214aea74101a2c643854b49b67036c92.ppt
- Количество слайдов: 43

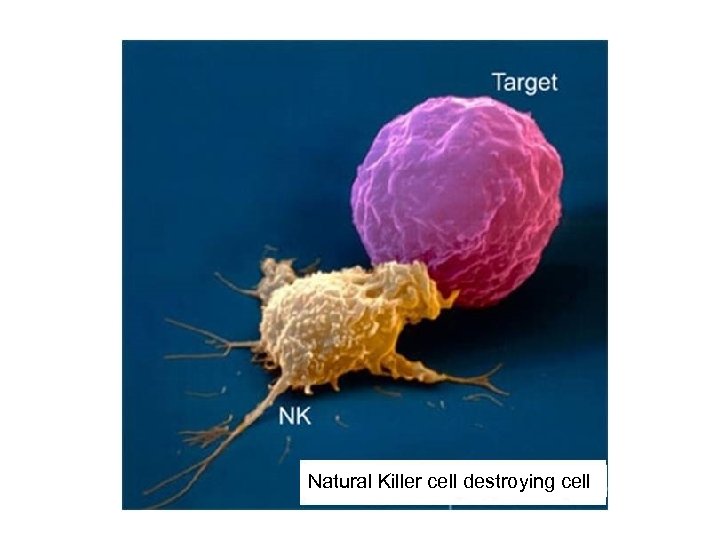 Natural Killer cell destroying cell
Natural Killer cell destroying cell
 Immunity II: Adaptive (specific) Defenses Lecture Outline 1. Introduction: • Properties of specific immunity • What is an antigen? Self vs. non-self antigens 2. B cells or B Lymphocytes: Antibody-mediated response • Types of B cells: Plasma and memory B cells • How B lymphocytes see an antigen? BCRs (immunoglobulins or antibodies) • Role of antibodies in immunity • Activation of B cells : effector (plasma) cells and memory cells 3. T cells or T lymphocytes: Cell-mediated response • Types of T cells: Helper, Cytotoxic, Memory, and Suppressor T cells • How T lymphocytes see an antigen? TCRs (T cell receptors) and MHCs • Activation and Clonal Selection of T cells - Activation of cytotoxic T cells = CD 8+ 1. - Activation of helper T cells = CD 4+ • Effector response - Apoptosis (cytotoxic T cell) - Release of IL-2 and selective cloning (helper T cell) § Vaccinations and Immune System Disorders (AIDS, autoimmunity, allergies)
Immunity II: Adaptive (specific) Defenses Lecture Outline 1. Introduction: • Properties of specific immunity • What is an antigen? Self vs. non-self antigens 2. B cells or B Lymphocytes: Antibody-mediated response • Types of B cells: Plasma and memory B cells • How B lymphocytes see an antigen? BCRs (immunoglobulins or antibodies) • Role of antibodies in immunity • Activation of B cells : effector (plasma) cells and memory cells 3. T cells or T lymphocytes: Cell-mediated response • Types of T cells: Helper, Cytotoxic, Memory, and Suppressor T cells • How T lymphocytes see an antigen? TCRs (T cell receptors) and MHCs • Activation and Clonal Selection of T cells - Activation of cytotoxic T cells = CD 8+ 1. - Activation of helper T cells = CD 4+ • Effector response - Apoptosis (cytotoxic T cell) - Release of IL-2 and selective cloning (helper T cell) § Vaccinations and Immune System Disorders (AIDS, autoimmunity, allergies)
 Immunity: Innate versus Adaptive § Innate – nonselective anything from physical barriers to phagocytosis § Adaptive – this is selective. It is preemptive ie antibodies and receptors are premade and just sit around and wait for the right antigen to enter the system.
Immunity: Innate versus Adaptive § Innate – nonselective anything from physical barriers to phagocytosis § Adaptive – this is selective. It is preemptive ie antibodies and receptors are premade and just sit around and wait for the right antigen to enter the system.
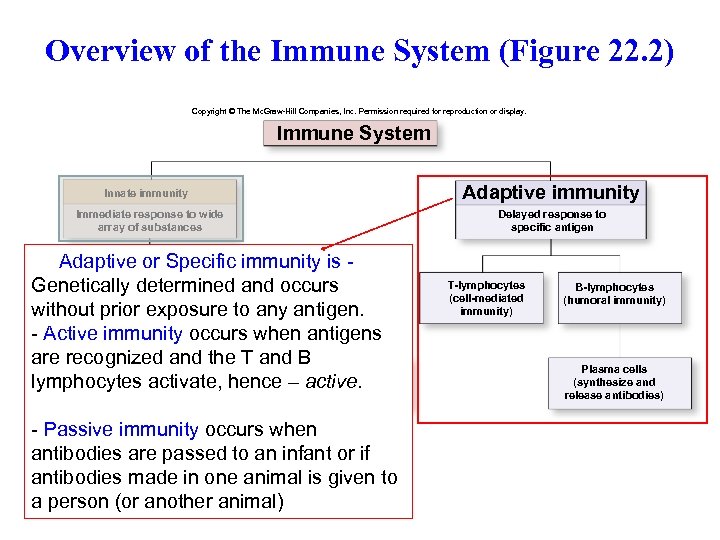 Overview of the Immune System (Figure 22. 2) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Immune System Adaptive immunity Innate immunity Immediate response to wide array of substances Delayed response to specific antigen Adaptive or Specific immunity is Skin and mucosal Nonspecific Genetically determined and occurs Membranes & barriers internal defenses (prevent prior without entry) exposure to any antigen. - Active immunity occurs when antigens are recognized and the T and B Chemicals Cells Physiologic responses (e. g. , interferon, (e. g. , macrophages, lymphocytes activate, hence –(e. g. , inflammation, active. NK cells) complement) fever) - Passive immunity occurs when antibodies are passed to an infant or if antibodies made in one animal is given to a person (or another animal) T-lymphocytes (cell-mediated immunity) B-lymphocytes (humoral immunity) Plasma cells (synthesize and release antibodies)
Overview of the Immune System (Figure 22. 2) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Immune System Adaptive immunity Innate immunity Immediate response to wide array of substances Delayed response to specific antigen Adaptive or Specific immunity is Skin and mucosal Nonspecific Genetically determined and occurs Membranes & barriers internal defenses (prevent prior without entry) exposure to any antigen. - Active immunity occurs when antigens are recognized and the T and B Chemicals Cells Physiologic responses (e. g. , interferon, (e. g. , macrophages, lymphocytes activate, hence –(e. g. , inflammation, active. NK cells) complement) fever) - Passive immunity occurs when antibodies are passed to an infant or if antibodies made in one animal is given to a person (or another animal) T-lymphocytes (cell-mediated immunity) B-lymphocytes (humoral immunity) Plasma cells (synthesize and release antibodies)
 Specific or Adaptive Immunity Specific defense mechanisms (immunity) – use specific receptors to recognize specific antigens Adaptive defense mechanisms adapt to what ever antigens are presented. There are kabillions of T cell and B cell receptors – poised on naïve lymphocytes, ie. cells borne with receptors that are untested (never been used) – just waiting for their specific antigen § B Cells § Provide antibody-mediated immunity (humoral immunity) § Defend against antigens and pathogens in body fluids (‘humors’) § T Cells § Provide cell-mediated immunity (cells must interact) § Defend against abnormal cells and pathogens that enter a cell and present the ‘foreign parts’ = antigens on the cell surface
