641b26f807aa1fd93964d12c541927a2.ppt
- Количество слайдов: 24
Neurocritical Care for the Newborn Taeun Chang, MD Director, Neonatal Neurology Children’s National Medical Center
Objectives n To understand the current state of neonatal neurocritical care (NNC). n To understand the role and potential contributions of a neonatal neurointensivist in the NICU n To understand the role of the multidisciplinary and regional nature of neuroprotective care
Children’s National Neonatal Neurocritical Care Three neonatal neurointensivists n Supported by 8 neurophysiologists, 6 EEG technologists & a biomedical engineer n Interacting with 7 neonatologists, 4 neuroradiologists, and 4 neurosurgeons n Using 4 NICU video EEG monitors (potential 8 machines) with a. EEG & bedside remote access, 6 NIRS, 1 portable CT, 1 MRI compatible incubator, and 2 MRI scanners n Attending a separate neonatal neurointensive care service with minimum twice daily bedside rounds n Independently reviewing studies to intervene as necessary in an acute manner n Daily bedside family & NICU updates & interdisciplinary family meetings after evaluation or prior to discharge n Follow up in neonatal neurology clinic or interdisciplinary clinics (perinatal brain injury clinic, cooling clinic)
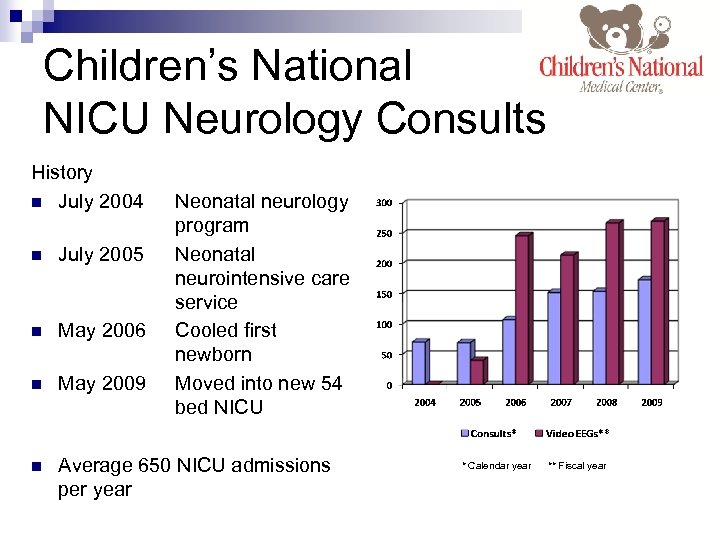
Children’s National NICU Neurology Consults History n July 2004 Neonatal neurology program Neonatal neurointensive care service Cooled first newborn Moved into new 54 bed NICU n July 2005 n May 2006 n May 2009 n Average 650 NICU admissions per year * Calendar year ** Fiscal year
Our Response to Hypothermia Case Our response and management to neonatal encephalopathy presenting for hypothermia: n Neurointensive care service notified of planned transfer to initiate any treatments prior to transport and to arrange EEG service. Placental pathology requested of birth hospital. n Initial neurologic assessment upon NICU arrival if in-house or as soon as possible. n Continuous video EEG started as soon as possible (typically 11 hours of life). Initial background assessed for risk of seizures. If infant considered high risk then EEG reviewed in 2 -3 hrs & neurophysiology service made aware. n Seizures treated with phenobarbital and protocol initiated for monitoring & treatment of status epilepticus. n Daily neurologic assessments, EEG review and bedside rounds made with NICU team & family. n Major issues and plan signed out at end of day to NICU, on-call neurology resident & neurophysiologist. Neurointensivist available by page by all team members. n MRI imaging performed at DOL#8 -10 using neonatal specific hypothermia protocols. n Joint NICU family meeting to review findings, studies, antecedent diagnosis and prognosis.
CASES
EEG monitoring to detect sentinel neurologic events.
