7848cb6cf90cca0863cfbd81a92fef5d.ppt
- Количество слайдов: 28
MULTIDRUGRESISTANT TUBERCULOSIS (MDRTB) by Dr Mat Zuki Mat Jaeb 1
LEARNING OBJECTIVES v. To identify those at risk of MDR-TB v. To learn on what to do when MDR-TB is suspected v. To learn the basic principles of treatment 2
MULTIDRUG- RESISTANT TUBERCULOSIS (MDR-TB) Outline v. Introduction v. Definition v. Risk Factors v. Diagnosis v. Principle of Management 3
INTRODUCTION v MDR & Extensively drug-resistant TB (XDR-TB) incidence & prevalence are increasing worldwide including Malaysia v. Rate of MDR-TB cultures had increased from 0. 3% in 2005 to 1. 3% in 2011 of all MTB cultures positive in Malaysia 1 v High mortality & morbidity v. In a study in Vietnam, mortality during MDR-TB treatment was 8. 7%2 1 Sistem Maklumat Tibi KKM, 2011 2 Quy HT et al. , Int J Tuberc Lung Dis, 2006 4
INTRODUCTION v. Complex treatment, costly & long treatment duration v. Drugs adverse effects - compliance issues v. Importance of strict infection control measures 5
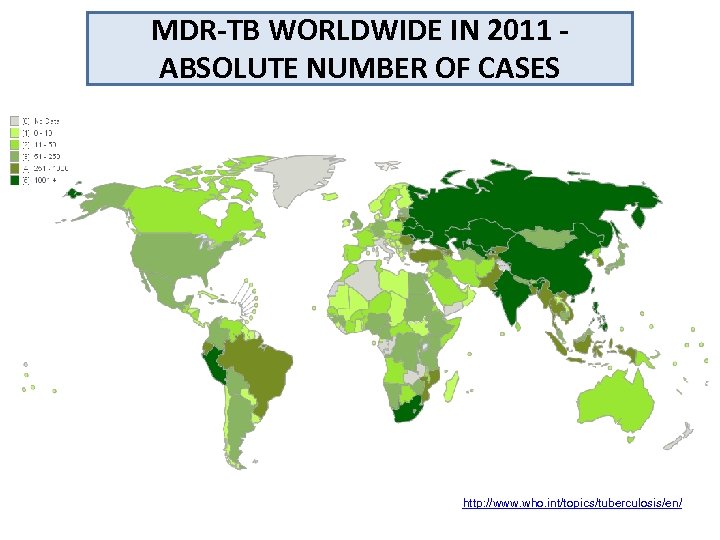