Specific or Adaptive Immunity Specific defense mechanisms (immunity) – use specific receptors to recognize specific antigens Adaptive defense mechanisms adapt to what ever antigens are presented. There are kabillions of T cell and B cell receptors – poised on naïve lymphocytes, ie. cells borne with receptors that are untested (never been used) – just waiting for their specific antigen § B Cells § Provide antibody-mediated immunity (humoral immunity) § Defend against antigens and pathogens in body fluids (‘humors’) § T Cells § Provide cell-mediated immunity (cells must interact) § Defend against abnormal cells and pathogens that enter a cell and present the ‘foreign parts’ = antigens on the cell surface
 Four properties of Specific Immunity § Specificity § Each T or B cell responds only to a specific antigen and since there are so many different lymphocytes this ‘army’ can respond to 1011 possible antigens (only 106 total genes) § Versatility § The body produces several types of lymphocytes, but kabillions of different receptors: § each recognizes a different type of antigen and a bacterium has many antigens so a bacterium is attacked by many different lymphocytes. § Memory § Activated lymphocytes make memory cells = exact copies or clones: § these clones are distributed throughout the body – waiting …. and if the same antigen reenters the system these clones are ready to react --- fast! § Tolerance § Immune system ignores “normal” (self) antigens, BUT if the selection process in the bone marrow and thymus fails, self antigens are recognized = autoimmunity. Alternatively some bacteria have antigens that mimic self antigens (Strep. pyrogens and scarlet fever) http: //en. wikipedia. org/wiki/Rheumatic_fever
Four properties of Specific Immunity § Specificity § Each T or B cell responds only to a specific antigen and since there are so many different lymphocytes this ‘army’ can respond to 1011 possible antigens (only 106 total genes) § Versatility § The body produces several types of lymphocytes, but kabillions of different receptors: § each recognizes a different type of antigen and a bacterium has many antigens so a bacterium is attacked by many different lymphocytes. § Memory § Activated lymphocytes make memory cells = exact copies or clones: § these clones are distributed throughout the body – waiting …. and if the same antigen reenters the system these clones are ready to react --- fast! § Tolerance § Immune system ignores “normal” (self) antigens, BUT if the selection process in the bone marrow and thymus fails, self antigens are recognized = autoimmunity. Alternatively some bacteria have antigens that mimic self antigens (Strep. pyrogens and scarlet fever) http: //en. wikipedia. org/wiki/Rheumatic_fever
 What is an antigen? § Antigen http: //en. wikipedia. org/wiki/Antigen § Any substance that is recognized by a B-cell receptor or T-cell receptor and elicits a response (4 -7 amino acids, virus proteins, etc) § Antigens are considered: § self antigens if they are normally formed in the same/HOST animal or § non-self antigens if they do not normally belong to the HOST animal (foreign sources, cancers, etc) § Concept: immune cells recognize different antigens and sites recognized can be very, very specific § Recognition of different amino acid sequences on a protein § Recognition of aa, sugars, configurations within a molecule
What is an antigen? § Antigen http: //en. wikipedia. org/wiki/Antigen § Any substance that is recognized by a B-cell receptor or T-cell receptor and elicits a response (4 -7 amino acids, virus proteins, etc) § Antigens are considered: § self antigens if they are normally formed in the same/HOST animal or § non-self antigens if they do not normally belong to the HOST animal (foreign sources, cancers, etc) § Concept: immune cells recognize different antigens and sites recognized can be very, very specific § Recognition of different amino acid sequences on a protein § Recognition of aa, sugars, configurations within a molecule
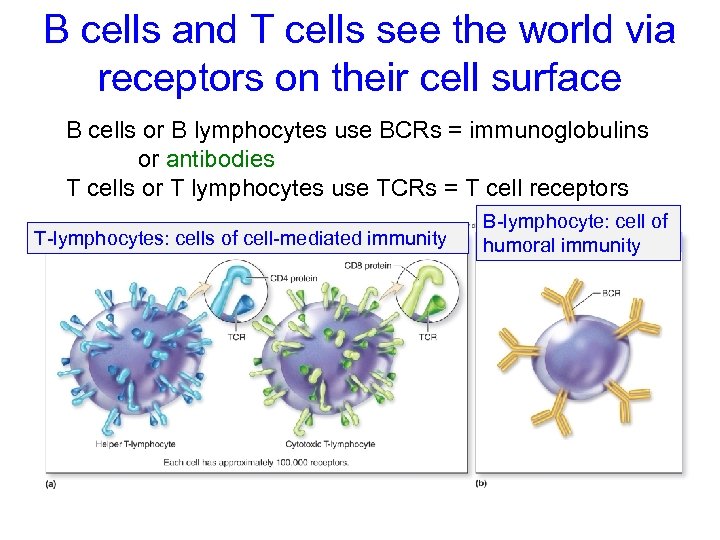 B cells and T cells see the world via receptors on their cell surface B cells or B lymphocytes use BCRs = immunoglobulins or antibodies T cells or T lymphocytes use TCRs = T cell receptors T-lymphocytes: cells of cell-mediated immunity B-lymphocyte: cell of humoral immunity
B cells and T cells see the world via receptors on their cell surface B cells or B lymphocytes use BCRs = immunoglobulins or antibodies T cells or T lymphocytes use TCRs = T cell receptors T-lymphocytes: cells of cell-mediated immunity B-lymphocyte: cell of humoral immunity
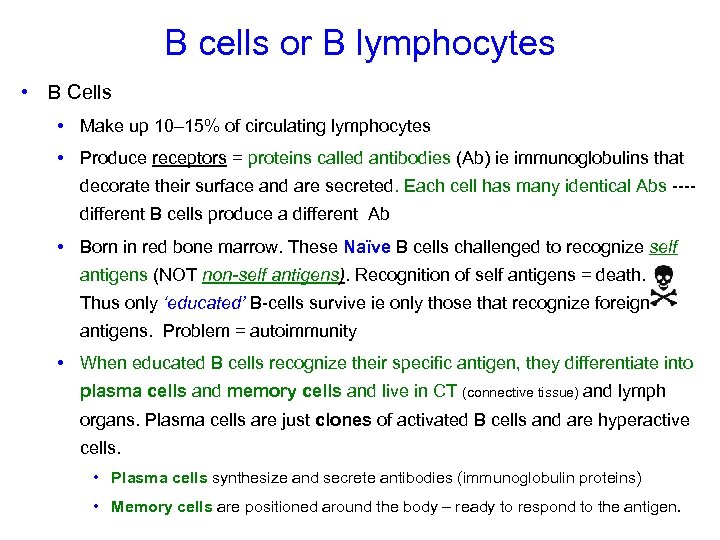 B cells or B lymphocytes • B Cells • Make up 10– 15% of circulating lymphocytes • Produce receptors = proteins called antibodies (Ab) ie immunoglobulins that decorate their surface and are secreted. Each cell has many identical Abs ---different B cells produce a different Ab • Born in red bone marrow. These Naïve B cells challenged to recognize self antigens (NOT non-self antigens). Recognition of self antigens = death. Thus only ‘educated’ B-cells survive ie only those that recognize foreign antigens. Problem = autoimmunity • When educated B cells recognize their specific antigen, they differentiate into plasma cells and memory cells and live in CT (connective tissue) and lymph organs. Plasma cells are just clones of activated B cells and are hyperactive cells. • Plasma cells synthesize and secrete antibodies (immunoglobulin proteins) • Memory cells are positioned around the body – ready to respond to the antigen.
