СТОМАТ 1.ppt
- Количество слайдов: 64
 Nervous System functions The nervous system serves three basic functions: Sensory Receptors monitor internal and external environment Integrative Processes sensory information and makes decisions for appropriate responses Motor Responds to integration decisions by signalling effectors
Nervous System functions The nervous system serves three basic functions: Sensory Receptors monitor internal and external environment Integrative Processes sensory information and makes decisions for appropriate responses Motor Responds to integration decisions by signalling effectors
 MOTOR SYSTEM § VOLUNTARY MOVEMENTS.
MOTOR SYSTEM § VOLUNTARY MOVEMENTS.
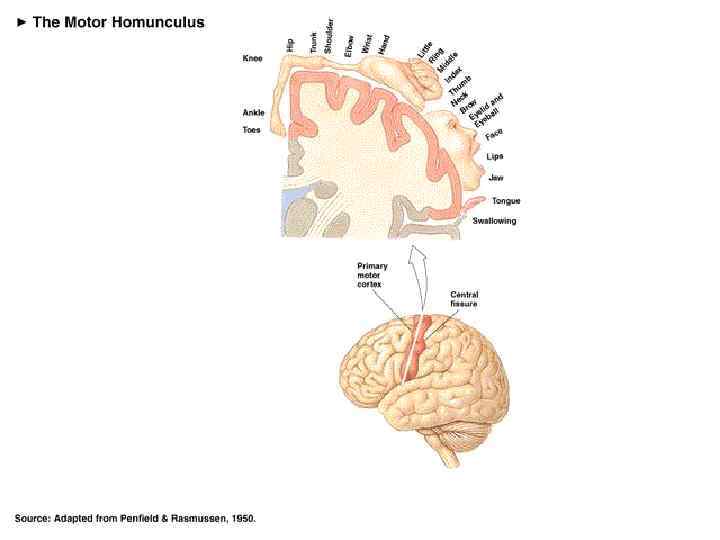
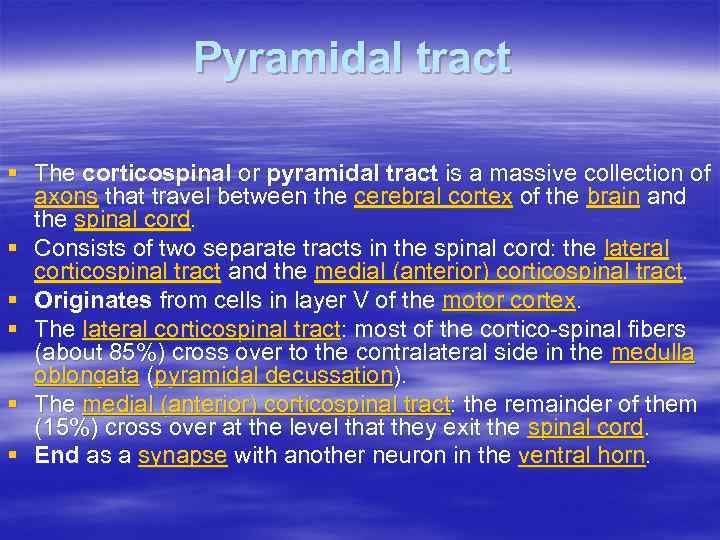 Pyramidal tract § The corticospinal or pyramidal tract is a massive collection of axons that travel between the cerebral cortex of the brain and the spinal cord. § Consists of two separate tracts in the spinal cord: the lateral corticospinal tract and the medial (anterior) corticospinal tract. § Originates from cells in layer V of the motor cortex. § The lateral corticospinal tract: most of the cortico-spinal fibers (about 85%) cross over to the contralateral side in the medulla oblongata (pyramidal decussation). § The medial (anterior) corticospinal tract: the remainder of them (15%) cross over at the level that they exit the spinal cord. § End as a synapse with another neuron in the ventral horn.
Pyramidal tract § The corticospinal or pyramidal tract is a massive collection of axons that travel between the cerebral cortex of the brain and the spinal cord. § Consists of two separate tracts in the spinal cord: the lateral corticospinal tract and the medial (anterior) corticospinal tract. § Originates from cells in layer V of the motor cortex. § The lateral corticospinal tract: most of the cortico-spinal fibers (about 85%) cross over to the contralateral side in the medulla oblongata (pyramidal decussation). § The medial (anterior) corticospinal tract: the remainder of them (15%) cross over at the level that they exit the spinal cord. § End as a synapse with another neuron in the ventral horn.
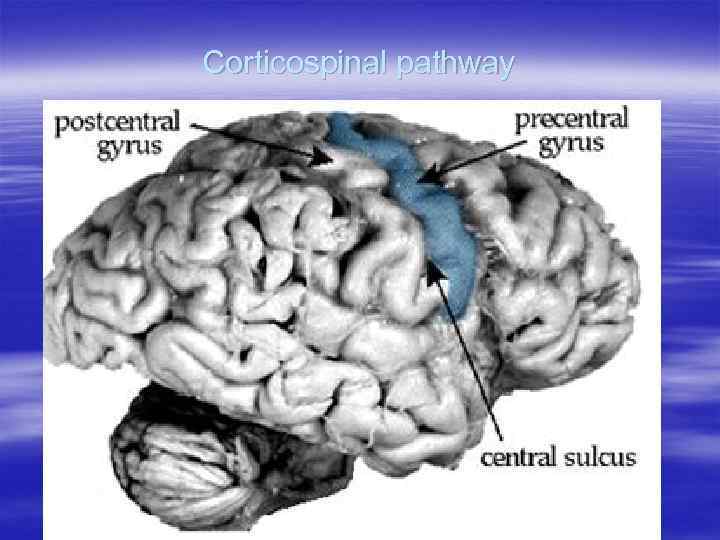 Corticospinal pathway
Corticospinal pathway
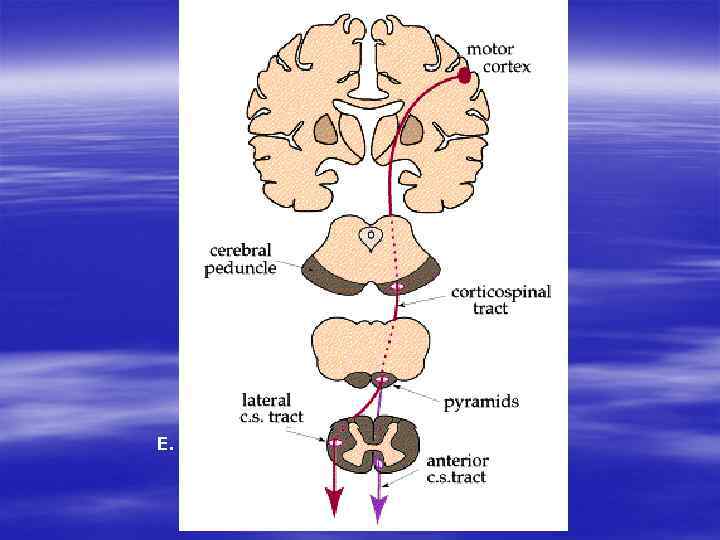 E. Clinical notes:
E. Clinical notes:
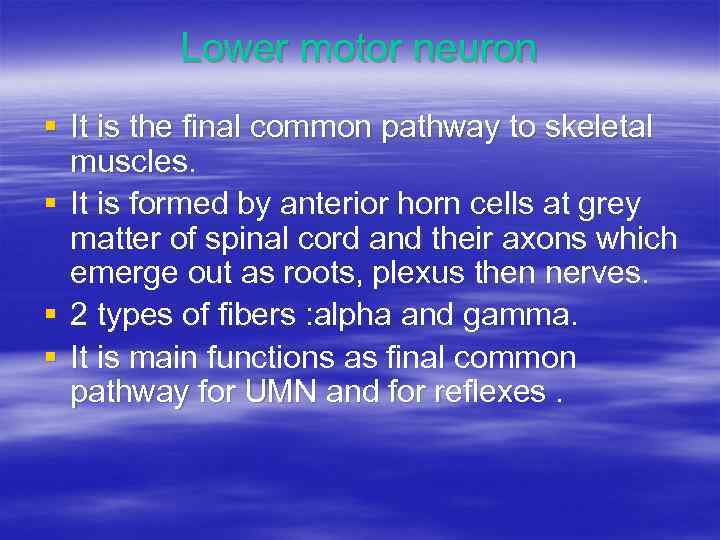 Lower motor neuron § It is the final common pathway to skeletal muscles. § It is formed by anterior horn cells at grey matter of spinal cord and their axons which emerge out as roots, plexus then nerves. § 2 types of fibers : alpha and gamma. § It is main functions as final common pathway for UMN and for reflexes.
Lower motor neuron § It is the final common pathway to skeletal muscles. § It is formed by anterior horn cells at grey matter of spinal cord and their axons which emerge out as roots, plexus then nerves. § 2 types of fibers : alpha and gamma. § It is main functions as final common pathway for UMN and for reflexes.
 A reflex is involuntary, stereotyped pattern of response brought about by a sensory stimulus.
A reflex is involuntary, stereotyped pattern of response brought about by a sensory stimulus.
