e184073df1689727b4f9fd4d76dafe48.ppt
- Количество слайдов: 130

N-205 Fundamentals Lecture Documentation

Objectives • Demonstrate the role of caregiver and communicator by documenting nursing care, following legal guidelines. • Understand the purpose of patient records, ethical accountability and confidentiality. • Review legal abbreviations used by all health care providers.

Objectives (cont’d. ) • As caregiver, understand the different methods of documenting care (narrative, pie charting, focus charting, charting by exception and computerized records). • Describe the difference between a Kardex graphic and flow sheet and progress notes. • As the communicator, describe what a change of shift report should include and its purpose.

Objectives (cont’d. ) • Discuss documentation mechanics that increase risk for legal problems. • Discuss difference between telephone reports and telephone orders • Identify ways to maintain confidentiality of records and reports

Important concepts: • Effective communication is essential to the coordination and continuity of care. – Avoid duplications and omission of care – Supports & complements one another’s care • 3 methods: – Documenting – Reporting – Conferring

Documenting Care Documentation – a written, legal record of all pertinent interactions with patient: assessing, diagnosing, planning, implementing and evaluating. › Contains data to facilitate patient care, serve as financial & legal records, help in clinical research, & decision analysis Patient record – a compilation of a patient’s health information. › legal document

What makes up the medical record? • • Face sheet Medical history & Physical exam Initial nursing assessment form Doctor’s order sheet Problem or nursing diagnosis list Nursing plan of care Graphic sheet

What makes up the medical record? • • Medication administration record Nurse’s progress notes Doctor’s progress notes Diagnostic findings Health care team records Consultation sheets Discharge plan and summary

Why is it important to document everything? • Patient record - a legal document that details all nurse’s interaction with the patient • It is the nurse’s best defense. • It should be: complete, accurate, concise, factual, organized and timely; legally prudent and confidential.

Guidelines for Effective Documentation • Content – Enter information in a complete, accurate, concise and factual manner – Record patient findings (not your interpretation but observation) – Reflects the nursing process & professional responsibilities – Avoid words like “good”, “average”, or “sufficient”; avoid generalizations “seems comfortable”

Guidelines for Effective Documentation • Content – Note problems in an orderly, sequential manner. – Document in a legally prudent manner. (adhere to agency policy & professional standards) – Document the nursing response to questionable medical orders or treatment (or failure to treat).

Guidelines … (cont’d. ) • Timing – Chart in a timely manner. Follow agency policy and modify if patient’s status warrants it. – Indicate the date and the time. • Most agencies used military time to avoid confusion. – Document as closely as possible to the time of their execution. – NEVER document interventions before carrying them out.

Military Clock Time

Guidelines. . (cont’d. ) • Format – Make sure you have the correct chart before writing. – Chart on the proper form as designated by agency policy. – Print or write legibly in dark ink. • Use correct grammar & spelling. • Use only standard terminology. • Follow computer documentation guidelines. – Date and time each entry – NEVER skip lines. Draw a single line through blank spaces. – Chart chronologically.

Guidelines (cont’d. ) Accountability › Sign your first initial, last name and title to each entry. › Do not use dittos, erasures or correcting fluids. Draw a single line Use words like “mistaken entry” or “error in charting” Re-write the entry correctly › Identify each page of record › Ensure patient record is complete before sending to medical records.

Guidelines … (cont’d. ) • Confidentiality – Patient have a moral and legal right to privacy. • Students should be familiar with agency policy • Most agencies allow students to access. • Students are bound professionally and ethically to keep in strict confidence all the info they read. • Actual patient names and other identifiers should not be used in reports.

What information is confidential? • All information about patients whether written on paper, saved on a computer or spoken aloud. – Names, addresses, telephone and fax numbers – Reason the patient is sick, treatments and info about past health condition.