B cells or B lymphocytes • B Cells • Make up 10– 15% of circulating lymphocytes • Produce receptors = proteins called antibodies (Ab) ie immunoglobulins that decorate their surface and are secreted. Each cell has many identical Abs ---different B cells produce a different Ab • Born in red bone marrow. These Naïve B cells challenged to recognize self antigens (NOT non-self antigens). Recognition of self antigens = death. Thus only ‘educated’ B-cells survive ie only those that recognize foreign antigens. Problem = autoimmunity • When educated B cells recognize their specific antigen, they differentiate into plasma cells and memory cells and live in CT (connective tissue) and lymph organs. Plasma cells are just clones of activated B cells and are hyperactive cells. • Plasma cells synthesize and secrete antibodies (immunoglobulin proteins) • Memory cells are positioned around the body – ready to respond to the antigen.
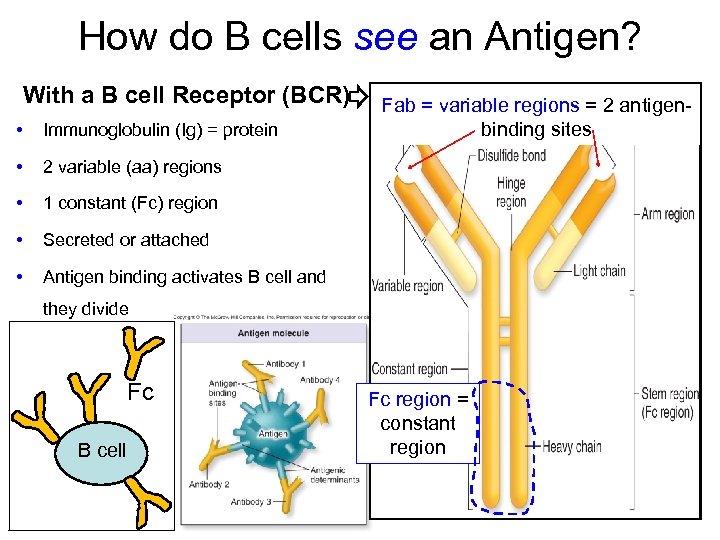 How do B cells see an Antigen? With a B cell Receptor (BCR) • Immunoglobulin (Ig) = protein • 2 variable (aa) regions • 1 constant (Fc) region • Secreted or attached • Fab = variable regions = 2 antigenbinding sites Antigen binding activates B cell and they divide Fc B cell Fc region = constant region
How do B cells see an Antigen? With a B cell Receptor (BCR) • Immunoglobulin (Ig) = protein • 2 variable (aa) regions • 1 constant (Fc) region • Secreted or attached • Fab = variable regions = 2 antigenbinding sites Antigen binding activates B cell and they divide Fc B cell Fc region = constant region
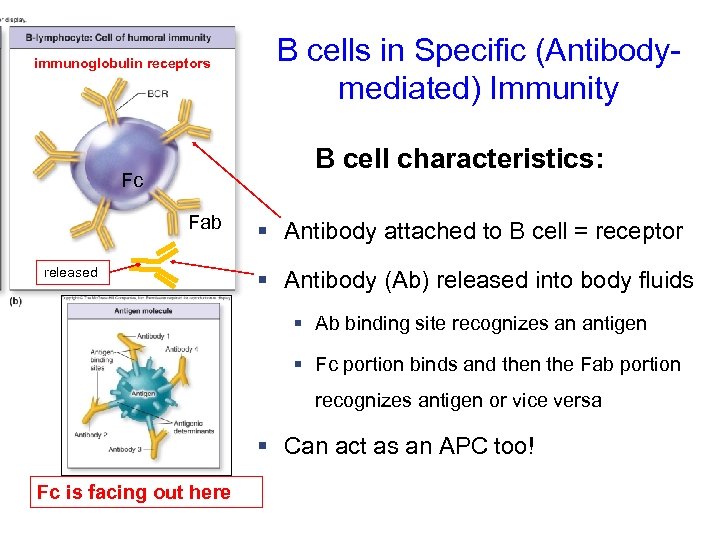 immunoglobulin receptors B cells in Specific (Antibodymediated) Immunity B cell characteristics: Fc Fab released § Antibody attached to B cell = receptor § Antibody (Ab) released into body fluids § Ab binding site recognizes an antigen § Fc portion binds and then the Fab portion recognizes antigen or vice versa § Can act as an APC too! Fc is facing out here
immunoglobulin receptors B cells in Specific (Antibodymediated) Immunity B cell characteristics: Fc Fab released § Antibody attached to B cell = receptor § Antibody (Ab) released into body fluids § Ab binding site recognizes an antigen § Fc portion binds and then the Fab portion recognizes antigen or vice versa § Can act as an APC too! Fc is facing out here
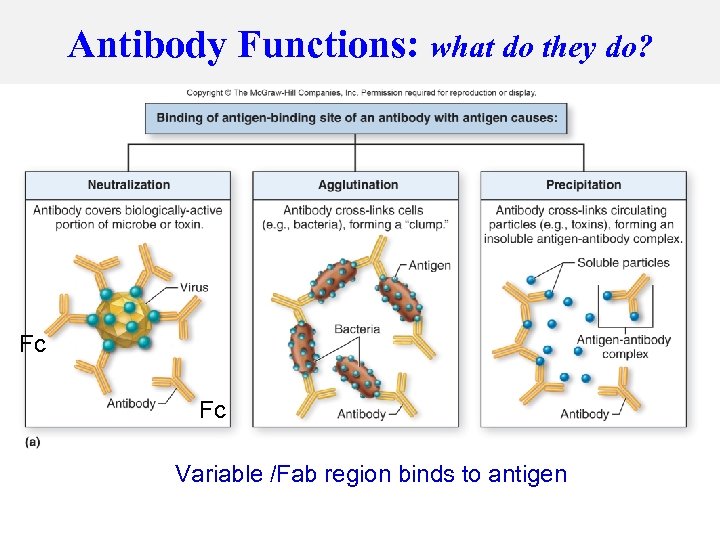 Antibody Functions: what do they do? Fc Fc Variable /Fab region binds to antigen
Antibody Functions: what do they do? Fc Fc Variable /Fab region binds to antigen
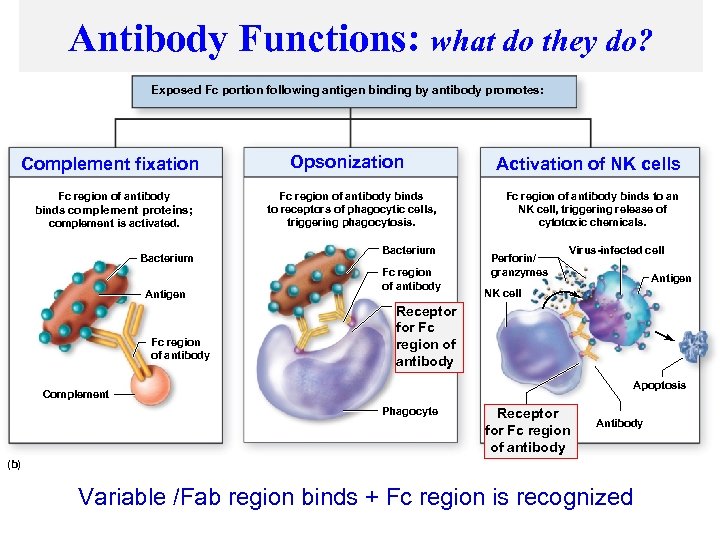 Antibody Functions: what do they do? Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Exposed Fc portion following antigen binding by antibody promotes: Complement fixation Fc region of antibody binds complement proteins; complement is activated. Bacterium Antigen Fc region of antibody Opsonization Fc region of antibody binds to receptors of phagocytic cells, triggering phagocytosis. Bacterium Fc region of antibody Activation of NK cells Fc region of antibody binds to an NK cell, triggering release of cytotoxic chemicals. Perforin/ granzymes Virus-infected cell Antigen NK cell Receptor for Fc region of antibody Apoptosis Complement Phagocyte Receptor for Fc region of antibody Antibody (b) Variable /Fab region binds + Fc region is recognized
Antibody Functions: what do they do? Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Exposed Fc portion following antigen binding by antibody promotes: Complement fixation Fc region of antibody binds complement proteins; complement is activated. Bacterium Antigen Fc region of antibody Opsonization Fc region of antibody binds to receptors of phagocytic cells, triggering phagocytosis. Bacterium Fc region of antibody Activation of NK cells Fc region of antibody binds to an NK cell, triggering release of cytotoxic chemicals. Perforin/ granzymes Virus-infected cell Antigen NK cell Receptor for Fc region of antibody Apoptosis Complement Phagocyte Receptor for Fc region of antibody Antibody (b) Variable /Fab region binds + Fc region is recognized
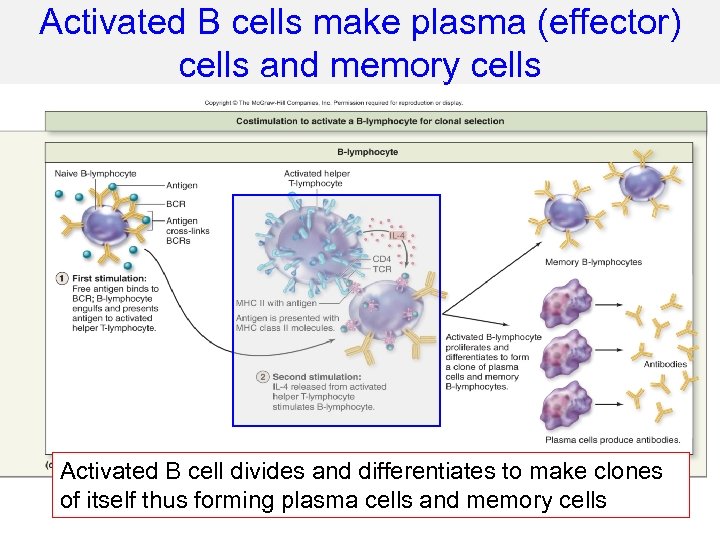 Activated B cells make plasma (effector) cells and memory cells Activated B cell divides and differentiates to make clones of itself thus forming plasma cells and memory cells
Activated B cells make plasma (effector) cells and memory cells Activated B cell divides and differentiates to make clones of itself thus forming plasma cells and memory cells
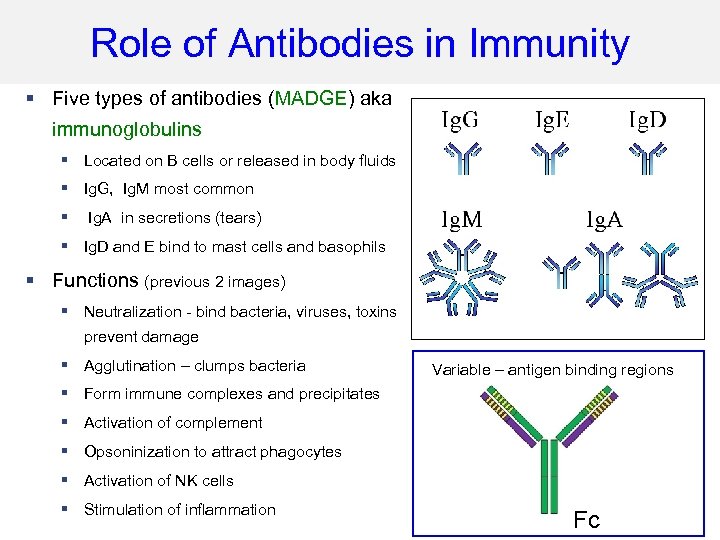 Role of Antibodies in Immunity § Five types of antibodies (MADGE) aka immunoglobulins § Located on B cells or released in body fluids § Ig. G, Ig. M most common § Ig. A in secretions (tears) § Ig. D and E bind to mast cells and basophils § Functions (previous 2 images) § Neutralization - bind bacteria, viruses, toxins to prevent damage § Agglutination – clumps bacteria Variable – antigen binding regions § Form immune complexes and precipitates § Activation of complement § Opsoninization to attract phagocytes § Activation of NK cells § Stimulation of inflammation Fc
