6d4755b7db519bc7bf5e6ef70dcd1421.ppt
- Количество слайдов: 71

 Neurocognitive Outcomes of Radiation Therapy in Children Aaron S. Kusano, SM University of Washington School of Medicine
Neurocognitive Outcomes of Radiation Therapy in Children Aaron S. Kusano, SM University of Washington School of Medicine
 Outline Topic Choice n Background/Current Practices n Studies of Neurocognitive Effects n Predictive Model Research n Interventions n Conclusion n
Outline Topic Choice n Background/Current Practices n Studies of Neurocognitive Effects n Predictive Model Research n Interventions n Conclusion n
 Why this topic? n n Balancing act of treatment objectives Implications in Patient Counseling/Education, Multidisciplinary Care and follow up Increasing survival = increasing long term side effects Challenging research – – – growing body of literature study design advancing technology and alternate approaches
Why this topic? n n Balancing act of treatment objectives Implications in Patient Counseling/Education, Multidisciplinary Care and follow up Increasing survival = increasing long term side effects Challenging research – – – growing body of literature study design advancing technology and alternate approaches
 Background n Childhood cancer survivors have changes/difficulties in: 1)Attention 2)Social Skills 3)Social Competence 4)Internalization 5)Externalization 6)Social Isolation 7)Mood and Behavioral Disorders n 40 -100% of long term brain tumor survivors have some form of cognitive dysfunction Glauser TA, Packer RJ: Cognitive deficits in long-term survivors of childhood brain tumors. Childs Nerv Syst 7: 2 -12, 1991 Schultz et al. Behavioral and Social Outcomes in Adolescent Survivors of Childhood Cancer: A report from the Childhood cancer survivor study.
Background n Childhood cancer survivors have changes/difficulties in: 1)Attention 2)Social Skills 3)Social Competence 4)Internalization 5)Externalization 6)Social Isolation 7)Mood and Behavioral Disorders n 40 -100% of long term brain tumor survivors have some form of cognitive dysfunction Glauser TA, Packer RJ: Cognitive deficits in long-term survivors of childhood brain tumors. Childs Nerv Syst 7: 2 -12, 1991 Schultz et al. Behavioral and Social Outcomes in Adolescent Survivors of Childhood Cancer: A report from the Childhood cancer survivor study.
 Background n n Survivors of pediatric brain tumors have lower rates of high school graduation and employment relative to the overall population There is fairly consistent evidence of increased neurocognitive morbidity with higher treatment doses and younger age at the time of treatment Hoppe-Hirsch E, Brunet L, Laroussinie F, et al: Intellectual outcome in children with malignant tumors of the posterior fossa: Influence of the field of irradiation and quality of surgery. Childs Nerv Syst 11: 340 -346, 1995 Kelaghan J, Myers MH, Mulvihill JJ, et al: Educational achievement of long-term survivors of childhood and adolescent cancer. Med Pediatr Oncol 16: 320 -326, 19 Suc E et al. Brain tumours under the age of three. The price of survival. A retrospective study of 20 long-term survivors. Acta Neurochir (Wien). 1990; 106(3 -4): 93 -