MDR-TB WORLDWIDE IN 2011 ABSOLUTE NUMBER OF CASES http: //www. who. int/topics/tuberculosis/en/ 6
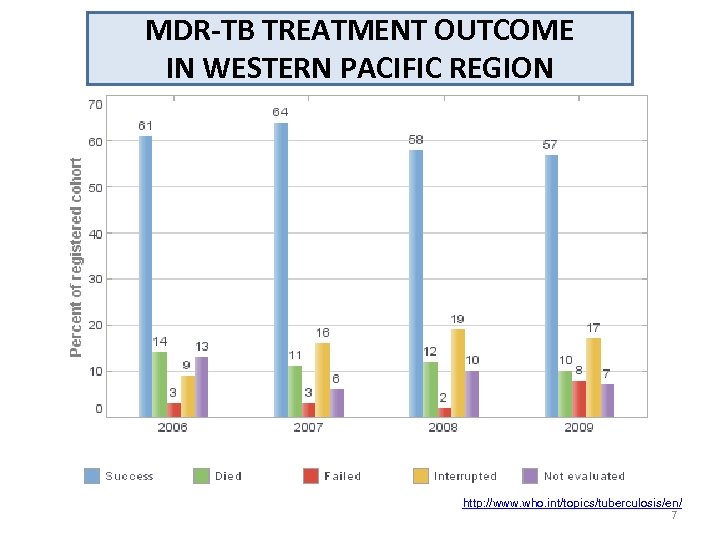
MDR-TB TREATMENT OUTCOME IN WESTERN PACIFIC REGION http: //www. who. int/topics/tuberculosis/en/ 7
DEFINITION v. Monodrug resistant v MTB resistant to any one of anti. TB drugs v. Polydrug resistant v MTB resistant to 2 or more anti. TB drugs v. Multidrug resistant v MTB resistant to both isoniazid & rifampicin with or without resistance to other anti. TB drugs 8
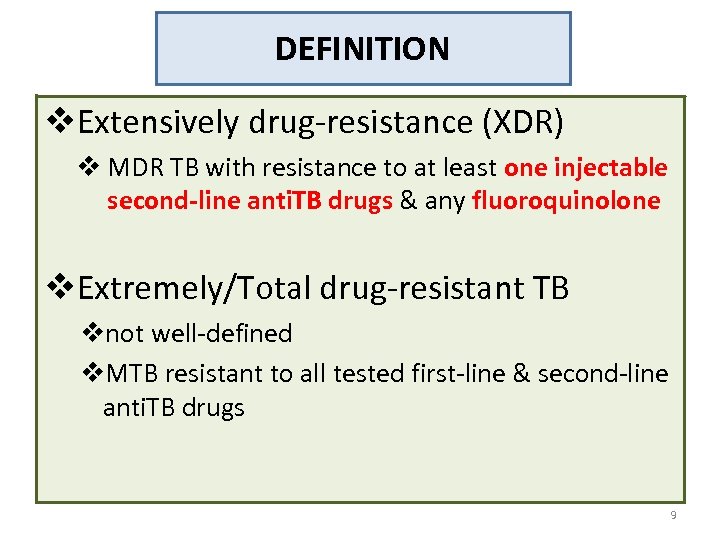
DEFINITION v. Extensively drug-resistance (XDR) v MDR TB with resistance to at least one injectable second-line anti. TB drugs & any fluoroquinolone v. Extremely/Total drug-resistant TB vnot well-defined v. MTB resistant to all tested first-line & second-line anti. TB drugs 9
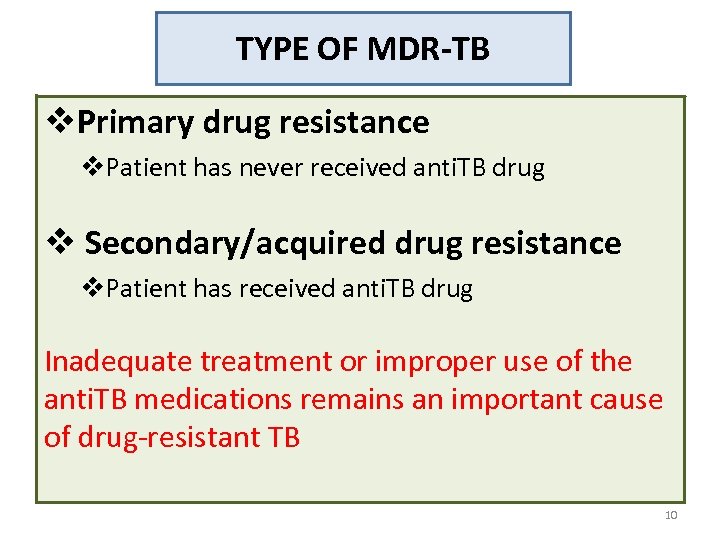
TYPE OF MDR-TB v. Primary drug resistance v. Patient has never received anti. TB drug v Secondary/acquired drug resistance v. Patient has received anti. TB drug Inadequate treatment or improper use of the anti. TB medications remains an important cause of drug-resistant TB 10
