c47d8f6fa778e0904a88179906c181a1.ppt
- Количество слайдов: 29
Morbidity & Mortality – Issues Surrounding Perioperative Anticoagulant “Bridging” By Mike Murchie St Vincent Hospital Internal Medicine Resident
Periprocedural Anticoagulant Bridging Case #1 • 80 yo female • PMH- Acute Upper Extremity DVT 5 months ago that led to diagnosis of Metastatic Ovarian CA [s/p resection currently undergoing chemo], HTN, Hyperlipidemia • Left breast mass suspicious for cancer on mammography, breast biopsy pending • On Coumadin chronically given active malignancy, unprovoked clot • Coumadin held 4 days prior to procedure, bridged with Lovenox 1. 5 mg / day before and after procedure until coumadin restarted and INR back up to 2 -3 range. • RESULTS: – No thrombotic or bleeding episodes occurred – Pt received total of 6 doses Lovenox administered by home health nursing – Estimated total cost = $990 – Estimated out of pocket expenses per patient’s daughter = $600
Periprocedural Anticoagulant Bridging Case #2 • 58 yo male presents to ER, POC troponin 0. 10, ER asks cardiology to see patient for possible ACS • Came to ER with CC of numbness, tingling left arm and mild dysarthria which started 12 hours ago while golfing, and at this point has almost resolved completely. • PMH- Paroxysmal, symptomatic Afib on coumadin since dx s/p CVA in ’ 04; CHF Ef 45%; HTN; Hyperlipidemia; PCM-ICD • Had been off coumadin before a screening colonoscopy last week and now back on, but INR is currently 1. 4. No bridging before or after procedure was given.
Periprocedural Anticoagulant Bridging Case #3 • 62 yo Male PMH- AVR ’ 04, HTN, DM 2, Afib admitted with acute cholecystitis which responds to antibiotics, fluids. • Stays in hospital for somewhat elective cholecystectomy • Coumadin d/c, Bridged with LMWH preop • Surgery involves conversion to open ccx given technically difficult procedure by laparoscope • At 12 hours post-op, hemoglobin “stable” and full dose LMWH restarted • Next day, patient transferred to ICU with hypotension, intrabdominal hemorrhage
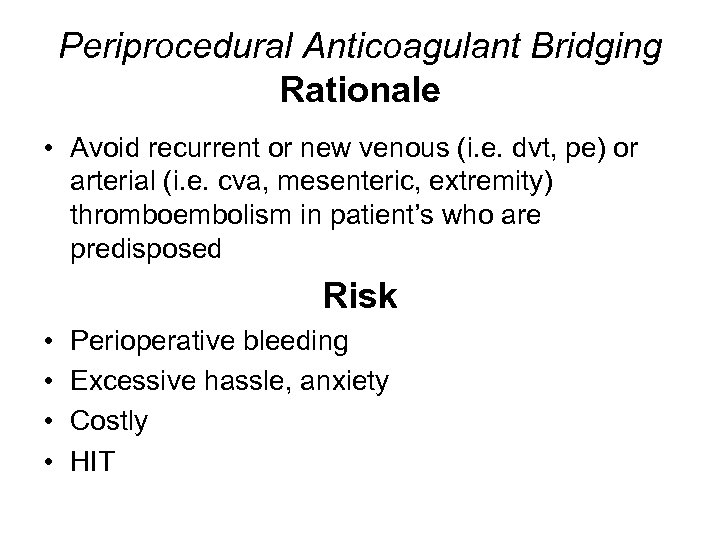
Periprocedural Anticoagulant Bridging Rationale • Avoid recurrent or new venous (i. e. dvt, pe) or arterial (i. e. cva, mesenteric, extremity) thromboembolism in patient’s who are predisposed Risk • • Perioperative bleeding Excessive hassle, anxiety Costly HIT
