f1665747d9a766e6e119d8b1691ac730.ppt
- Количество слайдов: 63
 MOTOR SYSTEMS REVIEW Dr. G. R. Leichnetz
MOTOR SYSTEMS REVIEW Dr. G. R. Leichnetz
 Pyramidal System
Pyramidal System
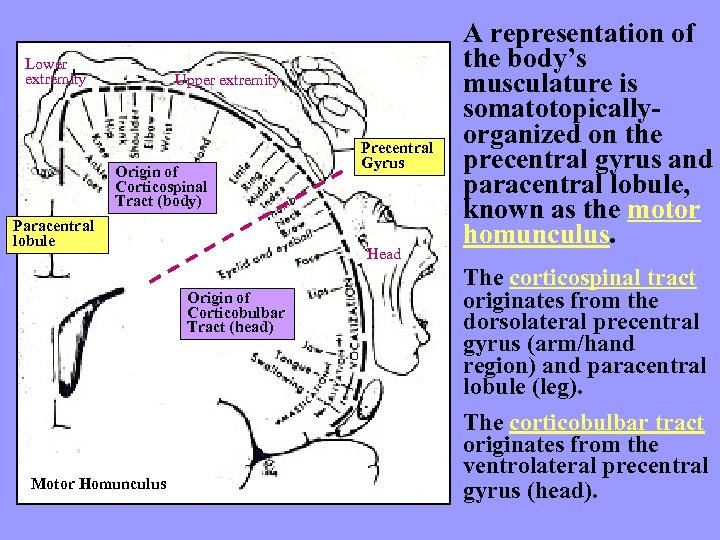 Lower extremity Upper extremity Origin of Corticospinal Tract (body) Paracentral lobule Head Origin of Corticobulbar Tract (head) Motor Homunculus Precentral Gyrus A representation of the body’s musculature is somatotopicallyorganized on the precentral gyrus and paracentral lobule, known as the motor homunculus. The corticospinal tract originates from the dorsolateral precentral gyrus (arm/hand region) and paracentral lobule (leg). The corticobulbar tract originates from the ventrolateral precentral gyrus (head).
Lower extremity Upper extremity Origin of Corticospinal Tract (body) Paracentral lobule Head Origin of Corticobulbar Tract (head) Motor Homunculus Precentral Gyrus A representation of the body’s musculature is somatotopicallyorganized on the precentral gyrus and paracentral lobule, known as the motor homunculus. The corticospinal tract originates from the dorsolateral precentral gyrus (arm/hand region) and paracentral lobule (leg). The corticobulbar tract originates from the ventrolateral precentral gyrus (head).
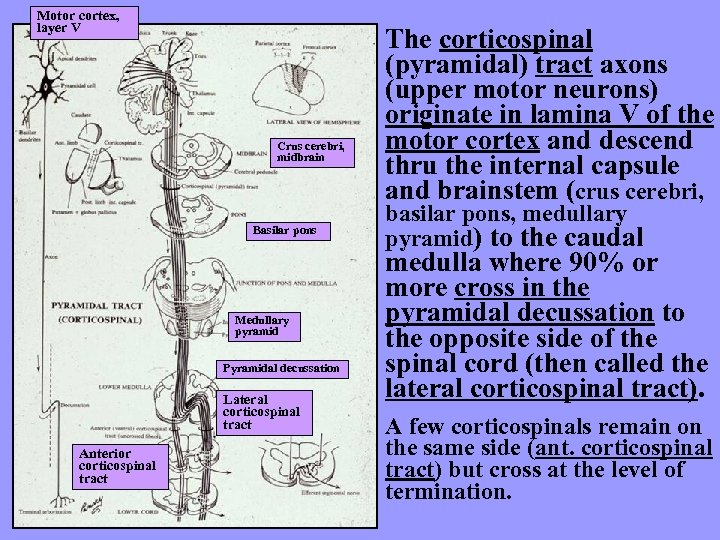 Motor cortex, layer V Crus cerebri, midbrain Basilar pons Medullary pyramid Pyramidal decussation Lateral corticospinal tract Anterior corticospinal tract The corticospinal (pyramidal) tract axons (upper motor neurons) originate in lamina V of the motor cortex and descend thru the internal capsule and brainstem (crus cerebri, basilar pons, medullary pyramid) to the caudal medulla where 90% or more cross in the pyramidal decussation to the opposite side of the spinal cord (then called the lateral corticospinal tract). A few corticospinals remain on the same side (ant. corticospinal tract) but cross at the level of termination.
Motor cortex, layer V Crus cerebri, midbrain Basilar pons Medullary pyramid Pyramidal decussation Lateral corticospinal tract Anterior corticospinal tract The corticospinal (pyramidal) tract axons (upper motor neurons) originate in lamina V of the motor cortex and descend thru the internal capsule and brainstem (crus cerebri, basilar pons, medullary pyramid) to the caudal medulla where 90% or more cross in the pyramidal decussation to the opposite side of the spinal cord (then called the lateral corticospinal tract). A few corticospinals remain on the same side (ant. corticospinal tract) but cross at the level of termination.
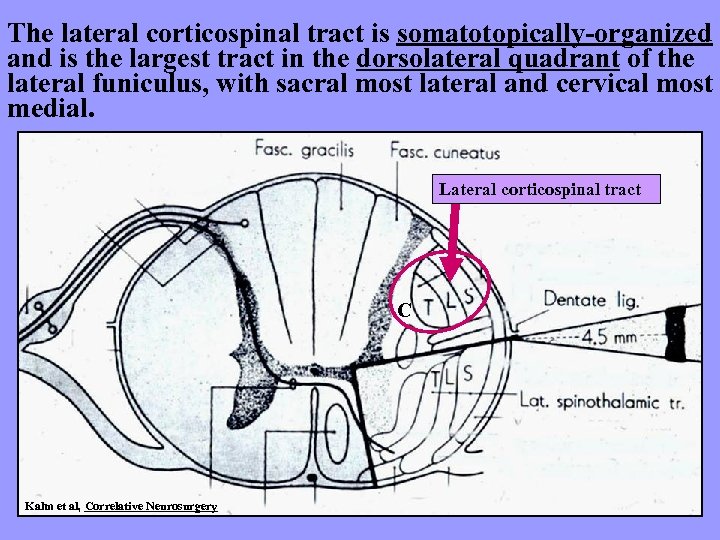 The lateral corticospinal tract is somatotopically-organized and is the largest tract in the dorsolateral quadrant of the lateral funiculus, with sacral most lateral and cervical most medial. Lateral corticospinal tract C Kahn et al, Correlative Neurosurgery
The lateral corticospinal tract is somatotopically-organized and is the largest tract in the dorsolateral quadrant of the lateral funiculus, with sacral most lateral and cervical most medial. Lateral corticospinal tract C Kahn et al, Correlative Neurosurgery
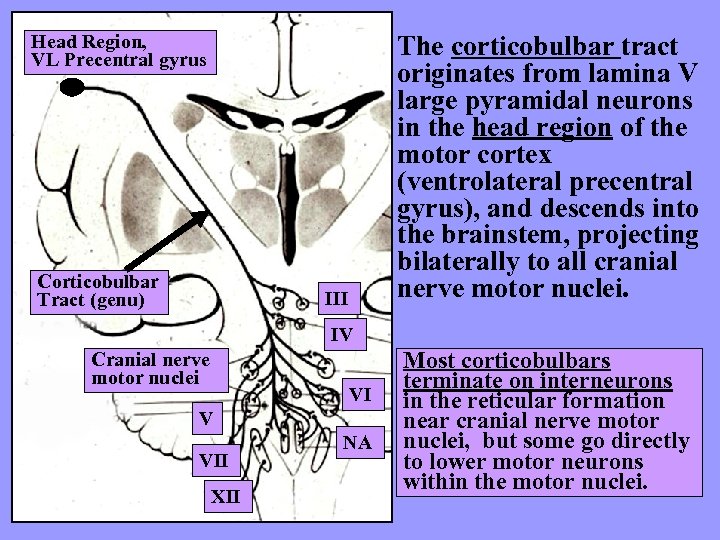 Head Region, VL Precentral gyrus Corticobulbar Tract (genu) The corticobulbar tract originates from lamina V large pyramidal neurons in the head region of the motor cortex (ventrolateral precentral gyrus), and descends into the brainstem, projecting bilaterally to all cranial nerve motor nuclei. III IV Cranial nerve motor nuclei VI V VII XII NA Most corticobulbars terminate on interneurons in the reticular formation near cranial nerve motor nuclei, but some go directly to lower motor neurons within the motor nuclei.
Head Region, VL Precentral gyrus Corticobulbar Tract (genu) The corticobulbar tract originates from lamina V large pyramidal neurons in the head region of the motor cortex (ventrolateral precentral gyrus), and descends into the brainstem, projecting bilaterally to all cranial nerve motor nuclei. III IV Cranial nerve motor nuclei VI V VII XII NA Most corticobulbars terminate on interneurons in the reticular formation near cranial nerve motor nuclei, but some go directly to lower motor neurons within the motor nuclei.
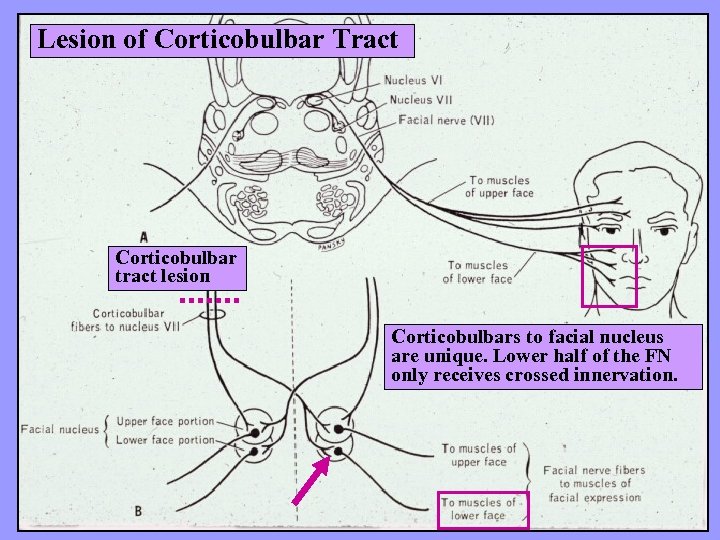 Lesion of Corticobulbar Tract Corticobulbar tract lesion Corticobulbars to facial nucleus are unique. Lower half of the FN only receives crossed innervation.
Lesion of Corticobulbar Tract Corticobulbar tract lesion Corticobulbars to facial nucleus are unique. Lower half of the FN only receives crossed innervation.
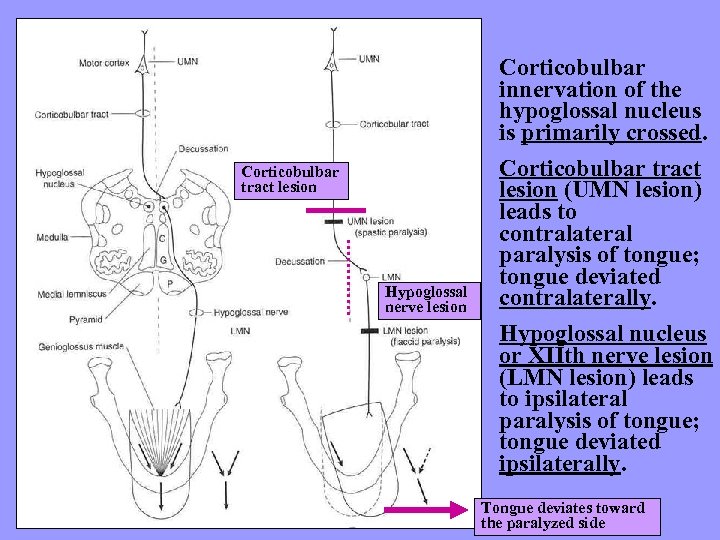 Corticobulbar tract lesion Hypoglossal nerve lesion Corticobulbar innervation of the hypoglossal nucleus is primarily crossed. Corticobulbar tract lesion (UMN lesion) leads to contralateral paralysis of tongue; tongue deviated contralaterally. Hypoglossal nucleus or XIIth nerve lesion (LMN lesion) leads to ipsilateral paralysis of tongue; tongue deviated ipsilaterally. Tongue deviates toward the paralyzed side
Corticobulbar tract lesion Hypoglossal nerve lesion Corticobulbar innervation of the hypoglossal nucleus is primarily crossed. Corticobulbar tract lesion (UMN lesion) leads to contralateral paralysis of tongue; tongue deviated contralaterally. Hypoglossal nucleus or XIIth nerve lesion (LMN lesion) leads to ipsilateral paralysis of tongue; tongue deviated ipsilaterally. Tongue deviates toward the paralyzed side
 Pyramidal Lesions
Pyramidal Lesions
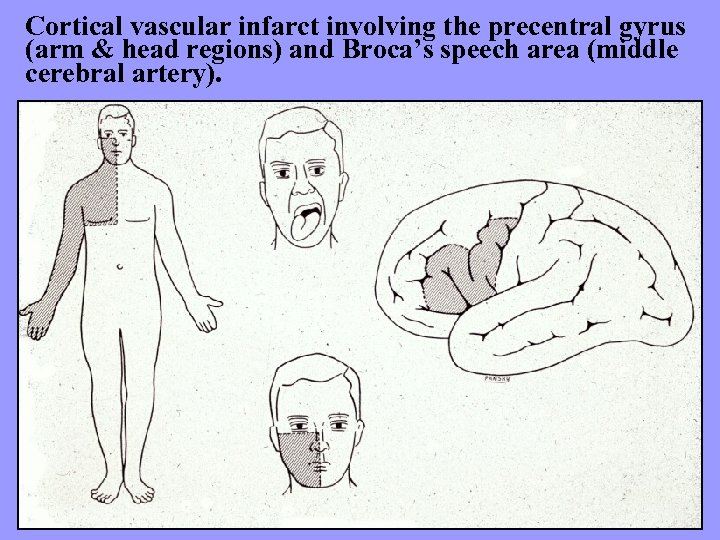 Cortical vascular infarct involving the precentral gyrus (arm & head regions) and Broca’s speech area (middle cerebral artery).