Background n n Survivors of pediatric brain tumors have lower rates of high school graduation and employment relative to the overall population There is fairly consistent evidence of increased neurocognitive morbidity with higher treatment doses and younger age at the time of treatment Hoppe-Hirsch E, Brunet L, Laroussinie F, et al: Intellectual outcome in children with malignant tumors of the posterior fossa: Influence of the field of irradiation and quality of surgery. Childs Nerv Syst 11: 340 -346, 1995 Kelaghan J, Myers MH, Mulvihill JJ, et al: Educational achievement of long-term survivors of childhood and adolescent cancer. Med Pediatr Oncol 16: 320 -326, 19 Suc E et al. Brain tumours under the age of three. The price of survival. A retrospective study of 20 long-term survivors. Acta Neurochir (Wien). 1990; 106(3 -4): 93 -
 Pathophysiology Destruction of oligodendrocytes and endothelial cells n Microvascular changes n – Endothelial injury leads to toxic reactions – Formation of free radicals – Cell swelling, increased vascular permeability, ischemia, edema and cell death n Evident on MRI with white and gray matter changes
Pathophysiology Destruction of oligodendrocytes and endothelial cells n Microvascular changes n – Endothelial injury leads to toxic reactions – Formation of free radicals – Cell swelling, increased vascular permeability, ischemia, edema and cell death n Evident on MRI with white and gray matter changes
 Medulloblastoma
Medulloblastoma
 Epidemiology of Medulloblastoma Embryonal tumor n ~20% of pediatric CNS tumors n Median age at presentation 6 years n 30 -40% of patients have CSF spread at time of diagnosis n 5 year survival rates for children with standard risk medulloblastoma approaches 80% n
Epidemiology of Medulloblastoma Embryonal tumor n ~20% of pediatric CNS tumors n Median age at presentation 6 years n 30 -40% of patients have CSF spread at time of diagnosis n 5 year survival rates for children with standard risk medulloblastoma approaches 80% n
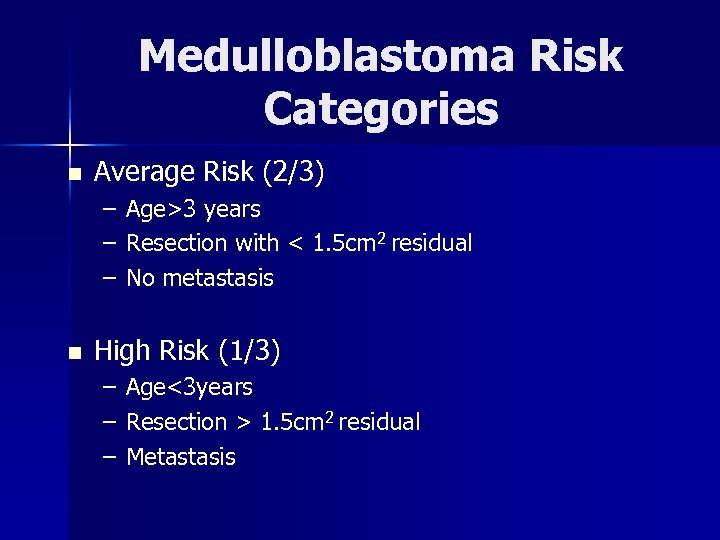 Medulloblastoma Risk Categories n Average Risk (2/3) – – – n Age>3 years Resection with < 1. 5 cm 2 residual No metastasis High Risk (1/3) – – – Age<3 years Resection > 1. 5 cm 2 residual Metastasis
Medulloblastoma Risk Categories n Average Risk (2/3) – – – n Age>3 years Resection with < 1. 5 cm 2 residual No metastasis High Risk (1/3) – – – Age<3 years Resection > 1. 5 cm 2 residual Metastasis
 Current Practices
Current Practices
 Categories n Standard Risk n High Risk n Infants
Categories n Standard Risk n High Risk n Infants
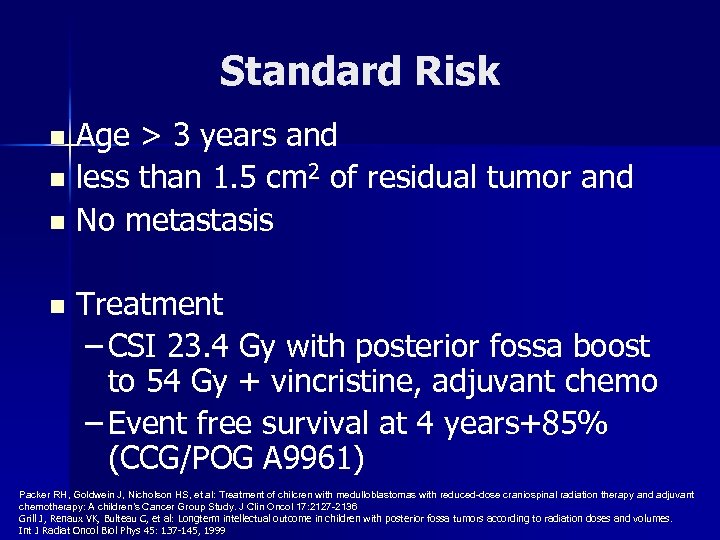 Standard Risk Age > 3 years and n less than 1. 5 cm 2 of residual tumor and n No metastasis n n Treatment – CSI 23. 4 Gy with posterior fossa boost to 54 Gy + vincristine, adjuvant chemo – Event free survival at 4 years+85% (CCG/POG A 9961) Packer RH, Goldwein J, Nicholson HS, et al: Treatment of chilcren with medulloblastomas with reduced-dose craniospinal radiation therapy and adjuvant chemotherapy: A children’s Cancer Group Study. J Clin Oncol 17: 2127 -2136 Grill J, Renaux VK, Bulteau C, et al: Longterm intellectual outcome in children with posterior fossa tumors according to radiation doses and volumes. Int J Radiat Oncol Biol Phys 45: 137 -145, 1999
