a010cbd50933a4225939daf8d4506c15.ppt
- Количество слайдов: 54
 Module 8 Management of Periodontal Disease in HIV-Infected Patients
Module 8 Management of Periodontal Disease in HIV-Infected Patients
 Management of Periodontal Disease in HIV-Infected Patients Mark A. Reynolds, D. D. S. , Ph. D. Niki M. Moutsopoulos, D. D. S. Department of Periodontics Dental School University of Maryland Baltimore and the Pennsylvania/Mid-Atlantic AIDS ETC
Management of Periodontal Disease in HIV-Infected Patients Mark A. Reynolds, D. D. S. , Ph. D. Niki M. Moutsopoulos, D. D. S. Department of Periodontics Dental School University of Maryland Baltimore and the Pennsylvania/Mid-Atlantic AIDS ETC
 Program Outline • Classification of Periodontal Diseases and Conditions • Periodontal Diseases and Conditions in HIV-Infected Patients • Periodontal Management of HIVInfected Patients
Program Outline • Classification of Periodontal Diseases and Conditions • Periodontal Diseases and Conditions in HIV-Infected Patients • Periodontal Management of HIVInfected Patients
 Program Objectives The objectives of this program are to: (1) Outline the current classification of periodontal diseases and conditions based on the 1999 international workshop for a classification of periodontal diseases and conditions; (2) Review selected periodontal diseases and conditions in HIV-infected patients (3) Provide an overview of considerations and approaches in the periodontal management of HIV-infected patients
Program Objectives The objectives of this program are to: (1) Outline the current classification of periodontal diseases and conditions based on the 1999 international workshop for a classification of periodontal diseases and conditions; (2) Review selected periodontal diseases and conditions in HIV-infected patients (3) Provide an overview of considerations and approaches in the periodontal management of HIV-infected patients
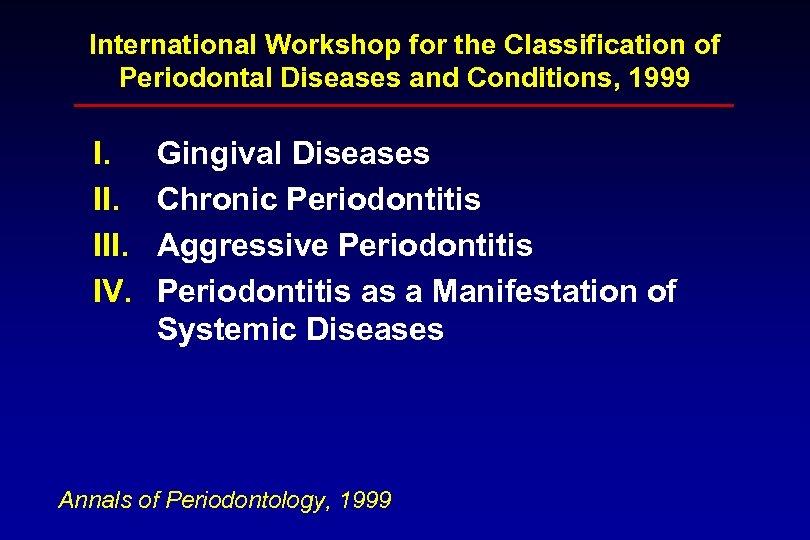 International Workshop for the Classification of Periodontal Diseases and Conditions, 1999 I. III. IV. Gingival Diseases Chronic Periodontitis Aggressive Periodontitis as a Manifestation of Systemic Diseases Annals of Periodontology, 1999
International Workshop for the Classification of Periodontal Diseases and Conditions, 1999 I. III. IV. Gingival Diseases Chronic Periodontitis Aggressive Periodontitis as a Manifestation of Systemic Diseases Annals of Periodontology, 1999
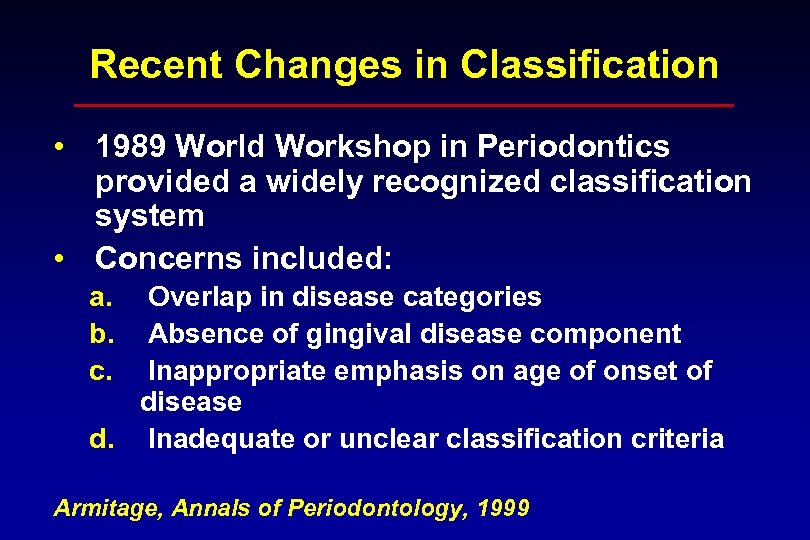 Recent Changes in Classification • 1989 World Workshop in Periodontics provided a widely recognized classification system • Concerns included: a. b. c. Overlap in disease categories Absence of gingival disease component Inappropriate emphasis on age of onset of disease d. Inadequate or unclear classification criteria Armitage, Annals of Periodontology, 1999
Recent Changes in Classification • 1989 World Workshop in Periodontics provided a widely recognized classification system • Concerns included: a. b. c. Overlap in disease categories Absence of gingival disease component Inappropriate emphasis on age of onset of disease d. Inadequate or unclear classification criteria Armitage, Annals of Periodontology, 1999
 International Workshop for the Classification of Periodontal Diseases and Conditions, 1999 V. Necrotizing Periodontal Diseases VI. Abscesses of the Periodontium VII. Periodontitis Associated with Endodontic Lesions VIII. Developmental or Acquired Deformities and Conditions Annals of Periodontology, 1999
International Workshop for the Classification of Periodontal Diseases and Conditions, 1999 V. Necrotizing Periodontal Diseases VI. Abscesses of the Periodontium VII. Periodontitis Associated with Endodontic Lesions VIII. Developmental or Acquired Deformities and Conditions Annals of Periodontology, 1999
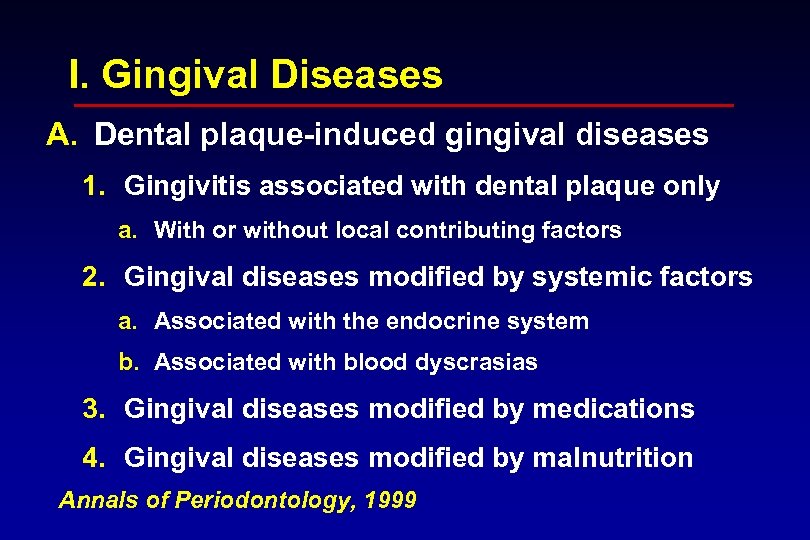 I. Gingival Diseases A. Dental plaque-induced gingival diseases 1. Gingivitis associated with dental plaque only a. With or without local contributing factors 2. Gingival diseases modified by systemic factors a. Associated with the endocrine system b. Associated with blood dyscrasias 3. Gingival diseases modified by medications 4. Gingival diseases modified by malnutrition Annals of Periodontology, 1999