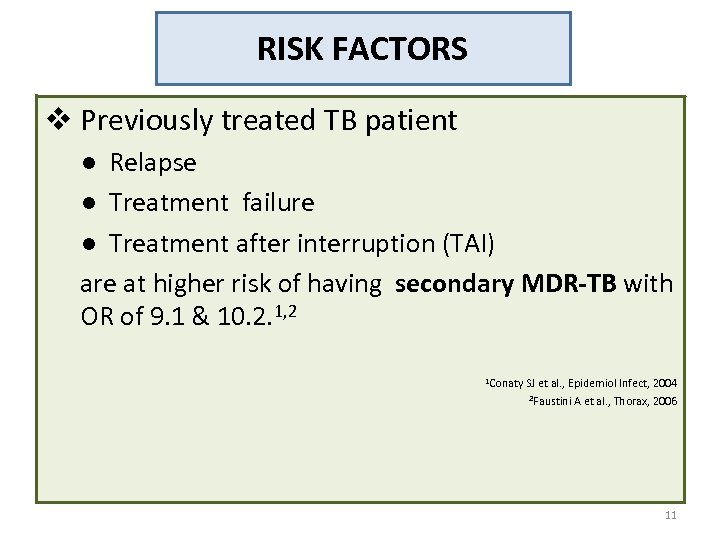
RISK FACTORS v Previously treated TB patient ● Relapse ● Treatment failure ● Treatment after interruption (TAI) are at higher risk of having secondary MDR-TB with OR of 9. 1 & 10. 2. 1, 2 1 Conaty SJ et al. , Epidemiol Infect, 2004 2 Faustini A et al. , Thorax, 2006 11
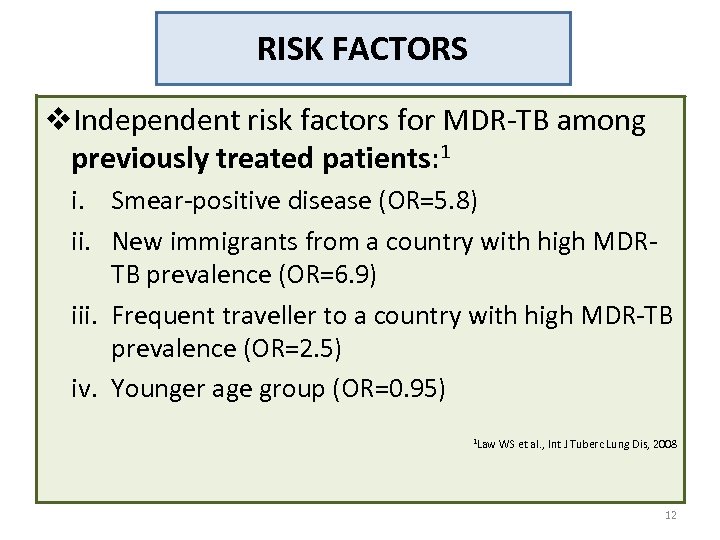
RISK FACTORS v. Independent risk factors for MDR-TB among previously treated patients: 1 i. Smear-positive disease (OR=5. 8) ii. New immigrants from a country with high MDRTB prevalence (OR=6. 9) iii. Frequent traveller to a country with high MDR-TB prevalence (OR=2. 5) iv. Younger age group (OR=0. 95) 1 Law WS et al. , Int J Tuberc Lung Dis, 2008 12
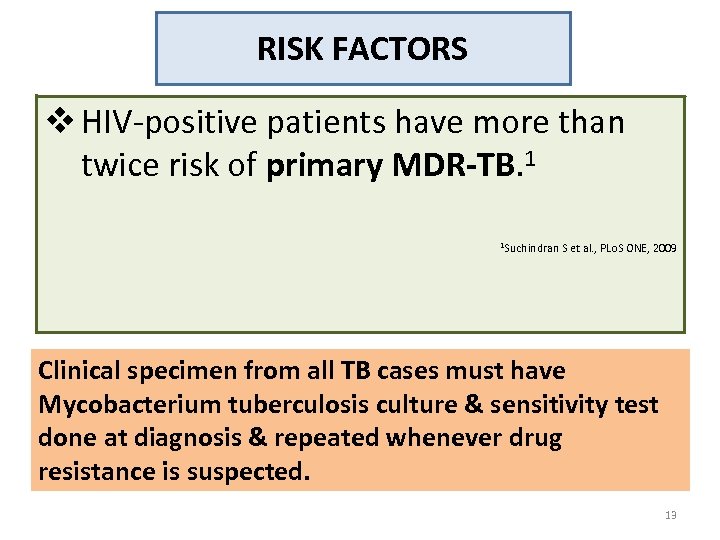
RISK FACTORS v HIV-positive patients have more than twice risk of primary MDR-TB. 1 1 Suchindran S et al. , PLo. S ONE, 2009 Clinical specimen from all TB cases must have Mycobacterium tuberculosis culture & sensitivity test done at diagnosis & repeated whenever drug resistance is suspected. 13
