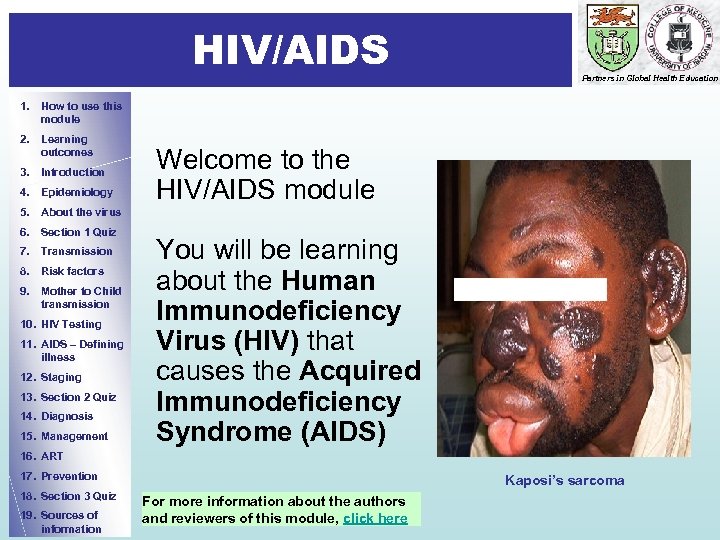
 n t r o d u c t i o n 1 HIV/AIDS Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Welcome to the HIV/AIDS module 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management You will be learning about the Human Immunodeficiency Virus (HIV) that causes the Acquired Immunodeficiency Syndrome (AIDS) 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Kaposi’s sarcoma For more information about the authors and reviewers of this module, click here
n t r o d u c t i o n 1 HIV/AIDS Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Welcome to the HIV/AIDS module 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management You will be learning about the Human Immunodeficiency Virus (HIV) that causes the Acquired Immunodeficiency Syndrome (AIDS) 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Kaposi’s sarcoma For more information about the authors and reviewers of this module, click here
 How to use this module 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology • • 5. About the virus 6. Section 1 Quiz 7. Transmission • 8. Risk factors 9. Mother to Child transmission • 10. HIV Testing 11. AIDS – Defining illness • 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Partners in Global Health Education This self-directed learning (SDL) module has been designed for medical and other health care students We suggest that you start with the learning outcomes and try to keep these in mind as you go through the module slide by slide and at your own pace. Print-out the answer sheet. Write your answers to the questions on the mark sheet as best you can before looking at the answers. Repeat the module until you have achieved a mark of > 10/13 (>80%). You should research any issues that you are unsure about. Look in your textbooks, access the on-line resources indicated at the end of the module and discuss with your peers and teachers. Finally, enjoy your learning! We hope that this module will complement your learning about Global Burden of Disease from other sources.
How to use this module 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology • • 5. About the virus 6. Section 1 Quiz 7. Transmission • 8. Risk factors 9. Mother to Child transmission • 10. HIV Testing 11. AIDS – Defining illness • 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Partners in Global Health Education This self-directed learning (SDL) module has been designed for medical and other health care students We suggest that you start with the learning outcomes and try to keep these in mind as you go through the module slide by slide and at your own pace. Print-out the answer sheet. Write your answers to the questions on the mark sheet as best you can before looking at the answers. Repeat the module until you have achieved a mark of > 10/13 (>80%). You should research any issues that you are unsure about. Look in your textbooks, access the on-line resources indicated at the end of the module and discuss with your peers and teachers. Finally, enjoy your learning! We hope that this module will complement your learning about Global Burden of Disease from other sources.
 I n t r o d u c t i o n 2 Learning Outcomes 1. How to use this module Partners in Global Health Education By the end of the module, you will be expected to be able to: 2. Learning outcomes 3. Introduction § state the routes of HIV transmission § name the risk factors for HIV transmission § describe how HIV causes disease following infection 8. Risk factors § list the specific clinical features of HIV infection 9. Mother to Child transmission § discuss disease staging and AIDS-defining illnesses 10. HIV Testing § discuss how clinical features and serology are used in diagnosis § describe how HIV is treated § describe important features of prevention programmes at the community level 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
I n t r o d u c t i o n 2 Learning Outcomes 1. How to use this module Partners in Global Health Education By the end of the module, you will be expected to be able to: 2. Learning outcomes 3. Introduction § state the routes of HIV transmission § name the risk factors for HIV transmission § describe how HIV causes disease following infection 8. Risk factors § list the specific clinical features of HIV infection 9. Mother to Child transmission § discuss disease staging and AIDS-defining illnesses 10. HIV Testing § discuss how clinical features and serology are used in diagnosis § describe how HIV is treated § describe important features of prevention programmes at the community level 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
 E p i d e m i o l o g y 1 What is HIV? 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education • HIV is the causative agent of AIDS • It is an RNA virus - its genetic information is stored on a single strand of RNA instead of the double-stranded DNA found in most organisms • The RNA includes 3 genes that are essential for retroviral replication: gag, env, pol • It belongs to the retrovirus family - distinguished by the presence of an enzyme called reverse transcriptase which converts RNA into DNA. HIV reverse transcriptase is error -prone and, therefore, introduces a high mutation rate in the viral genome • There are two types of HIV: HIV-1 and HIV-2 • Both HIV-1 and HIV-2 are associated with similar opportunistic infections and AIDS • HIV-1 is much more common worldwide • HIV-2 is found predominantly in West Africa, Angola, and Mozambique
E p i d e m i o l o g y 1 What is HIV? 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education • HIV is the causative agent of AIDS • It is an RNA virus - its genetic information is stored on a single strand of RNA instead of the double-stranded DNA found in most organisms • The RNA includes 3 genes that are essential for retroviral replication: gag, env, pol • It belongs to the retrovirus family - distinguished by the presence of an enzyme called reverse transcriptase which converts RNA into DNA. HIV reverse transcriptase is error -prone and, therefore, introduces a high mutation rate in the viral genome • There are two types of HIV: HIV-1 and HIV-2 • Both HIV-1 and HIV-2 are associated with similar opportunistic infections and AIDS • HIV-1 is much more common worldwide • HIV-2 is found predominantly in West Africa, Angola, and Mozambique
 Evolution of HIV epidemic Partners in Global Health Education 1. How to use this module 2. Learning outcomes 1981: CDC issues warning on a rare pneumonia in LA 2001: China’s acknowledgement 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Early 90 s: Central & Latin America Early/mid 1990 s: Asia End-1980 s: Sub Saharan Africa Source: UNAIDS, 2001
Evolution of HIV epidemic Partners in Global Health Education 1. How to use this module 2. Learning outcomes 1981: CDC issues warning on a rare pneumonia in LA 2001: China’s acknowledgement 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Early 90 s: Central & Latin America Early/mid 1990 s: Asia End-1980 s: Sub Saharan Africa Source: UNAIDS, 2001
 Epidemiology 1. How to use this module Partners in Global Health Education In 2008: • An estimated 33. 4 million people 2. Learning outcomes • 3. Introduction were living with HIV 2. 7 million people acquired HIV 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information AIDS orphans in Zambia In 2008: AIDS killed 2. 0 million people. The number of people living with HIV continues to rise in every region, with the steepest increases occurring in East and Central Asia and in Eastern Europe reflecting the combined effects of continued high rates of new HIV infections and the beneficial impacts of ART • Sub-Saharan Africa remains by far the worst affected region in the world, with 22. 4 million people living with HIV in 2008 • About two-thirds (67%) of all people living with HIV are in sub-Saharan Africa • More than three quarters (76%) of all women living with HIV live in sub. Saharan Africa Source: AIDS epidemic update, 2009; Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization
Epidemiology 1. How to use this module Partners in Global Health Education In 2008: • An estimated 33. 4 million people 2. Learning outcomes • 3. Introduction were living with HIV 2. 7 million people acquired HIV 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information AIDS orphans in Zambia In 2008: AIDS killed 2. 0 million people. The number of people living with HIV continues to rise in every region, with the steepest increases occurring in East and Central Asia and in Eastern Europe reflecting the combined effects of continued high rates of new HIV infections and the beneficial impacts of ART • Sub-Saharan Africa remains by far the worst affected region in the world, with 22. 4 million people living with HIV in 2008 • About two-thirds (67%) of all people living with HIV are in sub-Saharan Africa • More than three quarters (76%) of all women living with HIV live in sub. Saharan Africa Source: AIDS epidemic update, 2009; Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization
 Global epidemiology of HIV/AIDS 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education
Global epidemiology of HIV/AIDS 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education
 Molecular epidemiology 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education • HIV-1 strains can be classified into 3 groups: M (major), N (non-M) and O (outlier) • Groups N and O are limited to Cameroon and neighbouring countries • Group M is further divided into 9 subtypes (A, B, C, D, F, G, H, J and K) and several circulating recombinant forms • Subtype C is the most predominant globally and in Southern Africa • Subtype A is common in Central, West and East Africa • Subtype B in USA and Western Europe • All HIV-1 groups and subtypes have been reported in central Africa
