06b660804cfa4a5c4b36a99a2ad3462e.ppt
- Количество слайдов: 66
MR Venography Ivan Pedrosa, M. D. Beth Israel Deaconess Medical Center Harvard Medical School Boston, MA
Why MR Imaging? • Conventional venography – – – Multiple injections I. V. access in affected edematous extremity Radiation / iodinated contrast • US – Limited in central veins – Limited FOV and anatomic landmarks
Why MR Imaging? • CT – Radiation – Iodinated contrast – Pitfalls due to poor opacification / mixing artifacts • Nephrogenic Systemic Fibrosis (NSF) – Increased indications for non-contrast MRV
MRV • Techniques – Dark Blood Imaging – Bright Blood Imaging – Gd-enhanced MRV • Clinical Applications – Chest – Abdomen – Pelvis
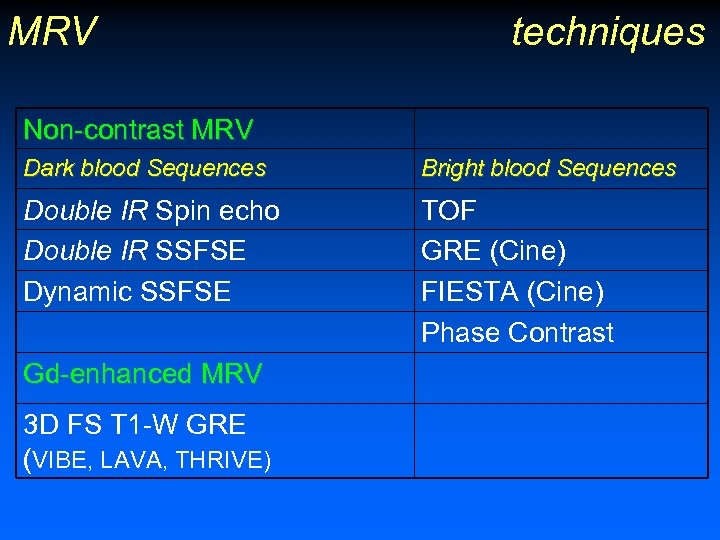
MRV techniques Non-contrast MRV Dark blood Sequences Bright blood Sequences Double IR Spin echo Double IR SSFSE Dynamic SSFSE TOF GRE (Cine) FIESTA (Cine) Phase Contrast Gd-enhanced MRV 3 D FS T 1 -W GRE (VIBE, LAVA, THRIVE)
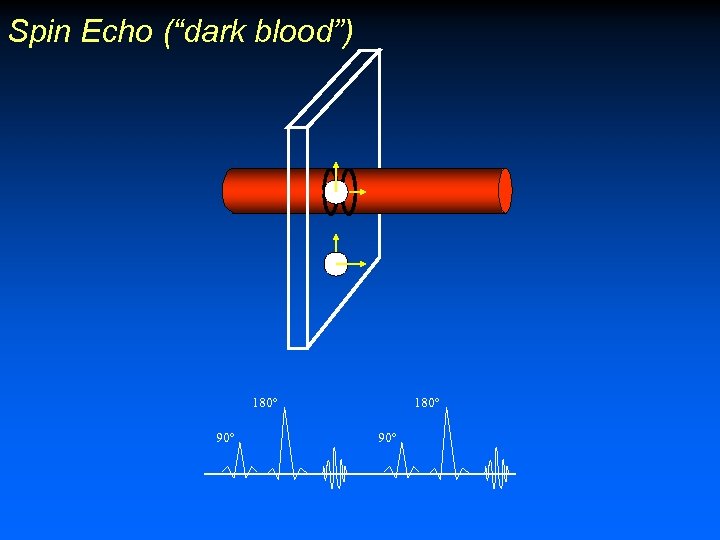
Spin Echo (“dark blood”) 180º 90º