Cortical vascular infarct involving the precentral gyrus (arm & head regions) and Broca’s speech area (middle cerebral artery).
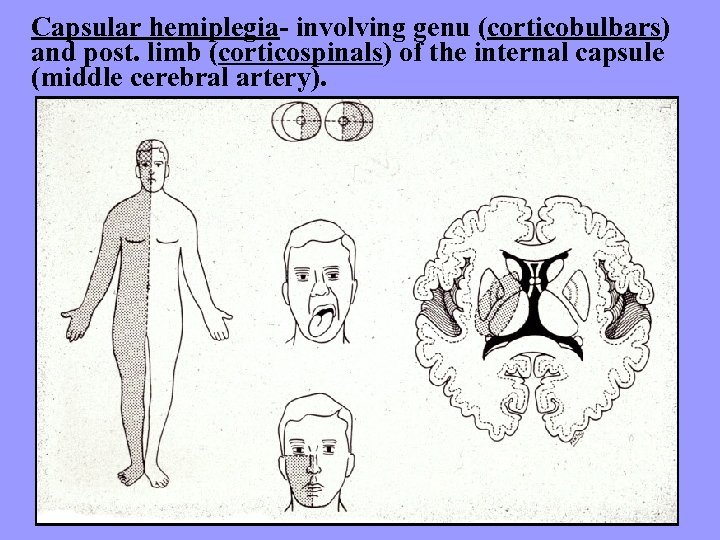 Capsular hemiplegia- involving genu (corticobulbars) and post. limb (corticospinals) of the internal capsule (middle cerebral artery).
Capsular hemiplegia- involving genu (corticobulbars) and post. limb (corticospinals) of the internal capsule (middle cerebral artery).
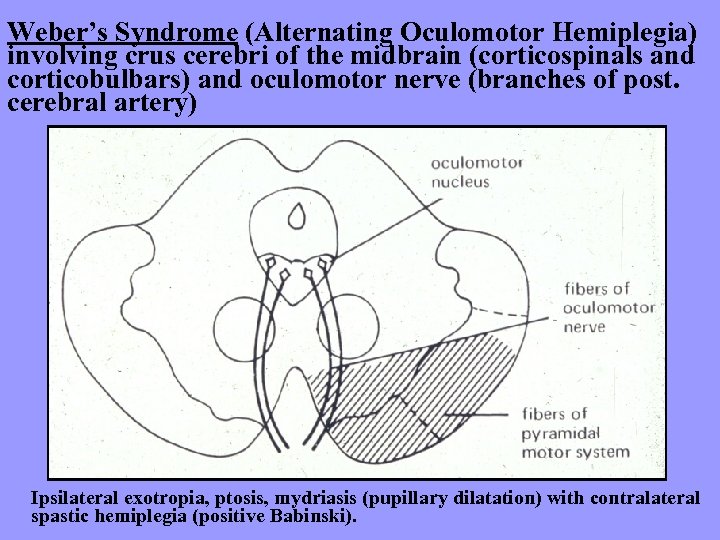 Weber’s Syndrome (Alternating Oculomotor Hemiplegia) involving crus cerebri of the midbrain (corticospinals and corticobulbars) and oculomotor nerve (branches of post. cerebral artery) Ipsilateral exotropia, ptosis, mydriasis (pupillary dilatation) with contralateral spastic hemiplegia (positive Babinski).
Weber’s Syndrome (Alternating Oculomotor Hemiplegia) involving crus cerebri of the midbrain (corticospinals and corticobulbars) and oculomotor nerve (branches of post. cerebral artery) Ipsilateral exotropia, ptosis, mydriasis (pupillary dilatation) with contralateral spastic hemiplegia (positive Babinski).
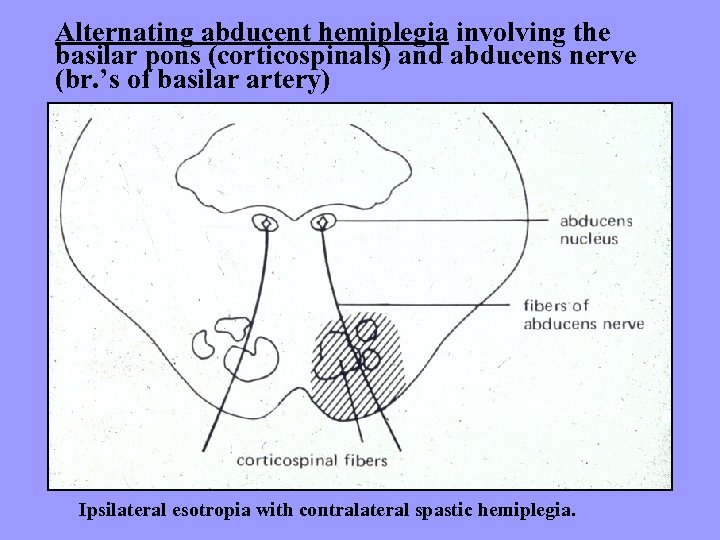 Alternating abducent hemiplegia involving the basilar pons (corticospinals) and abducens nerve (br. ’s of basilar artery) Ipsilateral esotropia with contralateral spastic hemiplegia.
Alternating abducent hemiplegia involving the basilar pons (corticospinals) and abducens nerve (br. ’s of basilar artery) Ipsilateral esotropia with contralateral spastic hemiplegia.
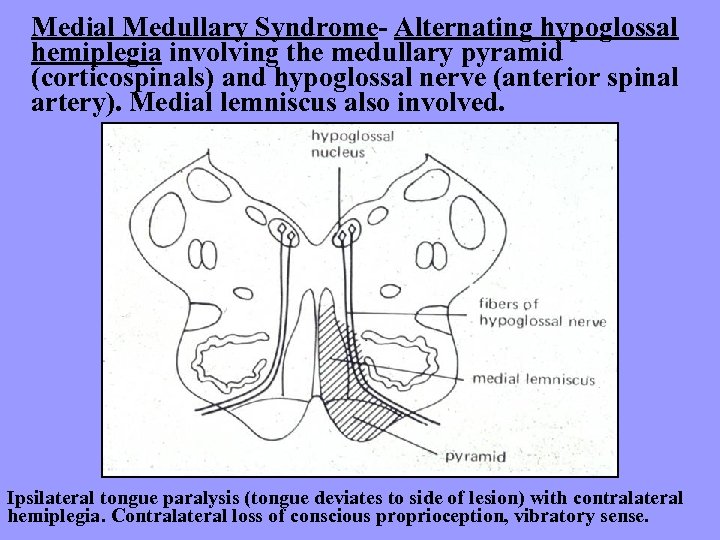 Medial Medullary Syndrome- Alternating hypoglossal hemiplegia involving the medullary pyramid (corticospinals) and hypoglossal nerve (anterior spinal artery). Medial lemniscus also involved. Ipsilateral tongue paralysis (tongue deviates to side of lesion) with contralateral hemiplegia. Contralateral loss of conscious proprioception, vibratory sense.
Medial Medullary Syndrome- Alternating hypoglossal hemiplegia involving the medullary pyramid (corticospinals) and hypoglossal nerve (anterior spinal artery). Medial lemniscus also involved. Ipsilateral tongue paralysis (tongue deviates to side of lesion) with contralateral hemiplegia. Contralateral loss of conscious proprioception, vibratory sense.
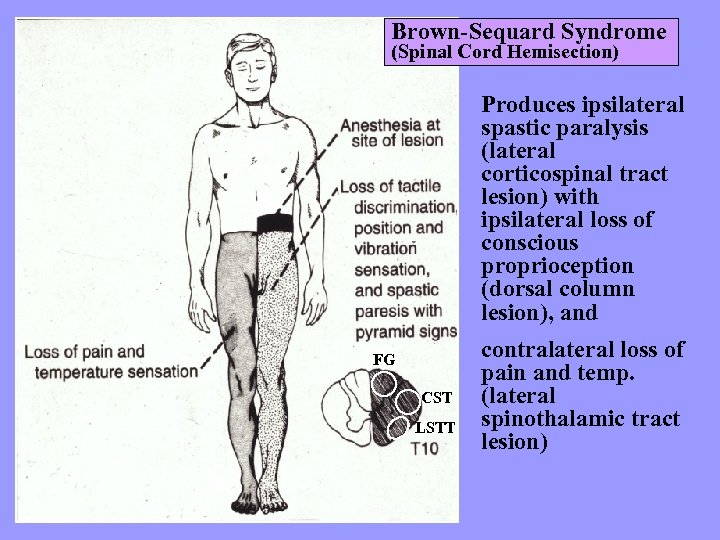 Brown-Sequard Syndrome (Spinal Cord Hemisection) Produces ipsilateral spastic paralysis (lateral corticospinal tract lesion) with ipsilateral loss of conscious proprioception (dorsal column lesion), and FG CST LSTT contralateral loss of pain and temp. (lateral spinothalamic tract lesion)
Brown-Sequard Syndrome (Spinal Cord Hemisection) Produces ipsilateral spastic paralysis (lateral corticospinal tract lesion) with ipsilateral loss of conscious proprioception (dorsal column lesion), and FG CST LSTT contralateral loss of pain and temp. (lateral spinothalamic tract lesion)
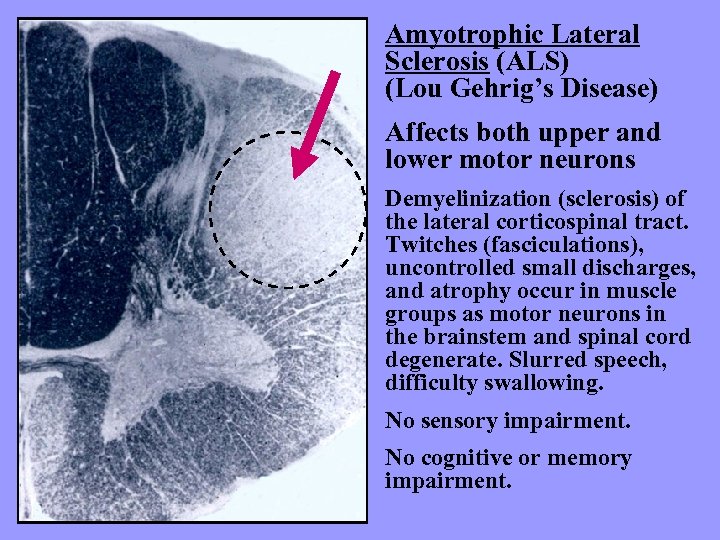 Amyotrophic Lateral Sclerosis (ALS) (Lou Gehrig’s Disease) Affects both upper and lower motor neurons Demyelinization (sclerosis) of the lateral corticospinal tract. Twitches (fasciculations), uncontrolled small discharges, and atrophy occur in muscle groups as motor neurons in the brainstem and spinal cord degenerate. Slurred speech, difficulty swallowing. No sensory impairment. No cognitive or memory impairment.