Breaches of confidentiality: • Discussing patient info in any public area. • Leaving patient medical info in a public area. • Leaving a computer unattended in an accessible area with record info unsecured • Failing to log off • Sharing or exposing passwords • Improperly accessing, reviewing and/or releasing info to media or other individuals

Type of Breach Displaying information on screen that is viewed by unauthorized users Screen should not face public areas. Install encryption software Sending confidential email msgs via public networks Use encryption software Sharing printers Computer How to prevent it Request for a separate printer Copiers Discarded copies of records Use secure disposal in trash container adjacent to copiers Cordless & Cellular Phones Holding conversations vulnerable to eavesdropping Use phone with built-in encryption technology Fax Machines Faxing confidential info Verify fax number Voice Pagers Sending confidential msgs Restrict use of voice pagers to nonconfidential msgs

HIPAA of 1996 • Health Insurance Portability and Accountability Act – Final regulations published in December 2000 – Modified and released in August 2002. – Every nurse undergo training about the HIPAA to maintain confidentiality. – Includes punishment for anyone violating privacy – Fines: $250, 000.

Permitted Disclosure • Authorization Rule – Release of patient’s health information (PHI) for purposes other than treatment, payment and routine health care operations authorization form must be signed. • 3 exceptions: – Public health activities – Law enforcement and judicial proceedings – Deceased individuals – for coroners, MEs and funeral directors, organ donations

Public health activities • Tracking and notification of disease outbreaks • Infection control • Statistics related to dangerous problems with drugs or medical equipment

Law enforcement and judicial proceedings • Medical records crucial to the investigation and prosecution of a crime • Medical records to identify victims of crime or disasters • Medical personnel reporting incidents of child abuse, neglect, or domestic violence • Medical records released according to a valid subpoena

Deceased individuals • PHI needed by coroners, medical examiners, and funeral directors • PHI needed to facilitate organ donations • PHI provided to law enforcement in the case of a death from a potential crime

Incidental Disclosure • Secondary disclosure that can not reasonably be prevented. • Limited in nature and occurs as a by-product of an otherwise permitted use or disclosure • Examples: – – Use of sign-in sheets Possibility of confidential conversation being overheard Placing patient charts outside exam rooms Use of white boards; calling out names in the waiting room; leaving appointment reminder voicemail msgs

Permitted Disclosure Necessary Conditions Use of sign-in sheets Provided that the sign-in sheet does not contain information on the reason for the patient's visit The possibility of a confidential conversation being overhead Provided that the surroundings are appropriate for a confidential conversation and voices are kept down Placing patient charts outside exam rooms Provided that unauthorized public traffic is not permitted in the area of the exam rooms and face sheets are turned toward the wall

Permitted Disclosure Necessary Conditions Use of white boards Provided that only the minimum information needed for the purpose of the white board is used X-ray light boards that can be seen by passers-by Provided that patient x-rays are not left unattended on the light board Calling out names in the waiting room Provided that the reason for the patient's visit is not mentioned Leaving appointment reminder voicemail messages Provided that the minimum amount of information is disclosed

QUESTION Choose all that apply: Which of the following documentation guidelines are correct? 1. Enter information in a complete, accurate, concise, factual, and organized manner. 2. Use word such as “good”, “average”, “normal” or “sufficient” to communicate judgment about data. 3. Wait until the end of shift to document nursing interventions to ensure comprehensive charting 4. Date and time every entry.

ANSWER 1&4 1. Enter information in a complete, accurate, concise, factual and organized manner. 4. Date and time every entry.

Important concepts: Agency policies indicate which personnel are responsible for recording on each form in the record. Additional policies regarding: › › › Frequency of entry Recording of routine care Identification manner of personnel after an entry Manner in which recording errors are handled Keeping of records – microfilmed or entered in to a computer › Types of abbreviations are acceptable

Common Abbreviations ACTIVITIES AMB Ambulatory BRP Bathroom priviliges OOB Out of bed up ad lib Up as desired Abdomen BP Blood pressure bx biopsy C Celsius/centigrade c/o Complains of dx Diagnosis ASSESSMENT DATA abd FUO CTA F Fever of unknown GI origin Clear to auscultation Fahrenheit Gastrointestinal GU Genitourinary H/A Headache h/o History of HPI History of present illness