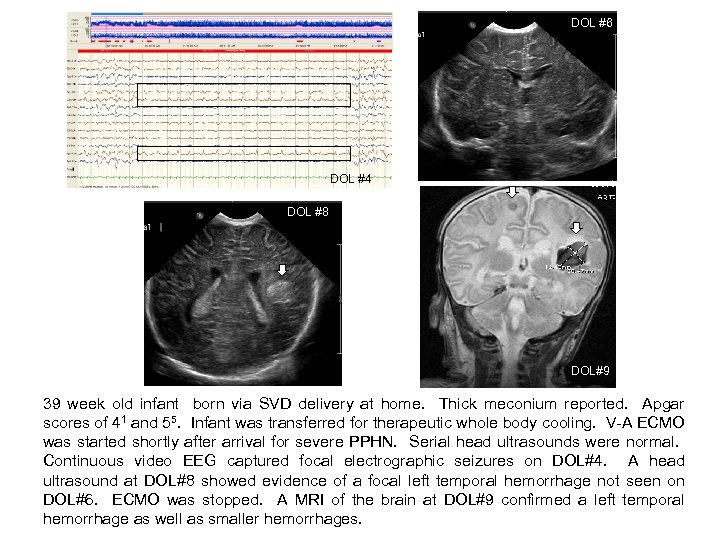
DOL #6 DOL#8 DOL #4 DOL #8 DOL#9 39 week old infant born via SVD delivery at home. Thick meconium reported. Apgar scores of 41 and 55. Infant was transferred for therapeutic whole body cooling. V-A ECMO was started shortly after arrival for severe PPHN. Serial head ultrasounds were normal. Continuous video EEG captured focal electrographic seizures on DOL#4. A head ultrasound at DOL#8 showed evidence of a focal left temporal hemorrhage not seen on DOL#6. ECMO was stopped. A MRI of the brain at DOL#9 confirmed a left temporal hemorrhage as well as smaller hemorrhages.
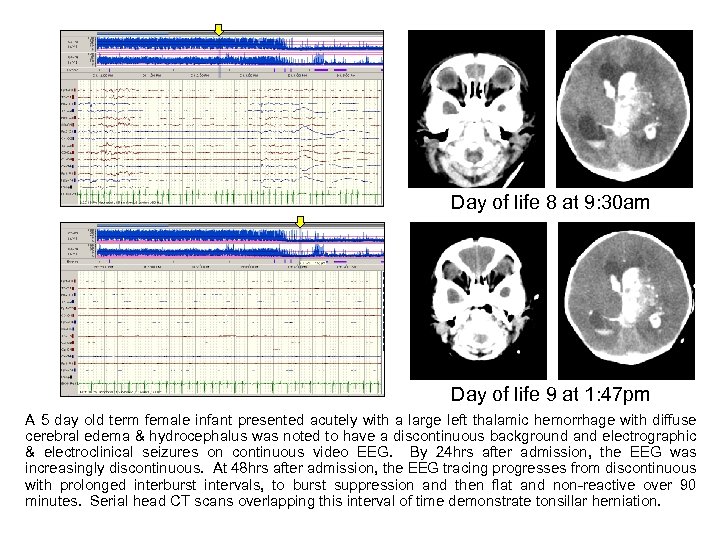
Day of life 8 at 9: 30 am Day of life 9 at 1: 47 pm A 5 day old term female infant presented acutely with a large left thalamic hemorrhage with diffuse cerebral edema & hydrocephalus was noted to have a discontinuous background and electrographic & electroclinical seizures on continuous video EEG. By 24 hrs after admission, the EEG was increasingly discontinuous. At 48 hrs after admission, the EEG tracing progresses from discontinuous with prolonged interburst intervals, to burst suppression and then flat and non-reactive over 90 minutes. Serial head CT scans overlapping this interval of time demonstrate tonsillar herniation.
Neonatal neurointensivist evaluation affecting NICU & Cardiology decision to escalate care.