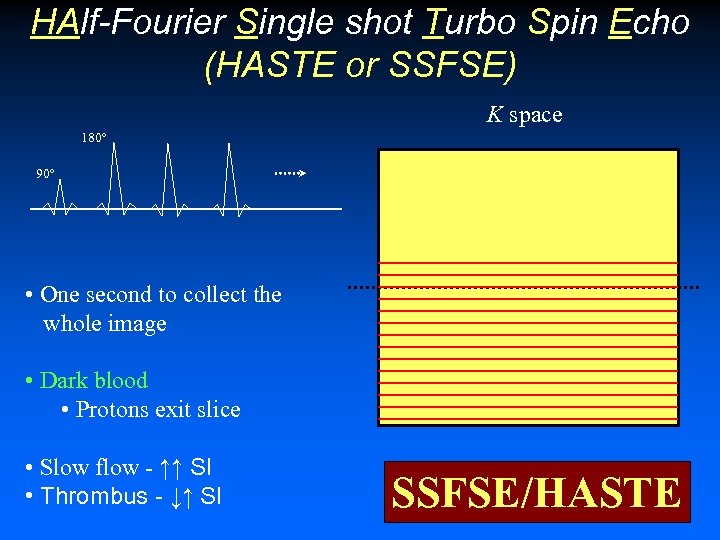
HAlf-Fourier Single shot Turbo Spin Echo (HASTE or SSFSE) K space 180º 90º • One second to collect the whole image • Dark blood • Protons exit slice • Slow flow - ↑↑ SI • Thrombus - ↓↑ SI SSFSE/HASTE
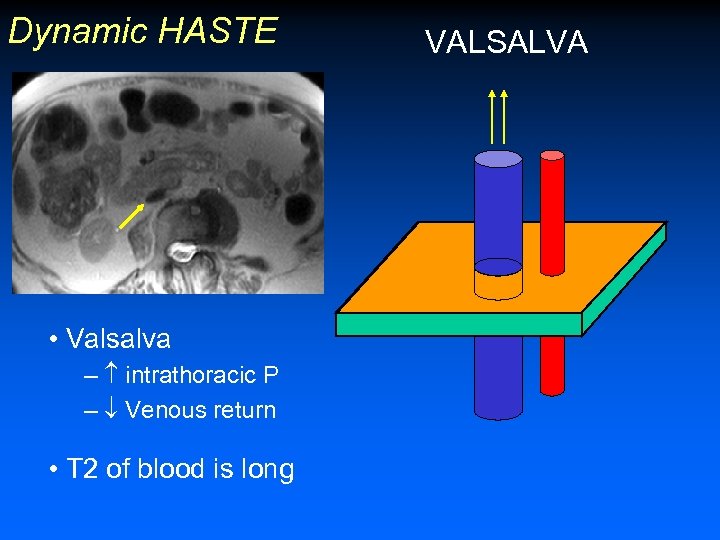
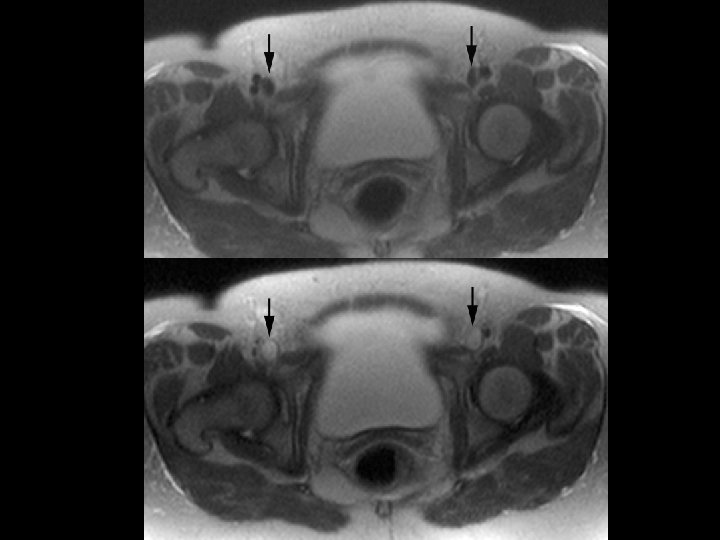
Dynamic HASTE • Intravascular signal void • Valsalva – intrathoracic P – Venous return • T 2 of blood is long VALSALVA
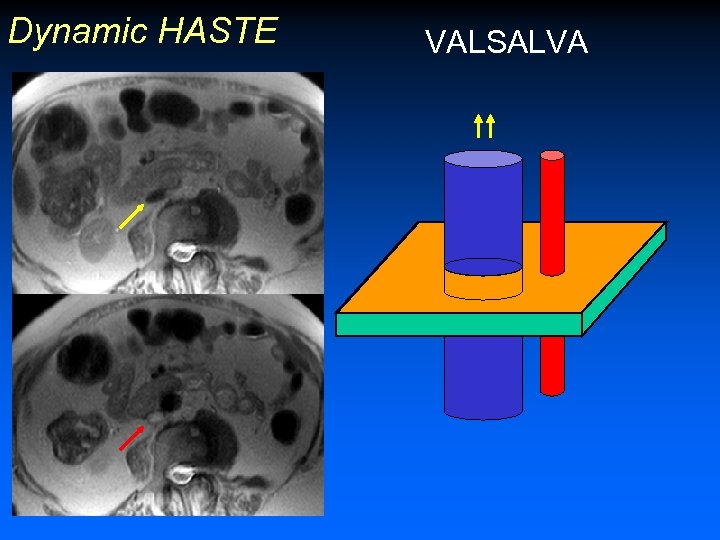
Dynamic HASTE • Valsalva – intrathoracic P – Venous return • T 2 of blood is long VALSALVA

DB HASTE (“dark blood”) 180º 90º TI 180º
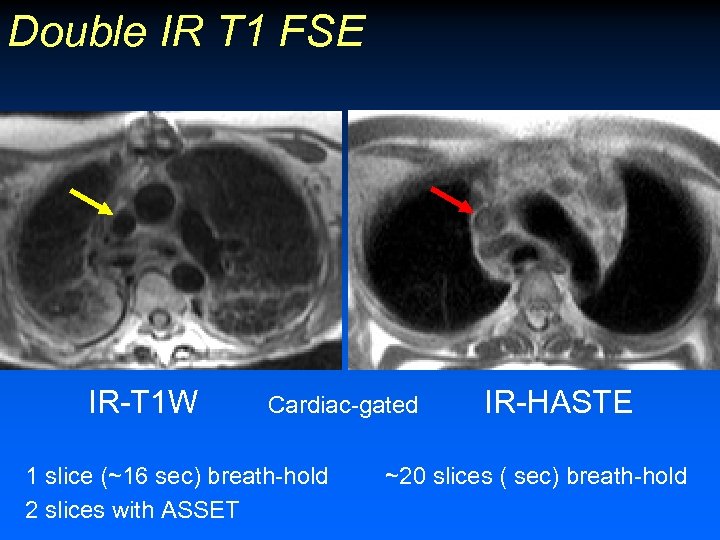
Double IR T 1 FSE IR-T 1 W Cardiac-gated 1 slice (~16 sec) breath-hold 2 slices with ASSET IR-HASTE ~20 slices ( sec) breath-hold
Bright blood Sequences • • TOF GRE (Cine) FIESTA (Cine) Phase Contrast
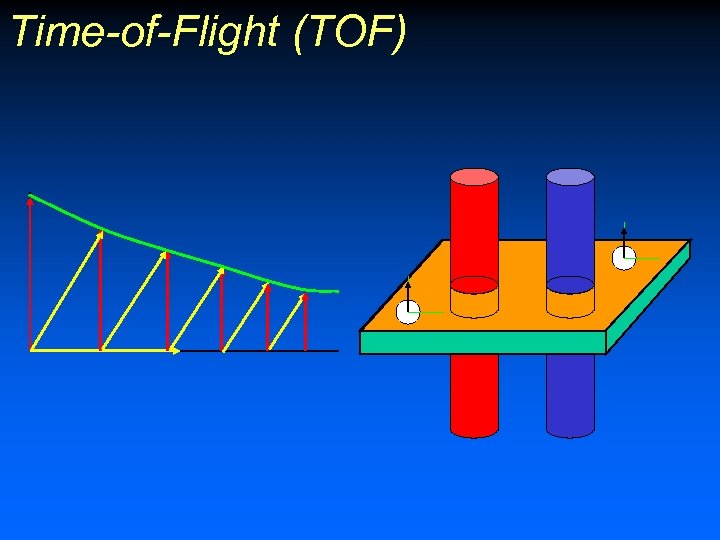
Time-of-Flight (TOF)
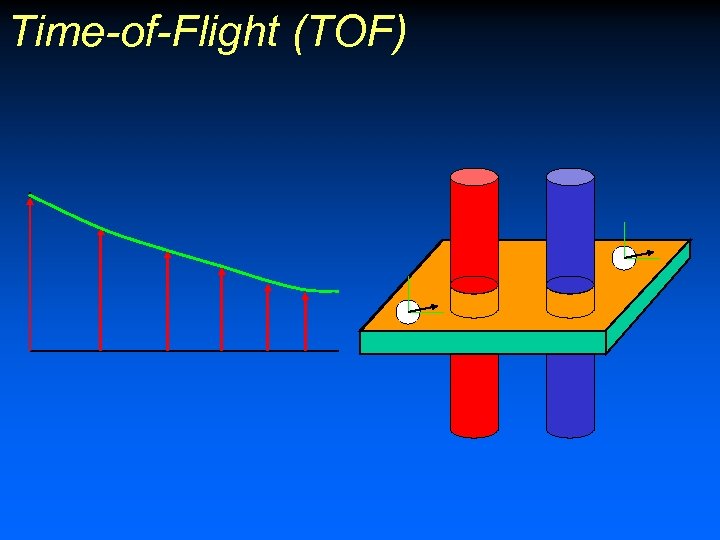
Time-of-Flight (TOF)
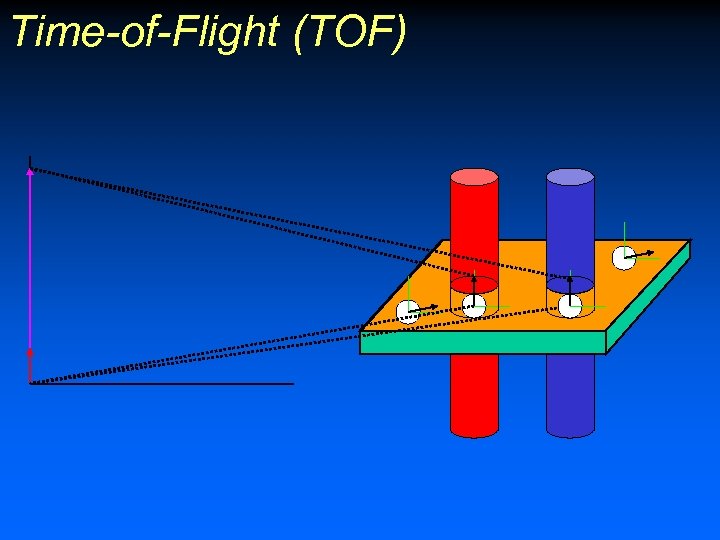