Common Abbreviations ASSESSMENT DATA Impressions lt or L Left MAE Moves all extremities NAD No apparent distress NKA No know allergies N/V Nausea & vomiting neg Negative PE Physical examination PMH Past medical history R Respirations R/O Rule out ROS P Review of systems rt or ® Pulse Right Short of breath Sx Symptoms T Temperature (+) Positive (-) negative SOB

Common Abbreviations DISEASES ASCVD Arteriosclerotic cardiovascular disease ASHD BPH Benign prostatic hypertrophy CA CAD Coronary artery disease CHF Congestive heart failure Chronic obstructive pulmonary disease CVA Cerebrovascular accident COPD DM Diabetes mellitus MI Myocardial infarction PVD Peripheral vascular disease URI Upper respiratory infection HTP (↑BP) PE STD Arteriosclerotic heart disease Cancer Hypertension Pulmonary emboli Sexually transmitted disease

Common Abbreviations DIAGNOSTIC STUDIES ABG Arterial blood gases BE Barium enema CBC Complete blood count CO 2 Carbon dioxide C&S Culture and sensitivity CXR Chest x-ray ECG (EKG) Cardiogram lytes Electrolytes RBC Red blood cells UGI Upper GI WBC White blood cells Before ad lib As desired AMA Against medical advice ASAP As soon as possible BM Bowel movement BSD UA Urinalysis MISCELLANEOUS ā C (with bar above) with CABG Bedside drainage Coronary artery bypass graft

Common Abbreviations MISCELLANEOUS CPR Cardiopulmonary resuscitation dc (disc) Discontinue DNR Do not resuscitate Dsg Dressing dx Diagnosis FOB Foot of bed Fx Fracture GHWT HOB Head of bed hs Good handwashing technique Hour of sleep Hx History I&O Intake and output IV Intravenous KVO Keep vein open NG Nasogastric noc Night Nothing by mouth NS Normal saline NPO (npo)

JCAHO “Do not use” abbreviations, acronyms or symbols Abbreviation Potential Problem Used instead U (for unit) Mistaken as 0 (zero), 4 (four) or cc Write unit. IU (for international unit) Mistaken as IV or 10 Write “international unit” Q. D. , QD, q. d. (daily) Mistaken for each other. Q. O. D. , QOD, qod, q. o. d. Write “daily” and “every other day. ” MS, MSO 4, Mg. SO 4 Write “morphine sulfate” or “magnesium sulfate” Can mean morphine sulfate or magnesium sulfate

Other “do not use” abbreviations: • > or < - maybe misinterpreted as 7 or the letter L • Abbreviations for drug names • @ - mistaken for 2. • c. c. – mistaken for U; write “m. L” • μg – mistaken for mg; write “mcg. ”

Purposes of Patient Records Communication Diagnostic & therapeutic orders Care Planning Quality Review Research Decision Analysis Education Legal Documentation Reimbursement Historical Documentation

Communication • To help healthcare professionals from different disciplines communicate with one another. • Foster continuity of care • Keep in mind that other healthcare professionals make judgments about nurses and nursing’s contributions to the healthcare team on what is documented.

Diagnostic & therapeutic orders • The chart contains all the diagnostic studies ordered for the patient since admission. • Nurses should ensure that these orders are entered and implemented. • Orders should be written and signed except: – Emergencies (verbal orders) – Practitioner is unable to be present on the unit (telephone or faxed orders)

Diagnostic orders… (cont’d. ) • Take order only from: (licensed and have credentials) – Physicians – Dentists – Psychologists – Podiatrists – Advanced practice nurses – Medical students: only when countersigned by the attending physician, nurse practitioner or a house officer

Verbal orders • Issued only during medical emergency when the physician/nurse practitioner is present but finds it impossible to write the order. • Order must be directly from the physician/nurse practitioner • Nurse receives, document and executes order • Mostly depends on agency policies.

Sample policy on verbal order documentation: • Record orders then read back the order to verify • Date and note the time orders were issued • Record V. O. , name of physician, followed by nurse’s own name & title • After the conclusion of emergency, physician should review orders and sign orders. Date and note the time he/she signs the orders.

