3ccf0f0d0b538df51189134adee2f446.ppt
- Количество слайдов: 44
MSH Orientation Geriatric Medicine Dr. Shabbir Alibhai | Dr. Arielle Berger | Dr. Vicky Chau Dr. Barry Goldlist | Dr. Dan Liberman | Dr. Karen Ng | Dr. Samir Sinha Mount Sinai Hospital Suite 475, 600 University Avenue Toronto, Ontario, M 5 G 1 X 5 (416) 586 -4800 x 7859
Outline • Why Geriatrics? • Continuum of Geriatric Models of Care • Geriatric Medicine Consultation Service & Clinics • Orientation Package • Orthopedic & Physiatry Residents
WHY GERIATRICS?
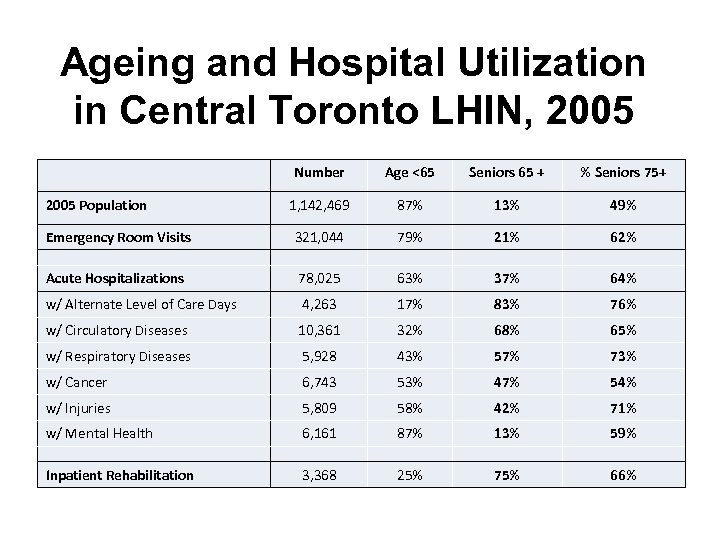
Ageing and Hospital Utilization in Central Toronto LHIN, 2005 Number Age <65 Seniors 65 + % Seniors 75+ 1, 142, 469 87% 13% 49% Emergency Room Visits 321, 044 79% 21% 62% Acute Hospitalizations 78, 025 63% 37% 64% w/ Alternate Level of Care Days 4, 263 17% 83% 76% w/ Circulatory Diseases 10, 361 32% 68% 65% w/ Respiratory Diseases 5, 928 43% 57% 73% w/ Cancer 6, 743 53% 47% 54% w/ Injuries 5, 809 58% 42% 71% w/ Mental Health 6, 161 87% 13% 59% Inpatient Rehabilitation 3, 368 25% 75% 66% 2005 Population Toronto Central LHIN, 2006
The Hazards of Hospitalization • Older people are particularly vulnerable to the risks of iatrogenic illness and functional decline • The pathogenesis of functional and cognitive decline is complex and involves an interaction amongst: – The ageing process – Comorbid and acute illnesses – The hospitalization process
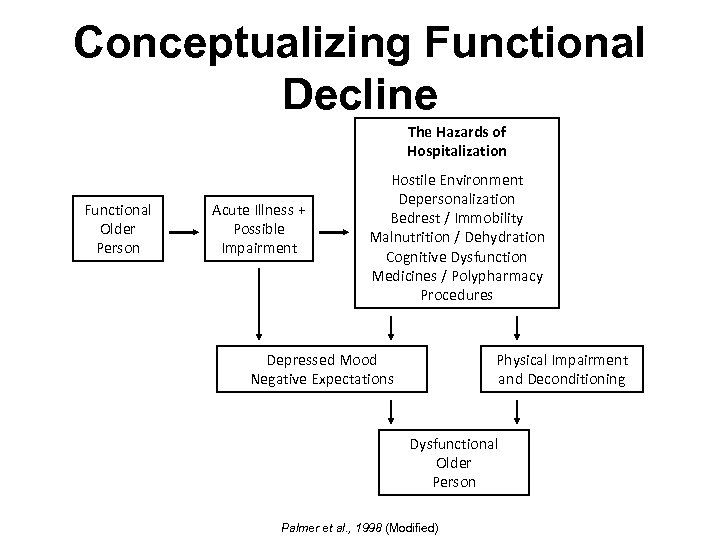