Time-of-Flight (TOF)
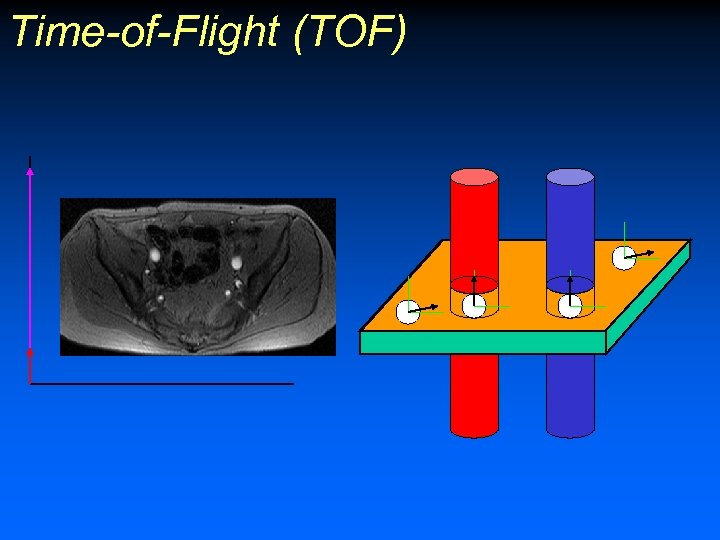
Time-of-Flight (TOF)
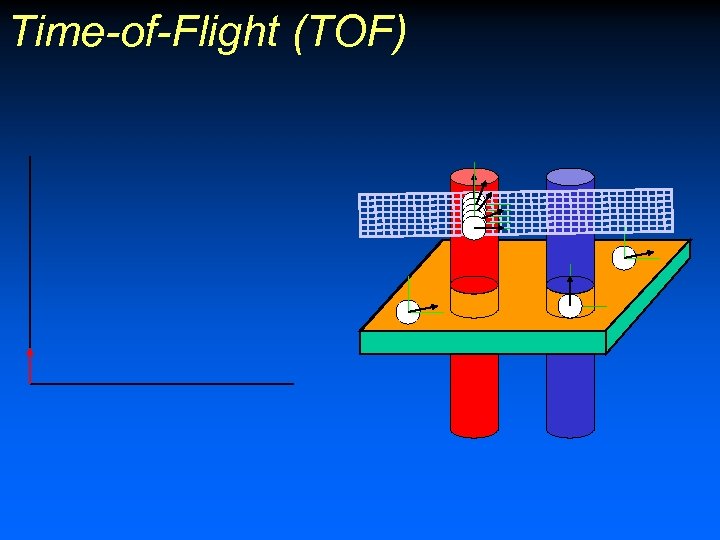
Time-of-Flight (TOF)
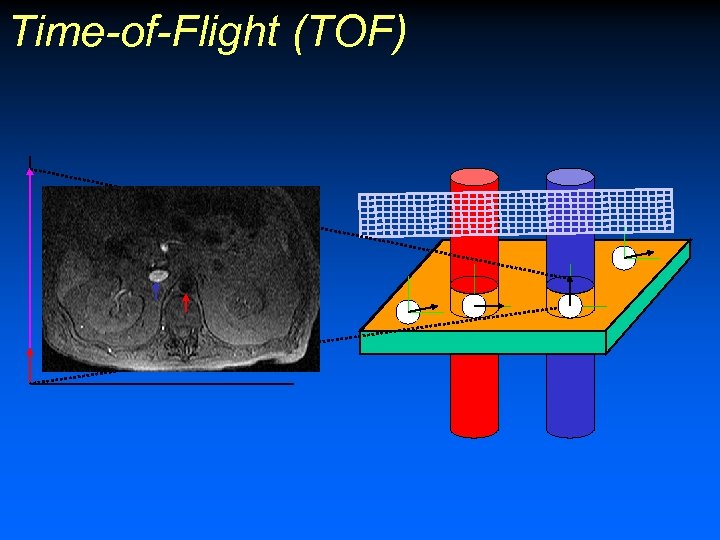
Time-of-Flight (TOF)
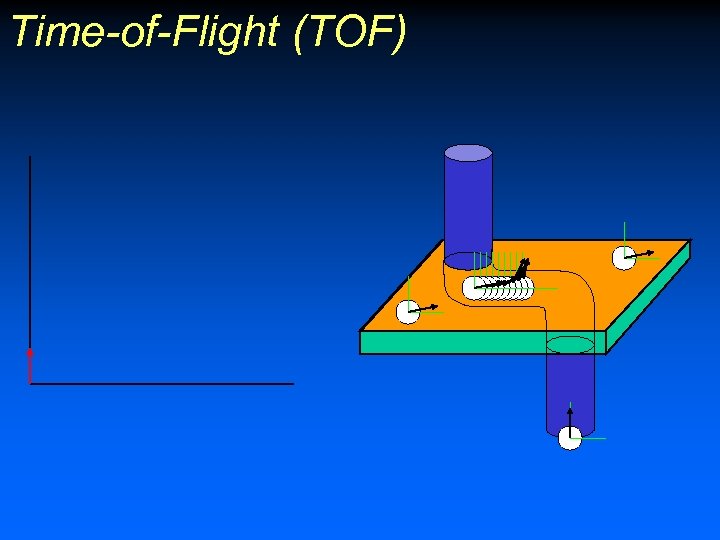
Time-of-Flight (TOF)
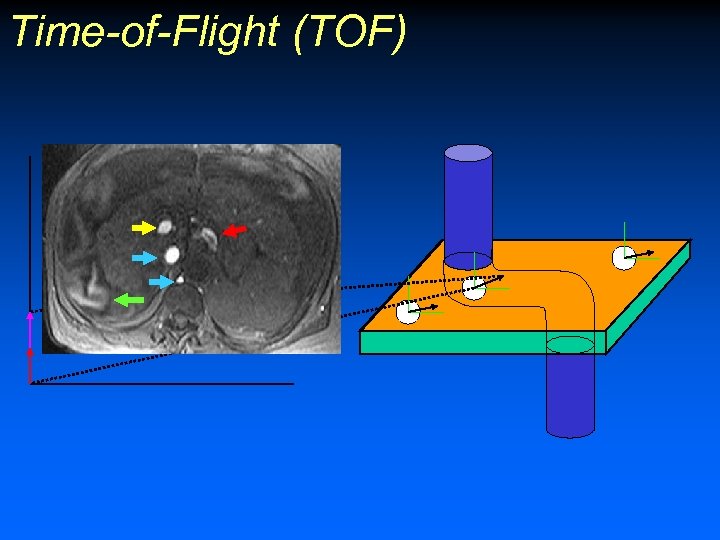
Time-of-Flight (TOF)

TOF
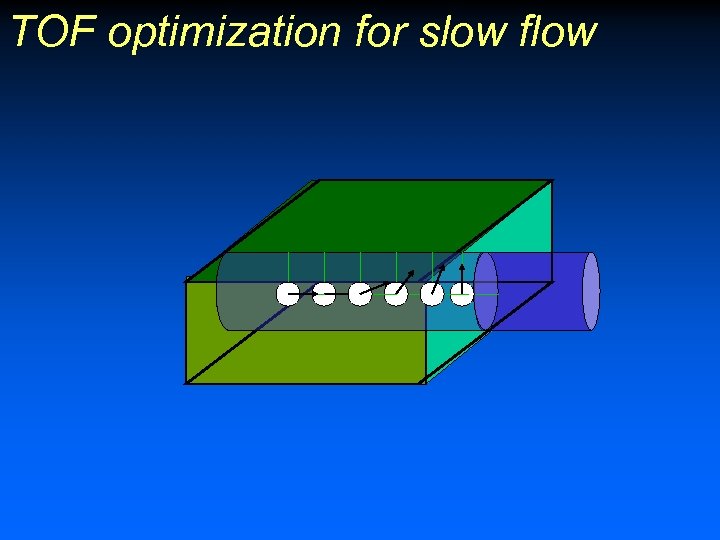
TOF optimization for slow flow
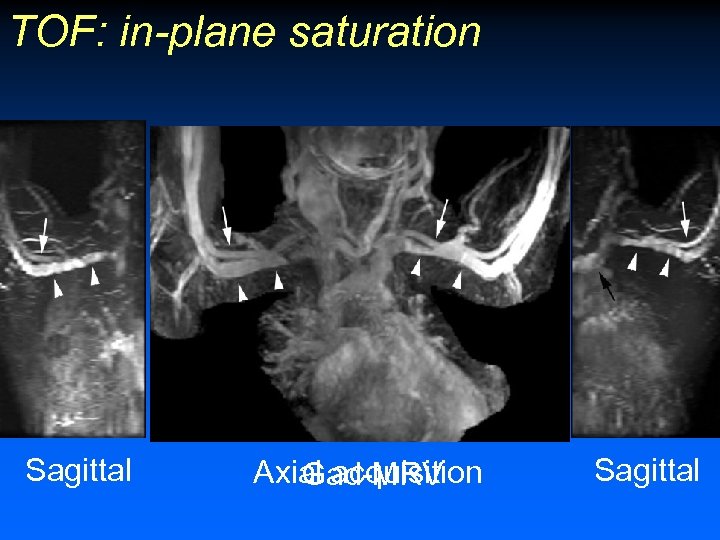
TOF: in-plane saturation Sagittal Axial acquisition Gad-MRV Sagittal

TOF optimization for slow flow • Slice perpendicular to vessel of interest • Decrease slice thickness • Cardiac gating? ECG Tracing Blood flow (Pulse Oximeter) Systole (arterial)
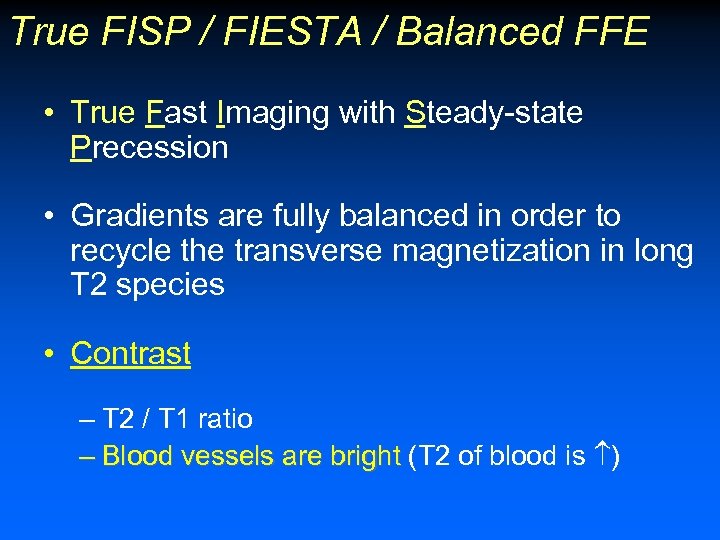
True FISP / FIESTA / Balanced FFE • True Fast Imaging with Steady-state Precession • Gradients are fully balanced in order to recycle the transverse magnetization in long T 2 species • Contrast – T 2 / T 1 ratio – Blood vessels are bright (T 2 of blood is )
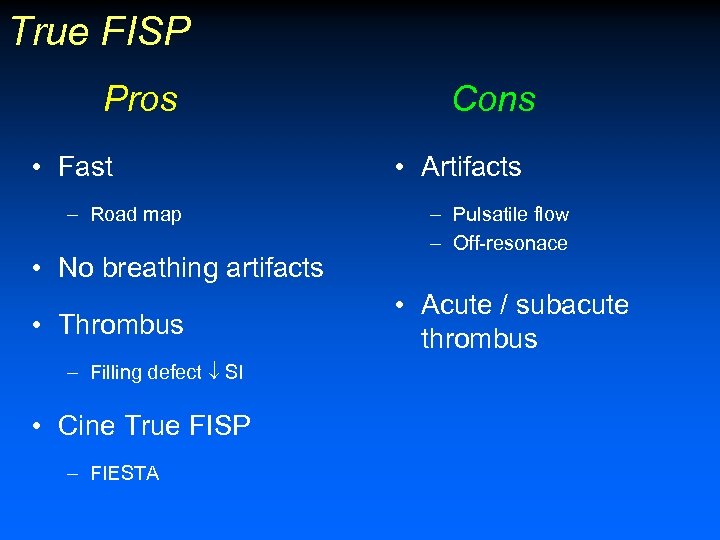