Telephone and Fax orders • Depends on agency policy. • Orders should be repeated back to the physician. • Must be transcribed on an order sheet. • Fax orders are acceptable as long as they are legible

Sample policy for telephone/fax orders Physician or nurse practitioner should be referred to a house officer/ RN or registered pharmacist Record the orders (T. O. ) on patient’s record. Read the order back. Date and note the time the orders were issued Sign the orders with name & title › “Demerol 100 mg IM now and q 4 hr p. r. n for pain. T. O. James E. Walker, MD/Mary Pint, RN”

Care Planning • Records help professionals how the patient is responding to the treatment plan from day to day. • Example: – If the patient is gradually becoming weaker and is not unable to tolerate ambulation, orders for physical therapy and other nurse-initiated ambulation will need to be modified.

Quality Review • Charts are usually evaluated for the quality of care patient’s received and the competence of the nurses • Nursing audits – random charts are selected and reviewed • Accreditations by agencies.

Research • Researchers use charts and study patient records. • Charts used in studies hoping to learn how best to recognize or treat identified health problems from the study of similar cases.

Decision Analysis • Charts/ records provide data needed by administrative strategies planners • Helps to identify needs and the means and strategies most likely to address needs • Record review might reveal: – Underused or overused services – Prolonged hospital stays – Financial information

Education • Healthcare students/professionals can learn a great deal about clinical manifestations of particular health problems. • Effective treatment modalities and factors that affect patient goal achievement can be highlighted.

Legal Documentation • Records may be used as evidence in court proceedings • Plays a big role in implicating or absolving health practitioners charged with improper care. • Record can also be used in accident or injury claims made by patient.

Reimbursement • Records are also used to demonstrate to payers (insurance companies) that patients received the care for which reimbursement is being sought.

Historical Documentation • specific dates of entries on records - the record has value as a historical document • Information concerning a patient’s past healthcare might be pertinent.

Documentation systems METHODS OF DOCUMENTATION

Methods of Documentation • • Source-oriented records Problem-oriented medical records PIE – Problem, Intervention, Evaluation Focus charting Charting by exception Case Management Model Computerized Records

Methods of Documentation Source-Oriented Records › Each healthcare group keeps data on its own separate form › Sections designated for nurses, physicians, laboratory and x-ray personnel, etc. › Notations are entered chronologically. › Advantage: Each discipline can easily find and chart pertinent data › Disadvantage: Difficult to track problems

Forms and information • Admission sheet – legal name, identification number – age, birthdate, sex – marital status – occupation and employer – religious preference – next of kin and person to notify in case of emergency – date, time, reason for admission – name of the attending physician – insurance information – discharge data

Forms and information • Admission and nursing assessment – Results of nursing history and physical assessment • Graphic sheet – Daily temperatures, pulse and respiratory rates, blood pressure (vital signs), pain level – Daily weight – Special measurements: I&O



Forms and information • Flow sheet to record routine care – Respiratory, cardiac, pain, nutrition, elimination, IV therapy, wound tubes – Hygiene, activity, sleep – Safety, equipment – Teaching and progress sheet




Forms and information • Narrative nurse’s notes – Descriptions of pertinent observations of patient – Statements specify nursing care including teaching and his or her responses to nursing care – Statements that describe patient’s condition and progress or lack of progress – Descriptions of patient’s complaints and how patient is coping or failing to cope


Forms and information • Medication Sheet – Name of prescribed medications administered on a regular or p. r. n. basis. – Dosage of medication administered – Route by which medication was administered, unless given orally – Time medication was administered – Name or initials of person administering the medication


Forms and information • Physician’s order sheet – Orders for medications – Orders for treatments – Other directives pertinent to a particular patient’s care • Physician’s progress notes – Interpretations of patient’s pathology – Responses of patient to medical therapy

Forms and information • Miscellaneous forms – Lab reports, x-ray film reports – Consultation reports – Dietary requirements – Results of social service consultations – Types and results of physical, respiratory and xray therapy

