fdb1a7128844b4ea9d8b5edb09164bbf.ppt
- Количество слайдов: 104
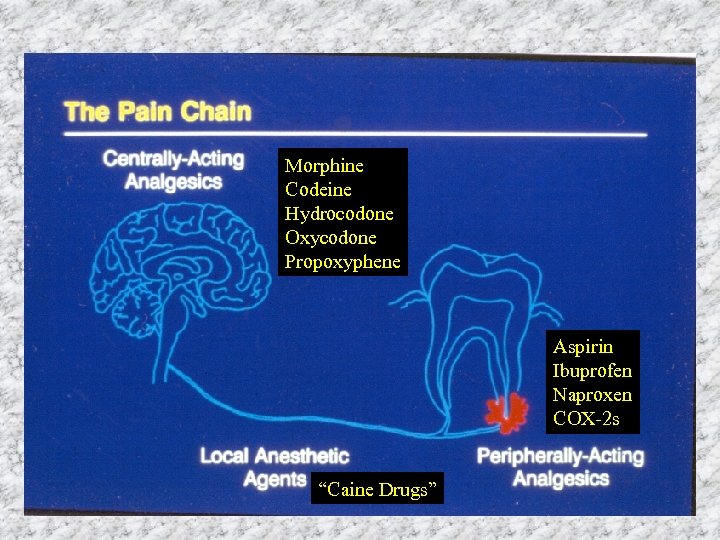
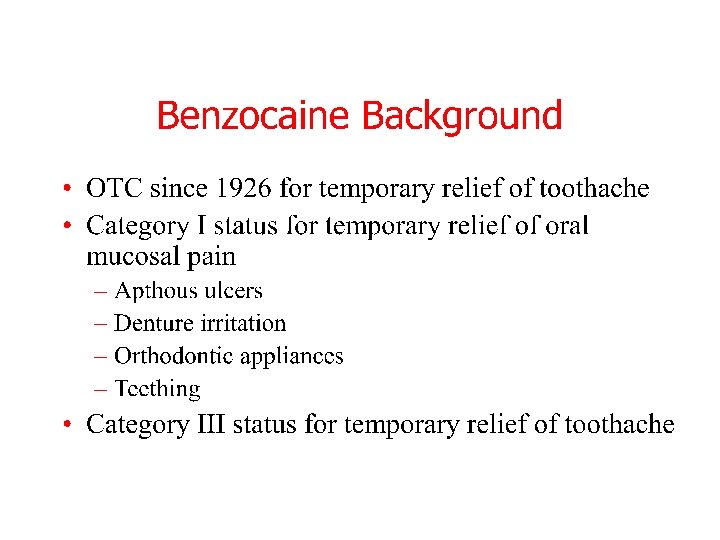
Morphine Codeine Hydrocodone Oxycodone Propoxyphene Aspirin Ibuprofen Naproxen COX-2 s “Caine Drugs”
Construction in Mouth
Erythoxylum Coca Shrub
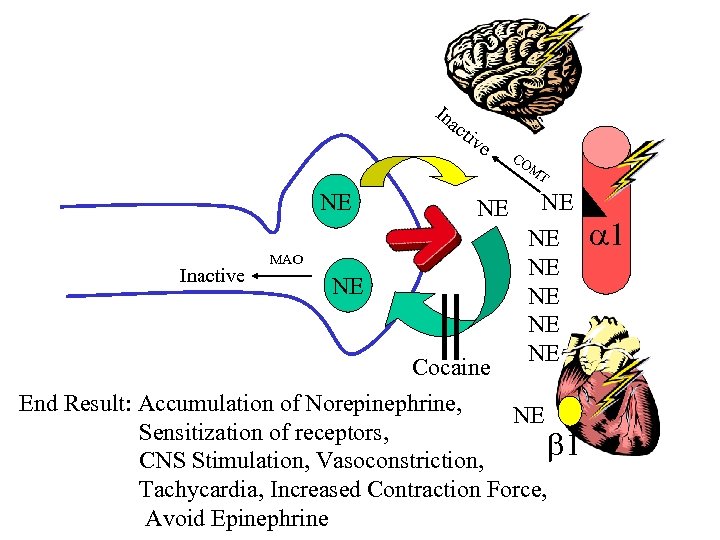
In ac ti ve CO M T NE Inactive MAO NE NE Cocaine End Result: Accumulation of Norepinephrine, NE Sensitization of receptors, 1 CNS Stimulation, Vasoconstriction, Tachycardia, Increased Contraction Force, Avoid Epinephrine 1
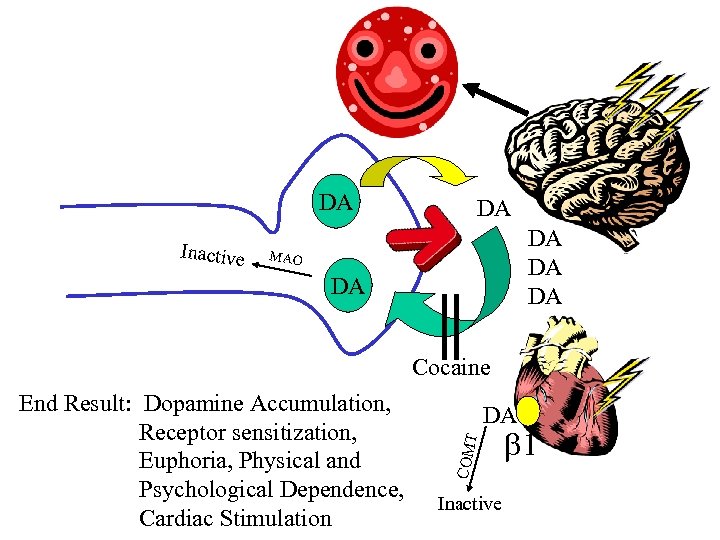
DA Inactive DA DA MAO DA Cocaine T DA COM End Result: Dopamine Accumulation, Receptor sensitization, Euphoria, Physical and Psychological Dependence, Cardiac Stimulation Inactive 1
Cocaine + Vasoconstrictors =
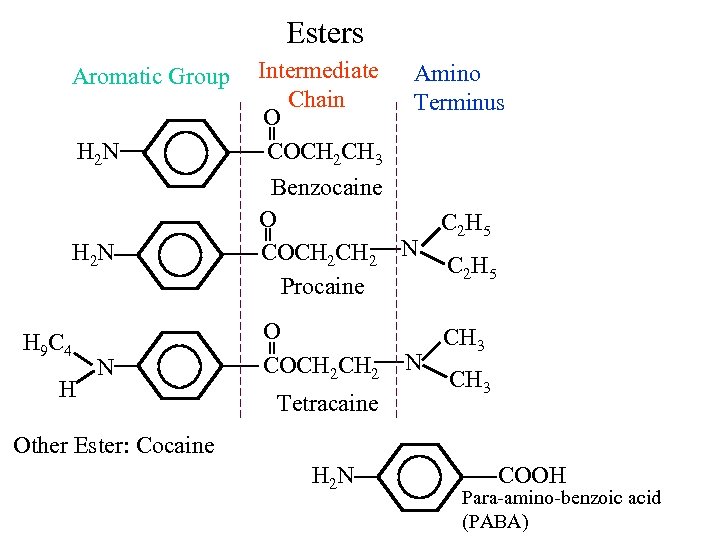
Esters Aromatic Group H 2 N H 9 C 4 H N Intermediate Amino Chain Terminus O COCH 2 CH 3 Benzocaine O C 2 H 5 COCH 2 N C 2 H 5 Procaine O COCH 2 Tetracaine N CH 3 Other Ester: Cocaine H 2 N COOH Para-amino-benzoic acid (PABA)
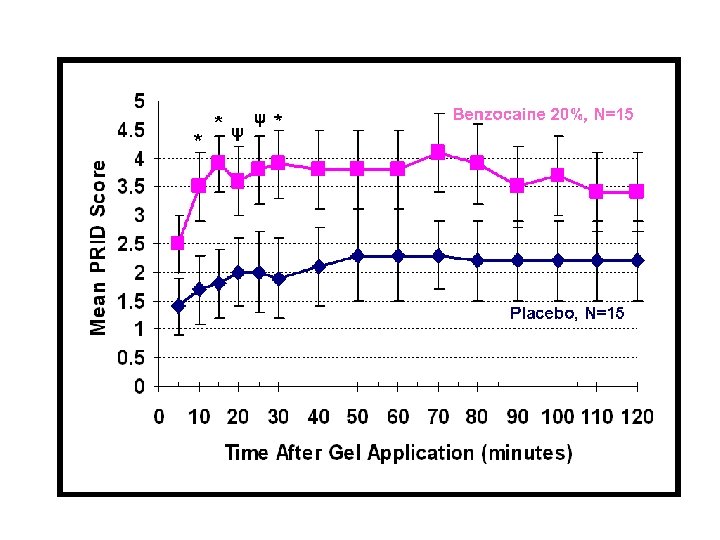
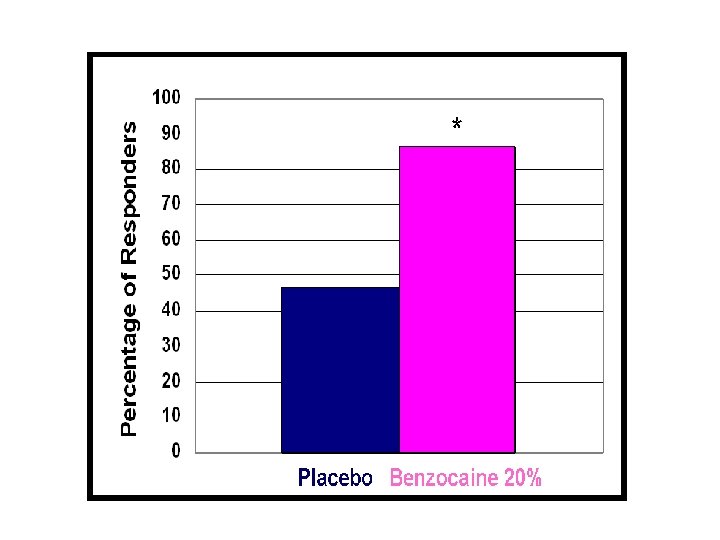
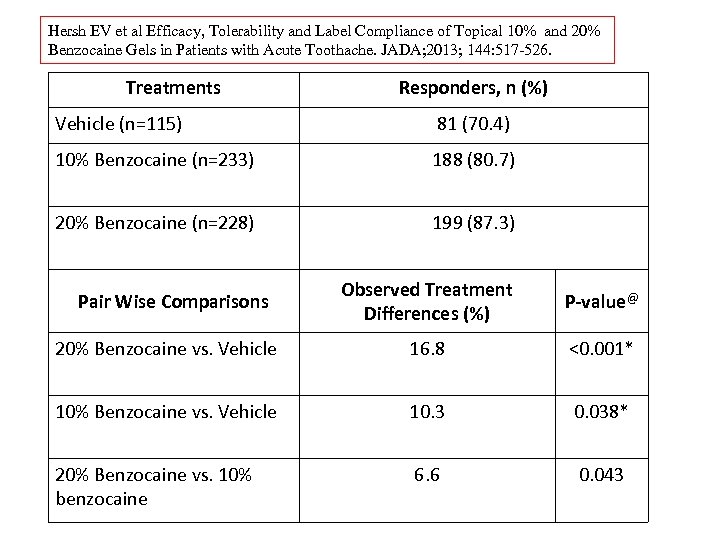
Hersh EV et al Efficacy, Tolerability and Label Compliance of Topical 10% and 20% Benzocaine Gels in Patients with Acute Toothache. JADA; 2013; 144: 517 -526. Treatments Responders, n (%) Vehicle (n=115) 81 (70. 4) 10% Benzocaine (n=233) 188 (80. 7) 20% Benzocaine (n=228) 199 (87. 3) Observed Treatment Differences (%) P-value@ 20% Benzocaine vs. Vehicle 16. 8 <0. 001* 10% Benzocaine vs. Vehicle 10. 3 0. 038* 20% Benzocaine vs. 10% benzocaine 6. 6 0. 043 Pair Wise Comparisons
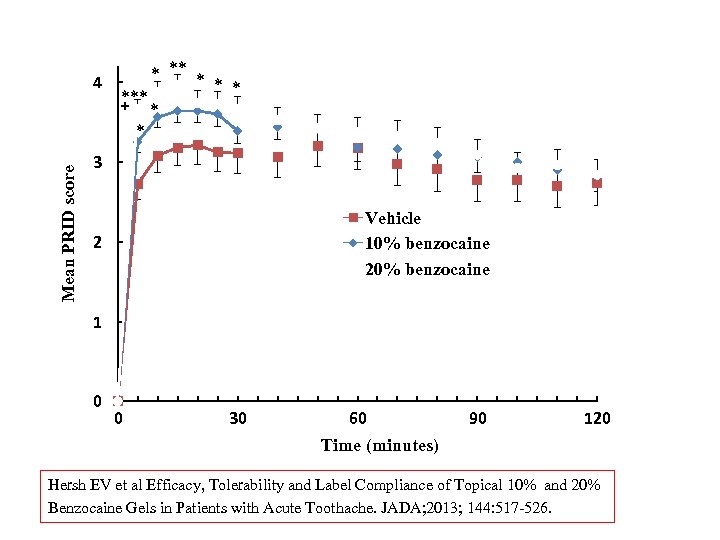
Mean PRID score 4 * *** + * * 3 Vehicle 10% benzocaine 2 1 0 0 30 60 90 120 Time (minutes) Hersh EV et al Efficacy, Tolerability and Label Compliance of Topical 10% and 20% Benzocaine Gels in Patients with Acute Toothache. JADA; 2013; 144: 517 -526.