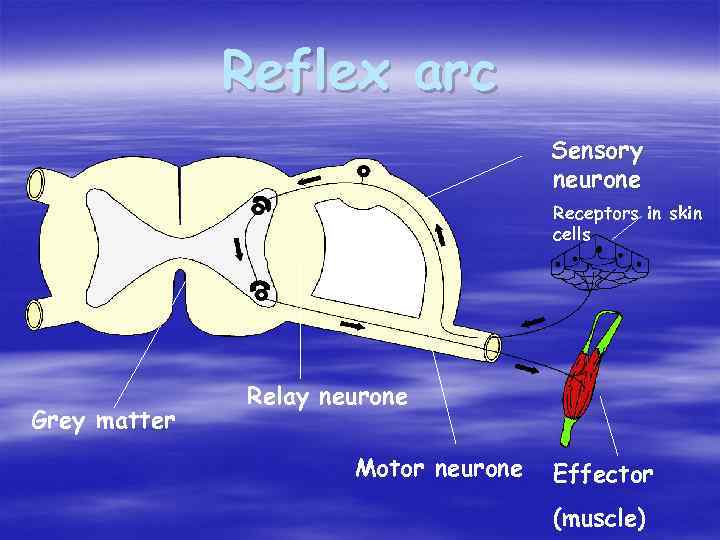 Reflex arc Sensory neurone Receptors in skin cells Grey matter Relay neurone Motor neurone Effector (muscle)
Reflex arc Sensory neurone Receptors in skin cells Grey matter Relay neurone Motor neurone Effector (muscle)
 The different reflex responses may be grouped into 2 categories on the basis of their clinical significance. 1) Normal (physiological) reflexes – 2) present during normal functioning of motor pathways. 2) Abnormal (pathological) reflexes – appear if upper motor neurone are damaged.
The different reflex responses may be grouped into 2 categories on the basis of their clinical significance. 1) Normal (physiological) reflexes – 2) present during normal functioning of motor pathways. 2) Abnormal (pathological) reflexes – appear if upper motor neurone are damaged.
 The normal reflexes are classified on two categories 1) Superficial reflexes. a) cutaneos; b) mucous. 2) Deep reflexes. a) tendons b) periostal.
The normal reflexes are classified on two categories 1) Superficial reflexes. a) cutaneos; b) mucous. 2) Deep reflexes. a) tendons b) periostal.
 Paresis - partial loss of voluntary motor control; weakness Paralysis - complete loss of voluntary motor control.
Paresis - partial loss of voluntary motor control; weakness Paralysis - complete loss of voluntary motor control.
 Monoparesis - this is weakness limited to a single arm or leg. Hemiparesis - this is weakness on one side of the body so that the arm and leg on that side are both weak. Sometimes one side of the face can also be weak. Paraparesis - this is weakness limited to the arms or legs. Tetraparesis – this is weakness of all extremities.
Monoparesis - this is weakness limited to a single arm or leg. Hemiparesis - this is weakness on one side of the body so that the arm and leg on that side are both weak. Sometimes one side of the face can also be weak. Paraparesis - this is weakness limited to the arms or legs. Tetraparesis – this is weakness of all extremities.
 Muscle tone - the normal, ongoing tension in a muscle; measured by resistance of a muscle to passive stretching.
Muscle tone - the normal, ongoing tension in a muscle; measured by resistance of a muscle to passive stretching.
 Upper motor neuron lesions § Symptoms : 1. Paralysis : 2. Spasticity : – Exaggerated tendon reflex resulting in increases resistance. – More in flexor of arm and extensor of leg (antigravity muscle). – Clasp-knife – Explained by loss of inhibitory descending pathway and increase in gamma neuron sensitivity.
Upper motor neuron lesions § Symptoms : 1. Paralysis : 2. Spasticity : – Exaggerated tendon reflex resulting in increases resistance. – More in flexor of arm and extensor of leg (antigravity muscle). – Clasp-knife – Explained by loss of inhibitory descending pathway and increase in gamma neuron sensitivity.
 3. Hyper reflexa: – Clonus – Spread reflexes – Explained like the spasticity. 4. Babinisky sign: nociceptive spinal flexion reflex.
3. Hyper reflexa: – Clonus – Spread reflexes – Explained like the spasticity. 4. Babinisky sign: nociceptive spinal flexion reflex.
 Lower motor neuron lesions § Symptoms: 1. Flaccidity : – No tone 2. Hypotonia. 3. Muscle Atrophy. (denervation atrophy). 4. Areflexia. 5. Paresis or plegia. 6. Fasciculation.
Lower motor neuron lesions § Symptoms: 1. Flaccidity : – No tone 2. Hypotonia. 3. Muscle Atrophy. (denervation atrophy). 4. Areflexia. 5. Paresis or plegia. 6. Fasciculation.
 CEREBELLUM Functions: § motor coordination § posture, balance § influences muscle tone § synergia (the interplay between agonist and antagonist muscle groups).
CEREBELLUM Functions: § motor coordination § posture, balance § influences muscle tone § synergia (the interplay between agonist and antagonist muscle groups).
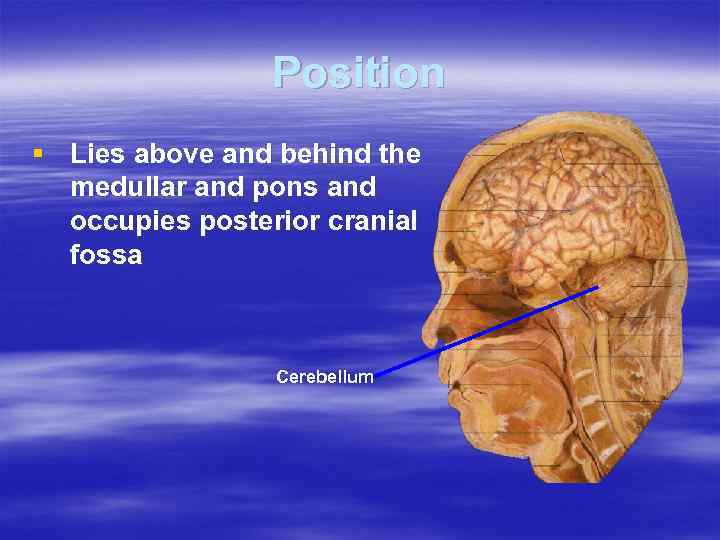 Position § Lies above and behind the medullar and pons and occupies posterior cranial fossa Cerebellum
Position § Lies above and behind the medullar and pons and occupies posterior cranial fossa Cerebellum
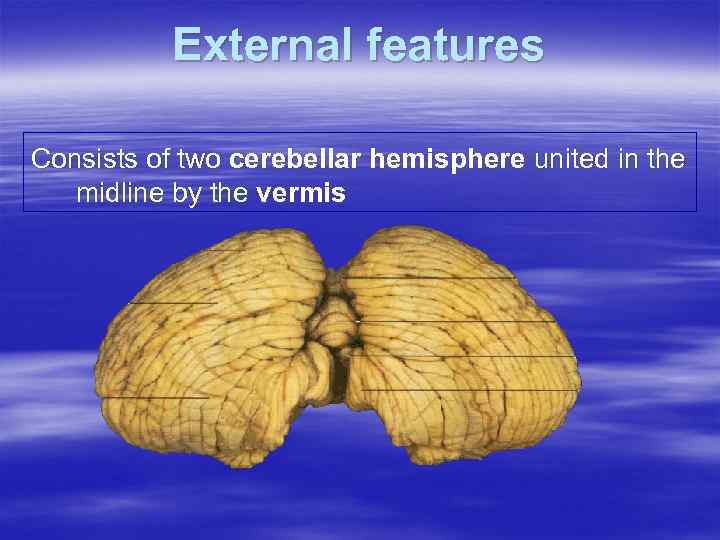 External features Consists of two cerebellar hemisphere united in the midline by the vermis
External features Consists of two cerebellar hemisphere united in the midline by the vermis
 Dyssynergia. Incoordination results in loss of smoothness of execution of a motor activity. Rebound Reflex The patient is unable to stop flexion of the arm on sudden release so the arm may strike the chest and doesn't recoil to the initial position. This is most likely due to failure of timely triceps contraction. Dysmetria. Inaccurate movements due to faulty judgment of distance (results in overshooting or undershooting of a target while attempting to reach an object). Error in Judgment of Range and Distance of Target
Dyssynergia. Incoordination results in loss of smoothness of execution of a motor activity. Rebound Reflex The patient is unable to stop flexion of the arm on sudden release so the arm may strike the chest and doesn't recoil to the initial position. This is most likely due to failure of timely triceps contraction. Dysmetria. Inaccurate movements due to faulty judgment of distance (results in overshooting or undershooting of a target while attempting to reach an object). Error in Judgment of Range and Distance of Target
 Dysequilibrium. It is a results in balance problems, and the patient falls to the affected side. Romberg Test perform by having the patient stand still with their heels together. Ask the patient to remain still and close their eyes. If the patient loses their balance, the test is positive. Dysdiadochokinesis. Inability to perform rapid alternating movements (a disturbance of the normal ability to make repeated supinations and pronations of the lower arms).
Dysequilibrium. It is a results in balance problems, and the patient falls to the affected side. Romberg Test perform by having the patient stand still with their heels together. Ask the patient to remain still and close their eyes. If the patient loses their balance, the test is positive. Dysdiadochokinesis. Inability to perform rapid alternating movements (a disturbance of the normal ability to make repeated supinations and pronations of the lower arms).
 Intention tremor. Tremor that occurs while performing a voluntary motor act and accelerates in pace on approaching the target. There are next probes for examinations of tremor: Toe-to-finger Finger-to-nose Heel-to-shin Scanning speech. It is characterized by poor modulation of the volume and pitch of the speech (speech is slow and slurred) with occasionally sudden unexpected force (explosive speech).
Intention tremor. Tremor that occurs while performing a voluntary motor act and accelerates in pace on approaching the target. There are next probes for examinations of tremor: Toe-to-finger Finger-to-nose Heel-to-shin Scanning speech. It is characterized by poor modulation of the volume and pitch of the speech (speech is slow and slurred) with occasionally sudden unexpected force (explosive speech).
 Nystagmus. It is involuntary movements of the eyeballs around their natural position (may be horizontal, vertical, rotational). Handwriting increases in size (macrographia).