True FISP Pros • Fast – Road map • No breathing artifacts • Thrombus – Filling defect SI • Cine True FISP – FIESTA Cons • Artifacts – Pulsatile flow – Off-resonace • Acute / subacute thrombus
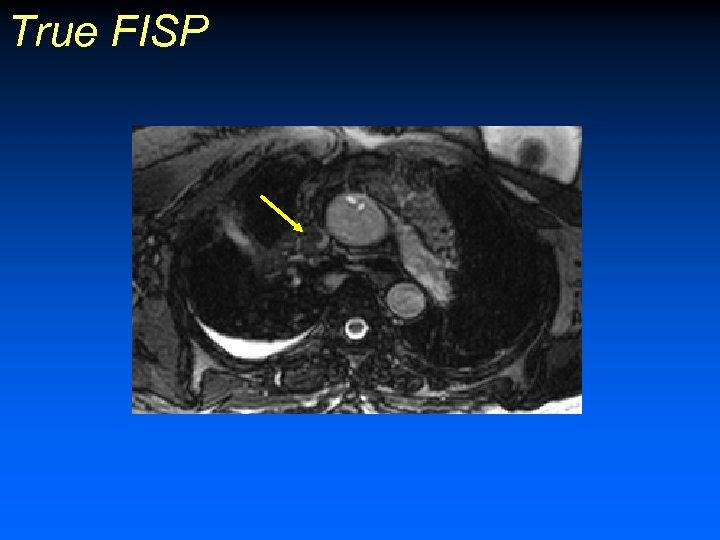
True FISP
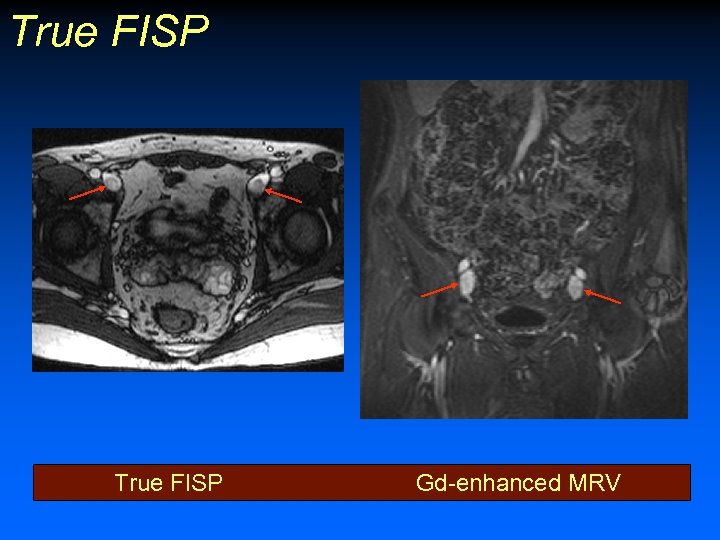
True FISP Gd-enhanced MRV
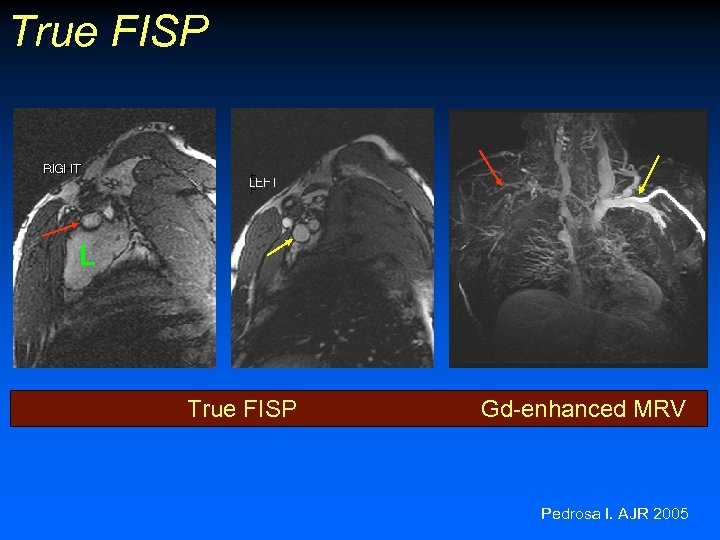
True FISP L True FISP Gd-enhanced MRV Pedrosa I. AJR 2005

Phase Contrast (PC) • 2 equal and opposite Venc gradients between the excitation and echo. • With stationary protons, phase shifts induced by the first gradient are reversed and canceled by the second gradient. • In moving protons, the second gradient does not quite cancel out phase shifts induced by the first gradient • These phase shifts are detected and proportional to the amount of motion in the direction of the encoding gradients
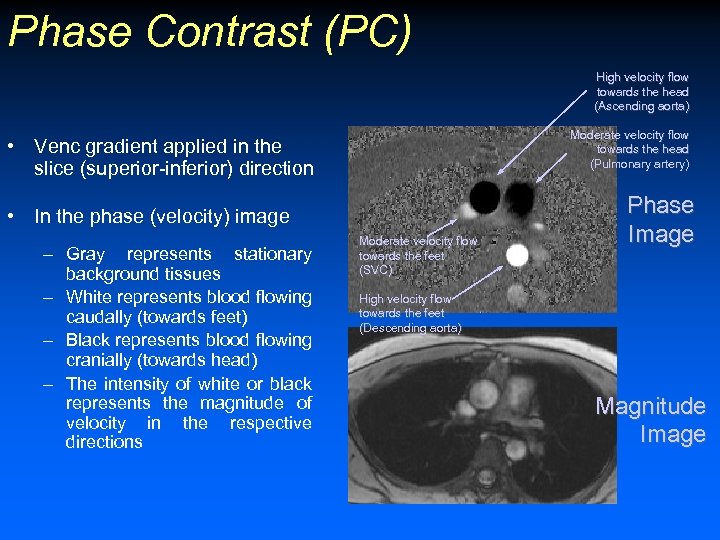