Neonatal neurointensivist evaluation affecting NICU decision to continue supportive care.
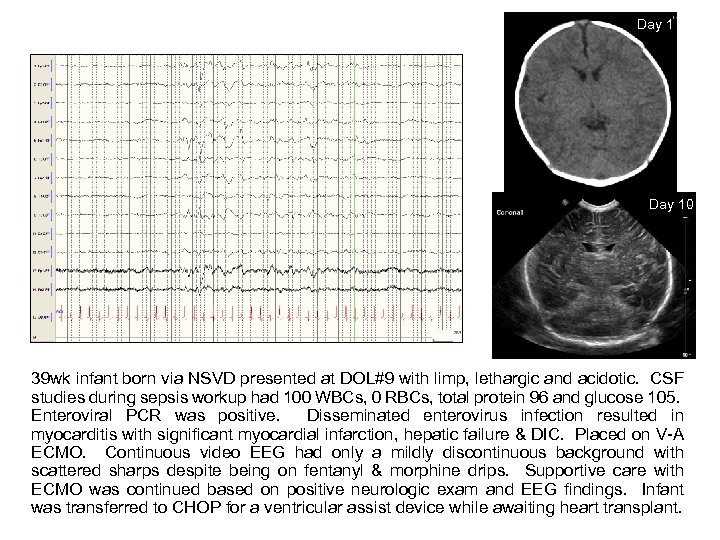
Day 10 39 wk infant born via NSVD presented at DOL#9 with limp, lethargic and acidotic. CSF studies during sepsis workup had 100 WBCs, 0 RBCs, total protein 96 and glucose 105. Enteroviral PCR was positive. Disseminated enterovirus infection resulted in myocarditis with significant myocardial infarction, hepatic failure & DIC. Placed on V-A ECMO. Continuous video EEG had only a mildly discontinuous background with scattered sharps despite being on fentanyl & morphine drips. Supportive care with ECMO was continued based on positive neurologic exam and EEG findings. Infant was transferred to CHOP for a ventricular assist device while awaiting heart transplant.
Neonatal neurointensivist evaluation leading to diagnosis of a non-sentinel case of neonatal encephalopathy. A newborn with refractory status epilepticus leading to a new neurocritical care protocol for NICU seizure management.
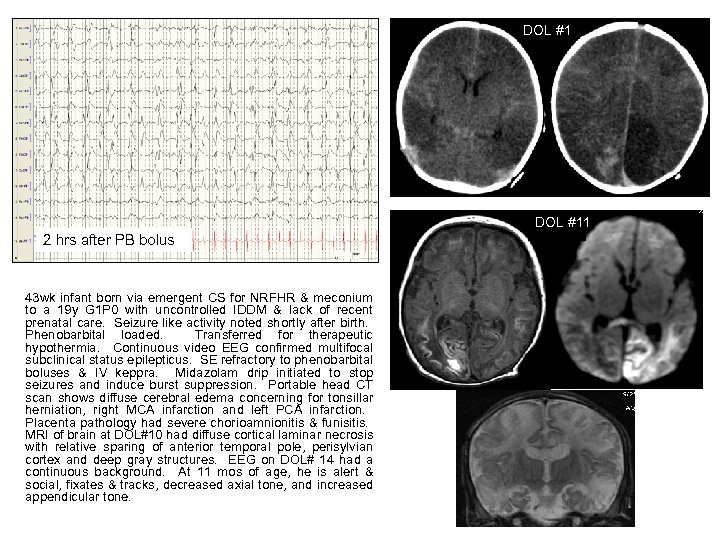
DOL #11 2 hrs after PB bolus 43 wk infant born via emergent CS for NRFHR & meconium to a 19 y G 1 P 0 with uncontrolled IDDM & lack of recent prenatal care. Seizure like activity noted shortly after birth. Phenobarbital loaded. Transferred for therapeutic hypothermia. Continuous video EEG confirmed multifocal subclinical status epilepticus. SE refractory to phenobarbital boluses & IV keppra. Midazolam drip initiated to stop seizures and induce burst suppression. Portable head CT scan shows diffuse cerebral edema concerning for tonsillar herniation, right MCA infarction and left PCA infarction. Placenta pathology had severe chorioamnionitis & funisitis. MRI of brain at DOL#10 had diffuse cortical laminar necrosis with relative sparing of anterior temporal pole, perisylvian cortex and deep gray structures. EEG on DOL# 14 had a continuous background. At 11 mos of age, he is alert & social, fixates & tracks, decreased axial tone, and increased appendicular tone.