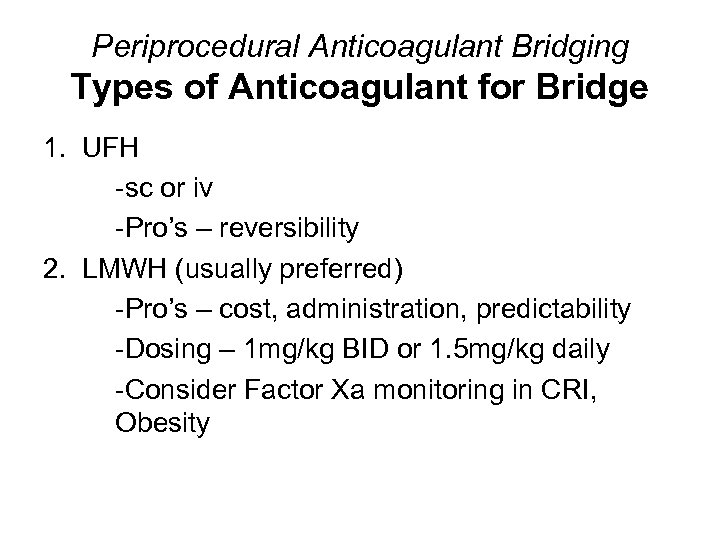
Periprocedural Anticoagulant Bridging Types of Anticoagulant for Bridge 1. UFH -sc or iv -Pro’s – reversibility 2. LMWH (usually preferred) -Pro’s – cost, administration, predictability -Dosing – 1 mg/kg BID or 1. 5 mg/kg daily -Consider Factor Xa monitoring in CRI, Obesity
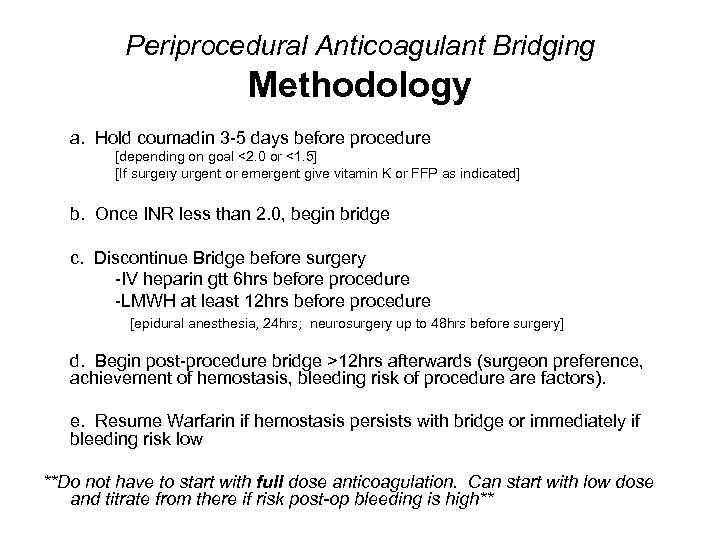
Periprocedural Anticoagulant Bridging Methodology a. Hold coumadin 3 -5 days before procedure [depending on goal <2. 0 or <1. 5] [If surgery urgent or emergent give vitamin K or FFP as indicated] b. Once INR less than 2. 0, begin bridge c. Discontinue Bridge before surgery -IV heparin gtt 6 hrs before procedure -LMWH at least 12 hrs before procedure [epidural anesthesia, 24 hrs; neurosurgery up to 48 hrs before surgery] d. Begin post-procedure bridge >12 hrs afterwards (surgeon preference, achievement of hemostasis, bleeding risk of procedure are factors). e. Resume Warfarin if hemostasis persists with bridge or immediately if bleeding risk low **Do not have to start with full dose anticoagulation. Can start with low dose and titrate from there if risk post-op bleeding is high**
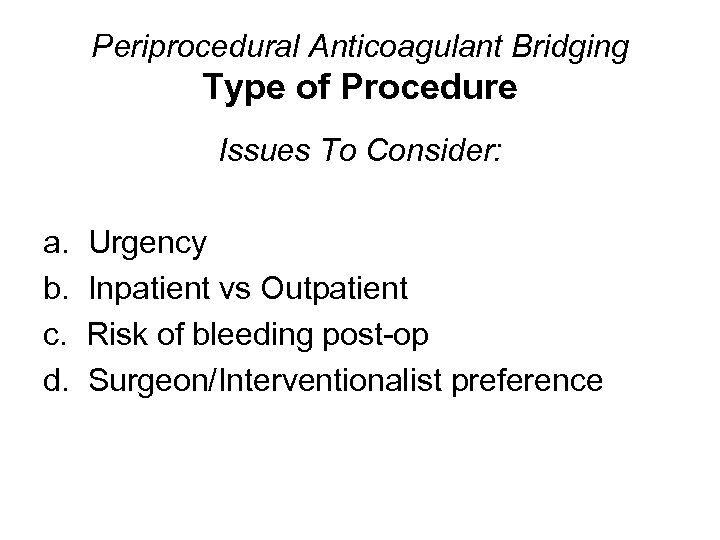
Periprocedural Anticoagulant Bridging Type of Procedure Issues To Consider: a. b. c. d. Urgency Inpatient vs Outpatient Risk of bleeding post-op Surgeon/Interventionalist preference
Periprocedural Anticoagulant Bridging Type of Procedures NOT requiring any changes: • • • Dermatologic biopsies (including Moh’s) Most dental procedures (including Tooth extractions) Pacemaker insertion Arthrocentesis Cataract surgery ***Still, important STAT INR done before procedure to guarantee INR not supratherapeutic*** ***Many will still have anticoagulation held 2 days before procedure***
Periprocedural Anticoagulant Bridging Type of Procedure • PCI – Preferable to d/c coumadin before cath, but can be done with INR 2 -3 if urgent – In urgent setting where cath to be completed in less than 24 hours preferable to bridge with IV heparin gtt