Conceptualizing Functional Decline The Hazards of Hospitalization Functional Older Person Acute Illness + Possible Impairment Hostile Environment Depersonalization Bedrest / Immobility Malnutrition / Dehydration Cognitive Dysfunction Medicines / Polypharmacy Procedures Depressed Mood Negative Expectations Physical Impairment and Deconditioning Dysfunctional Older Person Palmer et al. , 1998 (Modified)
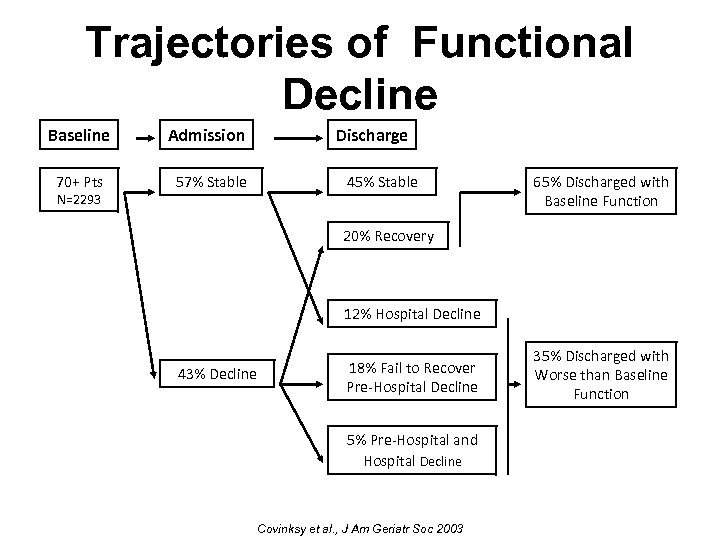
Trajectories of Functional Decline Baseline 70+ Pts N=2293 Admission 57% Stable Discharge 45% Stable 65% Discharged with Baseline Function 20% Recovery 12% Hospital Decline 43% Decline 18% Fail to Recover Pre-Hospital Decline 5% Pre-Hospital and Hospital Decline Covinksy et al. , J Am Geriatr Soc 2003 35% Discharged with Worse than Baseline Function
Costs of Functional Decline • The loss of independent functioning during hospitalization has been associated with: – – Prolonged lengths of hospital stay Increased readmission A greater risk of institutionalization Higher mortality rates Palmer et al. , 1998
Comprehensive Geriatrics Assessment (CGA) “ … a multidisciplinary diagnostic process intended to determine a frail elderly person’s medical, psychosocial, and functional capabilities and limitations in order to develop an overall plan for treatment and long term follow up” Rubenstein, 1982
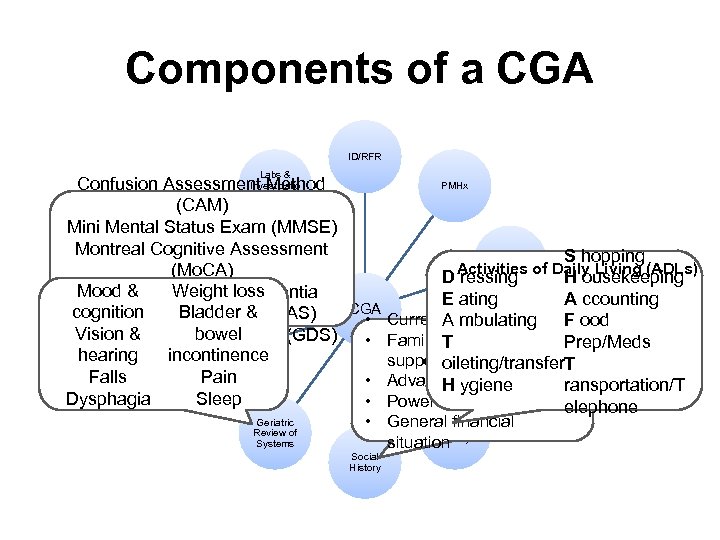