Molecular epidemiology 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education • HIV-1 strains can be classified into 3 groups: M (major), N (non-M) and O (outlier) • Groups N and O are limited to Cameroon and neighbouring countries • Group M is further divided into 9 subtypes (A, B, C, D, F, G, H, J and K) and several circulating recombinant forms • Subtype C is the most predominant globally and in Southern Africa • Subtype A is common in Central, West and East Africa • Subtype B in USA and Western Europe • All HIV-1 groups and subtypes have been reported in central Africa
 Morphology of HIV 1. How to use this module 2. Learning outcomes • It is icosahedral in shape 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Outer envelope studded with spikes formed by envelope (gp 120) and transmembrane (gp 41) glycoproteins • Central core contains consist of – viral proteins (e. g. p 24) – HIV RNA genome – enzymes Partners in Global Health Education
Morphology of HIV 1. How to use this module 2. Learning outcomes • It is icosahedral in shape 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Outer envelope studded with spikes formed by envelope (gp 120) and transmembrane (gp 41) glycoproteins • Central core contains consist of – viral proteins (e. g. p 24) – HIV RNA genome – enzymes Partners in Global Health Education
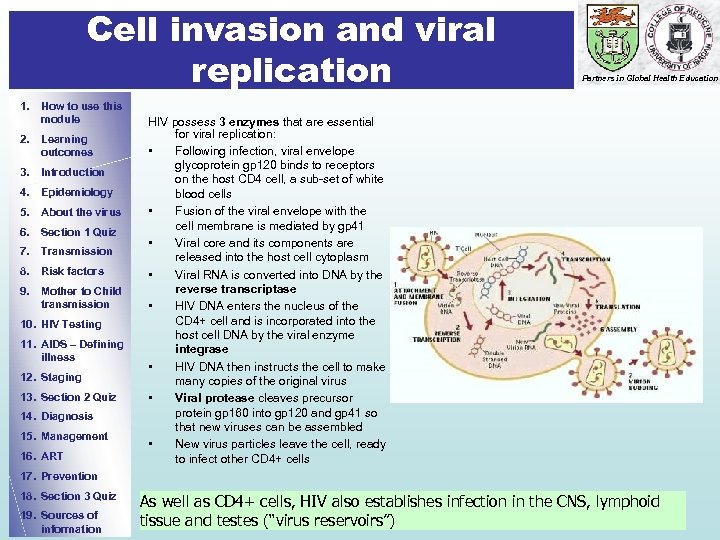 Cell invasion and viral replication 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART Partners in Global Health Education HIV possess 3 enzymes that are essential for viral replication: • Following infection, viral envelope glycoprotein gp 120 binds to receptors on the host CD 4 cell, a sub-set of white blood cells • Fusion of the viral envelope with the cell membrane is mediated by gp 41 • Viral core and its components are released into the host cell cytoplasm • Viral RNA is converted into DNA by the reverse transcriptase • HIV DNA enters the nucleus of the CD 4+ cell and is incorporated into the host cell DNA by the viral enzyme integrase • HIV DNA then instructs the cell to make many copies of the original virus • Viral protease cleaves precursor protein gp 160 into gp 120 and gp 41 so that new viruses can be assembled • New virus particles leave the cell, ready to infect other CD 4+ cells 17. Prevention 18. Section 3 Quiz 19. Sources of information As well as CD 4+ cells, HIV also establishes infection in the CNS, lymphoid tissue and testes (“virus reservoirs”)
Cell invasion and viral replication 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART Partners in Global Health Education HIV possess 3 enzymes that are essential for viral replication: • Following infection, viral envelope glycoprotein gp 120 binds to receptors on the host CD 4 cell, a sub-set of white blood cells • Fusion of the viral envelope with the cell membrane is mediated by gp 41 • Viral core and its components are released into the host cell cytoplasm • Viral RNA is converted into DNA by the reverse transcriptase • HIV DNA enters the nucleus of the CD 4+ cell and is incorporated into the host cell DNA by the viral enzyme integrase • HIV DNA then instructs the cell to make many copies of the original virus • Viral protease cleaves precursor protein gp 160 into gp 120 and gp 41 so that new viruses can be assembled • New virus particles leave the cell, ready to infect other CD 4+ cells 17. Prevention 18. Section 3 Quiz 19. Sources of information As well as CD 4+ cells, HIV also establishes infection in the CNS, lymphoid tissue and testes (“virus reservoirs”)
 End of Section 1 Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Well done! You have come to the end of the first section. 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We suggest that you answer Question 1 to assess your learning so far. Please remember to write your answers on the mark sheet before looking at the correct answers!
End of Section 1 Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Well done! You have come to the end of the first section. 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We suggest that you answer Question 1 to assess your learning so far. Please remember to write your answers on the mark sheet before looking at the correct answers!
 Question 1: Regarding HIV Write “T” or “F” on the answer sheet. When you have completed all 4 questions, click on the box and mark your answers 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education Click to for the correct answer a) Reverse transcriptase reliably converts the viral RNA into DNA in the host cell cytoplasm b) HIV infection rates are increasing most rapidly in sub-Saharan Africa c) HIV 1 subtype C is the most prevalent viral subtype d) As well as CD 4+ cells, primary infection of the brain occurs a b c d
Question 1: Regarding HIV Write “T” or “F” on the answer sheet. When you have completed all 4 questions, click on the box and mark your answers 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education Click to for the correct answer a) Reverse transcriptase reliably converts the viral RNA into DNA in the host cell cytoplasm b) HIV infection rates are increasing most rapidly in sub-Saharan Africa c) HIV 1 subtype C is the most prevalent viral subtype d) As well as CD 4+ cells, primary infection of the brain occurs a b c d
 How is HIV transmitted? 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Transmission routes: • 5. About the virus 6. Section 1 Quiz • 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing • 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education • Sexual contact: sexual intercourse (vaginal, oral or anal) Direct contact with HIVinfected body fluids such as semen, cervical and vaginal secretions Maternal-to-child transmission (MTCT): from mothers who are HIVpositive to their infants during pregnancy, labour, delivery, and breast-feeding Blood-to-blood transmission: transfusion or direct contact with HIV-infected blood HIV infection occurs in people of all ages, races and nationalities, the rich and the poor. Now that you know how HIV is transmitted, list 5 groups of people who are particularly at risk of acquiring infection. Answers on the next slide.
How is HIV transmitted? 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Transmission routes: • 5. About the virus 6. Section 1 Quiz • 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing • 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education • Sexual contact: sexual intercourse (vaginal, oral or anal) Direct contact with HIVinfected body fluids such as semen, cervical and vaginal secretions Maternal-to-child transmission (MTCT): from mothers who are HIVpositive to their infants during pregnancy, labour, delivery, and breast-feeding Blood-to-blood transmission: transfusion or direct contact with HIV-infected blood HIV infection occurs in people of all ages, races and nationalities, the rich and the poor. Now that you know how HIV is transmitted, list 5 groups of people who are particularly at risk of acquiring infection. Answers on the next slide.
 Major groups at risk of HIV infection Answers: Risk factors (1) 3 1. How to use this module 2. Learning outcomes • 3. Introduction 4. Epidemiology Partners in Global Health Education Sexually active men and women. The most common route of HIV transmission is unprotected, heterosexual intercourse. Women, especially young girls, are more likely than men to become infected due to a complex interplay between biological, socio-economic and cultural factors. Women taking oral contraceptives, which may alter the physical properties of the cervical mucosa, are at greater risk of infection. • People with multiple sexual partners • Being a prostitute or having unprotected sex with a prostitute 9. Mother to Child transmission • People who engage in unprotected anal intercourse 10. HIV Testing • The infants of infected mothers • IV drug abusers: injection using contaminated needles or syringes 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Other important risk factors are: • • • Lack of circumcision: uncircumcised men probably get more prepuceal trauma during intercourse Use of unsterilized instruments - e. g. in body piercing HIV infection also results from sexual abuse of infants and children
Major groups at risk of HIV infection Answers: Risk factors (1) 3 1. How to use this module 2. Learning outcomes • 3. Introduction 4. Epidemiology Partners in Global Health Education Sexually active men and women. The most common route of HIV transmission is unprotected, heterosexual intercourse. Women, especially young girls, are more likely than men to become infected due to a complex interplay between biological, socio-economic and cultural factors. Women taking oral contraceptives, which may alter the physical properties of the cervical mucosa, are at greater risk of infection. • People with multiple sexual partners • Being a prostitute or having unprotected sex with a prostitute 9. Mother to Child transmission • People who engage in unprotected anal intercourse 10. HIV Testing • The infants of infected mothers • IV drug abusers: injection using contaminated needles or syringes 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Other important risk factors are: • • • Lack of circumcision: uncircumcised men probably get more prepuceal trauma during intercourse Use of unsterilized instruments - e. g. in body piercing HIV infection also results from sexual abuse of infants and children
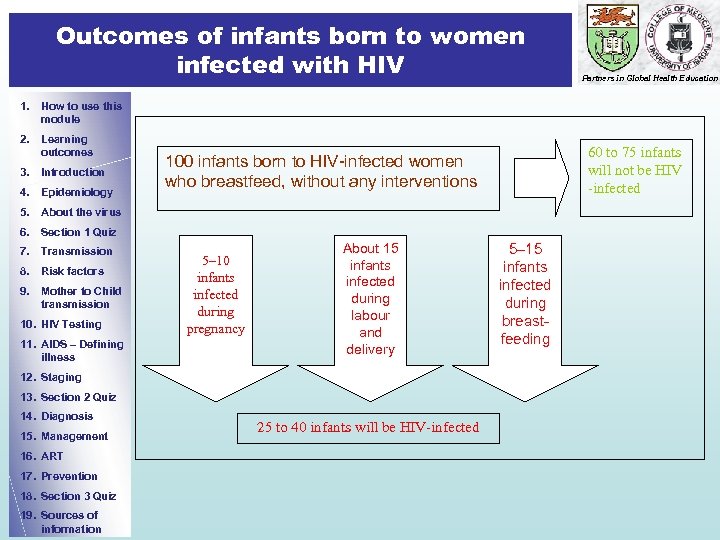 Outcomes of infants born to women infected with HIV Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 60 to 75 infants will not be HIV -infected 100 infants born to HIV-infected women who breastfeed, without any interventions 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 5– 10 infants infected during pregnancy About 15 infants infected during labour and delivery 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information 25 to 40 infants will be HIV-infected 5– 15 infants infected during breastfeeding