Nystagmus. It is involuntary movements of the eyeballs around their natural position (may be horizontal, vertical, rotational). Handwriting increases in size (macrographia).
 CEREBELLAR GAIT A drunken gait is the style of walking that is seen in a patient with a cerebellar lesion. It is characterized by: - the feet are separated widely; - steps are jerky and unsure, varying in size; -the trunk sways forward; - patient may fall to the side of the lesion.
CEREBELLAR GAIT A drunken gait is the style of walking that is seen in a patient with a cerebellar lesion. It is characterized by: - the feet are separated widely; - steps are jerky and unsure, varying in size; -the trunk sways forward; - patient may fall to the side of the lesion.
 Basal Ganglia Masses of gray matter found deep within the cortical white matter. § The main nuclei of the basal ganglia are, the caudate and putamen (together called the "striatum" or “neostriatum”), the substantia nigra, the globus pallidus (divided into internal and external portions), and the subthalamic nucleus (together called the “pallidum" or “paleostriatum”). § Topographically the putamen and globus pallidus constitute the lentiform nucleus.
Basal Ganglia Masses of gray matter found deep within the cortical white matter. § The main nuclei of the basal ganglia are, the caudate and putamen (together called the "striatum" or “neostriatum”), the substantia nigra, the globus pallidus (divided into internal and external portions), and the subthalamic nucleus (together called the “pallidum" or “paleostriatum”). § Topographically the putamen and globus pallidus constitute the lentiform nucleus.
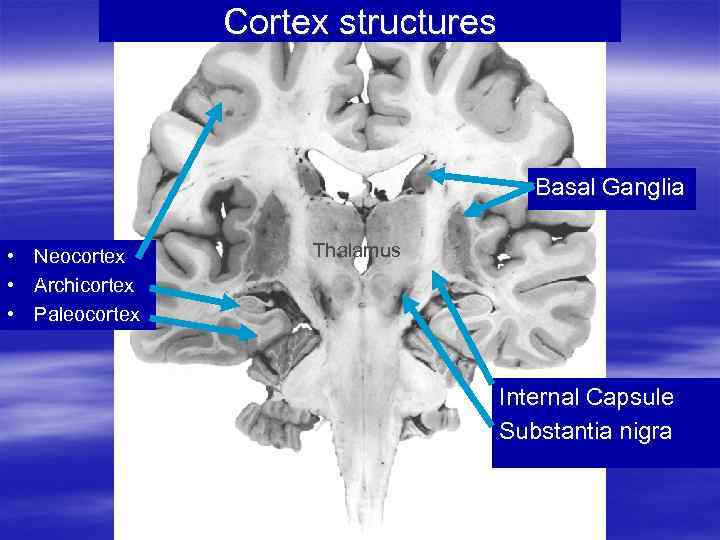 Cortex structures Basal Ganglia • Neocortex • Archicortex • Paleocortex Thalamus Internal Capsule Substantia nigra
Cortex structures Basal Ganglia • Neocortex • Archicortex • Paleocortex Thalamus Internal Capsule Substantia nigra
 Functions of Basal Ganglia § The main function of the basal ganglia is to initiate, correcting and stop movements, control of posture, controls muscle tone between different muscles’ group. § The basal ganglia also contribute to cognitive (i. e. , intelligence, knowledge, motor behavior and motor learning), affective (i. e. , emotional) and autonomic functions.
Functions of Basal Ganglia § The main function of the basal ganglia is to initiate, correcting and stop movements, control of posture, controls muscle tone between different muscles’ group. § The basal ganglia also contribute to cognitive (i. e. , intelligence, knowledge, motor behavior and motor learning), affective (i. e. , emotional) and autonomic functions.
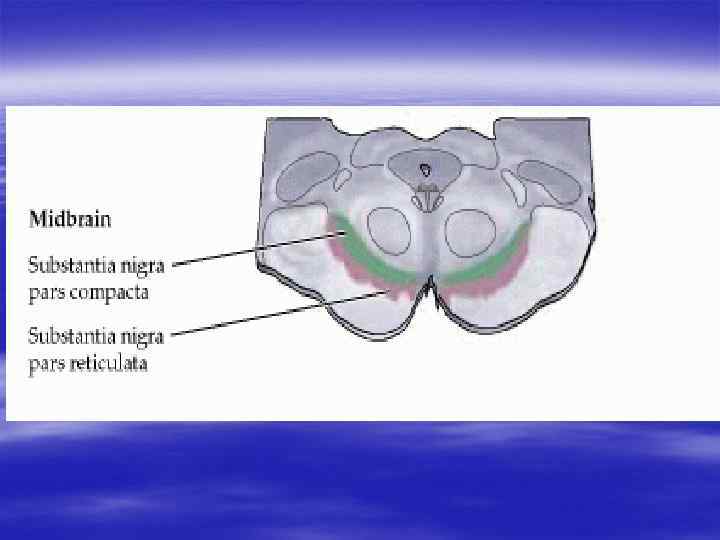
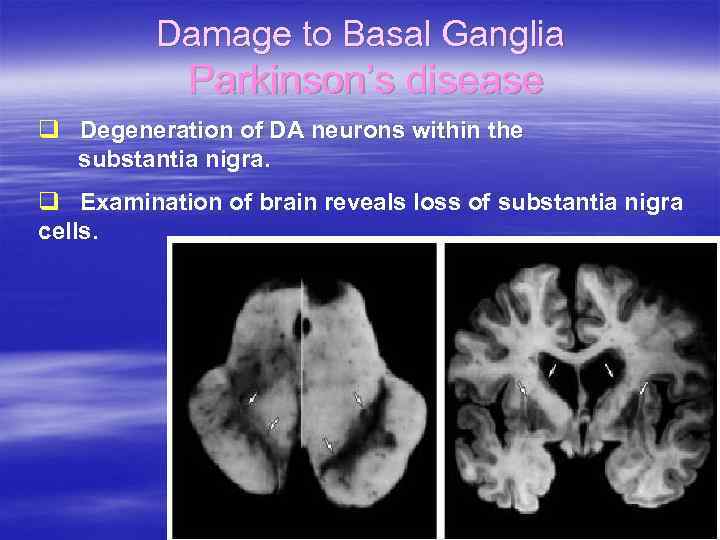 Damage to Basal Ganglia Parkinson’s disease q Degeneration of DA neurons within the substantia nigra. q Examination of brain reveals loss of substantia nigra cells.
Damage to Basal Ganglia Parkinson’s disease q Degeneration of DA neurons within the substantia nigra. q Examination of brain reveals loss of substantia nigra cells.
 Bradykinesia: pathologically slow movement, it produces: - reduced facial expression (mask-like) - reduced blinking - reduced adjustment of posture when seated. Kinesia paradoxica – when agitated the patient will move swiftly. Postural disturbance – flexion of limbs and trunk is associated with a failure to make quick postural adjustments to correct imbalance. The patients falls whilst turning or if pushed.
Bradykinesia: pathologically slow movement, it produces: - reduced facial expression (mask-like) - reduced blinking - reduced adjustment of posture when seated. Kinesia paradoxica – when agitated the patient will move swiftly. Postural disturbance – flexion of limbs and trunk is associated with a failure to make quick postural adjustments to correct imbalance. The patients falls whilst turning or if pushed.
 Tremor at rest ( «pill-rolling» , the thumb moving rhythmically backwards and forwards on the palm of the hand), decreasing with movements and disappears during sleep. Rigidity. Stiffness felt by examinator when passively moving a limb. This resistance is present to the same degree throughout the full range of movement, affecting flexor and extensor muscle groups equally and described as PLASTIC or LEAD PIPE rigidity. When tremor superimposed upon rigidity it produce a COGHWHEEL quality.
Tremor at rest ( «pill-rolling» , the thumb moving rhythmically backwards and forwards on the palm of the hand), decreasing with movements and disappears during sleep. Rigidity. Stiffness felt by examinator when passively moving a limb. This resistance is present to the same degree throughout the full range of movement, affecting flexor and extensor muscle groups equally and described as PLASTIC or LEAD PIPE rigidity. When tremor superimposed upon rigidity it produce a COGHWHEEL quality.
 Handwriting reduces in size (micrographia). Autonomic features occur – excessive sweating, greasy skin (seborrhoea), postural hypotension. Depression, dementia. Bradiphrenia.
Handwriting reduces in size (micrographia). Autonomic features occur – excessive sweating, greasy skin (seborrhoea), postural hypotension. Depression, dementia. Bradiphrenia.
 Parkinsonian gait. A parkinsonism gait is the manner of walking that is seen in patients with parkinsonism. Characteristics of this gait are: 1) hesitation in starting: akinesia 2) small, shuffling, hurried steps 3) lack of normal arm swing 5) kinesia paradoxica
Parkinsonian gait. A parkinsonism gait is the manner of walking that is seen in patients with parkinsonism. Characteristics of this gait are: 1) hesitation in starting: akinesia 2) small, shuffling, hurried steps 3) lack of normal arm swing 5) kinesia paradoxica
 The clinical syndromes of striatum’s impairment are associated with hyperkinetic (involuntary movements. ) There are conditions that consist of excessive and involuntary movement of the body’s parts.
The clinical syndromes of striatum’s impairment are associated with hyperkinetic (involuntary movements. ) There are conditions that consist of excessive and involuntary movement of the body’s parts.
 1. Chorea. 2. The term chorea means dance. 3. It refers to rapid, irregular, relatively small amplitude, 4. random-appearing, rather continuous, 5. non-stereotyped jerks, usually of the distal limbs. 2. Athetosis. 3. A wormlike, writhing, twisting movement, typically 4. of the limbs. 3. Choreo-Athetosis. A mix of 1 and 2.