I. Gingival Diseases A. Dental plaque-induced gingival diseases 1. Gingivitis associated with dental plaque only a. With or without local contributing factors 2. Gingival diseases modified by systemic factors a. Associated with the endocrine system b. Associated with blood dyscrasias 3. Gingival diseases modified by medications 4. Gingival diseases modified by malnutrition Annals of Periodontology, 1999
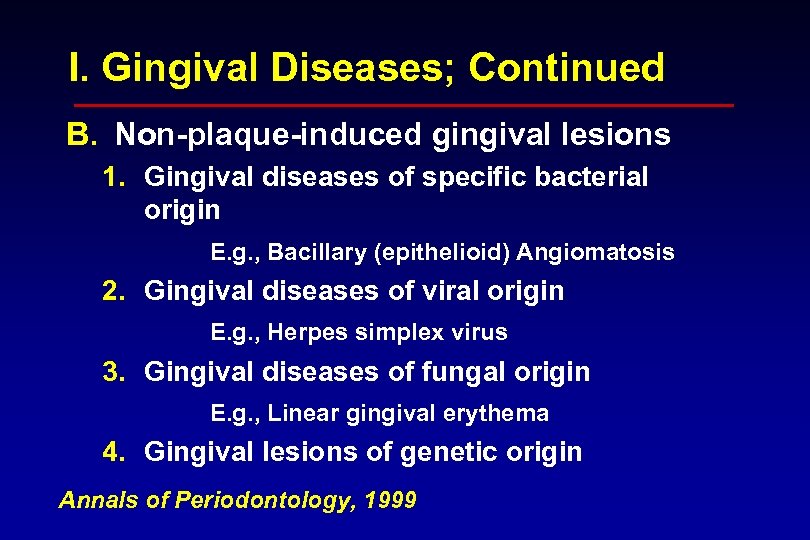 I. Gingival Diseases; Continued B. Non-plaque-induced gingival lesions 1. Gingival diseases of specific bacterial origin E. g. , Bacillary (epithelioid) Angiomatosis 2. Gingival diseases of viral origin E. g. , Herpes simplex virus 3. Gingival diseases of fungal origin E. g. , Linear gingival erythema 4. Gingival lesions of genetic origin Annals of Periodontology, 1999
I. Gingival Diseases; Continued B. Non-plaque-induced gingival lesions 1. Gingival diseases of specific bacterial origin E. g. , Bacillary (epithelioid) Angiomatosis 2. Gingival diseases of viral origin E. g. , Herpes simplex virus 3. Gingival diseases of fungal origin E. g. , Linear gingival erythema 4. Gingival lesions of genetic origin Annals of Periodontology, 1999
 I. Gingival Diseases B. Non-plaque-induced gingival lesions. Continued 5. Gingival manifestations of systemic conditions 1. Mucocutaneous disorders 2. Allergic reactions 6. Traumatic lesions (factitious, iatrogenic, accidental) Annals of Periodontology, 1999 7. Foreign body reactions
I. Gingival Diseases B. Non-plaque-induced gingival lesions. Continued 5. Gingival manifestations of systemic conditions 1. Mucocutaneous disorders 2. Allergic reactions 6. Traumatic lesions (factitious, iatrogenic, accidental) Annals of Periodontology, 1999 7. Foreign body reactions
 II. Chronic Periodontitis A. Localized B. Generalized III. Aggressive Periodontitis A. Localized B. Generalized Annals of Periodontology, 1999
II. Chronic Periodontitis A. Localized B. Generalized III. Aggressive Periodontitis A. Localized B. Generalized Annals of Periodontology, 1999
 IV. Periodontitis as a Manifestation of Systemic Diseases A. Associated with hematological disorders B. Associated with genetic disorders C. Not otherwise specified (NOS) Annals of Periodontology, 1999
IV. Periodontitis as a Manifestation of Systemic Diseases A. Associated with hematological disorders B. Associated with genetic disorders C. Not otherwise specified (NOS) Annals of Periodontology, 1999
 V. Necrotizing Periodontal Diseases A. Necrotizing ulcerative gingivitis (NUG) B. Necrotizing ulcerative periodontitis (NUP) Annals of Periodontology, 1999
V. Necrotizing Periodontal Diseases A. Necrotizing ulcerative gingivitis (NUG) B. Necrotizing ulcerative periodontitis (NUP) Annals of Periodontology, 1999
 VI. Abscesses of the Periodontium VII. Periodontitis Associated with Endodontic Lesions VIII. Developmental or Acquired Deformities and Conditions Annals of Periodontology, 1999
VI. Abscesses of the Periodontium VII. Periodontitis Associated with Endodontic Lesions VIII. Developmental or Acquired Deformities and Conditions Annals of Periodontology, 1999
 Periodontal Diseases and Conditions in HIV-Infected Patients • Unclear whethere are periodontal lesions specific to HIV infection • Exacerbation of periodontal conditions and disease, such as chronic periodontitis, may result from severe immunodeficiency or immunosuppression • Mixed infections Ø Opportunistic Ø Poly-microbial
Periodontal Diseases and Conditions in HIV-Infected Patients • Unclear whethere are periodontal lesions specific to HIV infection • Exacerbation of periodontal conditions and disease, such as chronic periodontitis, may result from severe immunodeficiency or immunosuppression • Mixed infections Ø Opportunistic Ø Poly-microbial
 Selected Gingival Diseases and Conditions in HIV-Infected Patients A. Dental plaque-induced gingival diseases i. e. , common gingivitis (not “HIV-gingivitis”) B. Non-plaque-induced gingival lesions 1. Gingival diseases of specific bacterial origin
Selected Gingival Diseases and Conditions in HIV-Infected Patients A. Dental plaque-induced gingival diseases i. e. , common gingivitis (not “HIV-gingivitis”) B. Non-plaque-induced gingival lesions 1. Gingival diseases of specific bacterial origin