Outcomes of infants born to women infected with HIV Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 60 to 75 infants will not be HIV -infected 100 infants born to HIV-infected women who breastfeed, without any interventions 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 5– 10 infants infected during pregnancy About 15 infants infected during labour and delivery 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information 25 to 40 infants will be HIV-infected 5– 15 infants infected during breastfeeding
 HIV cannot be transmitted by: Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz • • • 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness • • 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • • Coughing or sneezing Being bitten by an insect Touching or hugging Holding a baby Going to a public bath/pool Using a public toilet Shaking hands Using telephones Working or going to school with a person who is HIV-infected Drinking water or preparing or eating food Sharing cups, glasses, plates, or other utensils
HIV cannot be transmitted by: Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz • • • 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness • • 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • • Coughing or sneezing Being bitten by an insect Touching or hugging Holding a baby Going to a public bath/pool Using a public toilet Shaking hands Using telephones Working or going to school with a person who is HIV-infected Drinking water or preparing or eating food Sharing cups, glasses, plates, or other utensils
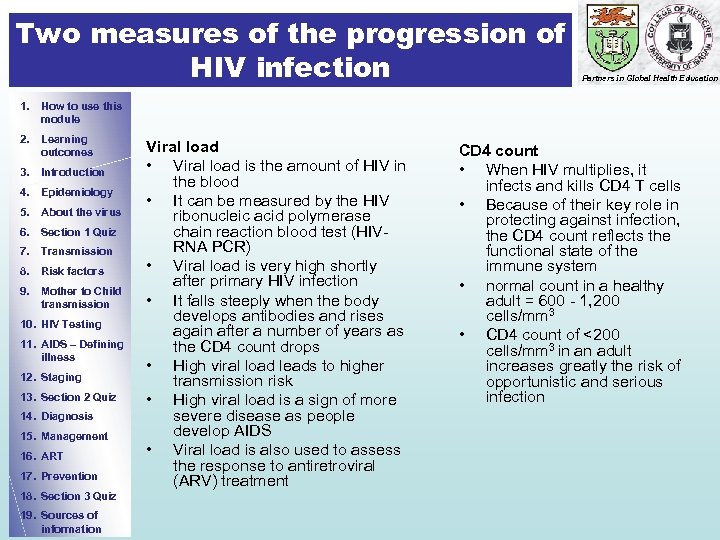 Two measures of the progression of HIV infection Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Viral load • Viral load is the amount of HIV in the blood • It can be measured by the HIV ribonucleic acid polymerase chain reaction blood test (HIVRNA PCR) • Viral load is very high shortly after primary HIV infection • It falls steeply when the body develops antibodies and rises again after a number of years as the CD 4 count drops • High viral load leads to higher transmission risk • High viral load is a sign of more severe disease as people develop AIDS • Viral load is also used to assess the response to antiretroviral (ARV) treatment CD 4 count • When HIV multiplies, it infects and kills CD 4 T cells • Because of their key role in protecting against infection, the CD 4 count reflects the functional state of the immune system • normal count in a healthy adult = 600 - 1, 200 cells/mm 3 • CD 4 count of <200 cells/mm 3 in an adult increases greatly the risk of opportunistic and serious infection
Two measures of the progression of HIV infection Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Viral load • Viral load is the amount of HIV in the blood • It can be measured by the HIV ribonucleic acid polymerase chain reaction blood test (HIVRNA PCR) • Viral load is very high shortly after primary HIV infection • It falls steeply when the body develops antibodies and rises again after a number of years as the CD 4 count drops • High viral load leads to higher transmission risk • High viral load is a sign of more severe disease as people develop AIDS • Viral load is also used to assess the response to antiretroviral (ARV) treatment CD 4 count • When HIV multiplies, it infects and kills CD 4 T cells • Because of their key role in protecting against infection, the CD 4 count reflects the functional state of the immune system • normal count in a healthy adult = 600 - 1, 200 cells/mm 3 • CD 4 count of <200 cells/mm 3 in an adult increases greatly the risk of opportunistic and serious infection
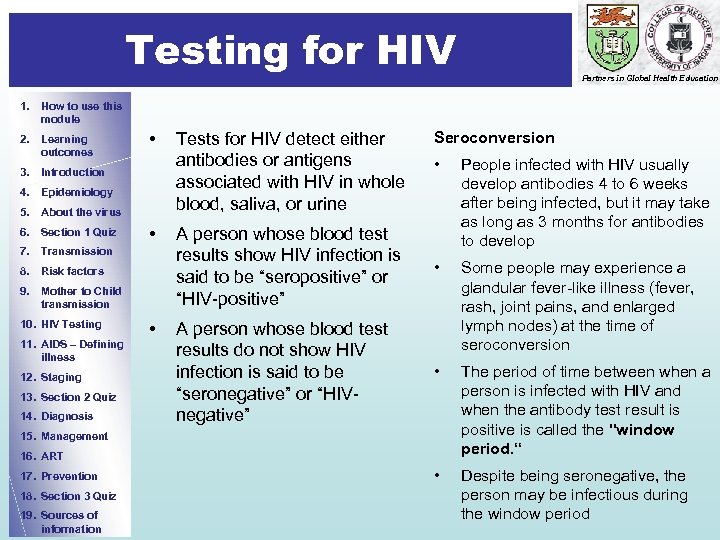 Testing for HIV Partners in Global Health Education 1. How to use this module 2. Learning outcomes • 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz • 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis • Tests for HIV detect either antibodies or antigens associated with HIV in whole blood, saliva, or urine Seroconversion • A person whose blood test results show HIV infection is said to be “seropositive” or “HIV-positive” People infected with HIV usually develop antibodies 4 to 6 weeks after being infected, but it may take as long as 3 months for antibodies to develop • A person whose blood test results do not show HIV infection is said to be “seronegative” or “HIVnegative” Some people may experience a glandular fever-like illness (fever, rash, joint pains, and enlarged lymph nodes) at the time of seroconversion • The period of time between when a person is infected with HIV and when the antibody test result is positive is called the "window period. “ • Despite being seronegative, the person may be infectious during the window period 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
Testing for HIV Partners in Global Health Education 1. How to use this module 2. Learning outcomes • 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz • 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis • Tests for HIV detect either antibodies or antigens associated with HIV in whole blood, saliva, or urine Seroconversion • A person whose blood test results show HIV infection is said to be “seropositive” or “HIV-positive” People infected with HIV usually develop antibodies 4 to 6 weeks after being infected, but it may take as long as 3 months for antibodies to develop • A person whose blood test results do not show HIV infection is said to be “seronegative” or “HIVnegative” Some people may experience a glandular fever-like illness (fever, rash, joint pains, and enlarged lymph nodes) at the time of seroconversion • The period of time between when a person is infected with HIV and when the antibody test result is positive is called the "window period. “ • Despite being seronegative, the person may be infectious during the window period 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
 Assessing the stage of disease Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction • There are several classification or staging systems in use • The US Centers for Disease Control and Prevention (CDC) categorizes HIV infection in adults on the basis of: 4. Epidemiology 5. About the virus – Associated clinical conditions (3 categories) 6. Section 1 Quiz 7. Transmission – CD 4+ T lymphocyte count (3 ranges) 8. Risk factors – This results in a matrix of nine mutually exclusive categories (next slide) 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Using this system – Any HIV-infected individual with a CD 4+ T cell count of <200/ml has AIDS (regardless of the presence of symptoms or opportunistic diseases), and – Any HIV-infected individual with an AIDS indicator (category C) condition has AIDS
Assessing the stage of disease Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction • There are several classification or staging systems in use • The US Centers for Disease Control and Prevention (CDC) categorizes HIV infection in adults on the basis of: 4. Epidemiology 5. About the virus – Associated clinical conditions (3 categories) 6. Section 1 Quiz 7. Transmission – CD 4+ T lymphocyte count (3 ranges) 8. Risk factors – This results in a matrix of nine mutually exclusive categories (next slide) 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Using this system – Any HIV-infected individual with a CD 4+ T cell count of <200/ml has AIDS (regardless of the presence of symptoms or opportunistic diseases), and – Any HIV-infected individual with an AIDS indicator (category C) condition has AIDS
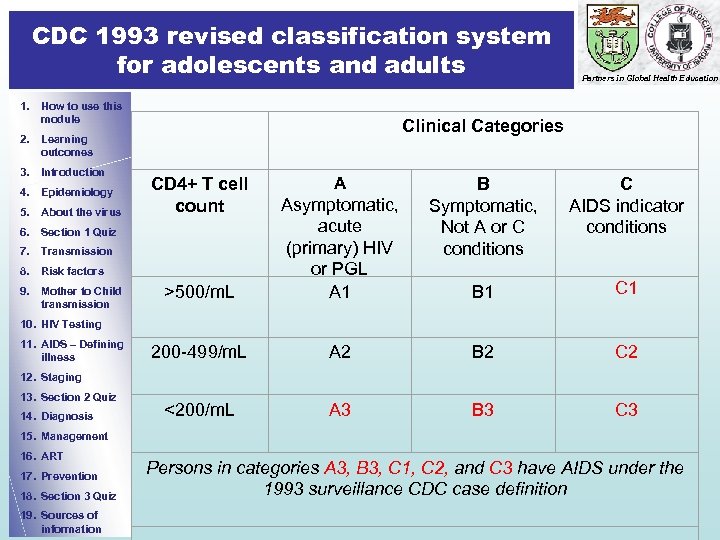 CDC 1993 revised classification system for adolescents and adults 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus CD 4+ T cell count Clinical Categories A B Symptomatic, Not A or C conditions C AIDS indicator conditions B 1 C 1 >500/m. L Asymptomatic, acute (primary) HIV or PGL A 1 200 -499/m. L A 2 B 2 C 2 <200/m. L A 3 B 3 C 3 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission Partners in Global Health Education 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Persons in categories A 3, B 3, C 1, C 2, and C 3 have AIDS under the 1993 surveillance CDC case definition
CDC 1993 revised classification system for adolescents and adults 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus CD 4+ T cell count Clinical Categories A B Symptomatic, Not A or C conditions C AIDS indicator conditions B 1 C 1 >500/m. L Asymptomatic, acute (primary) HIV or PGL A 1 200 -499/m. L A 2 B 2 C 2 <200/m. L A 3 B 3 C 3 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission Partners in Global Health Education 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Persons in categories A 3, B 3, C 1, C 2, and C 3 have AIDS under the 1993 surveillance CDC case definition
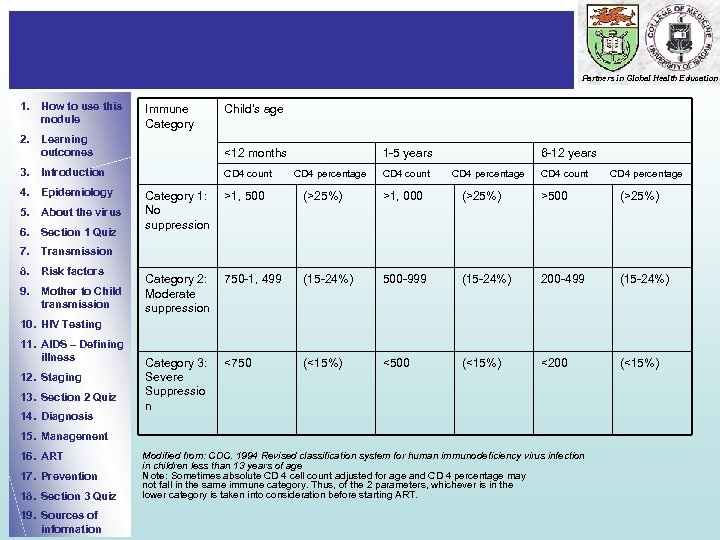 Partners in Global Health Education 1. How to use this module Immune Category Child’s age 2. Learning outcomes <12 months 1 -5 years 6 -12 years 3. Introduction CD 4 count CD 4 percentage Category 1: No suppression >1, 500 (>25%) >1, 000 (>25%) >500 (>25%) Category 2: Moderate suppression 750 -1, 499 (15 -24%) 500 -999 (15 -24%) 200 -499 (15 -24%) Category 3: Severe Suppressio n <750 (<15%) <500 (<15%) <200 (<15%) 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Modified from: CDC. 1994 Revised classification system for human immunodeficiency virus infection in children less than 13 years of age Note: Sometimes absolute CD 4 cell count adjusted for age and CD 4 percentage may not fall in the same immune category. Thus, of the 2 parameters, whichever is in the lower category is taken into consideration before starting ART.