Components of a CGA ID/RFR Labs & Investigatio PMHx Confusion Assessment Method ns (CAM) Mini Mental Status Exam (MMSE) Montreal Cognitive Assessment Physical S hopping Examinatio HPI Activities of Daily Living (ADLs) (Mo. CA) n D ressing H ousekeeping Mood & Universalloss Rowland Weight Dementia E ating A ccounting CGA Bladder & cognition Assessment Scale (RUDAS) • Current. A mbulating living situation F ood bowel Vision &Depression Scale (GDS) Geriatric • Family T community Prep/Meds & Cognitive Medication Assessme incontinence hearing s supports oileting/transfer. T nt Pain Falls • Advance care directivesransportation/T H ygiene Sleep Dysphagia • Powers of attorney elephone Geriatric • General financial Functional Review of Systems History situation Social History

MSH & UHN GERIATRIC CARE CONTINUUM
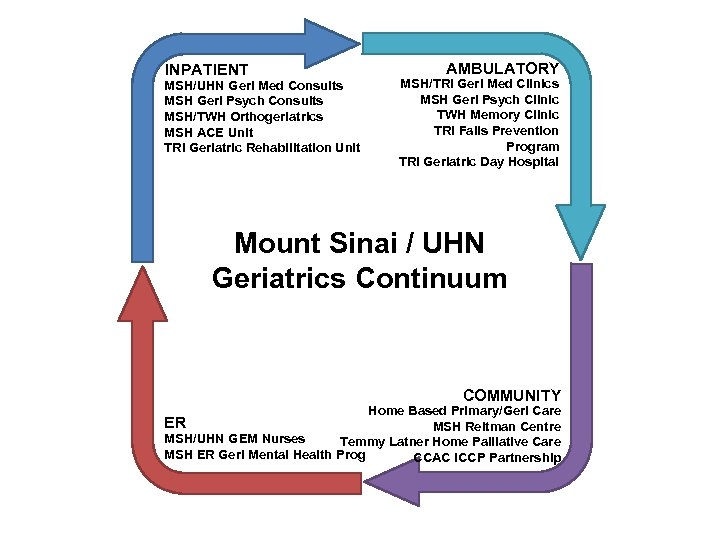
INPATIENT MSH/UHN Geri Med Consults MSH Geri Psych Consults MSH/TWH Orthogeriatrics MSH ACE Unit TRI Geriatric Rehabilitation Unit AMBULATORY MSH/TRI Geri Med Clinics MSH Geri Psych Clinic TWH Memory Clinic TRI Falls Prevention Program TRI Geriatric Day Hospital Mount Sinai / UHN Geriatrics Continuum COMMUNITY Home Based Primary/Geri Care ER MSH Reitman Centre MSH/UHN GEM Nurses Temmy Latner Home Palliative Care MSH ER Geri Mental Health Prog CCAC ICCP Partnership

GERIATRIC CONSULTATION SERVICE