Methods of Documentation • Problem-oriented medical records (POMR) – Originated by Dr. Lawrence Weed in 1960 s – Organized around a patient’s problems rather than around sources of information – All healthcare professionals record information on the same forms. – Advantages: entire healthcare teams works together in identifying a master list of patient problems • Collaborative plan of care

Methods of Documentation • Problem-oriented medical records (POMR) – Progress notes focus on patient problems – Major parts of POMR : • • • Defined database Problem list Care plans Progress notes Flow sheets – records information monitored over time Discharge notes – date of resolution of each problem; referrals; recommendations

Methods of Documentation • Problem-oriented medical records (POMR) – SOAP (IER) • • S – subjective data O – objective data (observations made by nurse) A – assessment (drawn from new data) P – plan (goals for action related to the patient’s problems

Defined database

Problem list

Care plan

Progress notes

Methods of Documentation • PIE – charting (Problem, Intervention, Evaluation) – It does not develop a separate plan of care. – Plan of care is incorporated into the progress notes. – A complete patient assessment is performed and documented at the beginning of each shift using pre-printed fill-in-the-blank assessment forms (flow sheets)

PIE charting

Methods of Documentation • Focus Charting – Purpose: to bring the focus of care back to the patient and the patient’s concerns – A focus column is used instead of problem list. – Topics in the focus column include • • patient concerns and behaviors therapies and responses Changes of condition Significant events (teaching, consultations, monitoring, management of ADLs

Methods of Documentation • Focus Charting – Uses DAR format • D – Data • A – Action • R – Response – Advantage: holistic emphasis on the patient and patient’s priorities; ease of charting – Disadvantage: artificial and not helpful when documenting care

Focus charting

Methods of Documentation • Charting by exception – A shorthand documentation method – Makes use of well-defined standards of practice – Only significant findings or “exceptions” to these standards are documented in narrative notes.

Methods of Documentation • Charting by exception – Advantages: decreased charting time (freeing time for direct patient care); a greater emphasis on significant data; timely retrieval of significant data; timely bedside charting; standardized assessment; greater interdisciplinary communication; better tracking of important patient responses, lower costs – Disadvantages: limited usefulness in high-quality safe care in response to negligence claim
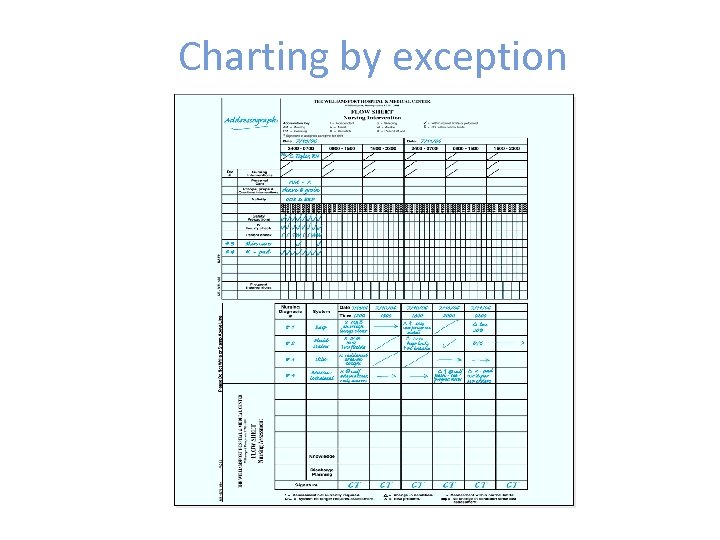
Charting by exception

Methods of Documentation • Case Management Model – Emphasis on quality, cost-effective care delivered within a limited time frame – An interdisciplinary tool that identify those outcomes that select groups of patients are expected to achieve on each day of care. – Promotes collaboration, communication and teamwork among caregivers. – Makes efficient use of time – Disadvantage: works best for “typical” patients with few individualized needs.