Partners in Global Health Education 1. How to use this module Immune Category Child’s age 2. Learning outcomes <12 months 1 -5 years 6 -12 years 3. Introduction CD 4 count CD 4 percentage Category 1: No suppression >1, 500 (>25%) >1, 000 (>25%) >500 (>25%) Category 2: Moderate suppression 750 -1, 499 (15 -24%) 500 -999 (15 -24%) 200 -499 (15 -24%) Category 3: Severe Suppressio n <750 (<15%) <500 (<15%) <200 (<15%) 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Modified from: CDC. 1994 Revised classification system for human immunodeficiency virus infection in children less than 13 years of age Note: Sometimes absolute CD 4 cell count adjusted for age and CD 4 percentage may not fall in the same immune category. Thus, of the 2 parameters, whichever is in the lower category is taken into consideration before starting ART.
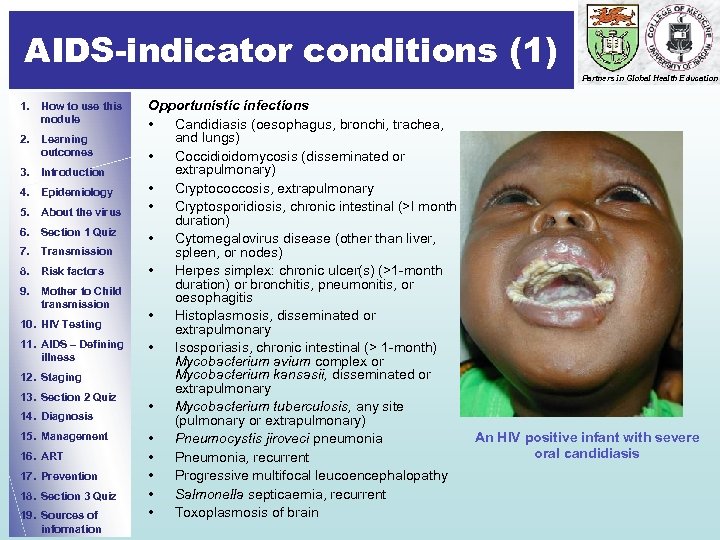 AIDS-indicator conditions (1) Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Opportunistic infections • Candidiasis (oesophagus, bronchi, trachea, and lungs) • Coccidioidomycosis (disseminated or extrapulmonary) • Cryptococcosis, extrapulmonary • Cryptosporidiosis, chronic intestinal (>I month duration) • Cytomegalovirus disease (other than liver, spleen, or nodes) • Herpes simplex: chronic ulcer(s) (>1 -month duration) or bronchitis, pneumonitis, or oesophagitis • Histoplasmosis, disseminated or extrapulmonary • Isosporiasis, chronic intestinal (> 1 -month) Mycobacterium avium complex or Mycobacterium kansasii, disseminated or extrapulmonary • Mycobacterium tuberculosis, any site (pulmonary or extrapulmonary) An HIV positive infant with severe • Pneumocystis jiroveci pneumonia oral candidiasis • Pneumonia, recurrent • Progressive multifocal leucoencephalopathy • Salmonella septicaemia, recurrent • Toxoplasmosis of brain
AIDS-indicator conditions (1) Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Opportunistic infections • Candidiasis (oesophagus, bronchi, trachea, and lungs) • Coccidioidomycosis (disseminated or extrapulmonary) • Cryptococcosis, extrapulmonary • Cryptosporidiosis, chronic intestinal (>I month duration) • Cytomegalovirus disease (other than liver, spleen, or nodes) • Herpes simplex: chronic ulcer(s) (>1 -month duration) or bronchitis, pneumonitis, or oesophagitis • Histoplasmosis, disseminated or extrapulmonary • Isosporiasis, chronic intestinal (> 1 -month) Mycobacterium avium complex or Mycobacterium kansasii, disseminated or extrapulmonary • Mycobacterium tuberculosis, any site (pulmonary or extrapulmonary) An HIV positive infant with severe • Pneumocystis jiroveci pneumonia oral candidiasis • Pneumonia, recurrent • Progressive multifocal leucoencephalopathy • Salmonella septicaemia, recurrent • Toxoplasmosis of brain
 AIDS-indicator conditions (2) Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors Neoplasia • Kaposi’s sarcoma • Lymphoma (Burkitt’s, immunoblastic, primary in brain) • Invasive cervical cancer 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information General • Wasting syndrome, HIVrelated • Encephalopathy, HIVrelated Kaposi’s sarcoma
AIDS-indicator conditions (2) Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors Neoplasia • Kaposi’s sarcoma • Lymphoma (Burkitt’s, immunoblastic, primary in brain) • Invasive cervical cancer 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information General • Wasting syndrome, HIVrelated • Encephalopathy, HIVrelated Kaposi’s sarcoma
 WHO staging system for HIV infection and disease in adults (1) Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus WHO identifes 4 clinical stages based on the performance level of the person and the associated illnesses: Clinical Stage II • Weight loss <10% of body weight • Minor mucocutaneous manifestations (seborrhoeic dermatitis, prurigo, fungal nail infections, recurrent oral ulcerations, angular cheilitis) • Herpes zoster within the last 5 years • Recurrent upper respiratory tract infections (e. g. , bacterial sinusitis) • And/or Performance Scale 2: symptomatic, normal activity 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention Clinical stage I • Asymptomatic • Generalised lymphadenopathy • Performance Scale 1: asymptomatic, normal activity 18. Section 3 Quiz 19. Sources of information Source: http: //www. who. int/docstore/hiv/scaling/anex 1. html
WHO staging system for HIV infection and disease in adults (1) Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus WHO identifes 4 clinical stages based on the performance level of the person and the associated illnesses: Clinical Stage II • Weight loss <10% of body weight • Minor mucocutaneous manifestations (seborrhoeic dermatitis, prurigo, fungal nail infections, recurrent oral ulcerations, angular cheilitis) • Herpes zoster within the last 5 years • Recurrent upper respiratory tract infections (e. g. , bacterial sinusitis) • And/or Performance Scale 2: symptomatic, normal activity 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention Clinical stage I • Asymptomatic • Generalised lymphadenopathy • Performance Scale 1: asymptomatic, normal activity 18. Section 3 Quiz 19. Sources of information Source: http: //www. who. int/docstore/hiv/scaling/anex 1. html
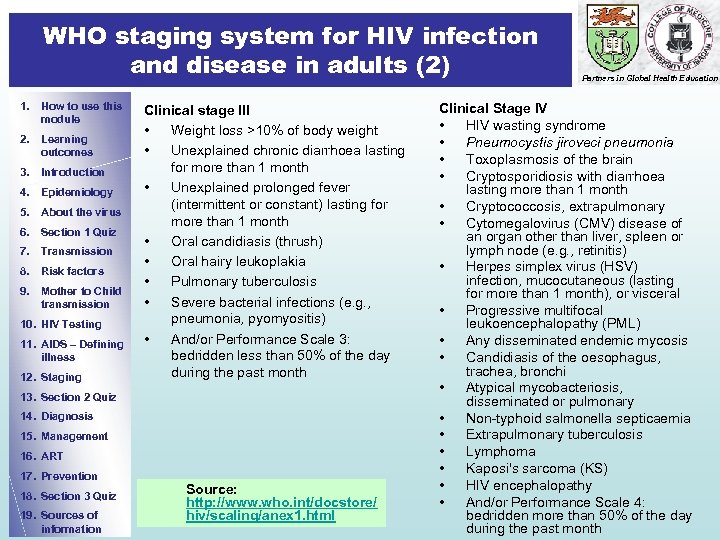 WHO staging system for HIV infection and disease in adults (2) 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging Clinical stage III • Weight loss >10% of body weight • Unexplained chronic diarrhoea lasting for more than 1 month • Unexplained prolonged fever (intermittent or constant) lasting for more than 1 month • Oral candidiasis (thrush) • Oral hairy leukoplakia • Pulmonary tuberculosis • Severe bacterial infections (e. g. , pneumonia, pyomyositis) • And/or Performance Scale 3: bedridden less than 50% of the day during the past month 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Source: http: //www. who. int/docstore/ hiv/scaling/anex 1. html Partners in Global Health Education Clinical Stage IV • HIV wasting syndrome • Pneumocystis jiroveci pneumonia • Toxoplasmosis of the brain • Cryptosporidiosis with diarrhoea lasting more than 1 month • Cryptococcosis, extrapulmonary • Cytomegalovirus (CMV) disease of an organ other than liver, spleen or lymph node (e. g. , retinitis) • Herpes simplex virus (HSV) infection, mucocutaneous (lasting for more than 1 month), or visceral • Progressive multifocal leukoencephalopathy (PML) • Any disseminated endemic mycosis • Candidiasis of the oesophagus, trachea, bronchi • Atypical mycobacteriosis, disseminated or pulmonary • Non-typhoid salmonella septicaemia • Extrapulmonary tuberculosis • Lymphoma • Kaposi's sarcoma (KS) • HIV encephalopathy • And/or Performance Scale 4: bedridden more than 50% of the day during the past month
WHO staging system for HIV infection and disease in adults (2) 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging Clinical stage III • Weight loss >10% of body weight • Unexplained chronic diarrhoea lasting for more than 1 month • Unexplained prolonged fever (intermittent or constant) lasting for more than 1 month • Oral candidiasis (thrush) • Oral hairy leukoplakia • Pulmonary tuberculosis • Severe bacterial infections (e. g. , pneumonia, pyomyositis) • And/or Performance Scale 3: bedridden less than 50% of the day during the past month 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Source: http: //www. who. int/docstore/ hiv/scaling/anex 1. html Partners in Global Health Education Clinical Stage IV • HIV wasting syndrome • Pneumocystis jiroveci pneumonia • Toxoplasmosis of the brain • Cryptosporidiosis with diarrhoea lasting more than 1 month • Cryptococcosis, extrapulmonary • Cytomegalovirus (CMV) disease of an organ other than liver, spleen or lymph node (e. g. , retinitis) • Herpes simplex virus (HSV) infection, mucocutaneous (lasting for more than 1 month), or visceral • Progressive multifocal leukoencephalopathy (PML) • Any disseminated endemic mycosis • Candidiasis of the oesophagus, trachea, bronchi • Atypical mycobacteriosis, disseminated or pulmonary • Non-typhoid salmonella septicaemia • Extrapulmonary tuberculosis • Lymphoma • Kaposi's sarcoma (KS) • HIV encephalopathy • And/or Performance Scale 4: bedridden more than 50% of the day during the past month