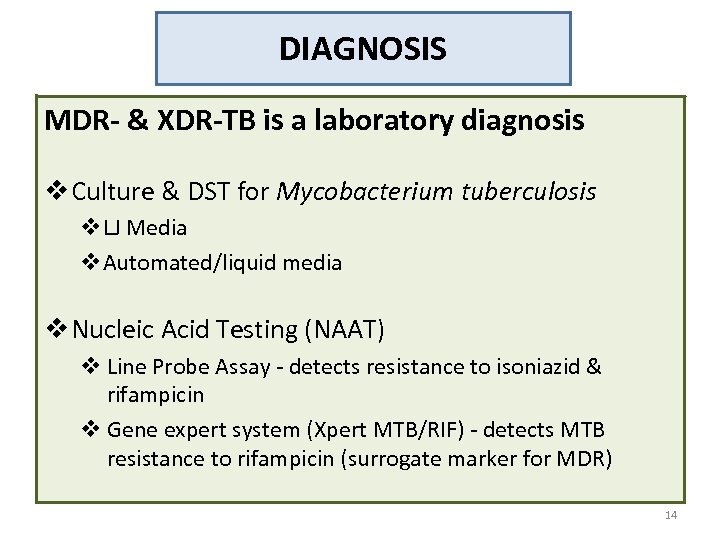
DIAGNOSIS MDR- & XDR-TB is a laboratory diagnosis v Culture & DST for Mycobacterium tuberculosis v. LJ Media v. Automated/liquid media v Nucleic Acid Testing (NAAT) v Line Probe Assay - detects resistance to isoniazid & rifampicin v Gene expert system (Xpert MTB/RIF) - detects MTB resistance to rifampicin (surrogate marker for MDR) 14
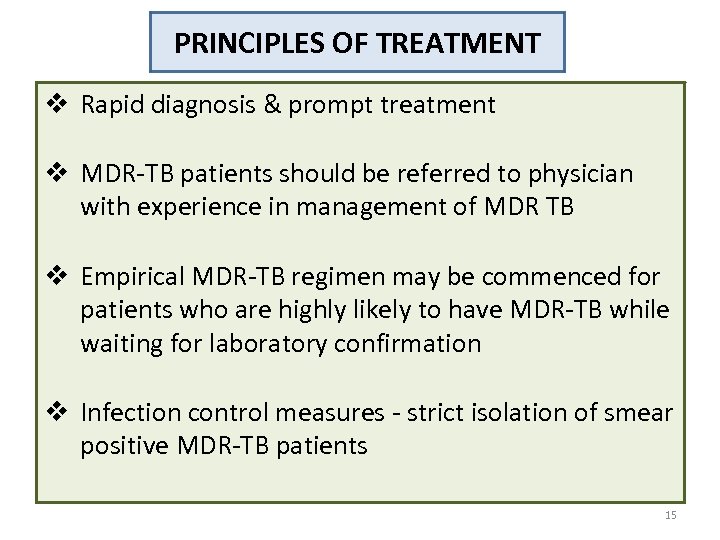
PRINCIPLES OF TREATMENT v Rapid diagnosis & prompt treatment v MDR-TB patients should be referred to physician with experience in management of MDR TB v Empirical MDR-TB regimen may be commenced for patients who are highly likely to have MDR-TB while waiting for laboratory confirmation v Infection control measures - strict isolation of smear positive MDR-TB patients 15
MDR-TB TREATMENT REGIMEN 1. Standard MDR-TB regimen (standardised approach) or 2. Individually-tailored regimen - regimen will be based on DST for second-line drugs 16
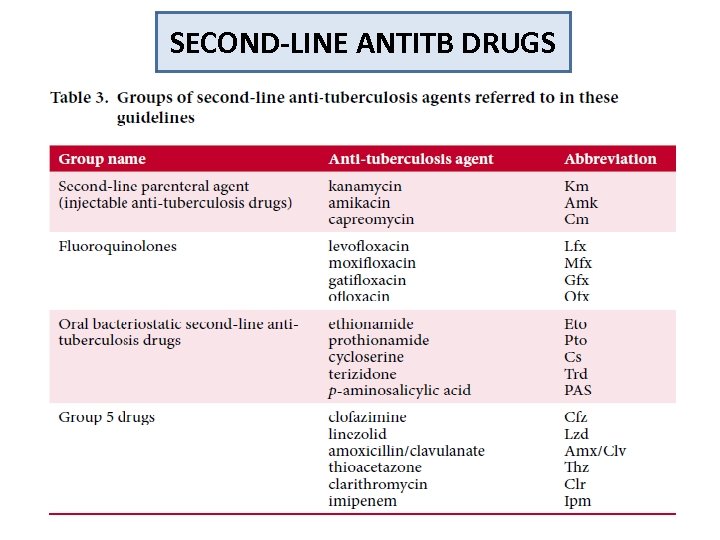
SECOND-LINE ANTITB DRUGS 17
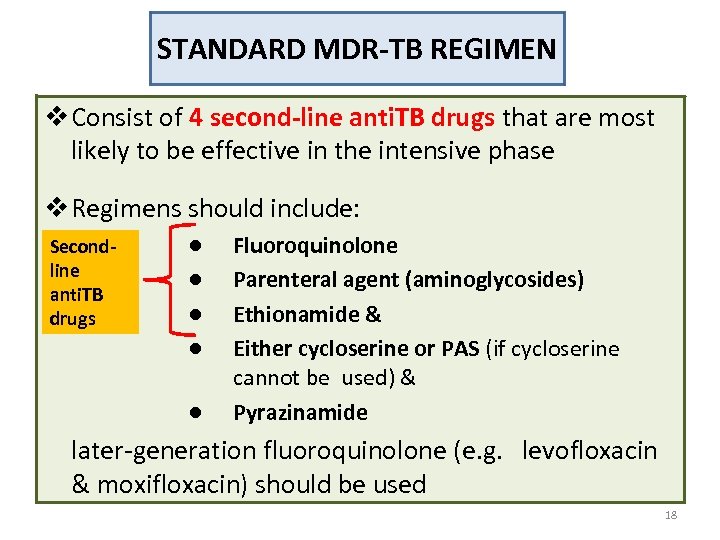
