b73914663902202560182300f5b175a3.ppt
- Количество слайдов: 50
 Narcan and Opioids: What You Need to Know to Manage at Job Corps Diane A. Tennies, Ph. D, LADC Lead TEAP Specialist John Kulig, MD, MPH Lead Medical Specialist
Narcan and Opioids: What You Need to Know to Manage at Job Corps Diane A. Tennies, Ph. D, LADC Lead TEAP Specialist John Kulig, MD, MPH Lead Medical Specialist
 Learning Objectives Participants will be able to: • Describe the scope, origins and consequences of the nation’s current epidemic of opioid misuse • Compare medication assisted treatment (MAT) options for opioid dependence • Recognize the signs and symptoms of opioid overdose • Treat suspected opioid overdose with intranasal naloxone (Narcan®)
Learning Objectives Participants will be able to: • Describe the scope, origins and consequences of the nation’s current epidemic of opioid misuse • Compare medication assisted treatment (MAT) options for opioid dependence • Recognize the signs and symptoms of opioid overdose • Treat suspected opioid overdose with intranasal naloxone (Narcan®)
 Definitions • opiate - a drug containing opium or its derivatives - e. g. , morphine, codeine, heroin • opioid - any synthetic narcotic that has opiate-like activities, but is not derived from opium – e. g. , hydrocodone, oxycodone, fentanyl, methadone • Note: The term “opioid” will be used throughout this presentation to include both opiates and opioids
Definitions • opiate - a drug containing opium or its derivatives - e. g. , morphine, codeine, heroin • opioid - any synthetic narcotic that has opiate-like activities, but is not derived from opium – e. g. , hydrocodone, oxycodone, fentanyl, methadone • Note: The term “opioid” will be used throughout this presentation to include both opiates and opioids
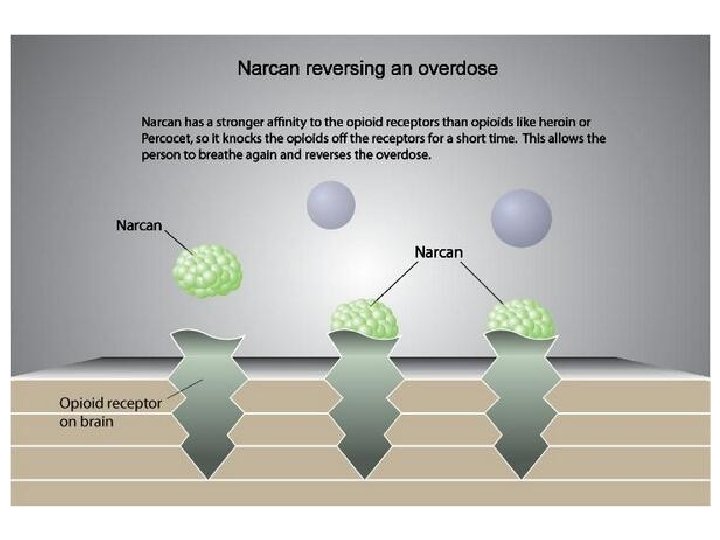
 More Definitions • Medication assisted treatment (MAT) is a type of addiction therapy, provided in a certified, licensed opioid treatment program or a physician's office-based treatment setting that provides maintenance medication. Treatment typically includes behavioral counseling in addition to medication. • Current MAT options include methadone, buprenorphine-naloxone (Suboxone) and naltrexone (Vivitrol). • Naloxone (brand name Narcan®) is a lifesaving, short-acting drug for emergency use in opioid overdose.
More Definitions • Medication assisted treatment (MAT) is a type of addiction therapy, provided in a certified, licensed opioid treatment program or a physician's office-based treatment setting that provides maintenance medication. Treatment typically includes behavioral counseling in addition to medication. • Current MAT options include methadone, buprenorphine-naloxone (Suboxone) and naltrexone (Vivitrol). • Naloxone (brand name Narcan®) is a lifesaving, short-acting drug for emergency use in opioid overdose.
 Origins of an Epidemic
Origins of an Epidemic
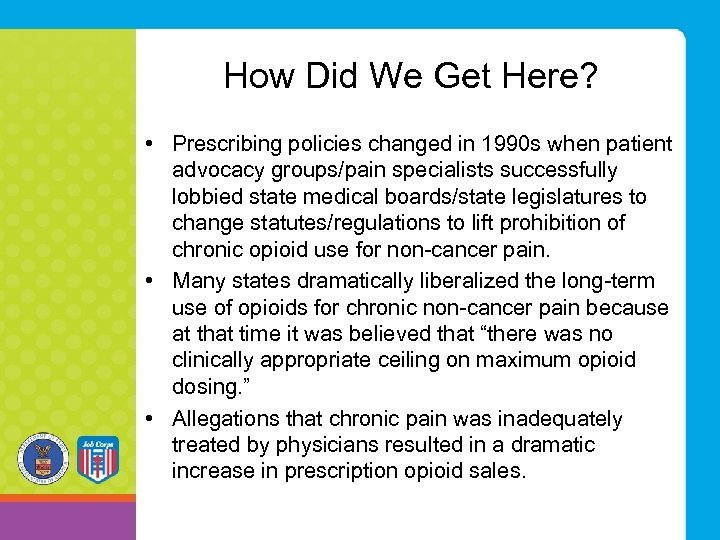 How Did We Get Here? • Prescribing policies changed in 1990 s when patient advocacy groups/pain specialists successfully lobbied state medical boards/state legislatures to change statutes/regulations to lift prohibition of chronic opioid use for non-cancer pain. • Many states dramatically liberalized the long-term use of opioids for chronic non-cancer pain because at that time it was believed that “there was no clinically appropriate ceiling on maximum opioid dosing. ” • Allegations that chronic pain was inadequately treated by physicians resulted in a dramatic increase in prescription opioid sales.