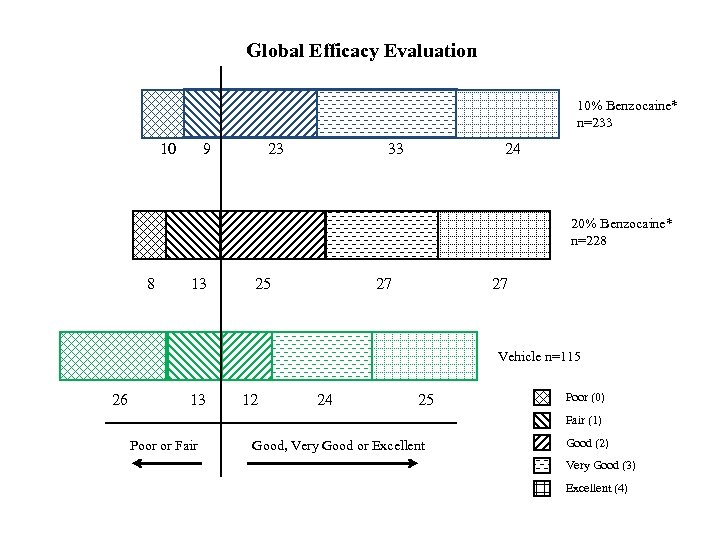
Global Efficacy Evaluation 10% Benzocaine* n=233 10 9 23 33 24 20% Benzocaine* n=228 8 13 25 27 27 Vehicle n=115 26 13 12 24 25 Poor (0) Fair (1) Poor or Fair Good, Very Good or Excellent Good (2) Very Good (3) Excellent (4)
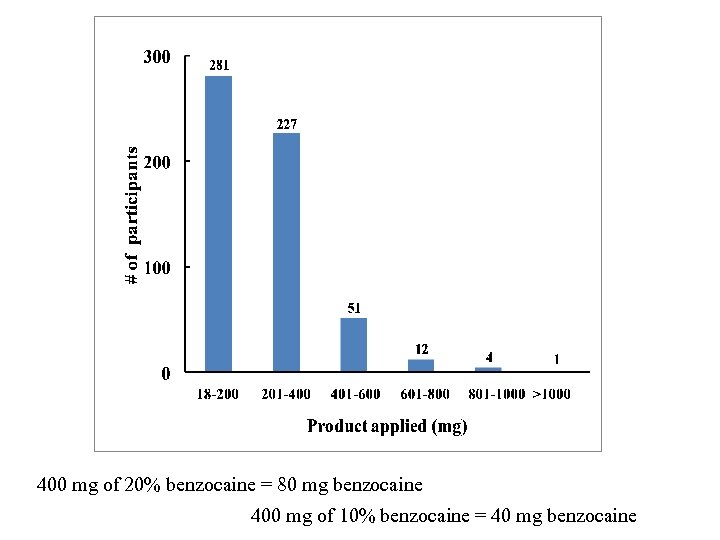
400 mg of 20% benzocaine = 80 mg benzocaine 400 mg of 10% benzocaine = 40 mg benzocaine
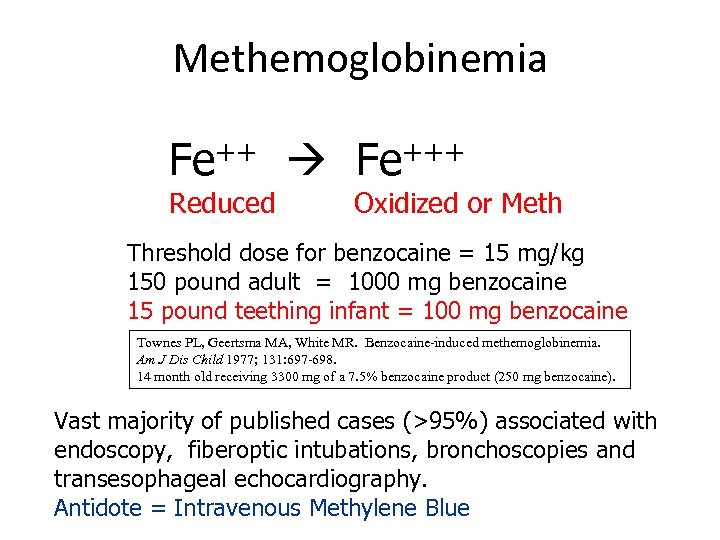
Methemoglobinemia Fe+++ Reduced Oxidized or Meth Threshold dose for benzocaine = 15 mg/kg 150 pound adult = 1000 mg benzocaine 15 pound teething infant = 100 mg benzocaine Townes PL, Geertsma MA, White MR. Benzocaine-induced methemoglobinemia. Am J Dis Child 1977; 131: 697 -698. 14 month old receiving 3300 mg of a 7. 5% benzocaine product (250 mg benzocaine). Vast majority of published cases (>95%) associated with endoscopy, fiberoptic intubations, bronchoscopies and transesophageal echocardiography. Antidote = Intravenous Methylene Blue
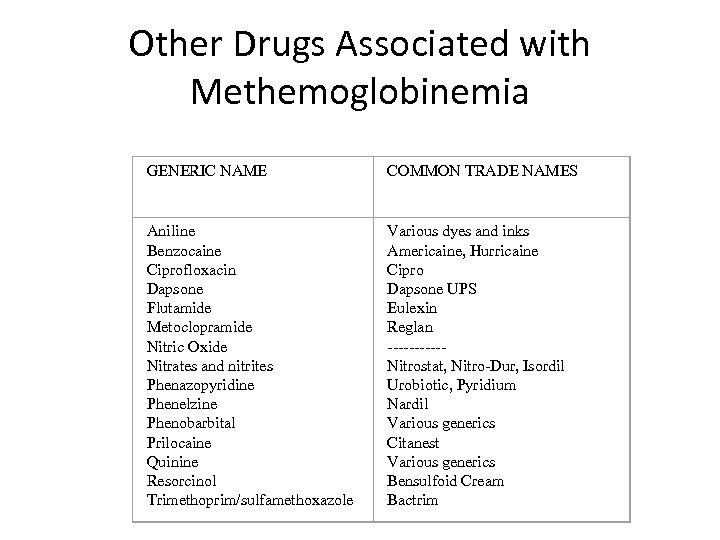
Other Drugs Associated with Methemoglobinemia GENERIC NAME COMMON TRADE NAMES Aniline Benzocaine Ciprofloxacin Dapsone Flutamide Metoclopramide Nitric Oxide Nitrates and nitrites Phenazopyridine Phenelzine Phenobarbital Prilocaine Quinine Resorcinol Trimethoprim/sulfamethoxazole Various dyes and inks Americaine, Hurricaine Cipro Dapsone UPS Eulexin Reglan -----Nitrostat, Nitro-Dur, Isordil Urobiotic, Pyridium Nardil Various generics Citanest Various generics Bensulfoid Cream Bactrim
Topical benzocaine was absolutely awesome for my battery acid burns
WHY USE THIS? St. Renatus, LLC
3% Tetracaine plus 0. 05% Oxymetazoline
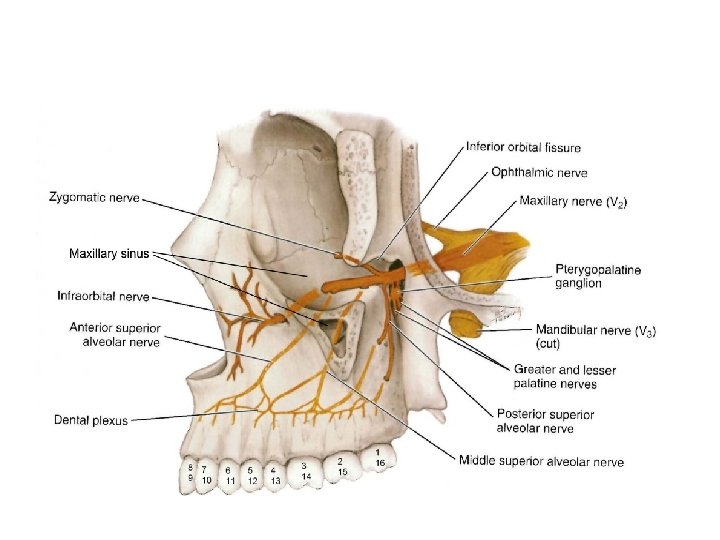
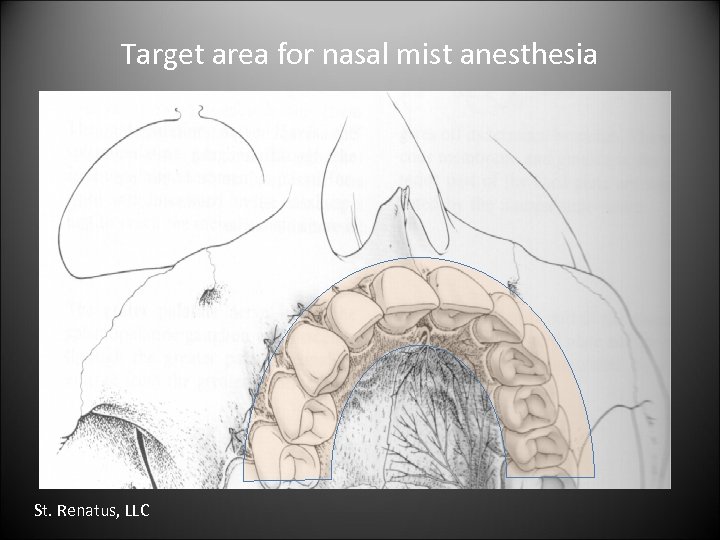
Target area for nasal mist anesthesia St. Renatus, LLC
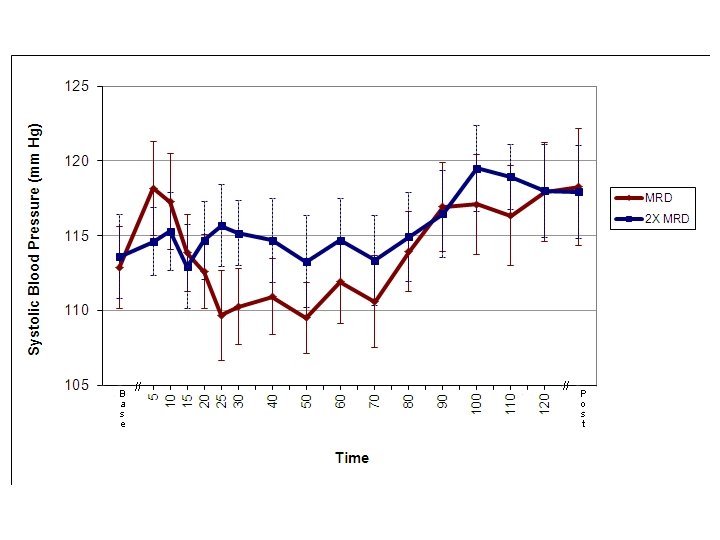
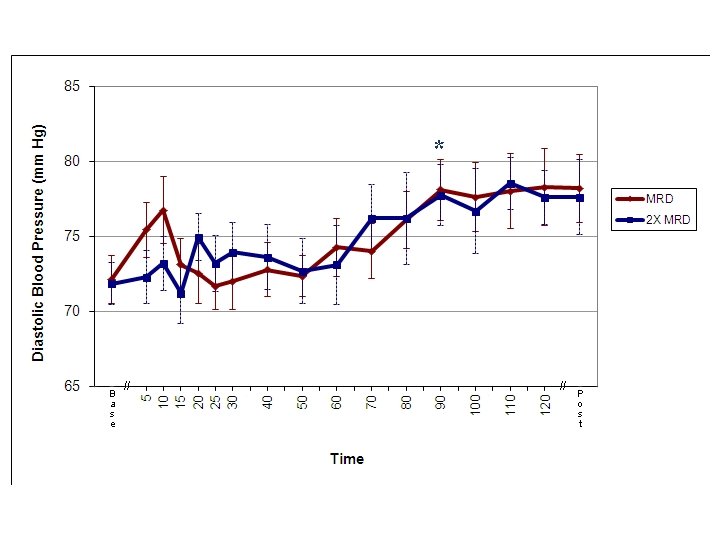
*
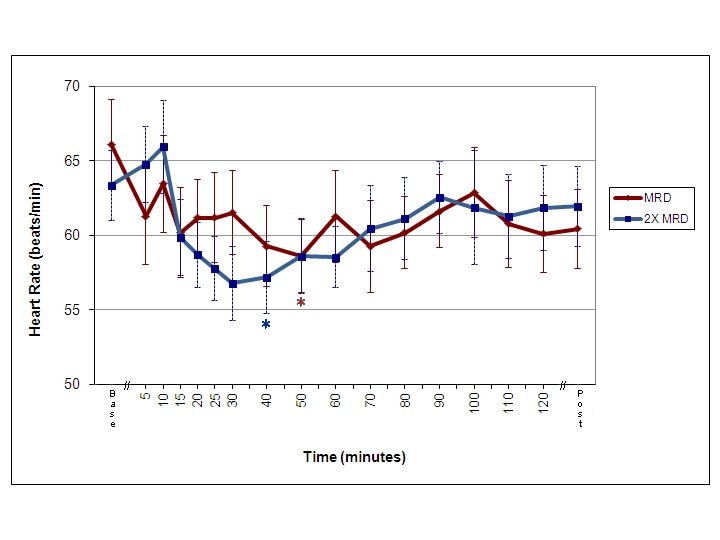
* *
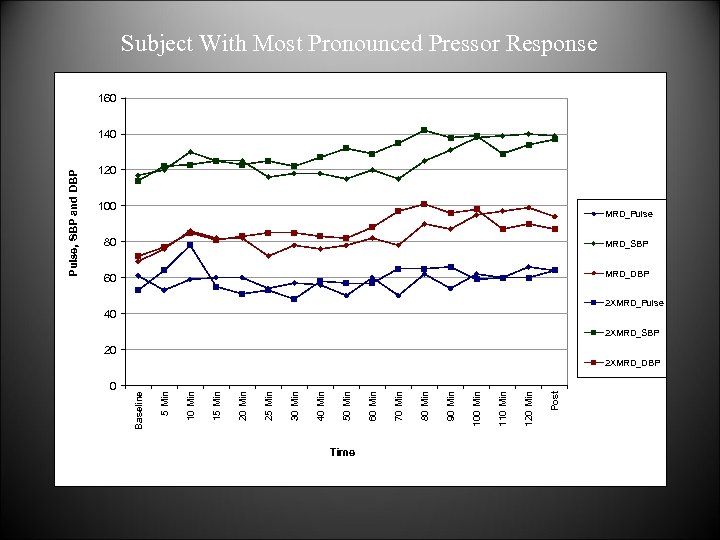
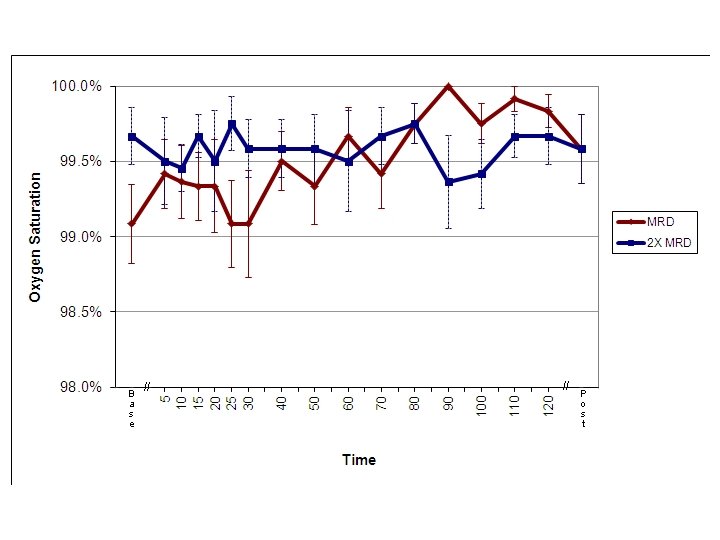
Subject With Most Pronounced Pressor Response 160 120 100 MRD_Pulse 80 MRD_SBP 60 MRD_DBP 2 XMRD_Pulse 40 2 XMRD_SBP 20 Time Post 120 Min 110 Min 100 Min 90 Min 80 Min 70 Min 60 Min 50 Min 40 Min 30 Min 25 Min 20 Min 15 Min 10 Min 0 5 Min 2 XMRD_DBP Baseline Pulse, SBP and DBP 140
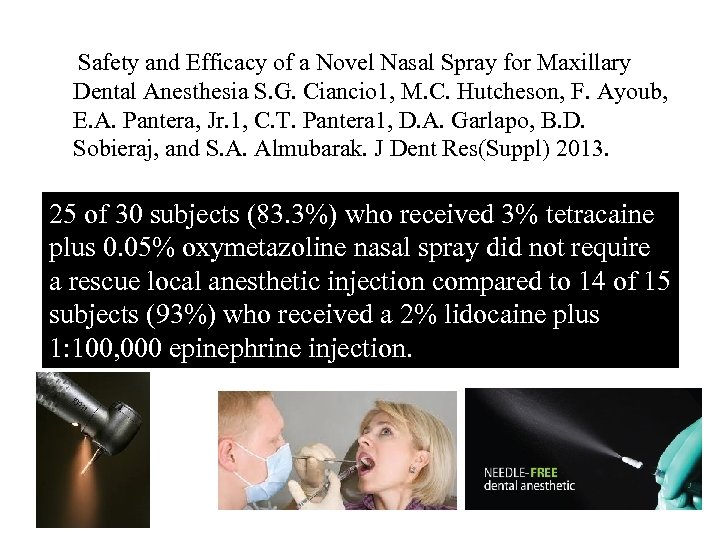
Safety and Efficacy of a Novel Nasal Spray for Maxillary Dental Anesthesia S. G. Ciancio 1, M. C. Hutcheson, F. Ayoub, E. A. Pantera, Jr. 1, C. T. Pantera 1, D. A. Garlapo, B. D. Sobieraj, and S. A. Almubarak. J Dent Res(Suppl) 2013. 25 of 30 subjects (83. 3%) who received 3% tetracaine plus 0. 05% oxymetazoline nasal spray did not require a rescue local anesthetic injection compared to 14 of 15 subjects (93%) who received a 2% lidocaine plus 1: 100, 000 epinephrine injection.
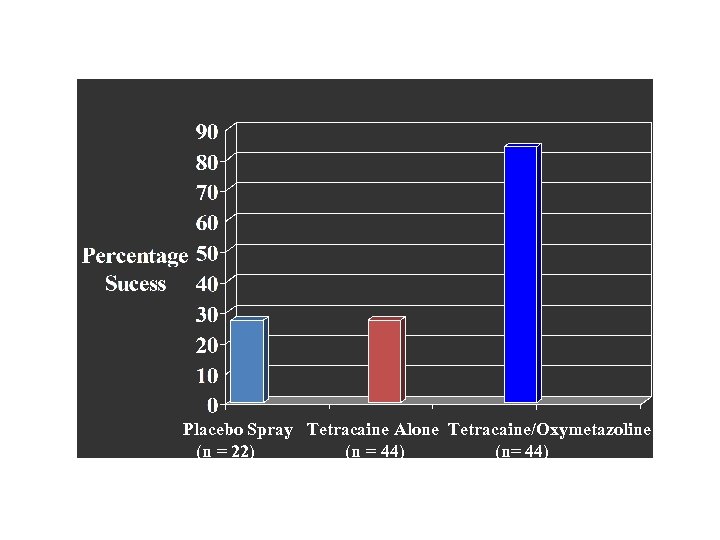
Placebo Spray Tetracaine Alone Tetracaine/Oxymetazoline (n = 22) (n = 44) (n= 44)
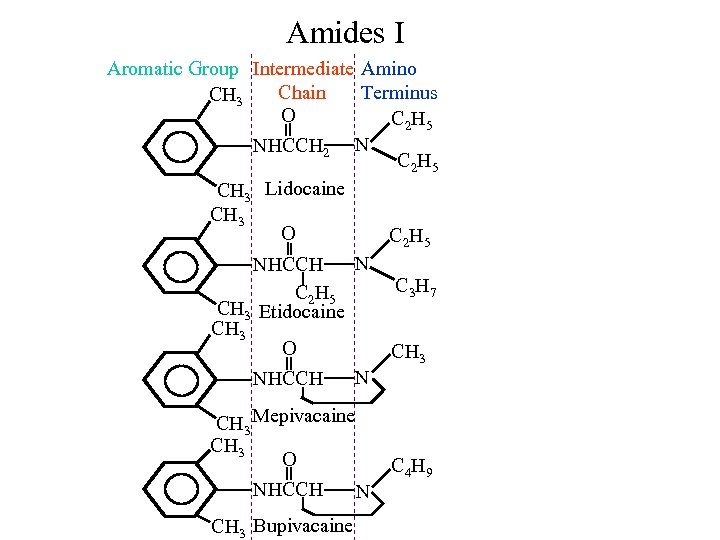
Amides I Aromatic Group Intermediate Amino Chain Terminus CH 3 O C 2 H 5 NHCCH 2 N C 2 H 5 CH 3 Lidocaine CH 3 O C 2 H 5 N NHCCH C 3 H 7 C 2 H 5 CH 3 Etidocaine CH 3 O CH 3 N NHCCH CH 3 Mepivacaine CH 3 O NHCCH N CH 3 Bupivacaine C 4 H 9
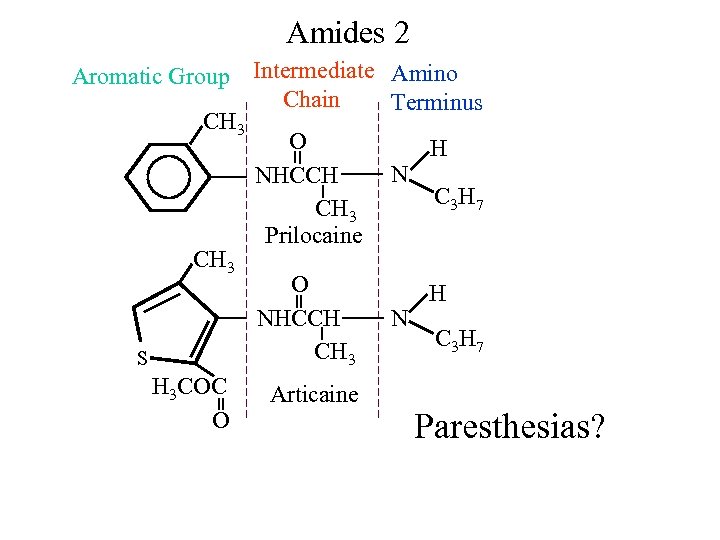
Amides 2 Aromatic Group Intermediate Amino Chain Terminus CH 3 O H N NHCCH C 3 H 7 CH 3 Prilocaine CH 3 O H NHCCH N C 3 H 7 CH 3 S H 3 COC Articaine O Paresthesias?