Standard Risk Age > 3 years and n less than 1. 5 cm 2 of residual tumor and n No metastasis n n Treatment – CSI 23. 4 Gy with posterior fossa boost to 54 Gy + vincristine, adjuvant chemo – Event free survival at 4 years+85% (CCG/POG A 9961) Packer RH, Goldwein J, Nicholson HS, et al: Treatment of chilcren with medulloblastomas with reduced-dose craniospinal radiation therapy and adjuvant chemotherapy: A children’s Cancer Group Study. J Clin Oncol 17: 2127 -2136 Grill J, Renaux VK, Bulteau C, et al: Longterm intellectual outcome in children with posterior fossa tumors according to radiation doses and volumes. Int J Radiat Oncol Biol Phys 45: 137 -145, 1999
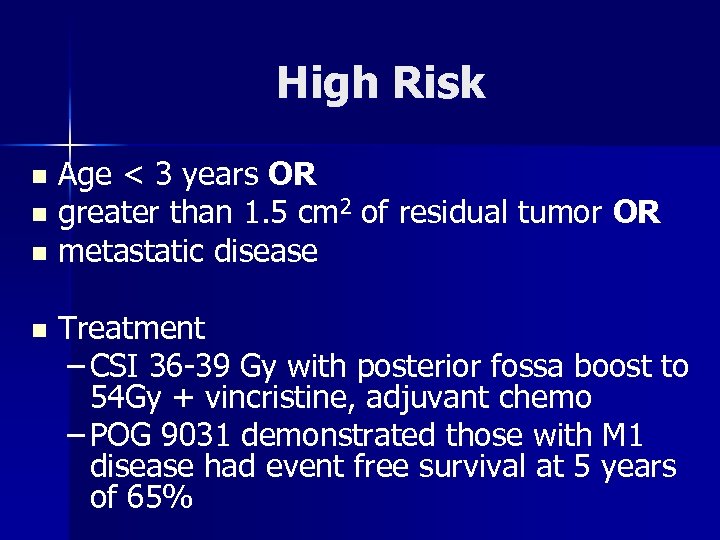 High Risk Age < 3 years OR n greater than 1. 5 cm 2 of residual tumor OR n metastatic disease n n Treatment – CSI 36 -39 Gy with posterior fossa boost to 54 Gy + vincristine, adjuvant chemo – POG 9031 demonstrated those with M 1 disease had event free survival at 5 years of 65%
High Risk Age < 3 years OR n greater than 1. 5 cm 2 of residual tumor OR n metastatic disease n n Treatment – CSI 36 -39 Gy with posterior fossa boost to 54 Gy + vincristine, adjuvant chemo – POG 9031 demonstrated those with M 1 disease had event free survival at 5 years of 65%
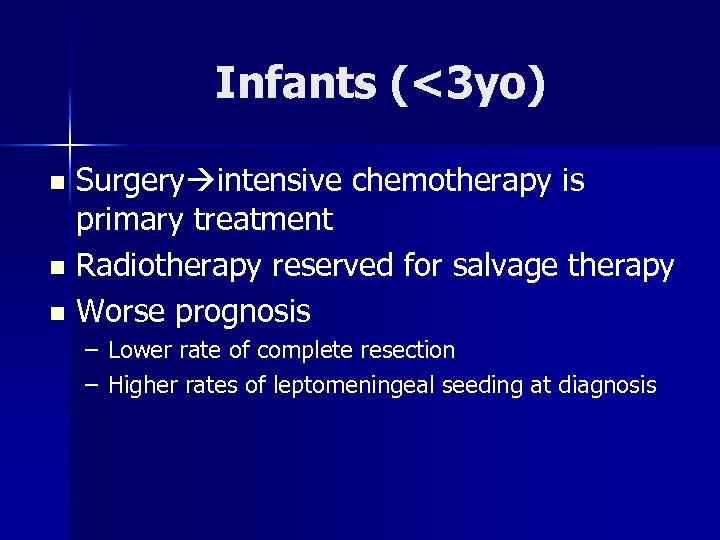 Infants (<3 yo) Surgery intensive chemotherapy is primary treatment n Radiotherapy reserved for salvage therapy n Worse prognosis n – Lower rate of complete resection – Higher rates of leptomeningeal seeding at diagnosis
Infants (<3 yo) Surgery intensive chemotherapy is primary treatment n Radiotherapy reserved for salvage therapy n Worse prognosis n – Lower rate of complete resection – Higher rates of leptomeningeal seeding at diagnosis
 Cognitive Measurement
Cognitive Measurement
 Wide Range Achievement Test (WRAT) n Ability to – Read words – Comprehend sentences – Spell – Math calculations
Wide Range Achievement Test (WRAT) n Ability to – Read words – Comprehend sentences – Spell – Math calculations
 Weschler Intelligence Scale n Full Scale IQ n Indices – Verbal Comprehension (vocab, comprehension) – Perceptual Reasoning (block design, picture concepts) – Processing Speed (timed coding activities) – Working Memory (repeating codes, sequences)
Weschler Intelligence Scale n Full Scale IQ n Indices – Verbal Comprehension (vocab, comprehension) – Perceptual Reasoning (block design, picture concepts) – Processing Speed (timed coding activities) – Working Memory (repeating codes, sequences)
 DSM-IV Criteria based on IQ Scores n n 50 -55 to 70: Mild Mental Retardation 35 -40 to 50 -55: Moderate Mental Retardation 20 -25 to 35 -40: Severe Mental Retardation 20 -25 and below: Profound Mental Retardation
DSM-IV Criteria based on IQ Scores n n 50 -55 to 70: Mild Mental Retardation 35 -40 to 50 -55: Moderate Mental Retardation 20 -25 to 35 -40: Severe Mental Retardation 20 -25 and below: Profound Mental Retardation
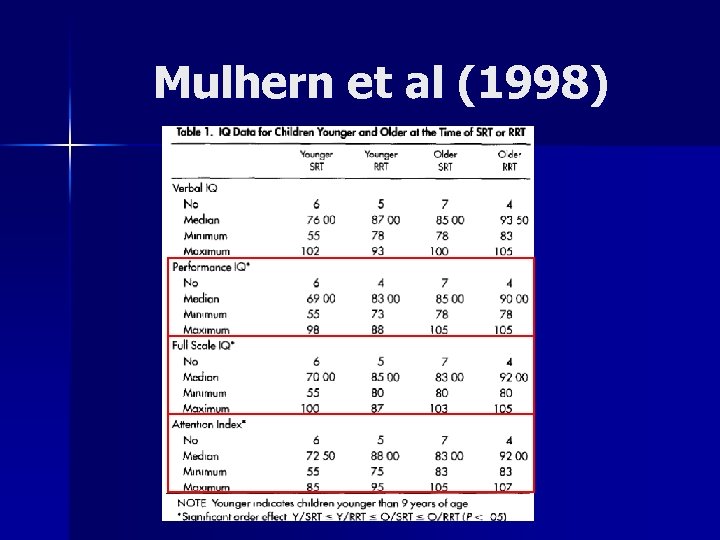
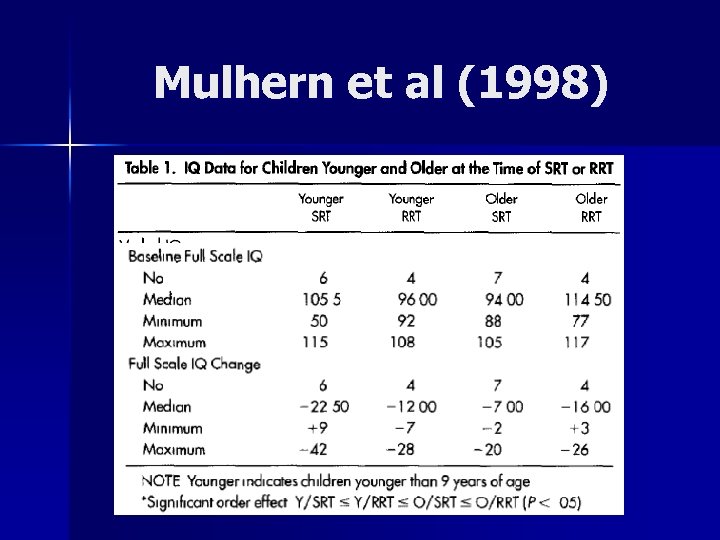
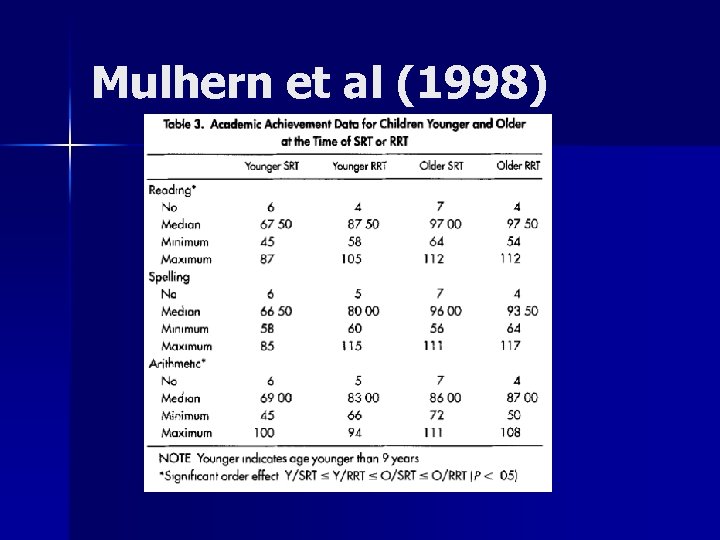
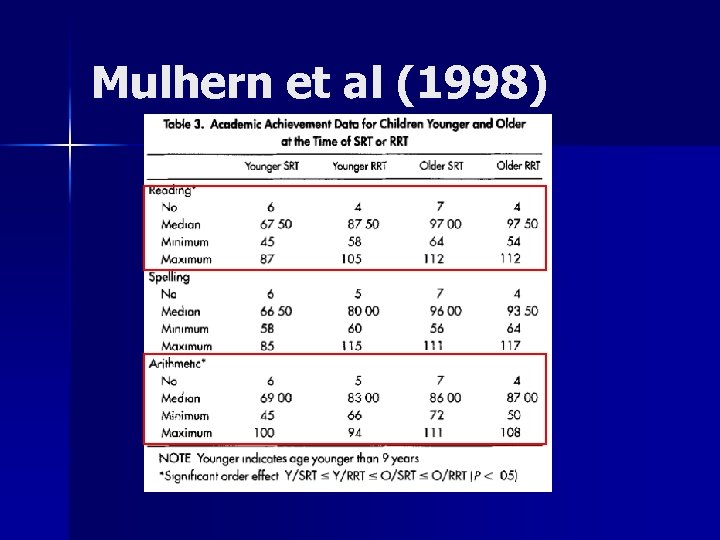
 Mulhern(1998)- Neuropsychologic functioning of survivors of childhood medulloblastoma POG 8631/CCG 923 n Treatment of average risk medulloblastomas n Hypothesis n – Children treated with lower initial radiation levels would experience less intellectual toxicity than those receiving higher levels – Also younger subjects suspected to have poorer outcome • Mulhern RK, Kepner JL, Thomas PR, et al: Neuropsychologic functioning of survivors of childhood medulloblastoma randomized to receive conventional or reduced-dose craniospinal irradiation: A Pediatric Oncology Group study. J Clin Oncol 16: 1723 -1728, 1998