How Did We Get Here? • Prescribing policies changed in 1990 s when patient advocacy groups/pain specialists successfully lobbied state medical boards/state legislatures to change statutes/regulations to lift prohibition of chronic opioid use for non-cancer pain. • Many states dramatically liberalized the long-term use of opioids for chronic non-cancer pain because at that time it was believed that “there was no clinically appropriate ceiling on maximum opioid dosing. ” • Allegations that chronic pain was inadequately treated by physicians resulted in a dramatic increase in prescription opioid sales.
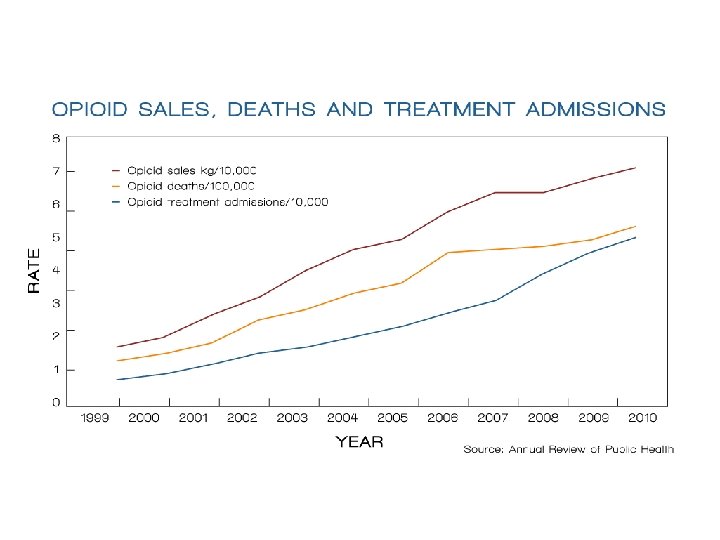
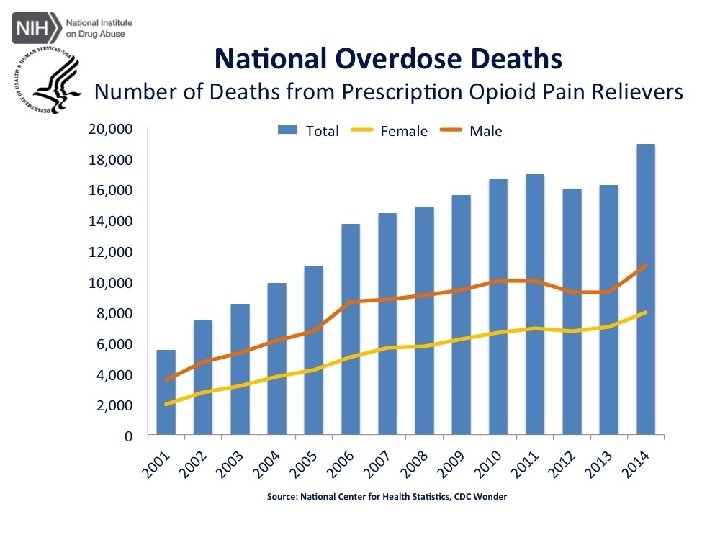
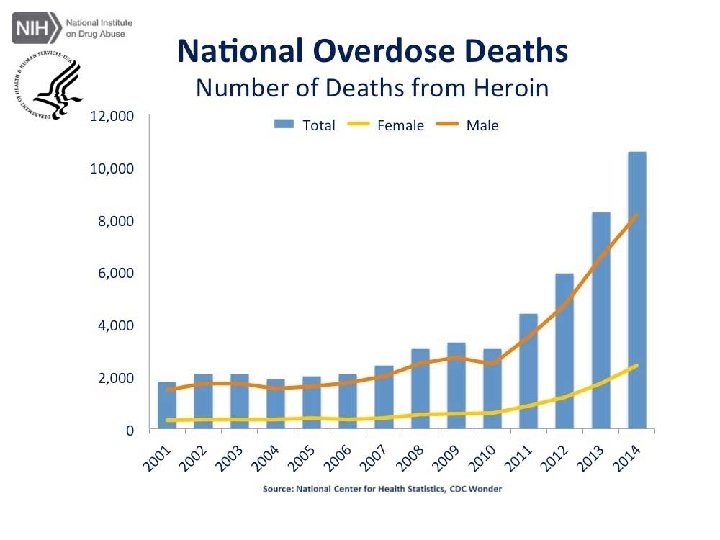
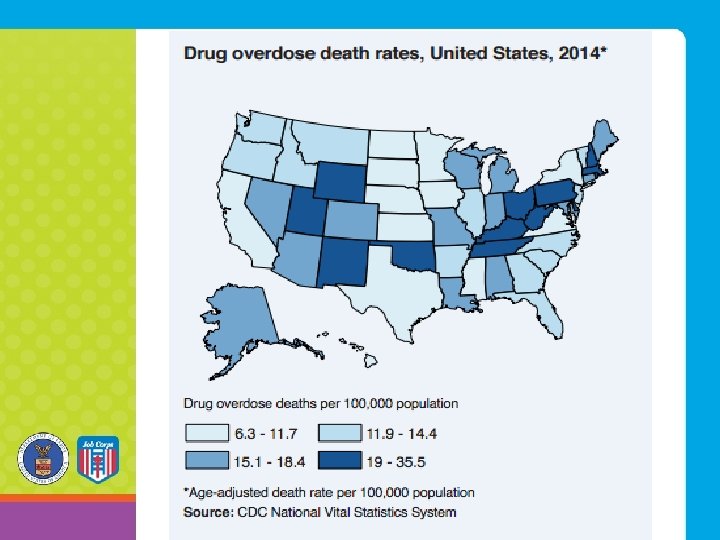
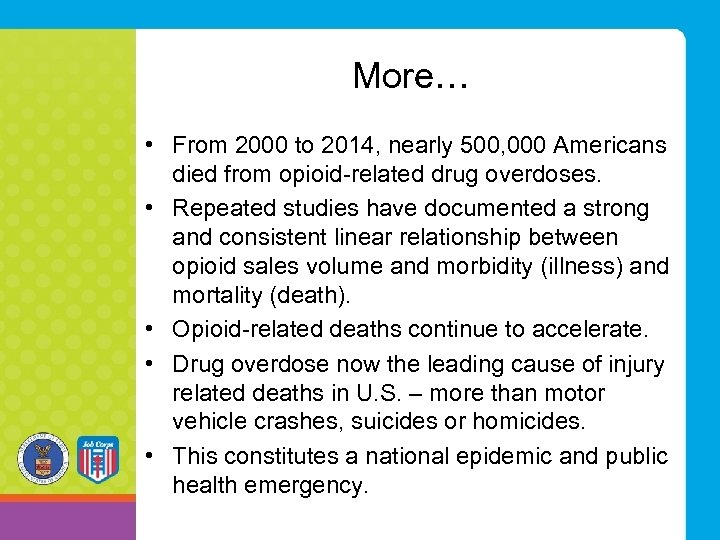 More… • From 2000 to 2014, nearly 500, 000 Americans died from opioid-related drug overdoses. • Repeated studies have documented a strong and consistent linear relationship between opioid sales volume and morbidity (illness) and mortality (death). • Opioid-related deaths continue to accelerate. • Drug overdose now the leading cause of injury related deaths in U. S. – more than motor vehicle crashes, suicides or homicides. • This constitutes a national epidemic and public health emergency.