 WHO staging system for HIV infection and disease in children 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education Clinical stage I • Asymptomatic • Generalised lymphadenopathy Clinical stage II • Chronic diarrhoea lasting more than 30 days in the absence of known etiology • Severe persistent or recurrent candidiasis outside the neonatal period • Weight loss or failure to thrive in the absence of known etiology • Persistent fever lasting longer than 30 days in the absence of known etiology • Recurrent severe bacterial infections other than septicaemia or meningitis (e. g. , osteomyelitis, bacterial (non-TB) pneumonia, abscesses) Clinical Stage III • AIDS-defining opportunistic infections • Severe failure to thrive (wasting) in the absence of known etiology • Progressive encephalopathy • Malignancy • Recurrent septicaemia or meningitis Source: Testing for HIV may be indicated in malnourished children in whom a specific cause can not be identified http: //www. who. int/hiv/pub/guidelines/clinicalstaging. pdf
WHO staging system for HIV infection and disease in children 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Partners in Global Health Education Clinical stage I • Asymptomatic • Generalised lymphadenopathy Clinical stage II • Chronic diarrhoea lasting more than 30 days in the absence of known etiology • Severe persistent or recurrent candidiasis outside the neonatal period • Weight loss or failure to thrive in the absence of known etiology • Persistent fever lasting longer than 30 days in the absence of known etiology • Recurrent severe bacterial infections other than septicaemia or meningitis (e. g. , osteomyelitis, bacterial (non-TB) pneumonia, abscesses) Clinical Stage III • AIDS-defining opportunistic infections • Severe failure to thrive (wasting) in the absence of known etiology • Progressive encephalopathy • Malignancy • Recurrent septicaemia or meningitis Source: Testing for HIV may be indicated in malnourished children in whom a specific cause can not be identified http: //www. who. int/hiv/pub/guidelines/clinicalstaging. pdf
 The 3 phases of HIV infection Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology The course of HIV infection can be best understood in terms of interplay between HIV and the immune system. Three phases can be recognized: Early, acute Middle chronic Final crisis 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Characteristic viral load (HIV RNA) and CD 4 count over time
The 3 phases of HIV infection Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology The course of HIV infection can be best understood in terms of interplay between HIV and the immune system. Three phases can be recognized: Early, acute Middle chronic Final crisis 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Characteristic viral load (HIV RNA) and CD 4 count over time
 Phases 1, 2 and 3 Partners in Global Health Education 1. How to use this module 1. The early, acute phase 2. Learning outcomes • 3. Introduction 4. Epidemiology 5. About the virus • 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission • • 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Initial response of an immunocompetent adult to HIV infection High level of virus production and viraemia widespread viral seeding of the lymphoid tissues Approximately 100 billion new viral particles are produced every day 1 -2 billion CD 4+ Tcells die each day Clinically, this stage is characterized by infectious mononucleosis-like features of sore throat, myalgias, fever, weight loss, and fatigue all of which are selflimiting 2. The middle, chronic phase • • • Relative containment of the virus and clinical latency Virus replication continues for several years, predominantly in the lymphoid tissues Immune system largely intact Clinically, patients are either asymptomatic or develop persistent generalized lymphadenopathy (PGL). Many patients have herpes zoster, oral thrush or thrombocytopaenia 3. The final, crisis phase • • breakdown of host defense CD 4 count usually < 200 cells/mm 3 sudden and rapid viraemia clinical disease Clinically, the patient presents with marked weight loss, chronic diarrhoea, and fever lasting more than 1 month Opportunistic infections (OI) occur The clinical picture of AIDS will depend on the type of OI or cancer
Phases 1, 2 and 3 Partners in Global Health Education 1. How to use this module 1. The early, acute phase 2. Learning outcomes • 3. Introduction 4. Epidemiology 5. About the virus • 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission • • 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • Initial response of an immunocompetent adult to HIV infection High level of virus production and viraemia widespread viral seeding of the lymphoid tissues Approximately 100 billion new viral particles are produced every day 1 -2 billion CD 4+ Tcells die each day Clinically, this stage is characterized by infectious mononucleosis-like features of sore throat, myalgias, fever, weight loss, and fatigue all of which are selflimiting 2. The middle, chronic phase • • • Relative containment of the virus and clinical latency Virus replication continues for several years, predominantly in the lymphoid tissues Immune system largely intact Clinically, patients are either asymptomatic or develop persistent generalized lymphadenopathy (PGL). Many patients have herpes zoster, oral thrush or thrombocytopaenia 3. The final, crisis phase • • breakdown of host defense CD 4 count usually < 200 cells/mm 3 sudden and rapid viraemia clinical disease Clinically, the patient presents with marked weight loss, chronic diarrhoea, and fever lasting more than 1 month Opportunistic infections (OI) occur The clinical picture of AIDS will depend on the type of OI or cancer
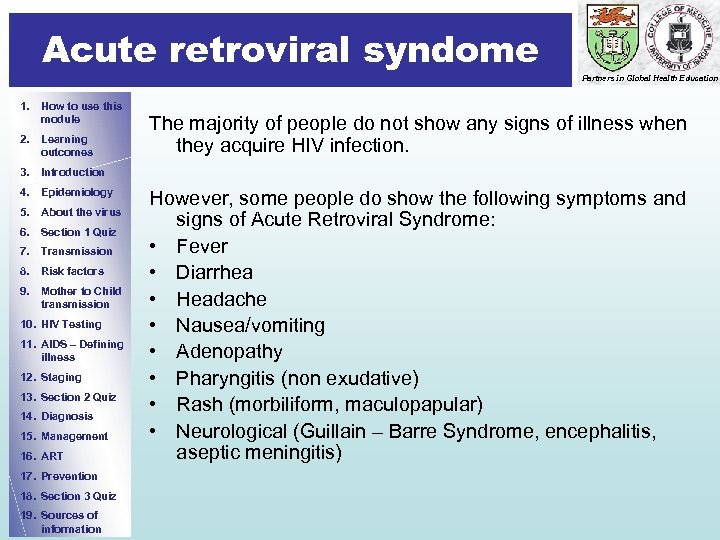 Acute retroviral syndome Partners in Global Health Education 1. How to use this module 2. Learning outcomes The majority of people do not show any signs of illness when they acquire HIV infection. 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information However, some people do show the following symptoms and signs of Acute Retroviral Syndrome: • Fever • Diarrhea • Headache • Nausea/vomiting • Adenopathy • Pharyngitis (non exudative) • Rash (morbiliform, maculopapular) • Neurological (Guillain – Barre Syndrome, encephalitis, aseptic meningitis)
Acute retroviral syndome Partners in Global Health Education 1. How to use this module 2. Learning outcomes The majority of people do not show any signs of illness when they acquire HIV infection. 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information However, some people do show the following symptoms and signs of Acute Retroviral Syndrome: • Fever • Diarrhea • Headache • Nausea/vomiting • Adenopathy • Pharyngitis (non exudative) • Rash (morbiliform, maculopapular) • Neurological (Guillain – Barre Syndrome, encephalitis, aseptic meningitis)
 Clinical phase 2 - Mother and child Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information This HIV-positive mother was asymptomatic apart from shingles. The child was also seropositive and had just recovered from pneumonia (below)
Clinical phase 2 - Mother and child Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information This HIV-positive mother was asymptomatic apart from shingles. The child was also seropositive and had just recovered from pneumonia (below)
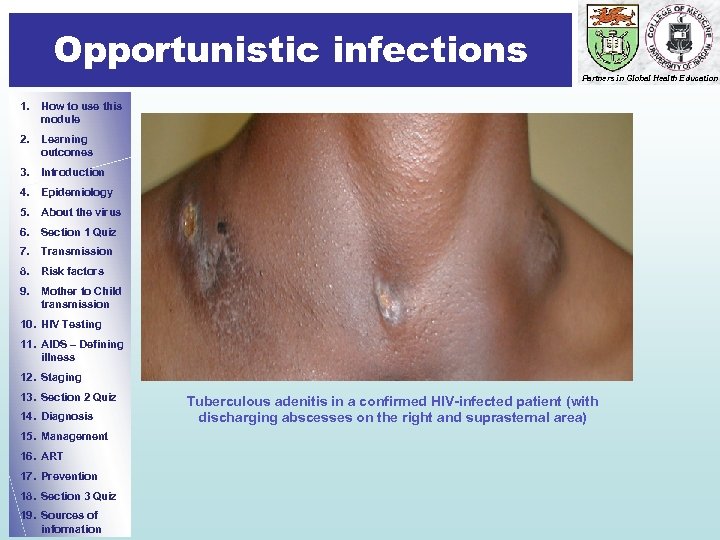 Opportunistic infections Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Tuberculous adenitis in a confirmed HIV-infected patient (with discharging abscesses on the right and suprasternal area)
Opportunistic infections Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Tuberculous adenitis in a confirmed HIV-infected patient (with discharging abscesses on the right and suprasternal area)
 HIV-associated malignancy Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Kaposi’s sarcoma The same patient after a course of cytotoxics
HIV-associated malignancy Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Kaposi’s sarcoma The same patient after a course of cytotoxics
 End of Section 2 Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Well done! This is the end of the second section. 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We suggest that you proceed to answer question 2 to assess your learning further. Do remember to write your answers on the mark sheet before looking at the right answer!
End of Section 2 Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology Well done! This is the end of the second section. 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We suggest that you proceed to answer question 2 to assess your learning further. Do remember to write your answers on the mark sheet before looking at the right answer!
