94b0cc0fd733bf41045db150170746b9.ppt
- Количество слайдов: 45
Neurology Intern Boot Camp BRYAN BONDER
Objectives 1) Review the neurological exam 2) Learn to recognize neurological emergencies 3) Learn the initial management of neurological emergencies
Localization Central ◦ Brain ◦ Spinal cord Peripheral ◦ ◦ ◦ Nerve root Plexus Peripheral nerve Neuromuscular junction Muscle Must distinguish central lesion from a peripheral lesion!
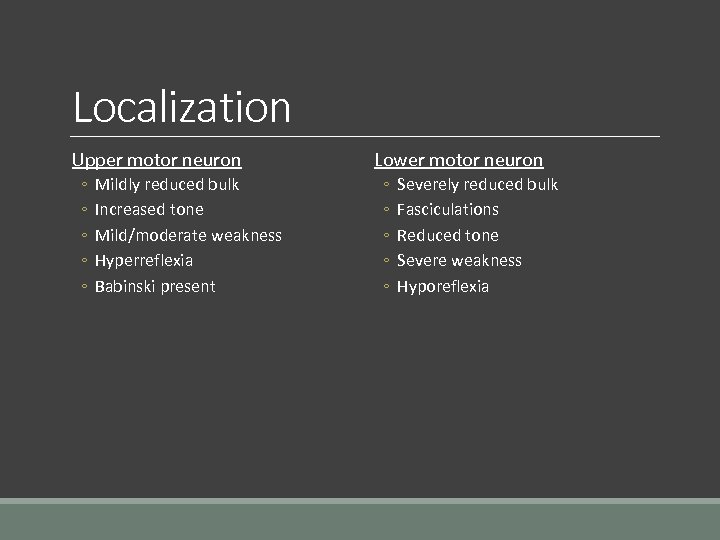
Localization Upper motor neuron ◦ ◦ ◦ Mildly reduced bulk Increased tone Mild/moderate weakness Hyperreflexia Babinski present Lower motor neuron ◦ ◦ ◦ Severely reduced bulk Fasciculations Reduced tone Severe weakness Hyporeflexia
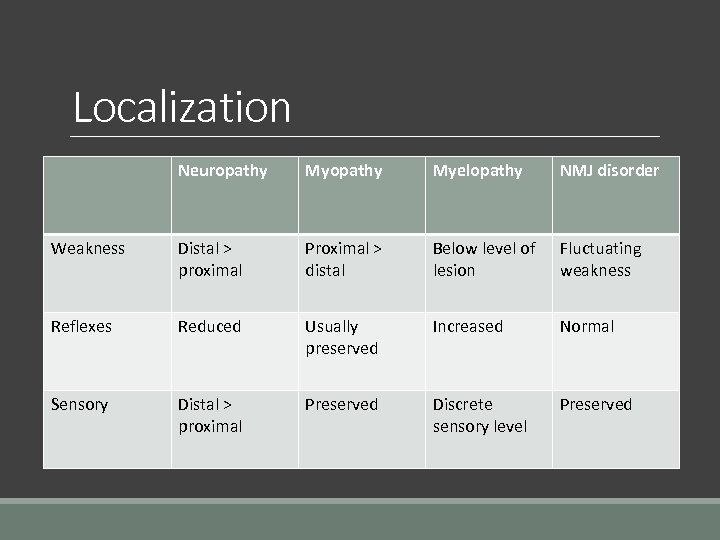
Localization Neuropathy Myelopathy NMJ disorder Weakness Distal > proximal Proximal > distal Below level of lesion Fluctuating weakness Reflexes Reduced Usually preserved Increased Normal Sensory Distal > proximal Preserved Discrete sensory level Preserved
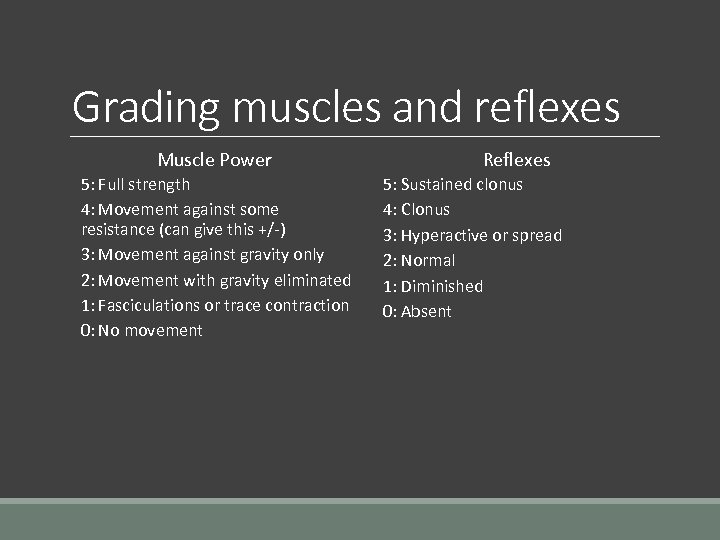
Grading muscles and reflexes Muscle Power 5: Full strength 4: Movement against some resistance (can give this +/-) 3: Movement against gravity only 2: Movement with gravity eliminated 1: Fasciculations or trace contraction 0: No movement Reflexes 5: Sustained clonus 4: Clonus 3: Hyperactive or spread 2: Normal 1: Diminished 0: Absent
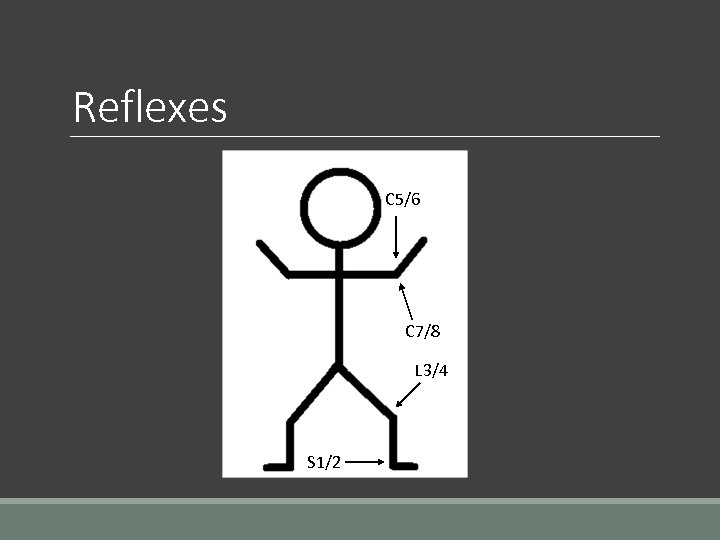
Reflexes C 5/6 C 7/8 L 3/4 S 1/2
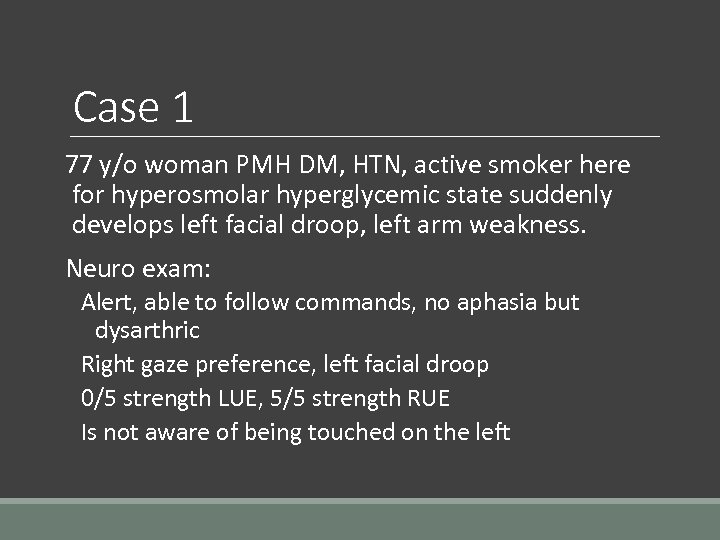