Role of Antibodies in Immunity § Five types of antibodies (MADGE) aka immunoglobulins § Located on B cells or released in body fluids § Ig. G, Ig. M most common § Ig. A in secretions (tears) § Ig. D and E bind to mast cells and basophils § Functions (previous 2 images) § Neutralization - bind bacteria, viruses, toxins to prevent damage § Agglutination – clumps bacteria Variable – antigen binding regions § Form immune complexes and precipitates § Activation of complement § Opsoninization to attract phagocytes § Activation of NK cells § Stimulation of inflammation Fc
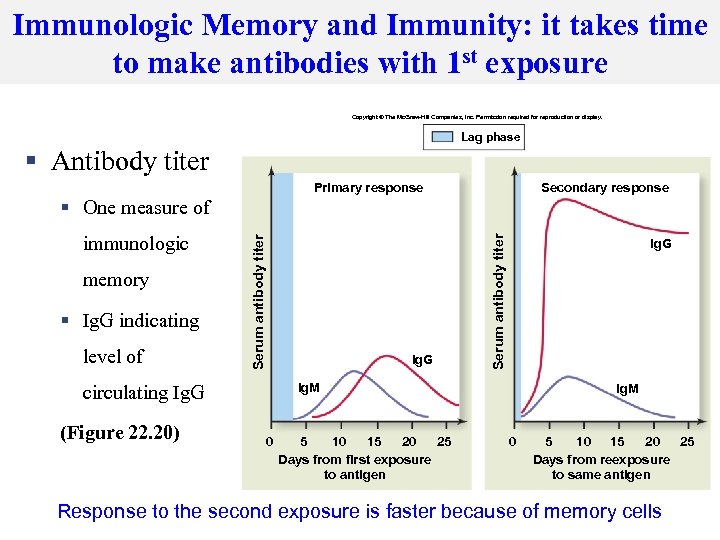 Immunologic Memory and Immunity: it takes time to make antibodies with 1 st exposure Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Lag phase § Antibody titer Primary response Secondary response memory § Ig. G indicating level of Ig. G Ig. M circulating Ig. G (Figure 22. 20) Ig. G Serum antibody titer immunologic Serum antibody titer § One measure of 0 5 10 15 20 25 Days from first exposure to antigen Ig. M 0 5 10 15 20 25 Days from reexposure to same antigen Response to the second exposure is faster because of memory cells
Immunologic Memory and Immunity: it takes time to make antibodies with 1 st exposure Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Lag phase § Antibody titer Primary response Secondary response memory § Ig. G indicating level of Ig. G Ig. M circulating Ig. G (Figure 22. 20) Ig. G Serum antibody titer immunologic Serum antibody titer § One measure of 0 5 10 15 20 25 Days from first exposure to antigen Ig. M 0 5 10 15 20 25 Days from reexposure to same antigen Response to the second exposure is faster because of memory cells
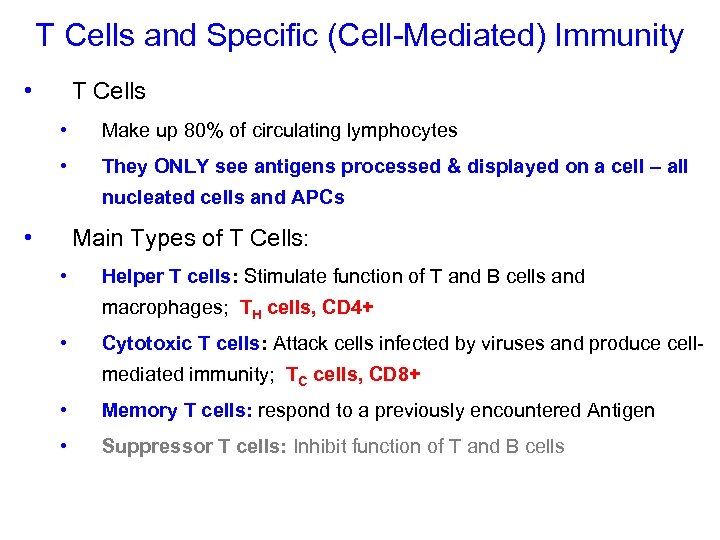 T Cells and Specific (Cell-Mediated) Immunity • T Cells • Make up 80% of circulating lymphocytes • They ONLY see antigens processed & displayed on a cell – all nucleated cells and APCs • Main Types of T Cells: • Helper T cells: Stimulate function of T and B cells and macrophages; TH cells, CD 4+ • Cytotoxic T cells: Attack cells infected by viruses and produce cellmediated immunity; TC cells, CD 8+ • Memory T cells: respond to a previously encountered Antigen • Suppressor T cells: Inhibit function of T and B cells
T Cells and Specific (Cell-Mediated) Immunity • T Cells • Make up 80% of circulating lymphocytes • They ONLY see antigens processed & displayed on a cell – all nucleated cells and APCs • Main Types of T Cells: • Helper T cells: Stimulate function of T and B cells and macrophages; TH cells, CD 4+ • Cytotoxic T cells: Attack cells infected by viruses and produce cellmediated immunity; TC cells, CD 8+ • Memory T cells: respond to a previously encountered Antigen • Suppressor T cells: Inhibit function of T and B cells
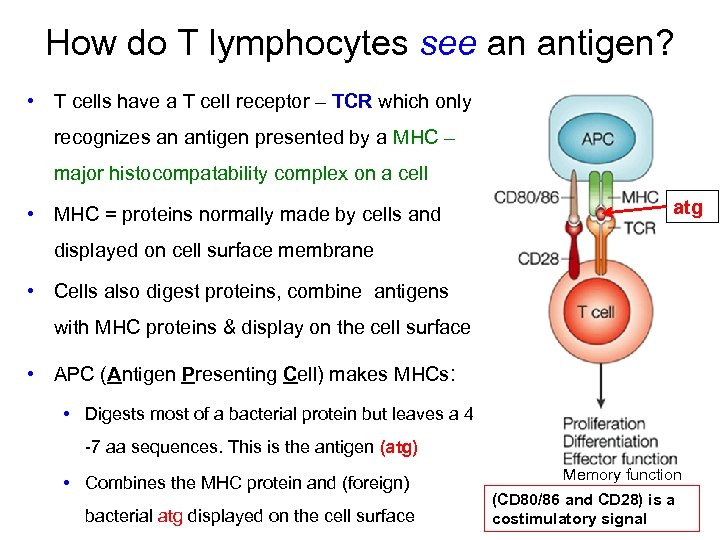 How do T lymphocytes see an antigen? • T cells have a T cell receptor – TCR which only recognizes an antigen presented by a MHC – major histocompatability complex on a cell • MHC = proteins normally made by cells and atg displayed on cell surface membrane • Cells also digest proteins, combine antigens with MHC proteins & display on the cell surface • APC (Antigen Presenting Cell) makes MHCs: • Digests most of a bacterial protein but leaves a 4 -7 aa sequences. This is the antigen (atg) • Combines the MHC protein and (foreign) bacterial atg displayed on the cell surface Memory function (CD 80/86 and CD 28) is a costimulatory signal
How do T lymphocytes see an antigen? • T cells have a T cell receptor – TCR which only recognizes an antigen presented by a MHC – major histocompatability complex on a cell • MHC = proteins normally made by cells and atg displayed on cell surface membrane • Cells also digest proteins, combine antigens with MHC proteins & display on the cell surface • APC (Antigen Presenting Cell) makes MHCs: • Digests most of a bacterial protein but leaves a 4 -7 aa sequences. This is the antigen (atg) • Combines the MHC protein and (foreign) bacterial atg displayed on the cell surface Memory function (CD 80/86 and CD 28) is a costimulatory signal
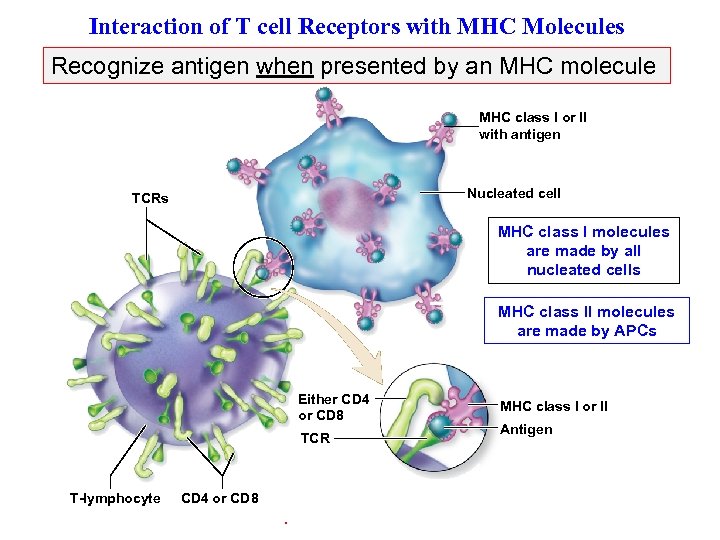 Interaction of T cell Receptors with MHC Molecules of Other Cells (Figure 22. 12) Recognize antigen when presented by an MHC molecule Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. MHC class I or II with antigen Nucleated cell TCRs MHC class I molecules are made by all nucleated cells MHC class II molecules are made by APCs Either CD 4 or CD 8 TCR T-lymphocyte CD 4 or CD 8 . MHC class I or II Antigen
Interaction of T cell Receptors with MHC Molecules of Other Cells (Figure 22. 12) Recognize antigen when presented by an MHC molecule Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. MHC class I or II with antigen Nucleated cell TCRs MHC class I molecules are made by all nucleated cells MHC class II molecules are made by APCs Either CD 4 or CD 8 TCR T-lymphocyte CD 4 or CD 8 . MHC class I or II Antigen
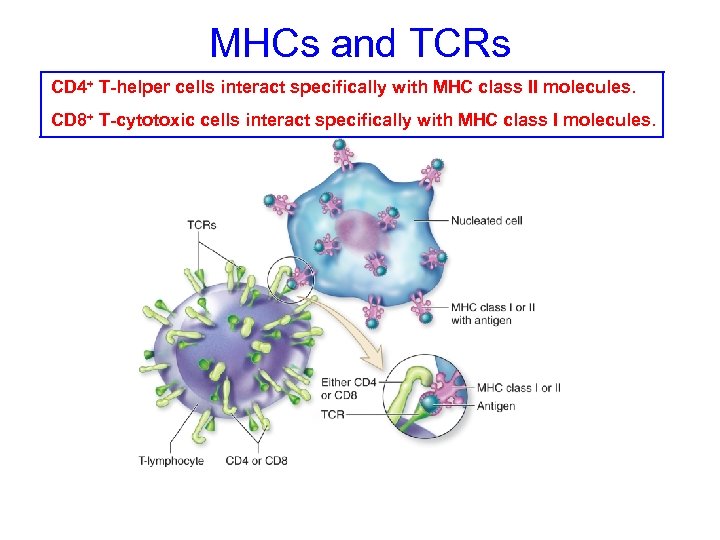 MHCs and TCRs CD 4+ T-helper cells interact specifically with MHC class II molecules. CD 8+ T-cytotoxic cells interact specifically with MHC class I molecules.
MHCs and TCRs CD 4+ T-helper cells interact specifically with MHC class II molecules. CD 8+ T-cytotoxic cells interact specifically with MHC class I molecules.