Inpatient Geriatric Medicine • Interprofessional team – Carm Marziliano, SW – Natasha Bhesania, PT – Chris Fan-Lun, Pharm • Common Referrals from MSH, TGH, & PMH – Delirium & dementia – Functional decline, falls – Diagnostic/treatment challenge – Transition to outpatient & home-based services (House Calls) – Goals of care & disposition
Other Common Referrals • Automatic consultations – Orthogeriatrics hip fracture patients – House Calls – ICCP • GEM Flags • Geriatric Psychiatry
Orthogeriatrics Automatic geriatric consultation for ALL fractured hip patients ≥ 65 years old * * Orthopedic residents focus on low trauma (fragility) hip fractures (NOT high trauma, periprosthestic, or pathological) but can be involved in medical & surgical cases for further learning • Orthopedic, Hospitalist, & Geriatric Medicine Co. Management Model • Referrals – Staff automatic e-mail notification – Jeanette Villapando/Tammy Mok, x 8419 – 11 S, x 4580
A Reactiv Proactive Strategy e • Delirium prevention & management • Functional recovery • Pain management • Falls prevention & bone health • Disposition planning Marcantonio et al, 2001; Siddiqi et al. , 2009
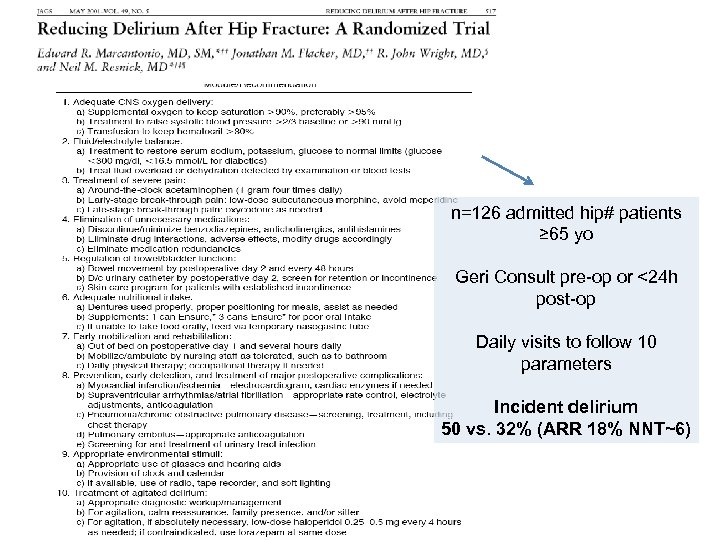
n=126 admitted hip# patients ≥ 65 yo Geri Consult pre-op or <24 h post-op Daily visits to follow 10 parameters Incident delirium 50 vs. 32% (ARR 18% NNT~6)
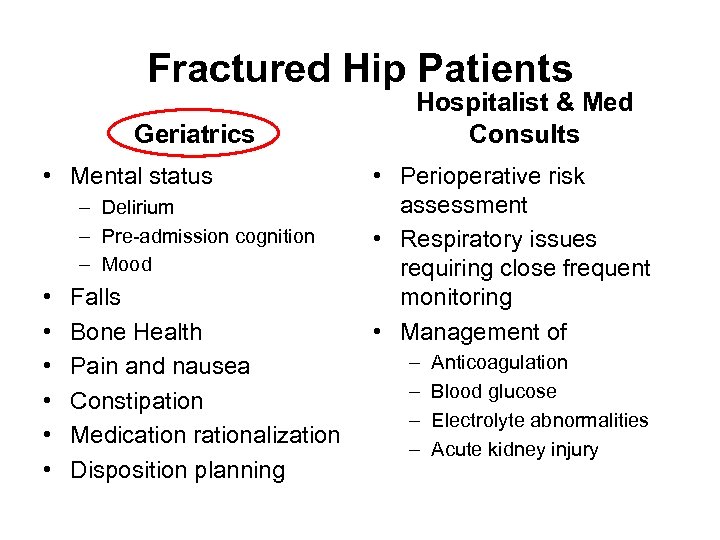
