 7/0. 6 37. 0/31. 3 41. 7/— Ulnar 6. 7/6. 1 0. 4/0. 3 17. 4/39. 8 —/ — Peroneal 5. 8/7. 3 0. 8*/1. 3* 39. 3/44. 0 —/ — Tibial 7. 0/8. 2 0. 7/0. 3 38. 6/42. 4 —/ — l *: conduction block l All SAPs were absent.
Nerve conduction study D 14 DML CMAP NCV F-wave Median 14. 9/16. 5 0. 7/0. 6 37. 0/31. 3 41. 7/— Ulnar 6. 7/6. 1 0. 4/0. 3 17. 4/39. 8 —/ — Peroneal 5. 8/7. 3 0. 8*/1. 3* 39. 3/44. 0 —/ — Tibial 7. 0/8. 2 0. 7/0. 3 38. 6/42. 4 —/ — l *: conduction block l All SAPs were absent.
 SIADH 6 4 2 8/ 9/
SIADH 6 4 2 8/ 9/
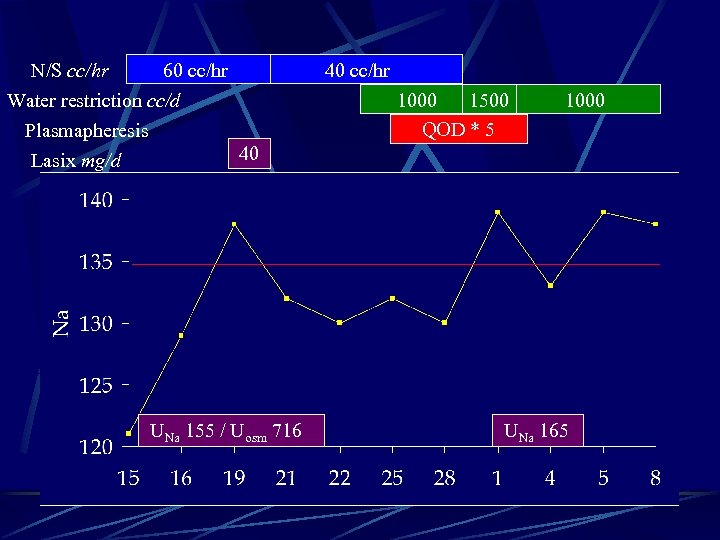 N/S cc/hr 60 cc/hr Water restriction cc/d Plasmapheresis 40 Lasix mg/d UNa 155 / Uosm 716 40 cc/hr 1000 1500 QOD * 5 1000 UNa 165
N/S cc/hr 60 cc/hr Water restriction cc/d Plasmapheresis 40 Lasix mg/d UNa 155 / Uosm 716 40 cc/hr 1000 1500 QOD * 5 1000 UNa 165
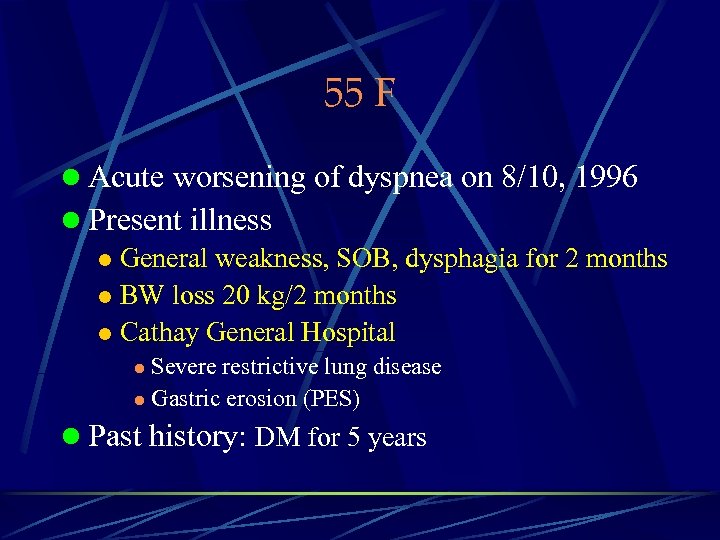 55 F l Acute worsening of dyspnea on 8/10, 1996 l Present illness l General weakness, SOB, dysphagia for 2 months l BW loss 20 kg/2 months l Cathay General Hospital Severe restrictive lung disease l Gastric erosion (PES) l l Past history: DM for 5 years