Case 1 77 y/o woman PMH DM, HTN, active smoker here for hyperosmolar hyperglycemic state suddenly develops left facial droop, left arm weakness. Neuro exam: Alert, able to follow commands, no aphasia but dysarthric Right gaze preference, left facial droop 0/5 strength LUE, 5/5 strength RUE Is not aware of being touched on the left
Stroke Signs and Symptoms Stroke is a sudden onset neurological deficit ◦ Sudden numbness or weakness of the face, arm or leg ◦ Sudden trouble speaking or understanding ◦ Sudden trouble seeing out of one or both eyes ◦ Sudden difficulty walking, dizziness, loss of balance or coordination ◦ Sudden severe headache with no known cause
Stroke types Ischemic ◦ Thrombotic ◦ Embolic – maximum symptoms at onset ◦ Lacunar Hemorrhagic ◦ ICH – Frequently related to HTN ◦ Subarachnoid – Trauma most common, aneurysmal second most common
Initial Management of Stroke Focused history with medications Time of “last seen normal/well? ” Vital signs NIHSS Examination Blood glucose, CBC, basic electrolytes, troponin, pregnancy test EKG STAT CT Brain (make sure disk goes with them if at VA) IV access IV TPA Eligibility checklist At UH Call BAT 41111 At VA UH transfer center 216 -844 -1111 to consult with stroke neurology for potential transfer
Focused history with medications What symptoms are you having? When did you notice them? Ever had a stroke before? When? What kind? What symptoms? How were they treated? Stroke risk factors? History of seizures or spells? On warfarin? DOAC? Heparin?
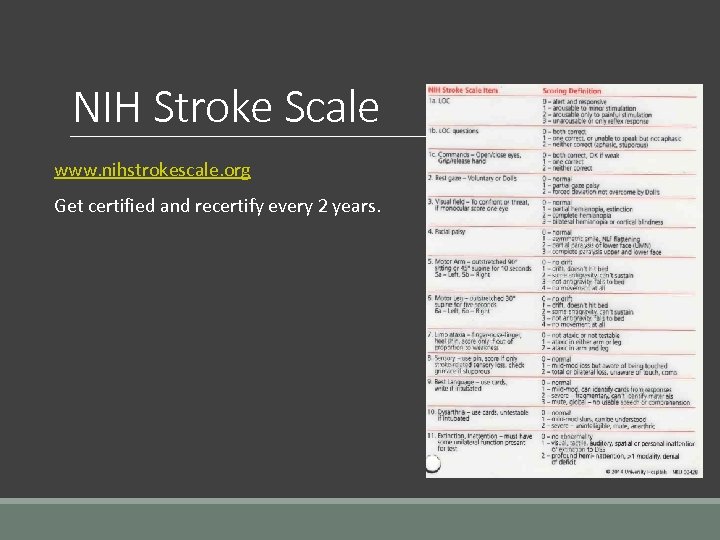
NIH Stroke Scale www. nihstrokescale. org Get certified and recertify every 2 years.