More… • From 2000 to 2014, nearly 500, 000 Americans died from opioid-related drug overdoses. • Repeated studies have documented a strong and consistent linear relationship between opioid sales volume and morbidity (illness) and mortality (death). • Opioid-related deaths continue to accelerate. • Drug overdose now the leading cause of injury related deaths in U. S. – more than motor vehicle crashes, suicides or homicides. • This constitutes a national epidemic and public health emergency.
 The Data • 21. 5 million Americans age 12 years or older had a substance use disorder in 2014. • 1. 9 million involved prescription pain relievers. • 586, 000 involved heroin. • An estimated 23% of individuals who use heroin develop opioid addiction. • In 2014, 467, 000 adolescents were current nonmedical users of pain reliever, with 168, 000 having an addiction to prescription pain meds. • In 2014, an estimated 28, 000 adolescents had used heroin in the past year, and an estimated 16, 000 were current heroin users.
The Data • 21. 5 million Americans age 12 years or older had a substance use disorder in 2014. • 1. 9 million involved prescription pain relievers. • 586, 000 involved heroin. • An estimated 23% of individuals who use heroin develop opioid addiction. • In 2014, 467, 000 adolescents were current nonmedical users of pain reliever, with 168, 000 having an addiction to prescription pain meds. • In 2014, an estimated 28, 000 adolescents had used heroin in the past year, and an estimated 16, 000 were current heroin users.
 Economic Impact • Economic impact of the Opioid Epidemic: $55 billion in health and social costs related to prescription opioid abuse each year (in 2011!) • $20 billion in emergency department and inpatient care for opioid poisonings.
Economic Impact • Economic impact of the Opioid Epidemic: $55 billion in health and social costs related to prescription opioid abuse each year (in 2011!) • $20 billion in emergency department and inpatient care for opioid poisonings.
 More Importantly – the Human Impact On an average day in the U. S. in 2014: • More than 650, 000 opioid prescriptions are dispensed. • 3, 900 people initiate nonmedical use of prescription opioids. • 580 people initiate heroin use. • 78 people die from an opioid-related overdose.
More Importantly – the Human Impact On an average day in the U. S. in 2014: • More than 650, 000 opioid prescriptions are dispensed. • 3, 900 people initiate nonmedical use of prescription opioids. • 580 people initiate heroin use. • 78 people die from an opioid-related overdose.
 Treatment Options: MAT
Treatment Options: MAT
 Medication Assisted Treatment (MAT) • In combination with behavioral therapy, MAT is an effective strategy to treat opioid addiction. • Medications work by reducing cravings and withdrawal symptoms. • Mental status is not altered during maintenance therapy. • Withdrawal can be precipitated if the medication is abruptly discontinued rather than slowly tapered.
Medication Assisted Treatment (MAT) • In combination with behavioral therapy, MAT is an effective strategy to treat opioid addiction. • Medications work by reducing cravings and withdrawal symptoms. • Mental status is not altered during maintenance therapy. • Withdrawal can be precipitated if the medication is abruptly discontinued rather than slowly tapered.
 MAT has been shown to … • Increase treatment retention • Reduce opioid use • Reduce risk behaviors that transmit HIV and hepatitis C virus infection • Reduce recidivism • Reduce mortality
MAT has been shown to … • Increase treatment retention • Reduce opioid use • Reduce risk behaviors that transmit HIV and hepatitis C virus infection • Reduce recidivism • Reduce mortality
 Four MAT Options 1. ) Daily methadone by mouth obtained at licensed clinics only. 2. ) Daily buprenorphine/naloxone by mouth (brand name Suboxone). This is a tablet or film that is taken and absorbed under the tongue on a daily basis. It must be prescribed by a physician with specific training and a distinct DEA registration number.
Four MAT Options 1. ) Daily methadone by mouth obtained at licensed clinics only. 2. ) Daily buprenorphine/naloxone by mouth (brand name Suboxone). This is a tablet or film that is taken and absorbed under the tongue on a daily basis. It must be prescribed by a physician with specific training and a distinct DEA registration number.
 More MAT Options 3. ) Buprenorphine/naloxone subdermal implant (brand name Probuphine): This must be inserted by a qualified clinician. It is effective for six months and is indicated only for patients on Suboxone 8 milligrams or less daily. Supplemental sublingual Suboxone may be needed. 4. ) Monthly naltrexone by intramuscular (IM) injection (brand name Vivitrol).
More MAT Options 3. ) Buprenorphine/naloxone subdermal implant (brand name Probuphine): This must be inserted by a qualified clinician. It is effective for six months and is indicated only for patients on Suboxone 8 milligrams or less daily. Supplemental sublingual Suboxone may be needed. 4. ) Monthly naltrexone by intramuscular (IM) injection (brand name Vivitrol).