1. Chorea. 2. The term chorea means dance. 3. It refers to rapid, irregular, relatively small amplitude, 4. random-appearing, rather continuous, 5. non-stereotyped jerks, usually of the distal limbs. 2. Athetosis. 3. A wormlike, writhing, twisting movement, typically 4. of the limbs. 3. Choreo-Athetosis. A mix of 1 and 2.
 4. Tremor: Rhythmic, oscillatory movements of distal parts of body, usually of the limbs. 5. Dystonia: Involuntary, sustained, patterned, and often repetitive muscle contractions of opposing muscles. Results in twisting, spasmodic or other abnormal postures of many body parts. Dystonias may be generalized (torsion dystonia) or partial (focal), for example, involuntary turning of the head by neck muscle contraction is referred to as Torticollis. 6. Tics: These are semi-involuntary, (often compulsive), repetitive, stereotyped movements (e. g. , facial grimace, eye squint, head flip, etc).
4. Tremor: Rhythmic, oscillatory movements of distal parts of body, usually of the limbs. 5. Dystonia: Involuntary, sustained, patterned, and often repetitive muscle contractions of opposing muscles. Results in twisting, spasmodic or other abnormal postures of many body parts. Dystonias may be generalized (torsion dystonia) or partial (focal), for example, involuntary turning of the head by neck muscle contraction is referred to as Torticollis. 6. Tics: These are semi-involuntary, (often compulsive), repetitive, stereotyped movements (e. g. , facial grimace, eye squint, head flip, etc).
 7. Hemiballismus: is a violent flinging movement of half of the body. It is associated with lesions of the subthalamic nucleus (ie, body of Louis). 8. Myoclonus: is a muscle jerk; it is a brief, generalized body-jerk, which is sometimes asymmetric. 9. Asterixis: is momentary loss of tone and flapping of the hand are seen when the patient extends his arms in front with the wrists dorsiflexed.
7. Hemiballismus: is a violent flinging movement of half of the body. It is associated with lesions of the subthalamic nucleus (ie, body of Louis). 8. Myoclonus: is a muscle jerk; it is a brief, generalized body-jerk, which is sometimes asymmetric. 9. Asterixis: is momentary loss of tone and flapping of the hand are seen when the patient extends his arms in front with the wrists dorsiflexed.
 Sensory modalities § General modalities: § Special 1 - Pain. 2 - Temperature. 3 - Touch: -simple touch. -discriminative touch. 4 - Pressure. 5 - Vibration. 6 - position: -conscious. -unconscious. modalities: 1 - Vision. 2 - Hearing. 3 - head position. 4 - Acceleration: -linear. -angular. 5 - Smell. 6 - Taste.
Sensory modalities § General modalities: § Special 1 - Pain. 2 - Temperature. 3 - Touch: -simple touch. -discriminative touch. 4 - Pressure. 5 - Vibration. 6 - position: -conscious. -unconscious. modalities: 1 - Vision. 2 - Hearing. 3 - head position. 4 - Acceleration: -linear. -angular. 5 - Smell. 6 - Taste.
 TYPES OF SENSATION Exteroceptive Proprioceptive Interoceptive (By Ch. Sherrington)
TYPES OF SENSATION Exteroceptive Proprioceptive Interoceptive (By Ch. Sherrington)
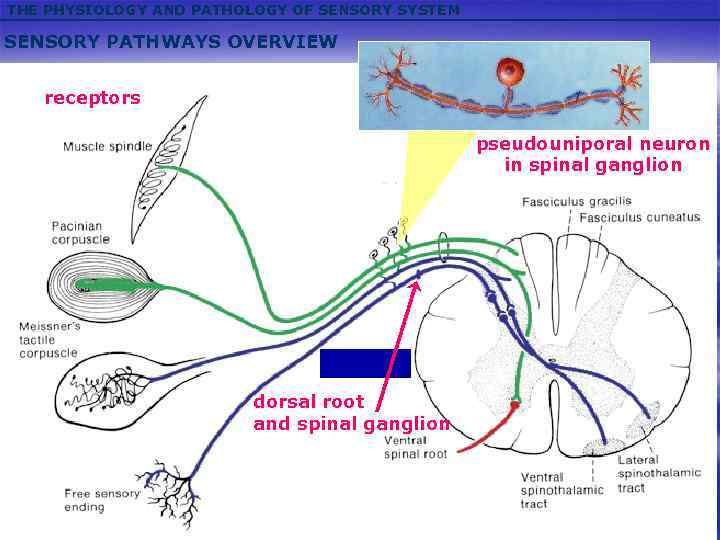 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM SENSORY PATHWAYS OVERVIEW receptors pseudouniporal neuron in spinal ganglion dorsal root and spinal ganglion
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM SENSORY PATHWAYS OVERVIEW receptors pseudouniporal neuron in spinal ganglion dorsal root and spinal ganglion
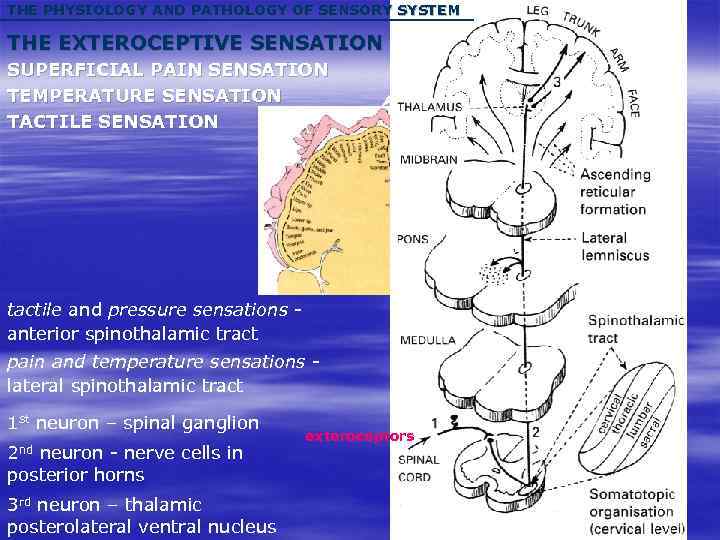 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM THE EXTEROCEPTIVE SENSATION SUPERFICIAL PAIN SENSATION TEMPERATURE SENSATION TACTILE SENSATION tactile and pressure sensations anterior spinothalamic tract pain and temperature sensations lateral spinothalamic tract 1 st neuron – spinal ganglion 2 nd neuron - nerve cells in posterior horns 3 rd neuron – thalamic posterolateral ventral nucleus exteroceptors
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM THE EXTEROCEPTIVE SENSATION SUPERFICIAL PAIN SENSATION TEMPERATURE SENSATION TACTILE SENSATION tactile and pressure sensations anterior spinothalamic tract pain and temperature sensations lateral spinothalamic tract 1 st neuron – spinal ganglion 2 nd neuron - nerve cells in posterior horns 3 rd neuron – thalamic posterolateral ventral nucleus exteroceptors
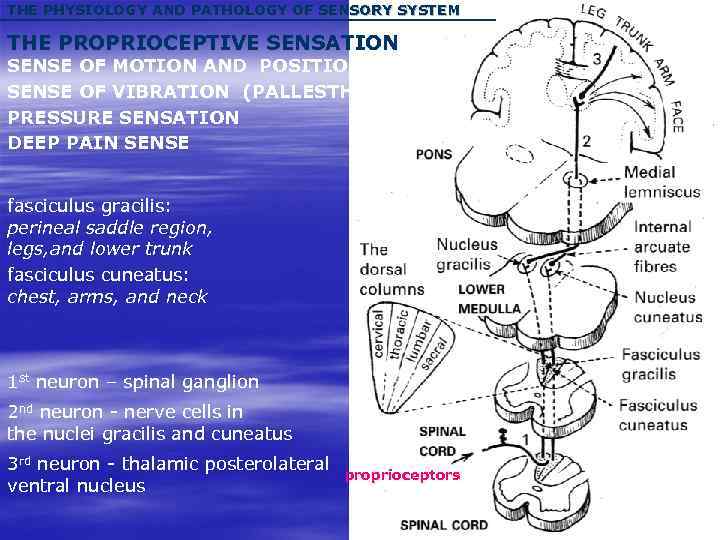 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM THE PROPRIOCEPTIVE SENSATION SENSE OF MOTION AND POSITION SENSE OF VIBRATION (PALLESTHESIA) PRESSURE SENSATION DEEP PAIN SENSE fasciculus gracilis: perineal saddle region, legs, and lower trunk fasciculus cuneatus: chest, arms, and neck 1 st neuron – spinal ganglion 2 nd neuron - nerve cells in the nuclei gracilis and cuneatus 3 rd neuron - thalamic posterolateral ventral nucleus proprioceptors
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM THE PROPRIOCEPTIVE SENSATION SENSE OF MOTION AND POSITION SENSE OF VIBRATION (PALLESTHESIA) PRESSURE SENSATION DEEP PAIN SENSE fasciculus gracilis: perineal saddle region, legs, and lower trunk fasciculus cuneatus: chest, arms, and neck 1 st neuron – spinal ganglion 2 nd neuron - nerve cells in the nuclei gracilis and cuneatus 3 rd neuron - thalamic posterolateral ventral nucleus proprioceptors