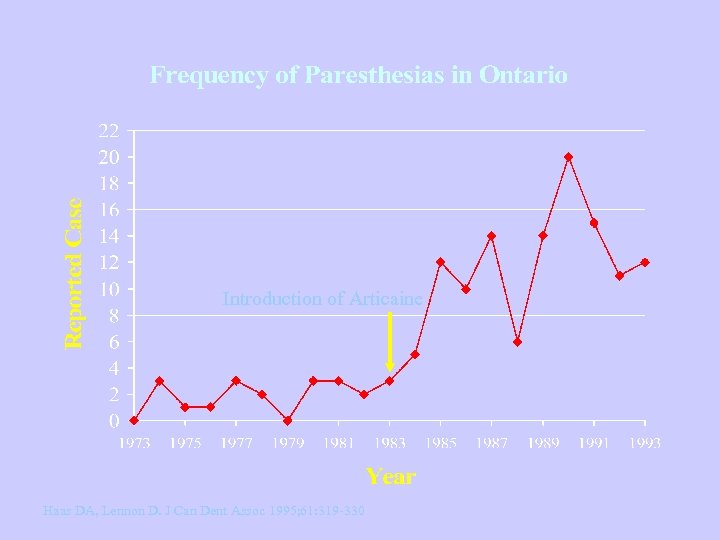
Introduction of Articaine Haas DA, Lennon D. J Can Dent Assoc 1995; 61: 319 -330
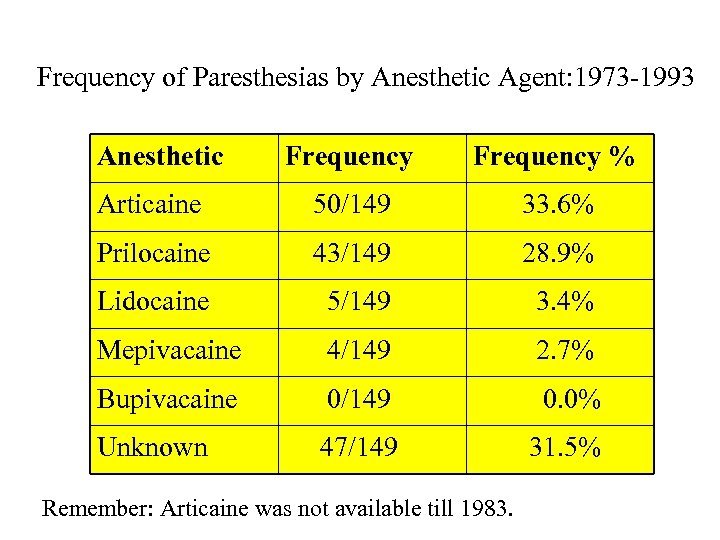
Frequency of Paresthesias by Anesthetic Agent: 1973 -1993 Anesthetic Frequency % Articaine 50/149 33. 6% Prilocaine 43/149 28. 9% Lidocaine 5/149 3. 4% Mepivacaine 4/149 2. 7% Bupivacaine 0/149 0. 0% Unknown 47/149 31. 5% Remember: Articaine was not available till 1983.
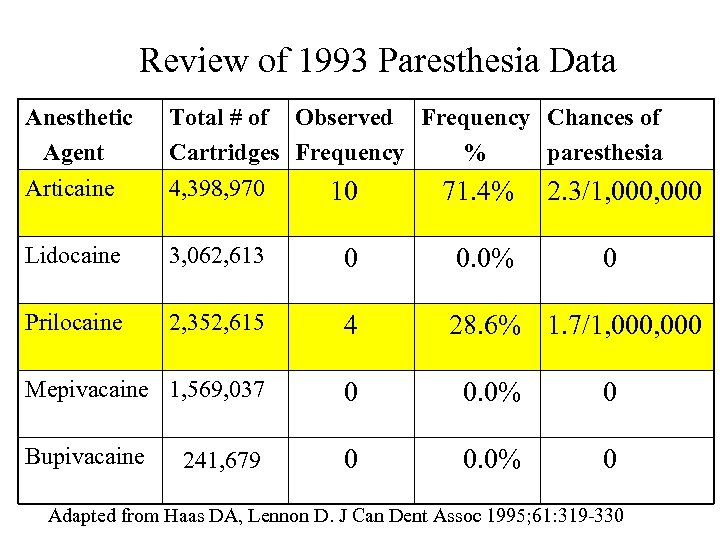
Review of 1993 Paresthesia Data Anesthetic Agent Articaine Total # of Observed Frequency Chances of Cartridges Frequency % paresthesia 4, 398, 970 10 71. 4% 2. 3/1, 000 Lidocaine 3, 062, 613 0 0. 0% Prilocaine 2, 352, 615 4 28. 6% 1. 7/1, 000 Mepivacaine 1, 569, 037 0 0. 0% 0 Bupivacaine 0 0. 0% 0 241, 679 0 Adapted from Haas DA, Lennon D. J Can Dent Assoc 1995; 61: 319 -330
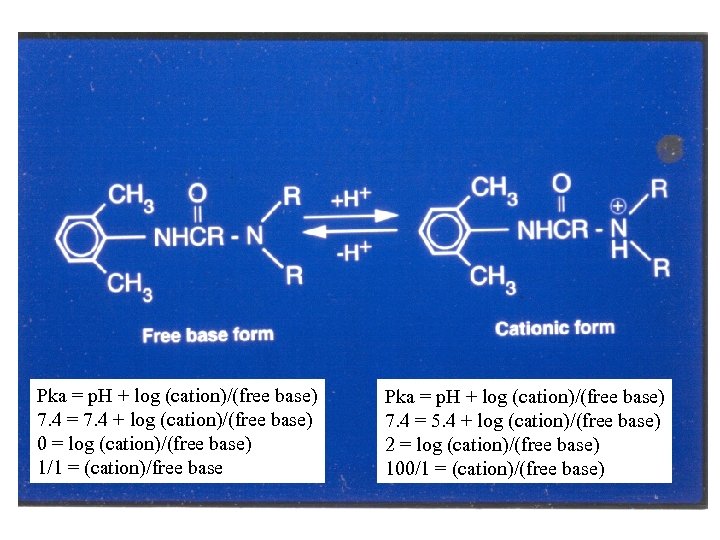
Pka = p. H + log (cation)/(free base) 7. 4 = 7. 4 + log (cation)/(free base) 0 = log (cation)/(free base) 1/1 = (cation)/free base Pka = p. H + log (cation)/(free base) 7. 4 = 5. 4 + log (cation)/(free base) 2 = log (cation)/(free base) 100/1 = (cation)/(free base)
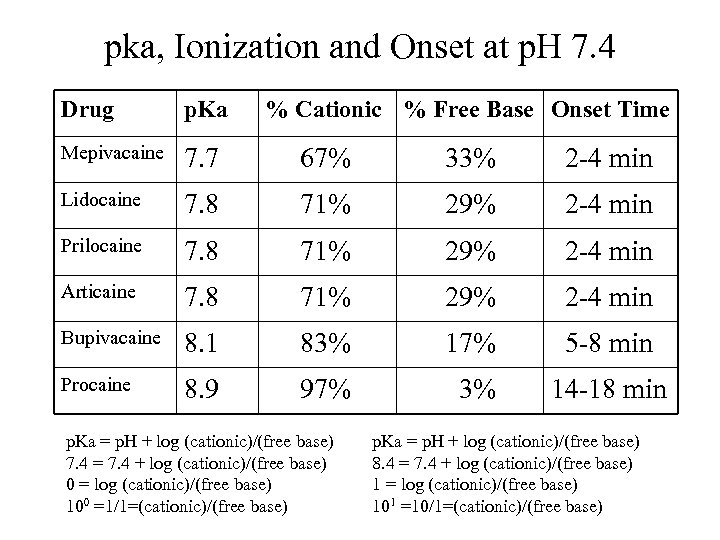
pka, Ionization and Onset at p. H 7. 4 Drug p. Ka % Cationic % Free Base Onset Time Mepivacaine 7. 7 67% 33% 2 -4 min Lidocaine 7. 8 71% 29% 2 -4 min Prilocaine 7. 8 71% 29% 2 -4 min Articaine 7. 8 71% 29% 2 -4 min Bupivacaine 8. 1 83% 17% 5 -8 min Procaine 8. 9 97% 3% 14 -18 min p. Ka = p. H + log (cationic)/(free base) 7. 4 = 7. 4 + log (cationic)/(free base) 0 = log (cationic)/(free base) 100 =1/1=(cationic)/(free base) p. Ka = p. H + log (cationic)/(free base) 8. 4 = 7. 4 + log (cationic)/(free base) 1 = log (cationic)/(free base) 101 =10/1=(cationic)/(free base)
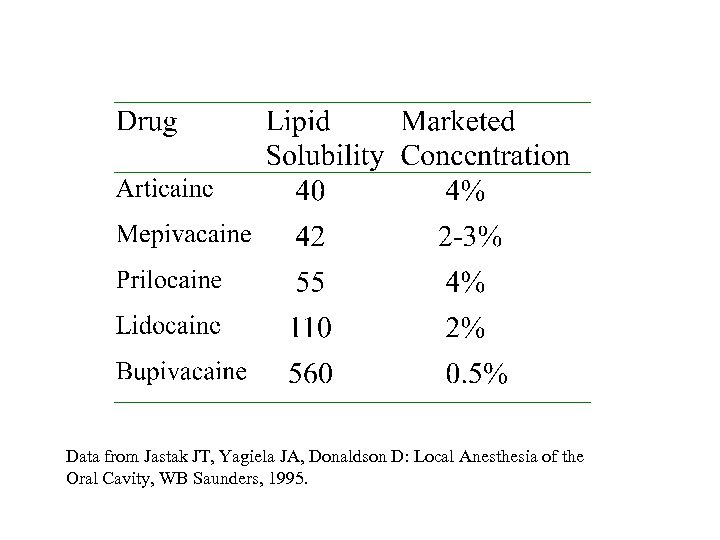
Data from Jastak JT, Yagiela JA, Donaldson D: Local Anesthesia of the Oral Cavity, WB Saunders, 1995.
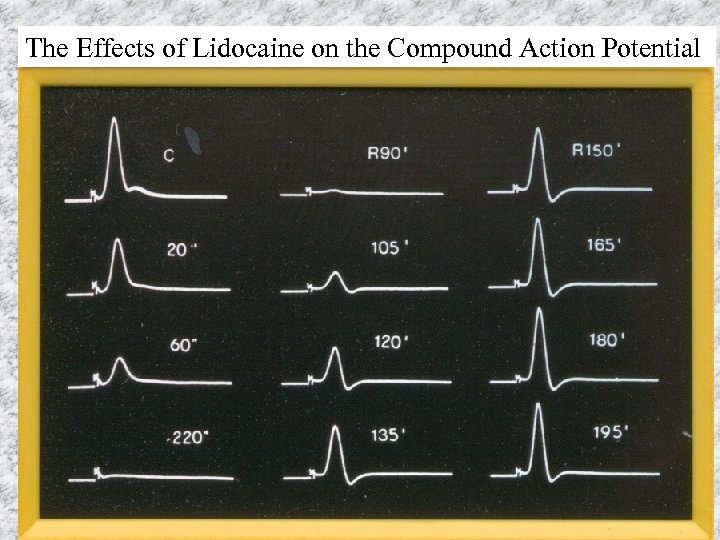
The Effects of Lidocaine on the Compound Action Potential
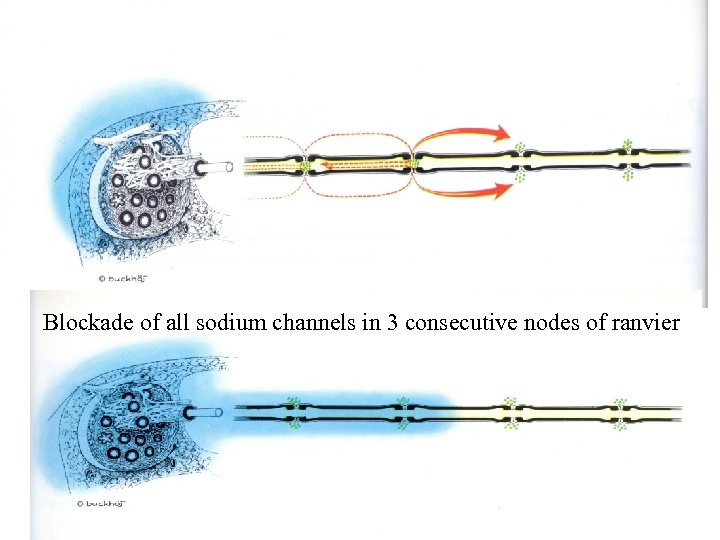
Blockade of all sodium channels in 3 consecutive nodes of ranvier
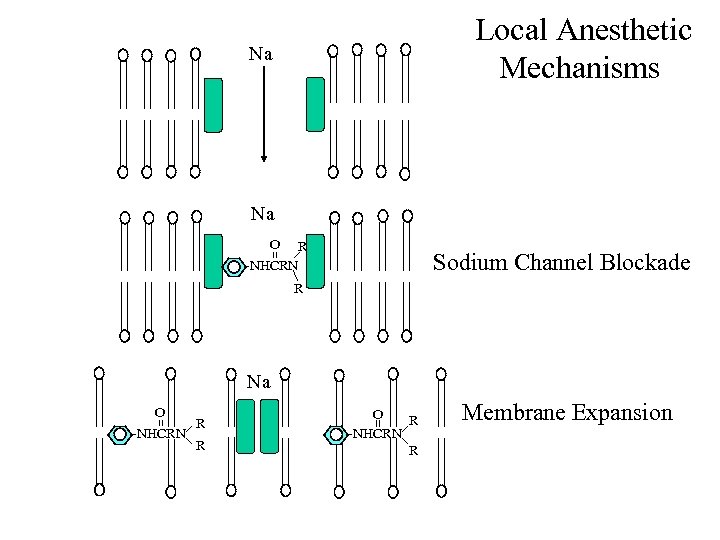
Local Anesthetic Mechanisms Na Na O R -NHCRN Sodium Channel Blockade R Na O -NHCRN R R O R -NHCRN R Membrane Expansion
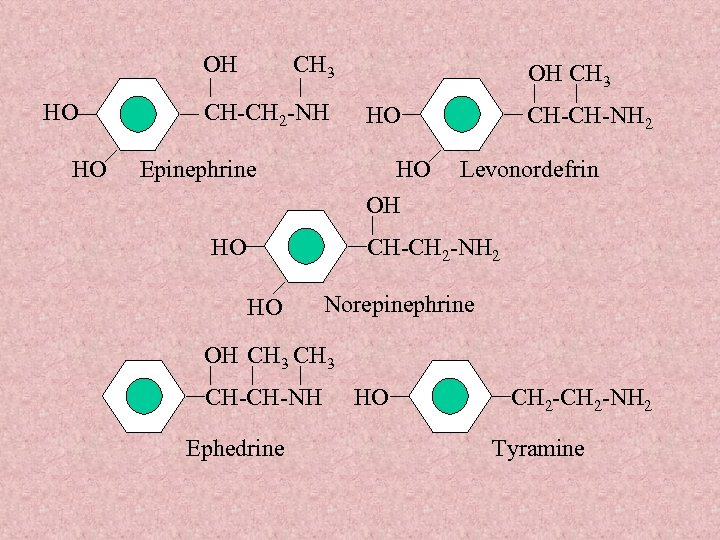
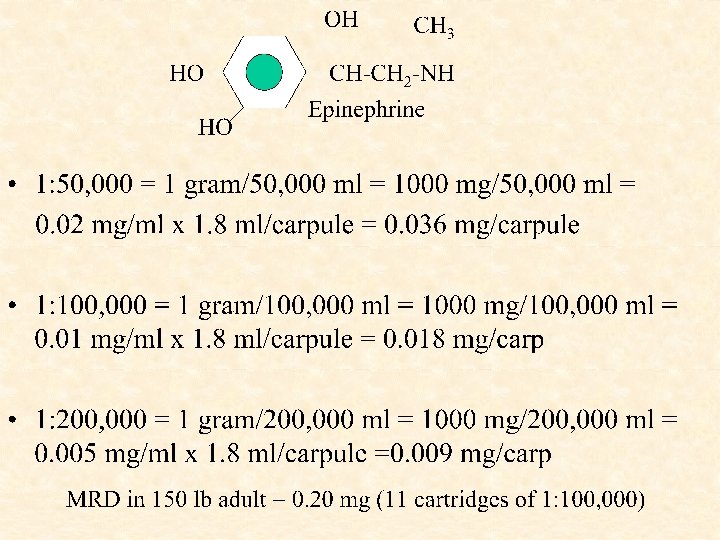
OH HO HO CH 3 CH-CH 2 -NH Epinephrine OH CH 3 HO HO OH HO CH-CH-NH 2 Levonordefrin CH-CH 2 -NH 2 HO Norepinephrine OH CH 3 CH-CH-NH Ephedrine HO CH 2 -NH 2 Tyramine
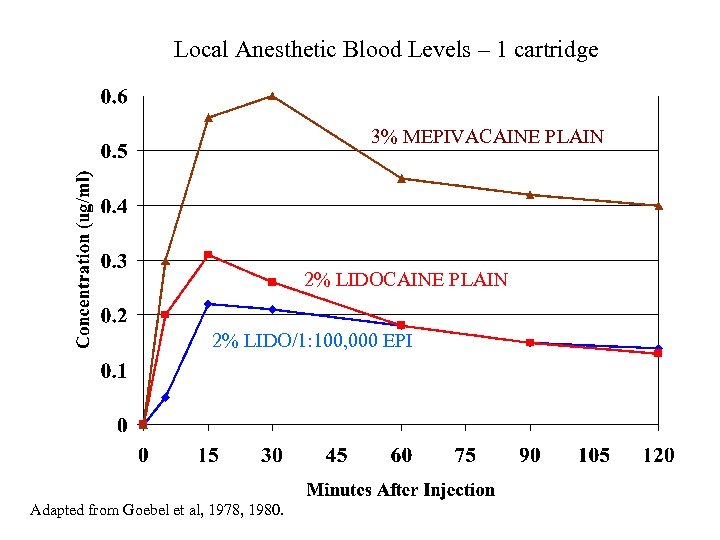
Local Anesthetic Blood Levels – 1 cartridge 3% MEPIVACAINE PLAIN 2% LIDO/1: 100, 000 EPI Adapted from Goebel et al, 1978, 1980.