 In Conclusion • Quality MAT has proven to be an effective treatment, but the majority of people with an opioid use disorder do not receive it. • The vast majority of individuals do not get any treatment and as a result … • Mortality for active IV heroin users has been estimated at 2% per year of use.
In Conclusion • Quality MAT has proven to be an effective treatment, but the majority of people with an opioid use disorder do not receive it. • The vast majority of individuals do not get any treatment and as a result … • Mortality for active IV heroin users has been estimated at 2% per year of use.
 The FY 2017 President’s Budget Requests Include • $920 million over two years for SAMHSA’s State Targeted Response Cooperative Agreements to expand access to MAT. • $15. 9 million for SAMHSA’s Pregnant and Postpartum Women (PPW) program that provides comprehensive residential substance use disorder treatment, prevention, and recovery support services for pregnant and postpartum women and their families. • $30 million over two years for SAMSHA to evaluate the effectiveness of treatment programs.
The FY 2017 President’s Budget Requests Include • $920 million over two years for SAMHSA’s State Targeted Response Cooperative Agreements to expand access to MAT. • $15. 9 million for SAMHSA’s Pregnant and Postpartum Women (PPW) program that provides comprehensive residential substance use disorder treatment, prevention, and recovery support services for pregnant and postpartum women and their families. • $30 million over two years for SAMSHA to evaluate the effectiveness of treatment programs.
 More… • $50 million over two years in National Health Service Corps funding for 900 health professionals to provide substance use disorder treatment services in areas across the country most in need of behavioral health providers. • $10 million for a Buprenorphine Prescribing Authority Demonstration to expand access to buprenorphine by allowing nurse practitioners and physician assistants to write prescriptions.
More… • $50 million over two years in National Health Service Corps funding for 900 health professionals to provide substance use disorder treatment services in areas across the country most in need of behavioral health providers. • $10 million for a Buprenorphine Prescribing Authority Demonstration to expand access to buprenorphine by allowing nurse practitioners and physician assistants to write prescriptions.
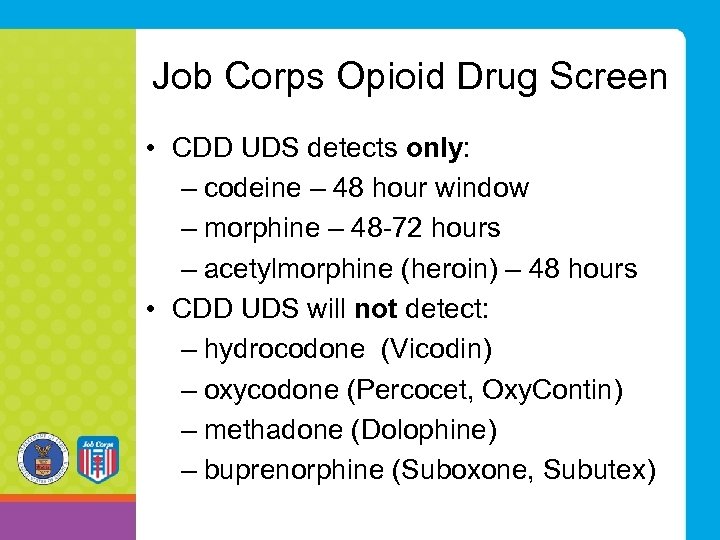 Job Corps Opioid Drug Screen • CDD UDS detects only: – codeine – 48 hour window – morphine – 48 -72 hours – acetylmorphine (heroin) – 48 hours • CDD UDS will not detect: – hydrocodone (Vicodin) – oxycodone (Percocet, Oxy. Contin) – methadone (Dolophine) – buprenorphine (Suboxone, Subutex)
Job Corps Opioid Drug Screen • CDD UDS detects only: – codeine – 48 hour window – morphine – 48 -72 hours – acetylmorphine (heroin) – 48 hours • CDD UDS will not detect: – hydrocodone (Vicodin) – oxycodone (Percocet, Oxy. Contin) – methadone (Dolophine) – buprenorphine (Suboxone, Subutex)
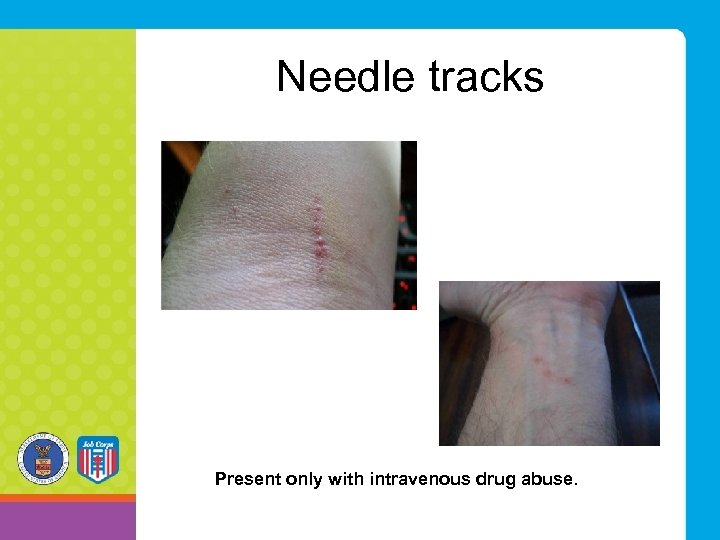 Needle tracks Present only with intravenous drug abuse.
Needle tracks Present only with intravenous drug abuse.