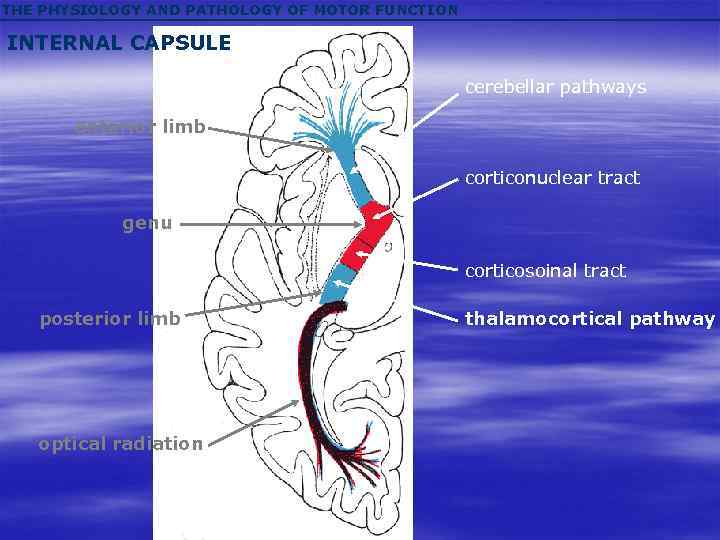 THE PHYSIOLOGY AND PATHOLOGY OF MOTOR FUNCTION INTERNAL CAPSULE cerebellar pathways anterior limb corticonuclear tract genu corticosoinal tract posterior limb optical radiation thalamocortical pathway
THE PHYSIOLOGY AND PATHOLOGY OF MOTOR FUNCTION INTERNAL CAPSULE cerebellar pathways anterior limb corticonuclear tract genu corticosoinal tract posterior limb optical radiation thalamocortical pathway
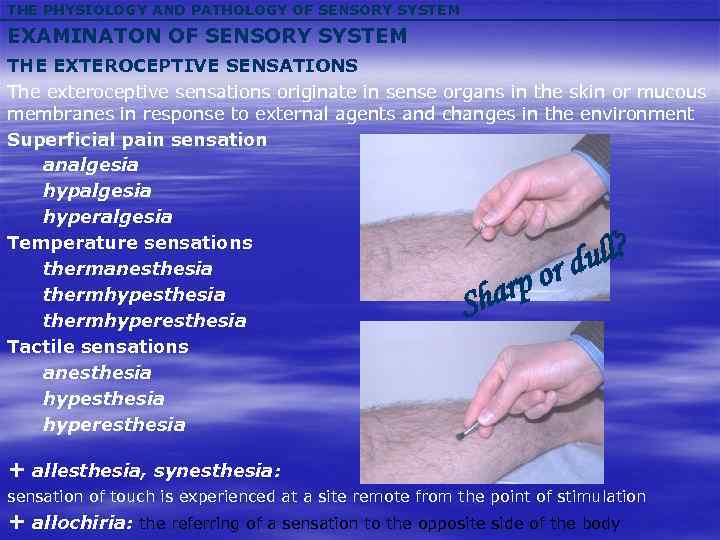 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM THE EXTEROCEPTIVE SENSATIONS The exteroceptive sensations originate in sense organs in the skin or mucous membranes in response to external agents and changes in the environment Superficial pain sensation analgesia hyperalgesia Temperature sensations thermanesthesia thermhyperesthesia Tactile sensations anesthesia hyperesthesia arp Sh ull? or d + allesthesia, synesthesia: sensation of touch is experienced at a site remote from the point of stimulation + allochiria: the referring of a sensation to the opposite side of the body
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM THE EXTEROCEPTIVE SENSATIONS The exteroceptive sensations originate in sense organs in the skin or mucous membranes in response to external agents and changes in the environment Superficial pain sensation analgesia hyperalgesia Temperature sensations thermanesthesia thermhyperesthesia Tactile sensations anesthesia hyperesthesia arp Sh ull? or d + allesthesia, synesthesia: sensation of touch is experienced at a site remote from the point of stimulation + allochiria: the referring of a sensation to the opposite side of the body
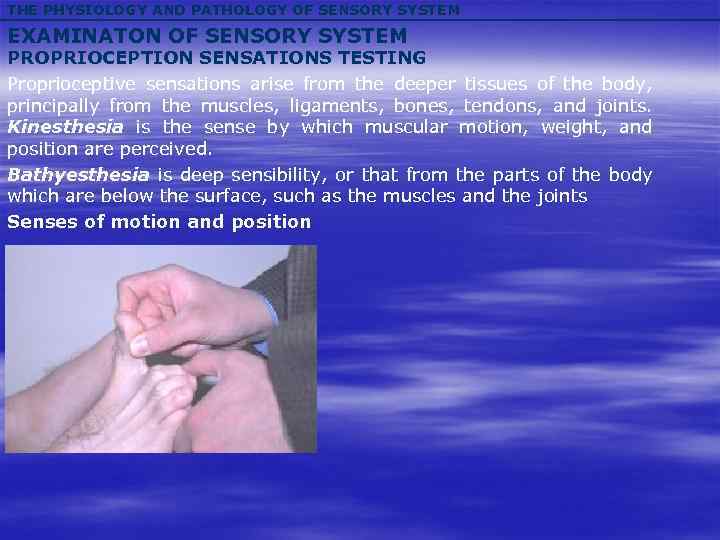 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM PROPRIOCEPTION SENSATIONS TESTING Proprioceptive sensations arise from the deeper tissues of the body, principally from the muscles, ligaments, bones, tendons, and joints. Kinesthesia is the sense by which muscular motion, weight, and position are perceived. Bathyesthesia is deep sensibility, or that from the parts of the body which are below the surface, such as the muscles and the joints Senses of motion and position
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM PROPRIOCEPTION SENSATIONS TESTING Proprioceptive sensations arise from the deeper tissues of the body, principally from the muscles, ligaments, bones, tendons, and joints. Kinesthesia is the sense by which muscular motion, weight, and position are perceived. Bathyesthesia is deep sensibility, or that from the parts of the body which are below the surface, such as the muscles and the joints Senses of motion and position
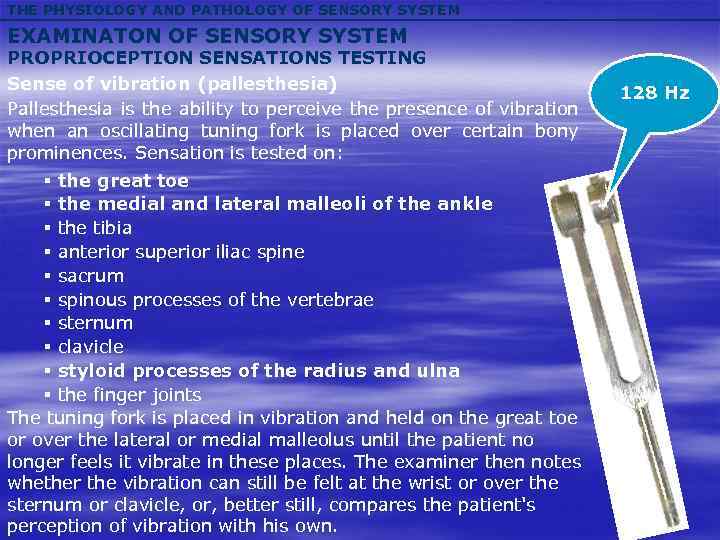 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM PROPRIOCEPTION SENSATIONS TESTING Sense of vibration (pallesthesia) Pallesthesia is the ability to perceive the presence of vibration when an oscillating tuning fork is placed over certain bony prominences. Sensation is tested on: § the great toe § the medial and lateral malleoli of the ankle § the tibia § anterior superior iliac spine § sacrum § spinous processes of the vertebrae § sternum § clavicle § styloid processes of the radius and ulna § the finger joints The tuning fork is placed in vibration and held on the great toe or over the lateral or medial malleolus until the patient no longer feels it vibrate in these places. The examiner then notes whether the vibration can still be felt at the wrist or over the sternum or clavicle, or, better still, compares the patient's perception of vibration with his own. 128 Hz
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM PROPRIOCEPTION SENSATIONS TESTING Sense of vibration (pallesthesia) Pallesthesia is the ability to perceive the presence of vibration when an oscillating tuning fork is placed over certain bony prominences. Sensation is tested on: § the great toe § the medial and lateral malleoli of the ankle § the tibia § anterior superior iliac spine § sacrum § spinous processes of the vertebrae § sternum § clavicle § styloid processes of the radius and ulna § the finger joints The tuning fork is placed in vibration and held on the great toe or over the lateral or medial malleolus until the patient no longer feels it vibrate in these places. The examiner then notes whether the vibration can still be felt at the wrist or over the sternum or clavicle, or, better still, compares the patient's perception of vibration with his own. 128 Hz
 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM PROPRIOCEPTION SENSATIONS TESTING Pressure sense is tested by firm touch upon the skin with a finger or a blunt object, and by pressure on the subcutaneous structures, such as the muscle masses, the tendons, and the nerves themselves, either by the use of a blunt object or by squeezing between the fingers, and one tests both the appreciation and the localization of pressure.
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM PROPRIOCEPTION SENSATIONS TESTING Pressure sense is tested by firm touch upon the skin with a finger or a blunt object, and by pressure on the subcutaneous structures, such as the muscle masses, the tendons, and the nerves themselves, either by the use of a blunt object or by squeezing between the fingers, and one tests both the appreciation and the localization of pressure.