Eligibility for TPA < 3 hours exclusion criteria: ◦ SBP > 185, DBP > 110 (control it!) ◦ Minor or isolated deficit (relative) ◦ Spontaneous resolution ◦ Suggest post ictal impairment ◦ Evidence of trauma, internal bleeding, fracture ◦ Hx of ICH or known intracerebral neoplasm, AVM or aneurysm ◦ Recent intracranial or intraspinal surgery ◦ Hx head trauma or prior stroke within 3 months ◦ Hx of MI within 3 months (relative)
Eligibility for TPA < 3 hours exclusion criteria continued: ◦ Hx of GI or urinary tract hemorrhage within 21 days (relative) ◦ Major surgery or trauma in the prior 14 days (relative) ◦ Arterial puncture at a noncompressible site within 14 days ◦ Blood glucose < 50 ◦ Hemorrhage on CT or hypodensity > 1/3 MCA territory ◦ Thrombocytopenia suspected or platelet count < 100 ◦ Warfarin use suspected or INR> 1. 7, heparin use with in 48 hours, LMWH within 3 days
Eligibility for TPA 3 -4. 5 hours exclusion criteria: ◦ Age equal to or greater than 80 ◦ Not on anticoagulants regardless of INR ◦ NIHSS < 25 ◦ No hx of diabetes AND stroke
Eligibility for TPA 4. 5 -6 hours: Consider endovascular reperfusion ◦ Major artery occlusion ◦ NIHSS > 6 ◦ Non-disabled at baseline ◦ CTH with no major early infarct changes
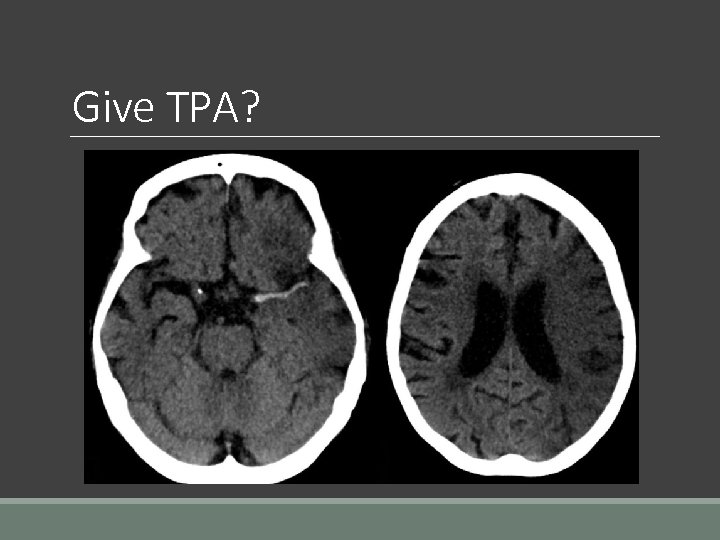
Give TPA?
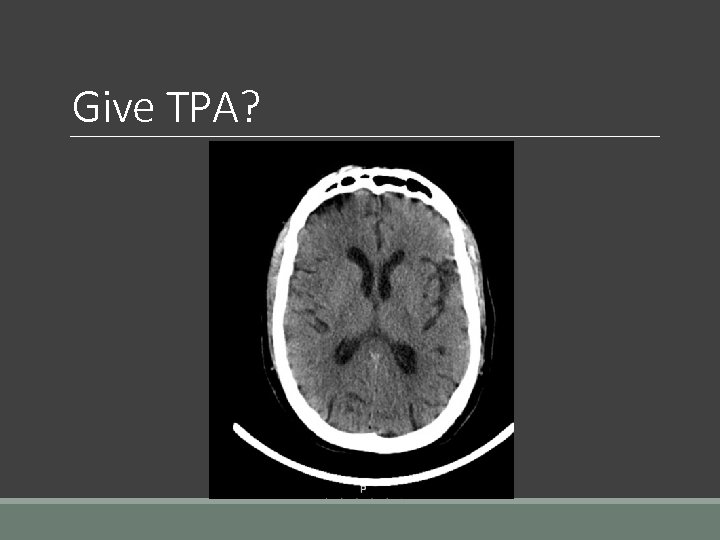
Give TPA?
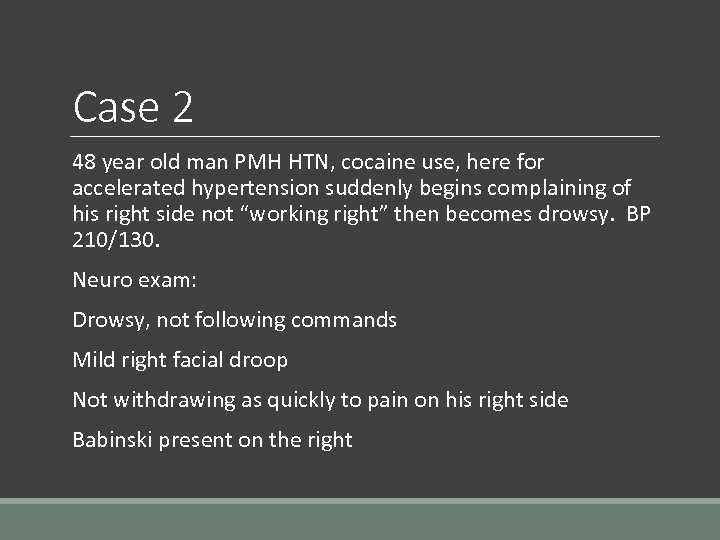
Case 2 48 year old man PMH HTN, cocaine use, here for accelerated hypertension suddenly begins complaining of his right side not “working right” then becomes drowsy. BP 210/130. Neuro exam: Drowsy, not following commands Mild right facial droop Not withdrawing as quickly to pain on his right side Babinski present on the right
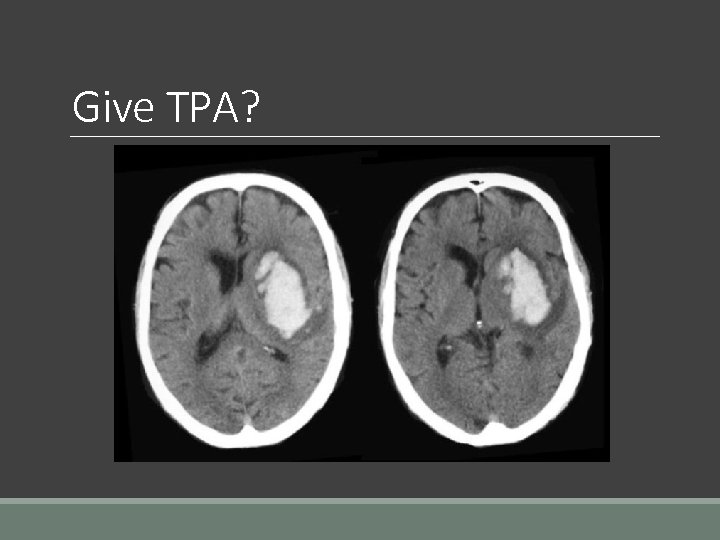
Give TPA?