Phase Contrast (PC) High velocity flow towards the head (Ascending aorta) Moderate velocity flow towards the head (Pulmonary artery) • Venc gradient applied in the slice (superior-inferior) direction • In the phase (velocity) image – Gray represents stationary background tissues – White represents blood flowing caudally (towards feet) – Black represents blood flowing cranially (towards head) – The intensity of white or black represents the magnitude of velocity in the respective directions Moderate velocity flow towards the feet (SVC) Phase Image High velocity flow towards the feet (Descending aorta) Magnitude Image
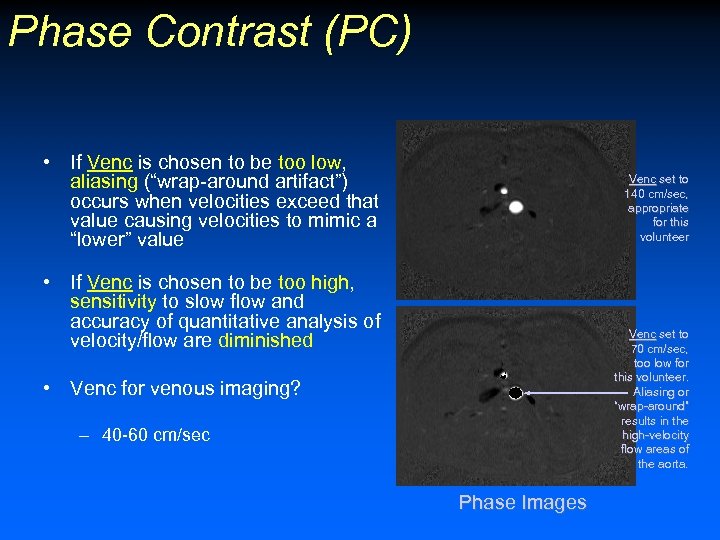
Phase Contrast (PC) • If Venc is chosen to be too low, aliasing (“wrap-around artifact”) occurs when velocities exceed that value causing velocities to mimic a “lower” value Venc set to 140 cm/sec, appropriate for this volunteer • If Venc is chosen to be too high, sensitivity to slow flow and accuracy of quantitative analysis of velocity/flow are diminished Venc set to 70 cm/sec, too low for this volunteer. Aliasing or “wrap-around” results in the high-velocity flow areas of the aorta. • Venc for venous imaging? – 40 -60 cm/sec Phase Images