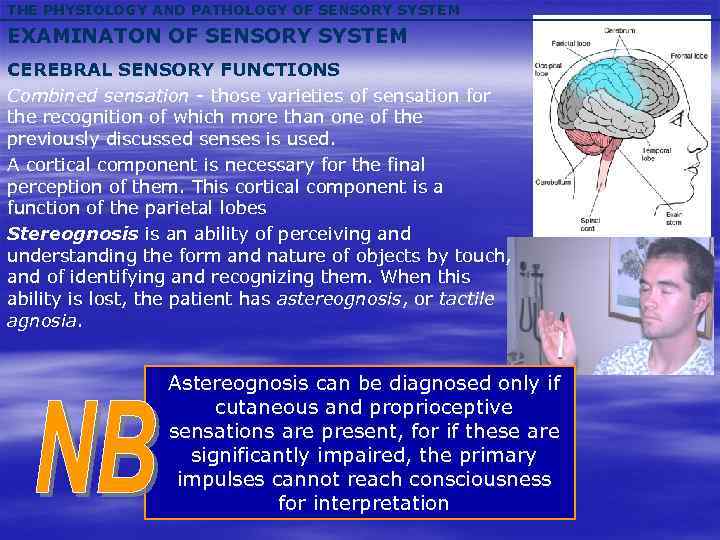 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM CEREBRAL SENSORY FUNCTIONS Combined sensation - those varieties of sensation for the recognition of which more than one of the previously discussed senses is used. A cortical component is necessary for the final perception of them. This cortical component is a function of the parietal lobes Stereognosis is an ability of perceiving and understanding the form and nature of objects by touch, and of identifying and recognizing them. When this ability is lost, the patient has astereognosis, or tactile agnosia. Astereognosis can be diagnosed only if cutaneous and proprioceptive sensations are present, for if these are significantly impaired, the primary impulses cannot reach consciousness for interpretation
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM CEREBRAL SENSORY FUNCTIONS Combined sensation - those varieties of sensation for the recognition of which more than one of the previously discussed senses is used. A cortical component is necessary for the final perception of them. This cortical component is a function of the parietal lobes Stereognosis is an ability of perceiving and understanding the form and nature of objects by touch, and of identifying and recognizing them. When this ability is lost, the patient has astereognosis, or tactile agnosia. Astereognosis can be diagnosed only if cutaneous and proprioceptive sensations are present, for if these are significantly impaired, the primary impulses cannot reach consciousness for interpretation
 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM CEREBRAL SENSORY FUNCTIONS Topesthesia, or topognosia, is the ability to localize a tactile sensation. Its loss is known as topoanesthesia, or topagnosia. Localization is impossible if there is cutaneous anesthesia, but the loss of the sense of localization with an intact exteroceptive sensibility usually signifies the presence of a lesion affecting the parietal lobe. Graphesthesia is a term used to designate the ability to recognize letters or numbers written on the skin, written on the forearm and legs with a pencil or a dull зут. Loss of this sensation is known as graphanesthesia. Loss of graphesthesia in the presence of intact peripheral sensation implies the presence of a cortical lesion. This is particularly true when the loss is unilateral. Two-point, or spatial, discrimination is the ability to differentiate cutaneous stimulation by one blunt point from stimulation by two points. The distance varies considerably in different parts of the body: greater distances are necessary for differentiation on the forearm, upper arm, torso, thigh, and leg.
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM CEREBRAL SENSORY FUNCTIONS Topesthesia, or topognosia, is the ability to localize a tactile sensation. Its loss is known as topoanesthesia, or topagnosia. Localization is impossible if there is cutaneous anesthesia, but the loss of the sense of localization with an intact exteroceptive sensibility usually signifies the presence of a lesion affecting the parietal lobe. Graphesthesia is a term used to designate the ability to recognize letters or numbers written on the skin, written on the forearm and legs with a pencil or a dull зут. Loss of this sensation is known as graphanesthesia. Loss of graphesthesia in the presence of intact peripheral sensation implies the presence of a cortical lesion. This is particularly true when the loss is unilateral. Two-point, or spatial, discrimination is the ability to differentiate cutaneous stimulation by one blunt point from stimulation by two points. The distance varies considerably in different parts of the body: greater distances are necessary for differentiation on the forearm, upper arm, torso, thigh, and leg.
 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM CEREBRAL SENSORY FUNCTIONS Autotopagnosia, or somatotopagnosia, is the loss of power to identify or orient the body or the relation of its individual parts – a defect in the body scheme. The patient may have complete loss of personal identification of one limb or of one half of the body. He may drop his hand from the table onto his lap and believe that some other object has fallen, or he may feel an arm next to his body and not be aware that it is his own. Lack of awareness of one half of the body is referred to as agnosia of the body half. Anosognosia is defined as the ignorance of the existence of disease and has been used specifically to imply the imperception of hemiplegia, or a feeling of depersonalization toward or loss of perception of paralyzed parts of the body, either due to anesthesia of the paralyzed parts or to amnesia for them. The patient may believe that he is able to use his paretic extremities in a normal manner. Anosognosia is most often found in lesions of the right parietal lobe.
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM EXAMINATON OF SENSORY SYSTEM CEREBRAL SENSORY FUNCTIONS Autotopagnosia, or somatotopagnosia, is the loss of power to identify or orient the body or the relation of its individual parts – a defect in the body scheme. The patient may have complete loss of personal identification of one limb or of one half of the body. He may drop his hand from the table onto his lap and believe that some other object has fallen, or he may feel an arm next to his body and not be aware that it is his own. Lack of awareness of one half of the body is referred to as agnosia of the body half. Anosognosia is defined as the ignorance of the existence of disease and has been used specifically to imply the imperception of hemiplegia, or a feeling of depersonalization toward or loss of perception of paralyzed parts of the body, either due to anesthesia of the paralyzed parts or to amnesia for them. The patient may believe that he is able to use his paretic extremities in a normal manner. Anosognosia is most often found in lesions of the right parietal lobe.
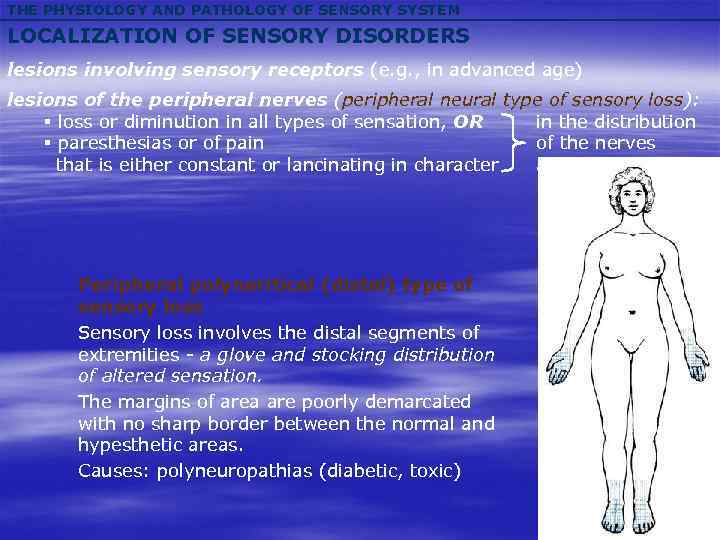 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS lesions involving sensory receptors (e. g. , in advanced age) lesions of the peripheral nerves (peripheral neural type of sensory loss): § loss or diminution in all types of sensation, OR in the distribution § paresthesias or of pain of the nerves that is either constant or lancinating in character affected Peripheral polyneritical (distal) type of sensory loss Sensory loss involves the distal segments of extremities - a glove and stocking distribution of altered sensation. The margins of area are poorly demarcated with no sharp border between the normal and hypesthetic areas. Causes: polyneuropathias (diabetic, toxic)