Amyotrophic Lateral Sclerosis (ALS) (Lou Gehrig’s Disease) Affects both upper and lower motor neurons Demyelinization (sclerosis) of the lateral corticospinal tract. Twitches (fasciculations), uncontrolled small discharges, and atrophy occur in muscle groups as motor neurons in the brainstem and spinal cord degenerate. Slurred speech, difficulty swallowing. No sensory impairment. No cognitive or memory impairment.
 Poliomyelitis (LMN lesion of the anterior horn motor neurons of the spinal cord) produces an ipsilateral flaccid paralysis with hypotonia, hyporeflexia and atrophy.
Poliomyelitis (LMN lesion of the anterior horn motor neurons of the spinal cord) produces an ipsilateral flaccid paralysis with hypotonia, hyporeflexia and atrophy.
 Oculomotor System
Oculomotor System
 Types of Eye Movements Conjugate Vestibulo-ocular (VOR) Saccades- voluntary (FEF) and reflexive (SC) Smooth Pursuit- tracking Optokinetic- moving visual scene Disconjugate Convergence- “near response”
Types of Eye Movements Conjugate Vestibulo-ocular (VOR) Saccades- voluntary (FEF) and reflexive (SC) Smooth Pursuit- tracking Optokinetic- moving visual scene Disconjugate Convergence- “near response”
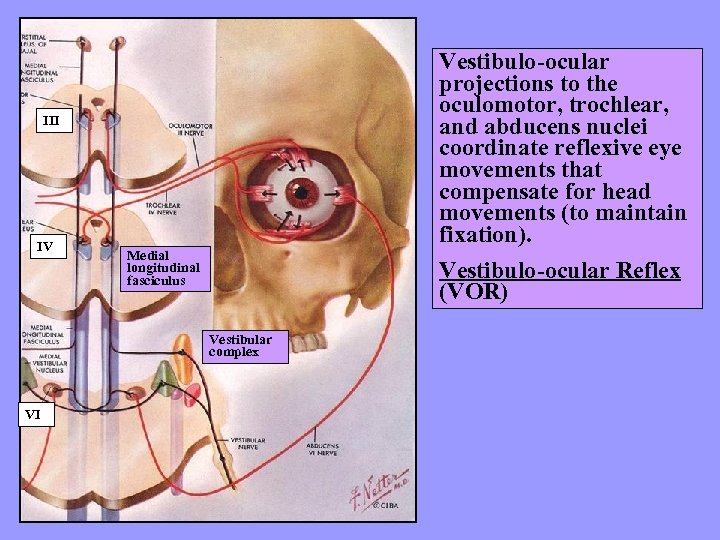 Vestibulo-ocular projections to the oculomotor, trochlear, and abducens nuclei coordinate reflexive eye movements that compensate for head movements (to maintain fixation). Vestibulo-ocular Reflex (VOR) III IV Medial longitudinal fasciculus Vestibular complex VI
Vestibulo-ocular projections to the oculomotor, trochlear, and abducens nuclei coordinate reflexive eye movements that compensate for head movements (to maintain fixation). Vestibulo-ocular Reflex (VOR) III IV Medial longitudinal fasciculus Vestibular complex VI
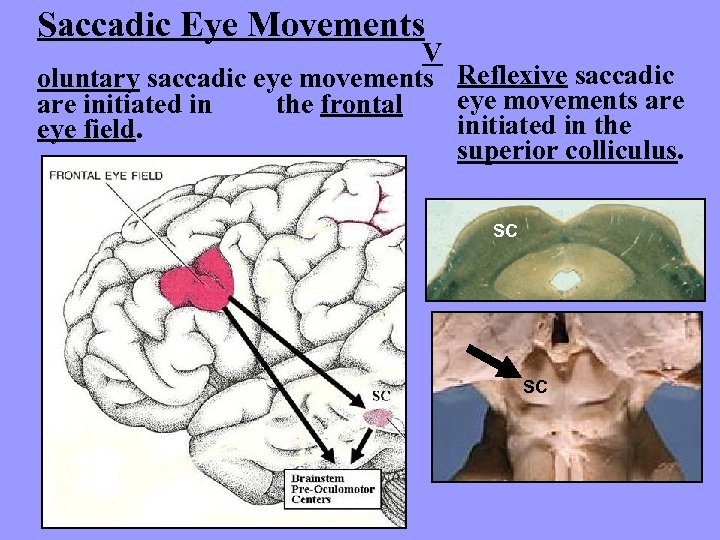 Saccadic Eye Movements V oluntary saccadic eye movements Reflexive saccadic eye movements are initiated in the frontal initiated in the eye field. superior colliculus. SC SC
Saccadic Eye Movements V oluntary saccadic eye movements Reflexive saccadic eye movements are initiated in the frontal initiated in the eye field. superior colliculus. SC SC
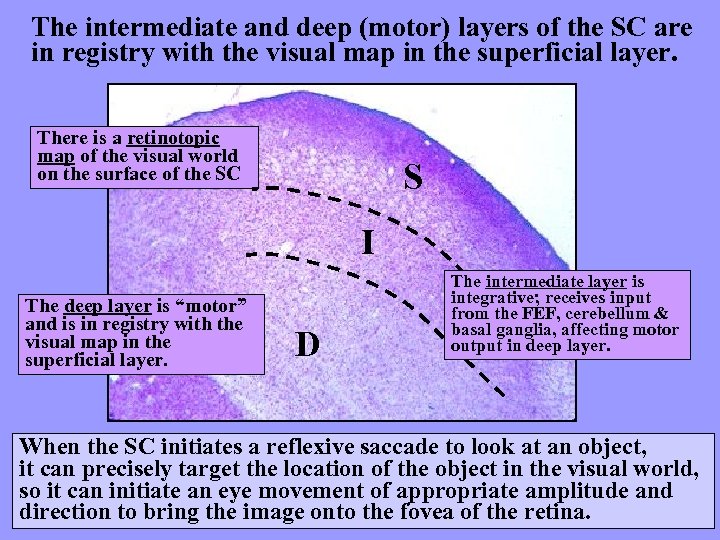 The intermediate and deep (motor) layers of the SC are in registry with the visual map in the superficial layer. There is a retinotopic map of the visual world on the surface of the SC S I The deep layer is “motor” and is in registry with the visual map in the superficial layer. D The intermediate layer is integrative; receives input from the FEF, cerebellum & basal ganglia, affecting motor output in deep layer. When the SC initiates a reflexive saccade to look at an object, it can precisely target the location of the object in the visual world, so it can initiate an eye movement of appropriate amplitude and direction to bring the image onto the fovea of the retina.
The intermediate and deep (motor) layers of the SC are in registry with the visual map in the superficial layer. There is a retinotopic map of the visual world on the surface of the SC S I The deep layer is “motor” and is in registry with the visual map in the superficial layer. D The intermediate layer is integrative; receives input from the FEF, cerebellum & basal ganglia, affecting motor output in deep layer. When the SC initiates a reflexive saccade to look at an object, it can precisely target the location of the object in the visual world, so it can initiate an eye movement of appropriate amplitude and direction to bring the image onto the fovea of the retina.
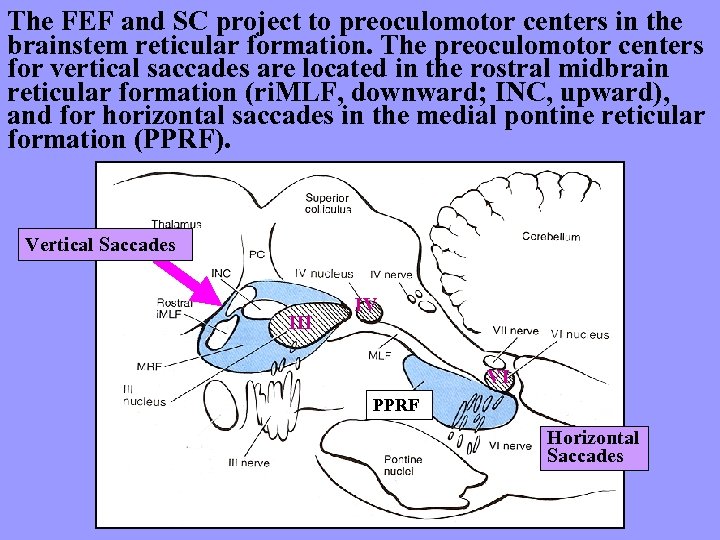 The FEF and SC project to preoculomotor centers in the brainstem reticular formation. The preoculomotor centers for vertical saccades are located in the rostral midbrain reticular formation (ri. MLF, downward; INC, upward), and for horizontal saccades in the medial pontine reticular formation (PPRF). Vertical Saccades III IV VI PPRF Horizontal Saccades
The FEF and SC project to preoculomotor centers in the brainstem reticular formation. The preoculomotor centers for vertical saccades are located in the rostral midbrain reticular formation (ri. MLF, downward; INC, upward), and for horizontal saccades in the medial pontine reticular formation (PPRF). Vertical Saccades III IV VI PPRF Horizontal Saccades
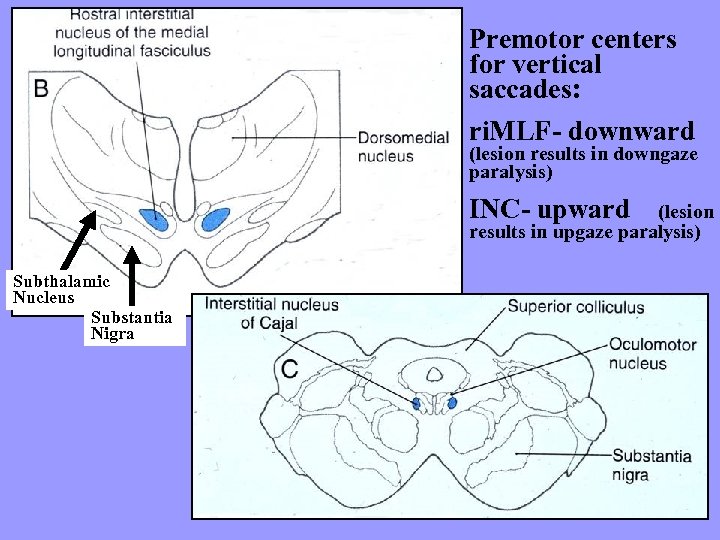 Premotor centers for vertical saccades: ri. MLF- downward (lesion results in downgaze paralysis) INC- upward (lesion results in upgaze paralysis) Subthalamic Nucleus Substantia Nigra
Premotor centers for vertical saccades: ri. MLF- downward (lesion results in downgaze paralysis) INC- upward (lesion results in upgaze paralysis) Subthalamic Nucleus Substantia Nigra
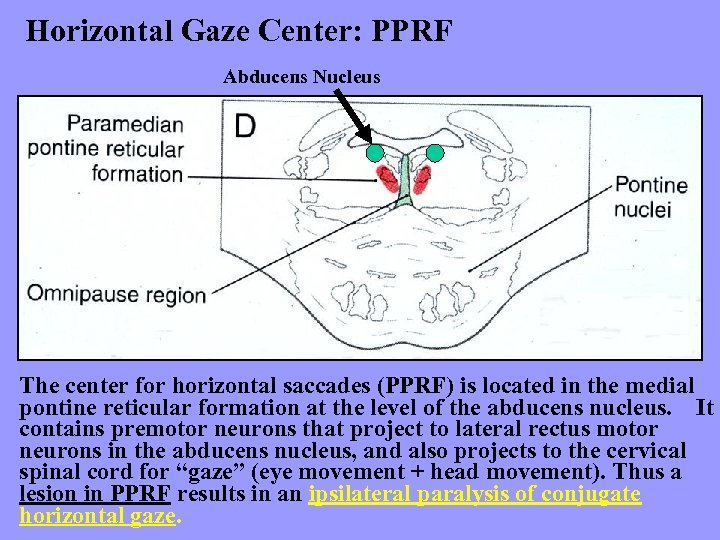 Horizontal Gaze Center: PPRF Abducens Nucleus The center for horizontal saccades (PPRF) is located in the medial pontine reticular formation at the level of the abducens nucleus. It contains premotor neurons that project to lateral rectus motor neurons in the abducens nucleus, and also projects to the cervical spinal cord for “gaze” (eye movement + head movement). Thus a lesion in PPRF results in an ipsilateral paralysis of conjugate horizontal gaze.
Horizontal Gaze Center: PPRF Abducens Nucleus The center for horizontal saccades (PPRF) is located in the medial pontine reticular formation at the level of the abducens nucleus. It contains premotor neurons that project to lateral rectus motor neurons in the abducens nucleus, and also projects to the cervical spinal cord for “gaze” (eye movement + head movement). Thus a lesion in PPRF results in an ipsilateral paralysis of conjugate horizontal gaze.