Neonatal neurointensivist evaluation leading to diagnosis of a perinatal arterial stroke.
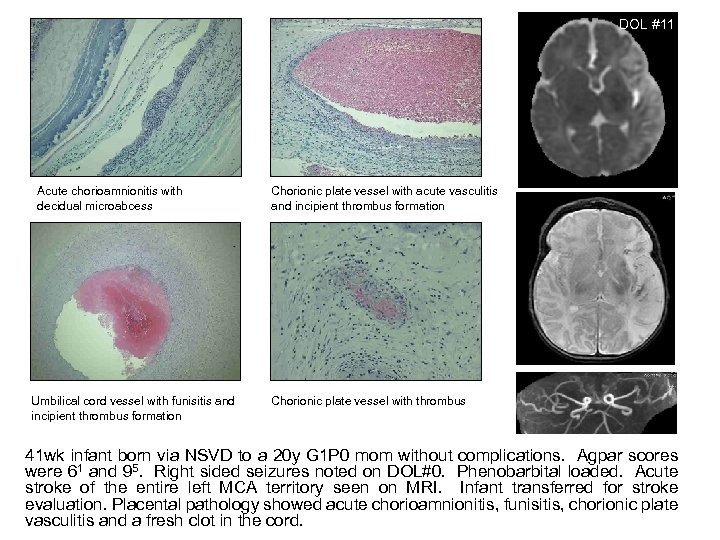
DOL #11 Acute chorioamnionitis with decidual microabcess Umbilical cord vessel with funisitis and incipient thrombus formation Chorionic plate vessel with acute vasculitis and incipient thrombus formation Chorionic plate vessel with thrombus 41 wk infant born via NSVD to a 20 y G 1 P 0 mom without complications. Agpar scores were 61 and 95. Right sided seizures noted on DOL#0. Phenobarbital loaded. Acute stroke of the entire left MCA territory seen on MRI. Infant transferred for stroke evaluation. Placental pathology showed acute chorioamnionitis, funisitis, chorionic plate vasculitis and a fresh clot in the cord.
Neurotherapeutics To identify areas of neurotherapeutic development in NNC & NICUs.