Collaborative Pathway • May also be called critical pathway or core map used in case management model • A part of computerized documentation system that integrates the collaborative pathway and documentation flow sheets to match each day’s outcomes • Advantage: reduced charting time by 40%, no dec in audited charting quality • Charting by exception also used

• Sample of Case Management Model. pdf

Variance Charting • Used when patient fails to meet an expected outcome or planned intervention in case management model • Format: – Unexpected event – Cause of the event – Actions taken in response to the event – Discharge planning, when appropriate

Methods of Documentation • Computerized records – Development of Computer-based patient record – Nurses calls up the admission assessment tool on the computer screen and keys in patient data – Develops plan of care (NANDA-approved diagnosis) – Adds data accordingly – Receives work list (treatments, procedures, medications) for the patient every shift – Documents care immediately beside the patient’s bedside

Computerized charting

Computerized charting • 3 nursing minimum data: – Nursing care elements (nursing dx) – Patient demographic elements – Service elements (admission, discharge date) • Data distributed among caregivers • Tracks progress of individual patients with ease; computerized outcome information compared with groups of patients with similar diagnoses.

Computerized charting • Necessitated development of policies and procedures to ensure the privacy and confidentiality • Strategies: – Never give your personal password or computer signature to anyone – Don’t leave computer terminal unattended after you have logged on – Follow correct protocol for correcting errors – Follow agency’s confidentiality procedures

FORMATS FOR NURSING DOCUMENTATION

Formats for Nursing Documentation Initial Nursing Assessment Kardex and Patient care summary Plan of Nursing care Critical/Collaborative Pathways Progress Notes Flow Sheets › › Graphic Clinical Record 24 -hr fluid balance record Medication record 24 -hr patient care records and acuity charting forms

Formats for Nursing Documentation • Discharge and Transfer Summary • Home Healthcare Documentation • Long-Term Care Documentation

Initial Nursing Assessment • Nursing history and physical assessment • Accurate documentation of these data is important • Provides baseline for later comparisons as patient’s condition changes

Kardex and patient care summary • Kardex care plan – used to communicate conveniently and concisely the plan of nursing care for each patient. • Karex is recorded on a folded card and placed in a central Kardex file where it is easily accessible.

Computer generated Kardex

Plan of Nursing Care • Contains patient’s problems or diagnoses; related goals; outcomes; and interventions; and progress or resolution of the problems. • Maybe written separately or incorporated into a multidisciplinary plan

Collaborative/Critical Pathways • Case management plan is detailed, standardized plan of care for a patient population with a designated diagnosis or procedure.

Progress Notes • Purpose is to inform caregivers of the progress a patient is making toward achieving expected outcomes. • SOAP notes, PIE notes, focus charting, charting by exception and flow sheet

Discharge and transfer summary • A written clinical report that concisely summarizes the reason for treatment, significant findings, the procedures performed and treatment rendered any specific instructions given to the patient and family.

Home Healthcare Documentation of home care visits Reports the patient’s progress at home Sent to attending physician if patient needs continuation of care OASIS – group of data elements that represent core items of a comprehensive assessment for an adult home care patient › Form basis for measuring patient outcomes › Encompasses socio-demographic, environmental, support system, health status etc.

Long-Term Care Documentation • RAI (Resident Assessment Instrument) – helps staff gather information on a resident’s strengths and needs • Tracks changes in a resident’s status • Helps residents achieve quality of care and quality of life. • Components: minimum data set; triggers; resident assessment protocols; utilization guidelines

Content and Mechanics POTENTIAL LEGAL PROBLEMS IN DOCUMENTATION

Documentation Content that increases risk for legal problems • Not in accordance with profession or healthcare organization standards. • Does not reflect patient needs • Does not include description(s) of situations that are out of the ordinary • Overgeneralizes patient assessment or nursing interventions • Incomplete or inconsistent • Does not include appropriate medical orders • Implies a potential or actual risk situation • Implies attitudinal bias

Documentation Mechanics that increase risk for legal problems • • • Lines between entries Countersigning documentation Tampering Different handwriting or obliterations Illegibility Sloppiness (sloppy care = sloppy charting) Dates and times ommitted Improper nurse signature or unidentifiable initials Transcription errors

REPORTING CARE

Reporting care • To give an account of care that has been done to other healthcare professionals • Can be oral, written, or computer-based communication of patient data to others

Face-to-face meeting • Advantages: – Message delivered immediately – Non-verbal messages are readily conveyed – Message can be clarified; receiver’s questions can be raised answered • Disadvantages: – Both parties must be available at the same time, in the same place – Ordinarily, no permanent record for later use.