 Smooth Pursuit System Smooth pursuit eye movements are slow eye movements used to follow a moving object across the visual field. To maintain fixation, the eyes must move at the same speed as the visual target (eye movement matches target velocity). Therefore, the pursuit system involves seeing the object (visual cortex), analyzing its motion (pre-occipital cortex, area MT), and orchestrating eye movements (cerebellum) that are the same velocity as the target.
Smooth Pursuit System Smooth pursuit eye movements are slow eye movements used to follow a moving object across the visual field. To maintain fixation, the eyes must move at the same speed as the visual target (eye movement matches target velocity). Therefore, the pursuit system involves seeing the object (visual cortex), analyzing its motion (pre-occipital cortex, area MT), and orchestrating eye movements (cerebellum) that are the same velocity as the target.
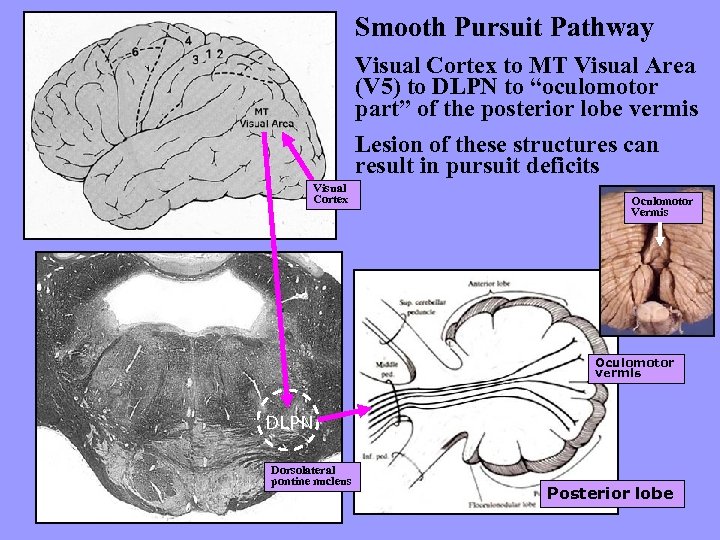 Smooth Pursuit Pathway Visual Cortex to MT Visual Area (V 5) to DLPN to “oculomotor part” of the posterior lobe vermis Lesion of these structures can result in pursuit deficits Visual Cortex Oculomotor Vermis Oculomotor vermis DLPN Dorsolateral pontine nucleus Posterior lobe
Smooth Pursuit Pathway Visual Cortex to MT Visual Area (V 5) to DLPN to “oculomotor part” of the posterior lobe vermis Lesion of these structures can result in pursuit deficits Visual Cortex Oculomotor Vermis Oculomotor vermis DLPN Dorsolateral pontine nucleus Posterior lobe
 Optokinetic System When the visual scene is moving (eg. riding on a train) to maintain fixation on an object (eg. following telephone poles) produces oscillating eye movements which consist of a slow component that follows the object and then a fast component where eyes snap back to attach to the next pole. Produces optokinetic eye movements, similar to nystagmus, called optokinetic nystagmus, OKN. The neural network for these eye movements involves the pretectum (receives visual input from the retina), which projects to the reticulotegmental nucleus (NRTP) of the pons, which then relays the information to the cerebellum (flocculonodular lobe).
Optokinetic System When the visual scene is moving (eg. riding on a train) to maintain fixation on an object (eg. following telephone poles) produces oscillating eye movements which consist of a slow component that follows the object and then a fast component where eyes snap back to attach to the next pole. Produces optokinetic eye movements, similar to nystagmus, called optokinetic nystagmus, OKN. The neural network for these eye movements involves the pretectum (receives visual input from the retina), which projects to the reticulotegmental nucleus (NRTP) of the pons, which then relays the information to the cerebellum (flocculonodular lobe).
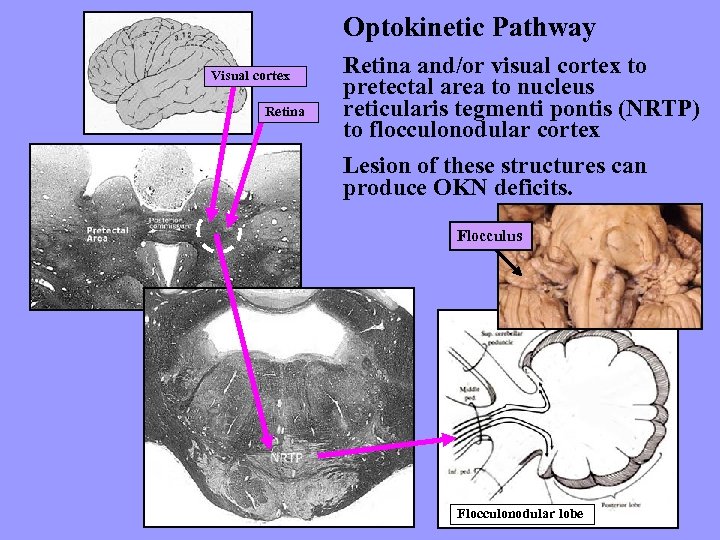 Optokinetic Pathway Visual cortex Retina and/or visual cortex to pretectal area to nucleus reticularis tegmenti pontis (NRTP) to flocculonodular cortex Lesion of these structures can produce OKN deficits. Flocculus Flocculonodular lobe
Optokinetic Pathway Visual cortex Retina and/or visual cortex to pretectal area to nucleus reticularis tegmenti pontis (NRTP) to flocculonodular cortex Lesion of these structures can produce OKN deficits. Flocculus Flocculonodular lobe
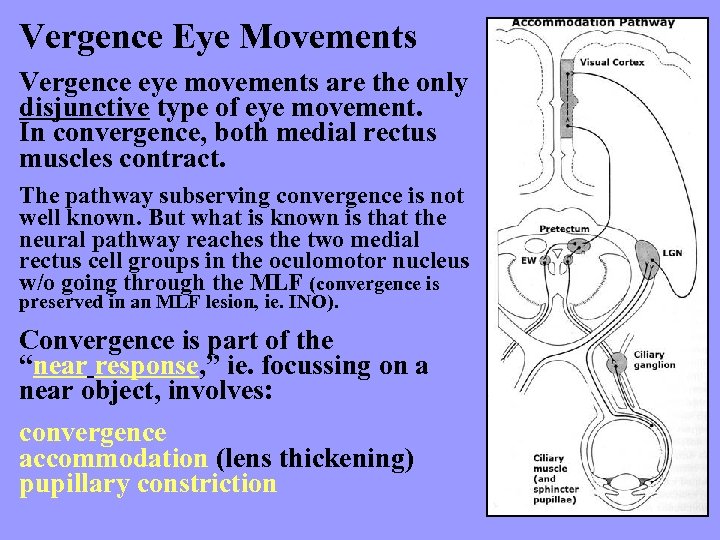 Vergence Eye Movements Vergence eye movements are the only disjunctive type of eye movement. In convergence, both medial rectus muscles contract. The pathway subserving convergence is not well known. But what is known is that the neural pathway reaches the two medial rectus cell groups in the oculomotor nucleus w/o going through the MLF (convergence is preserved in an MLF lesion, ie. INO). Convergence is part of the “near response, ” ie. focussing on a near object, involves: convergence accommodation (lens thickening) pupillary constriction
Vergence Eye Movements Vergence eye movements are the only disjunctive type of eye movement. In convergence, both medial rectus muscles contract. The pathway subserving convergence is not well known. But what is known is that the neural pathway reaches the two medial rectus cell groups in the oculomotor nucleus w/o going through the MLF (convergence is preserved in an MLF lesion, ie. INO). Convergence is part of the “near response, ” ie. focussing on a near object, involves: convergence accommodation (lens thickening) pupillary constriction
 Oculomotor Lesions
Oculomotor Lesions
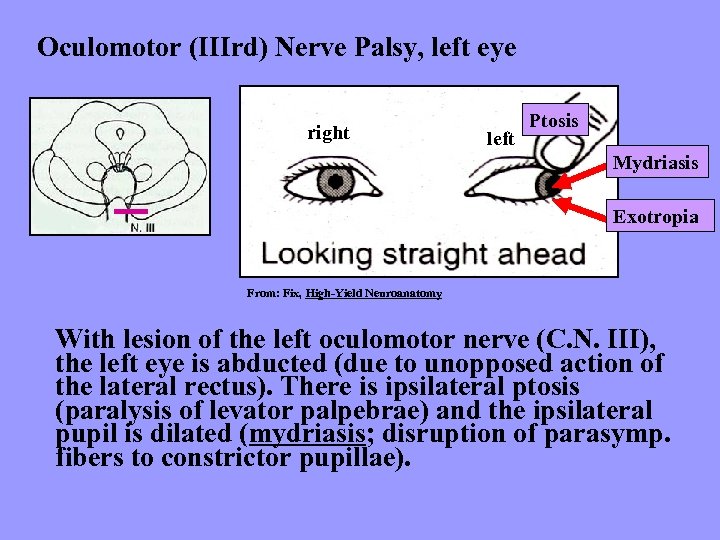 Oculomotor (IIIrd) Nerve Palsy, left eye right left Ptosis Mydriasis Exotropia From: Fix, High-Yield Neuroanatomy With lesion of the left oculomotor nerve (C. N. III), the left eye is abducted (due to unopposed action of the lateral rectus). There is ipsilateral ptosis (paralysis of levator palpebrae) and the ipsilateral pupil is dilated (mydriasis; disruption of parasymp. fibers to constrictor pupillae).
Oculomotor (IIIrd) Nerve Palsy, left eye right left Ptosis Mydriasis Exotropia From: Fix, High-Yield Neuroanatomy With lesion of the left oculomotor nerve (C. N. III), the left eye is abducted (due to unopposed action of the lateral rectus). There is ipsilateral ptosis (paralysis of levator palpebrae) and the ipsilateral pupil is dilated (mydriasis; disruption of parasymp. fibers to constrictor pupillae).
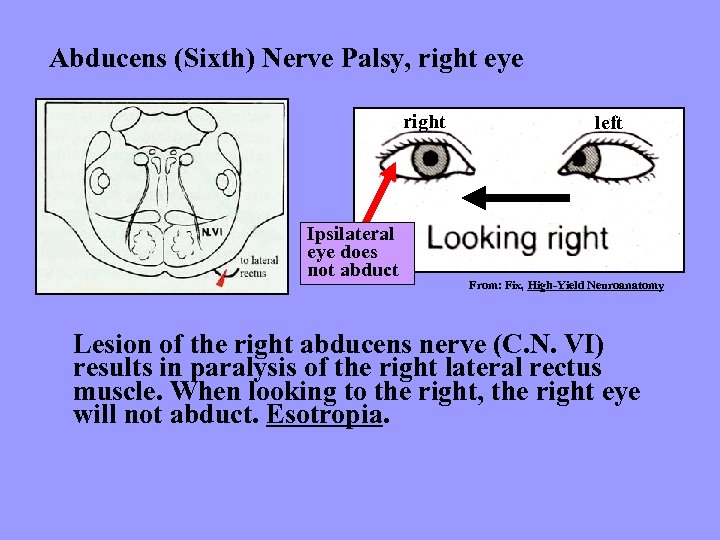 Abducens (Sixth) Nerve Palsy, right eye right Ipsilateral eye does not abduct left From: Fix, High-Yield Neuroanatomy Lesion of the right abducens nerve (C. N. VI) results in paralysis of the right lateral rectus muscle. When looking to the right, the right eye will not abduct. Esotropia.
Abducens (Sixth) Nerve Palsy, right eye right Ipsilateral eye does not abduct left From: Fix, High-Yield Neuroanatomy Lesion of the right abducens nerve (C. N. VI) results in paralysis of the right lateral rectus muscle. When looking to the right, the right eye will not abduct. Esotropia.