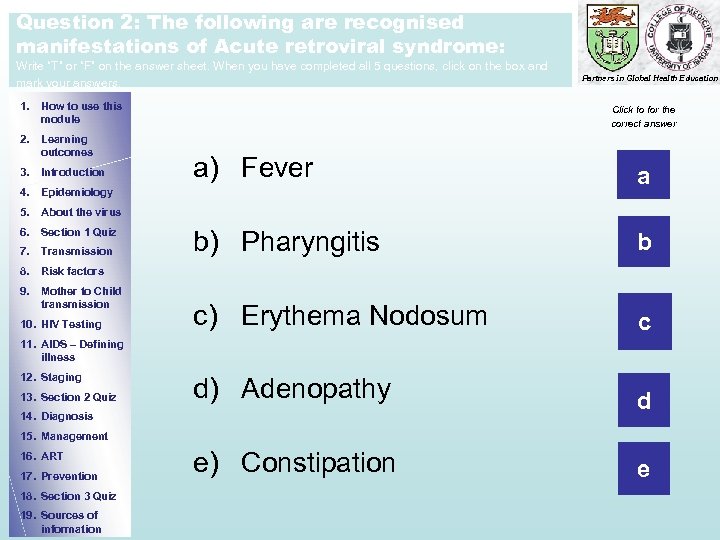 Question 2: The following are recognised manifestations of Acute retroviral syndrome: Write “T” or “F” on the answer sheet. When you have completed all 5 questions, click on the box and mark your answers. 1. How to use this module 2. Learning outcomes 3. Introduction Partners in Global Health Education Click to for the correct answer a) Fever a b) Pharyngitis b c) Erythema Nodosum c d) Adenopathy d e) Constipation e 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
Question 2: The following are recognised manifestations of Acute retroviral syndrome: Write “T” or “F” on the answer sheet. When you have completed all 5 questions, click on the box and mark your answers. 1. How to use this module 2. Learning outcomes 3. Introduction Partners in Global Health Education Click to for the correct answer a) Fever a b) Pharyngitis b c) Erythema Nodosum c d) Adenopathy d e) Constipation e 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
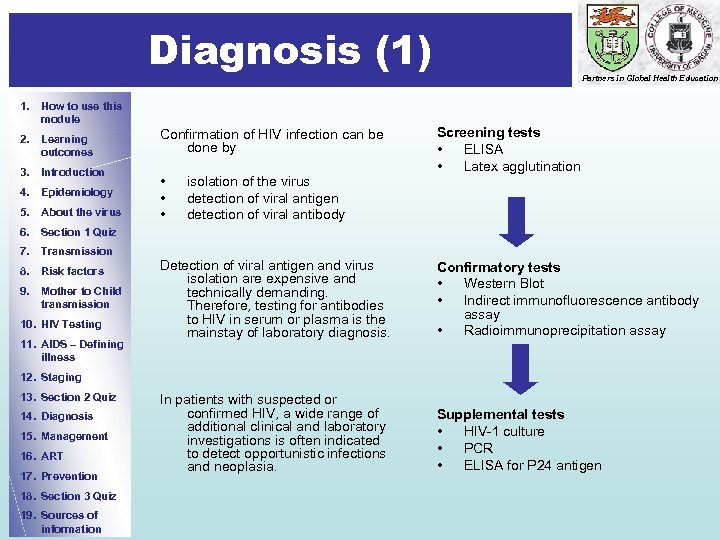 Diagnosis (1) 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus Confirmation of HIV infection can be done by • • • isolation of the virus detection of viral antigen detection of viral antibody Partners in Global Health Education Screening tests • ELISA • Latex agglutination 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness Detection of viral antigen and virus isolation are expensive and technically demanding. Therefore, testing for antibodies to HIV in serum or plasma is the mainstay of laboratory diagnosis. Confirmatory tests • Western Blot • Indirect immunofluorescence antibody assay • Radioimmunoprecipitation assay In patients with suspected or confirmed HIV, a wide range of additional clinical and laboratory investigations is often indicated to detect opportunistic infections and neoplasia. Supplemental tests • HIV-1 culture • PCR • ELISA for P 24 antigen 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
Diagnosis (1) 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus Confirmation of HIV infection can be done by • • • isolation of the virus detection of viral antigen detection of viral antibody Partners in Global Health Education Screening tests • ELISA • Latex agglutination 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness Detection of viral antigen and virus isolation are expensive and technically demanding. Therefore, testing for antibodies to HIV in serum or plasma is the mainstay of laboratory diagnosis. Confirmatory tests • Western Blot • Indirect immunofluorescence antibody assay • Radioimmunoprecipitation assay In patients with suspected or confirmed HIV, a wide range of additional clinical and laboratory investigations is often indicated to detect opportunistic infections and neoplasia. Supplemental tests • HIV-1 culture • PCR • ELISA for P 24 antigen 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information
 Diagnosis (2) 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Where diagnostic facilities are limited, AIDS can be diagnosed using the WHO Clinical Case Definition in adults : AIDS defined by the existence of • AT LEAST 2 major signs associated with • AT LEAST 1 minor sign • in the absence of known causes of immunosuppression Partners in Global Health Education Major signs • Weight loss >10% body weight • Chronic diarrhoea (lasting >1 month) • Fever intermittent or constant (lasting >1 month) Minor signs • Persistent cough (>1 month) • Generalized pruritic dermatitis • Recurrent herpes zoster • Oropharyngeal candidiasis • Chronic progressive and disseminated herpes virus infection • Generalized lymphadenopathy
Diagnosis (2) 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Where diagnostic facilities are limited, AIDS can be diagnosed using the WHO Clinical Case Definition in adults : AIDS defined by the existence of • AT LEAST 2 major signs associated with • AT LEAST 1 minor sign • in the absence of known causes of immunosuppression Partners in Global Health Education Major signs • Weight loss >10% body weight • Chronic diarrhoea (lasting >1 month) • Fever intermittent or constant (lasting >1 month) Minor signs • Persistent cough (>1 month) • Generalized pruritic dermatitis • Recurrent herpes zoster • Oropharyngeal candidiasis • Chronic progressive and disseminated herpes virus infection • Generalized lymphadenopathy
 Diagnosing HIV infection and AIDS in children 1. How to use this module 2. Learning outcomes < 18 months • 3. Introduction 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission seropositive (test again after 18 months) or born to positive mother with positive HIV culture, DNA PCR 4. Epidemiology 5. About the virus Partners in Global Health Education Or Meets clinical criteria for AIDS And/or CD 4 percentage < 20% >18 months • positive antibody tests Or Meets clinical criteria for AIDS. 10. HIV Testing 11. AIDS – Defining illness NB 12. Staging • 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • • Testing is performed in the immediate newborn period, at 1 -2 months and 3 -6 months of age. False negative are sometimes observed in the newborn period but the sensitivity of the test after 1 month is about 99%. If the child is being breastfed the test should be performed 3 months after cessation of breastfeeding). The diagnosis of HIV amongst children begins with the diagnosis in the mother In infected women, the maternal HIV antibody is passively transmitted across the placenta to the fetus during pregnancy. A single positive HIV-I DNA PCR test result should be interpreted with caution. Any infant with a positive result should be retested immediately.
Diagnosing HIV infection and AIDS in children 1. How to use this module 2. Learning outcomes < 18 months • 3. Introduction 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission seropositive (test again after 18 months) or born to positive mother with positive HIV culture, DNA PCR 4. Epidemiology 5. About the virus Partners in Global Health Education Or Meets clinical criteria for AIDS And/or CD 4 percentage < 20% >18 months • positive antibody tests Or Meets clinical criteria for AIDS. 10. HIV Testing 11. AIDS – Defining illness NB 12. Staging • 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • • Testing is performed in the immediate newborn period, at 1 -2 months and 3 -6 months of age. False negative are sometimes observed in the newborn period but the sensitivity of the test after 1 month is about 99%. If the child is being breastfed the test should be performed 3 months after cessation of breastfeeding). The diagnosis of HIV amongst children begins with the diagnosis in the mother In infected women, the maternal HIV antibody is passively transmitted across the placenta to the fetus during pregnancy. A single positive HIV-I DNA PCR test result should be interpreted with caution. Any infant with a positive result should be retested immediately.