 How do you form a protein & place it IEW in the plasma membrane? V RE o Transcription of DNA to m. RNA then translation o m. RNA to RER & thru Golgi apparatus o protein is placed in the membrane from the Golgi apparatus o protein is transferred to membrane surface = Mechanism used to put the MHC protein on the T cell plasma membrane
How do you form a protein & place it IEW in the plasma membrane? V RE o Transcription of DNA to m. RNA then translation o m. RNA to RER & thru Golgi apparatus o protein is placed in the membrane from the Golgi apparatus o protein is transferred to membrane surface = Mechanism used to put the MHC protein on the T cell plasma membrane
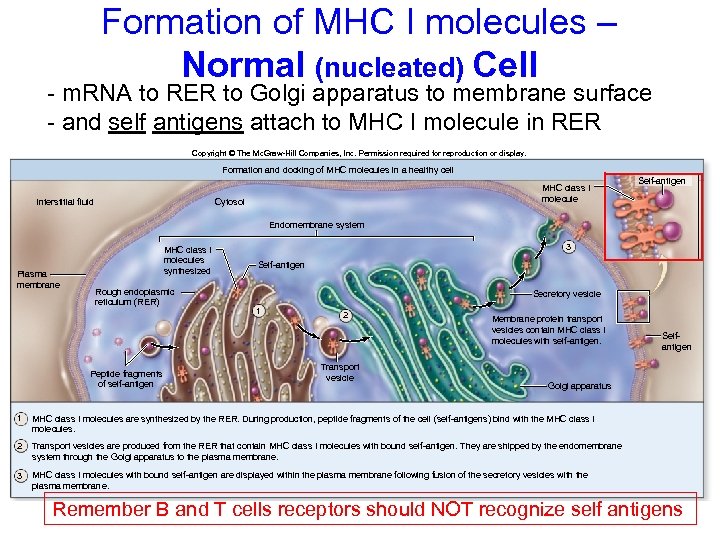 Formation of MHC I molecules – Normal (nucleated) Cell - m. RNA to RER to Golgi apparatus to membrane surface - and self antigens attach to MHC I molecule in RER Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Formation and docking of MHC molecules in a healthy cell Interstitial fluid MHC class I molecule Cytosol Self-antigen Endomembrane system Plasma membrane MHC class I molecules synthesized Rough endoplasmic reticulum (RER) Peptide fragments of self-antigen 3 Self-antigen Secretory vesicle 1 2 Transport vesicle Membrane protein transport vesicles contain MHC class I molecules with self-antigen. Selfantigen Golgi apparatus 1 MHC class I molecules are synthesized by the RER. During production, peptide fragments of the cell (self-antigens) bind with the MHC class I molecules. 2 Transport vesicles are produced from the RER that contain MHC class I molecules with bound self-antigen. They are shipped by the endomembrane system through the Golgi apparatus to the plasma membrane. 3 MHC class I molecules with bound self-antigen are displayed within the plasma membrane following fusion of the secretory vesicles with the plasma membrane. Remember B and T cells receptors should NOT recognize self antigens
Formation of MHC I molecules – Normal (nucleated) Cell - m. RNA to RER to Golgi apparatus to membrane surface - and self antigens attach to MHC I molecule in RER Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Formation and docking of MHC molecules in a healthy cell Interstitial fluid MHC class I molecule Cytosol Self-antigen Endomembrane system Plasma membrane MHC class I molecules synthesized Rough endoplasmic reticulum (RER) Peptide fragments of self-antigen 3 Self-antigen Secretory vesicle 1 2 Transport vesicle Membrane protein transport vesicles contain MHC class I molecules with self-antigen. Selfantigen Golgi apparatus 1 MHC class I molecules are synthesized by the RER. During production, peptide fragments of the cell (self-antigens) bind with the MHC class I molecules. 2 Transport vesicles are produced from the RER that contain MHC class I molecules with bound self-antigen. They are shipped by the endomembrane system through the Golgi apparatus to the plasma membrane. 3 MHC class I molecules with bound self-antigen are displayed within the plasma membrane following fusion of the secretory vesicles with the plasma membrane. Remember B and T cells receptors should NOT recognize self antigens
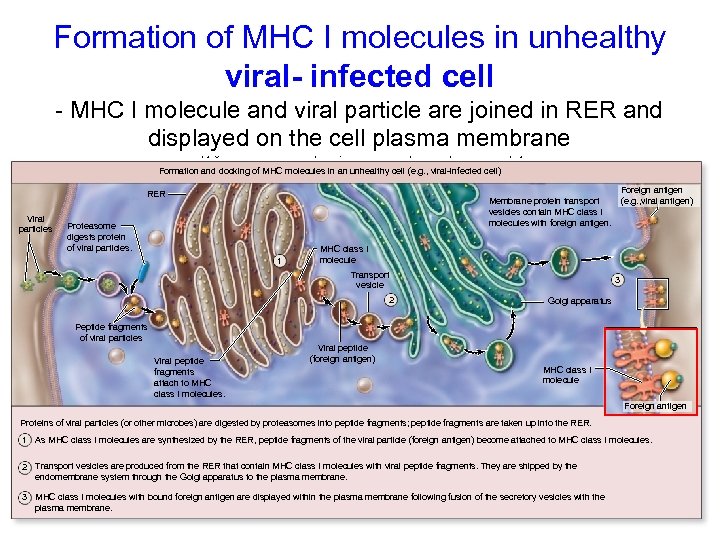 Formation of MHC I molecules in unhealthy viral- infected cell - MHC I molecule and viral particle are joined in RER and displayed on the cell plasma membrane Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Formation and docking of MHC molecules in an unhealthy cell (e. g. , viral-infected cell) Foreign antigen (e. g. , viral antigen) Membrane protein transport vesicles contain MHC class I molecules with foreign antigen. RER Viral particles Proteasome digests protein of viral particles. 1 MHC class I molecule Transport vesicle 2 3 Golgi apparatus Peptide fragments of viral particles Viral peptide fragments attach to MHC class I molecules. Viral peptide (foreign antigen) MHC class I molecule Foreign antigen Proteins of viral particles (or other microbes) are digested by proteasomes into peptide fragments; peptide fragments are taken up into the RER. 1 As MHC class I molecules are synthesized by the RER, peptide fragments of the viral particle (foreign antigen) become attached to MHC class I molecules. 2 Transport vesicles are produced from the RER that contain MHC class I molecules with viral peptide fragments. They are shipped by the endomembrane system through the Golgi apparatus to the plasma membrane. 3 MHC class I molecules with bound foreign antigen are displayed within the plasma membrane following fusion of the secretory vesicles with the plasma membrane.
Formation of MHC I molecules in unhealthy viral- infected cell - MHC I molecule and viral particle are joined in RER and displayed on the cell plasma membrane Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Formation and docking of MHC molecules in an unhealthy cell (e. g. , viral-infected cell) Foreign antigen (e. g. , viral antigen) Membrane protein transport vesicles contain MHC class I molecules with foreign antigen. RER Viral particles Proteasome digests protein of viral particles. 1 MHC class I molecule Transport vesicle 2 3 Golgi apparatus Peptide fragments of viral particles Viral peptide fragments attach to MHC class I molecules. Viral peptide (foreign antigen) MHC class I molecule Foreign antigen Proteins of viral particles (or other microbes) are digested by proteasomes into peptide fragments; peptide fragments are taken up into the RER. 1 As MHC class I molecules are synthesized by the RER, peptide fragments of the viral particle (foreign antigen) become attached to MHC class I molecules. 2 Transport vesicles are produced from the RER that contain MHC class I molecules with viral peptide fragments. They are shipped by the endomembrane system through the Golgi apparatus to the plasma membrane. 3 MHC class I molecules with bound foreign antigen are displayed within the plasma membrane following fusion of the secretory vesicles with the plasma membrane.