 Risk factors for overdose • Development of tolerance to opioids • Mixing opioids with other drugs and/or alcohol – benzodiazepines, sedatives, cocaine • Chronic medical conditions • Mode of administration • Previous non-fatal overdose • Variation in strength and content of “street drugs” • Using alone
Risk factors for overdose • Development of tolerance to opioids • Mixing opioids with other drugs and/or alcohol – benzodiazepines, sedatives, cocaine • Chronic medical conditions • Mode of administration • Previous non-fatal overdose • Variation in strength and content of “street drugs” • Using alone
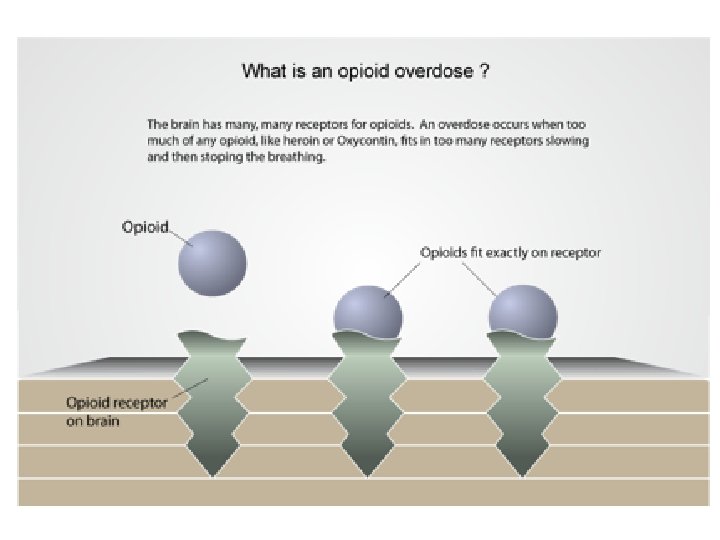

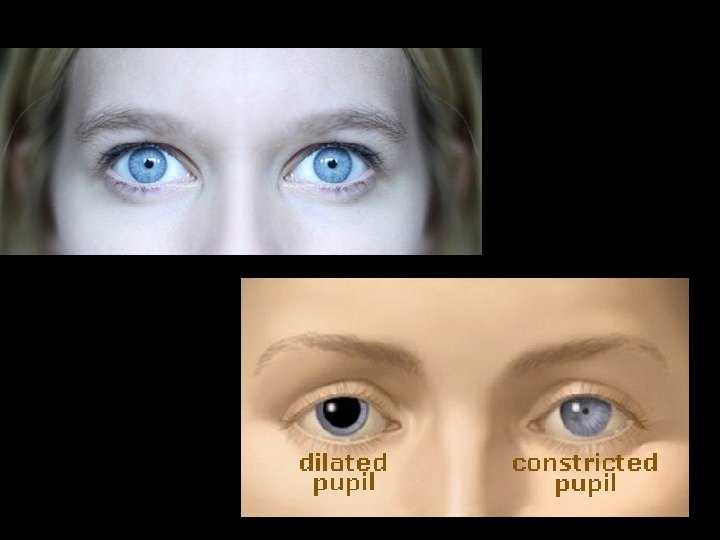
 Signs and symptoms of opioid overdose • An opioid overdose can be identified by a combination of three signs and symptoms referred to as the “opioid overdose triad. ” • Symptoms of the triad are: Ø pinpoint pupils Ø unconsciousness Ø respiratory depression
Signs and symptoms of opioid overdose • An opioid overdose can be identified by a combination of three signs and symptoms referred to as the “opioid overdose triad. ” • Symptoms of the triad are: Ø pinpoint pupils Ø unconsciousness Ø respiratory depression
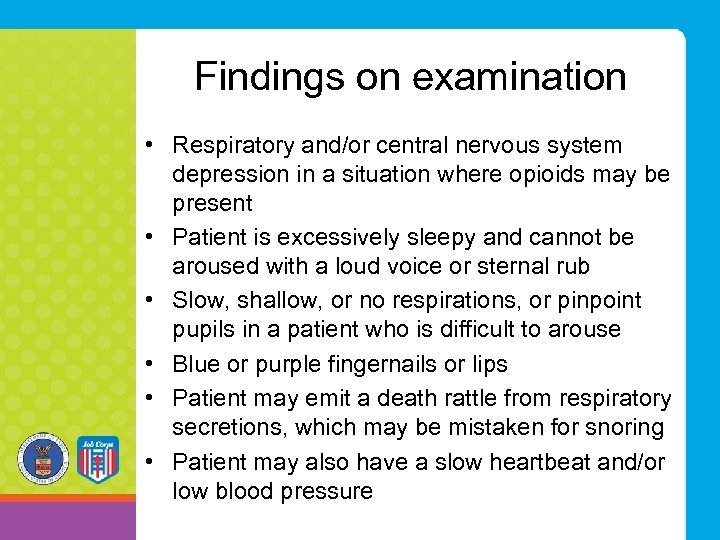 Findings on examination • Respiratory and/or central nervous system depression in a situation where opioids may be present • Patient is excessively sleepy and cannot be aroused with a loud voice or sternal rub • Slow, shallow, or no respirations, or pinpoint pupils in a patient who is difficult to arouse • Blue or purple fingernails or lips • Patient may emit a death rattle from respiratory secretions, which may be mistaken for snoring • Patient may also have a slow heartbeat and/or low blood pressure
Findings on examination • Respiratory and/or central nervous system depression in a situation where opioids may be present • Patient is excessively sleepy and cannot be aroused with a loud voice or sternal rub • Slow, shallow, or no respirations, or pinpoint pupils in a patient who is difficult to arouse • Blue or purple fingernails or lips • Patient may emit a death rattle from respiratory secretions, which may be mistaken for snoring • Patient may also have a slow heartbeat and/or low blood pressure
 Differentiating between overdose and an opioid high
Differentiating between overdose and an opioid high
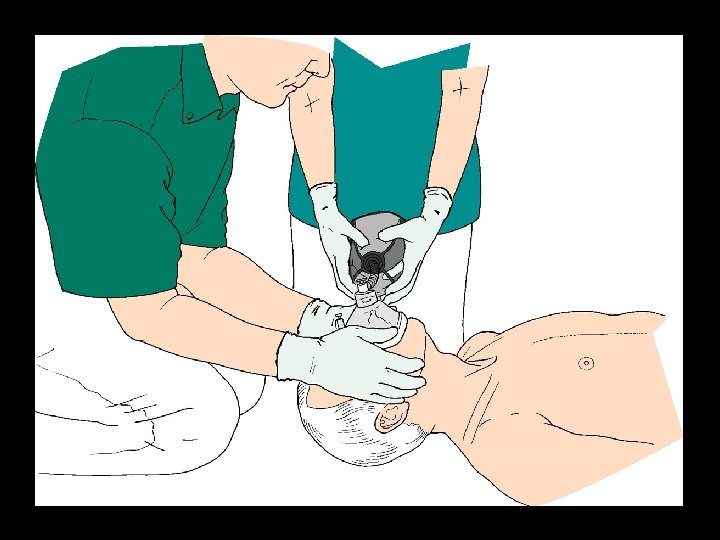
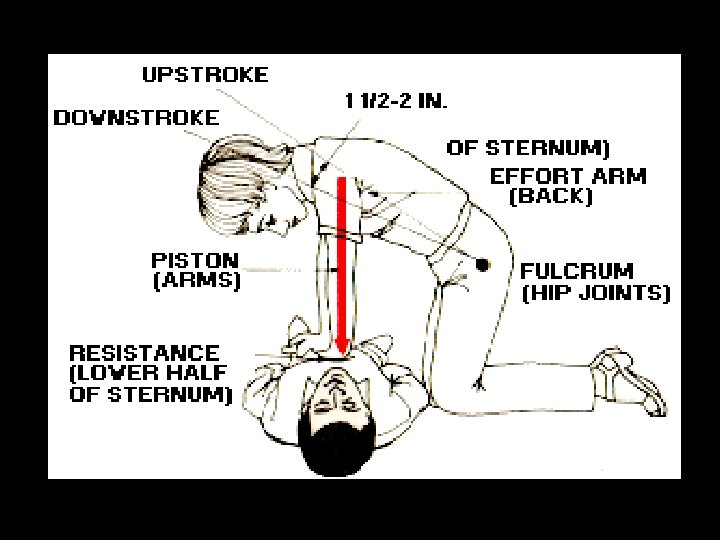