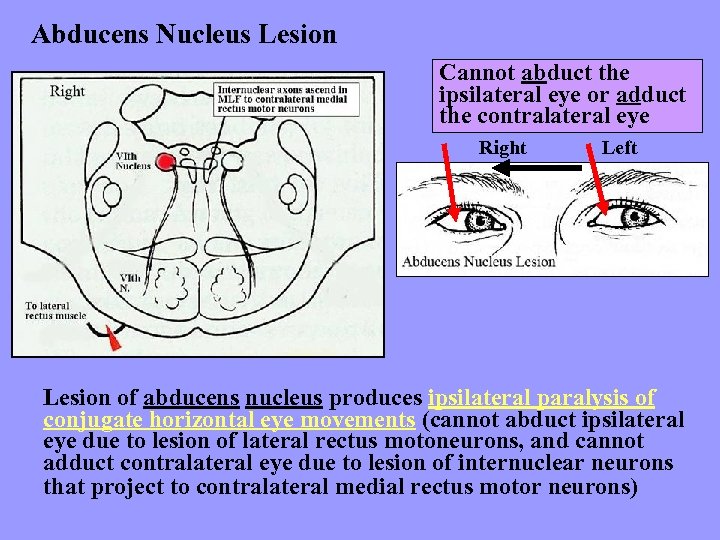 Abducens Nucleus Lesion Cannot abduct the ipsilateral eye or adduct the contralateral eye Right Left Lesion of abducens nucleus produces ipsilateral paralysis of conjugate horizontal eye movements (cannot abduct ipsilateral eye due to lesion of lateral rectus motoneurons, and cannot adduct contralateral eye due to lesion of internuclear neurons that project to contralateral medial rectus motor neurons)
Abducens Nucleus Lesion Cannot abduct the ipsilateral eye or adduct the contralateral eye Right Left Lesion of abducens nucleus produces ipsilateral paralysis of conjugate horizontal eye movements (cannot abduct ipsilateral eye due to lesion of lateral rectus motoneurons, and cannot adduct contralateral eye due to lesion of internuclear neurons that project to contralateral medial rectus motor neurons)
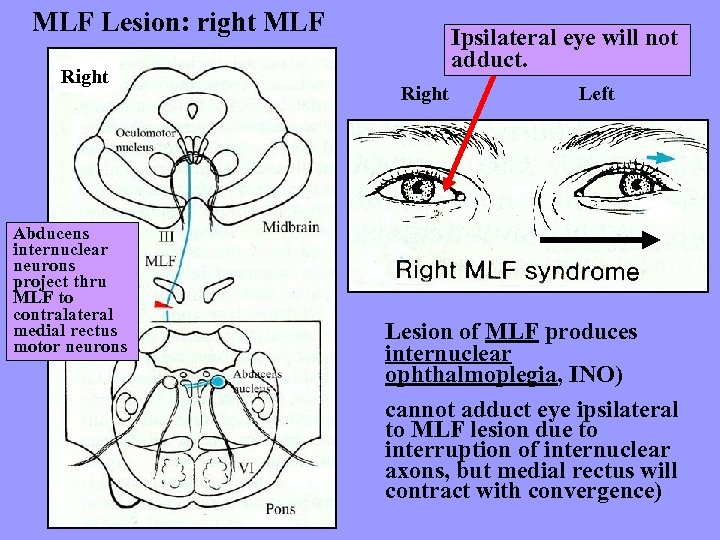 MLF Lesion: right MLF Right Abducens internuclear neurons project thru MLF to contralateral medial rectus motor neurons Ipsilateral eye will not adduct. Right Left Lesion of MLF produces internuclear ophthalmoplegia, INO) cannot adduct eye ipsilateral to MLF lesion due to interruption of internuclear axons, but medial rectus will contract with convergence)
MLF Lesion: right MLF Right Abducens internuclear neurons project thru MLF to contralateral medial rectus motor neurons Ipsilateral eye will not adduct. Right Left Lesion of MLF produces internuclear ophthalmoplegia, INO) cannot adduct eye ipsilateral to MLF lesion due to interruption of internuclear axons, but medial rectus will contract with convergence)
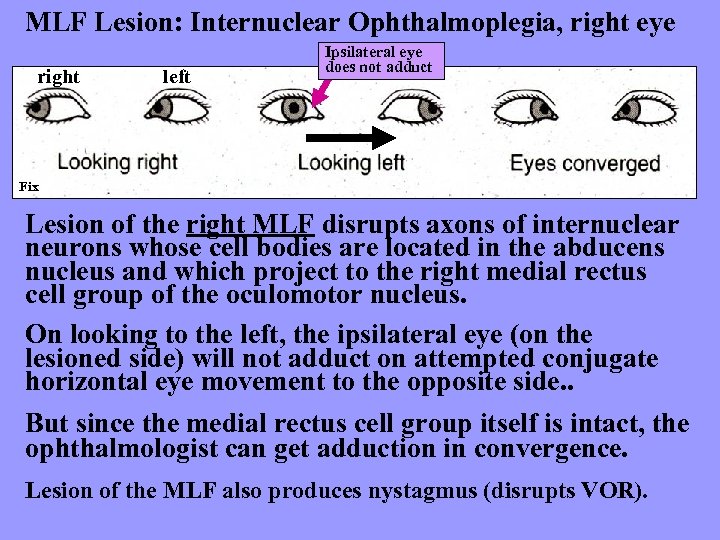 MLF Lesion: Internuclear Ophthalmoplegia, right eye right left Ipsilateral eye does not adduct Fix Lesion of the right MLF disrupts axons of internuclear neurons whose cell bodies are located in the abducens nucleus and which project to the right medial rectus cell group of the oculomotor nucleus. On looking to the left, the ipsilateral eye (on the lesioned side) will not adduct on attempted conjugate horizontal eye movement to the opposite side. . But since the medial rectus cell group itself is intact, the ophthalmologist can get adduction in convergence. Lesion of the MLF also produces nystagmus (disrupts VOR).
MLF Lesion: Internuclear Ophthalmoplegia, right eye right left Ipsilateral eye does not adduct Fix Lesion of the right MLF disrupts axons of internuclear neurons whose cell bodies are located in the abducens nucleus and which project to the right medial rectus cell group of the oculomotor nucleus. On looking to the left, the ipsilateral eye (on the lesioned side) will not adduct on attempted conjugate horizontal eye movement to the opposite side. . But since the medial rectus cell group itself is intact, the ophthalmologist can get adduction in convergence. Lesion of the MLF also produces nystagmus (disrupts VOR).
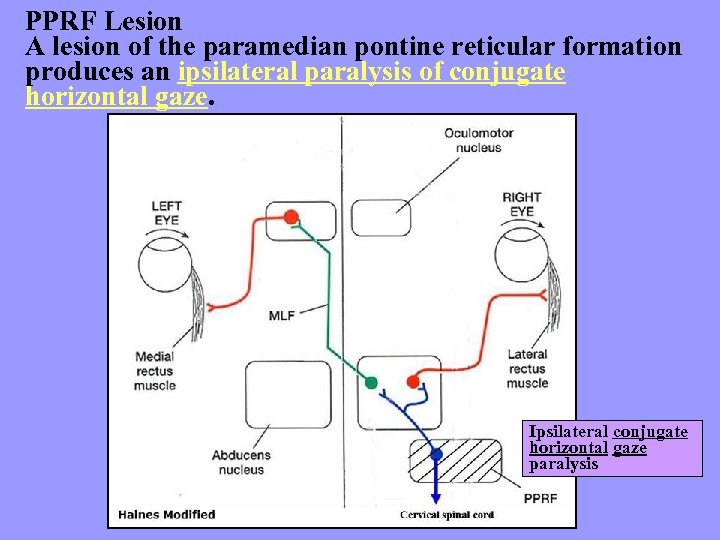 PPRF Lesion A lesion of the paramedian pontine reticular formation produces an ipsilateral paralysis of conjugate horizontal gaze. Ipsilateral conjugate horizontal gaze paralysis
PPRF Lesion A lesion of the paramedian pontine reticular formation produces an ipsilateral paralysis of conjugate horizontal gaze. Ipsilateral conjugate horizontal gaze paralysis
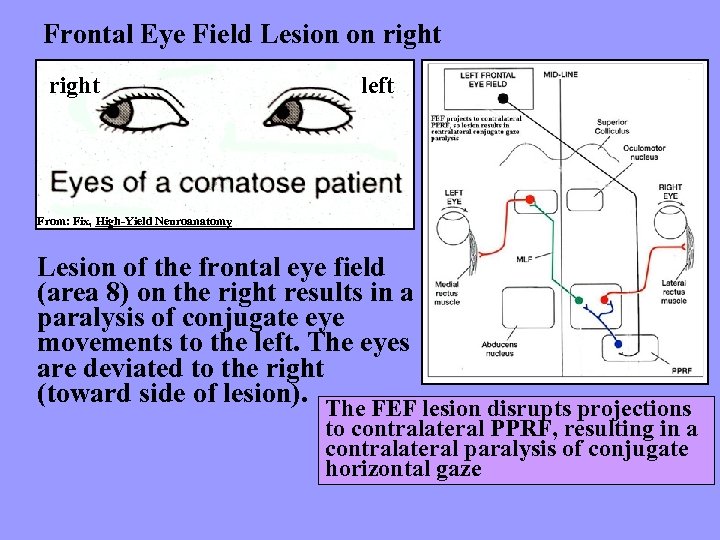 Frontal Eye Field Lesion on right left From: Fix, High-Yield Neuroanatomy Lesion of the frontal eye field (area 8) on the right results in a paralysis of conjugate eye movements to the left. The eyes are deviated to the right (toward side of lesion). The FEF lesion disrupts projections to contralateral PPRF, resulting in a contralateral paralysis of conjugate horizontal gaze
Frontal Eye Field Lesion on right left From: Fix, High-Yield Neuroanatomy Lesion of the frontal eye field (area 8) on the right results in a paralysis of conjugate eye movements to the left. The eyes are deviated to the right (toward side of lesion). The FEF lesion disrupts projections to contralateral PPRF, resulting in a contralateral paralysis of conjugate horizontal gaze
 Cerebellum
Cerebellum
 Cerebellum: Three Lobes Anterior Lobe- “paleocerebellum” proprioception Posterior Lobe- “neocerebellum” cortical (receives input from cortex via basilar pons) Flocculonodular Lobe- “archicerebellum” vestibular
Cerebellum: Three Lobes Anterior Lobe- “paleocerebellum” proprioception Posterior Lobe- “neocerebellum” cortical (receives input from cortex via basilar pons) Flocculonodular Lobe- “archicerebellum” vestibular
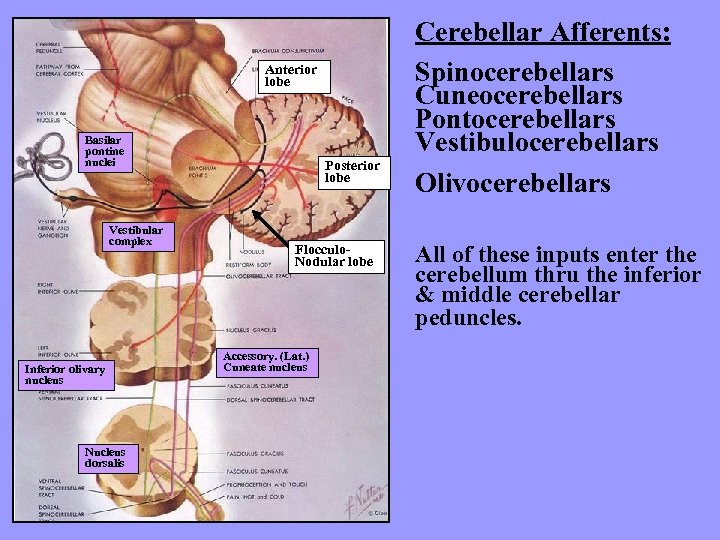 Anterior lobe Basilar pontine nuclei Vestibular complex Inferior olivary nucleus Nucleus dorsalis Posterior lobe Flocculo. Nodular lobe Accessory. (Lat. ) Cuneate nucleus Cerebellar Afferents: Spinocerebellars Cuneocerebellars Pontocerebellars Vestibulocerebellars Olivocerebellars All of these inputs enter the cerebellum thru the inferior & middle cerebellar peduncles.
Anterior lobe Basilar pontine nuclei Vestibular complex Inferior olivary nucleus Nucleus dorsalis Posterior lobe Flocculo. Nodular lobe Accessory. (Lat. ) Cuneate nucleus Cerebellar Afferents: Spinocerebellars Cuneocerebellars Pontocerebellars Vestibulocerebellars Olivocerebellars All of these inputs enter the cerebellum thru the inferior & middle cerebellar peduncles.