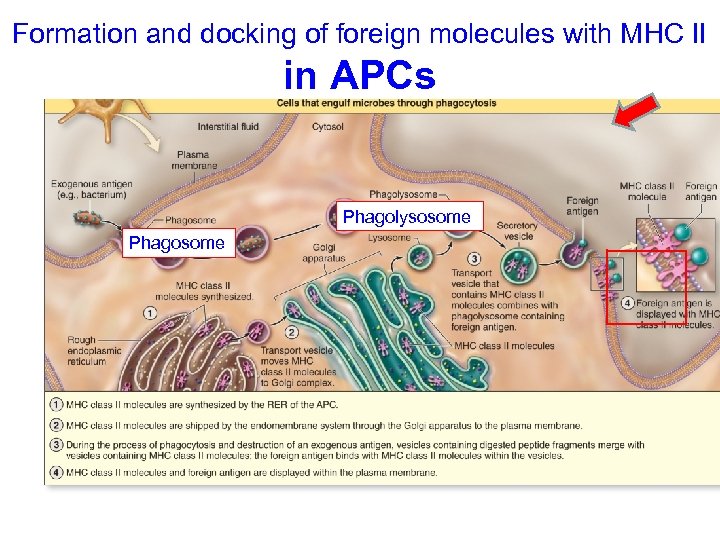 Formation and docking of foreign molecules with MHC II in APCs Phagolysosome Phagosome
Formation and docking of foreign molecules with MHC II in APCs Phagolysosome Phagosome
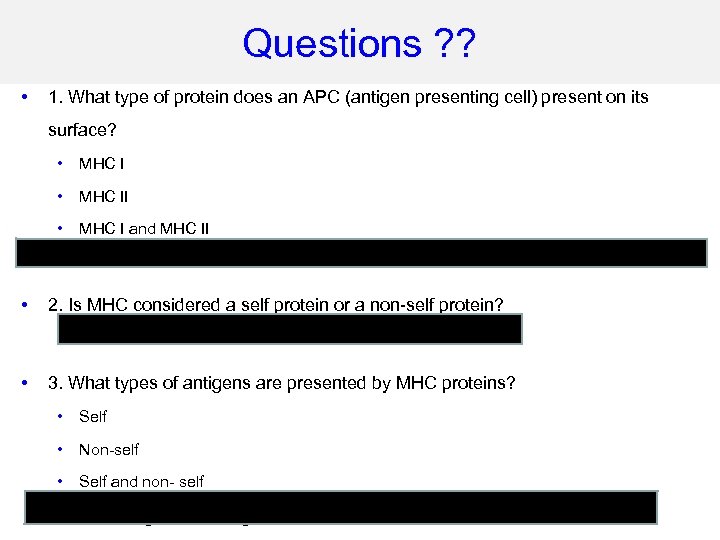 Questions ? ? • 1. What type of protein does an APC (antigen presenting cell) present on its surface? • MHC II • MHC I and MHC II Both – all APCs have MHC II and since an APC has a nucleus it also presents I • 2. Is MHC considered a self protein or a non-self protein? Self protein because it is produced normally in our own cells • 3. What types of antigens are presented by MHC proteins? • Self • Non-self • Self and non- self Both self and non self are presented but the lymphocytes – if educated correctly T cells should not recognize self antigens
Questions ? ? • 1. What type of protein does an APC (antigen presenting cell) present on its surface? • MHC II • MHC I and MHC II Both – all APCs have MHC II and since an APC has a nucleus it also presents I • 2. Is MHC considered a self protein or a non-self protein? Self protein because it is produced normally in our own cells • 3. What types of antigens are presented by MHC proteins? • Self • Non-self • Self and non- self Both self and non self are presented but the lymphocytes – if educated correctly T cells should not recognize self antigens
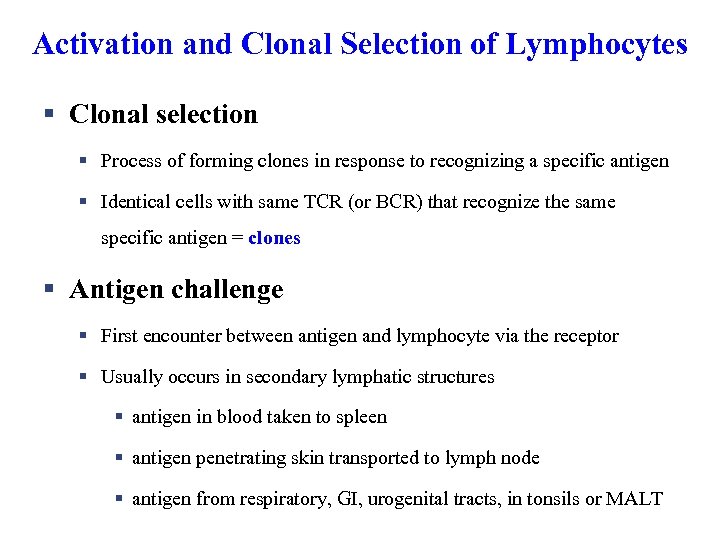 Activation and Clonal Selection of Lymphocytes § Clonal selection § Process of forming clones in response to recognizing a specific antigen § Identical cells with same TCR (or BCR) that recognize the same specific antigen = clones § Antigen challenge § First encounter between antigen and lymphocyte via the receptor § Usually occurs in secondary lymphatic structures § antigen in blood taken to spleen § antigen penetrating skin transported to lymph node § antigen from respiratory, GI, urogenital tracts, in tonsils or MALT
Activation and Clonal Selection of Lymphocytes § Clonal selection § Process of forming clones in response to recognizing a specific antigen § Identical cells with same TCR (or BCR) that recognize the same specific antigen = clones § Antigen challenge § First encounter between antigen and lymphocyte via the receptor § Usually occurs in secondary lymphatic structures § antigen in blood taken to spleen § antigen penetrating skin transported to lymph node § antigen from respiratory, GI, urogenital tracts, in tonsils or MALT
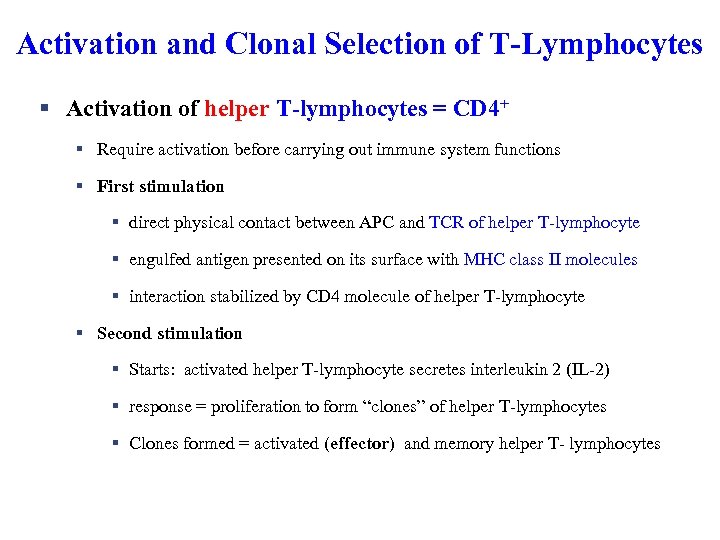 Activation and Clonal Selection of T-Lymphocytes § Activation of helper T-lymphocytes = CD 4+ § Require activation before carrying out immune system functions § First stimulation § direct physical contact between APC and TCR of helper T-lymphocyte § engulfed antigen presented on its surface with MHC class II molecules § interaction stabilized by CD 4 molecule of helper T-lymphocyte § Second stimulation § Starts: activated helper T-lymphocyte secretes interleukin 2 (IL-2) § response = proliferation to form “clones” of helper T-lymphocytes § Clones formed = activated (effector) and memory helper T- lymphocytes
Activation and Clonal Selection of T-Lymphocytes § Activation of helper T-lymphocytes = CD 4+ § Require activation before carrying out immune system functions § First stimulation § direct physical contact between APC and TCR of helper T-lymphocyte § engulfed antigen presented on its surface with MHC class II molecules § interaction stabilized by CD 4 molecule of helper T-lymphocyte § Second stimulation § Starts: activated helper T-lymphocyte secretes interleukin 2 (IL-2) § response = proliferation to form “clones” of helper T-lymphocytes § Clones formed = activated (effector) and memory helper T- lymphocytes
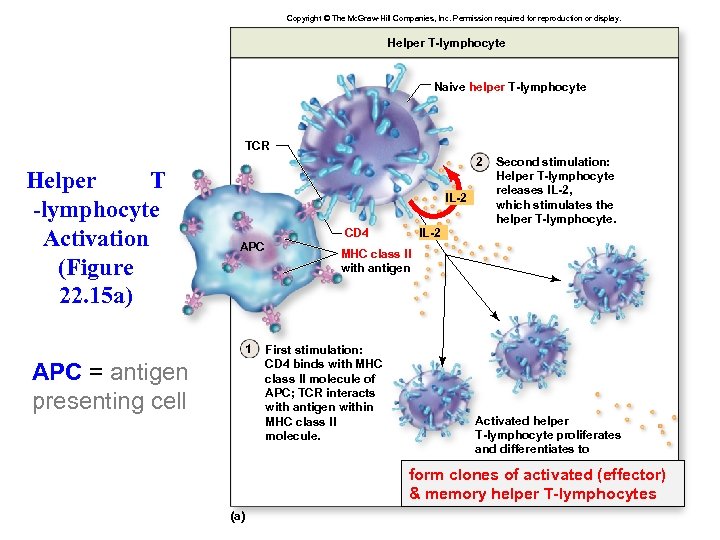 Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Helper T-lymphocyte Naive helper T-lymphocyte TCR Helper T -lymphocyte Activation (Figure 22. 15 a) 2 IL-2 APC 1 APC = antigen presenting cell CD 4 Second stimulation: Helper T-lymphocyte releases IL-2, which stimulates the helper T-lymphocyte. IL-2 MHC class II with antigen First stimulation: CD 4 binds with MHC class II molecule of APC; TCR interacts with antigen within MHC class II molecule. Activated helper T-lymphocyte proliferates and differentiates to form clones of activated (effector) & memory helper T-lymphocytes (a)
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Helper T-lymphocyte Naive helper T-lymphocyte TCR Helper T -lymphocyte Activation (Figure 22. 15 a) 2 IL-2 APC 1 APC = antigen presenting cell CD 4 Second stimulation: Helper T-lymphocyte releases IL-2, which stimulates the helper T-lymphocyte. IL-2 MHC class II with antigen First stimulation: CD 4 binds with MHC class II molecule of APC; TCR interacts with antigen within MHC class II molecule. Activated helper T-lymphocyte proliferates and differentiates to form clones of activated (effector) & memory helper T-lymphocytes (a)