Hemorrhagic strokes ICH ◦ Start with noncontrast CTH ◦ Reversal agents if on anticoagulation (talk to hematology or pharmacy if unsure) ◦ Goal SBP < 160 ◦ Contact Neurosurgery 30153 ◦ Transfer to NSU at UH
Case 2 continued On the way back from CT the patient’s breathing becomes extremely irregular and he becomes comatose. His BP is 190/80, his HR is 31. Neuro Exam: Comatose Right pupil fixed and dilated Not withdrawing to pain in any extremity
Increased ICP Intubate the patient Drain CSF if possible Start hyperosmolar therapy (mannitol 20% 0. 25 -1. 5 g/kg q 2 -6 hours) OR 3% - 23. 4% Na. Cl to target Na 150 -160 (note these are temporizing) Avoid hypovolemia Need ICP monitor Normoventilation and use hyperventilation for ICP spikes Hypothermia
Subarachnoid Hemorrhage Start with noncontrast CTH, do LP if suspicion persists Goal SBP < 160 Contact Neurosurgery Transfer to NSU at UH
Common stroke mimics Encephalopathy especially with sepsis Seizure Pain medication overdose/drugs Dementia with delirium When in doubt call a BAT!
Case 3 37 year old man with a PMH of alcoholism and epilepsy is admitted for alcohol detoxification. His last drink was 1 hour ago. The nurse calls you because he became very fearful, his right arm began “shaking” with his head turning to the right and eyes forced to the right. He then developed whole body “stiffening and shaking” which has continued off and on for the last 6 minutes. Neuro: obtunded, no facial asymmetry, normal tone, reflexes 3/4, plantar reflex downgoing