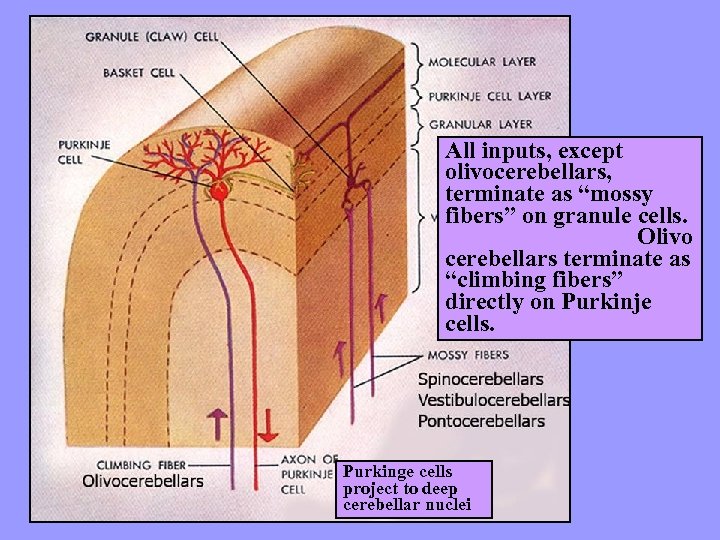 All inputs, except olivocerebellars, terminate as “mossy fibers” on granule cells. Olivo cerebellars terminate as “climbing fibers” directly on Purkinje cells. Purkinge cells project to deep cerebellar nuclei
All inputs, except olivocerebellars, terminate as “mossy fibers” on granule cells. Olivo cerebellars terminate as “climbing fibers” directly on Purkinje cells. Purkinge cells project to deep cerebellar nuclei
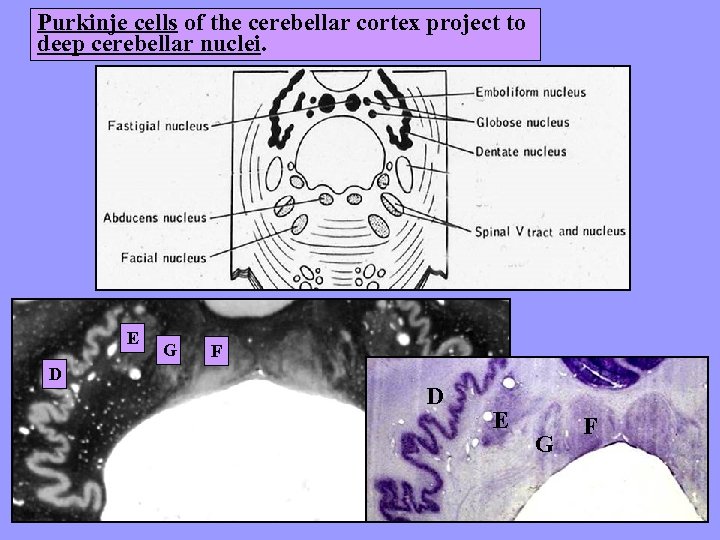 Purkinje cells of the cerebellar cortex project to deep cerebellar nuclei. E D G F D E G F
Purkinje cells of the cerebellar cortex project to deep cerebellar nuclei. E D G F D E G F
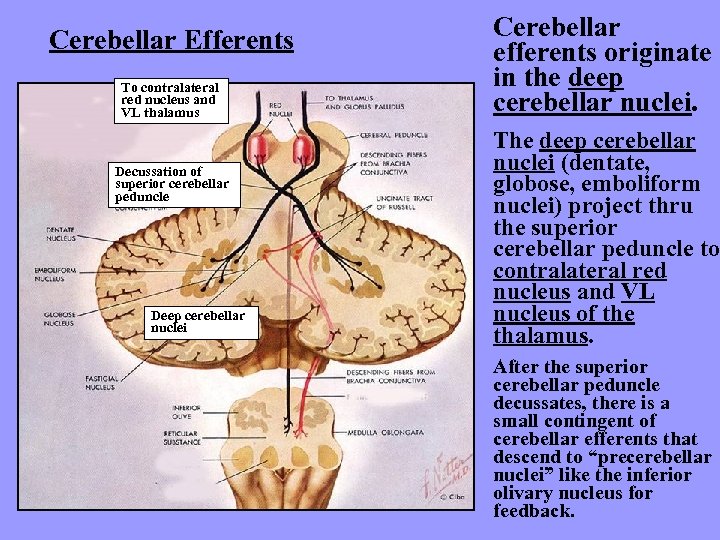 Cerebellar Efferents To contralateral red nucleus and VL thalamus Decussation of superior cerebellar peduncle Deep cerebellar nuclei Cerebellar efferents originate in the deep cerebellar nuclei. The deep cerebellar nuclei (dentate, globose, emboliform nuclei) project thru the superior cerebellar peduncle to contralateral red nucleus and VL nucleus of the thalamus. After the superior cerebellar peduncle decussates, there is a small contingent of cerebellar efferents that descend to “precerebellar nuclei” like the inferior olivary nucleus for feedback.
Cerebellar Efferents To contralateral red nucleus and VL thalamus Decussation of superior cerebellar peduncle Deep cerebellar nuclei Cerebellar efferents originate in the deep cerebellar nuclei. The deep cerebellar nuclei (dentate, globose, emboliform nuclei) project thru the superior cerebellar peduncle to contralateral red nucleus and VL nucleus of the thalamus. After the superior cerebellar peduncle decussates, there is a small contingent of cerebellar efferents that descend to “precerebellar nuclei” like the inferior olivary nucleus for feedback.
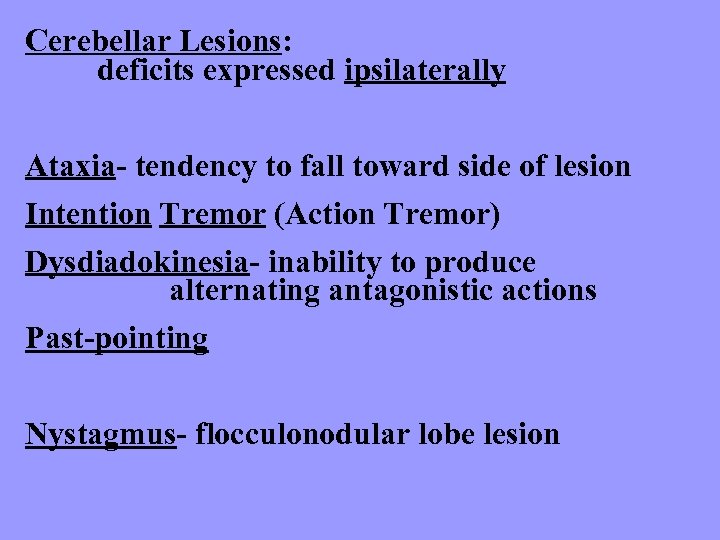 Cerebellar Lesions: deficits expressed ipsilaterally Ataxia- tendency to fall toward side of lesion Intention Tremor (Action Tremor) Dysdiadokinesia- inability to produce alternating antagonistic actions Past-pointing Nystagmus- flocculonodular lobe lesion
Cerebellar Lesions: deficits expressed ipsilaterally Ataxia- tendency to fall toward side of lesion Intention Tremor (Action Tremor) Dysdiadokinesia- inability to produce alternating antagonistic actions Past-pointing Nystagmus- flocculonodular lobe lesion
 Basal Ganglia
Basal Ganglia
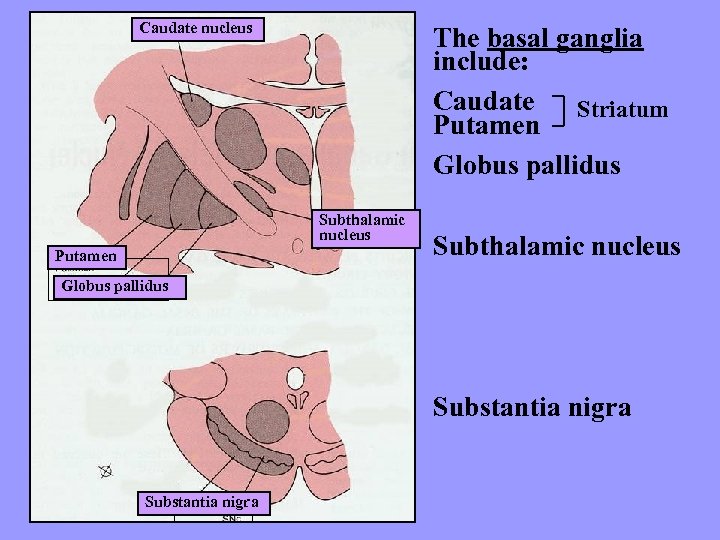 Caudate nucleus The basal ganglia include: Caudate Striatum Putamen Globus pallidus Subthalamic nucleus Putamen Subthalamic nucleus Globus pallidus Substantia nigra
Caudate nucleus The basal ganglia include: Caudate Striatum Putamen Globus pallidus Subthalamic nucleus Putamen Subthalamic nucleus Globus pallidus Substantia nigra
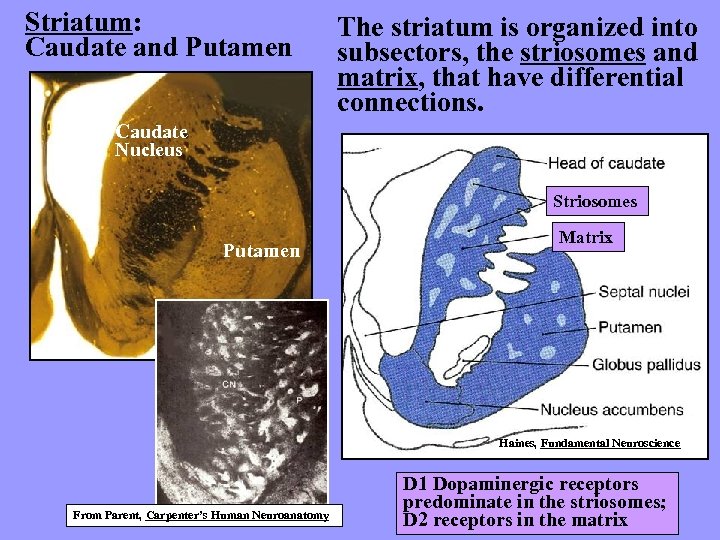 Striatum: Caudate and Putamen The striatum is organized into subsectors, the striosomes and matrix, that have differential connections. Caudate Nucleus Striosomes Putamen Matrix Haines, Fundamental Neuroscience From Parent, Carpenter’s Human Neuroanatomy D 1 Dopaminergic receptors predominate in the striosomes; D 2 receptors in the matrix
Striatum: Caudate and Putamen The striatum is organized into subsectors, the striosomes and matrix, that have differential connections. Caudate Nucleus Striosomes Putamen Matrix Haines, Fundamental Neuroscience From Parent, Carpenter’s Human Neuroanatomy D 1 Dopaminergic receptors predominate in the striosomes; D 2 receptors in the matrix
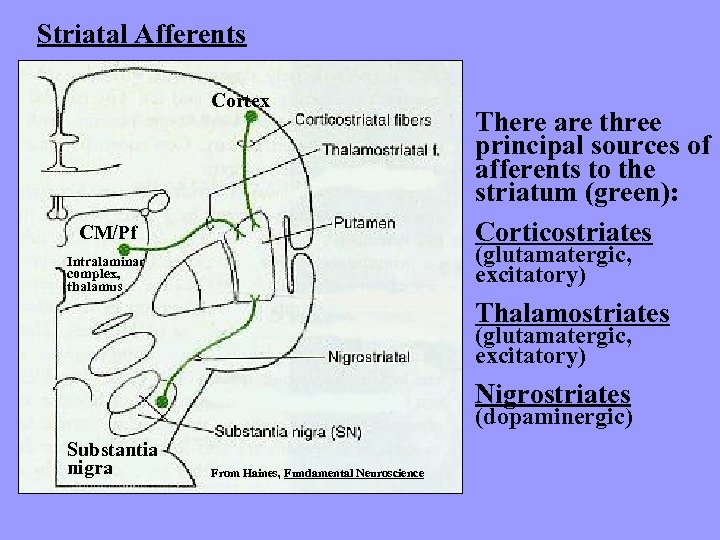 Striatal Afferents Cortex CM/Pf There are three principal sources of afferents to the striatum (green): Corticostriates (glutamatergic, excitatory) Intralaminar complex, thalamus Thalamostriates (glutamatergic, excitatory) Nigrostriates (dopaminergic) Substantia nigra From Haines, Fundamental Neuroscience
Striatal Afferents Cortex CM/Pf There are three principal sources of afferents to the striatum (green): Corticostriates (glutamatergic, excitatory) Intralaminar complex, thalamus Thalamostriates (glutamatergic, excitatory) Nigrostriates (dopaminergic) Substantia nigra From Haines, Fundamental Neuroscience
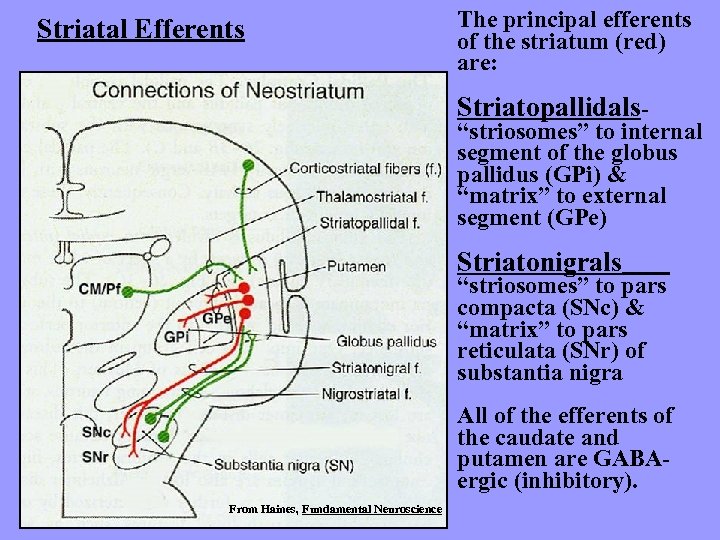 Striatal Efferents The principal efferents of the striatum (red) are: Striatopallidals- “striosomes” to internal segment of the globus pallidus (GPi) & “matrix” to external segment (GPe) Striatonigrals “striosomes” to pars compacta (SNc) & “matrix” to pars reticulata (SNr) of substantia nigra All of the efferents of the caudate and putamen are GABAergic (inhibitory). From Haines, Fundamental Neuroscience
Striatal Efferents The principal efferents of the striatum (red) are: Striatopallidals- “striosomes” to internal segment of the globus pallidus (GPi) & “matrix” to external segment (GPe) Striatonigrals “striosomes” to pars compacta (SNc) & “matrix” to pars reticulata (SNr) of substantia nigra All of the efferents of the caudate and putamen are GABAergic (inhibitory). From Haines, Fundamental Neuroscience
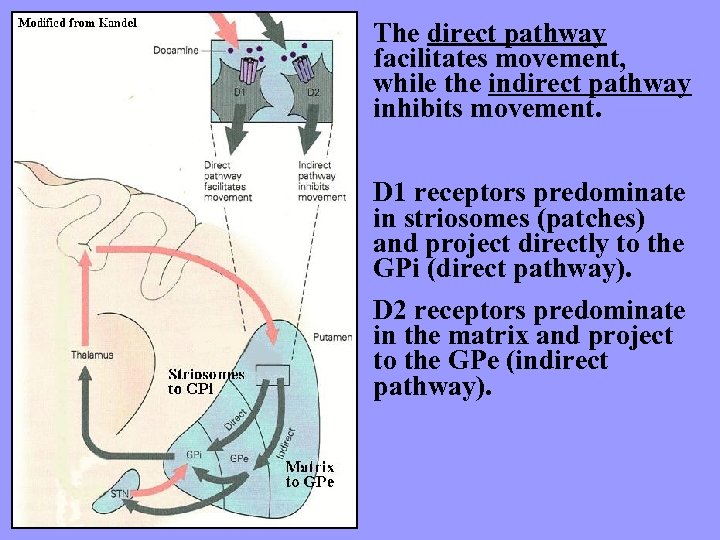 The direct pathway facilitates movement, while the indirect pathway inhibits movement. D 1 receptors predominate in striosomes (patches) and project directly to the GPi (direct pathway). D 2 receptors predominate in the matrix and project to the GPe (indirect pathway).