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS lesions involving sensory receptors (e. g. , in advanced age) lesions of the peripheral nerves (peripheral neural type of sensory loss): § loss or diminution in all types of sensation, OR in the distribution § paresthesias or of pain of the nerves that is either constant or lancinating in character affected Peripheral polyneritical (distal) type of sensory loss Sensory loss involves the distal segments of extremities - a glove and stocking distribution of altered sensation. The margins of area are poorly demarcated with no sharp border between the normal and hypesthetic areas. Causes: polyneuropathias (diabetic, toxic)
 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS disease of the dorsal root ganglia: lancinating pain (herpes zoster) ~ trophic changes radicular lesions (peripheral radicular type of sensory loss): § diminution or loss of sensation, OR the distribution is segmental § either pain or paresthesias in type Irritation of the nerve roots causes pain in a radicular, sometimes girdle, distribution (i. e. , encircling the body). site of the lesion Herpes zoster
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS disease of the dorsal root ganglia: lancinating pain (herpes zoster) ~ trophic changes radicular lesions (peripheral radicular type of sensory loss): § diminution or loss of sensation, OR the distribution is segmental § either pain or paresthesias in type Irritation of the nerve roots causes pain in a radicular, sometimes girdle, distribution (i. e. , encircling the body). site of the lesion Herpes zoster
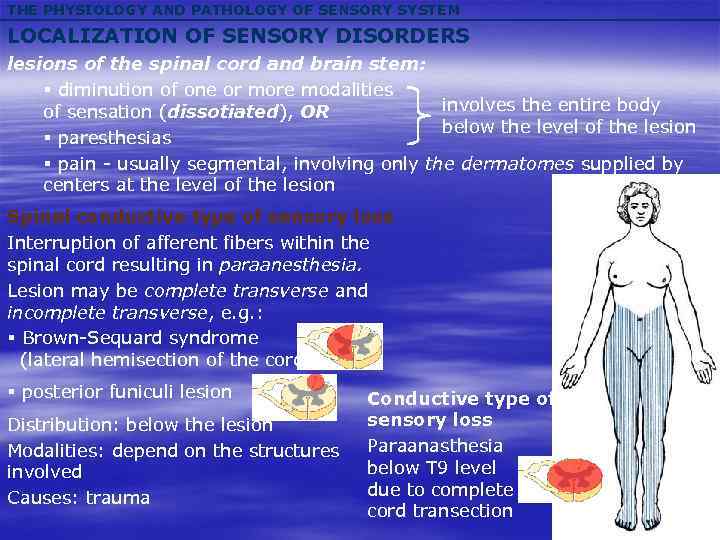 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS lesions of the spinal cord and brain stem: § diminution of one or more modalities involves the entire body of sensation (dissotiated), OR below the level of the lesion § paresthesias § pain - usually segmental, involving only the dermatomes supplied by centers at the level of the lesion Spinal conductive type of sensory loss Interruption of afferent fibers within the spinal cord resulting in paraanesthesia. Lesion may be complete transverse and incomplete transverse, e. g. : § Brown-Sequard syndrome (lateral hemisection of the cord) § posterior funiculi lesion Distribution: below the lesion Modalities: depend on the structures involved Causes: trauma Conductive type of sensory loss Paraanasthesia below T 9 level due to complete cord transection
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS lesions of the spinal cord and brain stem: § diminution of one or more modalities involves the entire body of sensation (dissotiated), OR below the level of the lesion § paresthesias § pain - usually segmental, involving only the dermatomes supplied by centers at the level of the lesion Spinal conductive type of sensory loss Interruption of afferent fibers within the spinal cord resulting in paraanesthesia. Lesion may be complete transverse and incomplete transverse, e. g. : § Brown-Sequard syndrome (lateral hemisection of the cord) § posterior funiculi lesion Distribution: below the lesion Modalities: depend on the structures involved Causes: trauma Conductive type of sensory loss Paraanasthesia below T 9 level due to complete cord transection
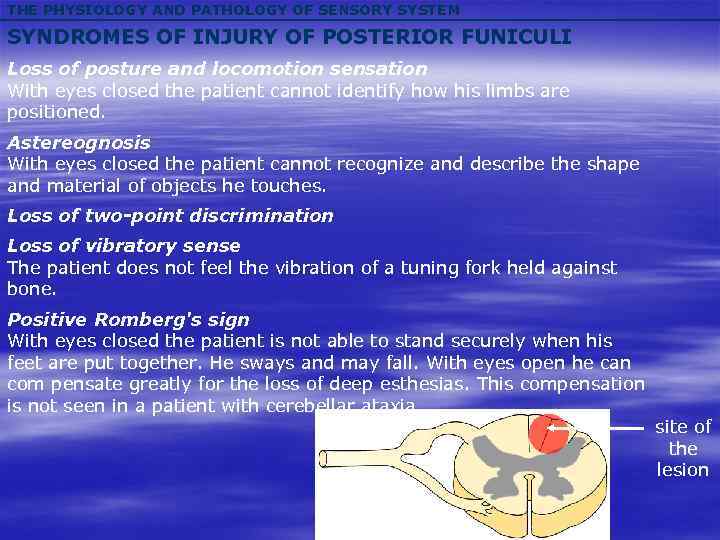 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM SYNDROMES OF INJURY OF POSTERIOR FUNICULI Loss of posture and locomotion sensation With eyes closed the patient cannot identify how his limbs are positioned. Astereognosis With eyes closed the patient cannot recognize and describe the shape and material of objects he touches. Loss of two-point discrimination Loss of vibratory sense The patient does not feel the vibration of a tuning fork held against bone. Positive Romberg's sign With eyes closed the patient is not able to stand securely when his feet are put together. He sways and may fall. With eyes open he can com pensate greatly for the loss of deep esthesias. This compensation is not seen in a patient with cerebellar ataxia. site of the lesion
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM SYNDROMES OF INJURY OF POSTERIOR FUNICULI Loss of posture and locomotion sensation With eyes closed the patient cannot identify how his limbs are positioned. Astereognosis With eyes closed the patient cannot recognize and describe the shape and material of objects he touches. Loss of two-point discrimination Loss of vibratory sense The patient does not feel the vibration of a tuning fork held against bone. Positive Romberg's sign With eyes closed the patient is not able to stand securely when his feet are put together. He sways and may fall. With eyes open he can com pensate greatly for the loss of deep esthesias. This compensation is not seen in a patient with cerebellar ataxia. site of the lesion
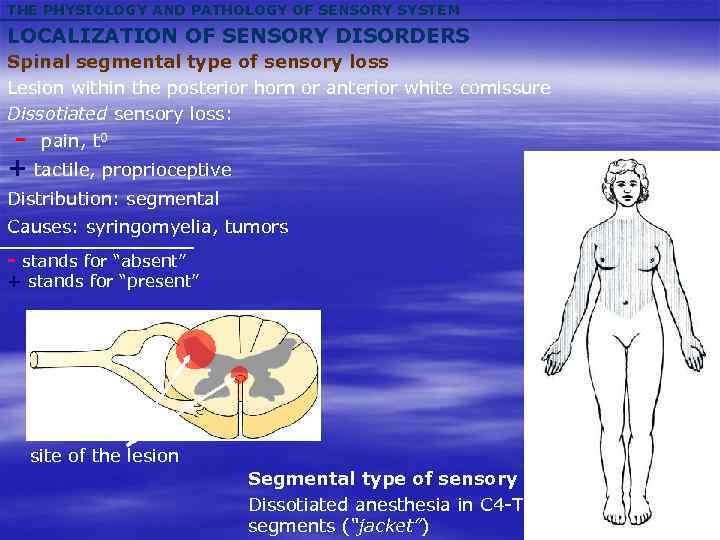 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS Spinal segmental type of sensory loss Lesion within the posterior horn or anterior white comissure Dissotiated sensory loss: - pain, t 0 + tactile, proprioceptive Distribution: segmental Causes: syringomyelia, tumors - stands for “absent” + stands for “present” site of the lesion Segmental type of sensory loss Dissotiated anesthesia in C 4 -T 10 segments (“jacket”)
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS Spinal segmental type of sensory loss Lesion within the posterior horn or anterior white comissure Dissotiated sensory loss: - pain, t 0 + tactile, proprioceptive Distribution: segmental Causes: syringomyelia, tumors - stands for “absent” + stands for “present” site of the lesion Segmental type of sensory loss Dissotiated anesthesia in C 4 -T 10 segments (“jacket”)
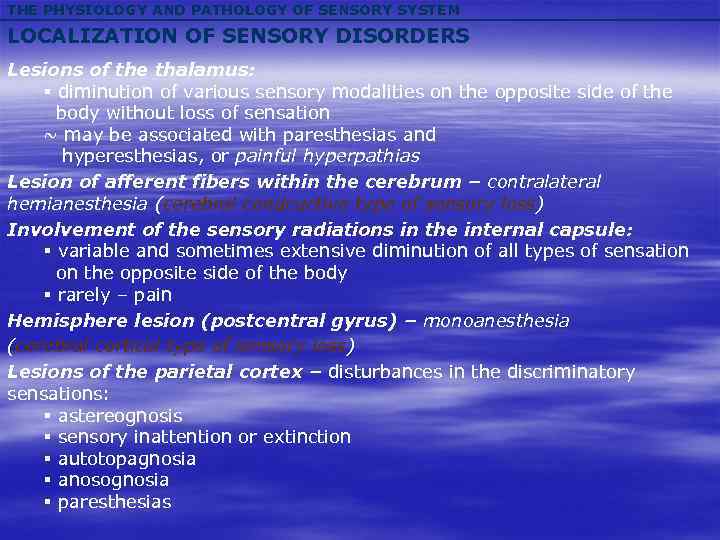 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS Lesions of the thalamus: § diminution of various sensory modalities on the opposite side of the body without loss of sensation ~ may be associated with paresthesias and hyperesthesias, or painful hyperpathias Lesion of afferent fibers within the cerebrum – contralateral hemianesthesia (cerebral condcuctive type of sensory loss) Involvement of the sensory radiations in the internal capsule: § variable and sometimes extensive diminution of all types of sensation on the opposite side of the body § rarely – pain Hemisphere lesion (postcentral gyrus) – monoanesthesia (cerebral cortical type of sensory loss) Lesions of the parietal cortex – disturbances in the discriminatory sensations: § astereognosis § sensory inattention or extinction § autotopagnosia § anosognosia § paresthesias