Convulsive Status Epilepticus Definition: 5 minutes or more of continuous seizures or 2 discrete seizures between which there is incomplete recovery of consciousness Common causes: ◦ Acute or remote structural brain lesion (stroke, meningitis, tumor) ◦ Antiseizure drug nonadherence ◦ Withdrawal from alcohol, barbituates etc. ◦ Metabolic abnormalities
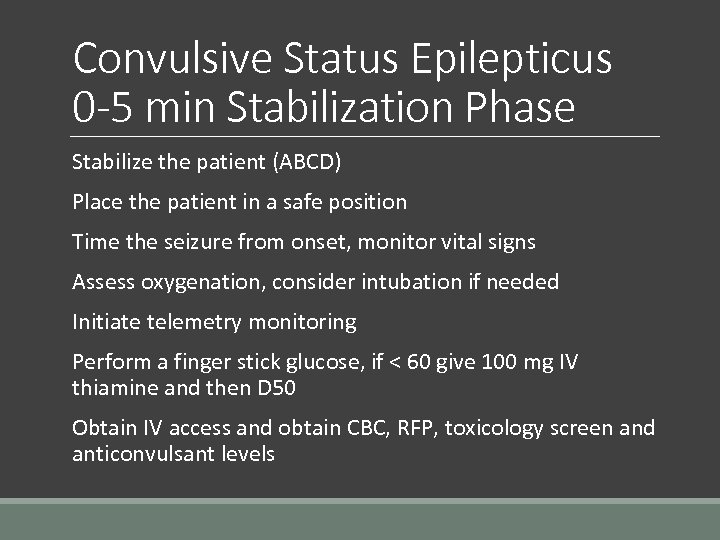
Convulsive Status Epilepticus 0 -5 min Stabilization Phase Stabilize the patient (ABCD) Place the patient in a safe position Time the seizure from onset, monitor vital signs Assess oxygenation, consider intubation if needed Initiate telemetry monitoring Perform a finger stick glucose, if < 60 give 100 mg IV thiamine and then D 50 Obtain IV access and obtain CBC, RFP, toxicology screen and anticonvulsant levels
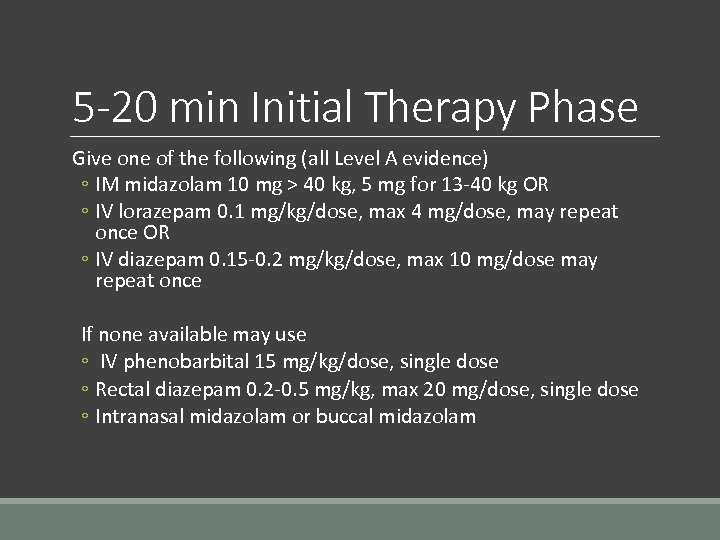
5 -20 min Initial Therapy Phase Give one of the following (all Level A evidence) ◦ IM midazolam 10 mg > 40 kg, 5 mg for 13 -40 kg OR ◦ IV lorazepam 0. 1 mg/kg/dose, max 4 mg/dose, may repeat once OR ◦ IV diazepam 0. 15 -0. 2 mg/kg/dose, max 10 mg/dose may repeat once If none available may use ◦ IV phenobarbital 15 mg/kg/dose, single dose ◦ Rectal diazepam 0. 2 -0. 5 mg/kg, max 20 mg/dose, single dose ◦ Intranasal midazolam or buccal midazolam
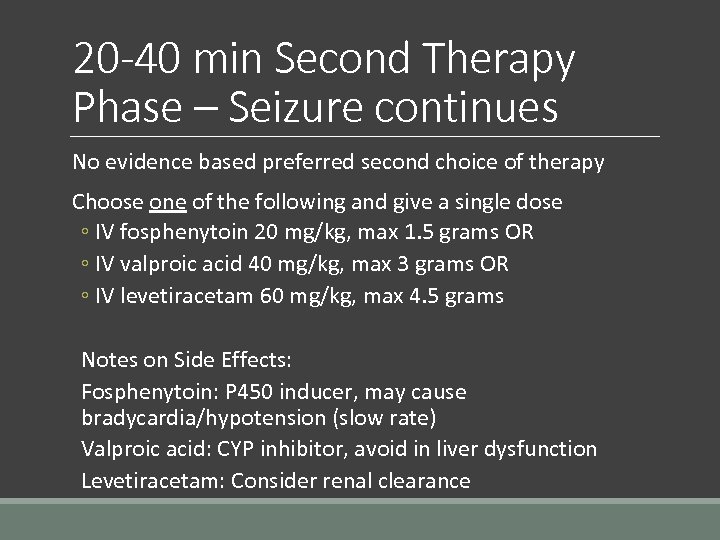
20 -40 min Second Therapy Phase – Seizure continues No evidence based preferred second choice of therapy Choose one of the following and give a single dose ◦ IV fosphenytoin 20 mg/kg, max 1. 5 grams OR ◦ IV valproic acid 40 mg/kg, max 3 grams OR ◦ IV levetiracetam 60 mg/kg, max 4. 5 grams Notes on Side Effects: Fosphenytoin: P 450 inducer, may cause bradycardia/hypotension (slow rate) Valproic acid: CYP inhibitor, avoid in liver dysfunction Levetiracetam: Consider renal clearance