Periprocedural Anticoagulant Bridging Risk of bleeding with bridging • Depends on timing and intensity of bridge • One study showed an 11% incidence of major bleeding in patients on full dose anticoagulation with a heparin gtt over 5 days of therapy post-op • 3% of major bleeding episodes are deadly • 50% of major bleeding episodes require an additional surgery
Periprocedural Anticoagulant Bridging Patient Characteristics • What is the indication for their anticoagulation? • How long have they been anticoagulated? • How well has their INR been controlled? • Inpatient vs outpatient? • Ambulatory vs bed bound?
Periprocedural Anticoagulant Bridging Prior Venous Thromboembolism What is the risk of clotting? • 100 x increased risk VTE in the post-op period for patients with h/o VTE off anticoagulation
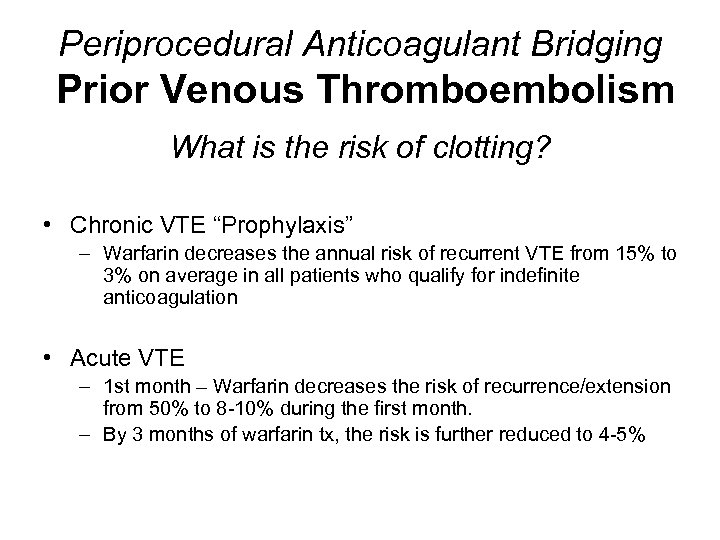
Periprocedural Anticoagulant Bridging Prior Venous Thromboembolism What is the risk of clotting? • Chronic VTE “Prophylaxis” – Warfarin decreases the annual risk of recurrent VTE from 15% to 3% on average in all patients who qualify for indefinite anticoagulation • Acute VTE – 1 st month – Warfarin decreases the risk of recurrence/extension from 50% to 8 -10% during the first month. – By 3 months of warfarin tx, the risk is further reduced to 4 -5%
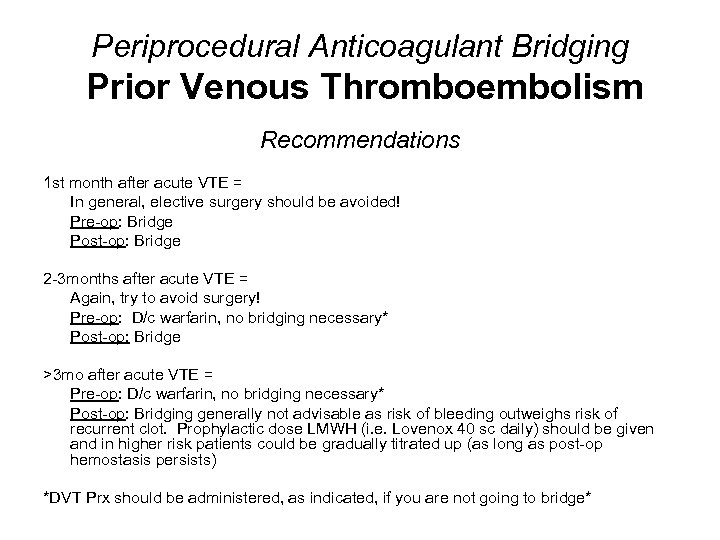
Periprocedural Anticoagulant Bridging Prior Venous Thromboembolism Recommendations 1 st month after acute VTE = In general, elective surgery should be avoided! Pre-op: Bridge Post-op: Bridge 2 -3 months after acute VTE = Again, try to avoid surgery! Pre-op: D/c warfarin, no bridging necessary* Post-op: Bridge >3 mo after acute VTE = Pre-op: D/c warfarin, no bridging necessary* Post-op: Bridging generally not advisable as risk of bleeding outweighs risk of recurrent clot. Prophylactic dose LMWH (i. e. Lovenox 40 sc daily) should be given and in higher risk patients could be gradually titrated up (as long as post-op hemostasis persists) *DVT Prx should be administered, as indicated, if you are not going to bridge*
Periprocedural Anticoagulant Bridging Prior Arterial Thromboembolism What is the key difference between VTE and ATE perioperative clotting risk? • There is no proven increased risk of ATE inherent to the post-op period
Periprocedural Anticoagulant Bridging Prior Arterial Thromboembolism What are the main causes / risk factors for ATE? • Atrial fibrillation • Prosthetic heart valves patients on chronic anticoagulation