Telephone conversation • Advantages: – Message delivered immediately – Message can be clarified – Two parties need not be present in same place • Disadvantages: – Only the tone of voice and voice inflections can be communicated – no non-verbal messages – Ordinarily, no permanent record

Written message • Advantages: – Message can be exchanged at times convenient for the people involved – Record is available – Time efficient • Disadvantages: – Message usually cannot be validated with sender

Audiotaped message • Advantages: – Convenient for people involved – Record is available – Time-efficient, if info communicated is complete • Disadvantages: – Cannot be validated with sender

Computer message • Advantages: – Message delivered immediately – even to those at a great distance – Parties need not be present in same place – Two-way communication is possible by email – Record is available – Many people can participate in exchange • Disadvantages: – No non-verbal messages can be communicated – Privacy concerns remain an issue

TYPES OF REPORTING CARE

Types of Reports: • • Change-of –shift report Telephone/telemedicine reports Transfer and discharge reports Reports to family members and significant others

Change-of-shift reports • Given by a primary nurse to the nurse replacing him/her or by the charge nurse to the nurse who assumes responsibility for continuing care of the patient • Maybe in written form or orally in a meeting

Components of a Change-of-shift Report • Basic identifying information • Current appraisal of each patient’s health status • Current orders • Summary of each newly admitted patient (medical dx, age, plan of therapy and gen. condition) • Report on patients who have been transferred or discharge

Telephone/Telemedicine Reports • Reports about changes in patient’s condition from other healthcare professionals • Nurses should to do the following: – Identify themselves and the patient. State their relationship to the patient. – Report concisely and accurately the change in the patient’s condition and what has been done – Report patient’s VS and clinical manifestations – Have patient’s record at hand – Concisely record time and date of call and what was communicated.

Transfer and Discharge Reports • A summary of patient’s condition and care when transferring patients from one unit or institution or agency to another • Example: from post-anesthesia unit to surgical floor) • Concisely summarize all patient data.

Reports to family members and significant others • Helps in keeping patient’s family and significant others updated about the patient’s condition and progress toward goal achievement. • Nurses should: – Clarify if any are entitled to progress reports – Clarify what types of information they are able to communicate. Use professional judgment if patient is unable to communicate

Incident reports • Also termed a variance or occurrence report • A tool used by healthcare agencies to document the occurrence of anything out of the ordinary that results in or has the potential to result in harm to a patient, employee or visitor. • Used for quality improvement • Should not be used for disciplinary action against staff members

CONFERRING ABOUT CARE

Conferring About Care • To consult with someone to exchange ideas or to seek information, advice or instructions • Nurse may consult with another nurse • Types: – Consultations and referrals – Nursing and interdisciplinary team care conferences – Nursing care rounds

Consultations and referrals • Consultation – process of inviting another professional to evaluate the patient and make recommendations about his or her treatment • Referrals – process of sending or guiding the patient to another source for assistance

Nursing and interdisciplinary team care conferences • Nurses and other healthcare professionals frequently confer in groups to plan and coordinate patient care. • Also used for instructing students and practitioners • Nursing care conference – meeting of nurses to discuss some aspect of a patient’s care

Nursing care rounds • Procedure in which a group of nurses visit selected patients individually at each patient’s bedside • Primary purpose: to gather information to help plan nursing care, to evaluate the nursing care the patient has received, and to provide the patient with an opportunity to discuss his or her care with those administering it.

ANY QUESTIONS? ? ?

End of lecture Thank you!
e184073df1689727b4f9fd4d76dafe48.ppt