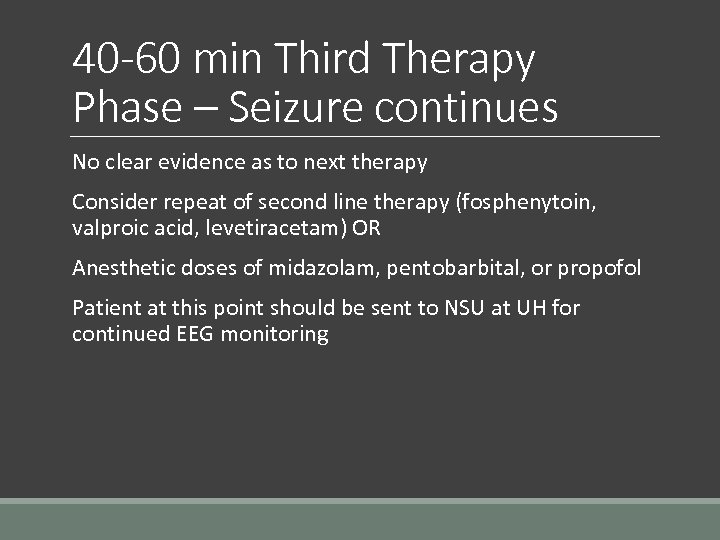
40 -60 min Third Therapy Phase – Seizure continues No clear evidence as to next therapy Consider repeat of second line therapy (fosphenytoin, valproic acid, levetiracetam) OR Anesthetic doses of midazolam, pentobarbital, or propofol Patient at this point should be sent to NSU at UH for continued EEG monitoring
Tips for admitting patients with epilepsy Continue home meds unless a contraindication Check available levels of antiepileptic drugs If making the patient NPO for a procedure, consult with pharmacy converting PO to IV If unable to convert PO to IV consult neurology
Case 4 37 year old man who presented with 3 day history of weakness and numbness in the feet which now involves the hands. He had a viral illness 1 week ago. Neuro Exam: Cranial nerves intact, ocular muscles intact, no facial asymmetry 5/5 strength in upper extremities except for 4/5 strength in finger flexors/extensors, 3/5 strength in lower extremities distally, 4/5 strength proximally Decreased tone Decreased sensation to pinprick and light touch Plantar reflex downgoing bilaterally
Guillain-Barre Syndrome Immune mediated damage to the nervous system which typically follows infection, classicly with areflexia and ascending weakness/numbness Commonly follows infection ◦ Campylobacter, CMV, EBV, mycoplasma pneumoniae Move to a telemetry floor (watch for arrhythmias!) Perform LP to look for cytoalbuminological dissocation Ask RT to perform NIF and VC every 8 hours Order EMG/NCS Send GM 1 antibodies or GQ 1 b antibodies as relevant Neuro consult