Periprocedural Anticoagulant Bridging Atrial Fibrillation • Length of time from ATE event important – 85% of thrombi in patients w/nonvalvular afib show resolution on TEE after 4 weeks of warfarin therapy • Morbidity of ATE associated with Afib is high – Afib related cva is fatal or associated with severe neurologic deficit in 60% of cases
Periprocedural Anticoagulant Bridging Atrial Fibrillation What is the risk of clotting? • • • CVA risk in healthy 70 yo pt is 1% per year On average, CVA risk in a fib patients 4 -5% per year Warfarin estimated to cut this risk by 62 -69%. • For the patient in your office, these numbers aren’t very accurate depending on his/her comorbidities – For example, 65 -75 yo pt with afib and no other risk factors => 4. 3% w/nada, 1. 4% w/ASA only, 1. 1% w/warfarin • The CHADS 2 risk stratification model helps come up with a patient specific yearly risk CVA for patients treated with warfarin, aspirin, or nothing • [CHADS 2 yearly risk / 365 ] * [ # of days with subtherapeutic INR] can be used to calculate patient specific risk of withholding bridging
Periprocedural Anticoagulant Bridging Atrial Fibrillation Recommendations 1 st month after ATE – avoid surgery Preop – Bridge Postop - Bridge if risk of postop bleeding is low >1 mo, nonvalvular afib with no high risk features – Preop – D/c warfarin, no bridging necessary Postop – Resume coumadin once hemostasis achieved >1 mo, with High risk features (prior ATE, rheumatic heart dz, left ventricular dysfunction, afib associated w/valvular heart dz) – controversial, but most recommend: Preop: Bridge Postop: Bridge, but carefully* *Intensity of post-op bridging depends on risk of bleeding. Given there is not an intrinsic increased risk of ATE in the post-op period, erring on the side of caution in regards to bleeding is advised **DVT Prx should be administered, when indicated, if you are not going to bridge
Periprocedural Anticoagulant Bridging Prosthetic Heart Valves • 60% receive mechanical – ALL are anticoagulated • 40% receive bioprosthesis – Some are anticoagulated