STANDARD MDR-TB REGIMEN v Consist of 4 second-line anti. TB drugs that are most likely to be effective in the intensive phase v Regimens should include: Secondline anti. TB drugs ● ● ● Fluoroquinolone Parenteral agent (aminoglycosides) Ethionamide & Either cycloserine or PAS (if cycloserine cannot be used) & Pyrazinamide later-generation fluoroquinolone (e. g. levofloxacin & moxifloxacin) should be used 18
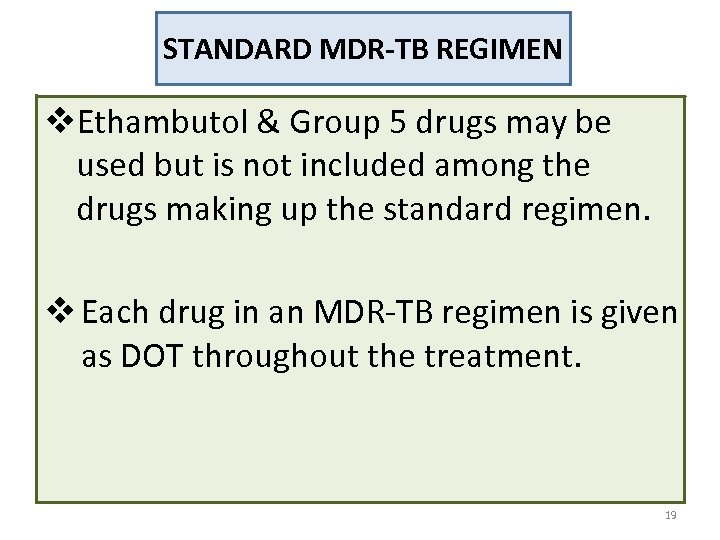
STANDARD MDR-TB REGIMEN v. Ethambutol & Group 5 drugs may be used but is not included among the drugs making up the standard regimen. v Each drug in an MDR-TB regimen is given as DOT throughout the treatment. 19
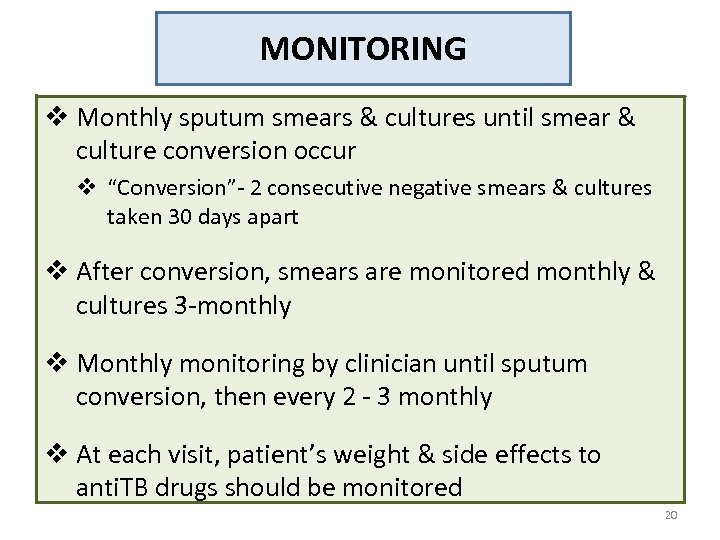
MONITORING v Monthly sputum smears & cultures until smear & culture conversion occur v “Conversion”- 2 consecutive negative smears & cultures taken 30 days apart v After conversion, smears are monitored monthly & cultures 3 -monthly v Monthly monitoring by clinician until sputum conversion, then every 2 - 3 monthly v At each visit, patient’s weight & side effects to anti. TB drugs should be monitored 20