Mulhern(1998)- Neuropsychologic functioning of survivors of childhood medulloblastoma POG 8631/CCG 923 n Treatment of average risk medulloblastomas n Hypothesis n – Children treated with lower initial radiation levels would experience less intellectual toxicity than those receiving higher levels – Also younger subjects suspected to have poorer outcome • Mulhern RK, Kepner JL, Thomas PR, et al: Neuropsychologic functioning of survivors of childhood medulloblastoma randomized to receive conventional or reduced-dose craniospinal irradiation: A Pediatric Oncology Group study. J Clin Oncol 16: 1723 -1728, 1998
 Mulhern et al (1998) Randomized to 36 Gy or 23. 4 Gy craniospinal radiation n Both groups receiving boost to 54 Gy to posterior fossa n Patient’s received baseline testing n Surviving patients in 1996 with no progressive disease were eligible for study n
Mulhern et al (1998) Randomized to 36 Gy or 23. 4 Gy craniospinal radiation n Both groups receiving boost to 54 Gy to posterior fossa n Patient’s received baseline testing n Surviving patients in 1996 with no progressive disease were eligible for study n
 Groupings Young (Y): Age < 9 years n Old (O): Age > 9 years n Standard dose radiation (SRT): 36 Gy n Reduced Dose (RRT): 23. 4 Gy n n Predicted trend of scores: – Y/SRT < Y/RRT < O/SRT < O/RRT
Groupings Young (Y): Age < 9 years n Old (O): Age > 9 years n Standard dose radiation (SRT): 36 Gy n Reduced Dose (RRT): 23. 4 Gy n n Predicted trend of scores: – Y/SRT < Y/RRT < O/SRT < O/RRT
 Subjects n Of 35 eligible participants, only 22 patients completed follow up testing – Wechsler Scales of Intelligence – Wide Range Achievement Test III Age 4. 1 -19. 0 years (median 8. 85) n 13 treated with SRT, 9 treated w/ RRT n
Subjects n Of 35 eligible participants, only 22 patients completed follow up testing – Wechsler Scales of Intelligence – Wide Range Achievement Test III Age 4. 1 -19. 0 years (median 8. 85) n 13 treated with SRT, 9 treated w/ RRT n
 Mulhern et al (1998)
Mulhern et al (1998)
 Mulhern et al (1998)
Mulhern et al (1998)
 Mulhern et al (1998)
Mulhern et al (1998)
 Mulhern et al (1998)
Mulhern et al (1998)
 Mulhern et al (1998)
Mulhern et al (1998)
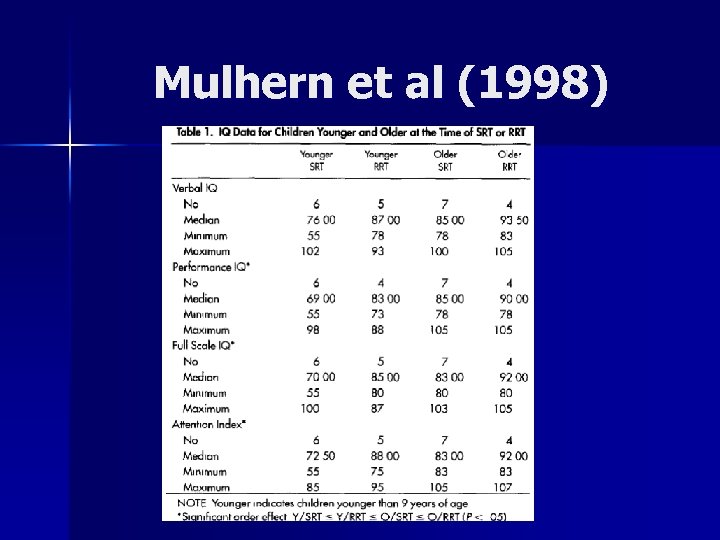
 Conclusions n n n Predicted ordering of distributions was seen for Performance IQ, Full Scale and Attention Index Unable to confirm significant differences in IQ change as a function of age or dose Distribution of scores was in the ordered direction for Reading and Arithmetic – 12/22 subjects were receiving or had received special educations services with similar proportions in each treatment group
Conclusions n n n Predicted ordering of distributions was seen for Performance IQ, Full Scale and Attention Index Unable to confirm significant differences in IQ change as a function of age or dose Distribution of scores was in the ordered direction for Reading and Arithmetic – 12/22 subjects were receiving or had received special educations services with similar proportions in each treatment group
 Limitations n Small numbers, low power, dichtomization of continuous variables n No longitudinal analysis
Limitations n Small numbers, low power, dichtomization of continuous variables n No longitudinal analysis
 Studies of Neurocognitive Decline
Studies of Neurocognitive Decline
 Question n What is the pattern of neurocognitive loss? n Loss vs. lack of gain vs. both?