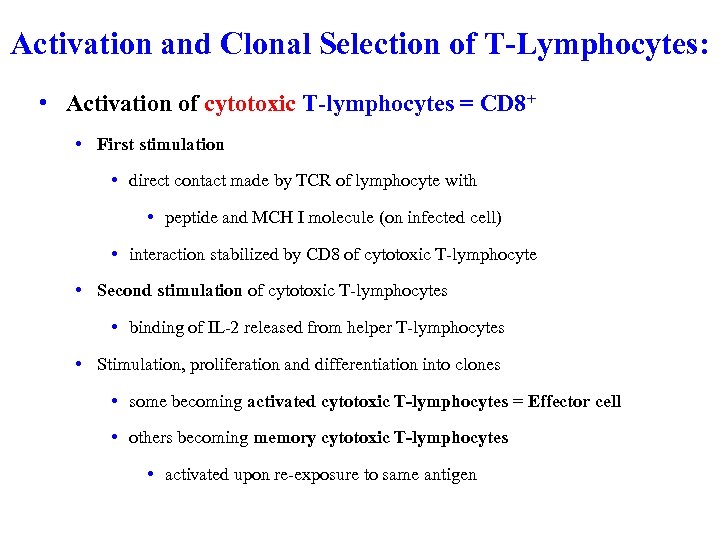 Activation and Clonal Selection of T-Lymphocytes: • Activation of cytotoxic T-lymphocytes = CD 8+ • First stimulation • direct contact made by TCR of lymphocyte with • peptide and MCH I molecule (on infected cell) • interaction stabilized by CD 8 of cytotoxic T-lymphocyte • Second stimulation of cytotoxic T-lymphocytes • binding of IL-2 released from helper T-lymphocytes • Stimulation, proliferation and differentiation into clones • some becoming activated cytotoxic T-lymphocytes = Effector cell • others becoming memory cytotoxic T-lymphocytes • activated upon re-exposure to same antigen
Activation and Clonal Selection of T-Lymphocytes: • Activation of cytotoxic T-lymphocytes = CD 8+ • First stimulation • direct contact made by TCR of lymphocyte with • peptide and MCH I molecule (on infected cell) • interaction stabilized by CD 8 of cytotoxic T-lymphocyte • Second stimulation of cytotoxic T-lymphocytes • binding of IL-2 released from helper T-lymphocytes • Stimulation, proliferation and differentiation into clones • some becoming activated cytotoxic T-lymphocytes = Effector cell • others becoming memory cytotoxic T-lymphocytes • activated upon re-exposure to same antigen
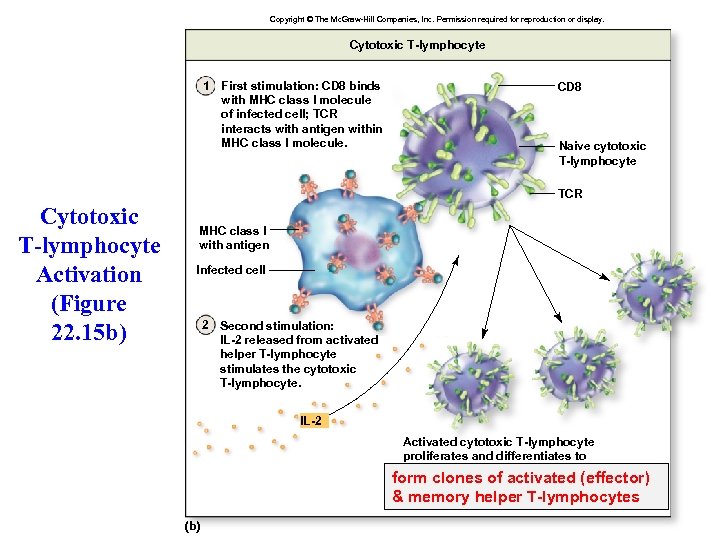 Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Cytotoxic T-lymphocyte 1 First stimulation: CD 8 binds with MHC class I molecule of infected cell; TCR interacts with antigen within MHC class I molecule. CD 8 Naive cytotoxic T-lymphocyte TCR Cytotoxic T-lymphocyte Activation (Figure 22. 15 b) MHC class I with antigen Infected cell 2 Second stimulation: IL-2 released from activated helper T-lymphocyte stimulates the cytotoxic T-lymphocyte. IL-2 Activated cytotoxic T-lymphocyte proliferates and differentiates to . form clones of activated (effector) & memory helper T-lymphocytes (b)
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Cytotoxic T-lymphocyte 1 First stimulation: CD 8 binds with MHC class I molecule of infected cell; TCR interacts with antigen within MHC class I molecule. CD 8 Naive cytotoxic T-lymphocyte TCR Cytotoxic T-lymphocyte Activation (Figure 22. 15 b) MHC class I with antigen Infected cell 2 Second stimulation: IL-2 released from activated helper T-lymphocyte stimulates the cytotoxic T-lymphocyte. IL-2 Activated cytotoxic T-lymphocyte proliferates and differentiates to . form clones of activated (effector) & memory helper T-lymphocytes (b)
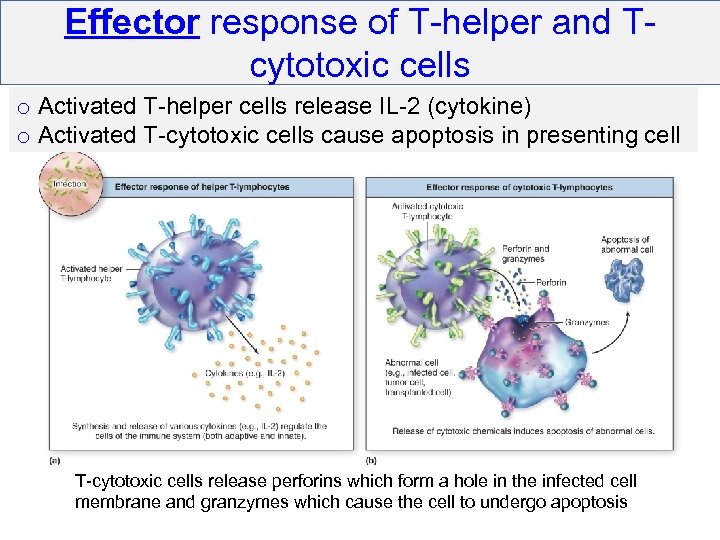 Effector response of T-helper and Tcytotoxic cells o Activated T-helper cells release IL-2 (cytokine) o Activated T-cytotoxic cells cause apoptosis in presenting cell T-cytotoxic cells release perforins which form a hole in the infected cell membrane and granzymes which cause the cell to undergo apoptosis
Effector response of T-helper and Tcytotoxic cells o Activated T-helper cells release IL-2 (cytokine) o Activated T-cytotoxic cells cause apoptosis in presenting cell T-cytotoxic cells release perforins which form a hole in the infected cell membrane and granzymes which cause the cell to undergo apoptosis
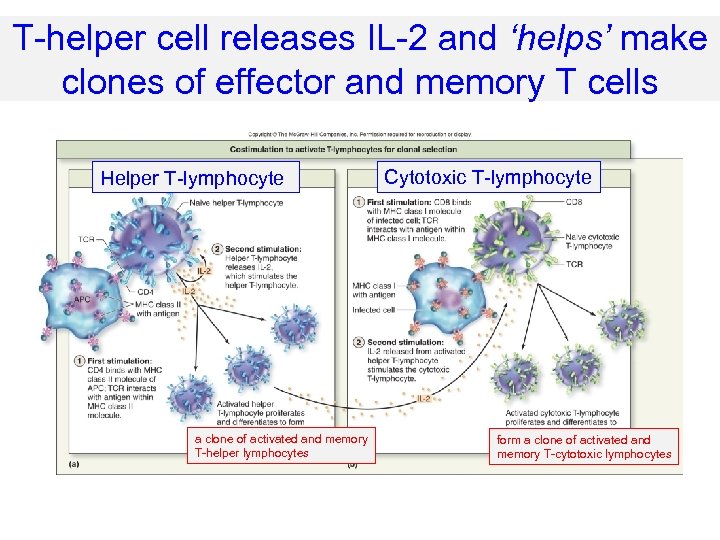 T-helper cell releases IL-2 and ‘helps’ make clones of effector and memory T cells Helper T-lymphocyte a clone of activated and memory T-helper lymphocytes Cytotoxic T-lymphocyte form a clone of activated and memory T-cytotoxic lymphocytes
T-helper cell releases IL-2 and ‘helps’ make clones of effector and memory T cells Helper T-lymphocyte a clone of activated and memory T-helper lymphocytes Cytotoxic T-lymphocyte form a clone of activated and memory T-cytotoxic lymphocytes
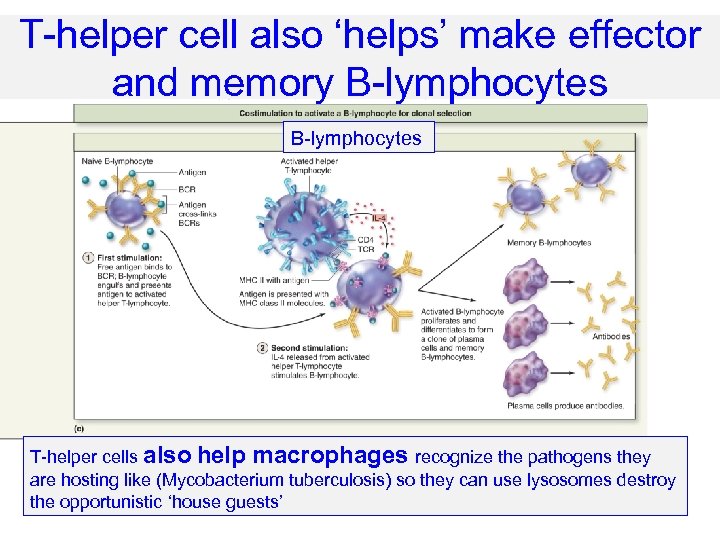 T-helper cell also ‘helps’ make effector and memory B-lymphocytes T-helper cells also help macrophages recognize the pathogens they are hosting like (Mycobacterium tuberculosis) so they can use lysosomes destroy the opportunistic ‘house guests’
T-helper cell also ‘helps’ make effector and memory B-lymphocytes T-helper cells also help macrophages recognize the pathogens they are hosting like (Mycobacterium tuberculosis) so they can use lysosomes destroy the opportunistic ‘house guests’
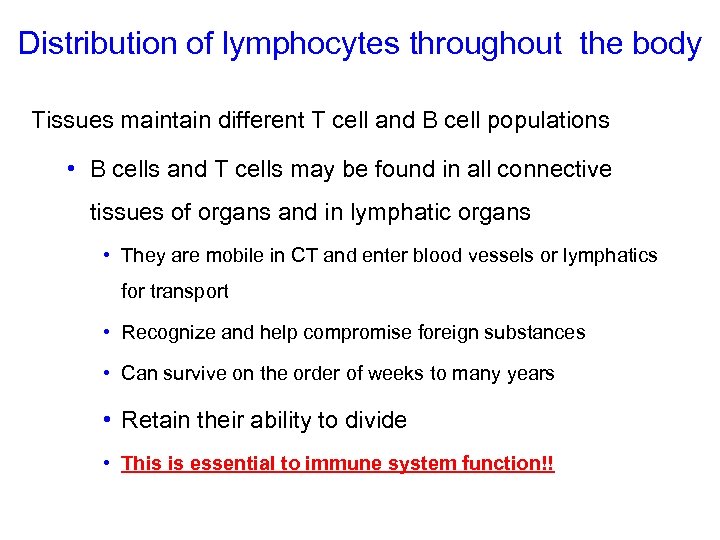 Distribution of lymphocytes throughout the body Tissues maintain different T cell and B cell populations • B cells and T cells may be found in all connective tissues of organs and in lymphatic organs • They are mobile in CT and enter blood vessels or lymphatics for transport • Recognize and help compromise foreign substances • Can survive on the order of weeks to many years • Retain their ability to divide • This is essential to immune system function!!
Distribution of lymphocytes throughout the body Tissues maintain different T cell and B cell populations • B cells and T cells may be found in all connective tissues of organs and in lymphatic organs • They are mobile in CT and enter blood vessels or lymphatics for transport • Recognize and help compromise foreign substances • Can survive on the order of weeks to many years • Retain their ability to divide • This is essential to immune system function!!
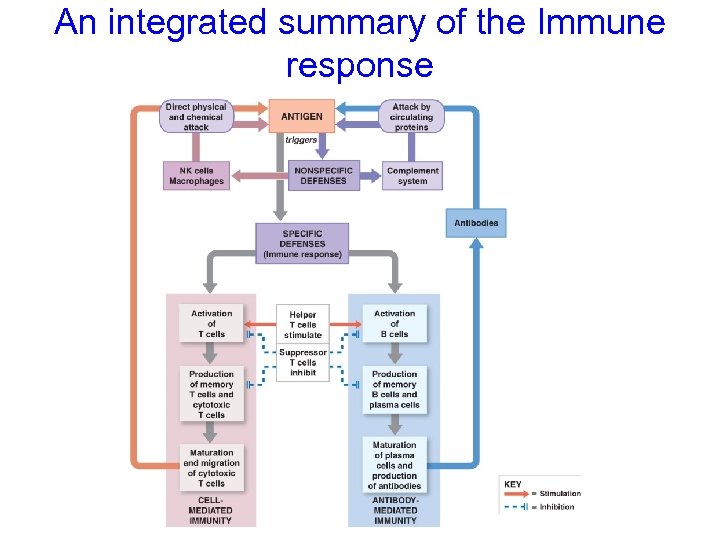 An integrated summary of the Immune response
An integrated summary of the Immune response
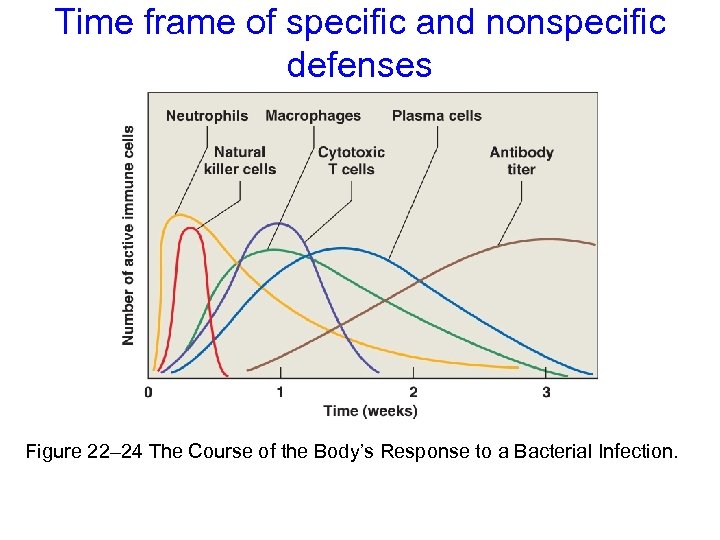 Time frame of specific and nonspecific defenses Figure 22– 24 The Course of the Body’s Response to a Bacterial Infection.