Periprocedural Anticoagulant Bridging Prosthetic Heart Valves What is the risk of clotting? • Mitral Valve – 2 x higher rate Arterial Thrombo. Embolus than Aortic valve • Risk of clotting also depends on type of mechanical valve placed • ATE yearly risk due to Prosthetic Heart Valves – [stats between studies vary dramatically] With Warfarin, 1. 0% per year (0. 8% for AV, 1. 4% for MV) With ASA, 2. 2% per year With nothing, 4% **Other case series list risk 12% per year AV, 23% per year MV with no anticoagulation!
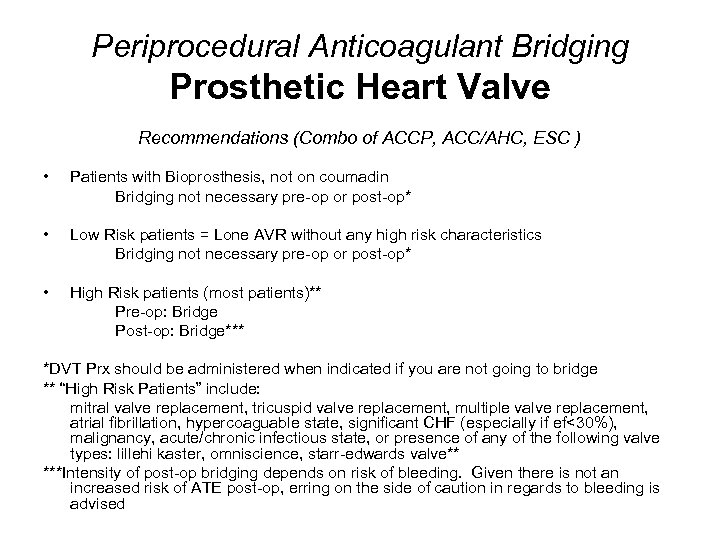
Periprocedural Anticoagulant Bridging Prosthetic Heart Valve Recommendations (Combo of ACCP, ACC/AHC, ESC ) • Patients with Bioprosthesis, not on coumadin Bridging not necessary pre-op or post-op* • Low Risk patients = Lone AVR without any high risk characteristics Bridging not necessary pre-op or post-op* • High Risk patients (most patients)** Pre-op: Bridge Post-op: Bridge*** *DVT Prx should be administered when indicated if you are not going to bridge ** “High Risk Patients” include: mitral valve replacement, tricuspid valve replacement, multiple valve replacement, atrial fibrillation, hypercoaguable state, significant CHF (especially if ef<30%), malignancy, acute/chronic infectious state, or presence of any of the following valve types: lillehi kaster, omniscience, starr-edwards valve** ***Intensity of post-op bridging depends on risk of bleeding. Given there is not an increased risk of ATE post-op, erring on the side of caution in regards to bleeding is advised
Key Points • Main difference between recommendations for ATE vs VTE stems from the fact that VTE patients have 100 x increased risk recurrence post-op, whereas ATE patient’s risk is the same as pre-op • Post-op bleeding complications with bridging are more common (though often less devastating) than is post-op thromboembolism without bridging • In order to minimize bleeding complications, bridging resumption post-op does not need to start at therapeutic anticoagulant doses
References • • • Cannegieter, et al. Thromboembolic & Bleeding Complications in Patients with Mechanical Heart Valve Prosthesis. Circulation. Vol 89, No 2, 2/1994, pgs 635 -41 Piazza, et al. Periprocedural Management of the Chronically Anticoagulated Patient. Critical Pathways in Cardiology. Vol 2, Number 2, 6/2003, pgs 96 -103 Salem, et al. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy: Evidence Based Guidelines. Chest. Volume 126(3), 9/2004. Kearon, et al. Management of Anticoagulation Before and After Elective Surgery. NEJM. Vol 336, Number 21, pgs 1506 -1511 Lip, Gregory. Management of Anticoagulation Before and After Elective Surgery. Up to Date online. Last updated 4/6/2007. Manning, et al. Anticoagulation to Prevent Embolization in Atrial Fibrillation. Up to Date online. Last updated 2/21/2007. Aurigemma, et al. Antithrombotic Therapy in Patients with Prosthetic Heart Valves. Up to Date online. Last updated 4/6/2007 Goldhaber, et al. “Bridging” and Mechanical Heart Valves. Circulation. Volume 113, 1/31/2006, pages 470 -472 Ansell, et al. Managing Oral Anticoagulant Therapy. Chest. Volume 119(1), 1/2001, Supplement, 22 S-38 S

Questions?
Periprocedural Anticoagulant Bridging Patient Characteristics: Prior Venous Thromboembolism What is the risk of bleeding post-op? • Depends on the surgery, patient, and the dose of anticoagulant bridge given • One study showed an 11% incidence of major bleeding in patients on full anticoagulation with a heparin gtt over 5 days of therapy post-op
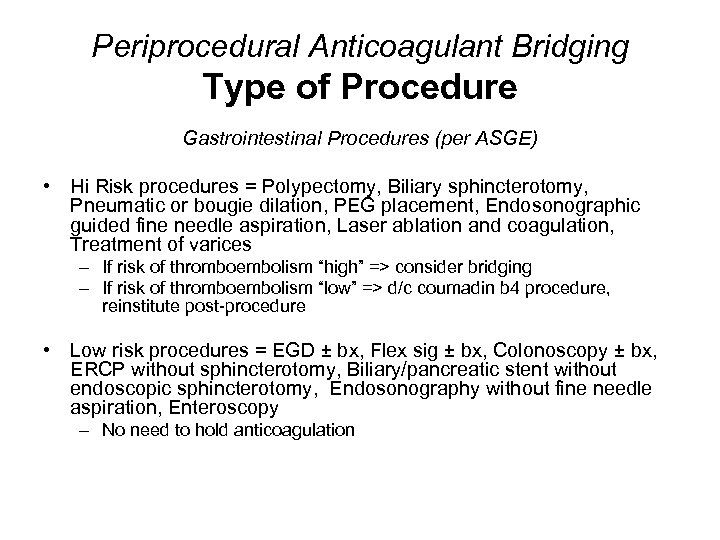
Periprocedural Anticoagulant Bridging Type of Procedure Gastrointestinal Procedures (per ASGE) • Hi Risk procedures = Polypectomy, Biliary sphincterotomy, Pneumatic or bougie dilation, PEG placement, Endosonographic guided fine needle aspiration, Laser ablation and coagulation, Treatment of varices – If risk of thromboembolism “high” => consider bridging – If risk of thromboembolism “low” => d/c coumadin b 4 procedure, reinstitute post-procedure • Low risk procedures = EGD ± bx, Flex sig ± bx, Colonoscopy ± bx, ERCP without sphincterotomy, Biliary/pancreatic stent without endoscopic sphincterotomy, Endosonography without fine needle aspiration, Enteroscopy – No need to hold anticoagulation
Periprocedural Anticoagulant Bridging Patient Characteristics: Hypercoaguable State Requiring Long Term Anticoagulation • I. e. Antiphospholipid antibody syndrome or combined heterozygosity for Factor V Leiden and PT gene mutation w/ h/o VTE • Bridge preop and postop • Best to consult with patient’s Hematologist
c47d8f6fa778e0904a88179906c181a1.ppt