DURATION OF TREATMENT v Intensive phase v. Defined by the duration of treatment with the injectable agent WHO recommends 8 months for most patients v Duration of treatment v. Newly MDR-TB (i. e. not previously treated for MDR-TB), a total treatment duration is 20 months for most patients May be modified according to the response to treatment based on patient’s cultures, smears, CXR & clinical status 21
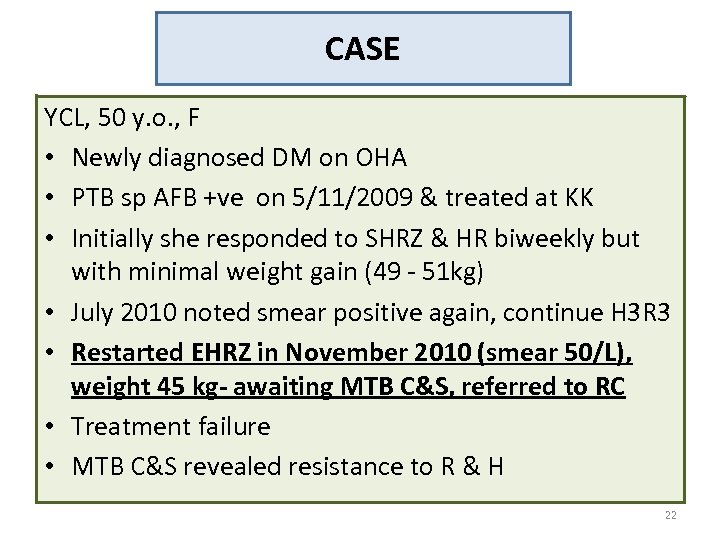
CASE YCL, 50 y. o. , F • Newly diagnosed DM on OHA • PTB sp AFB +ve on 5/11/2009 & treated at KK • Initially she responded to SHRZ & HR biweekly but with minimal weight gain (49 - 51 kg) • July 2010 noted smear positive again, continue H 3 R 3 • Restarted EHRZ in November 2010 (smear 50/L), weight 45 kg- awaiting MTB C&S, referred to RC • Treatment failure • MTB C&S revealed resistance to R & H 22
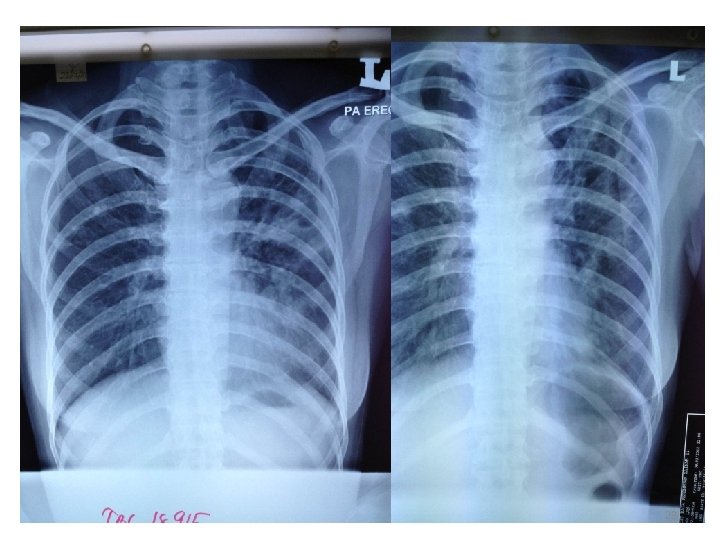
23
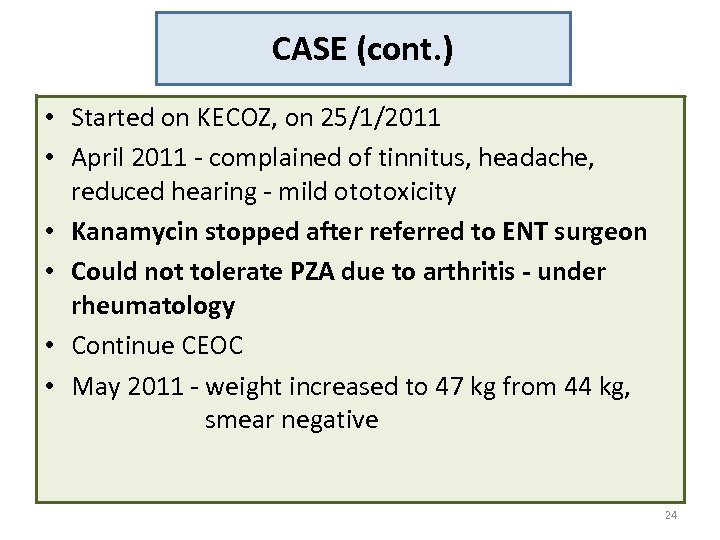