Question n What is the pattern of neurocognitive loss? n Loss vs. lack of gain vs. both?
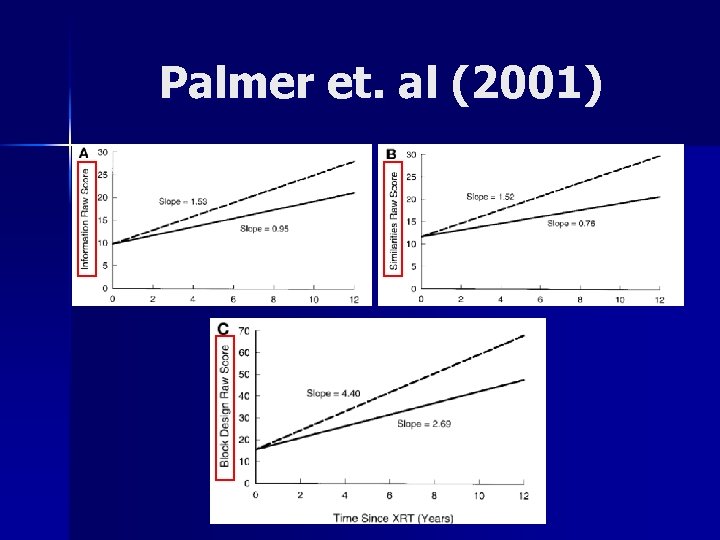
 Palmer et al. ( 2001 )- Patterns of Intellectual Development Among Survivors of Pediatric Medulloblastoma: A Longitudinal Analysis n Children could lose previously acquired information and skills, similar to adult dementia conditions OR n Children could continue to acquire new information and skills but at a slower rate than healthy age-related peers Palmer et al. ( Patterns of Intellectual Development Among Survivors of Pediatric Medulloblastoma: A Longitudinal Analysis Journal of Clinical Oncology, Vol 19, No 8 (April 15), 2001: pp 2302 -2308
Palmer et al. ( 2001 )- Patterns of Intellectual Development Among Survivors of Pediatric Medulloblastoma: A Longitudinal Analysis n Children could lose previously acquired information and skills, similar to adult dementia conditions OR n Children could continue to acquire new information and skills but at a slower rate than healthy age-related peers Palmer et al. ( Patterns of Intellectual Development Among Survivors of Pediatric Medulloblastoma: A Longitudinal Analysis Journal of Clinical Oncology, Vol 19, No 8 (April 15), 2001: pp 2302 -2308
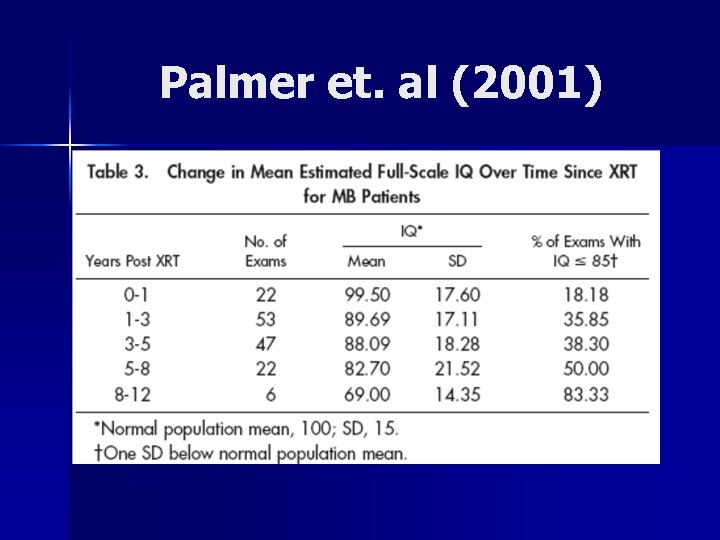
 Palmer et. al (2001) n 44 Patients – Histologically confirmed MB before age 17 – More than 1 psychological follow up with testing – No evidence of progressive disease n CSI Dosages – 33 treated with 35. 2 -38. 4 – 7 treated with 23. 4 -25 Gy – 4 treated with >40 Gy n All received posterior fossa boost 49. 2 -55. 8
Palmer et. al (2001) n 44 Patients – Histologically confirmed MB before age 17 – More than 1 psychological follow up with testing – No evidence of progressive disease n CSI Dosages – 33 treated with 35. 2 -38. 4 – 7 treated with 23. 4 -25 Gy – 4 treated with >40 Gy n All received posterior fossa boost 49. 2 -55. 8
 Palmer et. al (2001) Median 3 examinations per patient n Age Range at treatment: 1. 73 -12. 88 (mean 7. 84) n Years since XRT: 1. 9 -12. 6 (mean 5. 2) n
Palmer et. al (2001) Median 3 examinations per patient n Age Range at treatment: 1. 73 -12. 88 (mean 7. 84) n Years since XRT: 1. 9 -12. 6 (mean 5. 2) n
 Palmer et. al (2001)
Palmer et. al (2001)
 Palmer et. al (2001)
Palmer et. al (2001)
 Palmer et. al (2001)
Palmer et. al (2001)
 Palmer et. al (2001)
Palmer et. al (2001)
 Palmer et. al (2001)
Palmer et. al (2001)
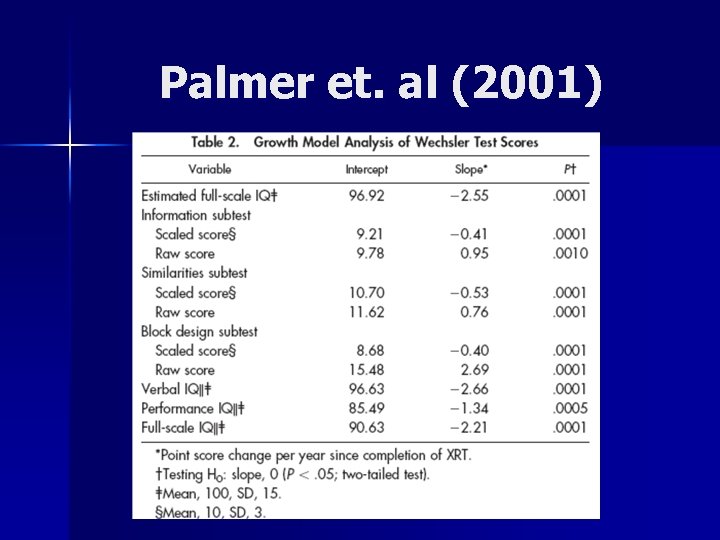
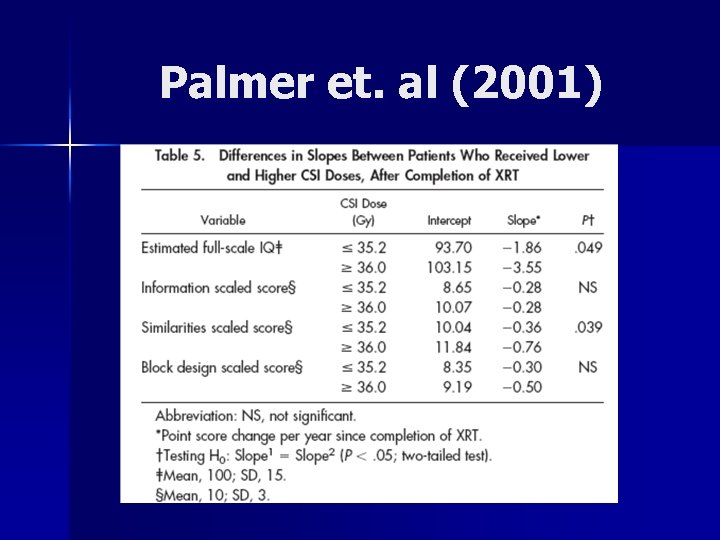
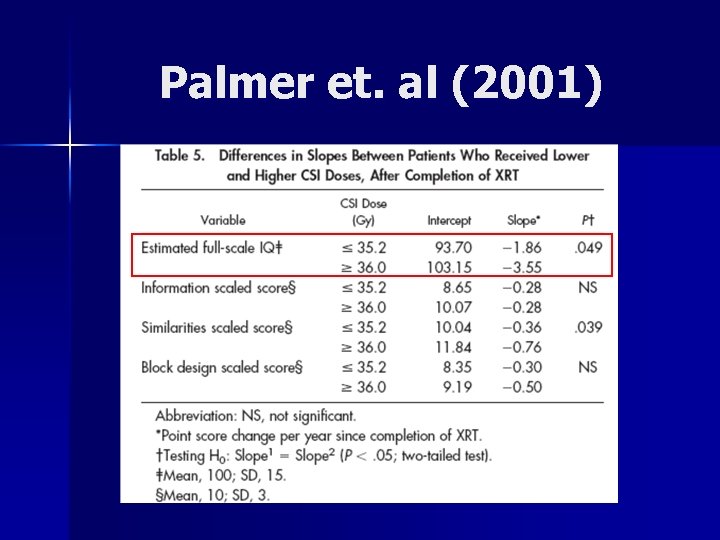
 Conclusion of Palmer Paper Declining pattern of functioning over time since completion of XRT n Patients continue to acquire new knowledge but at a fraction of the rate n Age at XRT ( <8. 02 vs >8. 02) was an effect modifier n CSI dose (<35. 2 vs >36. 0) were significantly different in their effects on IQ n
Conclusion of Palmer Paper Declining pattern of functioning over time since completion of XRT n Patients continue to acquire new knowledge but at a fraction of the rate n Age at XRT ( <8. 02 vs >8. 02) was an effect modifier n CSI dose (<35. 2 vs >36. 0) were significantly different in their effects on IQ n
 As technology changes, can we develop better predictive models for cognitive decline?
As technology changes, can we develop better predictive models for cognitive decline?