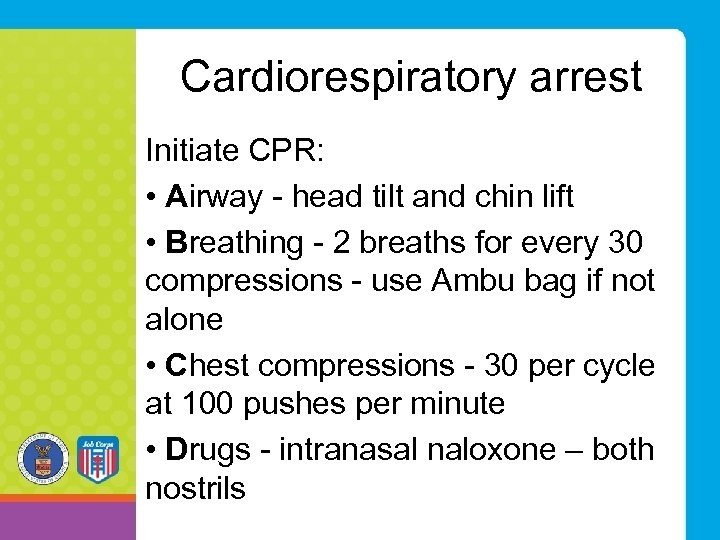 Cardiorespiratory arrest Initiate CPR: • Airway - head tilt and chin lift • Breathing - 2 breaths for every 30 compressions - use Ambu bag if not alone • Chest compressions - 30 per cycle at 100 pushes per minute • Drugs - intranasal naloxone – both nostrils
Cardiorespiratory arrest Initiate CPR: • Airway - head tilt and chin lift • Breathing - 2 breaths for every 30 compressions - use Ambu bag if not alone • Chest compressions - 30 per cycle at 100 pushes per minute • Drugs - intranasal naloxone – both nostrils

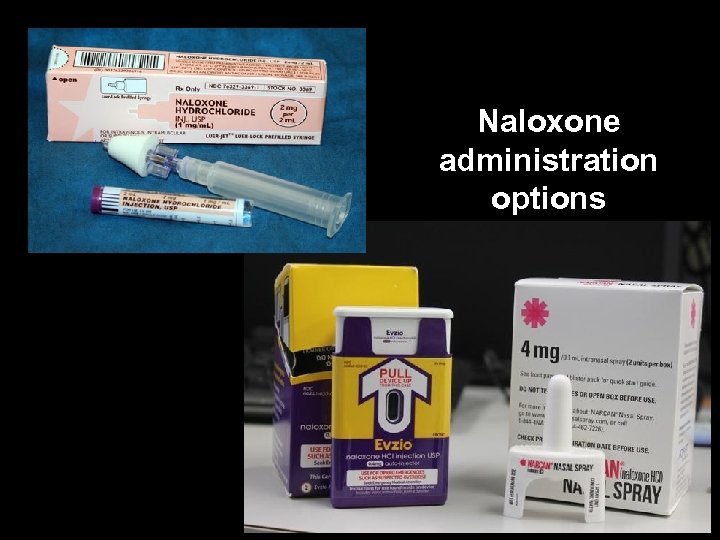 Naloxone administration options
Naloxone administration options
 Standing orders for naloxone • more than half of the 50 U. S. states now have naloxone standing order programs • statewide standing orders have increased the availability and accessibility of naloxone by allowing anyone to walk into their local pharmacy and buy the medication without a prescription • distribution is not limited to people at personal risk of overdose - a potential bystander, such as a family member, could obtain naloxone to administer in an emergency
Standing orders for naloxone • more than half of the 50 U. S. states now have naloxone standing order programs • statewide standing orders have increased the availability and accessibility of naloxone by allowing anyone to walk into their local pharmacy and buy the medication without a prescription • distribution is not limited to people at personal risk of overdose - a potential bystander, such as a family member, could obtain naloxone to administer in an emergency
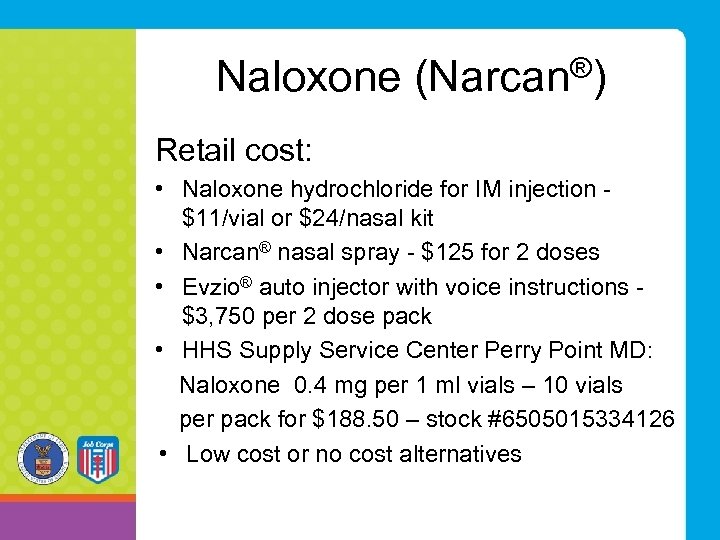 Naloxone (Narcan®) Retail cost: • Naloxone hydrochloride for IM injection - $11/vial or $24/nasal kit • Narcan® nasal spray - $125 for 2 doses • Evzio® auto injector with voice instructions - $3, 750 per 2 dose pack • HHS Supply Service Center Perry Point MD: Naloxone 0. 4 mg per 1 ml vials – 10 vials per pack for $188. 50 – stock #6505015334126 • Low cost or no cost alternatives
Naloxone (Narcan®) Retail cost: • Naloxone hydrochloride for IM injection - $11/vial or $24/nasal kit • Narcan® nasal spray - $125 for 2 doses • Evzio® auto injector with voice instructions - $3, 750 per 2 dose pack • HHS Supply Service Center Perry Point MD: Naloxone 0. 4 mg per 1 ml vials – 10 vials per pack for $188. 50 – stock #6505015334126 • Low cost or no cost alternatives
 How to administer naloxone nasal spray
How to administer naloxone nasal spray
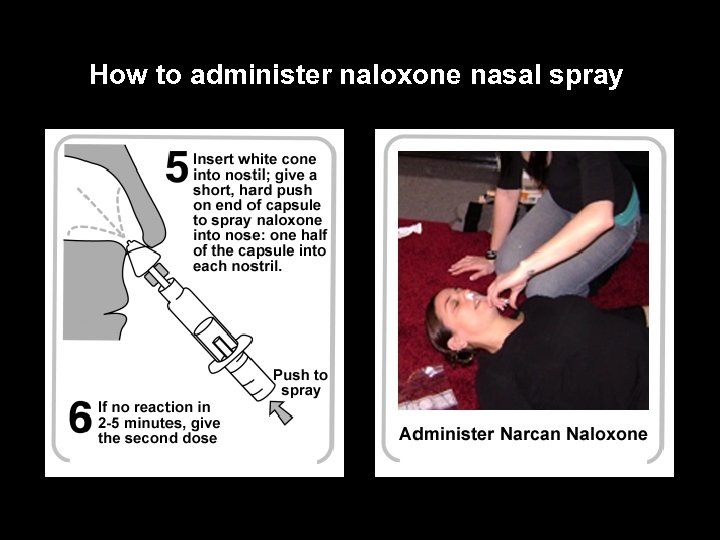 How to administer naloxone nasal spray
How to administer naloxone nasal spray