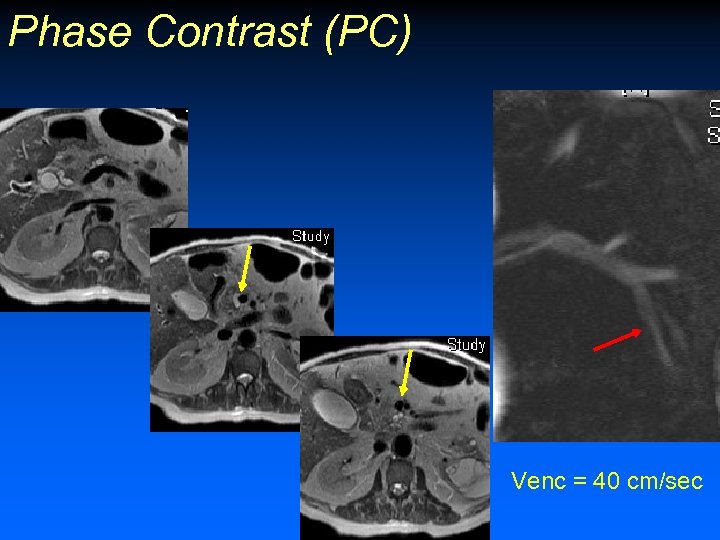
Phase Contrast (PC) Venc = 40 cm/sec
Phase Contrast (PC) 3 D PC
Gadolinium-enhanced MRV • Indirect MRV • Direct MRV
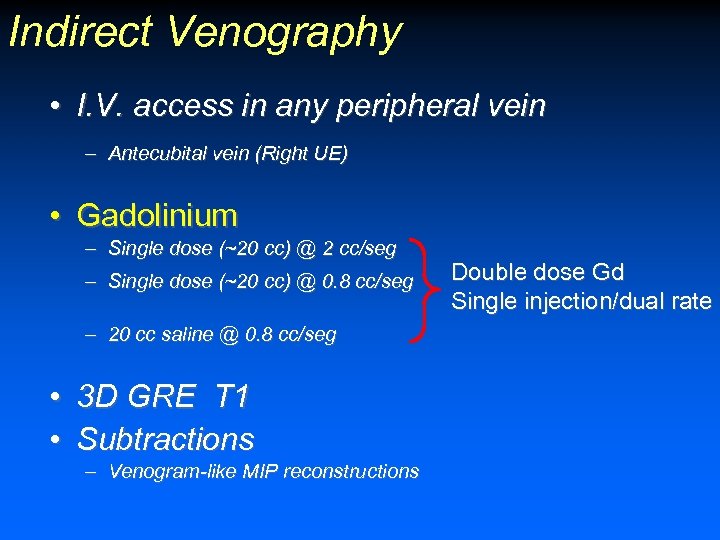
Indirect Venography • I. V. access in any peripheral vein – Antecubital vein (Right UE) • Gadolinium – Single dose (~20 cc) @ 2 cc/seg – Single dose (~20 cc) @ 0. 8 cc/seg – 20 cc saline @ 0. 8 cc/seg • 3 D GRE T 1 • Subtractions – Venogram-like MIP reconstructions Double dose Gd Single injection/dual rate
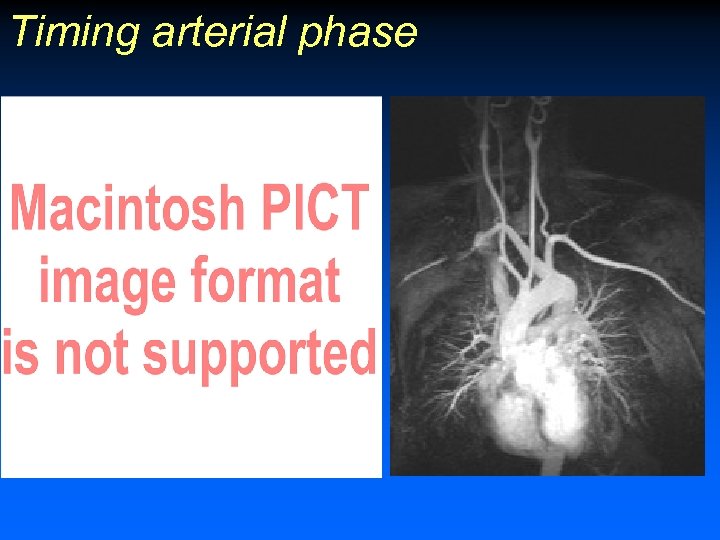
Timing arterial phase
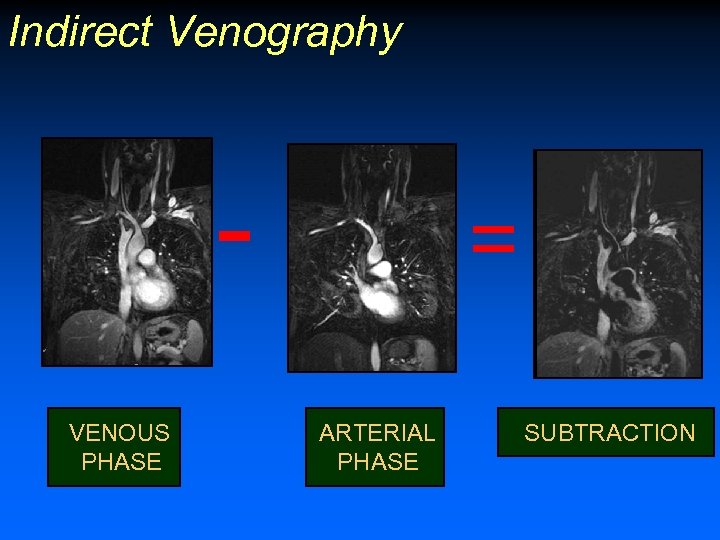
Indirect Venography VENOUS PHASE = ARTERIAL PHASE SUBTRACTION
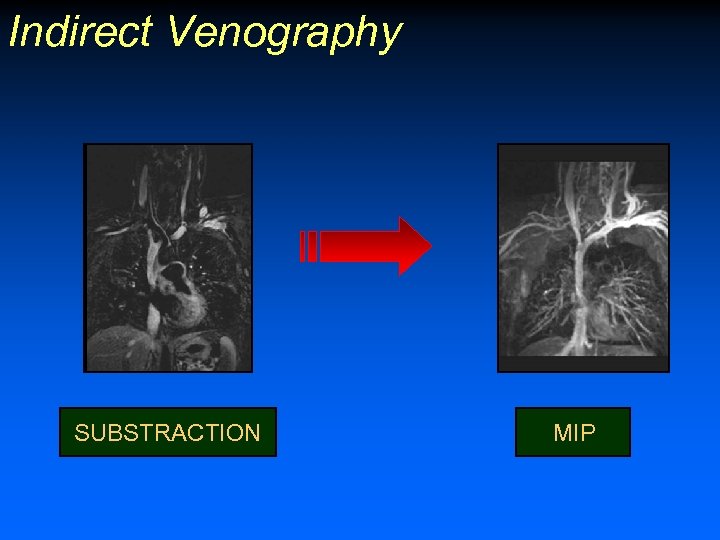
Indirect Venography SUBSTRACTION MIP

Direct Venography • I. V. access in affected extremity or bilateral • Gadolinium – 5 cc Gd in 100 cc saline (1: 20) • Tourniquet in lower extremities • 3 D GRE T 1 Li W et al. J Magn Reson Imaging 1998; 8(3): 630 -3
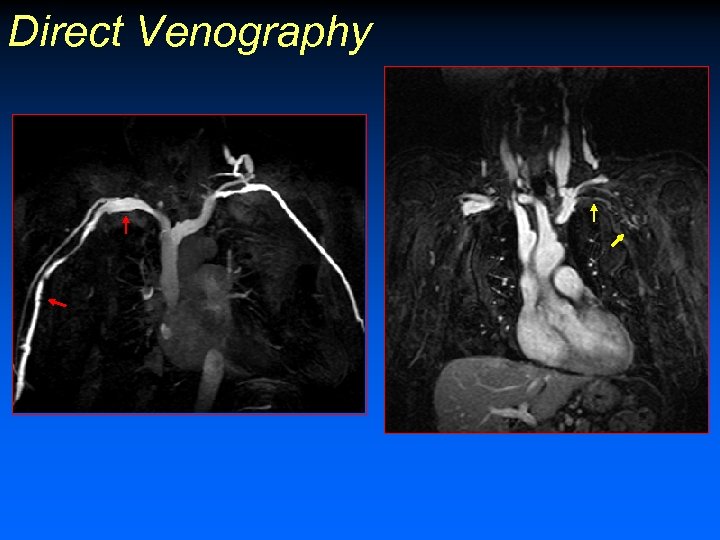