CASE (cont. ) • Started on KECOZ, on 25/1/2011 • April 2011 - complained of tinnitus, headache, reduced hearing - mild ototoxicity • Kanamycin stopped after referred to ENT surgeon • Could not tolerate PZA due to arthritis - under rheumatology • Continue CEOC • May 2011 - weight increased to 47 kg from 44 kg, smear negative 24
CASE (cont. ) • September 2011 - nausea, vomiting, numbness & poor appetite, weight reduced to 42 kg, hypoglycaemia - admitted to ward for dehydration CEOC was withheld few days then continued…. • Oct 2011, Dec 2011, Jan 2012, Feb 2012 - tolerating CEOC but not much improvement of appetite & weight with on/off cough • March 2012 - weight 39 kg, symptomatic, smear positive Persistent smear positive…. . Story continues…. . 25

26
TAKE HOME MESSAGES v MDR-TB must be suspected & investigated promptly in previously treated TB patient & high risk groups v Rapid test to diagnose MDR-TB should be carried out on MDR-TB suspect v MDR-TB should be treated by physician with experience in managing MDR v Strict infection control measures should be practiced to prevent MDR-TB transmission 27

THANK YOU Ømzek 4708@yahoo. com 28
7848cb6cf90cca0863cfbd81a92fef5d.ppt