Fractured Hip Patients Geriatrics • Mental status – Delirium – Pre-admission cognition – Mood • • • Falls Bone Health Pain and nausea Constipation Medication rationalization Disposition planning Hospitalist & Med Consults • Perioperative risk assessment • Respiratory issues requiring close frequent monitoring • Management of – – Anticoagulation Blood glucose Electrolyte abnormalities Acute kidney injury
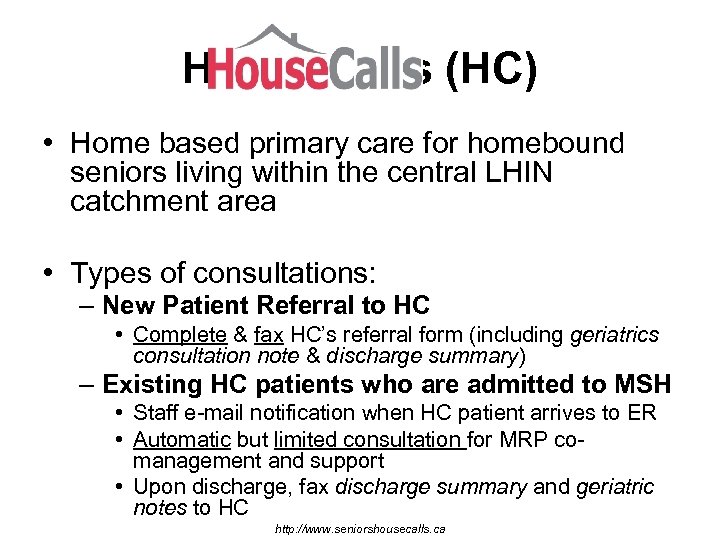
House Calls (HC) • Home based primary care for homebound seniors living within the central LHIN catchment area • Types of consultations: – New Patient Referral to HC • Complete & fax HC’s referral form (including geriatrics consultation note & discharge summary) – Existing HC patients who are admitted to MSH • Staff e-mail notification when HC patient arrives to ER • Automatic but limited consultation for MRP comanagement and support • Upon discharge, fax discharge summary and geriatric notes to HC http: //www. seniorshousecalls. ca
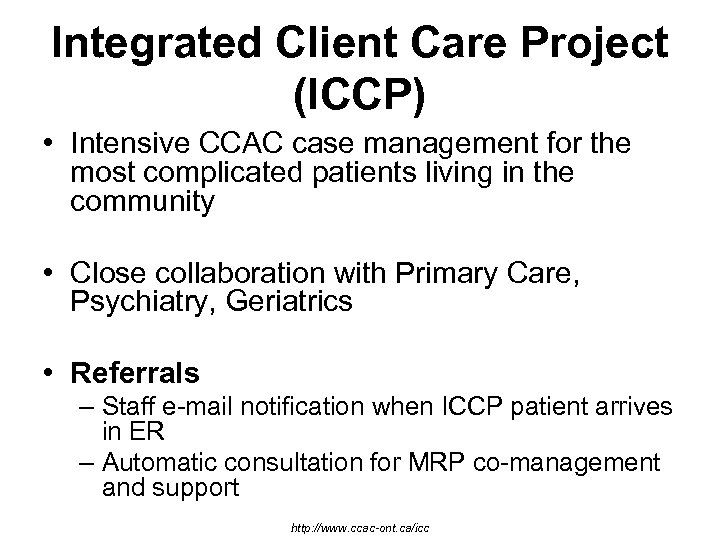
Integrated Client Care Project (ICCP) • Intensive CCAC case management for the most complicated patients living in the community • Close collaboration with Primary Care, Psychiatry, Geriatrics • Referrals – Staff e-mail notification when ICCP patient arrives in ER – Automatic consultation for MRP co-management and support http: //www. ccac-ont. ca/icc
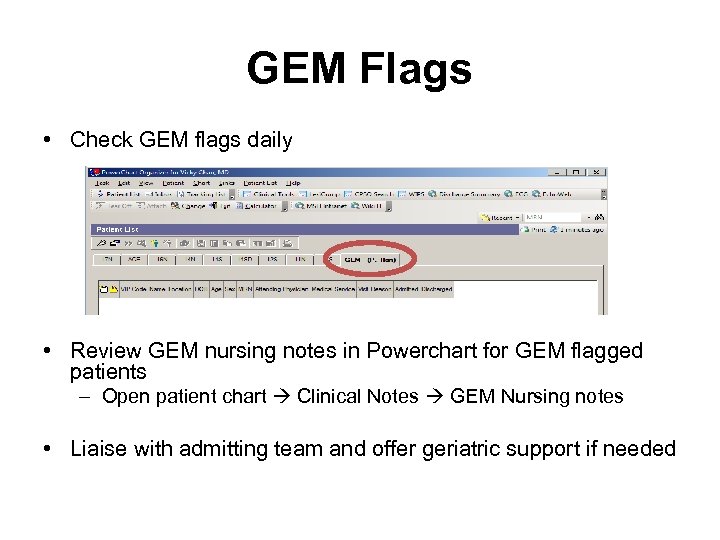
GEM Flags • Check GEM flags daily • Review GEM nursing notes in Powerchart for GEM flagged patients – Open patient chart Clinical Notes GEM Nursing notes • Liaise with admitting team and offer geriatric support if needed