The direct pathway facilitates movement, while the indirect pathway inhibits movement. D 1 receptors predominate in striosomes (patches) and project directly to the GPi (direct pathway). D 2 receptors predominate in the matrix and project to the GPe (indirect pathway).
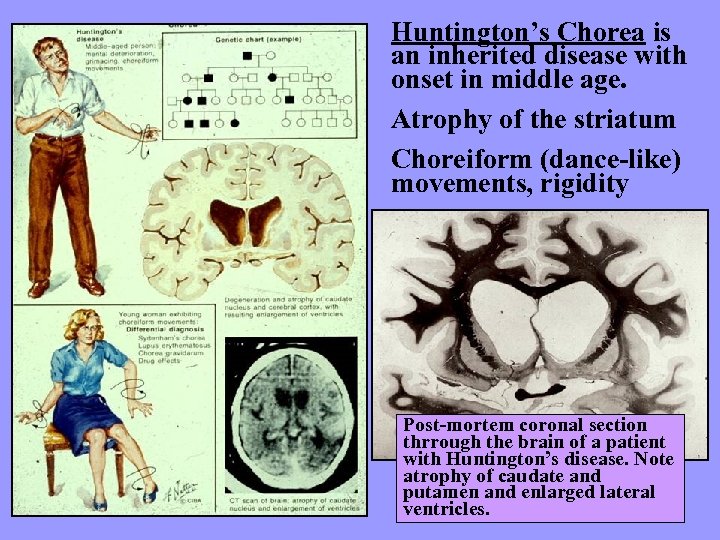 Huntington’s Chorea is an inherited disease with onset in middle age. Atrophy of the striatum Choreiform (dance-like) movements, rigidity Post-mortem coronal section thrrough the brain of a patient with Huntington’s disease. Note atrophy of caudate and putamen and enlarged lateral ventricles.
Huntington’s Chorea is an inherited disease with onset in middle age. Atrophy of the striatum Choreiform (dance-like) movements, rigidity Post-mortem coronal section thrrough the brain of a patient with Huntington’s disease. Note atrophy of caudate and putamen and enlarged lateral ventricles.
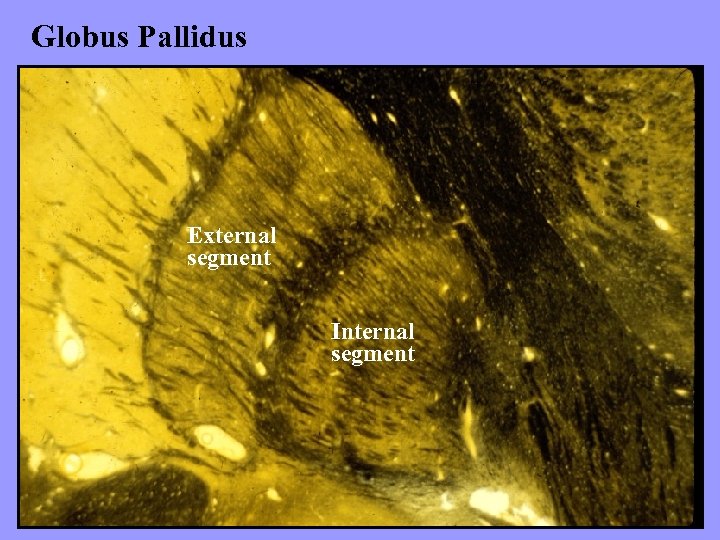 Globus Pallidus External segment Internal segment
Globus Pallidus External segment Internal segment
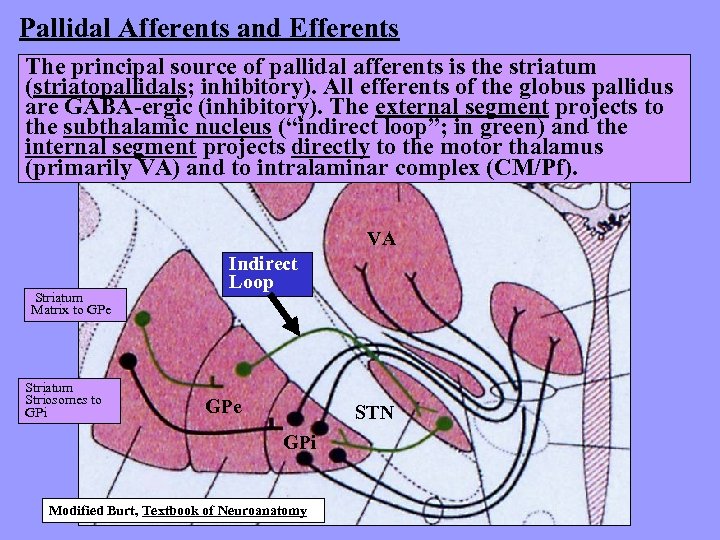 Pallidal Afferents and Efferents The principal source of pallidal afferents is the striatum (striatopallidals; inhibitory). All efferents of the globus pallidus are GABA-ergic (inhibitory). The external segment projects to the subthalamic nucleus (“indirect loop”; in green) and the internal segment projects directly to the motor thalamus (primarily VA) and to intralaminar complex (CM/Pf). VA Striatum Matrix to GPe Striatum Striosomes to GPi Indirect Loop GPe STN GPi Modified Burt, Textbook of Neuroanatomy
Pallidal Afferents and Efferents The principal source of pallidal afferents is the striatum (striatopallidals; inhibitory). All efferents of the globus pallidus are GABA-ergic (inhibitory). The external segment projects to the subthalamic nucleus (“indirect loop”; in green) and the internal segment projects directly to the motor thalamus (primarily VA) and to intralaminar complex (CM/Pf). VA Striatum Matrix to GPe Striatum Striosomes to GPi Indirect Loop GPe STN GPi Modified Burt, Textbook of Neuroanatomy
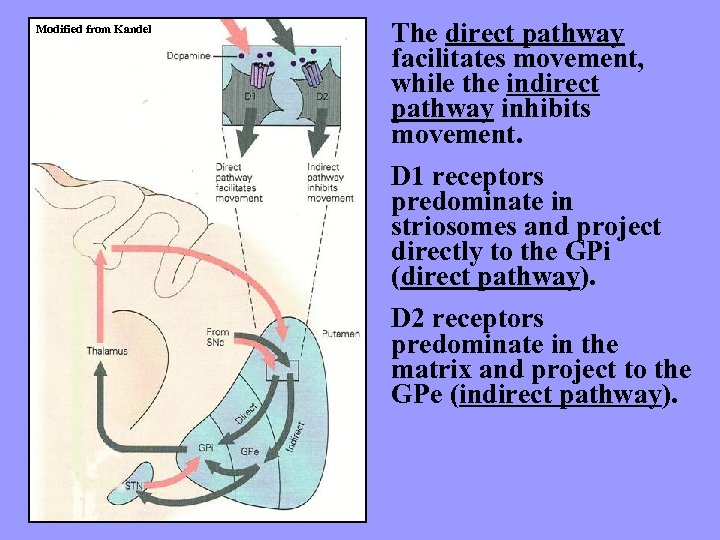 Modified from Kandel The direct pathway facilitates movement, while the indirect pathway inhibits movement. D 1 receptors predominate in striosomes and project directly to the GPi (direct pathway). D 2 receptors predominate in the matrix and project to the GPe (indirect pathway).
Modified from Kandel The direct pathway facilitates movement, while the indirect pathway inhibits movement. D 1 receptors predominate in striosomes and project directly to the GPi (direct pathway). D 2 receptors predominate in the matrix and project to the GPe (indirect pathway).