 Merchant et al. (2006) Modelling Radiation Dosimetry to Predict Cognitive Outcomes n Some studies had shown no difference in cognitive decline when comparing doses – Conventional boost treatments to the entire posterior fossa 40% of the entire brain receiving prescribed dose of 54 -55. 8 Gy (Mulhern et al 2004) n In an effort to reduce radiation dose and volume, attention now focuses on the manner in which the primary site is treated Merchant et al. Modeling Radiation dosimetry to predict cognitive outcomes in pediatric patients with CNS embryonal tumors including medulloblastoma. Int. J. Radiation Oncology bio. Phys. Vol 65, No 1, pp 210 -221, 2006
Merchant et al. (2006) Modelling Radiation Dosimetry to Predict Cognitive Outcomes n Some studies had shown no difference in cognitive decline when comparing doses – Conventional boost treatments to the entire posterior fossa 40% of the entire brain receiving prescribed dose of 54 -55. 8 Gy (Mulhern et al 2004) n In an effort to reduce radiation dose and volume, attention now focuses on the manner in which the primary site is treated Merchant et al. Modeling Radiation dosimetry to predict cognitive outcomes in pediatric patients with CNS embryonal tumors including medulloblastoma. Int. J. Radiation Oncology bio. Phys. Vol 65, No 1, pp 210 -221, 2006
 Volume, not just dose SJMB 96 trial- Patients treated with 23. 4 Gy CSI with conformal posterior fossa radiation to 36 Gy and conformal primary site radiation to 55. 8 Gy had IQ decline of 2. 4 points per year n Similar patients treated with 23. 4 Gy CSI and conventional posterior fossa radiation to 55. 8 Gy had decline of 5. 2 IQ points per year n
Volume, not just dose SJMB 96 trial- Patients treated with 23. 4 Gy CSI with conformal posterior fossa radiation to 36 Gy and conformal primary site radiation to 55. 8 Gy had IQ decline of 2. 4 points per year n Similar patients treated with 23. 4 Gy CSI and conventional posterior fossa radiation to 55. 8 Gy had decline of 5. 2 IQ points per year n
 Merchant et al. (2006) n Goal: Model the effects of the entire distribution of dose to specific volumes of brain on longitudinal IQ after radiation therapy
Merchant et al. (2006) n Goal: Model the effects of the entire distribution of dose to specific volumes of brain on longitudinal IQ after radiation therapy
 Patients n 39 patients, newly diagnosed embryonal tumors – 14 average risk (<1. 5 cm 2 residual, M 0) – 25 high risk
Patients n 39 patients, newly diagnosed embryonal tumors – 14 average risk (<1. 5 cm 2 residual, M 0) – 25 high risk
 Treatment Avg Risk: 23. 4 Gy CSI, conformal posterior fossa boost to 36 Gy and conformal primary-site boost to 55. 8 Gy n High Risk: 36 -39. 6 Gy CSI with conformal primary-site boost to 55. 8 Gy. n
Treatment Avg Risk: 23. 4 Gy CSI, conformal posterior fossa boost to 36 Gy and conformal primary-site boost to 55. 8 Gy n High Risk: 36 -39. 6 Gy CSI with conformal primary-site boost to 55. 8 Gy. n
 Testing n Neurocognitive testing performed at – Post surgery – 1 year – 2 years – 5 years
Testing n Neurocognitive testing performed at – Post surgery – 1 year – 2 years – 5 years
 Dosimetry n Composite Radiation Dosimetry – Merged 3 D CSI dosimetry with 3 D Primary site dosimetry n Normal volume contours made for – Total (entire) brain – Supratentorial brain – Infratentorial brain – Temporal lobes n Dose volume data then extracted
Dosimetry n Composite Radiation Dosimetry – Merged 3 D CSI dosimetry with 3 D Primary site dosimetry n Normal volume contours made for – Total (entire) brain – Supratentorial brain – Infratentorial brain – Temporal lobes n Dose volume data then extracted
 Statistical Analysis n Linear Mixed Model with Random Coefficients – IQ = dependent variable – Distribution of dose divided into intervals – Covariates n Fractional volume receiving dose over specified interval n Age, extent of disease, risk classification
Statistical Analysis n Linear Mixed Model with Random Coefficients – IQ = dependent variable – Distribution of dose divided into intervals – Covariates n Fractional volume receiving dose over specified interval n Age, extent of disease, risk classification
 Part 1 n Determine effect of dose-volume distribution on the change in IQ score over 5 different volumes of brain tissue – Total Brain – Supratentorial Brain – Infratentorial Brain – Temporal lobes (right and left)