 Clinical management Partners in Global Health Education 1. How to use this module 2. Learning outcomes Goals of treatment • – Prolong survival – Prevent disease progression – Minimize drug toxicity 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz • 8. Risk factors 9. Mother to Child transmission 10. HIV Testing • 13. Section 2 Quiz 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Immunological – Preserve immune function (CD 4 cell count in normal range) 12. Staging 14. Diagnosis Virological – Maximal and durable suppression of viral load for as long as possible to below detectable levels (currently defined as <50 copies/ml) 7. Transmission 11. AIDS – Defining illness Clinical • Public health – Reduce HIV transmission – Preserve future treatment options Management in practice Caring for people with HIV infection is often difficult for a number of reasons: • HIV infection is incurable • the infection is associated with stigmatization and discrimination • infected individuals need to be counselled to ensure they do not transmit the disease to others • diagnosing HIV-related diseases may be problematic, as they often present with atypical clinical manifestations and may occur simultaneously, even in the same organs • unavailability of treatment for some HIV-related diseases • patients often develop serious adverse effects to drugs • the number of healthcare workers with experience in counselling and managing people with HIV is limited, particularly in Africa
Clinical management Partners in Global Health Education 1. How to use this module 2. Learning outcomes Goals of treatment • – Prolong survival – Prevent disease progression – Minimize drug toxicity 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz • 8. Risk factors 9. Mother to Child transmission 10. HIV Testing • 13. Section 2 Quiz 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Immunological – Preserve immune function (CD 4 cell count in normal range) 12. Staging 14. Diagnosis Virological – Maximal and durable suppression of viral load for as long as possible to below detectable levels (currently defined as <50 copies/ml) 7. Transmission 11. AIDS – Defining illness Clinical • Public health – Reduce HIV transmission – Preserve future treatment options Management in practice Caring for people with HIV infection is often difficult for a number of reasons: • HIV infection is incurable • the infection is associated with stigmatization and discrimination • infected individuals need to be counselled to ensure they do not transmit the disease to others • diagnosing HIV-related diseases may be problematic, as they often present with atypical clinical manifestations and may occur simultaneously, even in the same organs • unavailability of treatment for some HIV-related diseases • patients often develop serious adverse effects to drugs • the number of healthcare workers with experience in counselling and managing people with HIV is limited, particularly in Africa
 Antiretroviral drug treatment Partners in Global Health Education 1. How to use this module 2. Learning outcomes • 3. Introduction 4. Epidemiology 5. About the virus • Drugs from different classes are used in combination to prevent emergence of resistance to single agents Critical questions are: • – – 6. Section 1 Quiz 7. Transmission – When to initiate therapy? 8. Risk factors 9. Mother to Child transmission – What is the optimal initial therapy? 10. HIV Testing – When to change therapy? 11. AIDS – Defining illness – What are the optimal subsequent therapies? 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Benefits of early therapy – Control of viral replication – – • easier Prevention of immune system compromise Lower risk of resistance with complete viral suppression Possible decreased risk of HIV transmission Avoid irreversible immune system depletion Risks of early therapy – Drug-related reduction in quality of life – Greater cumulative drugrelated adverse events – Earlier development of drug resistance – Limitation of future antiretroviral treatment options
Antiretroviral drug treatment Partners in Global Health Education 1. How to use this module 2. Learning outcomes • 3. Introduction 4. Epidemiology 5. About the virus • Drugs from different classes are used in combination to prevent emergence of resistance to single agents Critical questions are: • – – 6. Section 1 Quiz 7. Transmission – When to initiate therapy? 8. Risk factors 9. Mother to Child transmission – What is the optimal initial therapy? 10. HIV Testing – When to change therapy? 11. AIDS – Defining illness – What are the optimal subsequent therapies? 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Benefits of early therapy – Control of viral replication – – • easier Prevention of immune system compromise Lower risk of resistance with complete viral suppression Possible decreased risk of HIV transmission Avoid irreversible immune system depletion Risks of early therapy – Drug-related reduction in quality of life – Greater cumulative drugrelated adverse events – Earlier development of drug resistance – Limitation of future antiretroviral treatment options
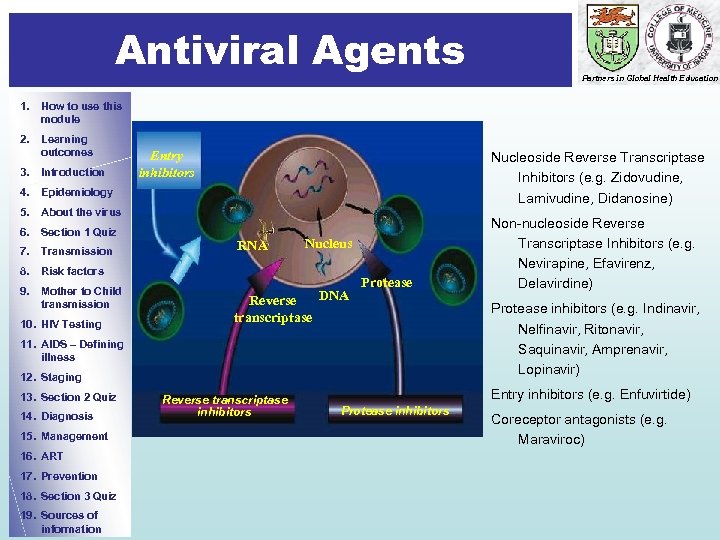 Antiviral Agents Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction Entry inhibitors Nucleoside Reverse Transcriptase Inhibitors (e. g. Zidovudine, Lamivudine, Didanosine) 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission RNA Nucleus 8. Risk factors 9. Mother to Child transmission 10. HIV Testing Reverse transcriptase DNA Protease 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Reverse transcriptase inhibitors Non-nucleoside Reverse Transcriptase Inhibitors (e. g. Nevirapine, Efavirenz, Delavirdine) Protease inhibitors (e. g. Indinavir, Nelfinavir, Ritonavir, Saquinavir, Amprenavir, Lopinavir) Entry inhibitors (e. g. Enfuvirtide) Protease inhibitors Coreceptor antagonists (e. g. Maraviroc)
Antiviral Agents Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction Entry inhibitors Nucleoside Reverse Transcriptase Inhibitors (e. g. Zidovudine, Lamivudine, Didanosine) 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission RNA Nucleus 8. Risk factors 9. Mother to Child transmission 10. HIV Testing Reverse transcriptase DNA Protease 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Reverse transcriptase inhibitors Non-nucleoside Reverse Transcriptase Inhibitors (e. g. Nevirapine, Efavirenz, Delavirdine) Protease inhibitors (e. g. Indinavir, Nelfinavir, Ritonavir, Saquinavir, Amprenavir, Lopinavir) Entry inhibitors (e. g. Enfuvirtide) Protease inhibitors Coreceptor antagonists (e. g. Maraviroc)
 Highly active antiretroviral therapy (HAART) Partners in Global Health Education 1. How to use this module Guidelines for starting HAART Criteria for treatment failure 2. Learning outcomes • • 3. Introduction • 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors • • 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness • Measure plasma HIV RNA levels – Immediately prior to initiation of Rx – At 2 -8 weeks after Rx – Repeat every 3 -4 months while being on therapy – In case of a clinical event or a significant decline in CD 4+ T cells • CD 4+ T cell count at the time of diagnosis and generally every 3 -6 months thereafter 13. Section 2 Quiz 14. Diagnosis 15. Management 17. Prevention 18. Section 3 Quiz 19. Sources of information • Monitoring HAART 12. Staging 16. ART All patients with WHO stage 3 and 4 irrespective of CD 4+ cell count CD 4+ count <350/mm 3 irrespective of HIV RNA level CD 4+ cell count between 200 -350/mm 3 and HIV RNA level >20, 000 copies/m. L CD 4+ cell count >350/mm 3 and HIV RNA level >55, 000 copies/m. L HIV+ child aged < 12 months HIV+ children over 1 year old who are symptomatic or immunosuppressed • Clinical – Onset of new or recurrence of opportunistic infections – Onset or recurrence of WHO stage III-defining condition Immunological – Return of CD 4 count to pretherapy level – 30% fall CD 4 count from peak level during therapy – Failure to achieve CD 4 cell count increase of 50 -100 cells per year Virological – Viral load not suppressed to undetectable levels after 4 -6 months of ART – A persistent increase in viral load following a period of adequate suppression
Highly active antiretroviral therapy (HAART) Partners in Global Health Education 1. How to use this module Guidelines for starting HAART Criteria for treatment failure 2. Learning outcomes • • 3. Introduction • 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors • • 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness • Measure plasma HIV RNA levels – Immediately prior to initiation of Rx – At 2 -8 weeks after Rx – Repeat every 3 -4 months while being on therapy – In case of a clinical event or a significant decline in CD 4+ T cells • CD 4+ T cell count at the time of diagnosis and generally every 3 -6 months thereafter 13. Section 2 Quiz 14. Diagnosis 15. Management 17. Prevention 18. Section 3 Quiz 19. Sources of information • Monitoring HAART 12. Staging 16. ART All patients with WHO stage 3 and 4 irrespective of CD 4+ cell count CD 4+ count <350/mm 3 irrespective of HIV RNA level CD 4+ cell count between 200 -350/mm 3 and HIV RNA level >20, 000 copies/m. L CD 4+ cell count >350/mm 3 and HIV RNA level >55, 000 copies/m. L HIV+ child aged < 12 months HIV+ children over 1 year old who are symptomatic or immunosuppressed • Clinical – Onset of new or recurrence of opportunistic infections – Onset or recurrence of WHO stage III-defining condition Immunological – Return of CD 4 count to pretherapy level – 30% fall CD 4 count from peak level during therapy – Failure to achieve CD 4 cell count increase of 50 -100 cells per year Virological – Viral load not suppressed to undetectable levels after 4 -6 months of ART – A persistent increase in viral load following a period of adequate suppression
 Highly active antiretroviral therapy (HAART) in special circumstances 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Guidelines for starting HAART for HIV/TB co-infection • All patients with active TB irrespective of HIV RNA level or CD 4+ cell count • TB treatment should be commenced first and ART commenced subsequently, as soon as possible and within the first 8 weeks of starting TB treatment. • The recommended 1 st line ART regimen in patients on TB treatment is AZT+3 TC+EFV or TDF+(3 TC or FTC)+ EFV. For those unable to tolerate or have contraindications to an EFV-based regimen, AZT+3 TC+NVP or TDF+3 TC or FTC+NVP or a triple NRTI regimen are recommended Guidelines for starting HAART for HIV/HBV co-infection • In those who require treatment for HBV infection, ART should be initiated irrespective of CD 4 cell count or WHO clinical stage. • In those eligible for treatment, 1 st line regimen should include TDF and 3 TC or FTC • In those failing treatment, 2 nd and subsequent ART regimens should include TDF+3 TC or FTC, both should be continued in the 2 nd line regimen for anti. HBV activity & to reduce the risk of hepatic flares, irrespective of the 2 nd line regimen Partners in Global Health Education ART for pregnant women • • Treat all pregnant women with CD 4 count <350, irrespective of WHO clinical stage Treat all pregnant with WHO stage 3 and 4, irrespective of CD 4 count One of the following regimens should be used for ART naïve pregnant women initiating ART – AZT +3 TC+EFVO (preferred) – AZT +3 TC+NVP (preferred) – TDF+(3 TC or FTC)+EFV – TDF+(3 TC or FTC)+NP It is recommended that an EFVbased 1 st-line regimen should not be initiated during the first trimester of pregnancy
Highly active antiretroviral therapy (HAART) in special circumstances 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Guidelines for starting HAART for HIV/TB co-infection • All patients with active TB irrespective of HIV RNA level or CD 4+ cell count • TB treatment should be commenced first and ART commenced subsequently, as soon as possible and within the first 8 weeks of starting TB treatment. • The recommended 1 st line ART regimen in patients on TB treatment is AZT+3 TC+EFV or TDF+(3 TC or FTC)+ EFV. For those unable to tolerate or have contraindications to an EFV-based regimen, AZT+3 TC+NVP or TDF+3 TC or FTC+NVP or a triple NRTI regimen are recommended Guidelines for starting HAART for HIV/HBV co-infection • In those who require treatment for HBV infection, ART should be initiated irrespective of CD 4 cell count or WHO clinical stage. • In those eligible for treatment, 1 st line regimen should include TDF and 3 TC or FTC • In those failing treatment, 2 nd and subsequent ART regimens should include TDF+3 TC or FTC, both should be continued in the 2 nd line regimen for anti. HBV activity & to reduce the risk of hepatic flares, irrespective of the 2 nd line regimen Partners in Global Health Education ART for pregnant women • • Treat all pregnant women with CD 4 count <350, irrespective of WHO clinical stage Treat all pregnant with WHO stage 3 and 4, irrespective of CD 4 count One of the following regimens should be used for ART naïve pregnant women initiating ART – AZT +3 TC+EFVO (preferred) – AZT +3 TC+NVP (preferred) – TDF+(3 TC or FTC)+EFV – TDF+(3 TC or FTC)+NP It is recommended that an EFVbased 1 st-line regimen should not be initiated during the first trimester of pregnancy
 What to start Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • It is recommended that one of the following regimens is used to initiate ART in ART-naïve individuals – – AZT+3 TC+EFV AZT+3 TC+NVP TDF+(3 TC or FTC)+EFV TDF+(3 TC or FTC)+NVP • Fixed dose combinations or co-packaged formulations are recommended wherever possible.