 When should naloxone be administered? • Unconscious individual with obvious signs of recent drug use - “works”/paraphernalia • Individual exhibiting symptoms of the opioid overdose triad - check pupils, breathing, level of consciousness • Unconscious individual with known history of opioid abuse, including patients currently on “medication assisted treatment” (MAT) for opioid dependence • Self-report of opioid use in a conscious individual developing symptoms of opioid overdose
When should naloxone be administered? • Unconscious individual with obvious signs of recent drug use - “works”/paraphernalia • Individual exhibiting symptoms of the opioid overdose triad - check pupils, breathing, level of consciousness • Unconscious individual with known history of opioid abuse, including patients currently on “medication assisted treatment” (MAT) for opioid dependence • Self-report of opioid use in a conscious individual developing symptoms of opioid overdose
 Time to intervene • With opioid overdoses, the difference between surviving and dying depends on breathing and oxygen. • Fortunately, opioid overdose is rarely instantaneous; people slowly stop breathing after the drug was used. • There may be time to intervene between when an overdose starts and a victim dies. • Furthermore, not all overdoses are fatal. Without any intervention, some overdose victims may become unresponsive with slowed breathing, but will still take in enough oxygen to survive and wake up.
Time to intervene • With opioid overdoses, the difference between surviving and dying depends on breathing and oxygen. • Fortunately, opioid overdose is rarely instantaneous; people slowly stop breathing after the drug was used. • There may be time to intervene between when an overdose starts and a victim dies. • Furthermore, not all overdoses are fatal. Without any intervention, some overdose victims may become unresponsive with slowed breathing, but will still take in enough oxygen to survive and wake up.
 What if naloxone is mistakenly administered? • No adverse effects in a healthy individual. • No altered mental status. • Not shown to produce tolerance or cause physical or psychological dependence. • When administered in usual doses in the absence of opioids, naloxone exhibits essentially no pharmacologic activity.
What if naloxone is mistakenly administered? • No adverse effects in a healthy individual. • No altered mental status. • Not shown to produce tolerance or cause physical or psychological dependence. • When administered in usual doses in the absence of opioids, naloxone exhibits essentially no pharmacologic activity.