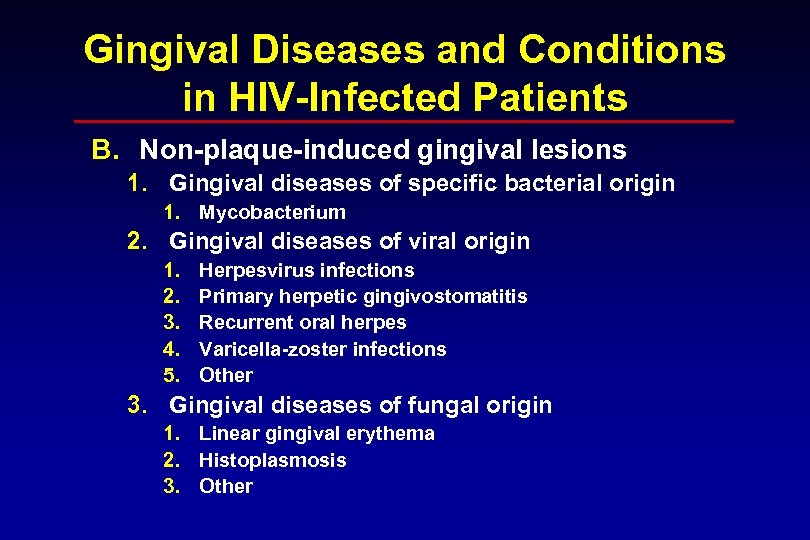 Gingival Diseases and Conditions in HIV-Infected Patients B. Non-plaque-induced gingival lesions 1. Gingival diseases of specific bacterial origin 1. Mycobacterium 2. Gingival diseases of viral origin 1. 2. 3. 4. 5. Herpesvirus infections Primary herpetic gingivostomatitis Recurrent oral herpes Varicella-zoster infections Other 3. Gingival diseases of fungal origin 1. Linear gingival erythema 2. Histoplasmosis 3. Other
Gingival Diseases and Conditions in HIV-Infected Patients B. Non-plaque-induced gingival lesions 1. Gingival diseases of specific bacterial origin 1. Mycobacterium 2. Gingival diseases of viral origin 1. 2. 3. 4. 5. Herpesvirus infections Primary herpetic gingivostomatitis Recurrent oral herpes Varicella-zoster infections Other 3. Gingival diseases of fungal origin 1. Linear gingival erythema 2. Histoplasmosis 3. Other
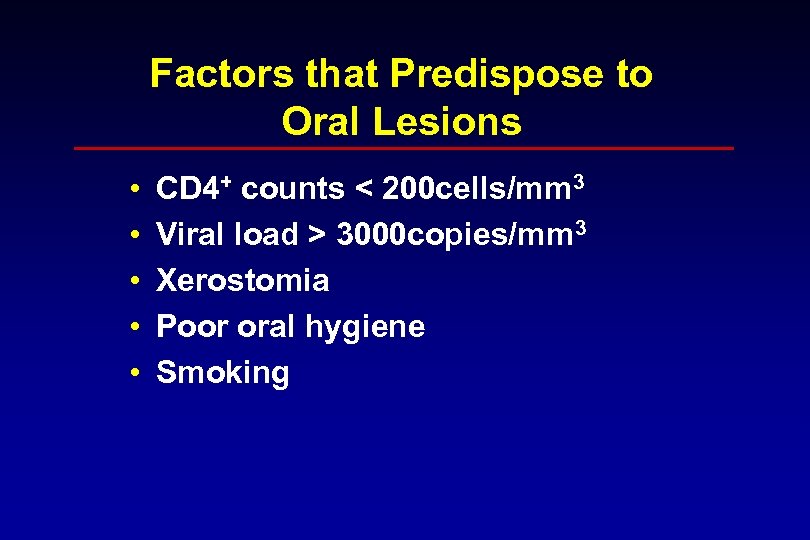 Factors that Predispose to Oral Lesions • • • CD 4+ counts < 200 cells/mm 3 Viral load > 3000 copies/mm 3 Xerostomia Poor oral hygiene Smoking
Factors that Predispose to Oral Lesions • • • CD 4+ counts < 200 cells/mm 3 Viral load > 3000 copies/mm 3 Xerostomia Poor oral hygiene Smoking
 HIV PROGRESSION CD 4 < 200 = AIDS • Immune deterioration • Opportunistic Infections • Oral Manifestations Adapted from Fauci et al. , 1983
HIV PROGRESSION CD 4 < 200 = AIDS • Immune deterioration • Opportunistic Infections • Oral Manifestations Adapted from Fauci et al. , 1983
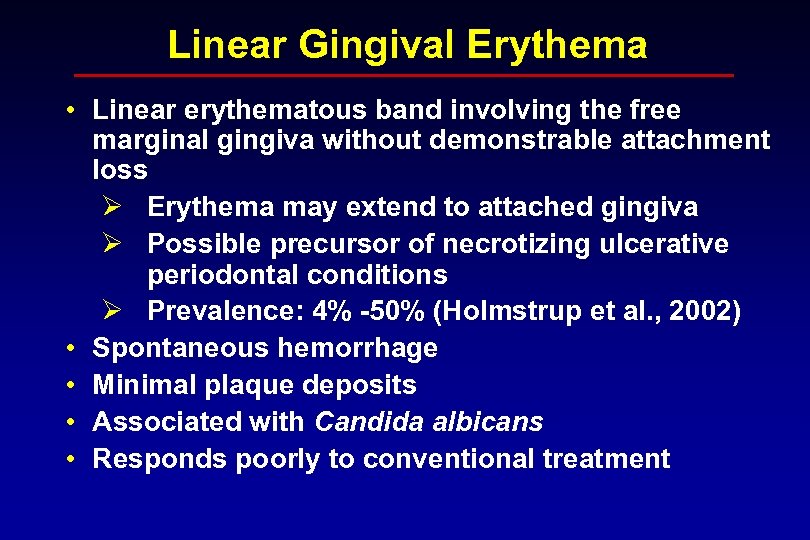 Linear Gingival Erythema • Linear erythematous band involving the free marginal gingiva without demonstrable attachment loss Ø Erythema may extend to attached gingiva Ø Possible precursor of necrotizing ulcerative periodontal conditions Ø Prevalence: 4% -50% (Holmstrup et al. , 2002) • Spontaneous hemorrhage • Minimal plaque deposits • Associated with Candida albicans • Responds poorly to conventional treatment
Linear Gingival Erythema • Linear erythematous band involving the free marginal gingiva without demonstrable attachment loss Ø Erythema may extend to attached gingiva Ø Possible precursor of necrotizing ulcerative periodontal conditions Ø Prevalence: 4% -50% (Holmstrup et al. , 2002) • Spontaneous hemorrhage • Minimal plaque deposits • Associated with Candida albicans • Responds poorly to conventional treatment
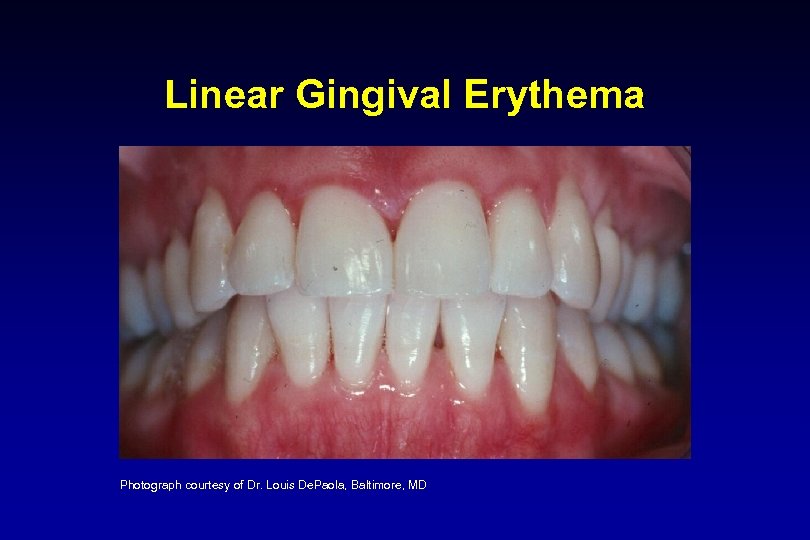 Linear Gingival Erythema Photograph courtesy of Dr. Louis De. Paola, Baltimore, MD
Linear Gingival Erythema Photograph courtesy of Dr. Louis De. Paola, Baltimore, MD
 Periodontal Diseases and Conditions in HIV-Infected Patients • Aggressive periodontitis Ø Severe localized forms reported in literature • Chronic periodontitis modified by immunosuppression Ø Recent interest in potential for accelerated rate of chronic periodontitis occurring in HIV+ patients Ø Rate of progression may be dependent upon the immunologic competency of the host as well as local inflammatory response to typical and atypical subgingival microorganisms (Lamster et al. , 1997)
Periodontal Diseases and Conditions in HIV-Infected Patients • Aggressive periodontitis Ø Severe localized forms reported in literature • Chronic periodontitis modified by immunosuppression Ø Recent interest in potential for accelerated rate of chronic periodontitis occurring in HIV+ patients Ø Rate of progression may be dependent upon the immunologic competency of the host as well as local inflammatory response to typical and atypical subgingival microorganisms (Lamster et al. , 1997)
 Chronic Periodontitis • It is not clear whether HIV+ patients develop a more progressive form of conventional periodontitis • One study demonstrated a three fold increase in the odds ratios of bone loss for males (Tomar et al. , 1995) • Chronic periodontitis modified by immunosuppression Ø Recent interest in potential for accelerated rate of chronic periodontitis occurring in HIV+ patients Ø Rate of progression may be dependent upon the immunologic competency of the host as well as local inflammatory response to typical and atypical subgingival microorganisms (Lamster et al. , 1997)