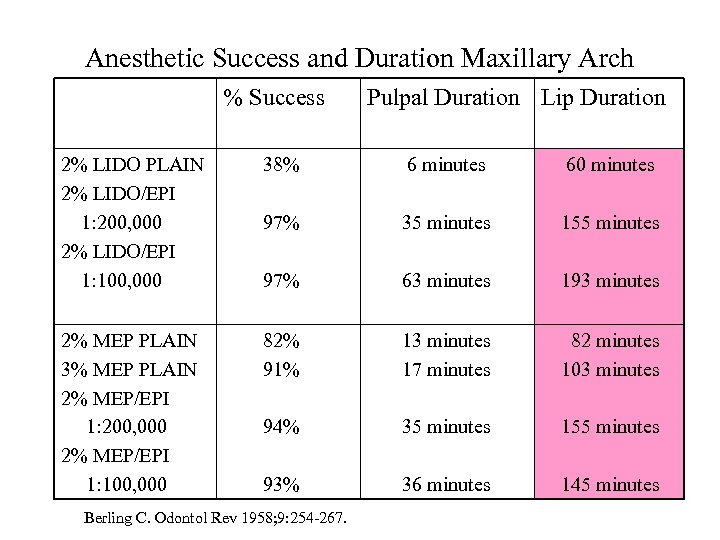
Anesthetic Success and Duration Maxillary Arch % Success Pulpal Duration Lip Duration 2% LIDO PLAIN 2% LIDO/EPI 1: 200, 000 2% LIDO/EPI 1: 100, 000 38% 6 minutes 60 minutes 97% 35 minutes 155 minutes 97% 63 minutes 193 minutes 2% MEP PLAIN 3% MEP PLAIN 2% MEP/EPI 1: 200, 000 2% MEP/EPI 1: 100, 000 82% 91% 13 minutes 17 minutes 82 minutes 103 minutes 94% 35 minutes 155 minutes 93% 36 minutes 145 minutes Berling C. Odontol Rev 1958; 9: 254 -267.
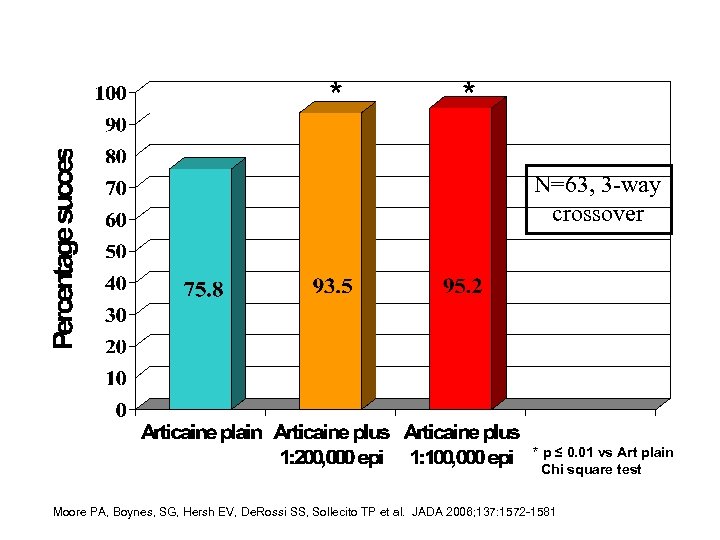
* * N=63, 3 -way crossover * p ≤ 0. 01 vs Art plain Chi square test Moore PA, Boynes, SG, Hersh EV, De. Rossi SS, Sollecito TP et al. JADA 2006; 137: 1572 -1581
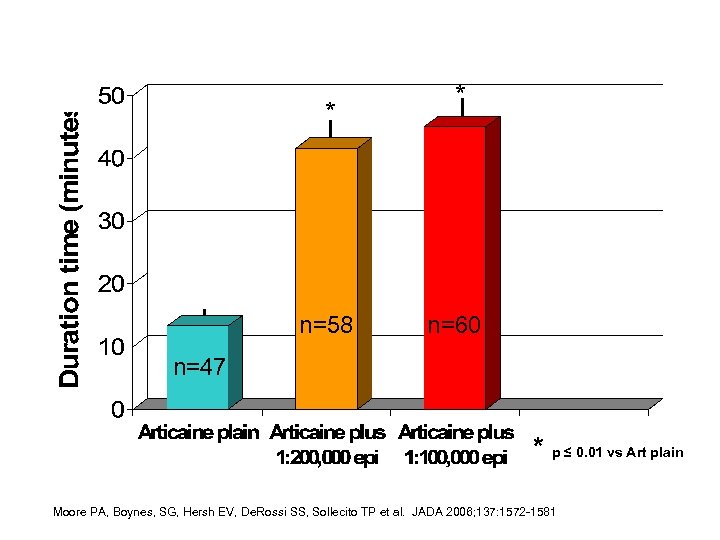
* n=58 * n=60 n=47 * p ≤ 0. 01 vs Art plain Moore PA, Boynes, SG, Hersh EV, De. Rossi SS, Sollecito TP et al. JADA 2006; 137: 1572 -1581
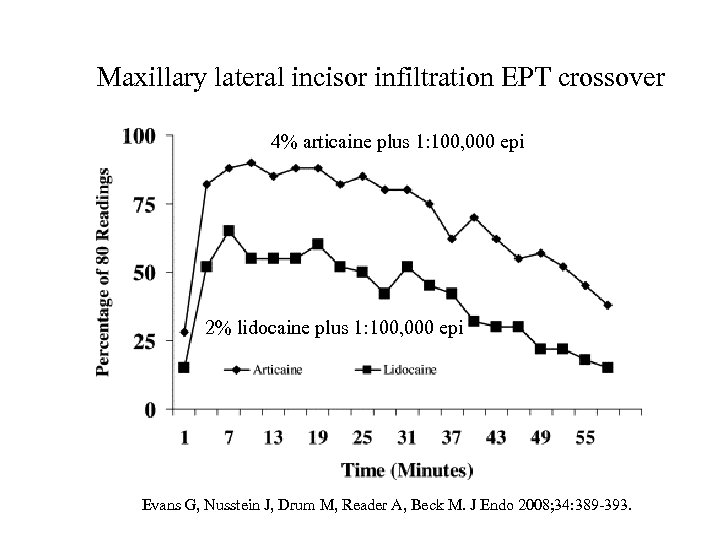
Maxillary lateral incisor infiltration EPT crossover 4% articaine plus 1: 100, 000 epi 2% lidocaine plus 1: 100, 000 epi Evans G, Nusstein J, Drum M, Reader A, Beck M. J Endo 2008; 34: 389 -393.
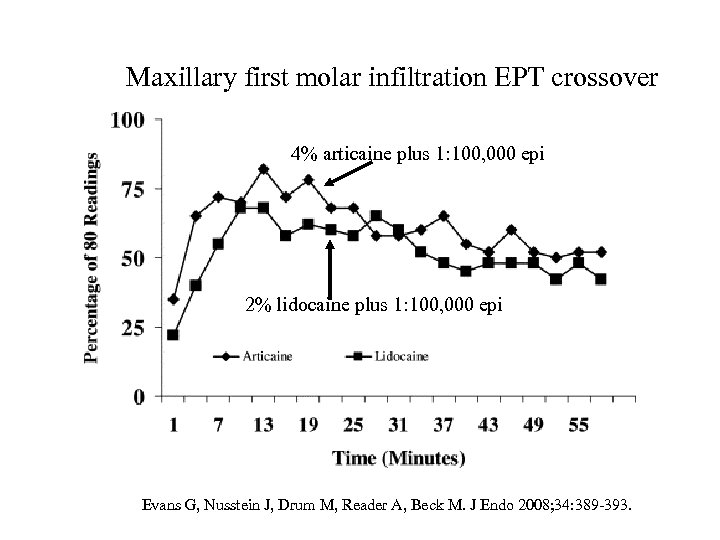
Maxillary first molar infiltration EPT crossover 4% articaine plus 1: 100, 000 epi 2% lidocaine plus 1: 100, 000 epi Evans G, Nusstein J, Drum M, Reader A, Beck M. J Endo 2008; 34: 389 -393.
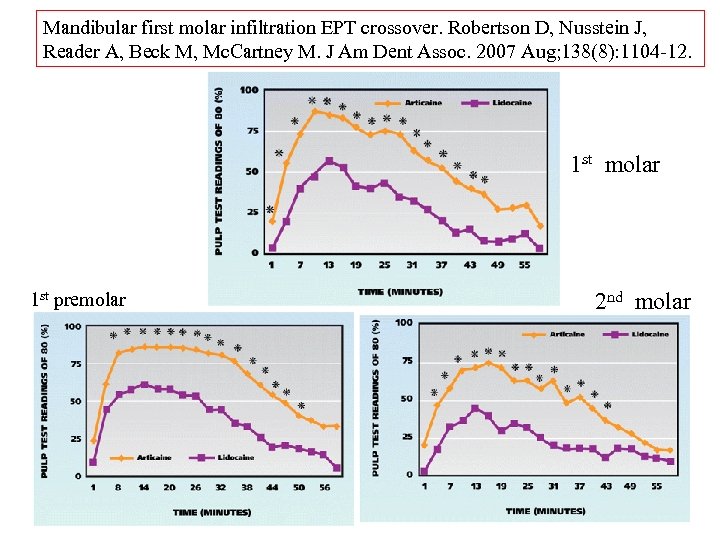
Mandibular first molar infiltration EPT crossover. Robertson D, Nusstein J, Reader A, Beck M, Mc. Cartney M. J Am Dent Assoc. 2007 Aug; 138(8): 1104 -12. 1 st molar 1 st premolar 2 nd molar
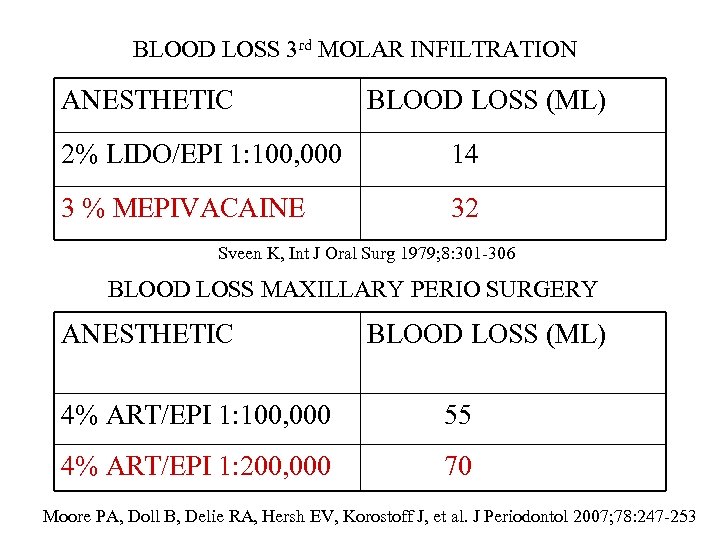
BLOOD LOSS 3 rd MOLAR INFILTRATION ANESTHETIC BLOOD LOSS (ML) 2% LIDO/EPI 1: 100, 000 14 3 % MEPIVACAINE 32 Sveen K, Int J Oral Surg 1979; 8: 301 -306 BLOOD LOSS MAXILLARY PERIO SURGERY ANESTHETIC BLOOD LOSS (ML) 4% ART/EPI 1: 100, 000 55 4% ART/EPI 1: 200, 000 70 Moore PA, Doll B, Delie RA, Hersh EV, Korostoff J, et al. J Periodontol 2007; 78: 247 -253
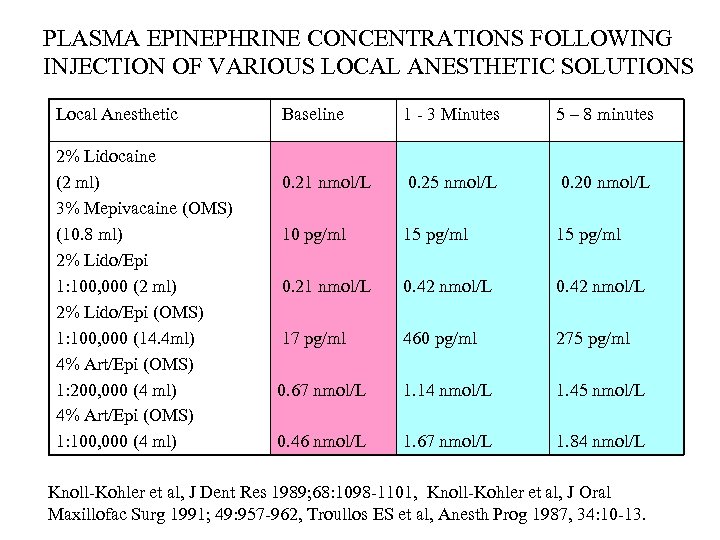
PLASMA EPINEPHRINE CONCENTRATIONS FOLLOWING INJECTION OF VARIOUS LOCAL ANESTHETIC SOLUTIONS Local Anesthetic 2% Lidocaine (2 ml) 3% Mepivacaine (OMS) (10. 8 ml) 2% Lido/Epi 1: 100, 000 (2 ml) 2% Lido/Epi (OMS) 1: 100, 000 (14. 4 ml) 4% Art/Epi (OMS) 1: 200, 000 (4 ml) 4% Art/Epi (OMS) 1: 100, 000 (4 ml) Baseline 1 - 3 Minutes 5 – 8 minutes 0. 21 nmol/L 0. 25 nmol/L 0. 20 nmol/L 10 pg/ml 15 pg/ml 0. 21 nmol/L 0. 42 nmol/L 17 pg/ml 460 pg/ml 275 pg/ml 0. 67 nmol/L 1. 14 nmol/L 1. 45 nmol/L 0. 46 nmol/L 1. 67 nmol/L 1. 84 nmol/L Knoll-Kohler et al, J Dent Res 1989; 68: 1098 -1101, Knoll-Kohler et al, J Oral Maxillofac Surg 1991; 49: 957 -962, Troullos ES et al, Anesth Prog 1987, 34: 10 -13.