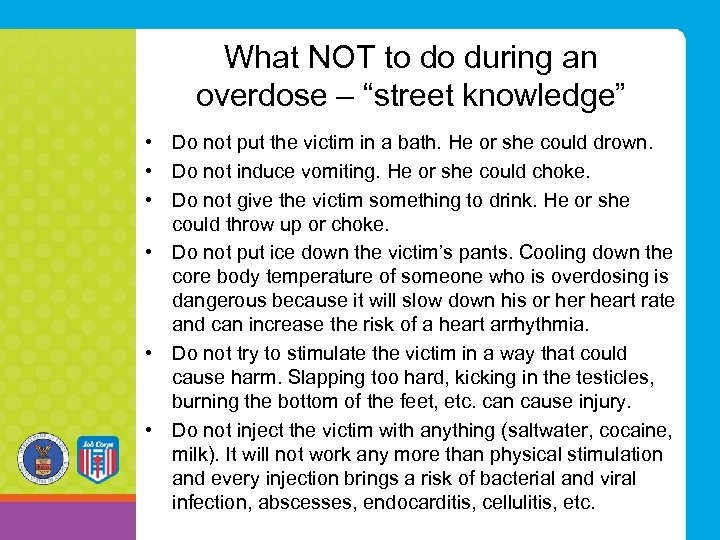 What NOT to do during an overdose – “street knowledge” • Do not put the victim in a bath. He or she could drown. • Do not induce vomiting. He or she could choke. • Do not give the victim something to drink. He or she could throw up or choke. • Do not put ice down the victim’s pants. Cooling down the core body temperature of someone who is overdosing is dangerous because it will slow down his or heart rate and can increase the risk of a heart arrhythmia. • Do not try to stimulate the victim in a way that could cause harm. Slapping too hard, kicking in the testicles, burning the bottom of the feet, etc. can cause injury. • Do not inject the victim with anything (saltwater, cocaine, milk). It will not work any more than physical stimulation and every injection brings a risk of bacterial and viral infection, abscesses, endocarditis, cellulitis, etc.
What NOT to do during an overdose – “street knowledge” • Do not put the victim in a bath. He or she could drown. • Do not induce vomiting. He or she could choke. • Do not give the victim something to drink. He or she could throw up or choke. • Do not put ice down the victim’s pants. Cooling down the core body temperature of someone who is overdosing is dangerous because it will slow down his or heart rate and can increase the risk of a heart arrhythmia. • Do not try to stimulate the victim in a way that could cause harm. Slapping too hard, kicking in the testicles, burning the bottom of the feet, etc. can cause injury. • Do not inject the victim with anything (saltwater, cocaine, milk). It will not work any more than physical stimulation and every injection brings a risk of bacterial and viral infection, abscesses, endocarditis, cellulitis, etc.
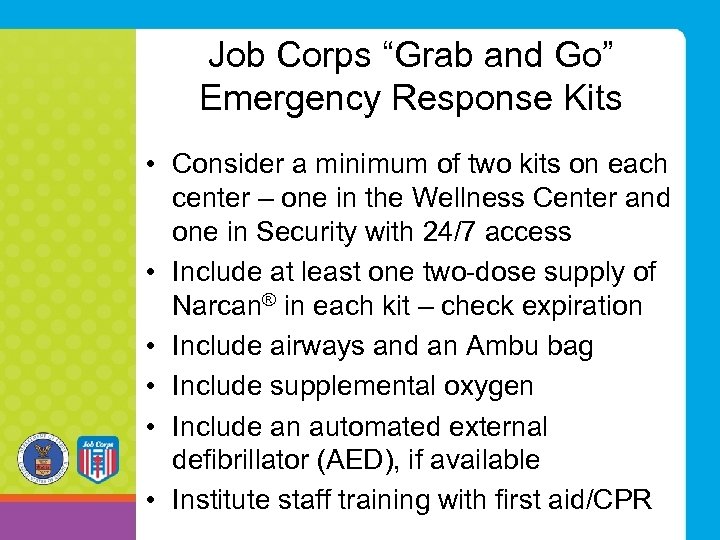 Job Corps “Grab and Go” Emergency Response Kits • Consider a minimum of two kits on each center – one in the Wellness Center and one in Security with 24/7 access • Include at least one two-dose supply of Narcan® in each kit – check expiration • Include airways and an Ambu bag • Include supplemental oxygen • Include an automated external defibrillator (AED), if available • Institute staff training with first aid/CPR
Job Corps “Grab and Go” Emergency Response Kits • Consider a minimum of two kits on each center – one in the Wellness Center and one in Security with 24/7 access • Include at least one two-dose supply of Narcan® in each kit – check expiration • Include airways and an Ambu bag • Include supplemental oxygen • Include an automated external defibrillator (AED), if available • Institute staff training with first aid/CPR
 References • https: //www. drugabuse. gov/drugs-abuse/opioids - NIDA information on opioids • http: //www. asam. org/docs/defaultsource/advocacy/opioid-addiction-disease-factsfigures. pdf - ASAM facts and figures 2016 • http: //www. mass. gov/eohhs/docs/dph/substanceabuse/core-competencies-for-naloxone-pilotparticipants. pdf - Massachusetts DPH education • http: //naloxoneinfo. org/case-studies/standing-orders - standing orders for Narcan • http: //www. cdc. gov/media/modules/dpk/2016/dpkpod/rr 6501 e 1 er-ebook. pdf - CDC guideline for prescribing opioids for chronic pain
References • https: //www. drugabuse. gov/drugs-abuse/opioids - NIDA information on opioids • http: //www. asam. org/docs/defaultsource/advocacy/opioid-addiction-disease-factsfigures. pdf - ASAM facts and figures 2016 • http: //www. mass. gov/eohhs/docs/dph/substanceabuse/core-competencies-for-naloxone-pilotparticipants. pdf - Massachusetts DPH education • http: //naloxoneinfo. org/case-studies/standing-orders - standing orders for Narcan • http: //www. cdc. gov/media/modules/dpk/2016/dpkpod/rr 6501 e 1 er-ebook. pdf - CDC guideline for prescribing opioids for chronic pain