Hypothermia Trials Cooling in transport – targeted temperature management n Delayed cooling – cooling beyond 6 hrs of insult/life n Cooling in premature infants n Cooling in ECMO patients n
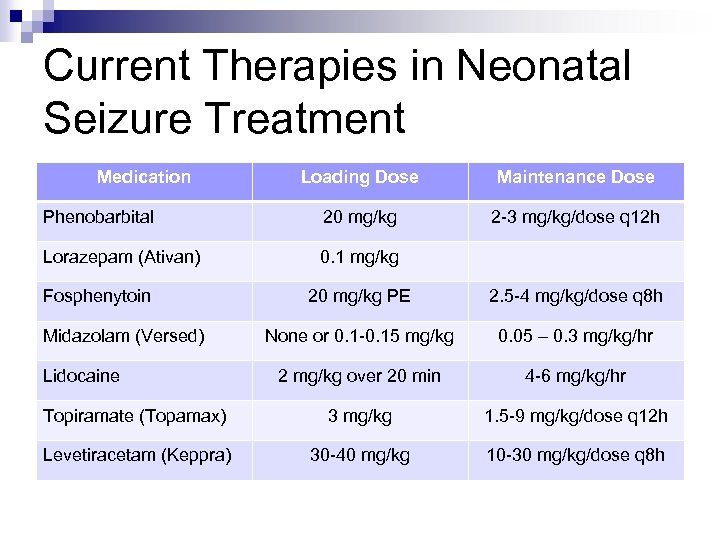
Current Therapies in Neonatal Seizure Treatment Medication Loading Dose Maintenance Dose Phenobarbital 20 mg/kg 2 -3 mg/kg/dose q 12 h Lorazepam (Ativan) 0. 1 mg/kg Fosphenytoin 20 mg/kg PE 2. 5 -4 mg/kg/dose q 8 h None or 0. 1 -0. 15 mg/kg 0. 05 – 0. 3 mg/kg/hr 2 mg/kg over 20 min 4 -6 mg/kg/hr Topiramate (Topamax) 3 mg/kg 1. 5 -9 mg/kg/dose q 12 h Levetiracetam (Keppra) 30 -40 mg/kg 10 -30 mg/kg/dose q 8 h Midazolam (Versed) Lidocaine
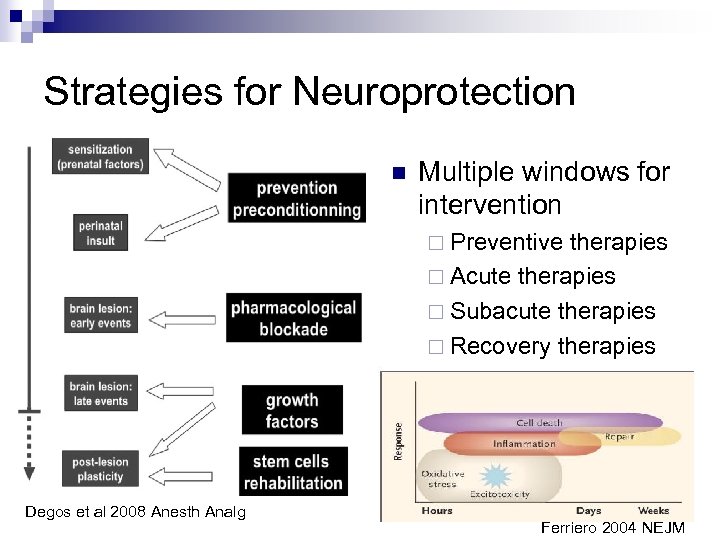
Strategies for Neuroprotection n Multiple windows for intervention ¨ Preventive therapies ¨ Acute therapies ¨ Subacute therapies ¨ Recovery therapies Degos et al 2008 Anesth Analg Ferriero 2004 NEJM
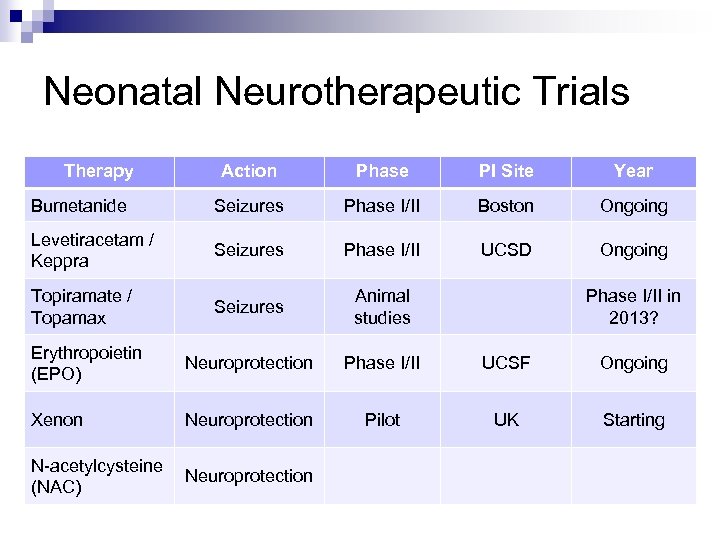
Neonatal Neurotherapeutic Trials Therapy Action Phase PI Site Year Bumetanide Seizures Phase I/II Boston Ongoing Levetiracetam / Keppra Seizures Phase I/II UCSD Ongoing Topiramate / Topamax Seizures Animal studies Erythropoietin (EPO) Neuroprotection Phase I/II UCSF Ongoing Xenon Neuroprotection Pilot UK Starting N-acetylcysteine (NAC) Neuroprotection Phase I/II in 2013?