Case 5 80 year old man with chronic arthritis and dementia here for delirium secondary to a UTI falls after getting up unassisted. At baseline patient is ambulatory. You are called to assess the patient. Neuro Exam: Awake, answers questions, oriented x 2 (baseline) Cranial nerves intact 5/5 strength in the upper extremities, 2/5 strength in both lower extremities Decreased sensation to pinprick below the C 6 Reflexes 3+ in biceps, 0+ in bilateral patella, plantar reflex extensor Rectal exam with loss of rectal tone
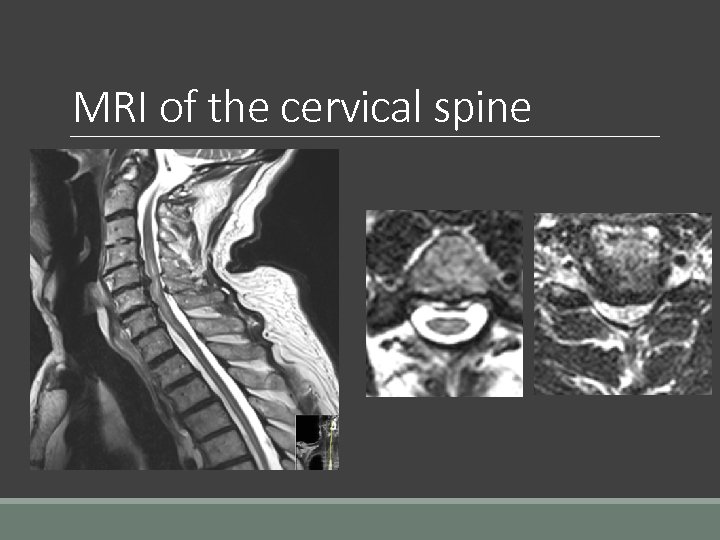
MRI of the cervical spine
Acute spinal cord compression Most important prognostic factor is pretreatment neurological status Call 4111, MRI of the entire spine STAT Traumatic – ◦ Consult neurosurgery/ortho spine ◦ Steroids are controversial due to complications Tumor – ◦ Consult radiation oncology, neurosurgery/ortho spine ◦ Give 10 mg IV dexamethasone then 4 mg every 6 hours Epidural abscess (usually SA) – ◦ Consult neurosurgery/ortho spine ◦ Draw cultures ◦ Broad spectrum antibiotics (start empirically)
Case 6 A 32 year old man is brought in by his family with one day history of headache, fevers and lethargy. Neuro Exam: Lethargic but arousable Significant difficulty flexing neck to chin 5/5 strength throughout Sensation normal to pinprick throughout
Meningitis May be bacterial (S. pneumoniae, N. meningitides, L. monocytogenes), fungal or viral Initial management for suspected bacterial: Start empiric antibiotics: Vancomycin, Ceftriaxone, Ampicillin Use Meropenem or Cefepime if impaired cellular immunity or health care associated If beta lactam allergy desensitize and Vancomycin plus moxifloxacin plus trimethoprim-sulfamethoxazole Give dexamethasone 0. 15 mg/kg every 6 hours starting with first dose if suspected pneumococcal infection If concern for encephalitis add acyclovir