Part 1 n Determine effect of dose-volume distribution on the change in IQ score over 5 different volumes of brain tissue – Total Brain – Supratentorial Brain – Infratentorial Brain – Temporal lobes (right and left)
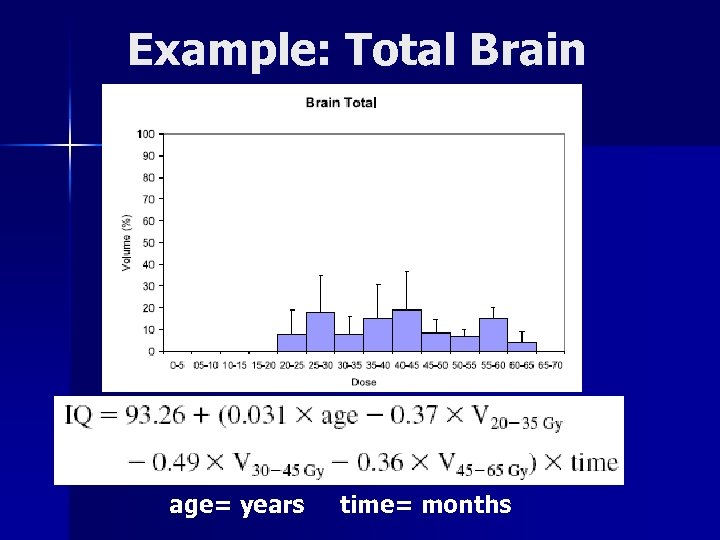 Example: Total Brain age= years time= months
Example: Total Brain age= years time= months
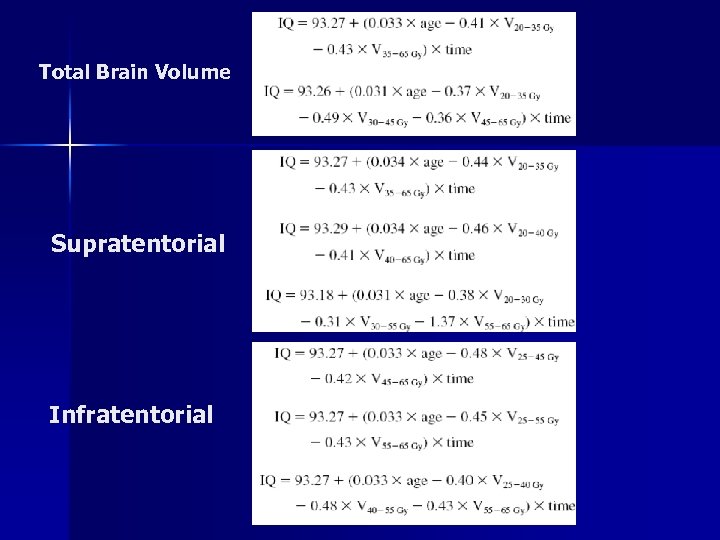 Total Brain Volume Supratentorial Infratentorial
Total Brain Volume Supratentorial Infratentorial
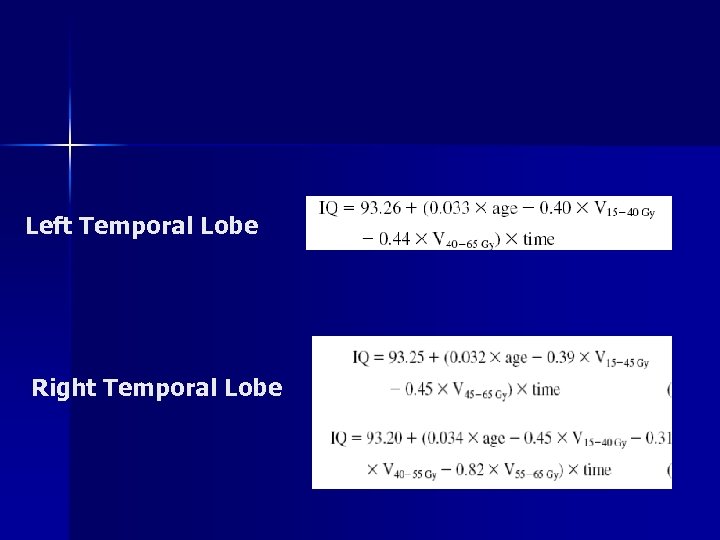 Left Temporal Lobe Right Temporal Lobe
Left Temporal Lobe Right Temporal Lobe
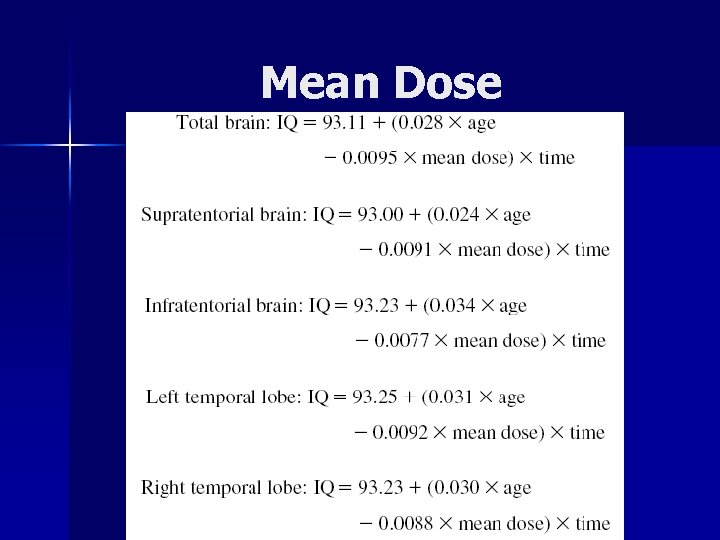 Mean Dose
Mean Dose
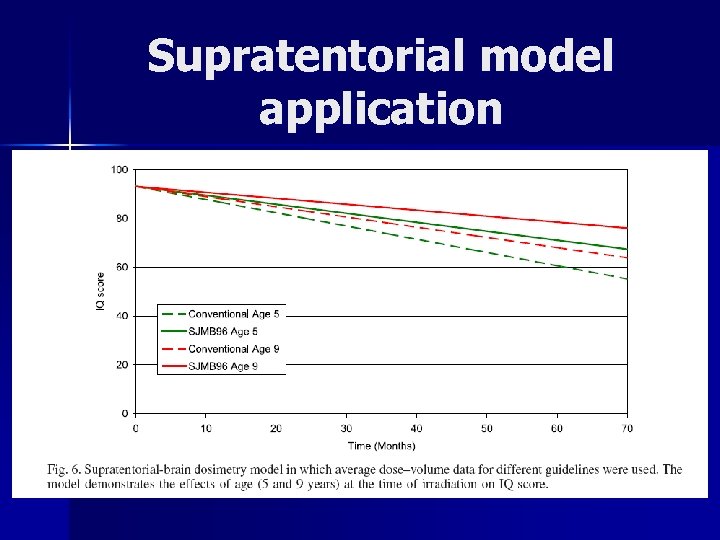 Supratentorial model application
Supratentorial model application
 Conclusions of Merchant et al. n Prediction of outcomes on basis of CSI dose alone will lose relevance over time – They’re approach is but one, requiring further validation n Limitations – Assumption of linearity – Limited follow up – Inability to account for other factors that might affect patient outcome
Conclusions of Merchant et al. n Prediction of outcomes on basis of CSI dose alone will lose relevance over time – They’re approach is but one, requiring further validation n Limitations – Assumption of linearity – Limited follow up – Inability to account for other factors that might affect patient outcome
 So what can we do?
So what can we do?
 Cognitive Remediation Luria-the brain is not a static organ and functional reorganization of neuro pathways can occur after a CNS insult n NIH consensus statement in 1998 supports use of cognitive rehabilitation n Educational intervention has been shown to be effective in addressing academic delays in children treated with cranial radiation for ALL n Anderson VA et. Al. Cognitive and academic outcome following cranial irradiation and chemotherapy in children: A longitudinal study. Br J Cancer 82: 255 -262
Cognitive Remediation Luria-the brain is not a static organ and functional reorganization of neuro pathways can occur after a CNS insult n NIH consensus statement in 1998 supports use of cognitive rehabilitation n Educational intervention has been shown to be effective in addressing academic delays in children treated with cranial radiation for ALL n Anderson VA et. Al. Cognitive and academic outcome following cranial irradiation and chemotherapy in children: A longitudinal study. Br J Cancer 82: 255 -262
 Ecological Importance of educating patients, caretakers, PCPs and teachers n Classroom accommodations n Impact of child’s disease on the family n
Ecological Importance of educating patients, caretakers, PCPs and teachers n Classroom accommodations n Impact of child’s disease on the family n
 Pharmacotherapy Mulhern et al. (2004) study of 83 ALL and BT survivors n Methylphenidate n – Double blind, 3 week home crossover study – Placebo vs. 0. 3 mg/kg vs. 0. 6 mg/kg Compared to placebo, parents and teachers reported attentional and social improvements n Ultimate effect on academic achievement? n Mulhern RK et al. Short-term efficacy of methylphenidate: a randomized, double-blind, placebo-controlled trial among survivors of childhood cancer. J Clin Oncol. 2004 Dec 1; 22(23): 4795 -803
Pharmacotherapy Mulhern et al. (2004) study of 83 ALL and BT survivors n Methylphenidate n – Double blind, 3 week home crossover study – Placebo vs. 0. 3 mg/kg vs. 0. 6 mg/kg Compared to placebo, parents and teachers reported attentional and social improvements n Ultimate effect on academic achievement? n Mulhern RK et al. Short-term efficacy of methylphenidate: a randomized, double-blind, placebo-controlled trial among survivors of childhood cancer. J Clin Oncol. 2004 Dec 1; 22(23): 4795 -803
 Conclusions Clear association between radiation therapy and cognitive decline n Decline appears to be progressive n Continued research with larger sample sizes and validation of predictive models n Important point to address initially and during follow up n
Conclusions Clear association between radiation therapy and cognitive decline n Decline appears to be progressive n Continued research with larger sample sizes and validation of predictive models n Important point to address initially and during follow up n
 Thanks!