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS Lesions of the thalamus: § diminution of various sensory modalities on the opposite side of the body without loss of sensation ~ may be associated with paresthesias and hyperesthesias, or painful hyperpathias Lesion of afferent fibers within the cerebrum – contralateral hemianesthesia (cerebral condcuctive type of sensory loss) Involvement of the sensory radiations in the internal capsule: § variable and sometimes extensive diminution of all types of sensation on the opposite side of the body § rarely – pain Hemisphere lesion (postcentral gyrus) – monoanesthesia (cerebral cortical type of sensory loss) Lesions of the parietal cortex – disturbances in the discriminatory sensations: § astereognosis § sensory inattention or extinction § autotopagnosia § anosognosia § paresthesias
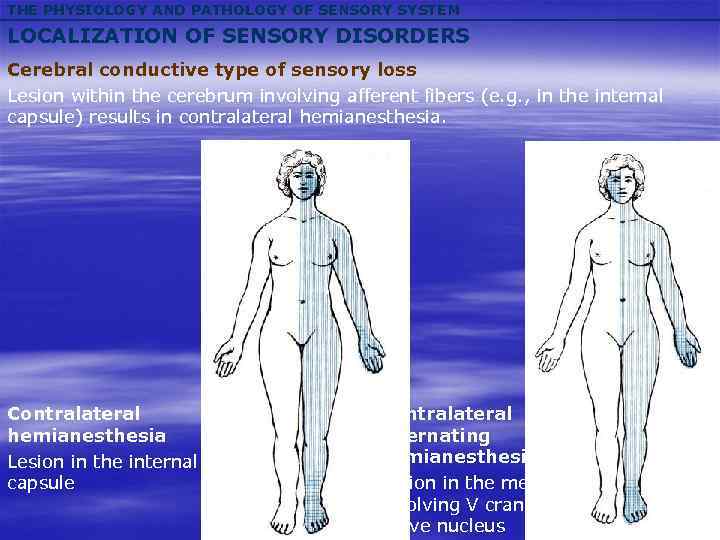 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS Cerebral conductive type of sensory loss Lesion within the cerebrum involving afferent fibers (e. g. , in the internal capsule) results in contralateral hemianesthesia. Contralateral hemianesthesia Lesion in the internal capsule Contralateral alternating hemianesthesia Lesion in the medulla involving V cranial nerve nucleus
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM LOCALIZATION OF SENSORY DISORDERS Cerebral conductive type of sensory loss Lesion within the cerebrum involving afferent fibers (e. g. , in the internal capsule) results in contralateral hemianesthesia. Contralateral hemianesthesia Lesion in the internal capsule Contralateral alternating hemianesthesia Lesion in the medulla involving V cranial nerve nucleus
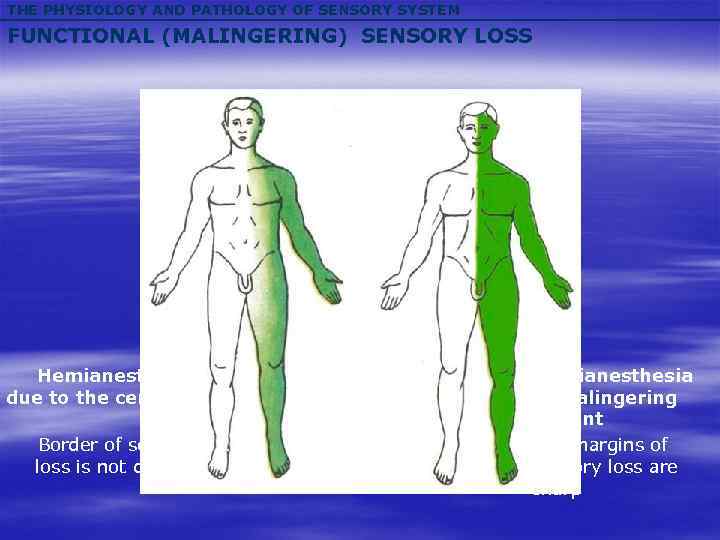 THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM FUNCTIONAL (MALINGERING) SENSORY LOSS Hemianesthesia due to the cerebral lesion Border of sensory loss is not distinct Hemianesthesia in malingering patient The margins of sensory loss are sharp
THE PHYSIOLOGY AND PATHOLOGY OF SENSORY SYSTEM FUNCTIONAL (MALINGERING) SENSORY LOSS Hemianesthesia due to the cerebral lesion Border of sensory loss is not distinct Hemianesthesia in malingering patient The margins of sensory loss are sharp
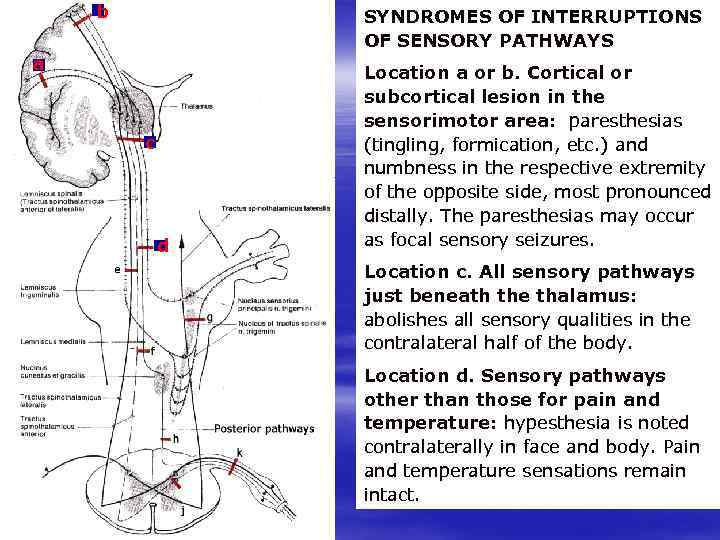 b SYNDROMES OF INTERRUPTIONS OF SENSORY PATHWAYS a Location a or b. Cortical or subcortical lesion in the sensorimotor area: paresthesias (tingling, formication, etc. ) and numbness in the respective extremity of the opposite side, most pronounced distally. The paresthesias may occur as focal sensory seizures. с d Location c. All sensory pathways just beneath the thalamus: abolishes all sensory qualities in the contralateral half of the body. i Location d. Sensory pathways other than those for pain and temperature: hypesthesia is noted contralaterally in face and body. Pain and temperature sensations remain intact.
b SYNDROMES OF INTERRUPTIONS OF SENSORY PATHWAYS a Location a or b. Cortical or subcortical lesion in the sensorimotor area: paresthesias (tingling, formication, etc. ) and numbness in the respective extremity of the opposite side, most pronounced distally. The paresthesias may occur as focal sensory seizures. с d Location c. All sensory pathways just beneath the thalamus: abolishes all sensory qualities in the contralateral half of the body. i Location d. Sensory pathways other than those for pain and temperature: hypesthesia is noted contralaterally in face and body. Pain and temperature sensations remain intact.
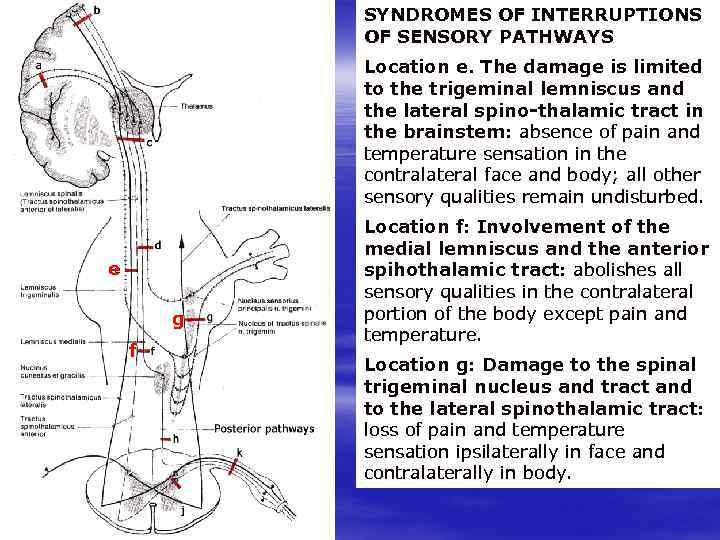 SYNDROMES OF INTERRUPTIONS OF SENSORY PATHWAYS Location e. The damage is limited to the trigeminal lemniscus and the lateral spino-thalamic tract in the brainstem: absence of pain and temperature sensation in the contralateral face and body; all other sensory qualities remain undisturbed. Location f: Involvement of the medial lemniscus and the anterior spihothalamic tract: abolishes all sensory qualities in the contralateral portion of the body except pain and temperature. e g f Location g: Damage to the spinal trigeminal nucleus and tract and to the lateral spinothalamic tract: loss of pain and temperature sensation ipsilaterally in face and contralaterally in body. i
SYNDROMES OF INTERRUPTIONS OF SENSORY PATHWAYS Location e. The damage is limited to the trigeminal lemniscus and the lateral spino-thalamic tract in the brainstem: absence of pain and temperature sensation in the contralateral face and body; all other sensory qualities remain undisturbed. Location f: Involvement of the medial lemniscus and the anterior spihothalamic tract: abolishes all sensory qualities in the contralateral portion of the body except pain and temperature. e g f Location g: Damage to the spinal trigeminal nucleus and tract and to the lateral spinothalamic tract: loss of pain and temperature sensation ipsilaterally in face and contralaterally in body. i
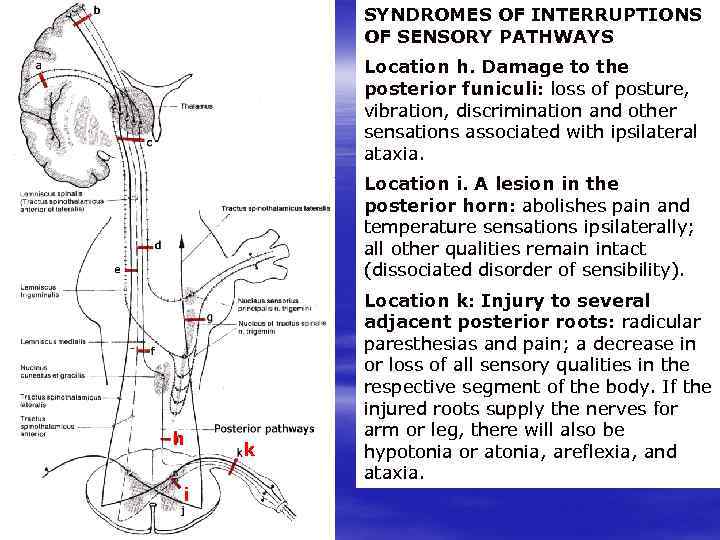 SYNDROMES OF INTERRUPTIONS OF SENSORY PATHWAYS Location h. Damage to the posterior funiculi: loss of posture, vibration, discrimination and other sensations associated with ipsilateral ataxia. Location i. A lesion in the posterior horn: abolishes pain and temperature sensations ipsilaterally; all other qualities remain intact (dissociated disorder of sensibility). h i k Location k: Injury to several adjacent posterior roots: radicular paresthesias and pain; a decrease in or loss of all sensory qualities in the respective segment of the body. If the injured roots supply the nerves for arm or leg, there will also be hypotonia or atonia, areflexia, and ataxia.
SYNDROMES OF INTERRUPTIONS OF SENSORY PATHWAYS Location h. Damage to the posterior funiculi: loss of posture, vibration, discrimination and other sensations associated with ipsilateral ataxia. Location i. A lesion in the posterior horn: abolishes pain and temperature sensations ipsilaterally; all other qualities remain intact (dissociated disorder of sensibility). h i k Location k: Injury to several adjacent posterior roots: radicular paresthesias and pain; a decrease in or loss of all sensory qualities in the respective segment of the body. If the injured roots supply the nerves for arm or leg, there will also be hypotonia or atonia, areflexia, and ataxia.