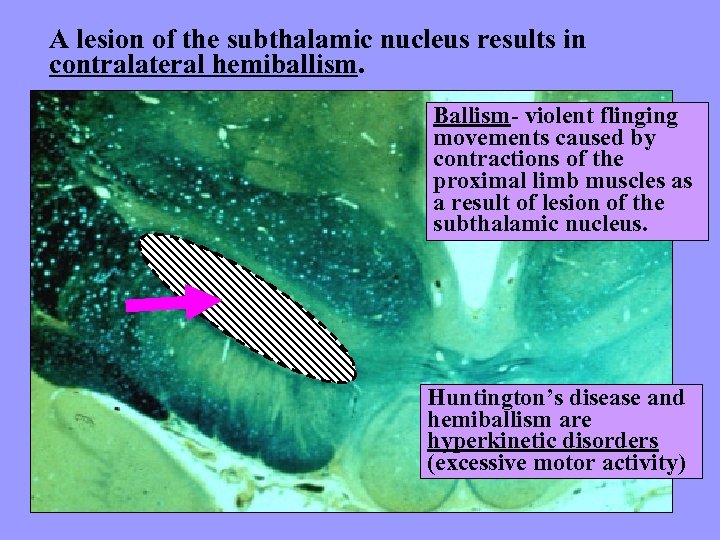 A lesion of the subthalamic nucleus results in contralateral hemiballism. Ballism- violent flinging movements caused by contractions of the proximal limb muscles as a result of lesion of the subthalamic nucleus. Huntington’s disease and hemiballism are hyperkinetic disorders (excessive motor activity)
A lesion of the subthalamic nucleus results in contralateral hemiballism. Ballism- violent flinging movements caused by contractions of the proximal limb muscles as a result of lesion of the subthalamic nucleus. Huntington’s disease and hemiballism are hyperkinetic disorders (excessive motor activity)
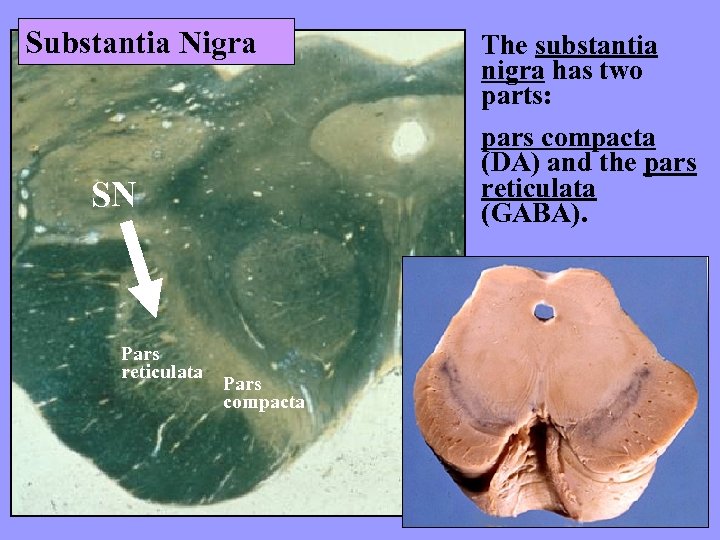 Substantia Nigra pars compacta (DA) and the pars reticulata (GABA). SN Pars reticulata The substantia nigra has two parts: Pars compacta
Substantia Nigra pars compacta (DA) and the pars reticulata (GABA). SN Pars reticulata The substantia nigra has two parts: Pars compacta
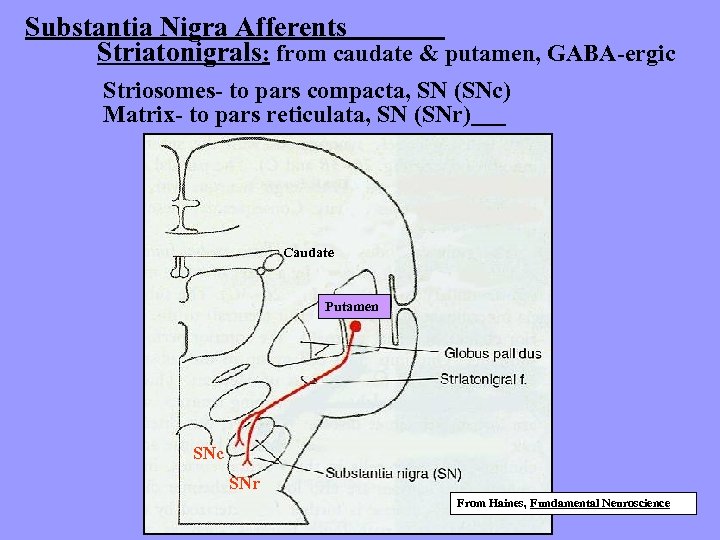 Substantia Nigra Afferents Striatonigrals: from caudate & putamen, GABA-ergic Striosomes- to pars compacta, SN (SNc) Matrix- to pars reticulata, SN (SNr) Caudate Putamen SNc SNr From Haines, Fundamental Neuroscience
Substantia Nigra Afferents Striatonigrals: from caudate & putamen, GABA-ergic Striosomes- to pars compacta, SN (SNc) Matrix- to pars reticulata, SN (SNr) Caudate Putamen SNc SNr From Haines, Fundamental Neuroscience
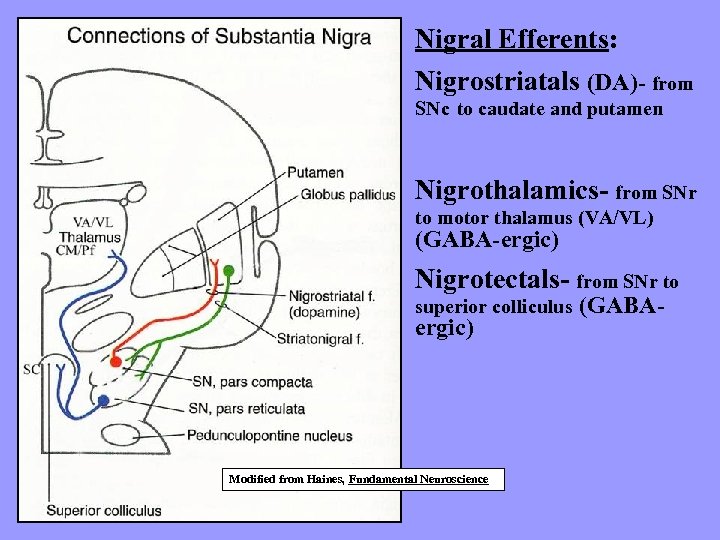 Nigral Efferents: Nigrostriatals (DA)- from SNc to caudate and putamen Nigrothalamics- from SNr to motor thalamus (VA/VL) (GABA-ergic) Nigrotectals- from SNr to superior colliculus ergic) Modified from Haines, Fundamental Neuroscience (GABA-
Nigral Efferents: Nigrostriatals (DA)- from SNc to caudate and putamen Nigrothalamics- from SNr to motor thalamus (VA/VL) (GABA-ergic) Nigrotectals- from SNr to superior colliculus ergic) Modified from Haines, Fundamental Neuroscience (GABA-
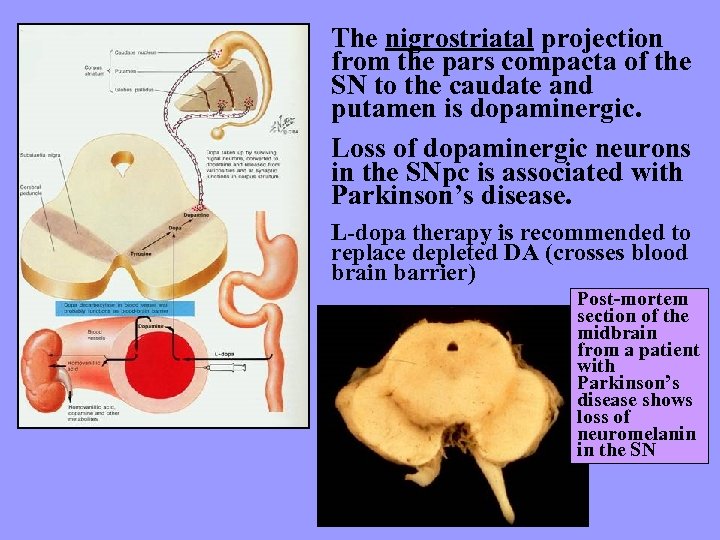 The nigrostriatal projection from the pars compacta of the SN to the caudate and putamen is dopaminergic. Loss of dopaminergic neurons in the SNpc is associated with Parkinson’s disease. L-dopa therapy is recommended to replace depleted DA (crosses blood brain barrier) Post-mortem section of the midbrain from a patient with Parkinson’s disease shows loss of neuromelanin in the SN
The nigrostriatal projection from the pars compacta of the SN to the caudate and putamen is dopaminergic. Loss of dopaminergic neurons in the SNpc is associated with Parkinson’s disease. L-dopa therapy is recommended to replace depleted DA (crosses blood brain barrier) Post-mortem section of the midbrain from a patient with Parkinson’s disease shows loss of neuromelanin in the SN
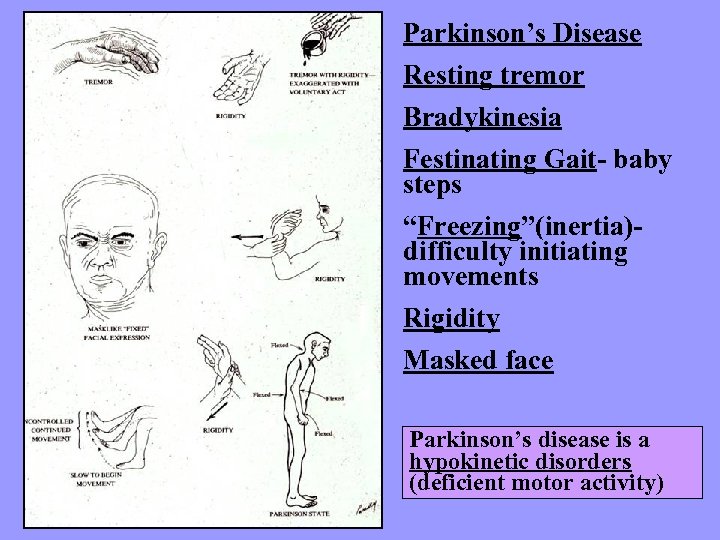 Parkinson’s Disease Resting tremor Bradykinesia Festinating Gait- baby steps “Freezing”(inertia)difficulty initiating movements Rigidity Masked face Parkinson’s disease is a hypokinetic disorders (deficient motor activity)
Parkinson’s Disease Resting tremor Bradykinesia Festinating Gait- baby steps “Freezing”(inertia)difficulty initiating movements Rigidity Masked face Parkinson’s disease is a hypokinetic disorders (deficient motor activity)
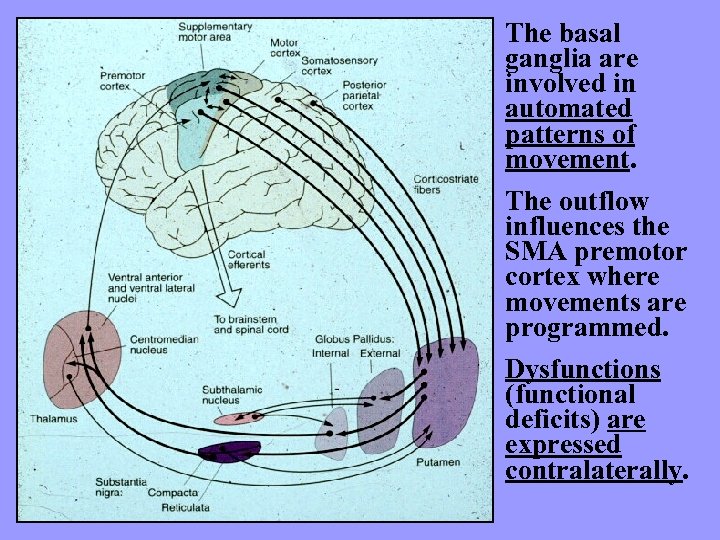 The basal ganglia are involved in automated patterns of movement. The outflow influences the SMA premotor cortex where movements are programmed. Dysfunctions (functional deficits) are expressed contralaterally.
The basal ganglia are involved in automated patterns of movement. The outflow influences the SMA premotor cortex where movements are programmed. Dysfunctions (functional deficits) are expressed contralaterally.
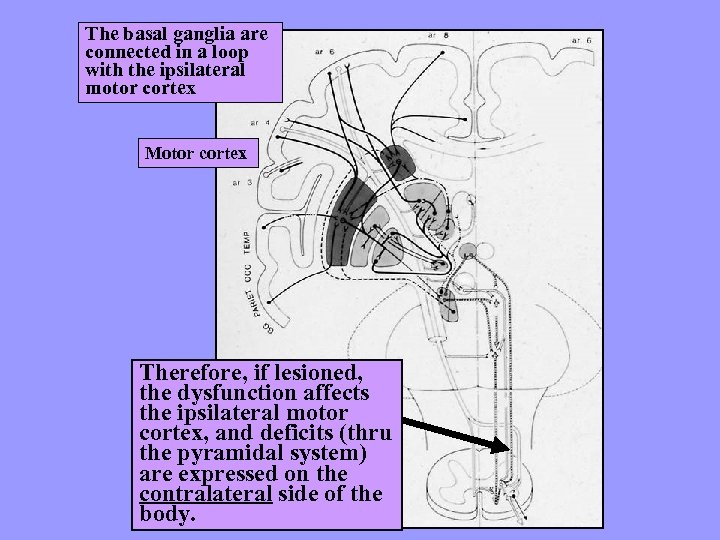 The basal ganglia are connected in a loop with the ipsilateral motor cortex Motor cortex Therefore, if lesioned, the dysfunction affects the ipsilateral motor cortex, and deficits (thru the pyramidal system) are expressed on the contralateral side of the body.
The basal ganglia are connected in a loop with the ipsilateral motor cortex Motor cortex Therefore, if lesioned, the dysfunction affects the ipsilateral motor cortex, and deficits (thru the pyramidal system) are expressed on the contralateral side of the body.