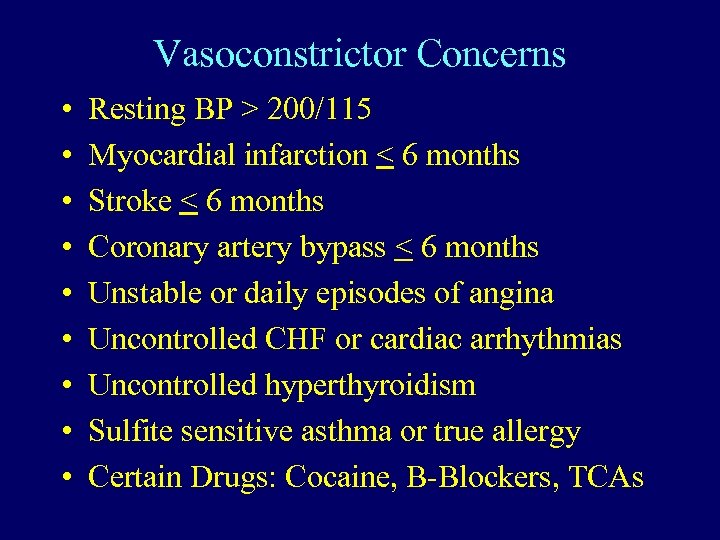
Vasoconstrictor Concerns • • • Resting BP > 200/115 Myocardial infarction < 6 months Stroke < 6 months Coronary artery bypass < 6 months Unstable or daily episodes of angina Uncontrolled CHF or cardiac arrhythmias Uncontrolled hyperthyroidism Sulfite sensitive asthma or true allergy Certain Drugs: Cocaine, B-Blockers, TCAs
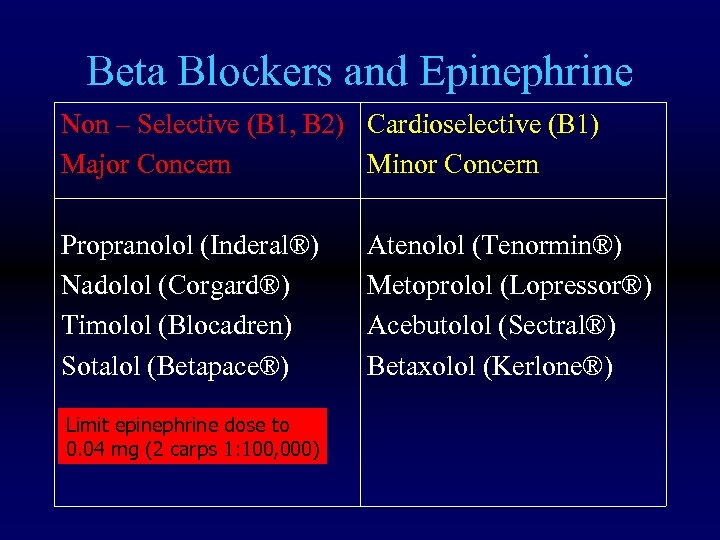
Beta Blockers and Epinephrine Non – Selective (B 1, B 2) Cardioselective (B 1) Major Concern Minor Concern Propranolol (Inderal®) Nadolol (Corgard®) Timolol (Blocadren) Sotalol (Betapace®) Limit epinephrine dose to 0. 04 mg (2 carps 1: 100, 000) Atenolol (Tenormin®) Metoprolol (Lopressor®) Acebutolol (Sectral®) Betaxolol (Kerlone®)
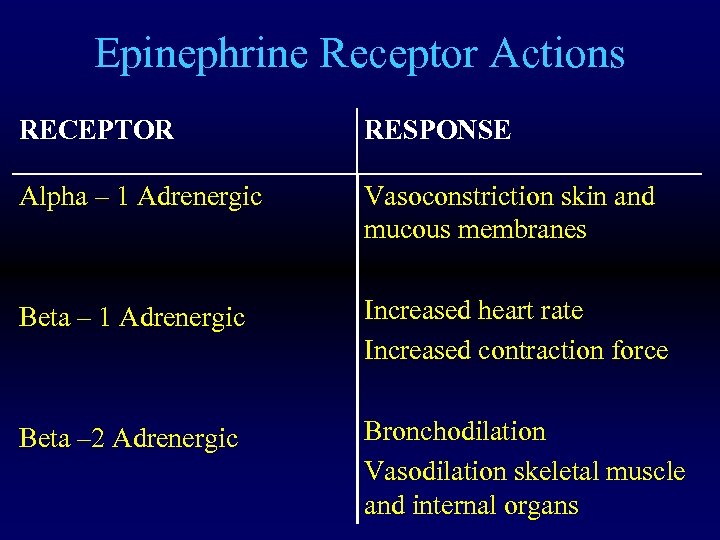
Epinephrine Receptor Actions RECEPTOR RESPONSE Alpha – 1 Adrenergic Vasoconstriction skin and mucous membranes Beta – 1 Adrenergic Increased heart rate Increased contraction force Beta – 2 Adrenergic Bronchodilation Vasodilation skeletal muscle and internal organs
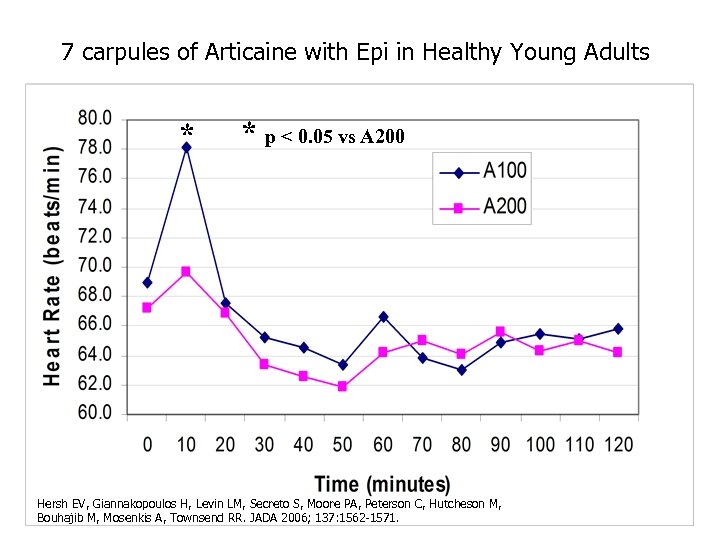
7 carpules of Articaine with Epi in Healthy Young Adults * * p < 0. 05 vs A 200 Hersh EV, Giannakopoulos H, Levin LM, Secreto S, Moore PA, Peterson C, Hutcheson M, Bouhajib M, Mosenkis A, Townsend RR. JADA 2006; 137: 1562 -1571.
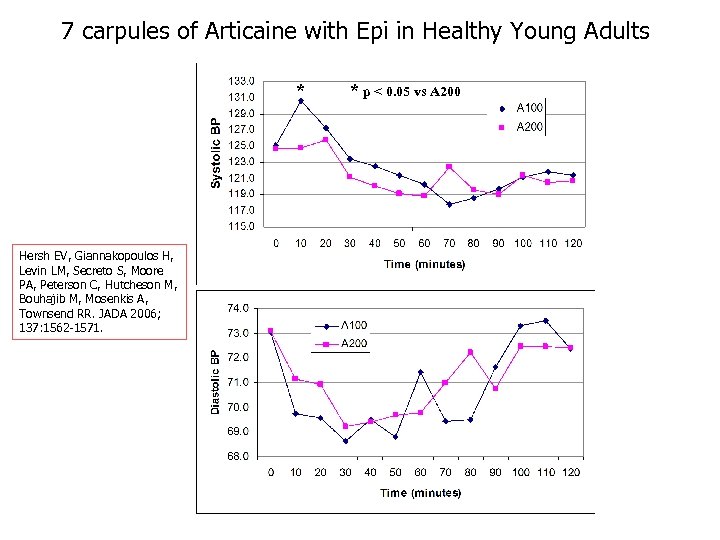
7 carpules of Articaine with Epi in Healthy Young Adults * Hersh EV, Giannakopoulos H, Levin LM, Secreto S, Moore PA, Peterson C, Hutcheson M, Bouhajib M, Mosenkis A, Townsend RR. JADA 2006; 137: 1562 -1571. * p < 0. 05 vs A 200
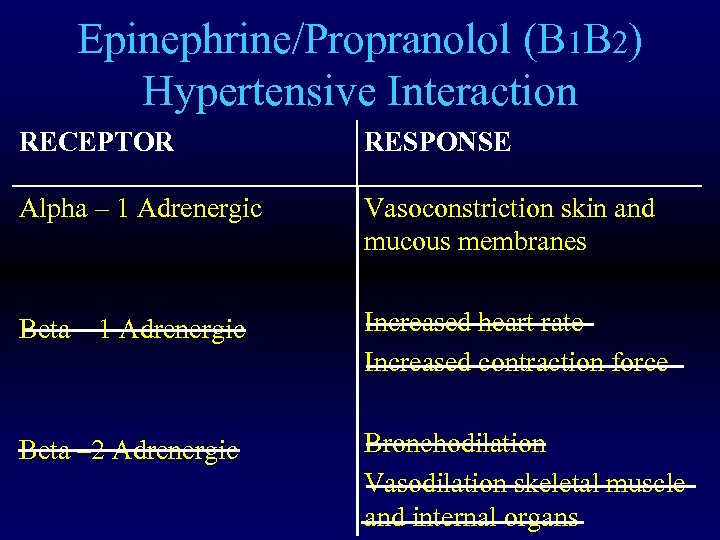
Epinephrine/Propranolol (B 1 B 2) Hypertensive Interaction RECEPTOR RESPONSE Alpha – 1 Adrenergic Vasoconstriction skin and mucous membranes Beta – 1 Adrenergic Increased heart rate Increased contraction force Beta – 2 Adrenergic Bronchodilation Vasodilation skeletal muscle and internal organs
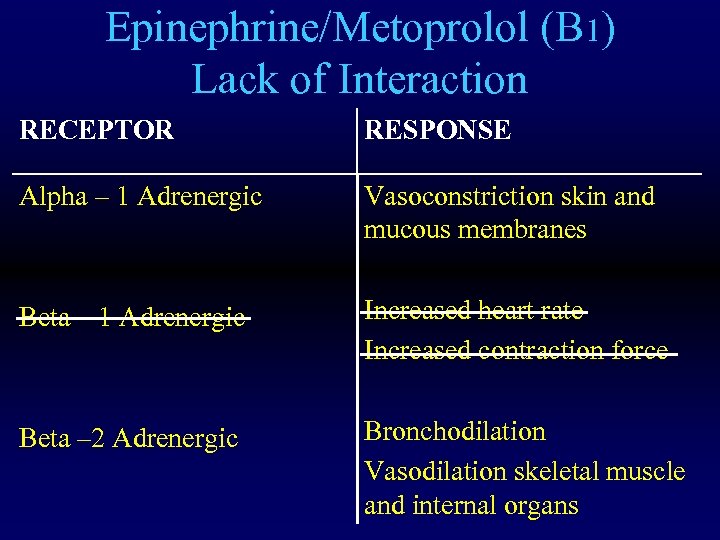
Epinephrine/Metoprolol (B 1) Lack of Interaction RECEPTOR RESPONSE Alpha – 1 Adrenergic Vasoconstriction skin and mucous membranes Beta – 1 Adrenergic Increased heart rate Increased contraction force Beta – 2 Adrenergic Bronchodilation Vasodilation skeletal muscle and internal organs
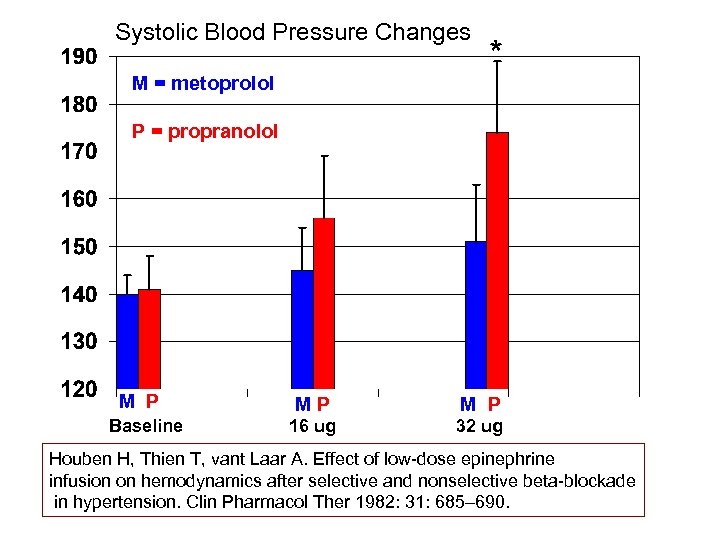
Systolic Blood Pressure Changes M = metoprolol * P = propranolol M P Baseline MP M P 16 ug 32 ug Houben H, Thien T, vant Laar A. Effect of low-dose epinephrine infusion on hemodynamics after selective and nonselective beta-blockade in hypertension. Clin Pharmacol Ther 1982: 31: 685– 690.
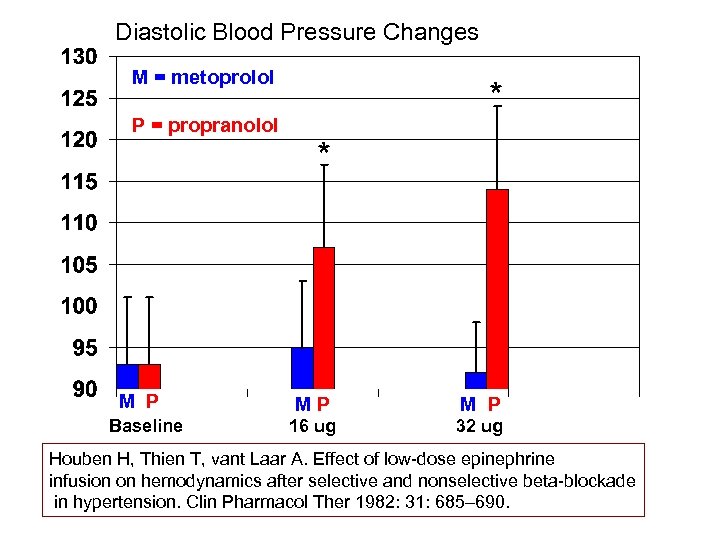
Diastolic Blood Pressure Changes M = metoprolol P = propranolol M P Baseline * * MP M P 16 ug 32 ug Houben H, Thien T, vant Laar A. Effect of low-dose epinephrine infusion on hemodynamics after selective and nonselective beta-blockade in hypertension. Clin Pharmacol Ther 1982: 31: 685– 690.