Time frame of specific and nonspecific defenses Figure 22– 24 The Course of the Body’s Response to a Bacterial Infection.
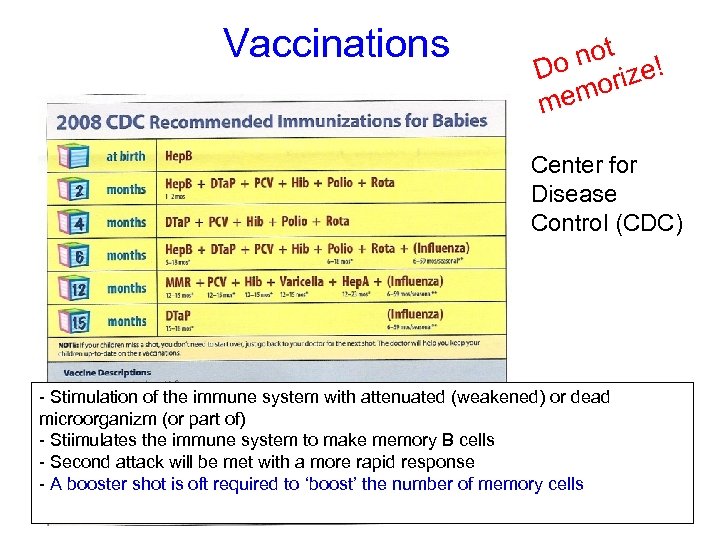 Vaccinations not Do ize! mor me Center for Disease Control (CDC) - Stimulation of the immune system with attenuated (weakened) or dead microorganizm (or part of) - Stiimulates the immune system to make memory B cells - Second attack will be met with a more rapid response - A booster shot is oft required to ‘boost’ the number of memory cells
Vaccinations not Do ize! mor me Center for Disease Control (CDC) - Stimulation of the immune system with attenuated (weakened) or dead microorganizm (or part of) - Stiimulates the immune system to make memory B cells - Second attack will be met with a more rapid response - A booster shot is oft required to ‘boost’ the number of memory cells
 Immune System Disorders § Autoimmune Disorders § A malfunction of system that recognizes and ignores “normal” antigens § Activated B cells make auto-antibodies against our own body’s cells § Examples include: § Multiple Sclerosis § Rheumatoid arthritis § Insulin-dependent diabetes mellitus (IDDM)
Immune System Disorders § Autoimmune Disorders § A malfunction of system that recognizes and ignores “normal” antigens § Activated B cells make auto-antibodies against our own body’s cells § Examples include: § Multiple Sclerosis § Rheumatoid arthritis § Insulin-dependent diabetes mellitus (IDDM)
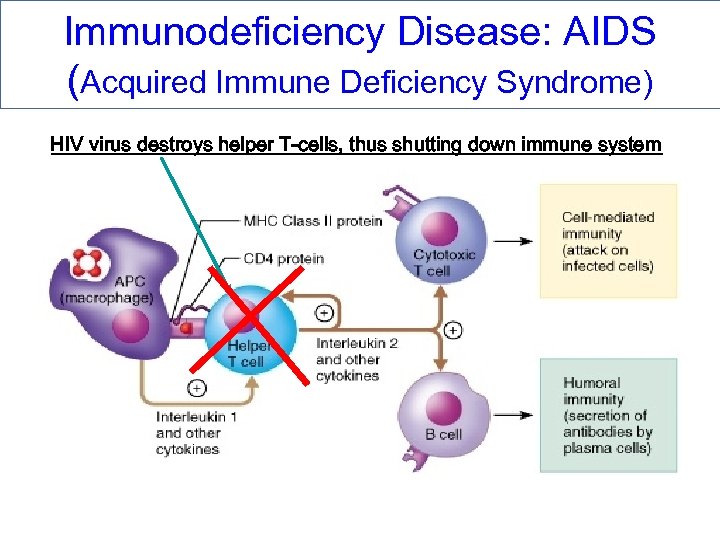 Immunodeficiency Disease: AIDS (Acquired Immune Deficiency Syndrome) HIV virus destroys helper T-cells, thus shutting down immune system
Immunodeficiency Disease: AIDS (Acquired Immune Deficiency Syndrome) HIV virus destroys helper T-cells, thus shutting down immune system
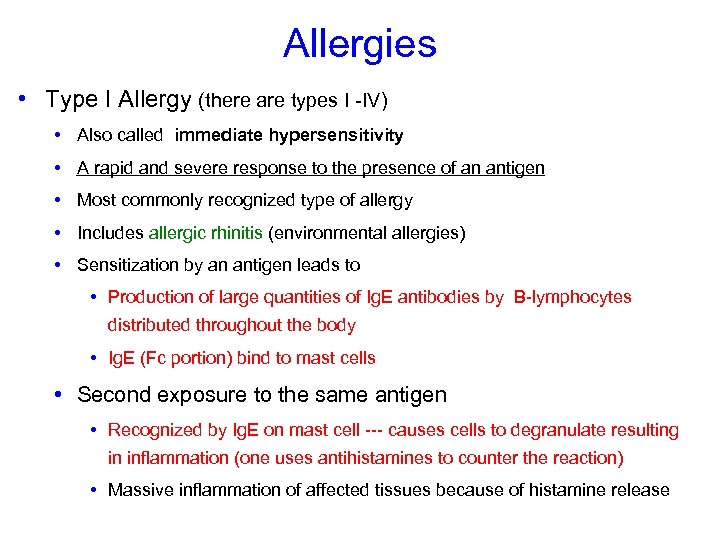 Allergies • Type I Allergy (there are types I -IV) • Also called immediate hypersensitivity • A rapid and severe response to the presence of an antigen • Most commonly recognized type of allergy • Includes allergic rhinitis (environmental allergies) • Sensitization by an antigen leads to • Production of large quantities of Ig. E antibodies by B-lymphocytes distributed throughout the body • Ig. E (Fc portion) bind to mast cells • Second exposure to the same antigen • Recognized by Ig. E on mast cell --- causes cells to degranulate resulting in inflammation (one uses antihistamines to counter the reaction) • Massive inflammation of affected tissues because of histamine release
Allergies • Type I Allergy (there are types I -IV) • Also called immediate hypersensitivity • A rapid and severe response to the presence of an antigen • Most commonly recognized type of allergy • Includes allergic rhinitis (environmental allergies) • Sensitization by an antigen leads to • Production of large quantities of Ig. E antibodies by B-lymphocytes distributed throughout the body • Ig. E (Fc portion) bind to mast cells • Second exposure to the same antigen • Recognized by Ig. E on mast cell --- causes cells to degranulate resulting in inflammation (one uses antihistamines to counter the reaction) • Massive inflammation of affected tissues because of histamine release
 Anaphylaxis: An extreme allergic reaction • Anaphylaxis • Ig. E causes mast cells and basophils to release chemicals like histamine and other vasodilators • Can be fatal • Affects cells throughout body • Changes capillary leaky (permeability) • Produce swelling (hives) on skin • Smooth muscles of respiratory system contract • Make breathing difficult (bronchioconstriction) • Peripheral vasodilatation • Can cause circulatory collapse (anaphylactic shock)
Anaphylaxis: An extreme allergic reaction • Anaphylaxis • Ig. E causes mast cells and basophils to release chemicals like histamine and other vasodilators • Can be fatal • Affects cells throughout body • Changes capillary leaky (permeability) • Produce swelling (hives) on skin • Smooth muscles of respiratory system contract • Make breathing difficult (bronchioconstriction) • Peripheral vasodilatation • Can cause circulatory collapse (anaphylactic shock)
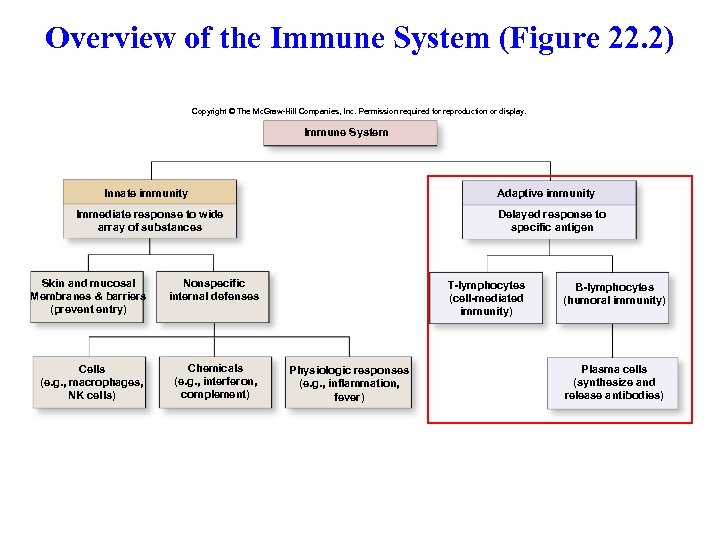 Overview of the Immune System (Figure 22. 2) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Immune System Innate immunity Adaptive immunity Immediate response to wide array of substances Skin and mucosal Membranes & barriers (prevent entry) Nonspecific internal defenses Cells (e. g. , macrophages, NK cells) Chemicals (e. g. , interferon, complement) Delayed response to specific antigen T-lymphocytes (cell-mediated immunity) Physiologic responses (e. g. , inflammation, fever) B-lymphocytes (humoral immunity) Plasma cells (synthesize and release antibodies)
Overview of the Immune System (Figure 22. 2) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Immune System Innate immunity Adaptive immunity Immediate response to wide array of substances Skin and mucosal Membranes & barriers (prevent entry) Nonspecific internal defenses Cells (e. g. , macrophages, NK cells) Chemicals (e. g. , interferon, complement) Delayed response to specific antigen T-lymphocytes (cell-mediated immunity) Physiologic responses (e. g. , inflammation, fever) B-lymphocytes (humoral immunity) Plasma cells (synthesize and release antibodies)