Direct Venography

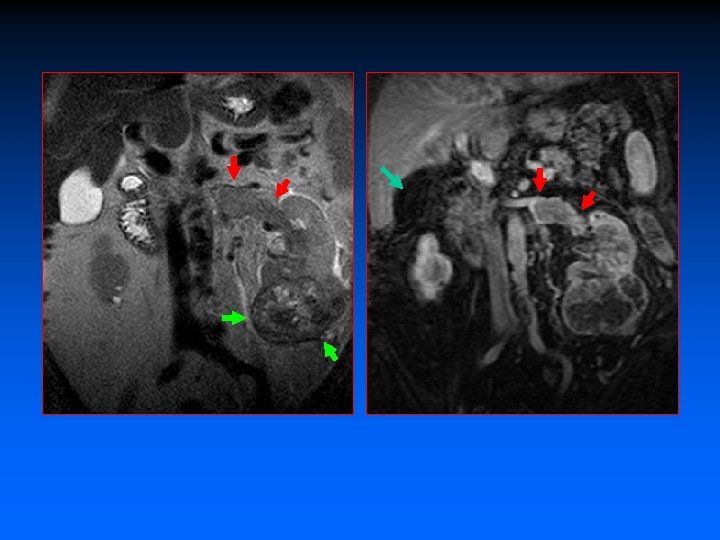
Thrombus Characterization – Bland thrombus No enhancement – Variable SI – – Tumor thrombus – Enhancement on Gd-MRV » Subtractions! » Absence of enhancement does NOT exclude tumor thrombus – SI on T 2 -weighted images

Tumor thrombus: Intravenous leiomyomatosis U
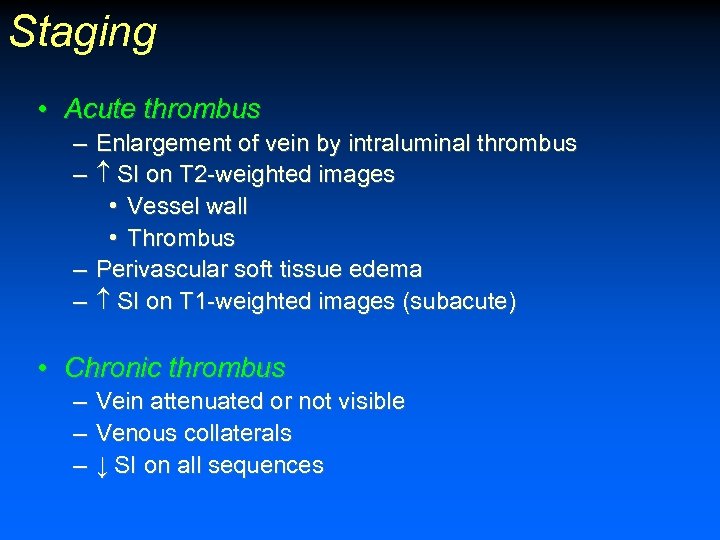
Staging • Acute thrombus – Enlargement of vein by intraluminal thrombus – SI on T 2 -weighted images • Vessel wall • Thrombus – Perivascular soft tissue edema – SI on T 1 -weighted images (subacute) • Chronic thrombus – Vein attenuated or not visible – Venous collaterals – ↓ SI on all sequences
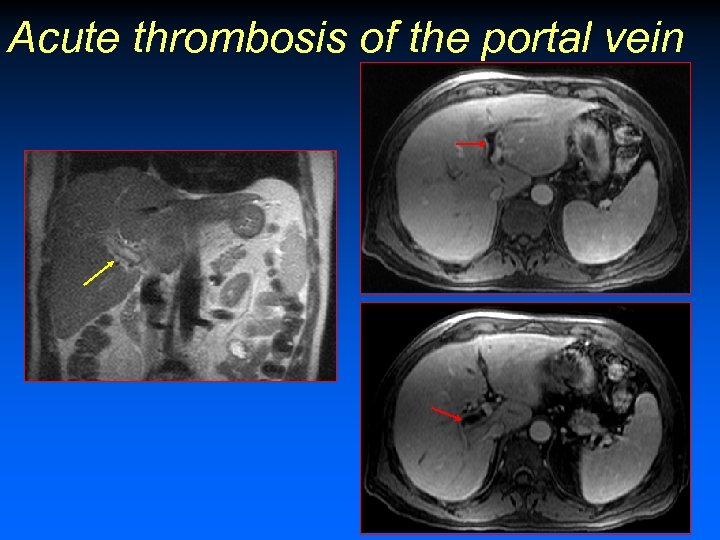
Acute thrombosis of the portal vein
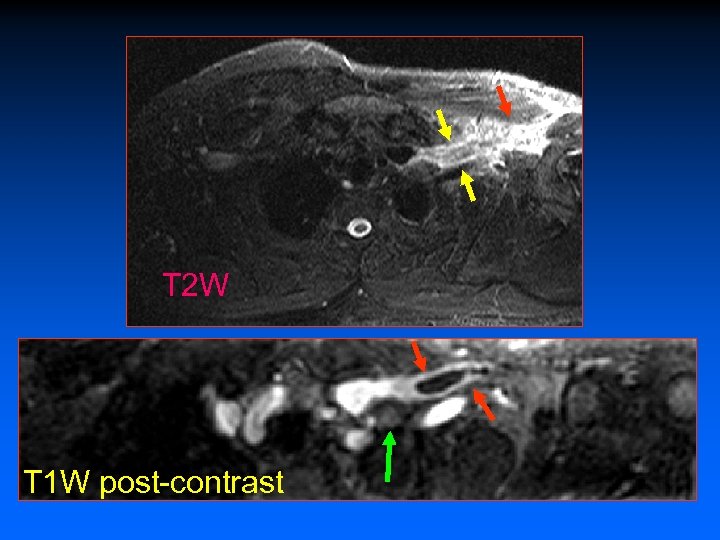
T 2 W T 1 W post-contrast
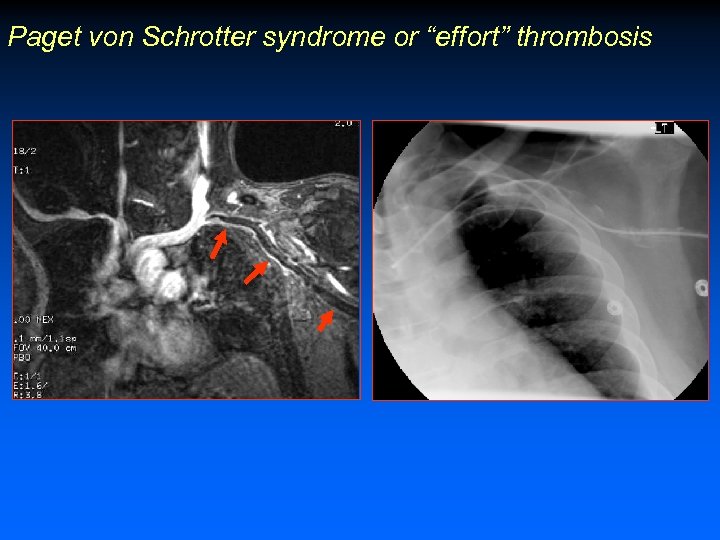
Paget von Schrotter syndrome or “effort” thrombosis

Chronic Thrombosis
Venous thrombosis Is the thrombosis acute or chronic? Do I need to anticoagulate this patient?