Chronic Periodontitis • It is not clear whether HIV+ patients develop a more progressive form of conventional periodontitis • One study demonstrated a three fold increase in the odds ratios of bone loss for males (Tomar et al. , 1995) • Chronic periodontitis modified by immunosuppression Ø Recent interest in potential for accelerated rate of chronic periodontitis occurring in HIV+ patients Ø Rate of progression may be dependent upon the immunologic competency of the host as well as local inflammatory response to typical and atypical subgingival microorganisms (Lamster et al. , 1997)
 Periodontal Diseases and Conditions in HIV-Infected Patients • Necrotizing Periodontal Diseases Ø Necrotizing ulcerative gingivitis (NUG) Ø Necrotizing ulcerative periodontitis (NUP)
Periodontal Diseases and Conditions in HIV-Infected Patients • Necrotizing Periodontal Diseases Ø Necrotizing ulcerative gingivitis (NUG) Ø Necrotizing ulcerative periodontitis (NUP)
 Necrotizing Ulcerative Gingivitis • Primarily affects the papillary and marginal gingiva • Gingival erythema and edema, with spontaneous bleeding • Yellowish-grayish (“pseudomembranous”) areas of marginal and/or papillary necrosis of gingiva Ø Loss of interdental papillae Ø Pain Ø Rapid progression and extension possible
Necrotizing Ulcerative Gingivitis • Primarily affects the papillary and marginal gingiva • Gingival erythema and edema, with spontaneous bleeding • Yellowish-grayish (“pseudomembranous”) areas of marginal and/or papillary necrosis of gingiva Ø Loss of interdental papillae Ø Pain Ø Rapid progression and extension possible
 Necrotizing Ulcerative Gingivitis Photograph courtesy of Dr. Valli I. Meeks, Baltimore, MD
Necrotizing Ulcerative Gingivitis Photograph courtesy of Dr. Valli I. Meeks, Baltimore, MD
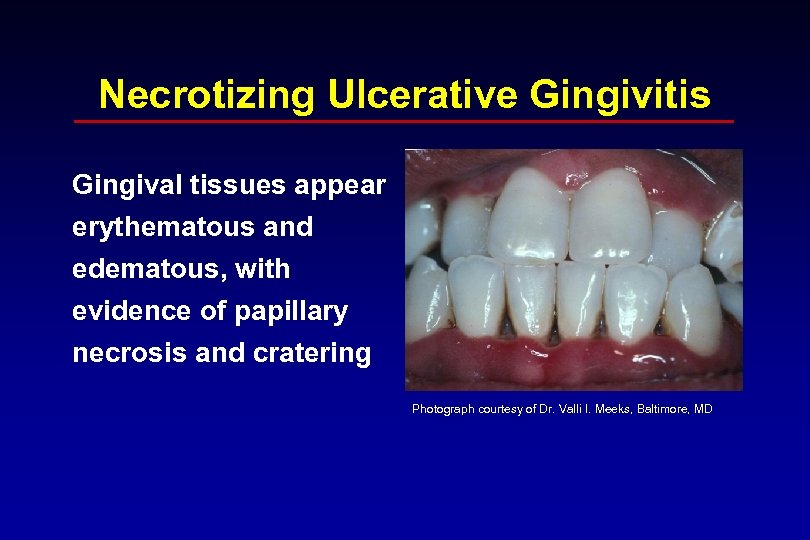 Necrotizing Ulcerative Gingivitis Gingival tissues appear erythematous and edematous, with evidence of papillary necrosis and cratering Photograph courtesy of Dr. Valli I. Meeks, Baltimore, MD
Necrotizing Ulcerative Gingivitis Gingival tissues appear erythematous and edematous, with evidence of papillary necrosis and cratering Photograph courtesy of Dr. Valli I. Meeks, Baltimore, MD
 Necrotizing Ulcerative Periodontitis • Interproximal ulceration, necrosis and cratering • Foetor is often present • Pain (severe, deep, localized in jaw) • Spontaneous bleeding • Soft tissue necrosis and rapid periodontal destruction • Prevalence: Ø 1%-88% (Holmstrup et al. , 2002). Ø One large study found a rate of 6. 3% (Glick et al. , 1994)
Necrotizing Ulcerative Periodontitis • Interproximal ulceration, necrosis and cratering • Foetor is often present • Pain (severe, deep, localized in jaw) • Spontaneous bleeding • Soft tissue necrosis and rapid periodontal destruction • Prevalence: Ø 1%-88% (Holmstrup et al. , 2002). Ø One large study found a rate of 6. 3% (Glick et al. , 1994)
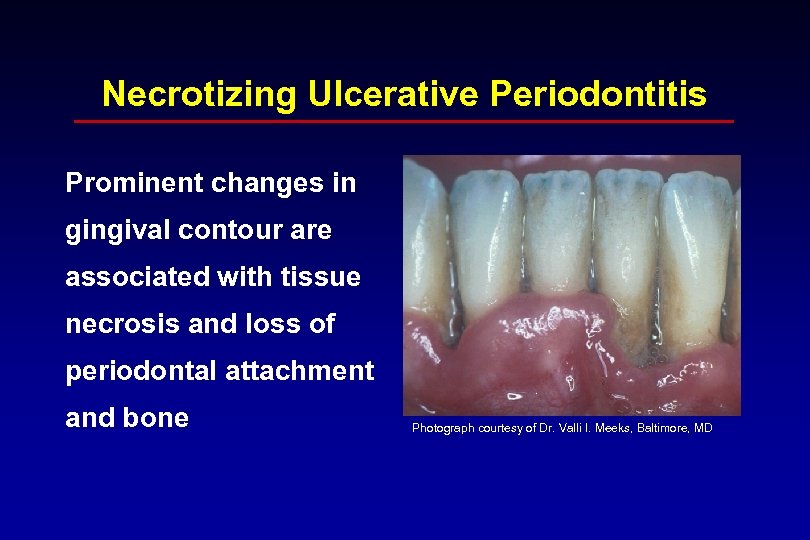 Necrotizing Ulcerative Periodontitis Prominent changes in gingival contour are associated with tissue necrosis and loss of periodontal attachment and bone Photograph courtesy of Dr. Valli I. Meeks, Baltimore, MD
Necrotizing Ulcerative Periodontitis Prominent changes in gingival contour are associated with tissue necrosis and loss of periodontal attachment and bone Photograph courtesy of Dr. Valli I. Meeks, Baltimore, MD
 General Considerations in the Management of HIV+ Patients • Universal precautions • Medical consultation a. Overall medical status b. Current medications c. Opportunistic infection(s) d. Stage of HIV disease a. CD 4 lymphocyte count b. Viral load • Management of oral infections • Comprehensive preventive and restorative oral health care
General Considerations in the Management of HIV+ Patients • Universal precautions • Medical consultation a. Overall medical status b. Current medications c. Opportunistic infection(s) d. Stage of HIV disease a. CD 4 lymphocyte count b. Viral load • Management of oral infections • Comprehensive preventive and restorative oral health care
 General Considerations in the Management of HIV+ Patients • In the absence of significant immunosuppression, the periodontal treatment of HIV+ patients should be guided by the same parameters of care appropriate for HIV- individuals.