Conclusions n Neonatal neurointensivists and neurocritical care units are becoming a new subspecialty field and ICU service. n Neuromonitoring & neurosupportive care should be incorporated in NICU protocols at levels appropriate for each facility. n New neurotherapeutics are being investigated specifically for neonates.
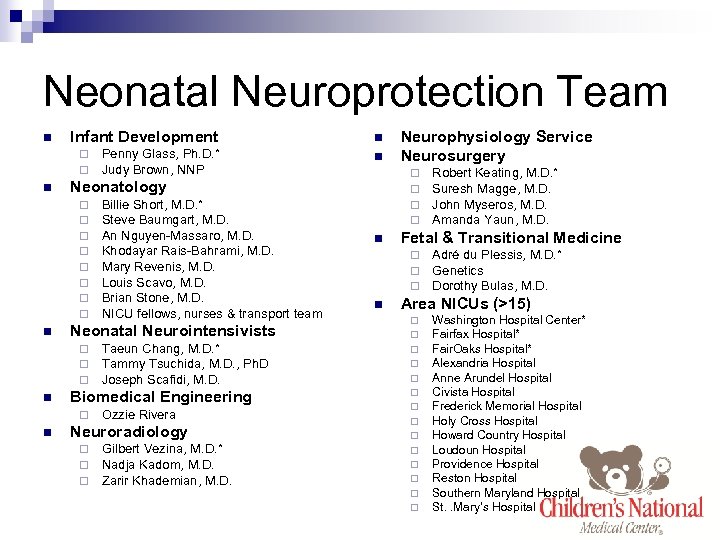
Neonatal Neuroprotection Team n Infant Development n Penny Glass, Ph. D. * Judy Brown, NNP n ¨ ¨ n n Taeun Chang, M. D. * Tammy Tsuchida, M. D. , Ph. D Joseph Scafidi, M. D. Biomedical Engineering ¨ n Billie Short, M. D. * Steve Baumgart, M. D. An Nguyen-Massaro, M. D. Khodayar Rais-Bahrami, M. D. Mary Revenis, M. D. Louis Scavo, M. D. Brian Stone, M. D. NICU fellows, nurses & transport team Neonatal Neurointensivists ¨ ¨ ¨ n ¨ ¨ Neonatology ¨ ¨ ¨ ¨ Ozzie Rivera Neuroradiology ¨ ¨ ¨ Gilbert Vezina, M. D. * Nadja Kadom, M. D. Zarir Khademian, M. D. Neurophysiology Service Neurosurgery n Fetal & Transitional Medicine ¨ ¨ ¨ n Robert Keating, M. D. * Suresh Magge, M. D. John Myseros, M. D. Amanda Yaun, M. D. Adré du Plessis, M. D. * Genetics Dorothy Bulas, M. D. Area NICUs (>15) ¨ ¨ ¨ ¨ Washington Hospital Center* Fairfax Hospital* Fair. Oaks Hospital* Alexandria Hospital Anne Arundel Hospital Civista Hospital Frederick Memorial Hospital Holy Cross Hospital Howard Country Hospital Loudoun Hospital Providence Hospital Reston Hospital Southern Maryland Hospital St. . Mary’s Hospital
Our Cool Babies Baby JP after arrival Baby M in NICU 24 months 19 months 4 months 12 months
641b26f807aa1fd93964d12c541927a2.ppt