Meningitis continued Blood cultures CT scan before LP if: ◦ ◦ ◦ Immunocompromised Hx of CNS disease (stroke, brain met etc. ) New onset seizure Papilledema Altered consciousness Focal neurological deficit Perform LP! Consider ID consult
Case 7 21 year old woman admitted for SOB, generalized weakness, productive cough with concern for CAP. Started on azithromycin and ceftriaxone in the ED. Patient begins complaining of difficulty swallowing and double vision. Neuro Exam: Bilateral ptosis worsening with upgaze, face symmetric, dysarthric, drooling Difficulty flexing and extending neck 3/5 strength in UE proximally, 4/5 strength in UE distally Sensation intact to LT, pinprick, DTR 2/4 throughout Babinski absent
Myasthenic Crisis Autoimmune disease caused by antibodies against Ach receptors Initial management: RT consult for NIF, VC DC offending agents if possible (aminoglycosides, -mycin, quinolones, lithium, phenytoin, beta blockers, procainamide, statins) If already on anticholinesterase drug (pyridostigmine) hold the drug Move to ICU for monitoring and place on telemetry Avoid steroids in the acute setting Neurology consult
Summary 1) Reviewed the neurological exam 2) Reviewed neurological emergencies including: ◦ ◦ ◦ ◦ Stroke Elevated ICP Status epilepticus Guillain-Barre Syndrome (AIDP) Acute spinal cord compression Meningitis Myasthenic crisis
Thank you and good luck on wards! Questions?
94b0cc0fd733bf41045db150170746b9.ppt