General Considerations in the Management of HIV+ Patients • In the absence of significant immunosuppression, the periodontal treatment of HIV+ patients should be guided by the same parameters of care appropriate for HIV- individuals.
 Management of Linear Gingival Erythema • Scaling and debridement • Topical and/or subgingival irrigation with antimicrobial chemotherapeutic agent Ø Povidine iodine 10%, chlorhexidine gluconate irrigation 0. 12%-0. 2%, or Listerine Antiseptic • Prescribe daily microbial mouth rinse Ø Chlorhexidine gluconate mouth 0. 12% (Rx)1 Ø Listerine Antiseptic (OTC)2 • Recommendation for tobacco cessation • Re-evaluate in 2 -3 weeks. 1. 2. Available only by Rx; Many State drug plans do not cover this agent Pfizer, Morris Plains, NJ 07950; OTC, inexpensive and efficacious
Management of Linear Gingival Erythema • Scaling and debridement • Topical and/or subgingival irrigation with antimicrobial chemotherapeutic agent Ø Povidine iodine 10%, chlorhexidine gluconate irrigation 0. 12%-0. 2%, or Listerine Antiseptic • Prescribe daily microbial mouth rinse Ø Chlorhexidine gluconate mouth 0. 12% (Rx)1 Ø Listerine Antiseptic (OTC)2 • Recommendation for tobacco cessation • Re-evaluate in 2 -3 weeks. 1. 2. Available only by Rx; Many State drug plans do not cover this agent Pfizer, Morris Plains, NJ 07950; OTC, inexpensive and efficacious
 Management of Linear Gingival Erythema. Continued • For nonresponsive lesions, evaluate for Candidal infection, and consider antifungal agent Ø Refer to module 6 • Selected narrow-spectrum antibiotics sparing gram-positive organisms may be beneficial Ø Metronidazole (250 mg, tid 7 -10 days) Ø In the absence of resolution, consideration should be given to other possible lesions, such as lymphomas, including referral for appropriate diagnostic testing (i. e. , biopsy) • Meticulous oral hygiene and frequent supportive maintenance
Management of Linear Gingival Erythema. Continued • For nonresponsive lesions, evaluate for Candidal infection, and consider antifungal agent Ø Refer to module 6 • Selected narrow-spectrum antibiotics sparing gram-positive organisms may be beneficial Ø Metronidazole (250 mg, tid 7 -10 days) Ø In the absence of resolution, consideration should be given to other possible lesions, such as lymphomas, including referral for appropriate diagnostic testing (i. e. , biopsy) • Meticulous oral hygiene and frequent supportive maintenance
 Periodontal Diseases and Conditions in HIV-infected Patients • Necrotizing Periodontal Diseases Ø Necrotizing ulcerative gingivitis Ø Necrotizing ulcerative periodontitis Ø Necrotizing stomatitis
Periodontal Diseases and Conditions in HIV-infected Patients • Necrotizing Periodontal Diseases Ø Necrotizing ulcerative gingivitis Ø Necrotizing ulcerative periodontitis Ø Necrotizing stomatitis
 Management of Necrotizing Ulcerative Gingivitis • Local debridement, scaling and root planing, and irrigation of affected areas with either povidine iodine 10% or chlorhexidine gluconate 0. 12 -0. 2%. Ø Povidine iodine provides some analgesic properties. • Daily rinses with antimicrobial Ø Chlorhexidine gluconate mouth 0. 12% 1 Ø Listerine Antiseptic 2 • Frequent (daily or every-other-day) follow up for 7 -10 days, repeating scaling and debridement as necessary • Reevaluation 1 mo following resolution of acute symptoms 1. Available only by Rx; Many State drug plans do not cover this agent 2. Pfizer, Morris Plains, NJ 07950; OTC, inexpensive and efficacious
Management of Necrotizing Ulcerative Gingivitis • Local debridement, scaling and root planing, and irrigation of affected areas with either povidine iodine 10% or chlorhexidine gluconate 0. 12 -0. 2%. Ø Povidine iodine provides some analgesic properties. • Daily rinses with antimicrobial Ø Chlorhexidine gluconate mouth 0. 12% 1 Ø Listerine Antiseptic 2 • Frequent (daily or every-other-day) follow up for 7 -10 days, repeating scaling and debridement as necessary • Reevaluation 1 mo following resolution of acute symptoms 1. Available only by Rx; Many State drug plans do not cover this agent 2. Pfizer, Morris Plains, NJ 07950; OTC, inexpensive and efficacious
 Management of Necrotizing Ulcerative Gingivitis • Systemic antibiotics Ø Metronidazole (250 mg tid, 7 -10 days) Ø When necessary, should administered concurrently with topical (e. g, clotrimazole troches or nystatin vaginal tablets and, in severe immunosuppression, systemic antifungal medication (e. g, fluconazole) • Reevaluation 1 mo following resolution of acute symptoms
Management of Necrotizing Ulcerative Gingivitis • Systemic antibiotics Ø Metronidazole (250 mg tid, 7 -10 days) Ø When necessary, should administered concurrently with topical (e. g, clotrimazole troches or nystatin vaginal tablets and, in severe immunosuppression, systemic antifungal medication (e. g, fluconazole) • Reevaluation 1 mo following resolution of acute symptoms
 Management of Necrotizing Ulcerative Periodontitis • Local debridement, scaling and root planing, and irrigation of affected areas with either povidine iodine 10% or chlorhexidine gluconate 0. 12 -0. 2%. Ø Povidine iodine provides some analgesic properties. • Daily rinses with antimicrobial Ø Chlorhexidine gluconate mouth 0. 12% Ø Listerine Antiseptic • Frequent (daily or every-other-day) follow up for 7 -10 days, repeating scaling and debridement as necessary
Management of Necrotizing Ulcerative Periodontitis • Local debridement, scaling and root planing, and irrigation of affected areas with either povidine iodine 10% or chlorhexidine gluconate 0. 12 -0. 2%. Ø Povidine iodine provides some analgesic properties. • Daily rinses with antimicrobial Ø Chlorhexidine gluconate mouth 0. 12% Ø Listerine Antiseptic • Frequent (daily or every-other-day) follow up for 7 -10 days, repeating scaling and debridement as necessary