Geriatric Psychiatry Consult Service • Shared care for complicated: – Mental health illnesses – Delirium management – Behavioural & psychological symptoms of dementia
Consultations E-mail new referrals to the interprofessional geriatric medicine team at MSH & TGH respectively
Consultations • Always record consult date, start, and stop time on your consult note • Store carbon copy of completed consults in the filing cabinet (middle drawer) in alphabetical order
Consult Recommendations • AVOID consult SUGGEST orders – Miscommunication – Delays in patient care • Always best to communicate recommendations directly to referring team • Direct order entry for geriatric related issues on fractured hip patients
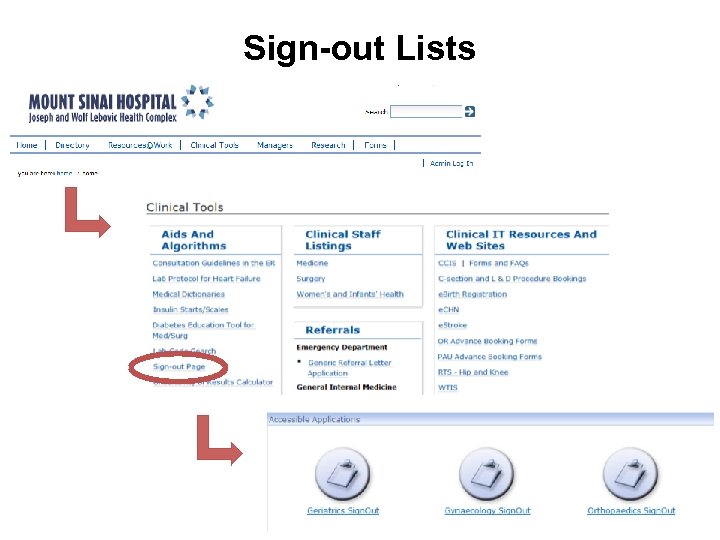
Sign-out Lists
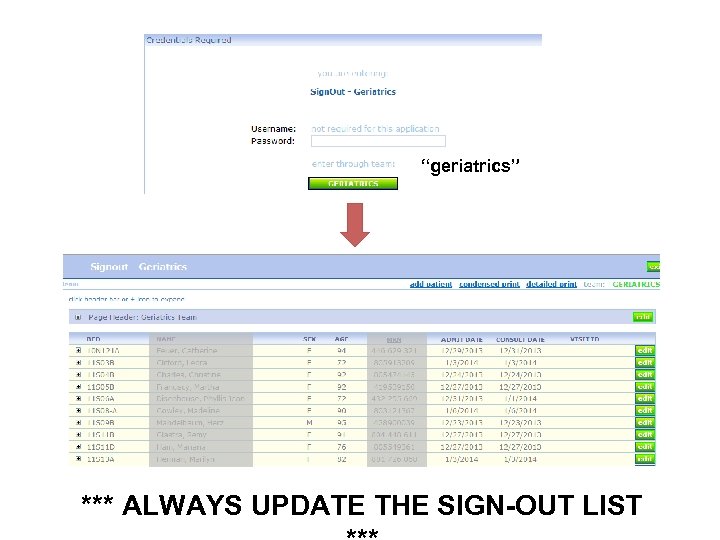
“geriatrics” *** ALWAYS UPDATE THE SIGN-OUT LIST

OUTPATIENT GERIATRIC & SPECIALTY CLINICS
Clinic • Please check your schedules & be on time for your clinic, as patients have been scheduled for you in advance
Geriatric Medicine Clinics TRI Outpatient Clinics Ground Floor (Elm Street Entrance) Drs. Alibhai, Berger, Chau, Liberman Ramona Gheorghe, NP, & Katie Stock, SW UC Outpatient Physician Clinics Admin (416) 597 -3422 x 4200 MSH AIMGP Area 4 th floor Drs. Goldlist, Ng, Sinha Chris Fan-Lun, Pharmacist Stephanie (416) 586 -4800 x 8563 * Please ensure you obtain an MSH and/or UHN dictation code at the beginning of your rotation *