Thanks!
 Additional Slides
Additional Slides
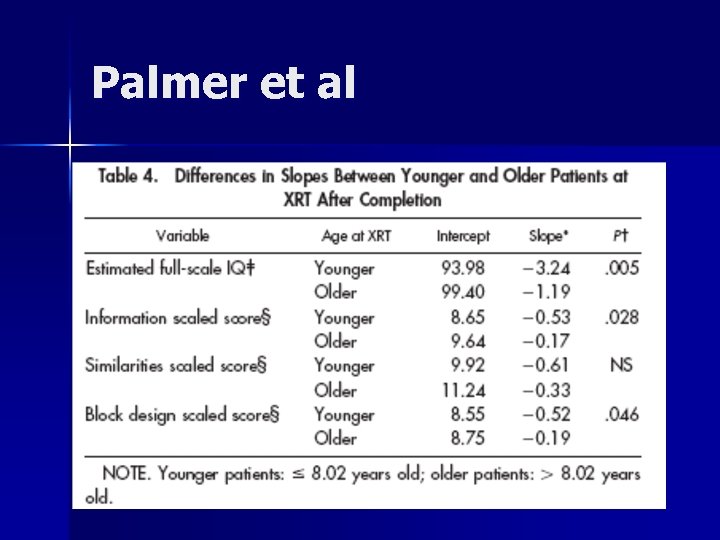 Palmer et al
Palmer et al
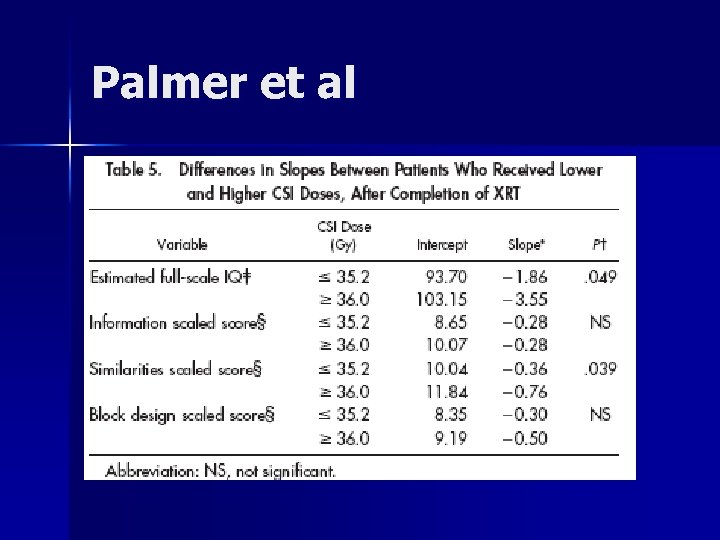 Palmer et al
Palmer et al
 Ris et al. (2001) Intellectual Outcome After Reduced-Dose Radiation Therapy Plus Adjuvant Chemotherapy for Medulloblastoma: A Children’s Cancer Group Study. J Clin Oncol 19: 3470 -3476.
Ris et al. (2001) Intellectual Outcome After Reduced-Dose Radiation Therapy Plus Adjuvant Chemotherapy for Medulloblastoma: A Children’s Cancer Group Study. J Clin Oncol 19: 3470 -3476.
 n n n Recently, treatment protocols have been developed to reduce this morbidity. This can be accomplished by simply decreasing the overall dose of RT to the brain or by combining such reductions in RT dose with adjuvant chemotherapy. Such approaches have shown promise in producing survival and tumor recurrence rates comparable to those of conventional therapy Deutsch M, Thomas PR, Krischer J, et al: Results of a prospective randomized trial comparing standard dose neuraxis irradiation (3600 c. Gy/20) with reduced neuraxis irradiation (2340 c. Gy/13) in patients with low-stage medulloblastoma: A combined Children’s Cancer Group-Pediatric Oncology Group Study. Pediatr Neurosurg 24: 167 -177, 1996 Bailey CC, Gnekow A, Wellek S: Prospective randomised trial of chemotherapy given before radiotherapy in childhood medulloblastoma: International Society of Paediatric Oncology (SIOP) and the (German) Society of Paediatric Oncology (GPO)—SIOP II. Med Pediatr Oncol 25: 166 -178, 1995
n n n Recently, treatment protocols have been developed to reduce this morbidity. This can be accomplished by simply decreasing the overall dose of RT to the brain or by combining such reductions in RT dose with adjuvant chemotherapy. Such approaches have shown promise in producing survival and tumor recurrence rates comparable to those of conventional therapy Deutsch M, Thomas PR, Krischer J, et al: Results of a prospective randomized trial comparing standard dose neuraxis irradiation (3600 c. Gy/20) with reduced neuraxis irradiation (2340 c. Gy/13) in patients with low-stage medulloblastoma: A combined Children’s Cancer Group-Pediatric Oncology Group Study. Pediatr Neurosurg 24: 167 -177, 1996 Bailey CC, Gnekow A, Wellek S: Prospective randomised trial of chemotherapy given before radiotherapy in childhood medulloblastoma: International Society of Paediatric Oncology (SIOP) and the (German) Society of Paediatric Oncology (GPO)—SIOP II. Med Pediatr Oncol 25: 166 -178, 1995
 Script your long term side effect discussion for… n 7 year old boy, newly diagnosed medulloblastoma
Script your long term side effect discussion for… n 7 year old boy, newly diagnosed medulloblastoma
 Script your long term side effect discussion for… n 7 year old boy, newly diagnosed medulloblastoma n 65 year old woman, newly diagnosed CNS lymphoma
Script your long term side effect discussion for… n 7 year old boy, newly diagnosed medulloblastoma n 65 year old woman, newly diagnosed CNS lymphoma
 Pharmacotherapy n n Meyers et al. - 30 patients with malignant gliomas exhibiting neurobehavioral slowing All patients met the DSM IV criteria for personality change secondary to medical condition 5 mg of MPH BID and titrated up by 10 mg every 2 weeks Dramatic improvement in psychomotor speed, memory , executive functioning, mood and ADLs were seen even in with progressive disease. Meyers CA, Weitzner MA, Valentine AD, Levin VA. Methylphenidate therapy improves cognition, mood, and function of brain tumor patients. J Clin Oncol. 1998 Jul; 16(7): 2522 -7.
Pharmacotherapy n n Meyers et al. - 30 patients with malignant gliomas exhibiting neurobehavioral slowing All patients met the DSM IV criteria for personality change secondary to medical condition 5 mg of MPH BID and titrated up by 10 mg every 2 weeks Dramatic improvement in psychomotor speed, memory , executive functioning, mood and ADLs were seen even in with progressive disease. Meyers CA, Weitzner MA, Valentine AD, Levin VA. Methylphenidate therapy improves cognition, mood, and function of brain tumor patients. J Clin Oncol. 1998 Jul; 16(7): 2522 -7.