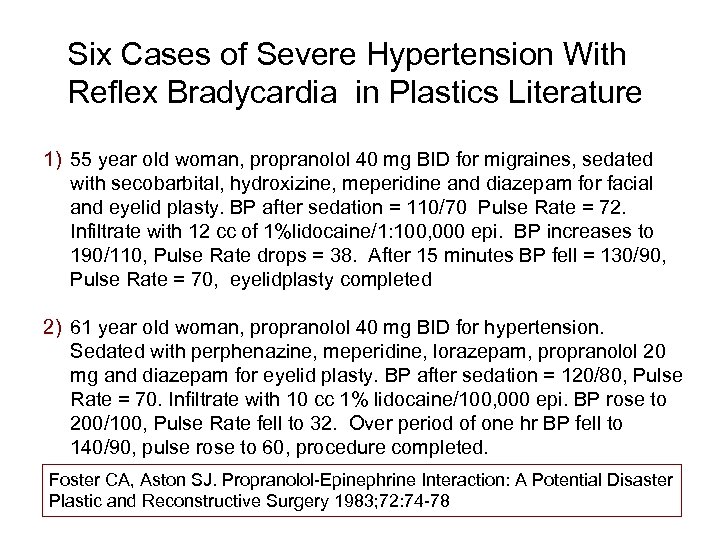
Six Cases of Severe Hypertension With Reflex Bradycardia in Plastics Literature 1) 55 year old woman, propranolol 40 mg BID for migraines, sedated with secobarbital, hydroxizine, meperidine and diazepam for facial and eyelid plasty. BP after sedation = 110/70 Pulse Rate = 72. Infiltrate with 12 cc of 1%lidocaine/1: 100, 000 epi. BP increases to 190/110, Pulse Rate drops = 38. After 15 minutes BP fell = 130/90, Pulse Rate = 70, eyelidplasty completed 2) 61 year old woman, propranolol 40 mg BID for hypertension. Sedated with perphenazine, meperidine, lorazepam, propranolol 20 mg and diazepam for eyelid plasty. BP after sedation = 120/80, Pulse Rate = 70. Infiltrate with 10 cc 1% lidocaine/100, 000 epi. BP rose to 200/100, Pulse Rate fell to 32. Over period of one hr BP fell to 140/90, pulse rose to 60, procedure completed. Foster CA, Aston SJ. Propranolol-Epinephrine Interaction: A Potential Disaster Plastic and Reconstructive Surgery 1983; 72: 74 -78
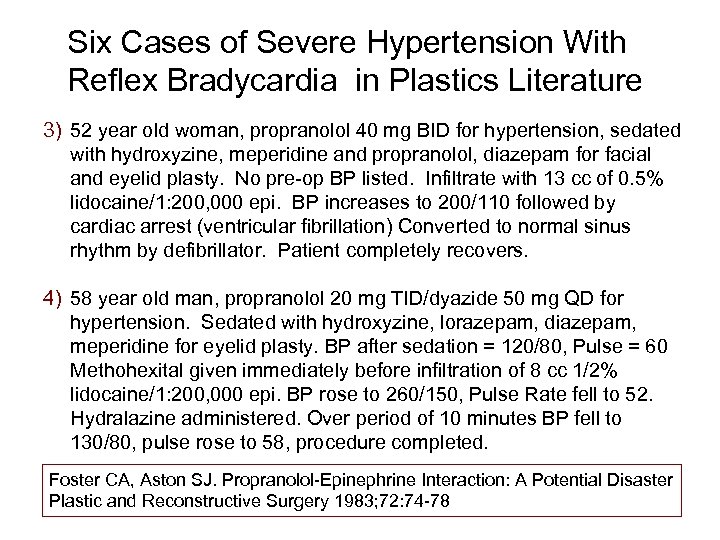
Six Cases of Severe Hypertension With Reflex Bradycardia in Plastics Literature 3) 52 year old woman, propranolol 40 mg BID for hypertension, sedated with hydroxyzine, meperidine and propranolol, diazepam for facial and eyelid plasty. No pre-op BP listed. Infiltrate with 13 cc of 0. 5% lidocaine/1: 200, 000 epi. BP increases to 200/110 followed by cardiac arrest (ventricular fibrillation) Converted to normal sinus rhythm by defibrillator. Patient completely recovers. 4) 58 year old man, propranolol 20 mg TID/dyazide 50 mg QD for hypertension. Sedated with hydroxyzine, lorazepam, diazepam, meperidine for eyelid plasty. BP after sedation = 120/80, Pulse = 60 Methohexital given immediately before infiltration of 8 cc 1/2% lidocaine/1: 200, 000 epi. BP rose to 260/150, Pulse Rate fell to 52. Hydralazine administered. Over period of 10 minutes BP fell to 130/80, pulse rose to 58, procedure completed. Foster CA, Aston SJ. Propranolol-Epinephrine Interaction: A Potential Disaster Plastic and Reconstructive Surgery 1983; 72: 74 -78
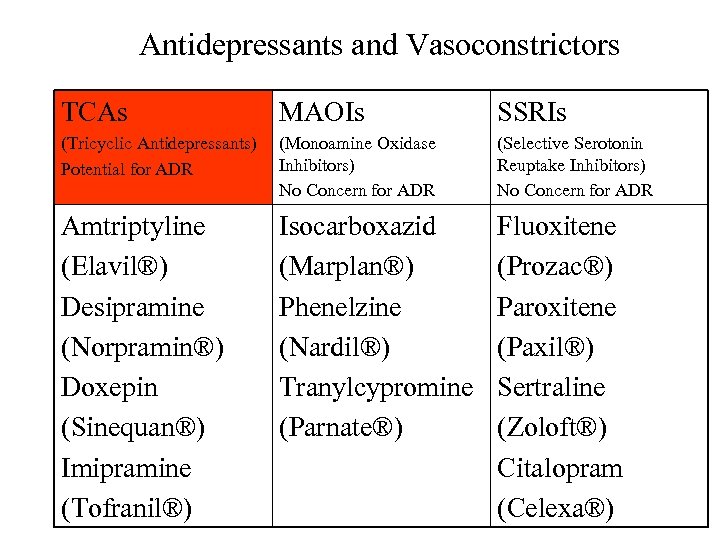
Antidepressants and Vasoconstrictors TCAs MAOIs SSRIs (Tricyclic Antidepressants) Potential for ADR (Monoamine Oxidase Inhibitors) No Concern for ADR (Selective Serotonin Reuptake Inhibitors) No Concern for ADR Amtriptyline (Elavil®) Desipramine (Norpramin®) Doxepin (Sinequan®) Imipramine (Tofranil®) Isocarboxazid (Marplan®) Phenelzine (Nardil®) Tranylcypromine (Parnate®) Fluoxitene (Prozac®) Paroxitene (Paxil®) Sertraline (Zoloft®) Citalopram (Celexa®)
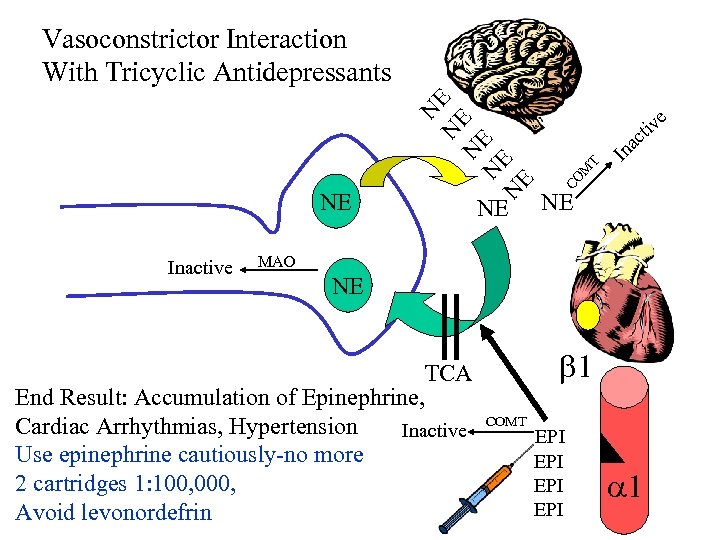
Inactive NE e tiv c a CO M T NE N N E N E E Vasoconstrictor Interaction With Tricyclic Antidepressants In NE MAO NE TCA End Result: Accumulation of Epinephrine, Cardiac Arrhythmias, Hypertension Inactive Use epinephrine cautiously-no more 2 cartridges 1: 100, 000, Avoid levonordefrin 1 COMT EPI EPI 1
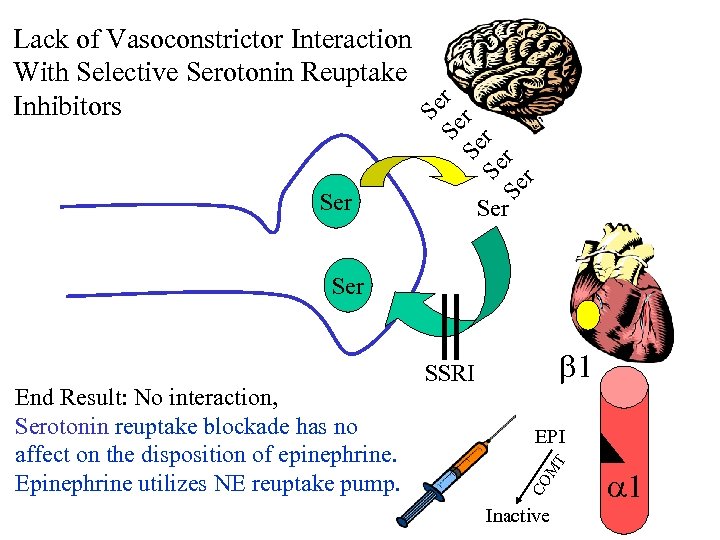
Ser Se Se r r Lack of Vasoconstrictor Interaction With Selective Serotonin Reuptake Inhibitors Ser M T EPI CO End Result: No interaction, Serotonin reuptake blockade has no affect on the disposition of epinephrine. Epinephrine utilizes NE reuptake pump. 1 SSRI Inactive 1
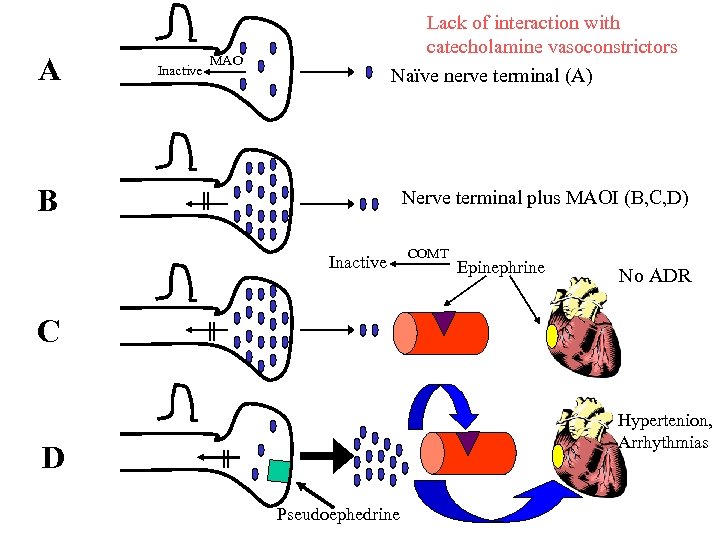
A Inactive Lack of interaction with catecholamine vasoconstrictors Naïve nerve terminal (A) MAO B Nerve terminal plus MAOI (B, C, D) Inactive COMT Epinephrine No ADR C Hypertenion, Arrhythmias D Pseudoephedrine
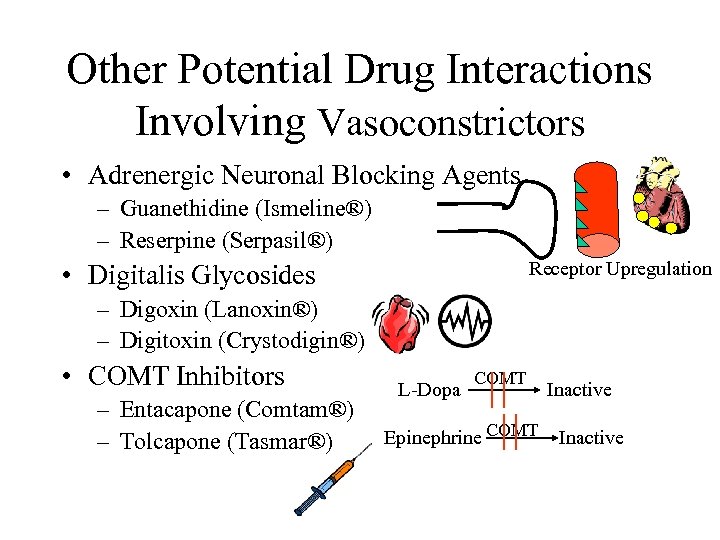
Other Potential Drug Interactions Involving Vasoconstrictors • Adrenergic Neuronal Blocking Agents – Guanethidine (Ismeline®) – Reserpine (Serpasil®) Receptor Upregulation • Digitalis Glycosides – Digoxin (Lanoxin®) – Digitoxin (Crystodigin®) • COMT Inhibitors – Entacapone (Comtam®) – Tolcapone (Tasmar®) L-Dopa COMT Epinephrine COMT Inactive
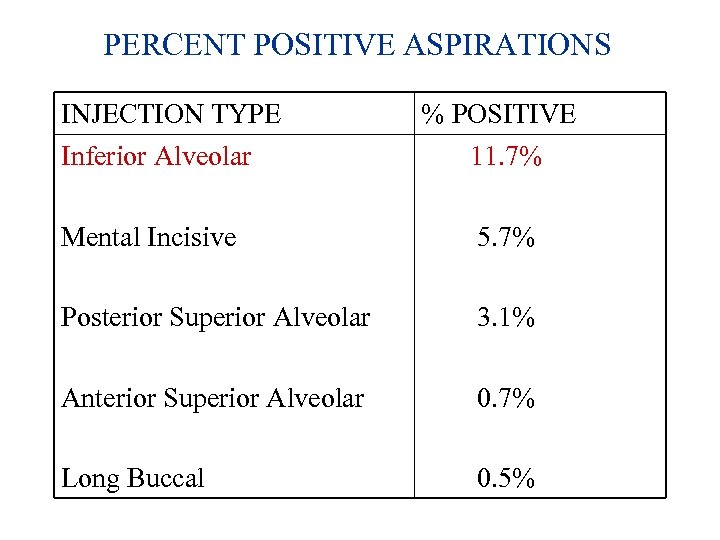
PERCENT POSITIVE ASPIRATIONS INJECTION TYPE Inferior Alveolar % POSITIVE 11. 7% Mental Incisive 5. 7% Posterior Superior Alveolar 3. 1% Anterior Superior Alveolar 0. 7% Long Buccal 0. 5%
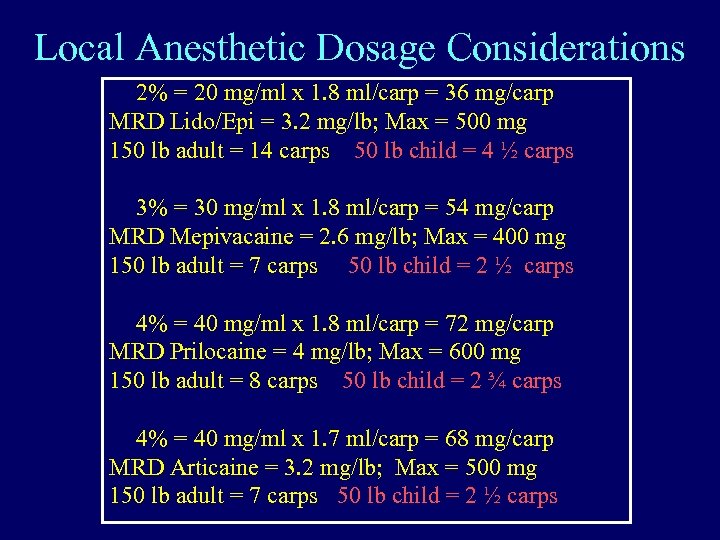
Local Anesthetic Dosage Considerations 2% = 20 mg/ml x 1. 8 ml/carp = 36 mg/carp MRD Lido/Epi = 3. 2 mg/lb; Max = 500 mg 150 lb adult = 14 carps 50 lb child = 4 ½ carps 3% = 30 mg/ml x 1. 8 ml/carp = 54 mg/carp MRD Mepivacaine = 2. 6 mg/lb; Max = 400 mg 150 lb adult = 7 carps 50 lb child = 2 ½ carps 4% = 40 mg/ml x 1. 8 ml/carp = 72 mg/carp MRD Prilocaine = 4 mg/lb; Max = 600 mg 150 lb adult = 8 carps 50 lb child = 2 ¾ carps 4% = 40 mg/ml x 1. 7 ml/carp = 68 mg/carp MRD Articaine = 3. 2 mg/lb; Max = 500 mg 150 lb adult = 7 carps 50 lb child = 2 ½ carps
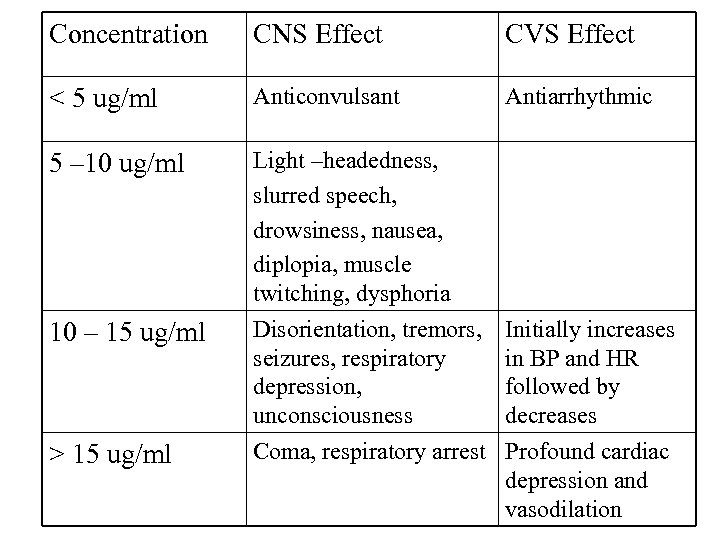
Concentration CNS Effect CVS Effect < 5 ug/ml Anticonvulsant Antiarrhythmic 5 – 10 ug/ml Light –headedness, slurred speech, drowsiness, nausea, diplopia, muscle twitching, dysphoria Disorientation, tremors, seizures, respiratory depression, unconsciousness Coma, respiratory arrest 10 – 15 ug/ml > 15 ug/ml Initially increases in BP and HR followed by decreases Profound cardiac depression and vasodilation
Why the heck did you take my sneaker off?
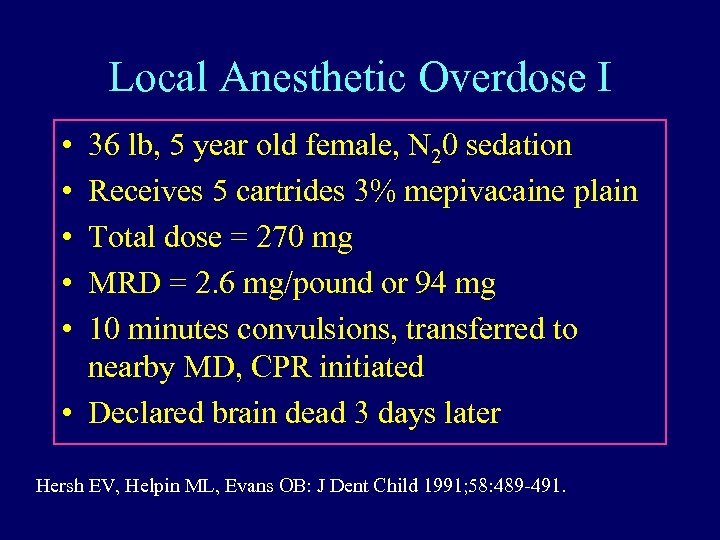
Local Anesthetic Overdose I • • • 36 lb, 5 year old female, N 20 sedation Receives 5 cartrides 3% mepivacaine plain Total dose = 270 mg MRD = 2. 6 mg/pound or 94 mg 10 minutes convulsions, transferred to nearby MD, CPR initiated • Declared brain dead 3 days later Hersh EV, Helpin ML, Evans OB: J Dent Child 1991; 58: 489 -491.
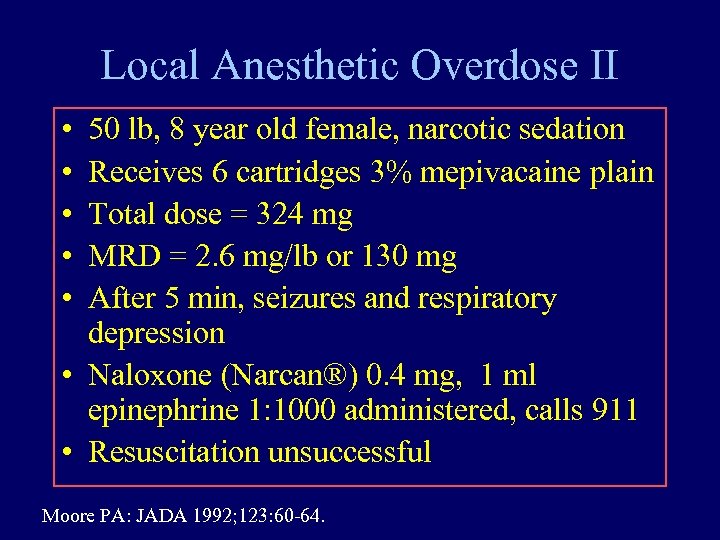
Local Anesthetic Overdose II • • • 50 lb, 8 year old female, narcotic sedation Receives 6 cartridges 3% mepivacaine plain Total dose = 324 mg MRD = 2. 6 mg/lb or 130 mg After 5 min, seizures and respiratory depression • Naloxone (Narcan®) 0. 4 mg, 1 ml epinephrine 1: 1000 administered, calls 911 • Resuscitation unsuccessful Moore PA: JADA 1992; 123: 60 -64.