 Management of Necrotizing Ulcerative Periodontitis • Systemic antibiotics Ø Metronidazole (250 mg tid, 7 -10 days; Robinson et al. , 1998) Ø Consideration should also be given to the prophylactic administration of topical (e. g, clotrimazole troches or nystatin vaginal tablets) and, in severe immunosuppression, systemic antifungal medication (e. g, fluconazole 100 mg, 1 td, 7 to 10 days) • Reevaluation 1 mo following resolution of acute symptoms • 3 mo supportive periodontal maintenance Ø 30% of patients experience recurrence in 2 years (Patton et al. , 2000) Ø History of NUP predisposes to Necrotizing Ulcerative Stomatitis (Robinson, 2002)
Management of Necrotizing Ulcerative Periodontitis • Systemic antibiotics Ø Metronidazole (250 mg tid, 7 -10 days; Robinson et al. , 1998) Ø Consideration should also be given to the prophylactic administration of topical (e. g, clotrimazole troches or nystatin vaginal tablets) and, in severe immunosuppression, systemic antifungal medication (e. g, fluconazole 100 mg, 1 td, 7 to 10 days) • Reevaluation 1 mo following resolution of acute symptoms • 3 mo supportive periodontal maintenance Ø 30% of patients experience recurrence in 2 years (Patton et al. , 2000) Ø History of NUP predisposes to Necrotizing Ulcerative Stomatitis (Robinson, 2002)
 Management of Necrotizing Ulcerative Stomatitis • Debridement of affected areas • Daily rinses with antimicrobial Ø Chlorhexidine gluconate mouth rinse 0. 12% Ø Listerine Antiseptic • Daily (or every-other-day) follow up for the first week, repeating debridement at each visit • Systemic antibiotics (e. g. , metronidazole 250 tid, 7 -10 days). Ø Consideration should also be given to the prophylactic administration of an antifungal medication (fluconazole 100 mg, 1 td or Itraconazole 200 mg, 1 td; for 7 to 10 days) • Reevaluation 1 mo following resolution of acute symptoms
Management of Necrotizing Ulcerative Stomatitis • Debridement of affected areas • Daily rinses with antimicrobial Ø Chlorhexidine gluconate mouth rinse 0. 12% Ø Listerine Antiseptic • Daily (or every-other-day) follow up for the first week, repeating debridement at each visit • Systemic antibiotics (e. g. , metronidazole 250 tid, 7 -10 days). Ø Consideration should also be given to the prophylactic administration of an antifungal medication (fluconazole 100 mg, 1 td or Itraconazole 200 mg, 1 td; for 7 to 10 days) • Reevaluation 1 mo following resolution of acute symptoms
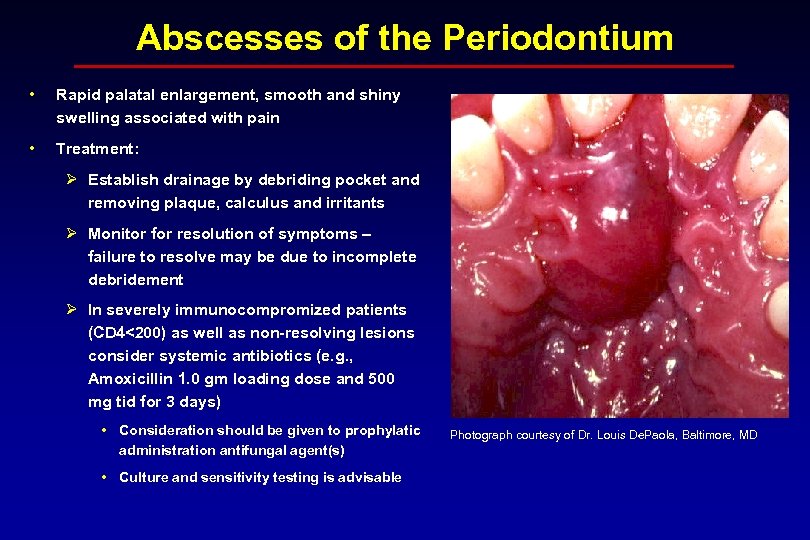 Abscesses of the Periodontium • Rapid palatal enlargement, smooth and shiny swelling associated with pain • Treatment: Ø Establish drainage by debriding pocket and removing plaque, calculus and irritants Ø Monitor for resolution of symptoms – failure to resolve may be due to incomplete debridement Ø In severely immunocompromized patients (CD 4<200) as well as non-resolving lesions consider systemic antibiotics (e. g. , Amoxicillin 1. 0 gm loading dose and 500 mg tid for 3 days) • Consideration should be given to prophylatic administration antifungal agent(s) • Culture and sensitivity testing is advisable Photograph courtesy of Dr. Louis De. Paola, Baltimore, MD
Abscesses of the Periodontium • Rapid palatal enlargement, smooth and shiny swelling associated with pain • Treatment: Ø Establish drainage by debriding pocket and removing plaque, calculus and irritants Ø Monitor for resolution of symptoms – failure to resolve may be due to incomplete debridement Ø In severely immunocompromized patients (CD 4<200) as well as non-resolving lesions consider systemic antibiotics (e. g. , Amoxicillin 1. 0 gm loading dose and 500 mg tid for 3 days) • Consideration should be given to prophylatic administration antifungal agent(s) • Culture and sensitivity testing is advisable Photograph courtesy of Dr. Louis De. Paola, Baltimore, MD
 Periodontal Microflora in HIV+ Patients • No major differences in the microbial composition of periodontal lesions between HIV and non-HIV infected patients • Colonization includes: Ø A. actinomycetemcomitans Ø P. gingivalis Ø P. intermedia Ø F. nucleatum in LGE and NUP • Recovery of human herpes virus types 6, 7, and 8, found in 90% of HIV+ patients Ø Over 2 X higher than in HIV- controls (Mardirossian et al, 1999)
Periodontal Microflora in HIV+ Patients • No major differences in the microbial composition of periodontal lesions between HIV and non-HIV infected patients • Colonization includes: Ø A. actinomycetemcomitans Ø P. gingivalis Ø P. intermedia Ø F. nucleatum in LGE and NUP • Recovery of human herpes virus types 6, 7, and 8, found in 90% of HIV+ patients Ø Over 2 X higher than in HIV- controls (Mardirossian et al, 1999)
 Considerations in the Use of Antibiotics • Preferred use of narrow spectrum antibiotics (e. g. , Metronidazole) to minimize development of antibiotic resistance • Possibility of presence of antibiotic resistant strains Ø Culture and antibiotic sensitivity may be indicated • Use of antibiotics may lead to overgrowth of Candida albicans Ø Antifungal treatment may be indicated in conjunction with systemic antibiotics • Local delivery antibiotics may be useful but have not been evaluated
Considerations in the Use of Antibiotics • Preferred use of narrow spectrum antibiotics (e. g. , Metronidazole) to minimize development of antibiotic resistance • Possibility of presence of antibiotic resistant strains Ø Culture and antibiotic sensitivity may be indicated • Use of antibiotics may lead to overgrowth of Candida albicans Ø Antifungal treatment may be indicated in conjunction with systemic antibiotics • Local delivery antibiotics may be useful but have not been evaluated