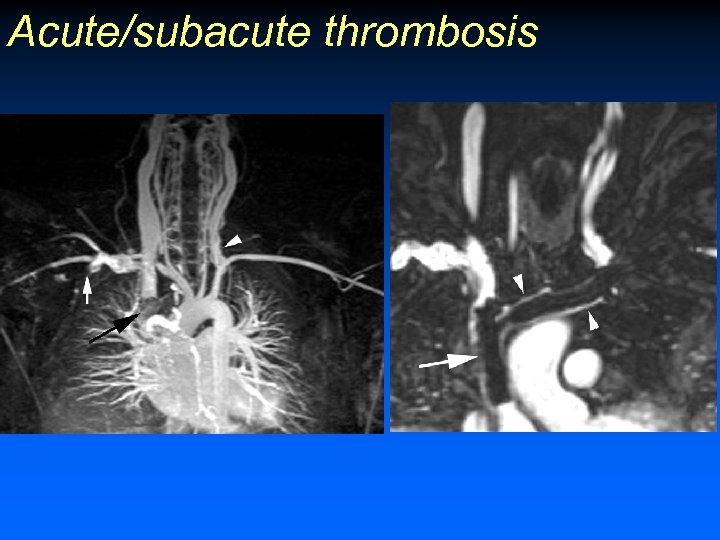
Acute/subacute thrombosis
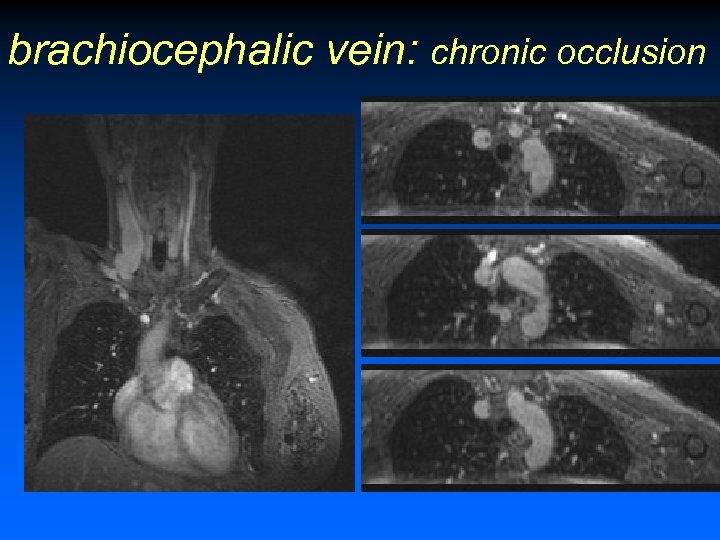
brachiocephalic vein: chronic occlusion
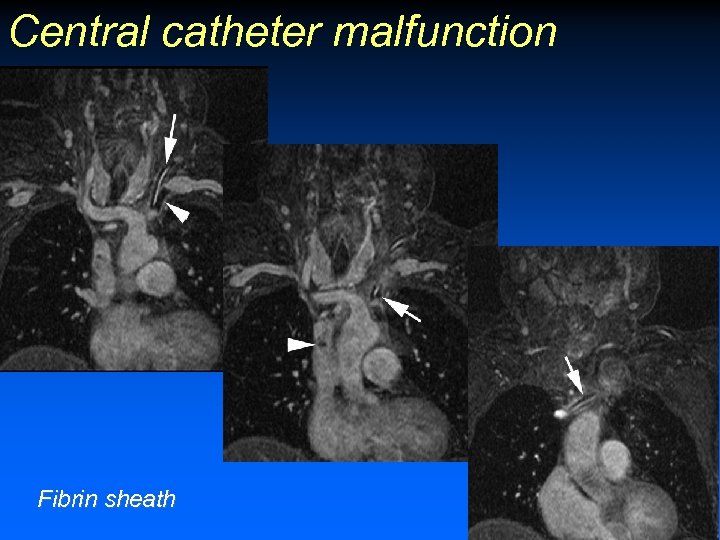
Central catheter malfunction Fibrin sheath
Clinical Indications
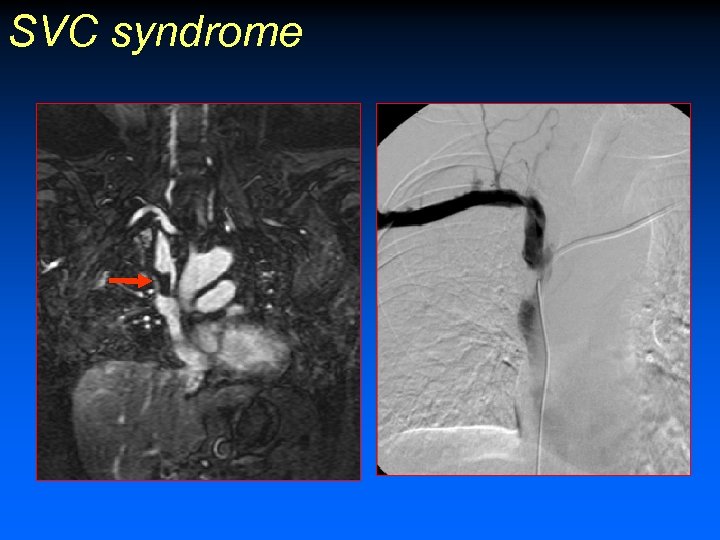
SVC syndrome
Venous Access • Central catheters – – Hemodyalisis Chemotherapy Parenteral nutrition Thrombosis in first 3 months (10%) • MRV chest – 15 pts with occlusion or stenosis central veins – Venous access possible in 14 pts Shinde TS et al. Radiology 1999; 213: 555 -560
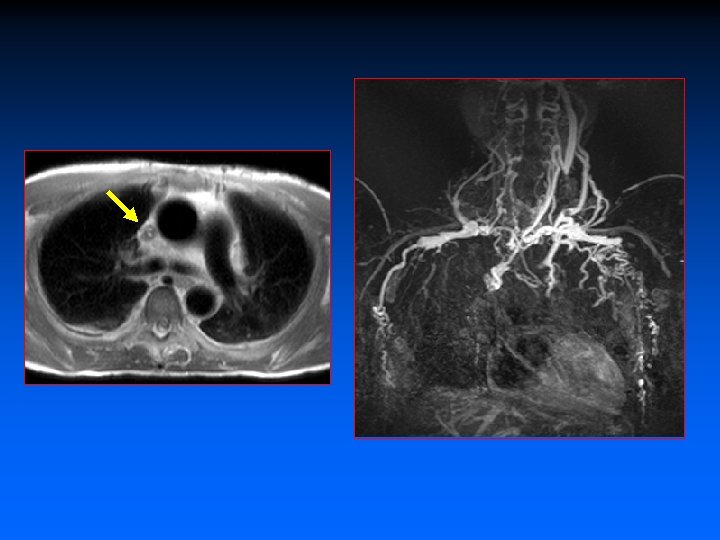

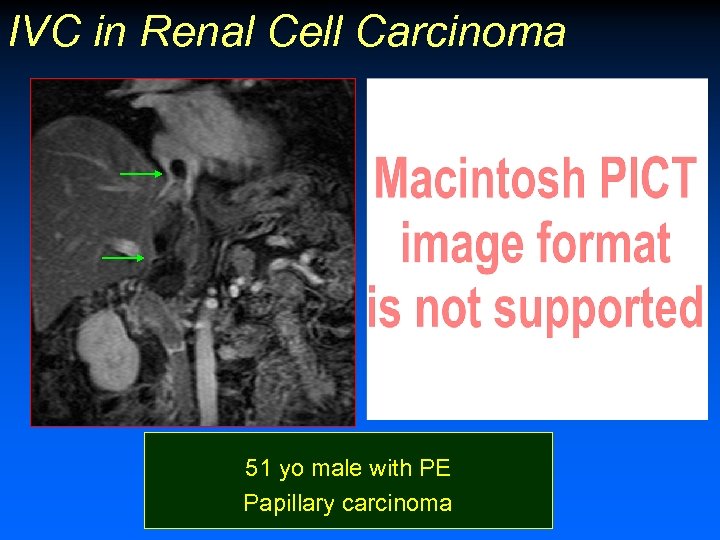
IVC in Renal Cell Carcinoma 51 yo male with PE Papillary carcinoma
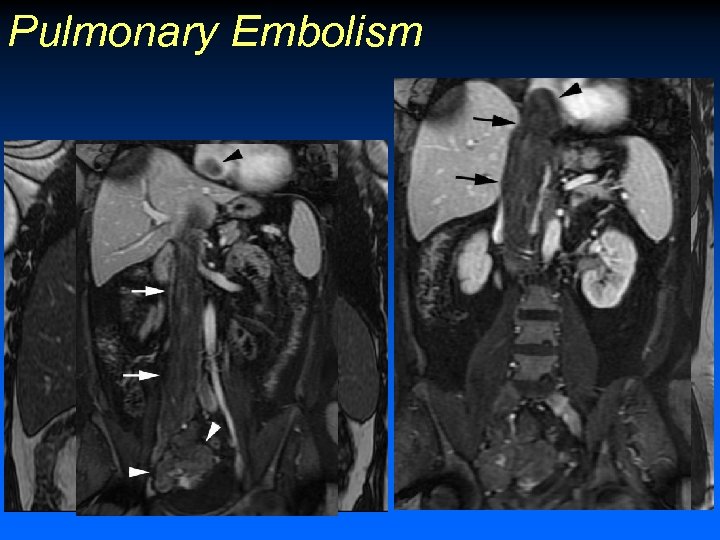
Pulmonary Embolism

Isolated Iliac Vein DVT


Conclusion • Central veins of the chest, abdomen and pelvis – Limited evaluation with US • Whole-body venous roadmap – Vascular access • Pregnancy
06b660804cfa4a5c4b36a99a2ad3462e.ppt