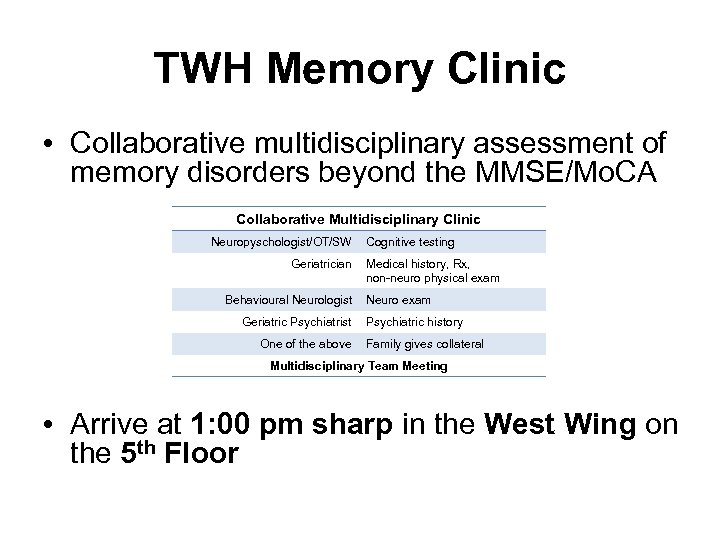
TWH Memory Clinic • Collaborative multidisciplinary assessment of memory disorders beyond the MMSE/Mo. CA Collaborative Multidisciplinary Clinic Neuropyschologist/OT/SW Geriatrician Behavioural Neurologist Geriatric Psychiatrist One of the above Cognitive testing Medical history, Rx, non-neuro physical exam Neuro exam Psychiatric history Family gives collateral Multidisciplinary Team Meeting • Arrive at 1: 00 pm sharp in the West Wing on the 5 th Floor
TRI Falls Prevention Clinic • Focused assessment of falls in older adults – Multidisciplinary intake assessment for consideration of a 12 Week Falls Prevention Program • Arrive at 1: 00 pm sharp for clinic orientation • Located in the outpatient clinic area on

ORIENTATION PACKAGE
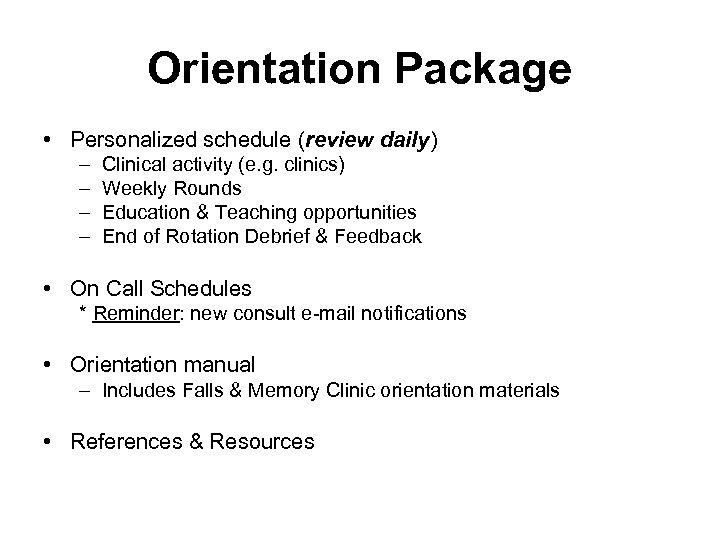
Orientation Package • Personalized schedule (review daily) – – Clinical activity (e. g. clinics) Weekly Rounds Education & Teaching opportunities End of Rotation Debrief & Feedback • On Call Schedules * Reminder: new consult e-mail notifications • Orientation manual – Includes Falls & Memory Clinic orientation materials • References & Resources
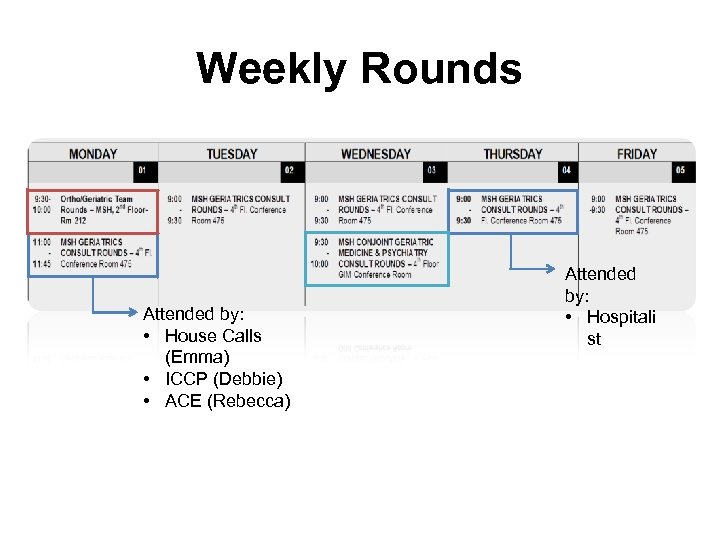
Weekly Rounds Attended by: • House Calls (Emma) • ICCP (Debbie) • ACE (Rebecca) Attended by: • Hospitali st
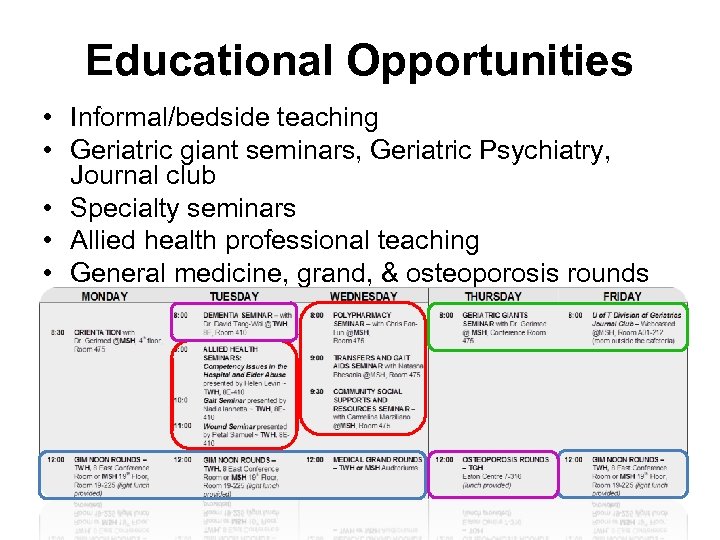