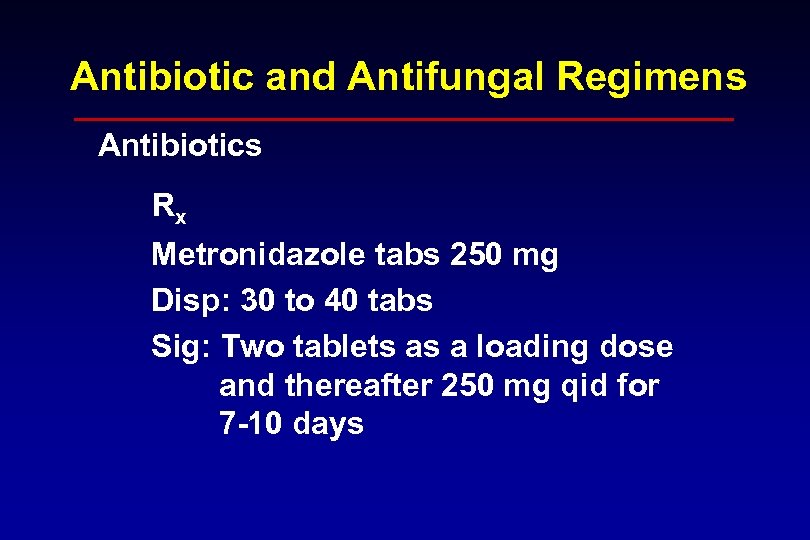 Antibiotic and Antifungal Regimens Antibiotics Rx Metronidazole tabs 250 mg Disp: 30 to 40 tabs Sig: Two tablets as a loading dose and thereafter 250 mg qid for 7 -10 days
Antibiotic and Antifungal Regimens Antibiotics Rx Metronidazole tabs 250 mg Disp: 30 to 40 tabs Sig: Two tablets as a loading dose and thereafter 250 mg qid for 7 -10 days
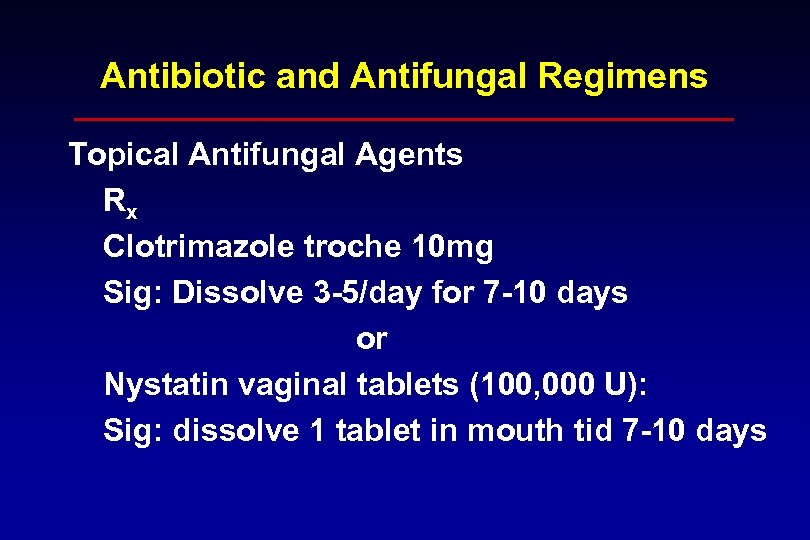 Antibiotic and Antifungal Regimens Topical Antifungal Agents Rx Clotrimazole troche 10 mg Sig: Dissolve 3 -5/day for 7 -10 days or Nystatin vaginal tablets (100, 000 U): Sig: dissolve 1 tablet in mouth tid 7 -10 days
Antibiotic and Antifungal Regimens Topical Antifungal Agents Rx Clotrimazole troche 10 mg Sig: Dissolve 3 -5/day for 7 -10 days or Nystatin vaginal tablets (100, 000 U): Sig: dissolve 1 tablet in mouth tid 7 -10 days
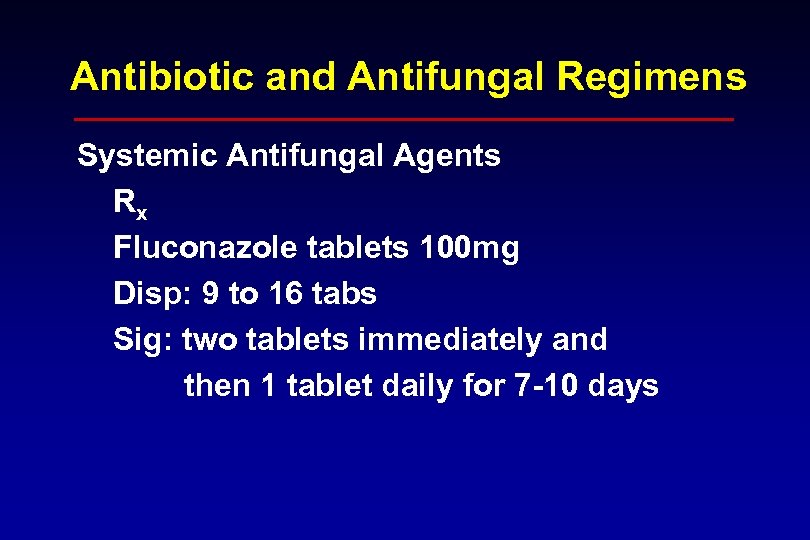 Antibiotic and Antifungal Regimens Systemic Antifungal Agents Rx Fluconazole tablets 100 mg Disp: 9 to 16 tabs Sig: two tablets immediately and then 1 tablet daily for 7 -10 days
Antibiotic and Antifungal Regimens Systemic Antifungal Agents Rx Fluconazole tablets 100 mg Disp: 9 to 16 tabs Sig: two tablets immediately and then 1 tablet daily for 7 -10 days
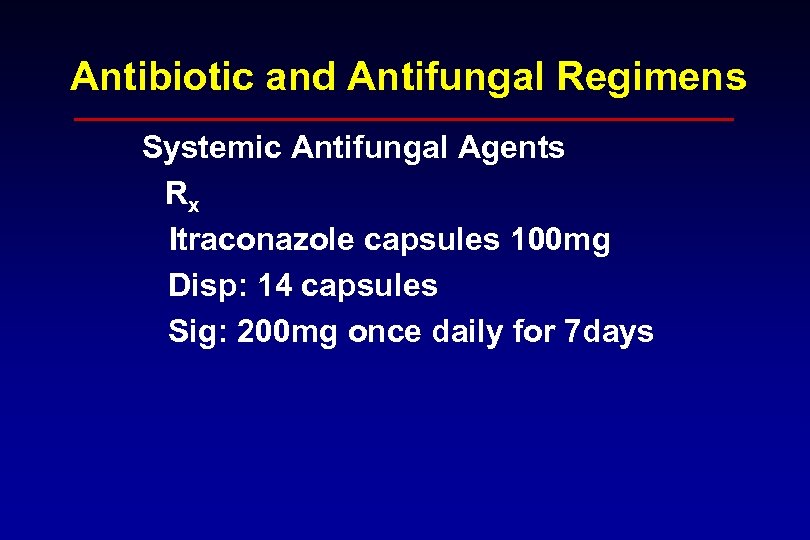 Antibiotic and Antifungal Regimens Systemic Antifungal Agents Rx Itraconazole capsules 100 mg Disp: 14 capsules Sig: 200 mg once daily for 7 days
Antibiotic and Antifungal Regimens Systemic Antifungal Agents Rx Itraconazole capsules 100 mg Disp: 14 capsules Sig: 200 mg once daily for 7 days
 Pediatric Patients • Oral lesions have been reported in HIV+ pediatric populations. The CDC revised the classification system for HIV infection in children <13 years of age to include oral lesions as markers of severity of HIV infection (1994) • Linear gingival erythema has been reported in approximately 10% of HIV+ children exhibit • Periodontal conditions and diseases, such as necrotizing ulcerative gingivitis and periodontitis, have been infrequently described
Pediatric Patients • Oral lesions have been reported in HIV+ pediatric populations. The CDC revised the classification system for HIV infection in children <13 years of age to include oral lesions as markers of severity of HIV infection (1994) • Linear gingival erythema has been reported in approximately 10% of HIV+ children exhibit • Periodontal conditions and diseases, such as necrotizing ulcerative gingivitis and periodontitis, have been infrequently described
 Considerations in Periodontal Therapy • The effects of systemic bacteremia created following Sc/RP have not been studied • The response of HIV+ patients to periodontal surgery has not been studied • The presence of antibiotic resistant oral bacteria has not been evaluated
Considerations in Periodontal Therapy • The effects of systemic bacteremia created following Sc/RP have not been studied • The response of HIV+ patients to periodontal surgery has not been studied • The presence of antibiotic resistant oral bacteria has not been evaluated
 Oral Manifestations in the HAART Era • Overall prevalence of oral infections has changed since introduction of highly active antiretroviral treatment (HAART) • Overall reductions in oral infections from 47. 6% to 37. 5% (Patton et al. , 2000) • Reductions in oral hairy leukoplakia and necrotizing ulcerative periodontitis • Increase in oral warts (Greenspan, 2002) • No change noted for oral candidiasis, oral ulcers, or Kaposi sarcoma
Oral Manifestations in the HAART Era • Overall prevalence of oral infections has changed since introduction of highly active antiretroviral treatment (HAART) • Overall reductions in oral infections from 47. 6% to 37. 5% (Patton et al. , 2000) • Reductions in oral hairy leukoplakia and necrotizing ulcerative periodontitis • Increase in oral warts (Greenspan, 2002) • No change noted for oral candidiasis, oral ulcers, or Kaposi sarcoma
 Web Resources 1. http: //www. hivatis. org. 2. https: //w 3. ada. org/prof/prac/issues/topics/icon trol/ic-recs/index. html. 3. http: //www. hivdent. org/dtc. htm. 4. http: //www. critpath. org/daac/standards. html
Web Resources 1. http: //www. hivatis. org. 2. https: //w 3. ada. org/prof/prac/issues/topics/icon trol/ic-recs/index. html. 3. http: //www. hivdent. org/dtc. htm. 4. http: //www. critpath. org/daac/standards. html
 Resources and Contact Information • • Mark A. Reynolds, D. D. S. , Ph. D. Niki M. Moutsopoulos, D. D. S. University of Maryland Dental School Department of Periodontics 666 West Baltimore Street Baltimore, Maryland 21201 (410) 706 -7152
Resources and Contact Information • • Mark A. Reynolds, D. D. S. , Ph. D. Niki M. Moutsopoulos, D. D. S. University of Maryland Dental School Department of Periodontics 666 West Baltimore Street Baltimore, Maryland 21201 (410) 706 -7152
 References • Classification and diagnostic criteria for oral lesions in HIV infection. ECClearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Immunodeficiency Virus. Oral Pathol Med 1993; 22: 289 -91. • Fauci, AS. The acquired immune deficiency syndrome. The everbroadening clinical spectrum. JAMA 1983 May 6; 249: 2375 -6. • Glick, M. , et al. Necrotizing ulcerative periodontitis: a marker for immune deterioration and a predictor for the diagnosis of AIDS. J Periodontol 1994; 65: 393 -397. • Greenspan, JS. Periodontal complications of HIV infection. Compend Suppl 1994; 18: S 694 -8. • Greenspan D. , Canchola A. , Mac. Phail C, Cheikh B, Greenspan J. Effect of Highly Active Antiretroviral Therapy on Frequency of Oral Warts. Lancet 2002; 357: 1411 -1412. • Horning, GM Necotizing gingivostomatitis: NUG to noma. Compend Contin Educ Dent 1996; 17: 951 -4, 956, 957 -8 • Holmstrup, P. and Glick, M. Treatment of periodontal disease in the immunodeficient patient. Periodontol 2000. 2002; 28: 190 -205.