What to start Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • It is recommended that one of the following regimens is used to initiate ART in ART-naïve individuals – – AZT+3 TC+EFV AZT+3 TC+NVP TDF+(3 TC or FTC)+EFV TDF+(3 TC or FTC)+NVP • Fixed dose combinations or co-packaged formulations are recommended wherever possible.
 Prevention and Control (1) Prevention Partners in Global Health Education 1. How to use this module • 2. Learning outcomes 3. Introduction 4. Epidemiology • 5. About the virus 6. Section 1 Quiz • 7. Transmission 8. Risk factors 9. Mother to Child transmission • 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • In the absence of a curative treatment or vaccine, prevention of HIV transmission is essential to controlling the epidemic Effective education about HIV transmission and ways to prevent its spread has been considered a “social vaccine” Successful prevention requires collaboration between the health care sector, civil society, many communitybased groups and faith-based organizations. Within the healthcare sector, clinicians, social workers, health education specialists, mental health specialists and patients must work together In all settings, especially those that are resource-poor, selection of the most cost-effective interventions is imperative because allocation of resources to one intervention may prevent implementation of other interventions
Prevention and Control (1) Prevention Partners in Global Health Education 1. How to use this module • 2. Learning outcomes 3. Introduction 4. Epidemiology • 5. About the virus 6. Section 1 Quiz • 7. Transmission 8. Risk factors 9. Mother to Child transmission • 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • In the absence of a curative treatment or vaccine, prevention of HIV transmission is essential to controlling the epidemic Effective education about HIV transmission and ways to prevent its spread has been considered a “social vaccine” Successful prevention requires collaboration between the health care sector, civil society, many communitybased groups and faith-based organizations. Within the healthcare sector, clinicians, social workers, health education specialists, mental health specialists and patients must work together In all settings, especially those that are resource-poor, selection of the most cost-effective interventions is imperative because allocation of resources to one intervention may prevent implementation of other interventions
 Prevention and Control (2) Prevention Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Since sexual contact accounts for most of HIV transmission globally, control measures directed against the spread of this infection must address squarely the issue of sexual promiscuity or excessive sexual activity Advice includes restriction to one partner only, if married. If unmarried, they should abstain or restrict themselves to the person they know best Condom use should be emphasized to those who cannot abstain People must be advised to screen themselves periodically if they expose themselves to more than one partner
Prevention and Control (2) Prevention Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information Since sexual contact accounts for most of HIV transmission globally, control measures directed against the spread of this infection must address squarely the issue of sexual promiscuity or excessive sexual activity Advice includes restriction to one partner only, if married. If unmarried, they should abstain or restrict themselves to the person they know best Condom use should be emphasized to those who cannot abstain People must be advised to screen themselves periodically if they expose themselves to more than one partner
 Prevention and Control (3) Prevention Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction Some key elements of AIDS prevention • 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing • • 11. AIDS – Defining illness • 12. Staging • 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • • Provide early diagnosis and treatment of STIs Make HIV testing and counselling widely available Provide suitable counselling for women who are HIV-negative Prevent unintended pregnancies among HIV positive women Testing and counselling of pregnant women ARV prophylaxis to mother –child pairs Modification of infant feeding practices to reduce transmission via breastfeeding Safe blood transfusion practices Use of sterile instruments including like needles and syringes
Prevention and Control (3) Prevention Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction Some key elements of AIDS prevention • 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing • • 11. AIDS – Defining illness • 12. Staging • 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information • • Provide early diagnosis and treatment of STIs Make HIV testing and counselling widely available Provide suitable counselling for women who are HIV-negative Prevent unintended pregnancies among HIV positive women Testing and counselling of pregnant women ARV prophylaxis to mother –child pairs Modification of infant feeding practices to reduce transmission via breastfeeding Safe blood transfusion practices Use of sterile instruments including like needles and syringes
 End of Section 3 Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology You have come a long way! This is the last of the sections. 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We suggest that you proceed to answer question 3 to assess your learning. Do remember to write your answers on the mark sheet before looking at the right answer!
End of Section 3 Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology You have come a long way! This is the last of the sections. 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We suggest that you proceed to answer question 3 to assess your learning. Do remember to write your answers on the mark sheet before looking at the right answer!
 Question 3: Following exposure to HIV: Write “T” or “F” on the answer sheet. When you have completed all 4 questions, click on the box and mark your answers. 1. How to use this module 2. Learning outcomes 3. Introduction Partners in Global Health Education Click to for the correct answer a) 4. Epidemiology HIV infection is synonymous with AIDS 5. About the virus a 6. Section 1 Quiz 7. Transmission 8. Risk factors b) 9. Mother to Child transmission Having antibodies to HIV indicates protection b 10. HIV Testing 11. AIDS – Defining illness 12. Staging c) 14. Diagnosis 16. ART d) Viral load is high shortly after 17. Prevention 18. Section 3 Quiz 19. Sources of information c seroconversion 13. Section 2 Quiz 15. Management A glandular fever-like illness at primary HIV infection d
Question 3: Following exposure to HIV: Write “T” or “F” on the answer sheet. When you have completed all 4 questions, click on the box and mark your answers. 1. How to use this module 2. Learning outcomes 3. Introduction Partners in Global Health Education Click to for the correct answer a) 4. Epidemiology HIV infection is synonymous with AIDS 5. About the virus a 6. Section 1 Quiz 7. Transmission 8. Risk factors b) 9. Mother to Child transmission Having antibodies to HIV indicates protection b 10. HIV Testing 11. AIDS – Defining illness 12. Staging c) 14. Diagnosis 16. ART d) Viral load is high shortly after 17. Prevention 18. Section 3 Quiz 19. Sources of information c seroconversion 13. Section 2 Quiz 15. Management A glandular fever-like illness at primary HIV infection d
 Sources of information / bibliography Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 1. 2. 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 3. 4. 5. 6. Joint United Nations Programme on AIDS http: //www. unaids. org/en/ Multiple information database available from the CDC website: http: //www. cdc. gov/ Science 2000; 287: 607 -614 Science 2000; 288 (5472): 1789 -1796 UNAIDS/WHO. AIDS epidemic update, 2004. Yusuph H, Garbati MA, Akeredolu P, Gashau W. HIV-1 and HIV-2 Seroprevalence and Risk Factors in Maiduguri, Nigeria. XV International AIDS Conference, Bangkok, Thailand July 11 -16, 2004 (abstract E 710 I 7776). 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information End of module
Sources of information / bibliography Partners in Global Health Education 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 1. 2. 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz 14. Diagnosis 3. 4. 5. 6. Joint United Nations Programme on AIDS http: //www. unaids. org/en/ Multiple information database available from the CDC website: http: //www. cdc. gov/ Science 2000; 287: 607 -614 Science 2000; 288 (5472): 1789 -1796 UNAIDS/WHO. AIDS epidemic update, 2004. Yusuph H, Garbati MA, Akeredolu P, Gashau W. HIV-1 and HIV-2 Seroprevalence and Risk Factors in Maiduguri, Nigeria. XV International AIDS Conference, Bangkok, Thailand July 11 -16, 2004 (abstract E 710 I 7776). 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information End of module
 Authors and Permissions 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz Partners in Global Health Education Dr. Yusuph Haruna, Senior Lecturer and Honorary Consultant Physician, Department of Medicine, University of Maiduguri Teaching Hospital, Nigeria. Dr. David Lewis, Learning Technologist and Prof. Steve Allen, Professor of Paediatrics and International Health, Swansea Medical School, Swansea, UK Dr. Mahibur Rahman, Senior House Officer, Singleton Hospital, Swansea, UK Permissions: Please note that many images included in this module are taken from readily-accessible websites. Verbal permission was granted from patients where appropriate. This module can be used for teaching purposes within our institutions but should not be used for any other purpose. 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We are very interested to receive feedback regarding any aspect of this module – especially if it helps us to improve it as a learning resource. Please e mail any comments to either s. j. allen@swansea. ac. uk. For further information about the Partnership in Global Health Education, visit: http: //isp. swanih. org/ Back
Authors and Permissions 1. How to use this module 2. Learning outcomes 3. Introduction 4. Epidemiology 5. About the virus 6. Section 1 Quiz 7. Transmission 8. Risk factors 9. Mother to Child transmission 10. HIV Testing 11. AIDS – Defining illness 12. Staging 13. Section 2 Quiz Partners in Global Health Education Dr. Yusuph Haruna, Senior Lecturer and Honorary Consultant Physician, Department of Medicine, University of Maiduguri Teaching Hospital, Nigeria. Dr. David Lewis, Learning Technologist and Prof. Steve Allen, Professor of Paediatrics and International Health, Swansea Medical School, Swansea, UK Dr. Mahibur Rahman, Senior House Officer, Singleton Hospital, Swansea, UK Permissions: Please note that many images included in this module are taken from readily-accessible websites. Verbal permission was granted from patients where appropriate. This module can be used for teaching purposes within our institutions but should not be used for any other purpose. 14. Diagnosis 15. Management 16. ART 17. Prevention 18. Section 3 Quiz 19. Sources of information We are very interested to receive feedback regarding any aspect of this module – especially if it helps us to improve it as a learning resource. Please e mail any comments to either s. j. allen@swansea. ac. uk. For further information about the Partnership in Global Health Education, visit: http: //isp. swanih. org/ Back