55 F l Acute worsening of dyspnea on 8/10, 1996 l Present illness l General weakness, SOB, dysphagia for 2 months l BW loss 20 kg/2 months l Cathay General Hospital Severe restrictive lung disease l Gastric erosion (PES) l l Past history: DM for 5 years
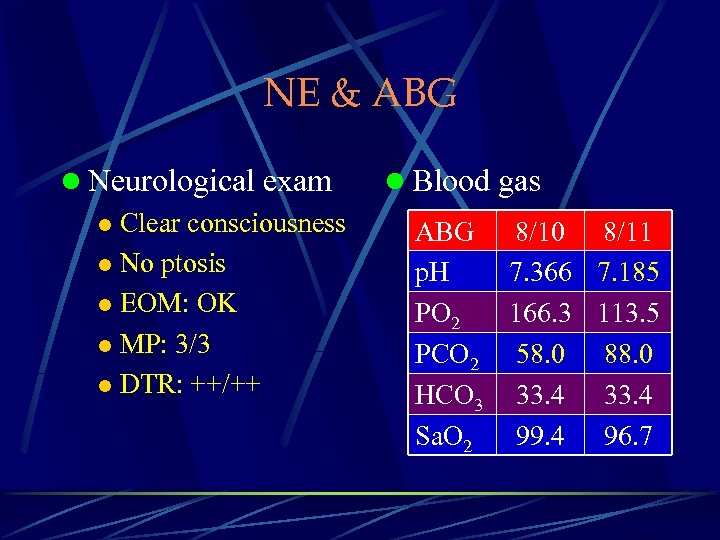 NE & ABG l Neurological exam l Clear consciousness l No ptosis l EOM: OK l MP: 3/3 l DTR: ++/++ l Blood gas ABG 8/10 8/11 p. H 7. 366 7. 185 PO 2 166. 3 113. 5 PCO 2 58. 0 88. 0 HCO 3 33. 4 Sa. O 2 99. 4 96. 7
NE & ABG l Neurological exam l Clear consciousness l No ptosis l EOM: OK l MP: 3/3 l DTR: ++/++ l Blood gas ABG 8/10 8/11 p. H 7. 366 7. 185 PO 2 166. 3 113. 5 PCO 2 58. 0 88. 0 HCO 3 33. 4 Sa. O 2 99. 4 96. 7
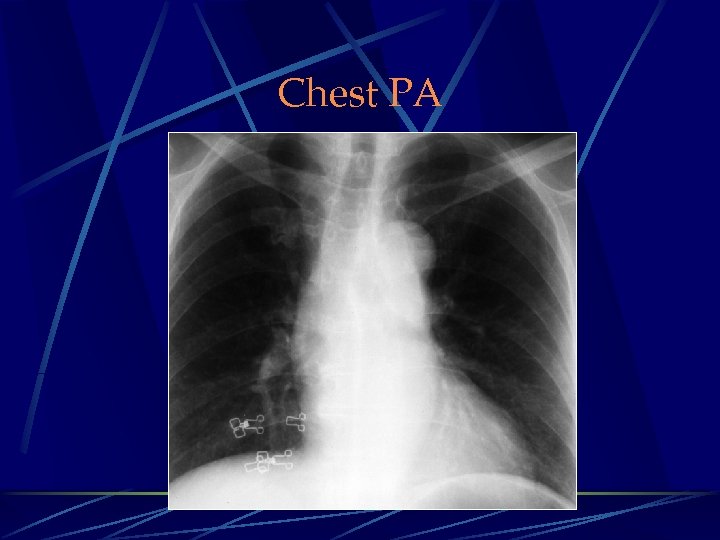 Chest PA
Chest PA
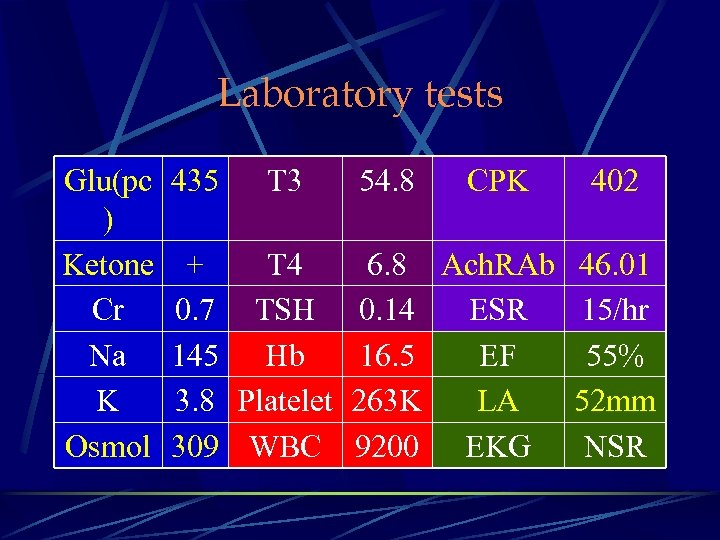 Laboratory tests Glu(pc ) Ketone Cr Na K Osmol 435 T 3 54. 8 CPK 402 + T 4 6. 8 Ach. RAb 46. 01 0. 7 TSH 0. 14 ESR 15/hr 145 Hb 16. 5 EF 55% 3. 8 Platelet 263 K LA 52 mm 309 WBC 9200 EKG NSR
Laboratory tests Glu(pc ) Ketone Cr Na K Osmol 435 T 3 54. 8 CPK 402 + T 4 6. 8 Ach. RAb 46. 01 0. 7 TSH 0. 14 ESR 15/hr 145 Hb 16. 5 EF 55% 3. 8 Platelet 263 K LA 52 mm 309 WBC 9200 EKG NSR
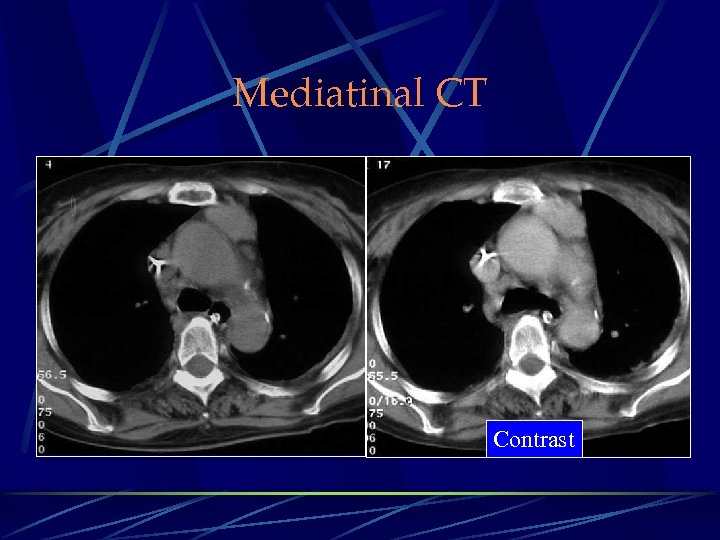 Mediatinal CT Contrast
Mediatinal CT Contrast