References • Classification and diagnostic criteria for oral lesions in HIV infection. ECClearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Immunodeficiency Virus. Oral Pathol Med 1993; 22: 289 -91. • Fauci, AS. The acquired immune deficiency syndrome. The everbroadening clinical spectrum. JAMA 1983 May 6; 249: 2375 -6. • Glick, M. , et al. Necrotizing ulcerative periodontitis: a marker for immune deterioration and a predictor for the diagnosis of AIDS. J Periodontol 1994; 65: 393 -397. • Greenspan, JS. Periodontal complications of HIV infection. Compend Suppl 1994; 18: S 694 -8. • Greenspan D. , Canchola A. , Mac. Phail C, Cheikh B, Greenspan J. Effect of Highly Active Antiretroviral Therapy on Frequency of Oral Warts. Lancet 2002; 357: 1411 -1412. • Horning, GM Necotizing gingivostomatitis: NUG to noma. Compend Contin Educ Dent 1996; 17: 951 -4, 956, 957 -8 • Holmstrup, P. and Glick, M. Treatment of periodontal disease in the immunodeficient patient. Periodontol 2000. 2002; 28: 190 -205.
 References • Holmstrup P, Glick M. Treatment of periodontal disease in the immunodeficient patient. Periodontol 2000 2002; 28: 190 -205. • Lamster IB, Grbic JT, Bucklan RS, Mitchell-Lewis D, Reynolds HS, Zambon JJ Oral Dis 1997; 3 Suppl 1: S 141 -8. • Murray, PA. Periodontal diseases in patients infected by human immunodeficiency virus. Periodontol 2000 1994; 6: 50 -67. • Narani N, Epstein JB. Classifications of oral lesions in HIV infection J Clin Periodontol 2001; 28: 137 -45. • Patton LL, Mc. Kaig R, Straauss R, Rogers D, Enron JJ Jr. Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 299 -304. • Parameter on Acute Periodontal Disease. Parameters of Care Supplement J Periodontol May 2000. • Rees, TD. Periodontal Management of HIV-Infected Patients. In MG Newman, HH Takei, FA Carranza (Eds) Carranza's Clinical Periodontology 9 th Edition, Chicago: W B Saunders, 2001.
References • Holmstrup P, Glick M. Treatment of periodontal disease in the immunodeficient patient. Periodontol 2000 2002; 28: 190 -205. • Lamster IB, Grbic JT, Bucklan RS, Mitchell-Lewis D, Reynolds HS, Zambon JJ Oral Dis 1997; 3 Suppl 1: S 141 -8. • Murray, PA. Periodontal diseases in patients infected by human immunodeficiency virus. Periodontol 2000 1994; 6: 50 -67. • Narani N, Epstein JB. Classifications of oral lesions in HIV infection J Clin Periodontol 2001; 28: 137 -45. • Patton LL, Mc. Kaig R, Straauss R, Rogers D, Enron JJ Jr. Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 299 -304. • Parameter on Acute Periodontal Disease. Parameters of Care Supplement J Periodontol May 2000. • Rees, TD. Periodontal Management of HIV-Infected Patients. In MG Newman, HH Takei, FA Carranza (Eds) Carranza's Clinical Periodontology 9 th Edition, Chicago: W B Saunders, 2001.
 References • Robinson PG, Sheiham A, Challacombe SJ, Wren MW, Zakrzewska JM. Gingival ulceration in HIV infection. A case series and case control. study. J Clin Periodontol 1998 Mar; 25: 260 -7. • Robinson PG, Periodontal diseases and HIV infection. Oral Dis 2002; 8 Suppl 2: 144 -50. • Ryder, MI. Periodontal management of HIV-infected patients. Periodontol 2000, 2000; 23: 85 -93. • Ryder, MI. State of the Art: An Update on HIV and Periodontal Disease. J. Periodontol 2002; 73: 1083 -1090. • Tomar SL, Swango PA, Kleinman DV, Burt BA. Loss of periodontal attachment in HIV-seropositive military personnel. J Periodontol 1995 Jun; 66: 421 -8. • Winkler JR, Murray PA, Grassi M, Hammerle C. Diagnosis and management of HIV-associated periodontal lesions. J Am Dent Assoc 1989; Suppl: 25 S-34 S. • Winkler JR, Robertson PB. Periodontal disease associated with HIV infection. Oral Surg Oral Med Oral Pathol 1992; 73: 145 -50. • 1999 International Workshop for a Classification of Periodontal Diseases and Conditions. Annals of Periodontol 1999; 4: 1 -112.
References • Robinson PG, Sheiham A, Challacombe SJ, Wren MW, Zakrzewska JM. Gingival ulceration in HIV infection. A case series and case control. study. J Clin Periodontol 1998 Mar; 25: 260 -7. • Robinson PG, Periodontal diseases and HIV infection. Oral Dis 2002; 8 Suppl 2: 144 -50. • Ryder, MI. Periodontal management of HIV-infected patients. Periodontol 2000, 2000; 23: 85 -93. • Ryder, MI. State of the Art: An Update on HIV and Periodontal Disease. J. Periodontol 2002; 73: 1083 -1090. • Tomar SL, Swango PA, Kleinman DV, Burt BA. Loss of periodontal attachment in HIV-seropositive military personnel. J Periodontol 1995 Jun; 66: 421 -8. • Winkler JR, Murray PA, Grassi M, Hammerle C. Diagnosis and management of HIV-associated periodontal lesions. J Am Dent Assoc 1989; Suppl: 25 S-34 S. • Winkler JR, Robertson PB. Periodontal disease associated with HIV infection. Oral Surg Oral Med Oral Pathol 1992; 73: 145 -50. • 1999 International Workshop for a Classification of Periodontal Diseases and Conditions. Annals of Periodontol 1999; 4: 1 -112.