Educational Opportunities • Informal/bedside teaching • Geriatric giant seminars, Geriatric Psychiatry, Journal club • Specialty seminars • Allied health professional teaching • General medicine, grand, & osteoporosis rounds
Resident Geriatric Office • Office workspace for you and others during your rotation, so please keep it clean and tidy • Obtain an office key from Phoebe Tian – $20 deposit - - returned at the end of rotation • Always lock the door and turn off the lights if you are the last one in the office
http: //www. mountsinai. on. ca/education/ geriatrics/resident-resources-andschedules/
ADDITIONAL NOTES FOR ORTHOPEDIC & PHYSIATRY RESIDENTS
Orthogeriatric Resident Schedule • 2 weeks hospitalist then 2 weeks geriatric medicine • Mandatory clinics & programs during your rotation – Falls Prevention Clinic – Geriatric Day Hospital • Additional medical consults teaching • 1 Weekend Home Call shift (see next slides)
Physiatry Resident Schedule • 8 Week block – 2 Weeks acute care geriatrics at MSH/UHN – 3 Weeks rehabilitation at TRI • Separate TRI Orientation upon start at TRI – 3 Weeks outpatient clinics & community experiences • 1 Weekend Home Call shift
Weekend Home Call • Geriatric medicine staff receives e-mail notification of new orthogeriatrics (and surgical) referrals and will divvy consults to the orthopedic resident on call • Contact your on-call staff prior to the weekend to exchange contacts
Thank You & Enjoy Your Rotation! • Questions?
3ccf0f0d0b538df51189134adee2f446.ppt