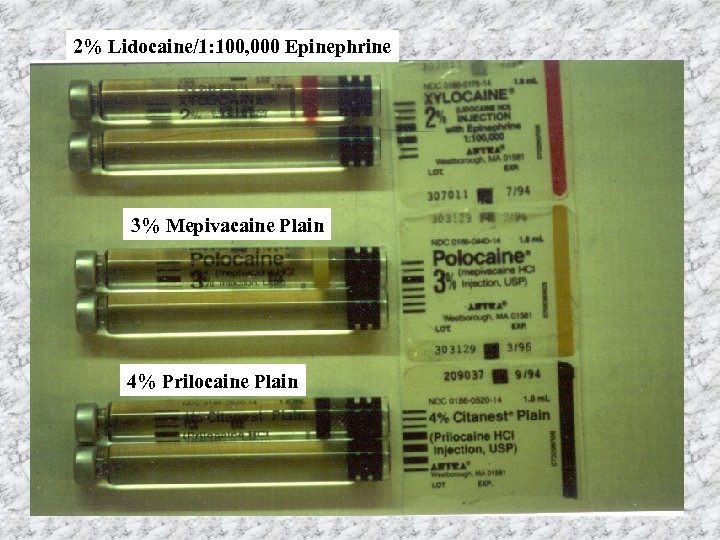
2% Lidocaine/1: 100, 000 Epinephrine 3% Mepivacaine Plain 4% Prilocaine Plain
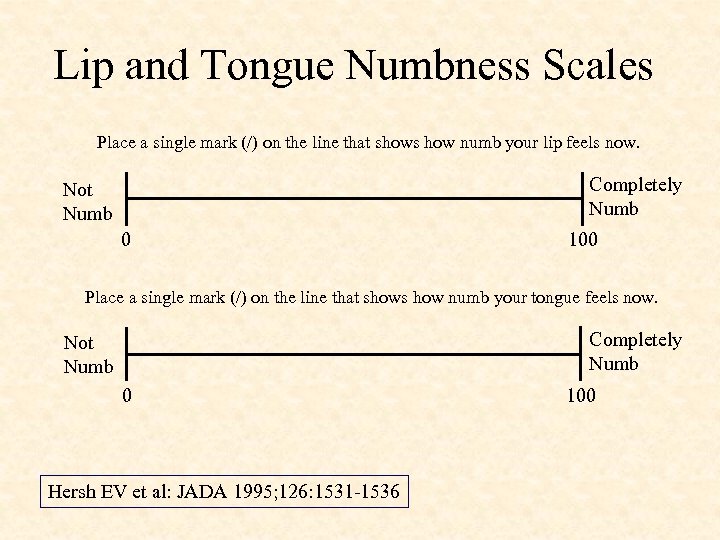
Lip and Tongue Numbness Scales Place a single mark (/) on the line that shows how numb your lip feels now. Completely Numb Not Numb 0 100 Place a single mark (/) on the line that shows how numb your tongue feels now. Completely Numb Not Numb 0 Hersh EV et al: JADA 1995; 126: 1531 -1536 100
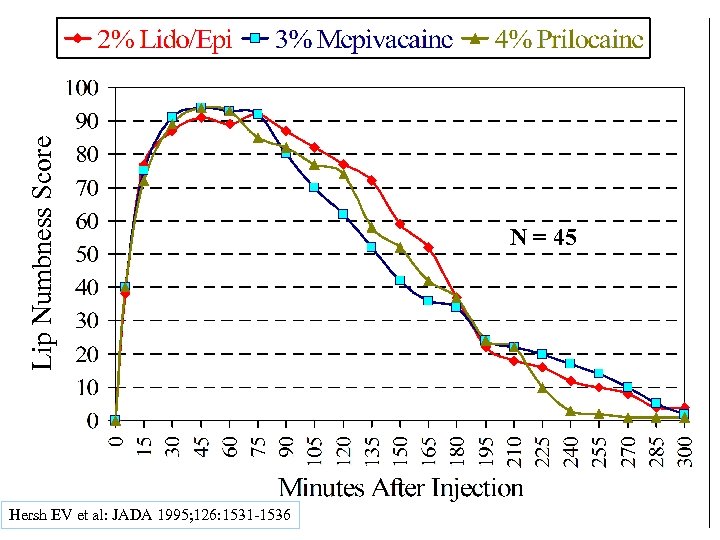
Lip Numbness Score Hersh EV et al: JADA 1995; 126: 1531 -1536 N = 45
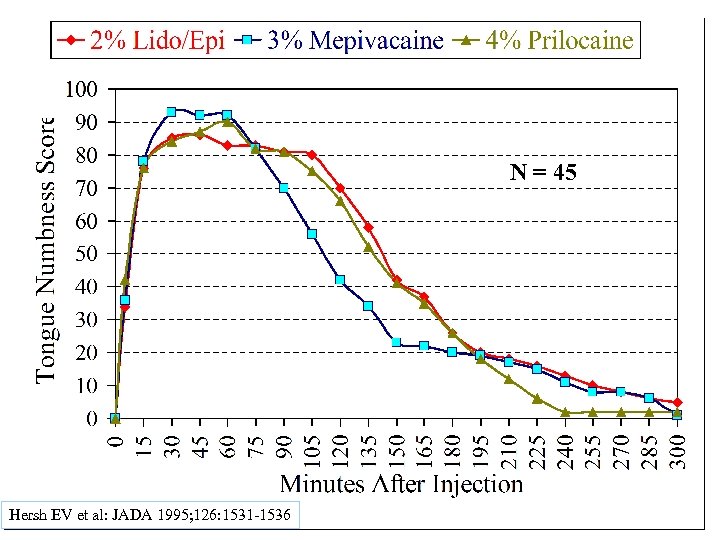
N = 45 Hersh EV et al: JADA 1995; 126: 1531 -1536
Conclusions • The time-course of soft tissue anesthesia – including onset, peak effects and overall duration was very similar between 2% lidocaine with epinephrine, 3% mepivacaine plain and 4% prilocaine plain. • Combining these observations with local anesthetic dosage recommendations, it is recommended that 2% lidocaine with epinephrine be employed when performing block injections in young children.
Quality of Life Issues Associated with Prolonged Lip and Tongue Numbness • In adults/teenagers - difficulty Smiling Speaking Drinking/Eating And everyone’s favorite: Drooling
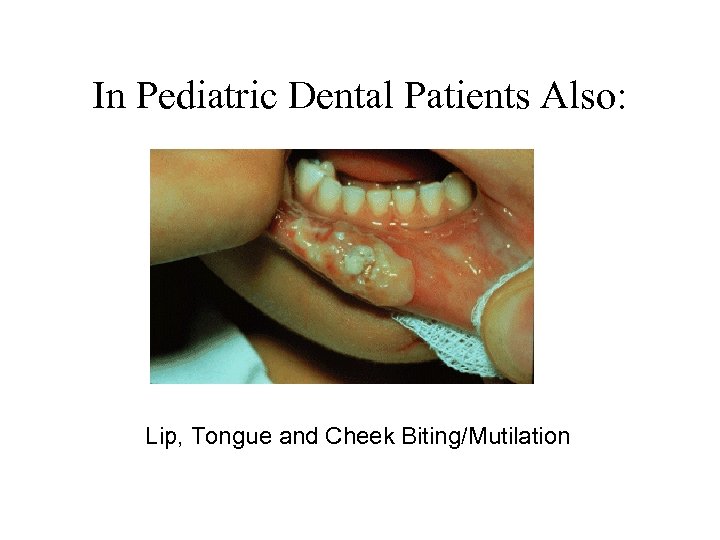
In Pediatric Dental Patients Also: Lip, Tongue and Cheek Biting/Mutilation
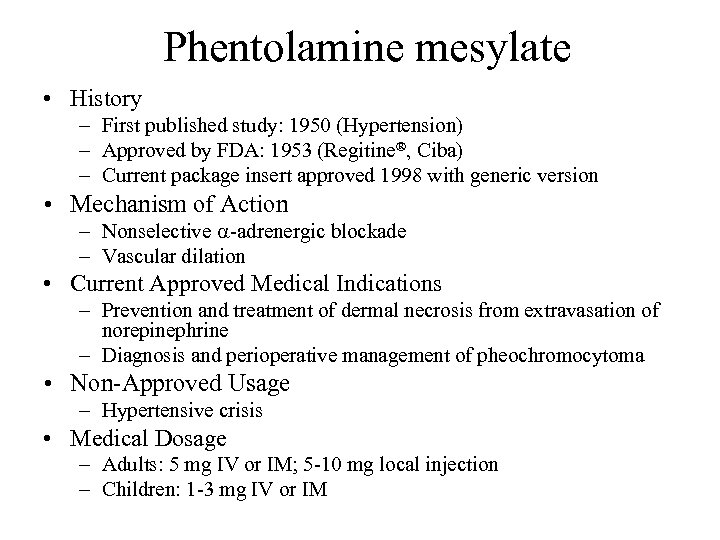
Phentolamine mesylate • History – First published study: 1950 (Hypertension) – Approved by FDA: 1953 (Regitine®, Ciba) – Current package insert approved 1998 with generic version • Mechanism of Action – Nonselective -adrenergic blockade – Vascular dilation • Current Approved Medical Indications – Prevention and treatment of dermal necrosis from extravasation of norepinephrine – Diagnosis and perioperative management of pheochromocytoma • Non-Approved Usage – Hypertensive crisis • Medical Dosage – Adults: 5 mg IV or IM; 5 -10 mg local injection – Children: 1 -3 mg IV or IM
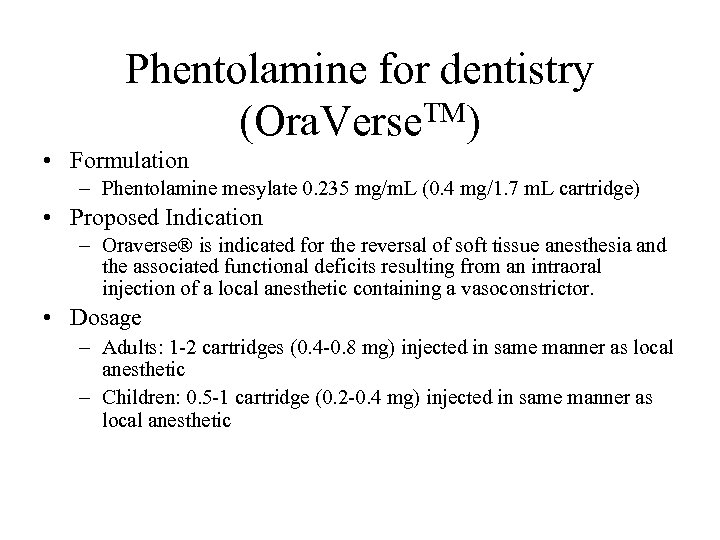
Phentolamine for dentistry (Ora. Verse. TM) • Formulation – Phentolamine mesylate 0. 235 mg/m. L (0. 4 mg/1. 7 m. L cartridge) • Proposed Indication – Oraverse® is indicated for the reversal of soft tissue anesthesia and the associated functional deficits resulting from an intraoral injection of a local anesthetic containing a vasoconstrictor. • Dosage – Adults: 1 -2 cartridges (0. 4 -0. 8 mg) injected in same manner as local anesthetic – Children: 0. 5 -1 cartridge (0. 2 -0. 4 mg) injected in same manner as local anesthetic
Purpose of Phase 3 Studies To evaluate the safety and efficacy of a new drug formulation containing the vasodilator, phentolamine mesylate, testing the hypotheses that, in adults, Ora. Verse : TM • is safe and well-tolerated • shortens duration of STA after routine local anesthetic (lidocaine with 1: 100, 000 epi, articaine with 1: 100, 000 epi, prilocaine with 1: 200, 000 epi, and mepivacaine with 1: 20, 000 levonordefrin) 89
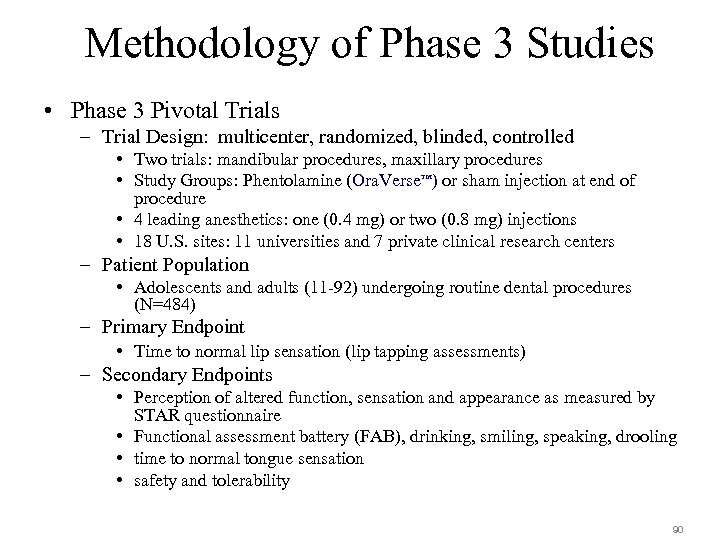
Methodology of Phase 3 Studies • Phase 3 Pivotal Trials – Trial Design: multicenter, randomized, blinded, controlled • Two trials: mandibular procedures, maxillary procedures • Study Groups: Phentolamine (Ora. Verse ) or sham injection at end of procedure • 4 leading anesthetics: one (0. 4 mg) or two (0. 8 mg) injections • 18 U. S. sites: 11 universities and 7 private clinical research centers TM – Patient Population • Adolescents and adults (11 -92) undergoing routine dental procedures (N=484) – Primary Endpoint • Time to normal lip sensation (lip tapping assessments) – Secondary Endpoints • Perception of altered function, sensation and appearance as measured by STAR questionnaire • Functional assessment battery (FAB), drinking, smiling, speaking, drooling • time to normal tongue sensation • safety and tolerability 90
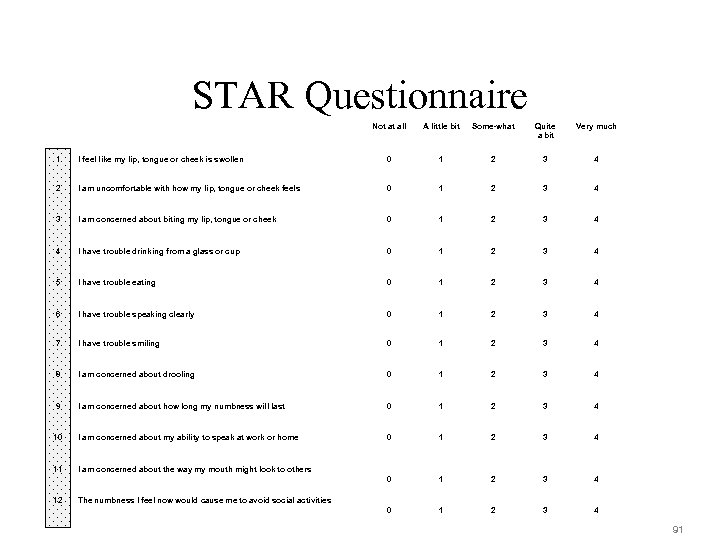
STAR Questionnaire Not at all A little bit Some-what Quite a bit Very much 1 I feel like my lip, tongue or cheek is swollen 0 1 2 3 4 2 I am uncomfortable with how my lip, tongue or cheek feels 0 1 2 3 4 3 I am concerned about biting my lip, tongue or cheek 0 1 2 3 4 4 I have trouble drinking from a glass or cup 0 1 2 3 4 5 I have trouble eating 0 1 2 3 4 6 I have trouble speaking clearly 0 1 2 3 4 7 I have trouble smiling 0 1 2 3 4 8 I am concerned about drooling 0 1 2 3 4 9 I am concerned about how long my numbness will last 0 1 2 3 4 10 I am concerned about my ability to speak at work or home 0 1 2 3 4 11 I am concerned about the way my mouth might look to others 0 1 2 3 4 12 The numbness I feel now would cause me to avoid social activities 91
Functional Evaluations of “Suzie sewed zippers on two new dresses at Bessie’s house. ” “She usually rushes to push the garage door closed. ” “Ruth caught a cold because she wouldn’t wear her new, warm, wool coat. ”
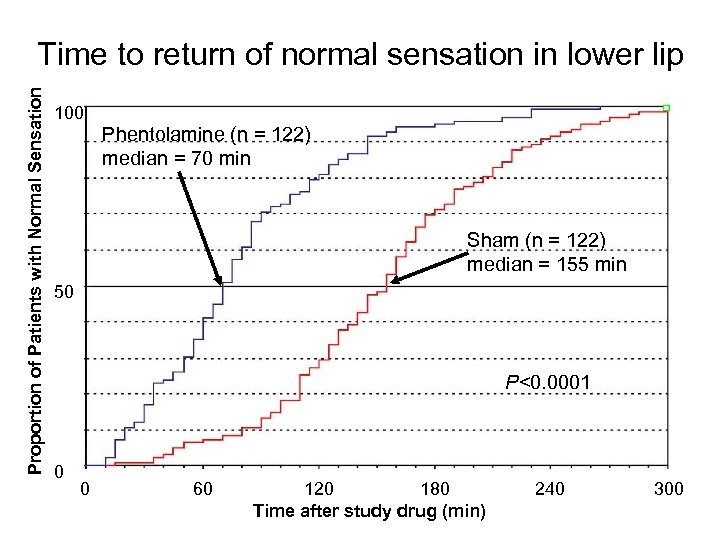
Proportion of Patients with Normal Sensation Time to return of normal sensation in lower lip 100 Phentolamine (n = 122) median = 70 min Sham (n = 122) median = 155 min 50 P<0. 0001 0 0 60 120 180 Time after study drug (min) 240 300
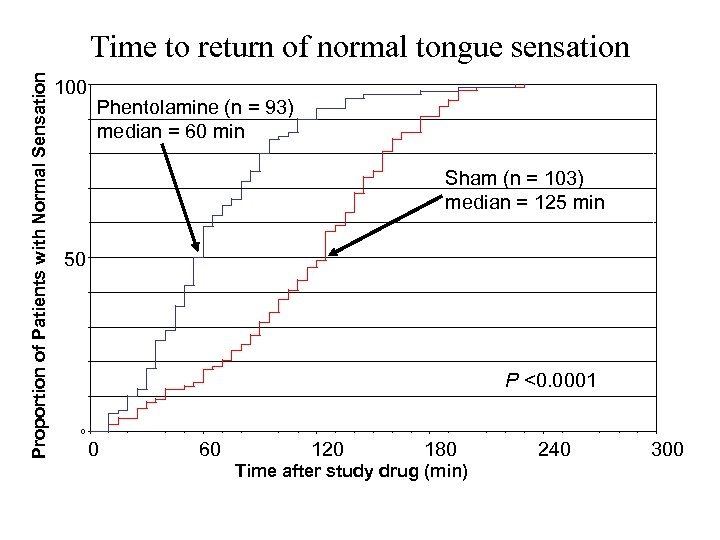
Proportion of Patients with Normal Sensation Time to return of normal tongue sensation 100 Phentolamine (n = 93) median = 60 min Sham (n = 103) median = 125 min 50 P <0. 0001 0 0 60 120 180 Time after study drug (min) 240 300
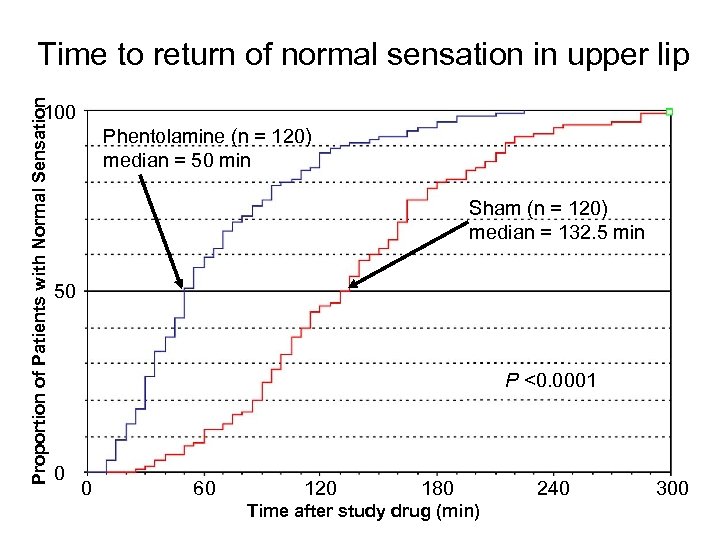
Proportion of Patients with Normal Sensation Time to return of normal sensation in upper lip 100 Phentolamine (n = 120) median = 50 min Sham (n = 120) median = 132. 5 min 50 P <0. 0001 0 0 60 120 180 Time after study drug (min) 240 300
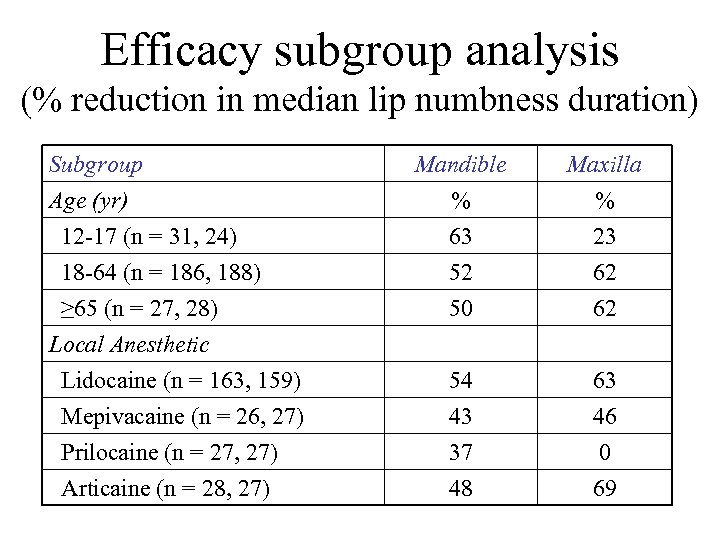
Efficacy subgroup analysis (% reduction in median lip numbness duration) Subgroup Age (yr) 12 -17 (n = 31, 24) 18 -64 (n = 186, 188) ≥ 65 (n = 27, 28) Local Anesthetic Lidocaine (n = 163, 159) Mepivacaine (n = 26, 27) Prilocaine (n = 27, 27) Articaine (n = 28, 27) Mandible % 63 52 Maxilla % 23 62 50 62 54 43 37 48 63 46 0 69
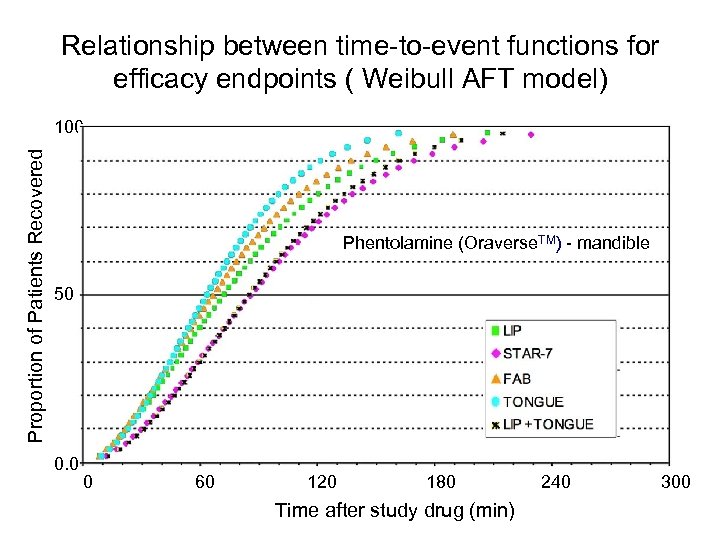
Relationship between time-to-event functions for efficacy endpoints ( Weibull AFT model) Proportion of Patients Recovered 100 NV-101 (n = 120) median = 50 min Phentolamine (Oraverse. TM) - mandible Sham (n = 120) median = 132. 5 min 50 P<0. 0001 0. 0 0 60 120 180 Time after study drug (min) 240 300
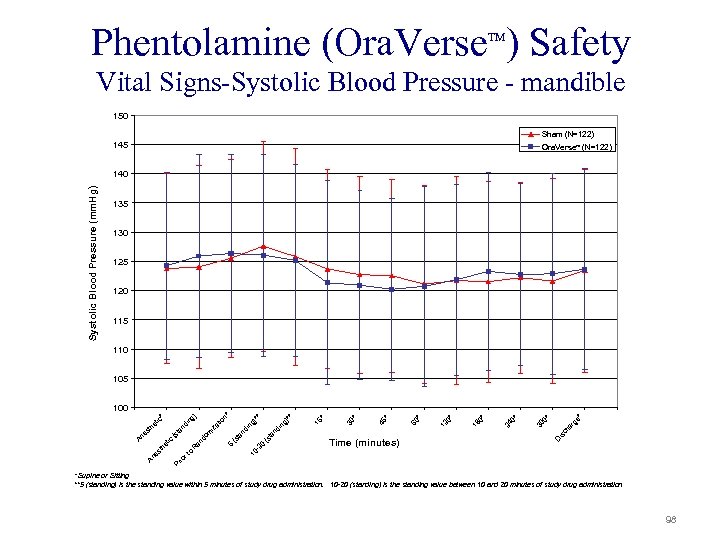
Phentolamine (Ora. Verse ) Safety TM Vital Signs-Systolic Blood Pressure - mandible 150 Sham (N=122) 145 Ora. Verse (N=122) TM Systolic Blood Pressure (mm. Hg) 140 135 130 125 120 115 110 105 * is ch ar ge 0* D 30 0* 24 0* 18 0* 12 * 60 * 45 * * 30 in ta nd 15 ** g) 0 -2 5 (s (s ta iz do m an R o Pr io rt nd in at nd i ta (s tic th e Time (minutes) 10 ) ng * tic th e An es io n* 100 * Supine or Sitting **5 (standing) is the standing value within 5 minutes of study drug administration. 10 -20 (standing) is the standing value between 10 and 20 minutes of study drug administration 98
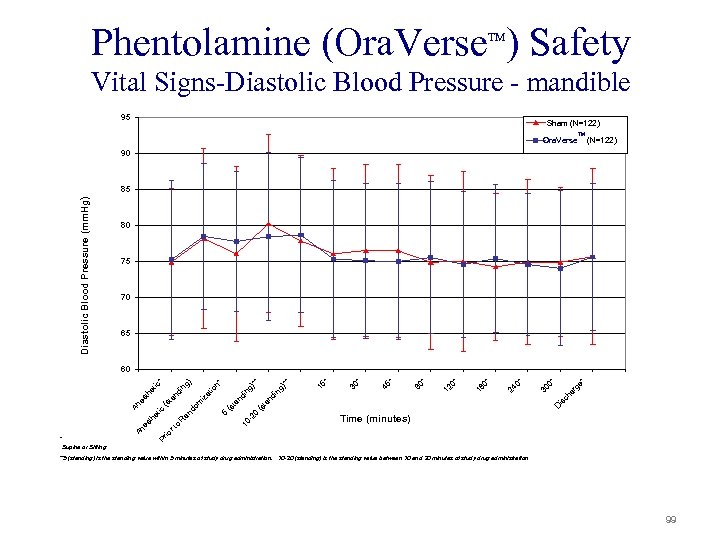
Phentolamine (Ora. Verse ) Safety TM Vital Signs-Diastolic Blood Pressure - mandible 95 Sham (N=122) Ora. Verse TM (N=122) 90 Diastolic Blood Pressure (mm. Hg) 85 80 75 70 65 ch ar ge * 0* is D (s -2 0 10 30 0* 24 0* 18 0* 12 * 60 * 45 * 30 * 15 g) ** * ta an di (s t 5 nd in ng )* n* io at m iz do o rt Pr * Time (minutes) io An es th et R an ic An (s t es th an di et ic ng ) * 60 Supine or Sitting **5 (standing) is the standing value within 5 minutes of study drug administration. 10 -20 (standing) is the standing value between 10 and 20 minutes of study drug administration 99
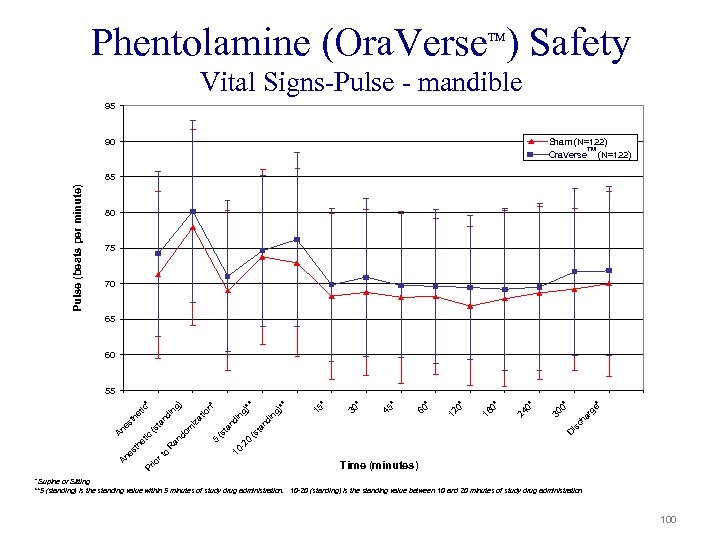
Phentolamine (Ora. Verse ) Safety TM Vital Signs-Pulse - mandible 95 90 Sham (N=122) TM Ora. Verse (N=122) Pulse (beats per minute) 85 80 75 70 65 60 e* ar g 0* is an ch 30 0* 24 0* 18 0* 12 60 * * 45 * * 30 g) di n 15 ** ** g) -2 0 D (s t ta 5 (s 10 R o io rt nd in io n* m iz at in an do (s tic Pr An es t he An es t ta nd he tic g) * 55 Time (minutes) * Supine or Sitting **5 (standing) is the standing value within 5 minutes of study drug administration. 10 -20 (standing) is the standing value between 10 and 20 minutes of study drug administration 100
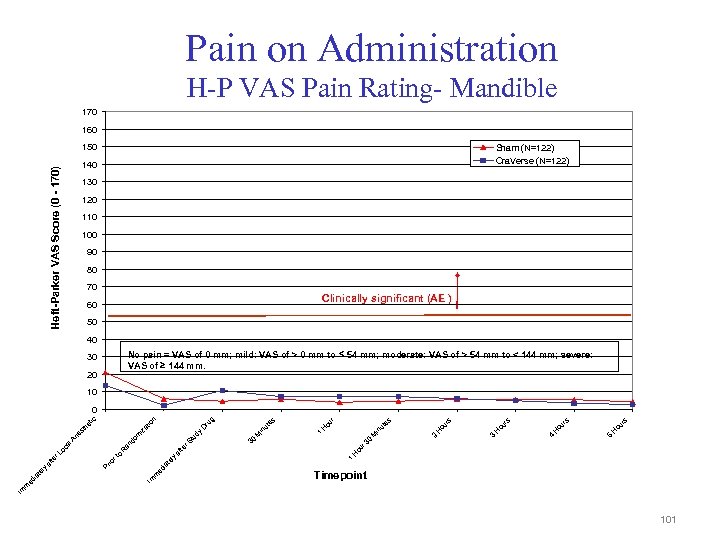
Pain on Administration H-P VAS Pain Rating- Mandible 170 160 150 Sham (N=122) Ora. Verse (N=122) Heft-Parker VAS Score (0 - 170) 140 130 120 110 100 90 80 70 Clinically significant (AE ) 60 50 40 No pain = VAS of 0 mm; mild: VAS of > 0 mm to 54 mm; moderate: VAS of > 54 mm to < 144 mm; severe: VAS of 144 mm. 30 20 10 ou rs H 5 ou rs H 4 ou rs H 3 ou rs H M in ou r 3 0 2 es ut ou r H in M 30 H 1 te af ly te ed ia Im m 1 ut e s ru g D dy r. S tu m an do R o rt io Pr Timepoint Im m ed ia te ly af te r. L oc al An e iz st at io n he tic 0 101
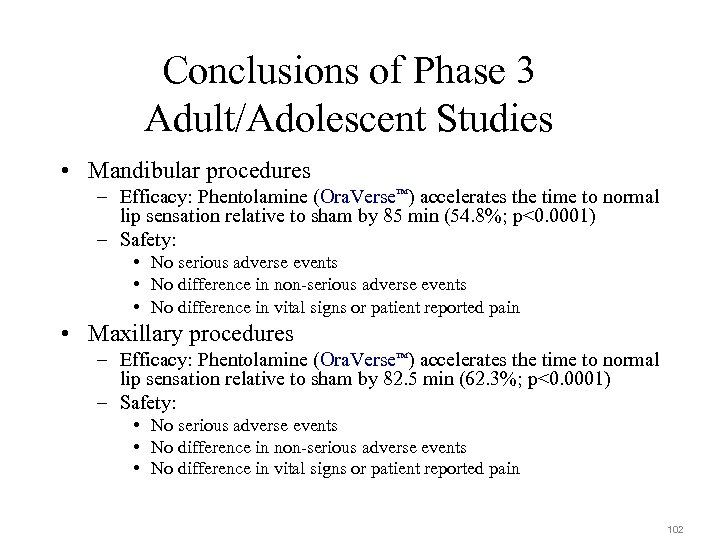
Conclusions of Phase 3 Adult/Adolescent Studies • Mandibular procedures – Efficacy: Phentolamine (Ora. Verse ) accelerates the time to normal lip sensation relative to sham by 85 min (54. 8%; p<0. 0001) – Safety: TM • No serious adverse events • No difference in non-serious adverse events • No difference in vital signs or patient reported pain • Maxillary procedures – Efficacy: Phentolamine (Ora. Verse ) accelerates the time to normal lip sensation relative to sham by 82. 5 min (62. 3%; p<0. 0001) – Safety: TM • No serious adverse events • No difference in non-serious adverse events • No difference in vital signs or patient reported pain 102
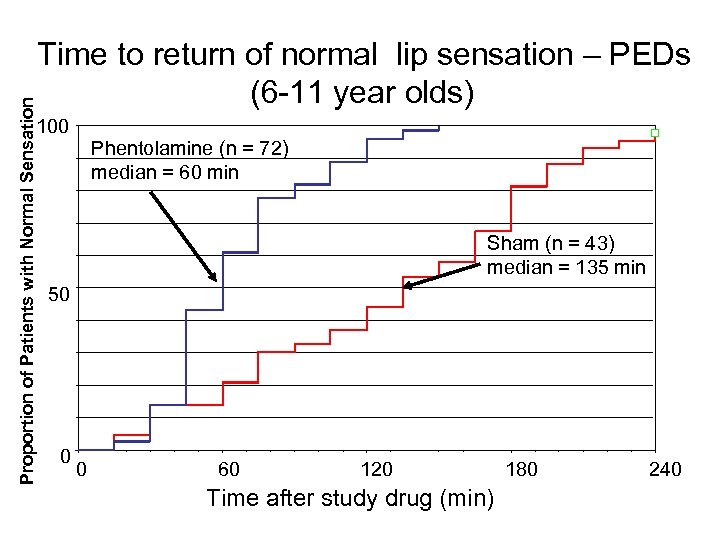
Proportion of Patients with Normal Sensation Time to return of normal lip sensation – PEDs (6 -11 year olds) 100 Phentolamine (n = 72) median = 60 min Sham (n = 43) median = 135 min 50 0 0 60 120 Time after study drug (min) 180 240
fdb1a7128844b4ea9d8b5edb09164bbf.ppt